Abstract
In recent years, Digital Technologies (DTs) are becoming an inseparable part of human lives. Thus, many scholars have conducted research to develop new tools and applications. Processing information, usually in the form of binary code, is the main task in DTs, which is happening through many devices, including computers, smartphones, robots, and applications. Surprisingly, the role of DTs has been highlighted in people’s life due to the COVID-19 pandemic. There are several different challenges to implement and intervene in DTs during the COVID-19 outbreak; therefore, the present study extended a new fuzzy approach under Hesitant Fuzzy Set (HFS) approach using Stepwise Weight Assessment Ratio Analysis (SWARA) and Weighted Aggregated Sum Product Assessment (WASPAS) method to evaluate and rank the critical challenges of DTs intervention to control the COVID-19 outbreak. In this regard, a comprehensive survey using literature and in-depth interviews have been carried out to identify the challenges under the SWOT (Strengths, Weaknesses, Opportunities, Threats) framework. Moreover, the SWARA procedure is applied to analyze and assess the challenges to DTs intervention during the COVID-19 outbreak, and the WASPAS approach is utilized to rank the DTs under hesitant fuzzy sets. Further, to demonstrate the efficacy and practicability of the developed framework, an illustrative case study has been analyzed. The results of this study found that Health Information Systems (HIS) was ranked as the first factor among other factors followed by a lack of digital knowledge, digital stratification, economic interventions, lack of reliable data, and cost inefficiency In conclusion, to confirm the steadiness and strength of the proposed framework, the obtained outputs are compared with other methods.
Keywords: Hesitant fuzzy sets, Fuzzy decision making, WASPAS, SWARA, Digital technologies, COVID-19 pandemic, Healthcare systems, MCDM
1. Introduction
The world has been challenged since late Dec. 2019 by the novel Coronavirus (COVID-19) detected for the first time in Wuhan, China. It is eventually becoming a pandemic since the number of infected people has rapidly increased, and the world’s leaders have disregarded the COVID-19 pandemic initially [1]. In this regard, the information management systems would be beneficial and impactful to contribute to the during and post COVID-19 outbreak [2]. Meanwhile, DT has a crucial role in decreasing the effects of COVID-19 on people’s life. For instance, many higher education institutions used digital technologies not only to resume their incomplete semester but also to control COVID-19 spreading Longhurst et al. [3] or digital technologies that can ease the communications of people with health workers through social media [4]. Digital Technologies (DT) such as Blockchain Technology (BT), Artificial Intelligence (AI), the Internet of Things (IoT), and big-data analytics would be critical to control and prevention of COVID-19 disease [5]. At the same time, there are interrelationships between all these mentioned digital technologies [6].
There is a growing interest in research in DTs since not only digital technologies develop rapidly, but also digital technologies are an inseparable part of human lives, owing to the ubiquity of computer technologies [7]. Processing information, usually in the form of binary code, is the main task in digital technologies, which is happening through many devices, including computers, robots, smartphones, and applications [8]. To be more specific, a majority of individuals use DTs to acquire and to share Information, upgrade their skills and knowledge, to work remotely, and so on [9]. However, as mentioned, the DTs’ footprint has been highlighted in the people living during the COVID-19 pandemic [10]. Ting et al. [11] researched to find whether DTs can help the healthcare system to deal with the problematic situations stem from the COVID-19 outbreak. The results indicated that DTs could benefit the healthcare system in at least four ways.
Firstly, a platform has been provided based on the Internet of Things (IoT), enabling public-health agencies to access the Information which has been used for observing the COVID-19 progress. For instance, for infected people, disease distribution through countries, and the rate of mortality can be daily checked on the ’World meter’ [11]. Secondly, courtesy of big data, an opportunity has been provided to perform modeling studies of viral status so that regarding this opportunity, the policymakers can enhance preparation for the pandemic. For instance, Wu, Leung and Leung [12] recommended a model based on several cases to forecast the possibility of pandemics in the world. On the other hand, the knowledge of new disease during a pandemic, such as the COVID-19 outbreak, is limited; thus, the level of uncertainty and complexity will be raised, which makes the forecasting model less reliable [13]. However, some scholars proposed precise forecasting models based on small datasets to deal with the uncertainty and complexity of these situations. For instance, Fong et al. [14] designed a machine-learning-based model to forecast the future of the COVID-19 outbreak using a small dataset.
Thirdly, in the field of health education, DTs can update people’s knowledge via communications in various platforms. For example, many healthcare agencies are currently used both Facebook and Twitter to share the real and latest Information and news around COVID-19 with people [11]. Fourthly, AI and deep learning can ease the process of detecting new cases infected by COVID-19, while diagnosing new cases of the disease is a severe challenge due to the cost and accuracy of the tests [15]. On the surface, interventions of DTs have considerable effects on the healthcare system, education system, communications, and especially in dealing with the COVID-19 pandemic.
Although there are several studies in the field of digital health interventions, there are a few previous studies focused on the key challenges and opportunities for adopting the healthcare system with DTs [16]. Regarding this, further studies and analyses are needed to explore the open issues stem from digital health interventions during the COVID-19 outbreak. To be more specific, there is a lack of study in which the challenges of digital health interventions during a disaster such as the COVID-19 pandemic has been evaluated; thus, the present study aims to bridge this research gap. The challenges comprise a wide range of issues, including what and how are the contributions of digital health interventions in dealing with training and awareness issues, economic and health hazard issues, treatment and procurement issues, and health hazard prediction issues.
Furthermore, some challenges can arise worries or even can be considered as threats, including infodemic risk [17], insecure applications [18], unreliable information [19], non-economical interventions [20], digital divide and illiteracy issue [21], and psychological issues [22]. Besides, digital health interventions can provide several opportunities, including creating a health information system [23], application of robots, and AI in the healthcare system, especially the medical diagnosis [24], [25]. According to this wide range of challenges, the present study used the SWOT (Strengths, Weaknesses, Opportunities, Threats) framework to classify the identified challenges based on strengths, weaknesses, opportunities, and threats. SWOT Analysis is a framework having four components, namely ’Strengths,’ ’weaknesses,’ ’opportunities,’ ’threats.’ Furthermore, the two first components are internal factors, while others are external factors.
Furthermore, a new extended fuzzy approach is proposed to rank four DT systems to identify the critical challenges of DT interventions to control the COVID-19 outbreak. Fuzzy sets were proposed first by Zadeh (1965) to deal with uncertainty, while it has been using in different fields by scholars since then [26]. Besides, multi-criteria decision making (MCDM) approaches could deal with the real-world issues effectively which include a wide variety of methods, including Analytic Hierarchy Process (AHP), Technique for Order Preference by Similarity to Ideal Solution (TOPSIS), Stepwise Weight Assessment Ratio Analysis (SWARA), and Weighted Aggregated Sum Product Assessment (WASPAS), and many other methods [27]. At present, the Hesitant Fuzzy Sets (HFSs) are proven as a potential structure to express the uncertainty and vagueness that eventually accessible in real-life complex MCDM problems [28], [29], [30], [31]. Because of its unique advantages, several authors have focused their attention on the development of new theories and methods related to HFSs. Driven by the richness of HFSs, the present paper explores within the context of HFSs.
It is evident from the earlier researches that there has been no study on developing the integrated decision-making methodology based on SWARA and WASPAS approaches with hesitant fuzzy information.
Besides, there has been no work in the literature regarding the proposed hesitant fuzzy-SWARA–WASPAS (HF-SWARA–WASPAS) framework in the assessment of digital health interventions during the COVID-19 outbreak. To the best of author’s knowledge, this is the first study that presents an integrated HF-SWARA–WASPAS methodology based on SWARA and WASPAS methods under the HFSs environment. In this methodology, the SWARA approach is utilized to derive the subjective criteria, which is more consistent and has a simple calculation procedure than other weight-determination approaches. Furthermore, the WASPAS method provides easy computational steps with accurate and consistent results in the assessment of digital health interventions in the COVID-19 outbreak. The contributions of this work are explained as follows:
-
•
A novel fuzzy approach under the HFS approach is developed to tackle complex MCDM problems.
-
•
A new HF-SWARA–WASPAS approach is introduced to evaluate the key challenges of digital health using the SWOT framework.
-
•
SWARA procedure is utilized to determine the digital health interventions in dealing with the COVID-19 outbreak.
-
•
WASPAS approach is used to rank the DT systems during the COVID-19 outbreak.
-
•
A survey study using interviews and literature has been carried out to identify the challenges of digital health interventions during the COVID-19 pandemic.
-
•
A new SWOT framework is developed to classify the challenges into ’Strength,’ ’weaknesses,’ ’opportunities,’ and ’threat.’
-
•
An empirical study is considered to prove the potentiality and usefulness of the proposed method within HFSs. The steadiness and strength of the introduced approach are analyzed through comparative analysis.
The rest part of this study is arranged as follows: Section 2 presents a comprehensive review of digital health interventions, and it presents the outputs of the SWOT analysis. Next, the methodology of the research is discussed in Section 3, and a literature review around hesitant fuzzy sets, SWARA, and WASPAS methods is presented in this section. Section 4 develops the new extended hesitant fuzzy-SWARA–WASPAS approach. The outcomes of the research and a comparative analysis are discussed in Section 5. An overall conclusion and some research avenues for future work are presented in Section 6.
2. Literature review
2.1. The theoretical background of DTs intervention in healthcare
The advent of technology has dramatically influenced human lives and their communities. As mentioned, DTs comprise a wide range of technologies that Information and Communication Technology (ICT) systems, owing to their rapid advancing and multi-functionality, have the potential for severe impact. ICT systems include computers, cellular devices, and personal digital assistants [32]. Besides, many companies utilized DTs and network communications and communications widely. At the same time, technology plays a crucial role in forecasting a natural disaster such as earthquakes, eruptions, hurricanes, floods, tsunami, and disease pandemic, such as COVID-19 pandemic, and it can recommend the way to deal with these disasters [25].
In the healthcare system, the quality and the coverage of health services and practices can be enhanced in the light of DTs since they provide many opportunities to cope with healthcare issues [33]. As a result, DT interventions may be utilized to ease interaction with people to extend contact coverage and to generate demand. Also, they may be used to help health workers to gain Information about clinical protocols immediately through telemedicine consultations or decision-support systems. Put simply, DTs can improve the quality of healthcare system services in different ways, while these technologies have been evolved owing to their dynamic nature [33]. Furthermore, the World Health Organization (WHO) defined the digital health intervention as a distinct performance of DTs that are employed for health purposes. On top of that, it can be applied via digital health application and information and communication technology systems, including a vast variety of communications channels such as social media or messengers [33].
