Abstract
Cleft rhinoplasty is a demanding, technique-sensitive procedure. Part art, part science; it poses several probing questions to the surgeon. The unilateral cleft nasal deformity is a distinct entity because the pursuit of symmetry in the unilateral cleft nose makes the repair much more challenging. The advent of nasoalveolar moulding, the gaining popularity of primary (early) nasal repair and greater refinements in secondary (definitive) rhinoplasty techniques have contributed to better nasal results in unilateral cleft repair. Yet, some obstacles remain. This paper aims to discuss the anatomy of the unilateral cleft nose, enumerate aims and objectives of repair at every stage, and to demonstrate the evolution and varied rationale of management of nasal deformities in the unilateral cleft lip and nose.
Keywords: Unilateral cleft lip, Cleft nasal deformity, Unilateral cleft nose, Cleft rhinoplasty
Introduction
Over the years, a multitude of surgical techniques for cleft repair have been introduced and discarded by surgical pioneers, with further refinements brought forth by a generation of surgeons thereafter. Yet, unlike an excellent lip repair, which can be reliably reproduced, the cleft nose remains a challenge. Despite better understanding of the pathology, improved surgical techniques/materials and attempts at addressing some of the nasal deformity early on, there are several factors that may have an effect on the final surgical result. Results of nasal repair may be compromised by a number of variables, these may include the degree of deformity, the effects of growth over time and/ or the sequelae of the repair itself. Combine this with the fact that any result can only be truly judged after a ‘surgical lifetime’, the cleft nose continues to remain an obstacle to the final aesthetics of cleft repair.
Understanding Aberrant Anatomy and Embryology
Appreciating the processes responsible for the cleft lip nasal deformity is crucial to the surgeon who desires to repair the condition. Although it is understood that every cleft is unique, any individual cleft nasal deformity occurs along a specific spectrum of potential deformities [1]. The anatomical and pathological subtleties of the unilateral cleft nose were first described as a separate entity (without being bunched with the often cited lip deformity) by Blair and Brown [2]. Huffman and Lierle [3] are credited with the earliest detailed description of the same. Understanding the embryological basis of the clinical appearance is paramount to the surgical correction of the cleft lip and nose. A combination of both internal (mesenchymal migration) and external (mechanical forces) stressors is attributed to deformational abnormalities such as this. A cleft lip, to put things simply, forms from an improper fusion of the medial and lateral nasal prominences with the maxillary process. It has been shown that the medial nasal process remains central and fails to meet the maxillary process in cleft patients. As embryogenesis proceeds, the unhampered forces, produced by the developing aberrant orbicularis musculature (which do not form a sphincter as the normal lip musculature does), further accentuate the deformed features of the cleft nose by their abnormal attachments to the maxilla, alar base and midline [4].
Previously, authors have attempted to simplify this complex interplay of mechanisms and deformities responsible for the cleft nose. They include the Origami models of Boo-Chai and Tange [5] which infers that the cleft nose is more ‘distortion and displacement’ rather than a deficiency, and the Tilted Tripod described by Hogan [6] to explain the septal deviation in the unilateral cleft lip. More recently, Fischer and Mann [7] have described a model elaborating the mechanisms responsible for the cleft lip nasal deformities, mild through severe, unilateral and bilateral. Their aim is a better understanding of the deformity through analysis of the model.