Several interventions are extended to boost medication adherence, while these might be ineffective or unsuccessful [34]. To be more specific, some interventions, such as recording information, counseling, and digital-based personal connection, are more successful in comparison with long-term interventions such as employing robots in the healthcare system [35]. Besides, digital interventions can decrease the amount of time consumed by the healthcare system so that scholars have shown interest in digital interventions that save loads of time [36]. Furthermore, some digital interventions, especially the applications, are currently accessible for medication adherence so that people utilized them in the field of medication diaries, medication reminders, and medication instructions [37]. These applications are likely emphasized on nonintentional adherence so that they are concerned about the individual patient in preference to the interaction between health care professionals and patients [35].
There are several studies in which digital health interventions have been investigated. Gagnon et al. [38] conducted a holistic review to evaluate the efficacy of ICT intervention in healthcare practices. The outputs of research showed a positive effect in adopting ICT with the healthcare system. Wu et al. [39] conducted review research to investigate the ICT interventions in clinical communications, and to find out how these interventions can boost clinical communication within hospitals. De Lima et al. [40] studied the efficacy of ICT interventions for supporting antiretroviral cure in mature with Human Immunodeficiency Virus (HIV). Outputs showed that the application of ICT in the healthcare system could make care more accessible. Anand et al. [41] evaluated the role of digital interventions in altering diet and in improving physical activity Myocardial Infarction (MI) risk within the South Asian population.
Morton et al. [42] investigated the benefits and drawbacks of the application of ICT interventions for decreasing blood pressure, and to find out the best process of identifying both advantages and disadvantages of ICT interventions in this field. Besides, a few research has conducted during the COVID-19 pandemic; for example, Lakshmiprabha and Mahalakshmi [43] did assess the contribution of DTs to control the COVID-19 outbreak in India. The results indicated that DTs could improve the process of monitoring the patients, and they can ease communications among patients and health workers. Golinelli et al. [4] conducted a quick review to identify which digital health interventions can be better solutions for dealing with the COVID-19 pandemic. The results showed that AI is an appropriate technology for medical diagnosis, while social media is useful for surveillance measures and prevention. Hernandez-Orallo et al. [44] investigated the role of smartphones in reducing COVID-19 spreading. To this end, an epidemic model was proposed to assess the cost and efficiency of the measures.
2.2. SWOT analysis
As mentioned, the identified challenges are classified on strengths, weaknesses, opportunities, and threats based on the SWOT framework. In the following, all four classifications and their sub-components are presented in detail.
2.2.1. Strengths
Digital treatment
DTs, especially robotics, mobile application, and thermal imaging via AI, can be utilized for different purposes, including self-assessment for COVID-19, information circulation through social media, and identifying infected people [45], [46]. For instance, a mobile application named BlueDot is used to trace infected people in India, which works based on big data, machine learning, and AI [25]. Therefore, it is believed that DTs can bear out medical cures and boost them.
Awareness & training
As mentioned, DTs in the form of different platforms such as online learning portals, social media, and websites can boost awareness of people around COVID-19 news [20]. On top of that, many universities and institutions are utilizing DTs to resume their programs remotely [47]. Besides, Zaman et al. [48] mentioned that DTs, especially in the form of social media, provide Information around COVID-19 pandemic in various ways, including training of preventing measures, online education, data visualization, and monitoring healthcare system. Therefore, DTs’ health interventions not only can increase social awareness around the COVID-19 pandemic but also can train people and health workers to deal with problems stemming from the COVID-19 pandemic.
Health hazard prediction
ICT interventions can benefit people in the field of hazard mapping and epidemic and pandemic prediction through data analytic and AI [49]. For instance, Zlatanova and Fabbri [50] integrated ICT with GIS to provide a risk map, and hazard map, and Zhong and Xiao [51] proposed a framework based upon ICT to enhance health prediction through big data and deep learning. Therefore, health hazard prediction is one of the invaluable strengths of ICT interventions having a significant role in controlling the COVID-19 outbreak [52].
Non-virtual support
DTs can help the healthcare system physically apart from their virtual support. Put simply, DTs in the form of drones, modern robots, and 3D Printers can improve the humanitarian supply management and logistics and medical transportation during COVID-19 outbreak [53], [54]. Also, Tavakoli, Carriere and Torabi [55] conducted a research to find how robots can help health workers by providing this opportunity to triage and monitor patients’ symptoms from a safe distance, and to investigate the application telehealth and telepresence technologies in healthcare service delivery during COVID-19 pandemic. Therefore, it is believed that DTs can assist health workers so that face-to-face interaction will be reduced [56]. On top of that, robots can be employed in the healthcare system in forms of nurses, receptionists, serving robots, telemedicine robots, cleaning and spraying robots, and surgical robots [24].
Medicine development
DTs can be used to discover new drugs and vaccines in the form of biotechnical platforms. As a result, digital interventions can boost the progression in a different step of drug development, while they can optimize the process of drug designing through advanced analytics and algorithms [57]. Furthermore, Zaman et al. [48] mentioned that over 30% of participants in the research believe that in the light of AI and epidemiological analysis and Genome sequencing, the process of detecting infected people can be performed more precisely so that discovering vaccines and drugs for controlling COVID-19 will be more achievable.
Economic interventions
A majority of economists have mentioned that economic status has directly or indirectly affected by DTs, especially ICT [58]. Besides, DTs are mean of crisis prediction so that the economic crisis can be controlled through this ability. To be specific, DTs can visualize economic effects using data analytic tools. On top of that, it is believed that countries can bring back economic sustainability to their businesses after COVID-19 through ICT economic interventions [59].
2.2.2. Weakness
Lack of reliable data
A large amount of information is accessible in ICT domains such as social media and website. At the same time, a majority of individuals have propagated unreliable Information on the internet, primarily social media [19]. Besides, all the participants in a research conducted by Zaman et al. [48] mentioned that the critical weakness of ICT health interventions is the lack of reliable data in the ICT domains so that during the COVID-19 pandemic, it is necessary to hinder infodemic through data validation.
Mock Information
One of the biggest problems in the field of crisis management is controlling unauthentic Information, misleading both individuals and medical personnel [60]. Also, the authenticity of data is considered as one of the weaknesses of ICT health interventions during COVID-19 pandemic Zaman et al. [48] since the unauthentic Information on the COVID-19 pandemic have circulating fast among people being rooted in myths and pretended cures [61].
Cost inefficiency
A massive amount of time, energy, and money are required to employ DTs in different fields, including the healthcare system, education system, and supply chain management. Also, the cost-efficiency in developing countries and the least developed countries is a vital factor [20]. For example, two types of costs should be considered in online education, including the cost of online education technologies and the cost of distributing and receiving knowledge through the internet [62].
Lack of digital knowledge
Digital literacy aids people in getting knowledge easy and fast through advanced technology. At the same time, they need to boost their technical skills to take full advantage of DTs in their daily works [63]. However, individuals who do not have enough digital knowledge cannot benefit from digital systems created by different companies for controlling the COVID-19 pandemic [64].
Digital divide
Many areas in the world are deprived of the internet and limited resources so that the digital divide is considered as another weakness of digital health interventions [21]. Also, the digital divide has increased due to the rapid applications of DTs during the COVID-19 outbreak. However, the demand for DTs saw an increase in response to the COVID-19 [65].
Insecure applications
The governments have managed to use big data and tracing applications to trace movements of people during the COVID-19 pandemic so that people may be concerned about a lack of privacy [65]. The trace application has raised privacy concerns since service providers should store users’ data on their central servers [18]. Besides, over half of participants in Zaman et al. [48] specified that the lack of security is one of the significant weaknesses observed in artificial intelligence and mobile applications.
2.2.3. Opportunities
Accurate prediction system
It is believed that countries can use data analytic and artificial intelligence to predict the imminent epidemic precisely [66]. Besides, it is vital to identify the main reasons for the epidemic and the bad sectors leading into pandemic such as COVID-19, so that countries can employ DTs to perform the identification processes more effectively [67], [68]. For instance, Ogundokun and Bamidele [66] used a neural network, linear regression, and support vector regression to predict COVID-19 disease precisely, or Dur-e-Ahmad and Imran [69] used a dynamic transmission model to predict the number of infected people during the COVID-19 in the five countries.
Automatization of healthcare
There is a growing interest in the application of automation and robots in the healthcare system. Also, robots can boost the efficiency of healthcare practices, since not only do they reduce the workload of medical staff and physicians, but also aid them to cope with problematic situations more precisely [24]. Besides, Zaman et al. [48] specified that over 90% of participants in their research believed that “Robotic Process Automation (RPA)” can be considered as an opportunity to save loads of time and cost, and perform the repetitive processes behalf humans. Therefore, RPA enables medical staff and health workers to treat patients precisely so that it has a crucial role in controlling the COVID-19 pandemic.
Health information systems (HIS)
Health Information Systems (HIS) are considered as the interplay among the technologies, individuals, and processes to bear out practices and management in delivering vital information to boost the quality of healthcare performance [23]. Health information systems comprise health informatics, health information technology, and electronic medical records. Besides, the risk of social system collapse would be reduced during the COVID-19 pandemic if accessing the secured personal health record was maintained through the Health Information System [70].
Digital health education
Digital health applies ICT in health services through related internet-based technologies [71]. Surprisingly, some patients are not skillful and willing to utilize digital health services so that there is a necessity to educate them in digital health care [64]. On top of that, not only how to use digital health services should be thought, but also social engagement about the utilize of digital health services should be provided [72]. Therefore, this pandemic may create a window of opportunity for increasing the level of required knowledge in digital health services.
Digital diagnosis
Obtaining an accurate, swift various diagnosis of the source of human disease is a vital step of diagnostic medicine, specifically in viral infections, to boost the delivery of healthcare services [73]. Besides, a majority of COVID-19 diagnosis methods that are currently used are sluggish in nature, prolonging the pandemic period. Therefore, the application of ICT in medical diagnosis is another opportunity for ICT health interventions can be employed in the same situation as the COVID-19 pandemic in the future [74]. For instance, Saiz and Barandiaran [75] applied a deep learning method to detect the COVID-19 through chest X-RAY Images. Their findings indicated that the introduced model achieved a high sensibility and specificity in COVID-19 detection, which makes the proposed model suitable for this purpose.
Research framework in Epidemiology
The most important lesson out of the COVID-19 pandemic is that the world does not have enough preparedness to cope with Coronavirus so that a comprehensive research framework is needed to deal with the COVID-19 and future pandemics [76], [77]. Also, it is believed that genetic analysis could be useful to discover which type of viruses may attack humans affecting the level of preparedness of the healthcare system [78]. Nevertheless, this can only be feasible through a robust collaborative research framework.
2.2.4. Threats
Non-digital interferences
Religions and political organizations may interfere with the rapid and free growth of ICT since there is a dichotomy between their beliefs and political value and DT [79]. As a result, controlling the pandemic may be clumsy and slow, owing to non-cooperative responses of such organizations that have negatively affected the process of data gathering [48].
Infodemic risk
Infodemic is as dangerous as pandemic since fake news and false rumors have significant adverse effects on society. Put simply, the epidemic and infodemic are two sides of a coin in the highly digitalized countries [17]. Besides, the discrepant differences in the data and a massive amount of data have confused people. Therefore, it is difficult for the majority of individuals to verify the trustworthiness and the sources of information [80]. Thus, effective interventions of the health services have threatened by infodemic risk.
Privacy worries
Many tasks have moved online in the light of the COVID-19 pandemic affecting the privacy of people. Although this pandemic is a temporary situation, it has long-lasting impacts on people’s liberty, since a massive amount of health information is needed to control the COVID-19 pandemic [81]. In contrast, this Information is personal so that the expansion of personal information on the internet may have disruptive consequences [82].
Unaffordability
Although the operational cost is improved through the application of DTs, especially the combination of AI and IoT, some scholars believe that it may not be affordable in some cases [56]. Put simply, and it is difficult to reap the advantages of ICT health interventions in some countries during the COVID-19 pandemic, especially underdeveloped and least developed countries, owing to the high cost of infrastructure and development [83]. The patients may stop utilizing ICT based health services, considering the cost-benefit trade-off. Therefore, a cost-effective ICT-based health system is required to deal with the unaffordability threat.
Exacerbation of paranoia
A new type of phobia, namely ”Corona phobia”, has recently generated owing to the COVID-19 pandemic. The main reason for generating this phobia is infodemic, though the application of ICT health interventions may be another reason [22]. For instance, color codes are given to people through color-coded apps to segregate infected people from the rest. As a result, these situations have psychological impacts on people’s minds boosting the exacerbation of paranoia among people [84].
Digital stratification
Considering the wealth of nations, the diffusion rate of digital health services is wary in different nations. The reasons could be related to cost constraints and national policies or commitments. People are divided into different strata based on their social classes affecting the level of accessibility to DTs [21]. Therefore, the digital divide affects digital stratification being a threat to digital health interventions [85].
3. Methodology
As mentioned, this study aims to introduce a new framework to evaluate the challenges of digital health intervention adoption during the COVID-19 outbreak. To this end, firstly, the related literature has been scrutinized to do not only observe the current status of digital health interventions in the world, especially during the COVID-19 pandemic but also to identify the challenges of digital health intervention adoption. Next, a survey study through interviews has been carried out to collect data concerning the identified challenges and alternatives. In this step, the experts have been asked to give their support in assessing the relative significances of attributes and alternatives using linguistic variables (See Table 1, Table 2). The experts were chosen from different expertise, for instance, ICT experts and IT managers. Subsequently, a new extended hesitant fuzzy-SWARA–WASPAS approach (See Section 4) has been proposed to assess the challenges of digital health interventions. At last, a comparative analysis has been conducted to evaluate the performance and robustness of the proposed method in comparison with the HF-COPRAS method.
Table 1.
Performance ratings of the criteria and decision experts.
| LVs | HFNs | Decision experts risk preference |
||
|---|---|---|---|---|
| Pessimist | Moderate | Optimist | ||
| Very high (VH) | [0.85, 1.00] | 0.85 | 0.925 | 1.00 |
| High (H) | [0.70, 0.85] | 0.70 | 0.775 | 0.85 |
| Medium high (MH) | [0.55, 0.70] | 0.55 | 0.625 | 0.70 |
| Medium (M) | [0.40, 0.55] | 0.40 | 0.475 | 0.55 |
| Medium low (ML) | [0.30, 0.40] | 0.30 | 0.35 | 0.40 |
| Low (L) | [0.15, 0.30] | 0.15 | 0.225 | 0.30 |
| Very low (VL) | [0.00, 0.15] | 0.00 | 0.075 | 0.15 |
Table 2.
Linguistic ratings for the significance of criteria and alternatives.
| LVs | HFNs | Decision experts risk preference |
||
|---|---|---|---|---|
| Pessimist | Moderate | Optimist | ||
| Extremely preferable (EP) | [0.90, 1.00] | 0.90 | 0.95 | 1.00 |
| Strong preferable (SP) | [0.75, 0.90] | 0.75 | 0.825 | 0.90 |
| Preferable (P) | [0.60, 0.75] | 0.60 | 0.675 | 0.75 |
| Moderately preferable (MP) | [0.50, 0.60] | 0.50 | 0.55 | 0.60 |
| Moderate (M) | [0.40, 0.50] | 0.40 | 0.45 | 0.50 |
| Moderately undesirable (MU) | [0.30, 0.40] | 0.30 | 0.35 | 0.40 |
| Undesirable (U) | [0.20, 0.30] | 0.20 | 0.25 | 0.30 |
| Strong undesirable (SU) | [0.10, 0.20] | 0.10 | 0.15 | 0.20 |
| Extremely undesirable (EU) | [0.00, 0.10] | 0.00 | 0.05 | 0.10 |
3.1. Hesitant fuzzy sets
The notion of fuzzy sets (FSs) originated by Zadeh [26] has accomplished great success in different areas for handling such type of uncertainty. In several real-life examples, it is not an easy task to express the membership function of an FS due to increasing complexity, time boundedness, the vagueness of the human mind, and many other reasons. To deal with this issue, Torra [86] initiated the notion of the Hesitant Fuzzy Set (HFS), which permits the membership degree of an element to a given set, having a few different values. Torra [86] also conferred the associations between HFS and extended form of FSs, which are intuitionistic fuzzy set (Atanassov [87]), type-2 fuzzy set [88], [89] and fuzzy multi-set (Yager [90]). As the extension of FSs, HFSs have proven as accessible and useful tools to portray the imprecise and vague information that occurred in real-life applications.
Due to the effectiveness of HFS in dealing with human hesitancy, many theories and applications have been introduced under the HFSs context [28], [31], [91], [92]. For example, Xu and Zhang[93] suggested the hesitant fuzzy TOPSIS model for solving MCDM problems with HFSs. Farhadinia [94] recommended the methodical transformation of the entropy into the similarity measure for HFSs and interval-valued hesitant fuzzy sets. Liao and Xu [95] designed a novel interactive technique to solve the MCDM problems with hesitant fuzzy (HF) information.
Next, Thakur, Thakur, Singh and Engineering [96] proposed some new aggregation operators for HFSs. Ashtiani and Azgomi[97] suggested an innovative hesitant fuzzy-based computational trust model deal with the vagueness and hesitancy of trust MCDM problems. Faizi et al. [98] pioneered a new hesitant fuzzy-based Characteristic Objects Method to tackle the group decision-making problems. Lan, et al. [99] studied a novel MCDM model based on priority degrees for HFSs. Alcantud and Giarlotta [100] designed a hybrid hesitant fuzzy decision-making model based on necessary and possible preferences. Aktas and Kabak [101] suggested an integrated framework based on the combination of HF-AHP and HF-TOPSIS approaches for the evaluation of solar power plant location sites. Hussain and Yang [102] introduced HF-entropy measures based on the Hausdorff Metric and applied them to construct an MCDM framework with HF-information. Mishra, Rani and Pardasani [103] developed the HF-COmplex PRoportional ASsessment (COPRAS) methodology based on Shapley’s function to cope with the service quality selection problem within the HFSs context. Xu and Zhang [104] summarized the applications of HF-group decision making into three categories: theory, support, and methods. Mishra, et al. [105] evaluated the green supplier selection problem under the HFSs environment by employing the HF-WASPAS method. Wang [106] considered the aggregation of HF-similarity measures and then developed the synthetical similarity formula. Lalotra and Singh [107] developed the axiomatic definition of HF-knowledge measure and presented an equation between the HF-knowledge and HF-entropy measures.
3.1.1. SWARA method
Keršuliene, Zavadskas and Turskis [108] pioneered the concept of the SWARA approach to calculate the subjective weights of the criteria weights during the MCDM process. This approach has an easy calculation procedure and high consistency as compared to other weight-determining approaches such as AHP and Best Worst Method (BWM). Just a while ago, many scholarly articles have combined the SWARA and several other MCDM methods for estimating the criteria importance degrees and ranking the alternatives, respectively. For instance, Rani and Mishra [109] designed a combined SWARA and VIKOR based framework under single-valued neutrosophic sets (SVNSs) context and then employed to evaluate and choose desirable eco-industrial thermal power plant. Their outcomes indicated that the introduced framework is well consistent and more efficient in comparison with other frameworks developed based on SVNSs. On top of that, the stability of the proposed framework concerning the various set of criteria weights has been approved through sensitivity analysis, and it is concluded that their framework can tackle the problems with indeterminate and inconsistent information.
Further, Mishra et al. [110] presented an intuitionistic fuzzy MCDM method by integrating SWARA and COPRAS techniques for evaluating bioenergy production technology options. The results indicated that there is an excellent conformity between the proposed method and with IF-WASPAS. Furthermore, not only the calculations of the proposed are simple, but also it can determine the realistic criteria weight through a simple procedure, which makes the proposed method more stable. Rani et al. [111] developed a combined SWARA and VIKOR based methodology to assess and choose the most appropriate solar panel alternative with PFSs. The findings concluded that their methodology is more useful, robust, and practical in comparison with PF–TOPSIS. On top of that, the tangible sub-criteria can be enumerated successfully using the proposed method, and the significant degree of the decision experts can be estimated correctly and without any modification through the proposed method.
3.1.2. WASPAS Method
With the increasing complexity and wide-spread changes in today’s environment, several authors have focused their attention on the development of new MCDM methods. The WASPAS (Weighted Aggregated Sum Product Assessment) method pioneered by Zavadskas et al. [112], is a utility degree-based technique that has been widely employed in numerous real-life MCDM problems. It is an integration of the Weighted Sum Model (WSM) and Weighted Product Model (WPM); hence, it is more accurate than WSM and WPM. The classical WASPAS technique has been employed for different purposes [113], [114].
A hybrid methodology based on AHP-WASPAS approaches with FSs were introduced by Turskis et al. [115]. The results indicated that the proposed hybrid method could practically rank the alternatives in the large scale problems concerning the multiple conflicting attributes. Ghorabaee et al. [116] suggested a new WASPAS method for solving MCDM problems within Interval Type-2 Fuzzy Sets (IT2FSs) context. The results indicated that the stability of the proposed method could increase through the combination of the objective and subjective weights. On top of that, the computations of the proposed method in the interval type-2 fuzzy environment are simple, and it can transform the non-beneficial into the beneficial criteria through normalization. Mishra and Rani [117] studied an Interval-Valued Intuitionistic Fuzzy (IVIF)-WASPAS method to evaluate the control management policy for reservoir flood. The findings indicated that their IVIF-WASPAS model is more practical in comparison with the IVIF-VIKOR. Also, the computations of the proposed method in the IVIF environment are straightforward; thus, the proposed method can cope with MCDM issues with IVIF information practically.
Moreover, Deveci, Cantez and Gökaşar [118] initiated a combined WASPAS and TOPSIS based approach for evaluating and choosing a suitable car-sharing station alternative with IT2FSs. The results indicated that the introduced framework could be considered as an MCDM tool that can tackle selection issues involving uncertainty and inconsistency. Also, the robustness of the proposed method has been shown in comparison with IT2F-TOPSIS and IT2F-WASPAS. Mishra et al. [105] recommended the HF-information measures based WASPAS methodology for evaluating the green supplier selection problem. The outcomes indicated that the developed method is more efficient in comparison with the HF-VIKOR. Also, the proposed method is compatible with other methods developed under the hesitant fuzzy environment; thus, it can deal with group decision-making problems.
Mishra, Singh and Motwani [119] studied an extended WASPAS method for assessing the telephone service providers’ performances within the intuitionistic fuzzy set’s context. Results indicated that the stability of the proposed method is high, owing to its specific method to evaluate the realistic weights. Also, the proposed method is well-consistent with Fuzzy-AHP-ELECTRE and hybrid AHP-DEA model. Rani, Mishra and Pardasani [120] introduced a combined framework by integrating information measures and WASPAS approach with intuitionistic fuzzy type-2 sets and applied to solve the physician selection problem. Results indicated that a combination of the objective and subjective of criteria weights could boost the stability of the proposed method. On top of that, regarding the comparative analysis, the developed approach is compatible with the previous ranking method, such as MABAC under Pythagorean fuzzy sets.
4. Proposed framework
4.1. Preliminaries
This section firstly recalls the basic concepts related to HFSs.
Definition 4.1 [86] —
Suppose be a fixed set. An HFS on is a function that maps each element of to a subset of .
For better understanding, Xia and Xu [94] defined the mathematical expression of HFS, presented as
| (1) |
where is a set of some values in , which presents the possible belongingness degrees of an element to the set . Xia, and Xu [94] defined the hesitant fuzzy element (HFE), given by . Here, and describe the terms of and a total number of terms in , respectively.
Definition 4.2 [86], [121] —
Let and be a real number. Then the following operational laws are defined:
(i) ,
(ii) ,
(iii) ,
(iv) ,
(v) ,
(vi) ,
(vii) .
Definition 4.3 [94] —
Let be an HFE. Then, the score value and variance function of are presented as
(2)
(3) Based on and , a systematic procedure is derived as follows:
If , then
If ,then
if , then
if , then .
Definition 4.4 [121], [122] —
Consider a set of HFEs , then the Hesitant Fuzzy Weighted Averaging (HFWA) and Hesitant Fuzzy Weighted Geometric (HFWG) operators are defined as
(4)
(5)
Definition 4.5 [103] —
Suppose that . Then, an entropy measure for HFS is given as
(6)
4.2. New extended hesitant fuzzy-SWARA-WASPAS approach
This section pioneers an integrated decision-making model based on SWARA and WASPAS approaches with HFSs and named as hesitant fuzzy WASPAS (HF-SWARA–WASPAS). For the development of the HF-SWARA–WASPAS method, the notions and operations of the HFNs, score function, discrimination measure, SWARA, and WASPAS methods are utilized under the context of HFSs. The procedural steps of an introduced model are given as follows:
Step 1: Originate the option and criteria
A set of decision experts (DEs) determines the sets of options and criteria , respectively. Because of the vagueness of the human’s mind, imprecise knowledge, and lack of data about the options, the decision experts allocate HFNs to evaluate his/her decision on option concerning the criteria .
Step 2: Determine crisp decision experts’ weights
To find the decision experts’ weights, firstly, the importance degrees of the decision experts are assumed as linguistic terms (LTs) and then expressed by HFNs. For evaluation of th decision expert, let is the HFN, then the procedure for evaluating th decision expert’s weight is as
| (7) |
Here, and .
Step 3: Aggregate the HF-decision matrices
To find the aggregated HF-decision (AHF-D) matrix, HFWA operator given by Eq. (4) is applied and then , ,, where is the AHF-D matrix and
| (8) |
Step 4: Evaluating the criteria weights using SWARA approach
The procedure for evaluating the relative weights of the criteria using the SWARA method is presented in the following steps:
Step 4-A Find the score degrees of HFEs by using Eq. (2).
Step 4-B: Determine the criterion ranking order. According to DE’s choice, all criteria are arranged from the best to the slightest essential degrees of criteria.
Step 4-C: Assess the degree of comparative importance. The comparative importance is evaluated from a criterion which is mentioned at the 2nd-position, and succeeding importance degree is determined to compute the difference of criteria placed th and positions, respectively.
Step 4-D: Evaluate the coefficient as Eq. (9)
| (9) |
wherein denotes the comparative importance of score degree [108].
Step 4-E: Compute the weight by using
| (10) |
Step 4-F: Compute the relative weights
| (11) |
Step 5: Compute the normalized AHF-D matrix
In order to normalize the AHF-D matrix , , into , the formula is as follows:
| (12) |
where and describe the benefit and non-benefit criteria sets, respectively.
Step 6: Determine the degrees of weighted sum and product models
The relative significance degree of th option as the sum or additive aggregation measure, called as WSM, is evaluated as
| (13) |
where denotes the weight of a criterion, .
On a similar line, the relative significance degree of th option as product aggregation measure, known as WPM, is calculated by
| (14) |
Step 7: Evaluate the WASPAS measure
The aggregated significance degree is computed by integrating WSM and WPM, and the formula is given as
| (15) |
Wherein the parameter denotes the aggregation decision coefficient, which computes the degree of exactness of WASPAS measure (when , then WASPAS converts to WPM and when , then WASPAS converts to WSM). It has been examined that the accuracy and consistency of the WASPAS method are higher than the WSM and WPM.
Step 8: Arrange the options as per their preference order and find the optimal one.
5. Results
Table 1, Table 2 express the Linguistic Variables (LVs) and their corresponding hesitant fuzzy numbers (HFNs) for the evaluation of relative significances of the criteria/attributes and the alternatives during the given MCDM process, respectively. Due to imprecise knowledge, the uncertainty of the human mind, restriction of time, and qualitative nature of chosen criteria, it is easy for the decision experts to articulate their opinions based on LVs [105].
Assume that the decision experts’ weights are presented as {H, MH, M}. Now, to find the crisp form of decision experts’ weights, we have utilized Table 1 and Eqs. (6)–(7) and attained as . The individual decision opinions are given by the decision experts’ : k 1, 2, 3 are presented in Table 3. Further, with the use of Table 3 and Eq. (8), we have created the AHF-D matrix in Table 4.
Table 3.
Linguistic values for criteria performance given by DEs.
| Criteria | Symbol | DEs | ||||
|---|---|---|---|---|---|---|
| Digital treatment | MP | M | MU | MP | ||
| M | MU | P | MU | |||
| P | MP | M | P | |||
| Awareness & training | P | MP | M | P | ||
| P | U | MU | P | |||
| M | P | M | P | |||
| Health hazard prediction | MP | MU | MP | MP | ||
| SP | MP | P | M | |||
| P | U | MU | P | |||
| Non-virtual support | U | M | M | P | ||
| MP | SP | MU | M | |||
| M | P | M | P | |||
| Medicine development | M | MU | U | M | ||
| M | U | P | MU | |||
| MP | MU | U | U | |||
| Economic interventions | M | M | M | MP | ||
| SP | M | MU | M | |||
| M | SU | M | SU | |||
| Digital divide | MP | MU | U | U | ||
| M | SU | M | SU | |||
| P | M | SP | P | |||
| Lack of Digital knowledge | MP | P | M | MP | ||
| P | MP | MU | U | |||
| M | M | SP | P | |||
| Cost inefficiency | MU | P | MP | M | ||
| MP | M | SP | SU | |||
| P | SP | P | M | |||
| Mock information | SP | EP | MP | P | ||
| M | P | P | MP | |||
| P | MP | P | M | |||
| Lack of reliable data | MP | EP | SP | M | ||
| SP | MP | MP | MU | |||
| P | MU | U | M | |||
| Insecure applications | P | SP | P | M | ||
| P | MP | P | M | |||
| P | MU | U | M | |||
| Accurate prediction system | MP | MP | P | MU | ||
| MU | M | M | MP | |||
| M | P | MU | P | |||
| Automatization of Healthcare | MP | P | M | SP | ||
| P | MP | MP | MP | |||
| SP | P | MU | M | |||
| Research framework in Epidemiology | U | P | M | P | ||
| SP | SP | SP | M | |||
| M | MU | P | MP | |||
| Digital health education | M | P | MU | P | ||
| SP | P | MU | M | |||
| M | MU | P | MU | |||
| Digital diagnosis | M | P | MU | MU | ||
| M | MU | P | P | |||
| P | MU | M | P | |||
| Health information systems (HIS) | U | MP | MP | P | ||
| MU | MP | MU | U | |||
| P | MU | U | SU | |||
| Non-digital interferences | MP | M | M | P | ||
| SP | MP | M | M | |||
| M | SP | P | M | |||
| Digital stratification | U | MU | MU | P | ||
| MU | P | MP | MU | |||
| MU | MU | MU | M | |||
| Privacy worries | MP | P | MU | MU | ||
| P | P | U | M | |||
| M | U | P | MP | |||
| Unaffordability | M | P | MU | MU | ||
| MP | MU | P | P | |||
| P | MU | MU | MP | |||
| Exacerbation of paranoia | MU | P | MP | P | ||
| MU | MP | MU | MU | |||
| MP | MU | U | SU | |||
| Infodemic risk | MP | M | MP | P | ||
| P | P | M | MP | |||
| MP | SP | P | M | |||
Table 4.
AHF-D matrix for an option over the criteria.
| Criteria | ||||
|---|---|---|---|---|
| 0.540 | 0.422 | 0.507 | 0.543 | |
| 0.553 | 0.487 | 0.404 | 0.631 | |
| 0.639 | 0.407 | 0.539 | 0.540 | |
| 0.462 | 0.615 | 0.388 | 0.587 | |
| 0.472 | 0.321 | 0.415 | 0.377 | |
| 0.575 | 0.369 | 0.455 | 0.419 | |
| 0.540 | 0.341 | 0.525 | 0.372 | |
| 0.529 | 0.534 | 0.536 | 0.487 | |
| 0.543 | 0.619 | 0.652 | 0.359 | |
| 0.639 | 0.749 | 0.574 | 0.546 | |
| 0.639 | 0.696 | 0.577 | 0.439 | |
| 0.631 | 0.595 | 0.555 | 0.440 | |
| 0.427 | 0.526 | 0.523 | 0.513 | |
| 0.551 | 0.615 | 0.465 | 0.627 | |
| 0.540 | 0.612 | 0.626 | 0.543 | |
| 0.576 | 0.564 | 0.480 | 0.487 | |
| 0.491 | 0.471 | 0.507 | 0.562 | |
| 0.416 | 0.483 | 0.407 | 0.390 | |
| 0.590 | 0.588 | 0.527 | 0.527 | |
| 0.340 | 0.483 | 0.418 | 0.499 | |
| 0.560 | 0.564 | 0.453 | 0.457 | |
| 0.526 | 0.443 | 0.494 | 0.485 | |
| 0.440 | 0.511 | 0.395 | 0.420 | |
| 0.560 | 0.635 | 0.569 | 0.534 |
In Table 5, the score degrees of HFNs are calculated based on experts’ knowledge and experiences. Based on Table 5, the criterion with the utmost significant degree is depicted as the first rank, and the criterion with a less significant degree is mentioned in the last place (see Table 6). Hence, the subjective weights of criteria are computed with the use of Eqs. (9)–(11) and Table 6, and given as:
Table 5.
Criteria Performances in terms of LVs.
| Criteria |
LVs provided by DEs |
DEs gives HFNs |
|||||
|---|---|---|---|---|---|---|---|
| U | MP | P | 0.25 | 0.55 | 0.675 | 0.519 | |
| M | P | P | 0.50 | 0.60 | 0.675 | 0.600 | |
| U | M | M | 0.30 | 0.45 | 0.50 | 0.424 | |
| M | M | P | 0.40 | 0.45 | 0.675 | 0.523 | |
| M | MP | M | 0.45 | 0.55 | 0.60 | 0.540 | |
| P | P | P | 0.6 | 0.675 | 0.675 | 0.657 | |
| U | P | SP | 0.25 | 0.675 | 0.75 | 0.605 | |
| SP | M | SP | 0.75 | 0.45 | 0.75 | 0.677 | |
| P | MP | P | 0.60 | 0.55 | 0.675 | 0.615 | |
| U | P | MP | 0.30 | 0.675 | 0.55 | 0.537 | |
| MP | M | SP | 0.55 | 0.50 | 0.75 | 0.616 | |
| MU | MP | M | 0.40 | 0.55 | 0.50 | 0.492 | |
| U | MP | P | 0.25 | 0.60 | 0.75 | 0.575 | |
| M | P | MP | 0.45 | 0.75 | 0.55 | 0.612 | |
| U | MU | M | 0.30 | 0.30 | 0.40 | 0.337 | |
| U | M | P | 0.25 | 0.45 | 0.75 | 0.525 | |
| M | P | M | 0.45 | 0.75 | 0.45 | 0.587 | |
| P | MP | P | 0.75 | 0.55 | 0.75 | 0.699 | |
| U | M | P | 0.25 | 0.50 | 0.675 | 0.501 | |
| SP | M | SP | 0.75 | 0.40 | 0.75 | 0.667 | |
| P | MP | MP | 0.60 | 0.55 | 0.50 | 0.560 | |
| MU | P | MP | 0.30 | 0.60 | 0.55 | 0.502 | |
| P | MU | SP | 0.60 | 0.35 | 0.75 | 0.596 | |
| MU | M | MU | 0.35 | 0.45 | 0.40 | 0.406 | |
Table 6.
Results obtained by SWARA method.
| Criteria | Crisp degrees | Comparative importance of criteria () | Coefficient () | Recalculated weight () | Weight () |
|---|---|---|---|---|---|
| 0.699 | – | 1.000 | 1.000 | 0.0480 | |
| 0.677 | 0.022 | 1.022 | 0.978 | 0.0469 | |
| 0.667 | 0.010 | 1.010 | 0.968 | 0.0465 | |
| 0.657 | 0.010 | 1.010 | 0.958 | 0.0460 | |
| 0.616 | 0.041 | 1.041 | 0.920 | 0.0442 | |
| 0.615 | 0.001 | 1.001 | 0.919 | 0.0441 | |
| 0.612 | 0.003 | 1.003 | 0.916 | 0.0440 | |
| 0.605 | 0.007 | 1.007 | 0.907 | 0.0435 | |
| 0.600 | 0.005 | 1.005 | 0.902 | 0.0433 | |
| 0.596 | 0.004 | 1.004 | 0.898 | 0.0431 | |
| 0.587 | 0.009 | 1.009 | 0.890 | 0.0427 | |
| 0.575 | 0.012 | 1.012 | 0.879 | 0.0422 | |
| 0.560 | 0.015 | 1.015 | 0.866 | 0.0416 | |
| 0.540 | 0.020 | 1.020 | 0.849 | 0.0407 | |
| 0.537 | 0.003 | 1.003 | 0.846 | 0.0406 | |
| 0.525 | 0.012 | 1.012 | 0.836 | 0.0401 | |
| 0.523 | 0.002 | 1.002 | 0.834 | 0.0400 | |
| 0.519 | 0.004 | 1.004 | 0.831 | 0.0399 | |
| 0.502 | 0.017 | 1.017 | 0.817 | 0.0392 | |
| 0.501 | 0.001 | 1.001 | 0.816 | 0.0392 | |
| 0.492 | 0.009 | 1.009 | 0.809 | 0.0388 | |
| 0.424 | 0.068 | 1.068 | 0.757 | 0.0363 | |
| 0.406 | 0.018 | 1.018 | 0.744 | 0.0357 | |
| 0.337 | 0.069 | 1.069 | 0.696 | 0.0334 |
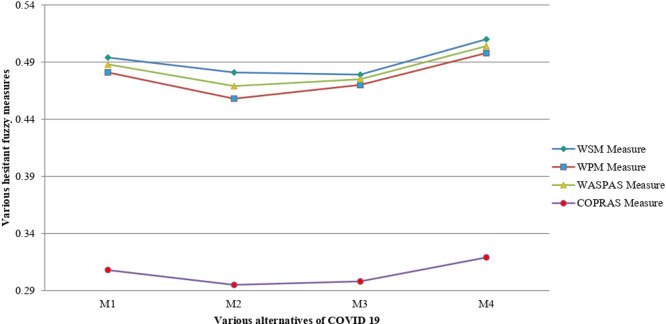
With the help of Table 4 and Eq. (12), the normalized AHF-D matrix is determined and shown in Table 7. By employing Table 7 and Eqs. (13)–(14), the degree of addition and product aggregation measures are evaluated. Next, by using Eq. (15), the HF-WASPAS measure (with ) is evaluated and shown in Table 8. According to Table 8, the preference ordering of the options is obtained as , therefore, is the best alternative.
Table 7.
Normalized AHF-D matrix for an alternative over criteria.
| Criteria | ||||
|---|---|---|---|---|
| 0.540 | 0.422 | 0.507 | 0.543 | |
| 0.553 | 0.487 | 0.404 | 0.631 | |
| 0.639 | 0.407 | 0.539 | 0.540 | |
| 0.462 | 0.615 | 0.388 | 0.587 | |
| 0.472 | 0.321 | 0.415 | 0.377 | |
| 0.425 | 0.631 | 0.545 | 0.581 | |
| 0.460 | 0.659 | 0.475 | 0.628 | |
| 0.471 | 0.466 | 0.464 | 0.513 | |
| 0.457 | 0.381 | 0.348 | 0.641 | |
| 0.361 | 0.251 | 0.426 | 0.454 | |
| 0.639 | 0.696 | 0.577 | 0.439 | |
| 0.369 | 0.405 | 0.445 | 0.560 | |
| 0.573 | 0.474 | 0.477 | 0.487 | |
| 0.449 | 0.385 | 0.535 | 0.373 | |
| 0.540 | 0.612 | 0.626 | 0.543 | |
| 0.576 | 0.564 | 0.480 | 0.487 | |
| 0.509 | 0.529 | 0.493 | 0.438 | |
| 0.416 | 0.483 | 0.407 | 0.390 | |
| 0.410 | 0.412 | 0.473 | 0.473 | |
| 0.340 | 0.483 | 0.418 | 0.499 | |
| 0.440 | 0.436 | 0.547 | 0.543 | |
| 0.474 | 0.557 | 0.506 | 0.515 | |
| 0.560 | 0.489 | 0.605 | 0.580 | |
| 0.440 | 0.365 | 0.431 | 0.466 |
Table 8.
Degree of various alternatives by HF-SWARA–WASPAS method.
| Options | HF-WSM () | HF-WPM () | HF-WASPAS () | Ranking |
|---|---|---|---|---|
| 0.494 | 0.481 | 0.488 | 2 | |
| 0.481 | 0.458 | 0.469 | 4 | |
| 0.479 | 0.470 | 0.475 | 3 | |
| 0.510 | 0.498 | 0.504 | 1 |
5.1. Comparison with HF-COPRAS method
In this section, we applied the HF-COPRAS method proposed by Mishra, Rani and Pardasani [103] to solve the above-discussed MCDM problem and compared it with the proposed HF-SWARA–WASPAS framework.
Steps 1-4: Similar to the HF-SWARA–WASPAS method
Step 5: Sum of the cost-type and benefit-type criteria values
In this step, each alternative is articulated with the addition of values for benefit-type criterion , and cost-type criterion , respectively, which means optimization evaluations are maximization and minimization, respectively and defined as
Let be a benefit-type criterion set, the higher degrees of which are better. Then, the benefit-type criterion , degree for each alternative is given as
| (16) |
Let be cost-type criteria set, the lesser degrees of which are superior. The cost-type criterion , degree for each alternative is described as
| (17) |
In formulae (16), (17), is the number of beneficial criteria, and n is the whole criteria.
Step 6: Assess the relative degree of option
To compute the relative degree of each option, the formula is presented below:
| (18) |
where and present the score degrees of and , respectively.
Step 7: Create a priority degree of alternatives
Remember that the priority degree of alternatives is specified considering the relative values of available options. The maximum relative value of alternative is ranked as a higher priority; as a result, it can be taken into account as the optimum option.
| (19) |
Step 8: Estimate the utility degree
The utility degree is determined by using the formula
| (20) |
Here, and describe the relative significances of the options given by Eqs. (18)–(19).
Considering the Eqs. (16)–(20), the computational results of the HF-COPRAS method are presented in Table 9.
Table 9.
The computational outcomes of HF-SWARA–COPRAS approach.
| Option | Ranking | ||||
|---|---|---|---|---|---|
| 0.291 | 0.346 | 0.308 | 96.58% | 2 | |
| 0.277 | 0.361 | 0.295 | 92.31% | 4 | |
| 0.256 | 0.332 | 0.298 | 93.26% | 3 | |
| 0.271 | 0.307 | 0.319 | 100.00% | 1 |
Based on Table 9, the ranking order of the options is , and thus, is the best choice. It is clear from Table 8, Table 9 that the desirable choice () is the same as all the developed and existing models. Hence, it is obtained that the proposed HF-SWARA–WASPAS methodology is remarkably consistent with the HF-COPRAS approach (see Fig. 1). In comparison with HF-COPRAS method [106], the proposed methodology is more reliable, well-consistent, and has broader applicability. The main advantages of the proposed approach are listed as follows:
Fig. 1.
Degree of utility for each option over different measures.
-
•
In the proposed approach, the subjective weights of the criteria during the process of digital health interventions are determined by the SWARA technique that makes the proposed framework a more capable, effective, and reasonable model.
-
•
The WASPAS model is the utility based MCDM approach that chooses an alternative that has the highest score (or the maximum utility). While the existing models, which are compromising models, choose an alternative that is closest to the ideal solution.
-
•
The WASPAS, integration of the WSM and WPM, is one of the robust new MCDM utility determining methods. The accuracy of this method is more consistent than WPM and WSM.WASPAS enables us to attain the highest accuracy of estimation, applying the suggested methodology for optimization of weighted aggregated function.
-
•
The WASPAS method has the potential to involve the decision experts’ opinions into decision-making practices, while the COPRAS approach is unable to do so. In comparison with the COPRAS method, the WASPAS approach has fewer mathematical steps, well-consistent, and straightforward in terms of analysis and implementation.
-
•
The introduced methodology could provide a more precise explanation under uncertain conditions because of computing the criteria and decision-makers’ weights and applying them in the procedure of the developed framework. Besides, two other considered as central features in the process of the developed framework lead the computational results to a reliable solution. These features include the last aggregation method to avoid the loss of data and to tailor the proposed approach based on HFSs Information.
6. Conclusion
In this work, we have introduced a new decision-making model by integrating SWARA, and WASPAS approaches with HFSs. In the proposed framework, the HF-SWARA method has been utilized to weigh the criteria for DT intervention to control the COVID-19 outbreak. In addition, the WASPAS method has been employed to rank the DT systems. The comparative study has been discussed to validate the results, which shows the robustness of the proposed framework. The findings of this paper demonstrated that the HIS factor had the first rank in adopting the healthcare system with DTs, followed by the lack of digital knowledge, digital stratification, economic interventions, lack of reliable data, and cost inefficiency. The present model has many advantages in comparison with previous methods and models that applied to deal with the COVID-19 issues. For instance, Fong et al. [14] proposed a Monte-Carlo model for fuzzy decision making with incomplete information. However, they used the conventional fuzzy sets to deal with the uncertainty, while in the present paper, a new extension of fuzzy sets, named hesitant fuzzy sets, has been used to deal with complex MCDM issues. It is difficult to express the membership function of a conventional fuzzy set owing to time boundedness, the vagueness of the human mind, and increasing complexity; therefore, this study aimed to integrate HFSs with the proposed framework. Furthermore, Ren, Liao and Liu [123] proposed a new decision-making model to select the medication for the people being infected by the Coronavirus. Although they Generalized Z-numbers with HFSs to deal with uncertainty, their ranking method might not have enough novelty in comparison with the proposed framework in the present paper, named HF-SWARA–WASPAS. The integration of SWARA and WASPAS not only makes make the proposed framework a more capable, efficient, and sensible tool but also provides this opportunity to attain the highest accuracy of estimation. According to the current literature review and the best of our knowledge, we found that there is no study in the literature to provide a comprehensive framework DT intervention to control the COVID-19 outbreak. Therefore, the outcomes of this study will be useful for policymakers, governments, researchers, and practitioners to organize, use and develop the necessary initiatives for DT intervention to control the COVID-19 pandemic in adopting the healthcare system developing or infected countries. Moreover, the results of the study present several implications for further work. For example, to examine the main essential factors DT intervention to control the COVID-19 pandemic in the healthcare systems of the developed and developing nations. There are several limitations and opportunities for further work for adopting the healthcare system with DTs for DT intervention to control the COVID-19 outbreak. To doing so, in this study, we have tried to develop a new framework based on DT’s intervention to control the COVID-19 outbreak. Also, this study attempted to provide comprehensive factors to find the main factors in adopting the healthcare system to control the COVID-19 pandemic. Therefore, it is recommended that future studies can consider the framework of this study to implement in their studies. Furthermore, this study investigates several factors in adopting the healthcare system with DTs for DT intervention to control the COVID-19 outbreak. Therefore, the future study would focus on the other aspects of DT intervention to control the COVID-19 outbreak. In addition, it is recommended that further study needs to identify the critical issues by considering the organizational, professional, systemic and individual factors to adopt and design of the DT intervention to control the COVID-19 outbreak In addition, further work would implement some other methods (like as Additive Ratio Assessment (ARAS), Multi-Objective Optimization by Ratio Analysis plus the Full Multiplicative Form (MULTIMOORA), Double Normalization-Based Multiple Aggregation (DNMA) or Gain Loss Dominance method (GLDS)) to evaluate COVID-19 medication selection, sustainable biomass crop selection, and other decision-making problems.
CRediT authorship contribution statement
Abbas Mardani: Written the introduction, conclusion and discussion, Writing - review & editing. Mahyar Kamali Saraji: Written the literature review framework and references. Arunodaya Raj Mishra: Proposed the method, Comparison methods. Pratibha Rani: Analysis, Sensitivity analysis, Drafting.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Gössling S., Scott D., Hall C.M. Pandemics, tourism and global change: a rapid assessment of COVID-19. J. Sustain. Tour. 2020:1–20. [Google Scholar]
- 2.Barnes S.J. Information management research and practice in the post-COVID-19 world. Int. J. Inf. Manage. 2020 doi: 10.1016/j.ijinfomgt.2020.102175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Longhurst G.J., Stone D.M., Dulohery K., Scully D., Campbell T., Smith C.F. Strength, weakness, opportunity, threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the COIVD-19 pandemic. Anat. Sci. Educ. 2020 doi: 10.1002/ase.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Golinelli D., Boetto E., Carullo G., Landini M.P., Fantini M.P. How the COVID-19 pandemic is favoring the adoption of digital technologies in healthcare: a rapid literature review. medRxiv. 2020 doi: 10.2196/22280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sein M.K. The serendipitous impact of COVID-19 pandemic: A rare opportunity for research and practice. Int. J. Inf. Manage. 2020 doi: 10.1016/j.ijinfomgt.2020.102164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eisenhauer C.M., Brito F.A., Yoder A.M., Kupzyk K.A., Pullen C.H., Salinas K.E., Miller J., Hageman P.A. Mobile technology intervention for weight loss in rural men: protocol for a pilot pragmatic randomised controlled trial. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2019-035089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arbatani T.R., Asadi H., Omidi A. Competitiveness in Emerging Markets. Springer; 2018. Media innovations in digital music distribution: the case of beeptunes. com; pp. 93–108. [Google Scholar]
- 8.Shah S.G.S., Nogueras D., van Woerden H.C., Kiparoglou V. The effectiveness of digital technology interventions to reduce loneliness in adult people: A protocol for a systematic review and meta-analysis. medRxiv. 2019 doi: 10.1136/bmjopen-2019-032455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nambisan S. Digital entrepreneurship: Toward a digital technology perspective of entrepreneurship. Entrepreneurship Theory Pract. 2017;41:1029–1055. [Google Scholar]
- 10.De’ R., Pandey N., Pal A. Impact of digital surge during Covid-19 pandemic: A viewpoint on research and practice. Int. J. Inf. Manage. 2020 doi: 10.1016/j.ijinfomgt.2020.102171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ting D.S.W., Carin L., Dzau V., Wong T.Y. Digital technology and COVID-19. Nature Med. 2020;26:459–461. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2019;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahalle P., Kalamkar A.B., Dey N., Chaki J., Shinde G.R. 2020. Forecasting models for coronavirus (Covid-19): A survey of the state-of-the-art. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fong S.J., Li G., Dey N., Crespo R.G., Herrera-Viedma E. 2020. Finding an accurate early forecasting model from small dataset: A case of 2019-ncov novel coronavirus outbreak. arXiv preprint arXiv:2003.10776. [Google Scholar]
- 15.Sipior J.C. Considerations for development and use of AI in response to COVID-19. Int. J. Inf. Manage. 2020 doi: 10.1016/j.ijinfomgt.2020.102170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papagiannidis S., Harris J., Morton D. WHO led the digital transformation of your company? A reflection of IT related challenges during the pandemic. Int. J. Inf. Manage. 2020 doi: 10.1016/j.ijinfomgt.2020.102166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallotti R., Valle F., Castaldo N., Sacco P., De Domenico M. 2020. Assessing the risks of “infodemics” in response to COVID-19 epidemics. [DOI] [PubMed] [Google Scholar]
- 18.Zastrow M. Coronavirus contact-tracing apps: can they slow the spread of COVID-19? Nature. 2020 doi: 10.1038/d41586-020-01514-2. [DOI] [PubMed] [Google Scholar]
- 19.Fink M., Ma X., Traue H. 2015. Trust in Digital Technology: Reliability and Validity. [Google Scholar]
- 20.Cecilio Fernandes D., Parisi M., Santos T., Sandars J. The COVID-19 pandemic and the challenge of using technology for medical education in low and middle income countries. MedEdPublish. 2020;9 doi: 10.15694/mep.2020.000074.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee S.-O., Hong A., Hwang J. ICT diffusion as a determinant of human progress. Inf. Technol. Dev. 2017;23:687–705. [Google Scholar]
- 22.Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M., Chatterjee S., Lahiri D., Lavie C. Psychosocial impact of COVID-19. Diabetes Metab. Syndrome Clin. Res. Rev. 2020;14 doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Almunawar M.N., Anshari M. 2012. Health Information Systems (HIS): Concept and Technology. [Google Scholar]
- 24.Khan Z., Siddique A., Lee C. Robotics utilization for healthcare digitization in global COVID-19 management. Int. J. Environ. Res. Public Health. 2020;17:1–23. doi: 10.3390/ijerph17113819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahalakshmi K. Role of digital Technologies and applications against COVID-19 in India. Gedrag Organ. 2020;33:1751. [Google Scholar]
- 26.Zadeh L.A. Fuzzy sets. Inf. Control. 1965;8:338–353. [Google Scholar]
- 27.Bagga P., Joshi A., Hans R. Qos based web service selection and multi-criteria decision making methods. Int. J. Interact. Multimedia Artif. Intell. 2019;5 [Google Scholar]
- 28.Farhadinia B., Herrera-Viedma E. Multiple criteria group decision making method based on extended hesitant fuzzy sets with unknown weight information. Appl. Soft Comput. 2019;78:310–323. [Google Scholar]
- 29.Guo J., Yin J., Zhang L., Lin Z., Li X. Extended TODIM method for CCUS storage site selection under probabilistic hesitant fuzzy environment. Appl. Soft Comput. 2020;93 [Google Scholar]
- 30.Liu P., Zhang X. A new hesitant fuzzy linguistic approach for multiple attribute decision making based on Dempster–Shafer evidence theory. Appl. Soft Comput. 2020;86 [Google Scholar]
- 31.Song C., Zhang Y., Xu Z. An improved structure learning algorithm of Bayesian network based on the hesitant fuzzy information flow. Appl. Soft Comput. 2019;82 [Google Scholar]
- 32.Lanigan J.D. A sociotechnological model for family research and intervention: How information and communication technologies affect family life. Marriage Family Rev. 2009;45:587–609. [Google Scholar]
- 33.World Health Organization . World Health Organization; 2019. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening: Web Supplement 2: Summary of Findings and GRADE Tables. [PubMed] [Google Scholar]
- 34.van Dulmen S., Sluijs E., van Dijk L., de Ridder D., Heerdink R., Bensing J. International expert forum on patient adherence furthering patient adherence: a position paper of the international expert forum on patient adherence based on an internet forum discussion. BMC Health Serv. Res. 2008;8:47. doi: 10.1186/1472-6963-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thomson K., Brouwers C., Damman O.C., de Bruijne M.C., Timmermans D.R., Melles M. How health care professionals evaluate a digital intervention to improve medication adherence: qualitative exploratory study. JMIR Hum. Factors. 2018;5 doi: 10.2196/humanfactors.8948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Borkum E., Sivasankaran A., Sridharan S., Rotz D., Sethi S., Manoranjini M., Ramakrishnan L., Rangarajan A. Evaluation of the information and communication technology (ICT) continuum of care services (CCS) intervention in Bihar. Princeton: Math. Policy Res. 2015 [Google Scholar]
- 37.Ediriweera D.S., Kasturiratne A., Pathmeswaran A., Gunawardena N.K., Wijayawickrama B.A., Jayamanne S.F., Isbister G.K., Dawson A., Giorgi E., Diggle P.J. Mapping the risk of snakebite in Sri Lanka-a national survey with geospatial analysis. PLoS Neglect. Trop. Dis. 2016;10 doi: 10.1371/journal.pntd.0004813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gagnon M.P., Légaré F., Labrecque M., Frémont P., Pluye P., Gagnon J., Car J., Pagliari C., Desmartis M., Turcot L. Interventions for promoting information and communication technologies adoption in healthcare professionals. Cochrane Database Syst. Rev. 2009 doi: 10.1002/14651858.CD006093.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu R.C., Tran K., Lo V., O’Leary K.J., Morra D., Quan S.D., Perrier L. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int. J. Med. Inform. 2012;81:723–732. doi: 10.1016/j.ijmedinf.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 40.de Lima I.C.V., Galvão M.T.G., de Oliveira Alexandre H., Lima F.E.T., de Araújo T.L. Information and communication technologies for adherence to antiretroviral treatment in adults with HIV/AIDS. Int. J. Med. Inform. 2016;92:54–61. doi: 10.1016/j.ijmedinf.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 41.Anand S.S., Samaan Z., Middleton C., Irvine J., Desai D., Schulze K.M., Sothiratnam S., Hussain F., Shah B.R., Pare G. A digital health intervention to lower cardiovascular risk: a randomized clinical trial. JAMA Cardiol. 2016;1:601–606. doi: 10.1001/jamacardio.2016.1035. [DOI] [PubMed] [Google Scholar]
- 42.Morton K., Dennison L., Bradbury K., Band R.J., May C., Raftery J., Little P., McManus R.J., Yardley L. Qualitative process study to explore the perceived burdens and benefits of a digital intervention for self-managing high blood pressure in primary care in the UK. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-020843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lakshmiprabha S., Mahalakshmi K. Role of digital Technologies and applications against COVID-19 in India. Gedrag Organ. 2020;33:1751. [Google Scholar]
- 44.Hernandez-Orallo E., Manzoni P., Calafate C., Cano J.-C. Evaluating how smartphone contact tracing technology can reduce the spread of infectious diseases: the case of COVID-19. IEEE Access. 2020;PP:1. doi: 10.1109/ACCESS.2020.2998042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen B., Marvin S., While A. Containing COVID-19 in China: AI and the robotic restructuring of future cities. Dialogues Hum. Geogr. 2020 [Google Scholar]
- 46.Khan Z.H., Siddique A., Lee C.W. Robotics utilization for healthcare digitization in global COVID-19 management. Int. J. Environ. Res. Public Health. 2020;17:3819. doi: 10.3390/ijerph17113819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zayapragassarazan Z. COVID-19: Strategies for engaging remote learners in medical education. Education. 2020;1000:273. [Google Scholar]
- 48.Zaman A., Islam M.N., Zaki T., Hossain M.S. 2020. ICT intervention in the containment of the pandemic spread of COVID-19: An exploratory study. arXiv preprint arXiv:2004.09888. [Google Scholar]
- 49.Younes A.B., Hasan Z. COVID-19: Modeling, prediction, and control. Appl. Sci. 2020;10:3666. [Google Scholar]
- 50.Zlatanova S., Fabbri A. 2009. Geo-ICT for risk and disaster management; pp. 239–266. [Google Scholar]
- 51.Zhong H., Xiao J. Enhancing health risk prediction with deep learning on big data and revised fusion node paradigm. Sci. Program. 2017;2017 [Google Scholar]
- 52.Bhardwaj R. A predictive model for the evolution of COVID-19. medRxiv. 2020 doi: 10.1007/s41403-020-00130-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Armani A.M., Hurt D.E., Hwang D., McCarthy M.C., Scholtz A. Low-tech solutions for the COVID-19 supply chain crisis. Nat. Rev. Mater. 2020:1–4. doi: 10.1038/s41578-020-0205-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ivanov D., Dolgui A. A digital supply chain twin for managing the disruption risks and resilience in the era of industry 4.0. Prod. Plan. Control. 2020:1–14. [Google Scholar]
- 55.Tavakoli M., Carriere J., Torabi A. 2020. Robotics for COVID-19: How can robots help health care in the fight against coronavirus. [Google Scholar]
- 56.M. Alam, R. Parveen, I.R. Khan, Role of Information Technology in Covid-19 prevention, 5 (2020) 65–78.
- 57.Plotnikov V., Kuznetsova V. The prospects for the use of digital technology “blockchain” in the pharmaceutical market. MATEC Web Conf. 2018;193:02029. [Google Scholar]
- 58.Pradhan R.P., Mallik G., Bagchi T.P. Information communication technology (ICT) infrastructure and economic growth: A causality evinced by cross-country panel data. IIMB Manage. Rev. 2018;30:91–103. [Google Scholar]
- 59.Bukhari S.H., Bukhari S.M.H. The post-corona world and international political landscape: Emerging challenges. J. Bus. Soc. Rev. Emerg. Econ. 2020;6:453–461. [Google Scholar]
- 60.Sriwijitalai W., Wiwanitkit V. Exaggerated information and COVID-19 outbreak. Eur. J. Clin. Invest. 2020;50 doi: 10.1111/eci.13226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pulido C., Villarejo B., Redondo-Sama G., Gomez A. COVID-19 infodemic: More retweets for science-based information on coronavirus than for false information. Int. Sociol. 2020 [Google Scholar]
- 62.Rumble G. Bibliotheks-und Informationssystem der Universität Oldenburg Oldenburg; 2004. Papers and Debates on the Economics and Costs of Distance and Online Learning. [Google Scholar]
- 63.Baharuddin M.F. Digital literacy awareness among students. Res. Hub. 2016;2:57. [Google Scholar]
- 64.Triana A.J., Gusdorf R.E., Shah K.P., Horst S.N. Technology literacy as a barrier to telehealth during COVID-19. Telemed. e-Health. 2020 doi: 10.1089/tmj.2020.0155. [DOI] [PubMed] [Google Scholar]
- 65.UN-HABITAT . 2020. Digital technologies and the COVID-19 pandemic. [Google Scholar]
- 66.Ogundokun R., Bamidele A. 2020. Machine learning prediction for covid 19 pandemic in india. [Google Scholar]
- 67.Qin L., Yang Y., Cao Q., Cheng Z., Wang X., Sun Q., Yan F., Qu J., Yang W. A predictive model and scoring system combining clinical and CT characteristics for the diagnosis of COVID-19. Eur. Radiol. 2020:1–11. doi: 10.1007/s00330-020-07022-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang C., Qin L., Li K., Wang Q., Zhao Y., Xu B., Liang L., Dai Y., Feng Y., Sun J. A novel scoring system for prediction of disease severity in COVID-19. Front. Cell. Infect. Microbiol. 2020;10:318. doi: 10.3389/fcimb.2020.00318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dur-e Ahmad M., Imran M. Transmission dynamics model of coronavirus COVID-19 for the outbreak in most affected countries of the world. Int. J. Interact. Multimedia Artif. Intell. 2020;6 [Google Scholar]
- 70.Sittig D.F., Singh H. COVID-19 and the need for a national health information technology infrastructure. JAMA. 2020;323:2373–2374. doi: 10.1001/jama.2020.7239. [DOI] [PubMed] [Google Scholar]
- 71.Caballero-Uribe C. 2018. An Education in Digital Health; pp. 329–338. [Google Scholar]
- 72.Kim J., Gewertz B. Teleurology and digital health app in COVID-19 pandemic. Investig. Clin. Urol. 2020;61:333–334. doi: 10.4111/icu.2020.61.4.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Feyzioğlu B., Altindis M. Emerging technologies for the diagnosis of viral infections and SARS-CoV-2. Gazi Med. J. 2020 [Google Scholar]
- 74.Sarbadhikari S., Sarbadhikari S.N. The global experience of digital health interventions in COVID-19 management. Indian J. Publ. Health. 2020;64:117. doi: 10.4103/ijph.IJPH_457_20. [DOI] [PubMed] [Google Scholar]
- 75.Saiz F.A., Barandiaran I. COVID-19 detection in chest X-ray images using a deep learning approach. Int. J. Interact. Multimedia Artif. Intell. 2020;6(2):1. doi: 10.9781/ijimai.2020.04.003. [DOI] [Google Scholar]
- 76.Park M., Cook A., Lim J., Sun Y., Dickens B. A systematic review of COVID-19 epidemiology based on current evidence. J. Clin. Med. 2020;9:967. doi: 10.3390/jcm9040967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.allah Kalteh E., Rajabi A. COVID-19 and digital epidemiology. Z. Gesundheitswissenschaften. 2020:1. doi: 10.1007/s10389-020-01295-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bandyopadhyay A.R., Chatterjee D., Ghosh K., Sarkar P. COVID 19: An epidemiological and host genetics appraisal. Asian J. Med. Sci. 2020;11:71–76. [Google Scholar]
- 79.Albugami S.S., Ahmed V. Effects of culture and religion on the use of ICT in the Saudi education system. IIER Int. Inst. Eng. Res. 2016:25–27. [Google Scholar]
- 80.Vokinger K.N., Nittas V., Witt C.M., Fabrikant S.I., von Wyl V. Digital health and the COVID-19 epidemic: an assessment framework for apps from an epidemiological and legal perspective. Swiss Med. Wkly. 2020;150 doi: 10.4414/smw.2020.20282. [DOI] [PubMed] [Google Scholar]
- 81.Goldkind L., LaMendola W., Taylor-Beswick A. Tackling COVID-19 is a crucible for privacy. J. Technol. Hum. Serv. 2020;38:89–90. [Google Scholar]
- 82.Lenert L., McSwain B.Y. Balancing health privacy, health information exchange, and research in the context of the COVID-19 pandemic. J. Am. Med. Inform. Assoc. 2020;27:963–966. doi: 10.1093/jamia/ocaa039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jiang X., Ming W.-K., You J.H. The cost-effectiveness of digital health interventions on the management of cardiovascular diseases: systematic review. J. Med. Internet Res. 2019;21 doi: 10.2196/13166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Orben A., Tomova L., Blakemore S.-J. The effects of social deprivation on adolescent development and mental health. Lancet Child Adolescent Health. 2020 doi: 10.1016/S2352-4642(20)30186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ramsetty A., Adams C. Impact of the digital divide in the age of COVID-19. J. Am. Med. Inform. Assoc. 2020 doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Torra V. Hesitant fuzzy sets. Int. J. Intell. Syst. 2010;25:529–539. [Google Scholar]
- 87.Atanassov K.T. Springer; 1999. Intuitionistic Fuzzy Sets; pp. 1–137. [Google Scholar]
- 88.Dubois D.J. Academic Press; 1980. Fuzzy Sets and Systems: Theory and Applications. [Google Scholar]
- 89.Zadeh L.A. The concept of a linguistic variable and its application to approximate reasoning-III. Inf. Sci. 1975;9:43–80. [Google Scholar]
- 90.Yager R.R. On the theory of bags. Int. J. Gen. Syst. 1986;13:23–37. [Google Scholar]
- 91.Asan U., Kadaifci C., Bozdag E., Soyer A., Serdarasan S. A new approach to DEMATEL based on interval-valued hesitant fuzzy sets. Appl. Soft Comput. 2018;66:34–49. [Google Scholar]
- 92.Liao H., Yang L., Xu Z. Two new approaches based on ELECTRE II to solve the multiple criteria decision making problems with hesitant fuzzy linguistic term sets. Appl. Soft Comput. 2018;63:223–234. [Google Scholar]
- 93.Xu Z., Zhang X. Hesitant fuzzy multi-attribute decision making based on TOPSIS with incomplete weight information. Knowl.-Based Syst. 2013;52:53–64. [Google Scholar]
- 94.Farhadinia B. Information measures for hesitant fuzzy sets and interval-valued hesitant fuzzy sets. Inform. Sci. 2013;240:129–144. [Google Scholar]
- 95.Liao H., Xu Z. Satisfaction degree based interactive decision making under hesitant fuzzy environment with incomplete weights. Int. J. Uncertain. Fuzziness Knowl.-Based Syst. 2014;22:553–572. [Google Scholar]
- 96.G. Thakur, R. Thakur, R.J.F.I. Singh, Engineering, new hesitant fuzzy operators, 6 (2014) 379–392.
- 97.Ashtiani M., Azgomi M.A. A hesitant fuzzy model of computational trust considering hesitancy, vagueness and uncertainty. Appl. Soft Comput. 2016;42:18–37. [Google Scholar]
- 98.S. Faizi, W. Sałabun, T. Rashid, J. Wątróbski, S. Zafar, Group decision-making for hesitant fuzzy sets based on characteristic objects method, 9 (2017) 136.
- 99.Lan J., Jin R., Zheng Z., Hu M. Priority degrees for hesitant fuzzy sets: Application to multiple attribute decision making. Oper. Res. Perspect. 2017;4:67–73. [Google Scholar]
- 100.Alcantud J.C.R., Giarlotta A. Necessary and possible hesitant fuzzy sets: A novel model for group decision making. Inf. Fusion. 2019;46:63–76. [Google Scholar]
- 101.Aktas A., Kabak M. A hybrid hesitant fuzzy decision-making approach for evaluating solar power plant location sites. Arab. J. Sci. Eng. 2018;44:7235–7247. [Google Scholar]
- 102.Hussain Z., Yang M.-S. Entropy for hesitant fuzzy sets based on hausdorff metric with construction of hesitant fuzzy TOPSIS. Int. J. Fuzzy Syst. 2018;20:2517–2533. [Google Scholar]
- 103.Mishra A.R., Rani P., Pardasani K.R. Multiple-criteria decision-making for service quality selection based on shapley COPRAS method under hesitant fuzzy sets. Granul. Comput. 2019;4:435–449. [Google Scholar]
- 104.Xu Z., Zhang S. An overview on the applications of the hesitant fuzzy sets in group decision-making: Theory, support and methods. Front. Eng. Manage. 2019:1–20. [Google Scholar]
- 105.Mishra A.R., Rani P., Pardasani K.R., Mardani A. A novel hesitant fuzzy WASPAS method for assessment of green supplier problem based on exponential information measures. J. Cleaner Prod. 2019;238 [Google Scholar]
- 106.Wang F. Aggregation similarity measure based on hesitant fuzzy closeness degree and its application to clustering analysis. J. Syst. Sci. Inf. 2019;7:70–89. [Google Scholar]
- 107.Lalotra S., Singh S. Knowledge measure of hesitant fuzzy set and its application in multi-attribute decision-making. Comput. Appl. Math. 2020;39:1–31. [Google Scholar]
- 108.Keršuliene V., Zavadskas E.K., Turskis Z. Selection of rational dispute resolution method by applying new step-wise weight assessment ratio analysis (SWARA) J. Bus. Econ. Manage. 2010;11:243–258. [Google Scholar]
- 109.Rani P., Mishra A.R. Single-valued neutrosophic SWARA-VIKOR framework for performance assessment of eco-industrial thermal power plants. ICSES Trans. Neural Fuzzy Comput. ITNFC. 2020;3:1–9. [Google Scholar]
- 110.Mishra A.R., Rani P., Pandey K., Mardani A., Streimikis J., Streimikiene D., Alrasheedi M. Novel multi-criteria intuitionistic fuzzy SWARA–COPRAS approach for sustainability evaluation of the bioenergy production process. Sustainability. 2020;12:4155. [Google Scholar]
- 111.Rani P., Mishra A.R., Mardani A., Cavallaro F., Štreimikiene D., Khan S.A.R. Pythagorean fuzzy SWARA–VIKOR framework for performance evaluation of solar panel selection. Sustainability. 2020;12:4278. [Google Scholar]
- 112.Zavadskas E.K., Turskis Z., Antucheviciene J., Zakarevicius A. Optimization of weighted aggregated sum product assessment. Elektron. Elektrotechn. 2012;122:3–6. [Google Scholar]
- 113.Badalpur M., Nurbakhsh E. An application of WASPAS method in risk qualitative analysis: a case study of a road construction project in Iran. Int. J. Construct. Manage. 2019:1–9. [Google Scholar]
- 114.Chakraborty S., Zavadskas E.K. Applications of WASPAS method in manufacturing decision making. Informatica. 2014;25:1–20. [Google Scholar]
- 115.Turskis Z., Zavadskas E.K., Antucheviciene J., Kosareva N. A hybrid model based on fuzzy AHP and fuzzy WASPAS for construction site selection. Int. J. Comput. Commun. Control. 2015;10:113–128. [Google Scholar]
- 116.Ghorabaee M.K., Zavadskas E.K., Amiri M., Esmaeili A. Multi-criteria evaluation of green suppliers using an extended WASPAS method with interval type-2 fuzzy sets. J. Cleaner Prod. 2016;137:213–229. [Google Scholar]
- 117.Mishra A.R., Rani P. Interval-valued intuitionistic fuzzy WASPAS method: application in reservoir flood control management policy. Group Decis. Negot. 2018;27:1047–1078. [Google Scholar]
- 118.Deveci M., Canıtez F., Gökaşar I. WASPAS and TOPSIS based interval type-2 fuzzy MCDM method for a selection of a car sharing station. Sustainable Cities Soc. 2018;41:777–791. [Google Scholar]
- 119.Mishra A.R., Singh R.K., Motwani D. Multi-criteria assessment of cellular mobile telephone service providers using intuitionistic fuzzy WASPAS method with similarity measures. Granul. Comput. 2019;4:511–529. [Google Scholar]
- 120.Rani P., Mishra A.R., Pardasani K.R. A novel WASPAS approach for multi-criteria physician selection problem with intuitionistic fuzzy type-2 sets. Soft Comput. 2020;24:2355–2367. [Google Scholar]
- 121.Xia M., Xu Z. Hesitant fuzzy information aggregation in decision making. Int. J. Approx. Reason. 2011;52:395–407. [Google Scholar]
- 122.Liao H., Xu Z., Xia M. Multiplicative consistency of hesitant fuzzy preference relation and its application in group decision making. Int. J. Inf. Technol. Decis. Mak. 2014;13:47–76. [Google Scholar]
- 123.Ren Z., Liao H., Liu Y. Generalized z-numbers with hesitant fuzzy linguistic information and its application to medicine selection for the patients with mild symptoms of the COVID-19. Comput. Ind. Eng. 2020 doi: 10.1016/j.cie.2020.106517. [DOI] [PMC free article] [PubMed] [Google Scholar]