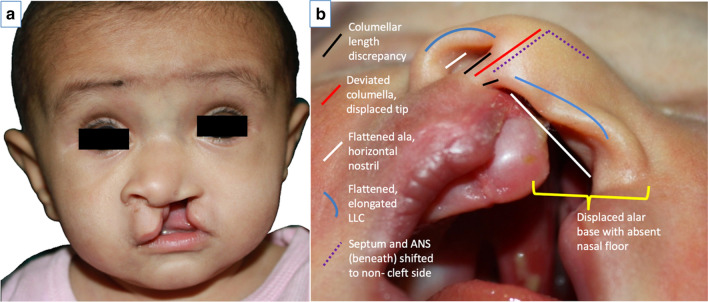
‘Classic’ features of the unilateral cleft nose have been described by several authors [1, 8–11] (Table 1). These features tend to exaggerate as the child grows. This worsening of asymmetry and deviation of the nose generally ceases around the end of puberty [12]. There has been significant debate regarding the apparent paucity of tissues. For now though, there seems to be some consensus on the matter. This has been made possible by separating the deformity into three separate parts—cutaneous/mucosal, chondrous and osseous components. Authors have conjectured, about the cutaneous or mucosal aspect of the deformity; studies thus far do not prove either way if the tissues are deficient in some manner or in excess. However, it is believed that, whatever it may be, the skin/mucosal elements of the unilateral cleft nose do not interfere with construction of a nostril of similar size and shape to the other side [13]. Meanwhile, the debate regarding whether the cartilaginous elements are hypoplastic compared to the non-cleft side seems to be settled, at least theoretically. Dissection studies of stillborn children with clefts by Atherton [14], McComb [15] and more recently by Li et al. [16] concur that the lower lateral cartilage (LLC) is of normal length, width and thickness. Deformed they may be, deficient they are not. As demonstrated by Kim et al. [17], the medial crural footplate is merely displaced downwards, therefore drawing the genu medially and tethering the lateral crura taut laterally. The upper lateral cartilage may also be pulled inferomedially by the deviant antero-caudal septum [17] (Fig. 1). The third aspect of the cleft nose merits no discord. On the cleft side, a defect in the osseous maxilla is apparent. Fisher et al. [18] have analysed these parameters three-dimensionally via computed tomography in 3-month-old infants with complete unilateral cleft lip and palate and have shown a gross anterior and lateral movement of the premaxilla towards the non-cleft side. The piriform is more posterior, the vomer is deviated, and the anterior nasal spine turns towards the opposite side. This is the raison d’être for the anterior nasal spine, antero-caudal septum and the base of the columella to tilt towards the non-cleft side.
Table 1.
Features of the unilateral cleft nose
| 1. Shorter columella on cleft side | |
| 2. Deviation of columella to non-cleft side | |
| 3. Flattened, elongated lateral crus of cleft side lower lateral cartilage | |
| 4. Displaced nasal tip (in frontal and horizontal planes) | |
| 5. Flattened ala, with resultant horizontal orientation of nostril | |
| 6. Asymmetric nostrils, with retro-positioned cleft side nostril (due to underlying osseous deformity) | |
| 7. Alar base is displaced laterally and/or posteriorly and sometimes inferiorly | |
| 8. Cleft side nasal floor is generally caudal and absent (depending on cleft severity) | |
| 9. Septum and anterior nasal spine shifted to non-cleft side with varying degrees of septal deviation | |
| 10. Hypertrophic inferior turbinate on the cleft side |
Fig. 1.
The unilateral cleft nasal deformity, features apparent in frontal (a) and basal views (b) (as described in previous table)
Timing of Surgical Repair (Changing Concepts)
Based on timing, cleft lip nasal surgery can be classified into primary, intermediate and definitive repairs. Primary rhinoplasty is defined as any correction done at the time of primary lip repair [19]. Intermediate rhinoplasty can be described as procedures performed before nasal growth is completed [20]. Broadly speaking, the so-called intermediate rhinoplasties fall under two specific categories, based on the age at which they are performed. Nasal work done between 4 and 6 years of age, often in conjunction with lip revision, is popularly known by the term ‘preschool rhinoplasty’. The surgical reasoning being deformity correction to minimise any peer psychological pressure [20]. Another school of thought believes if primary nasal work has already been done, intermediate revisions are better done between 8 and 12 years of age, after completion of orthodontic alignment and secondary alveolar bone grafting; allowing a more ‘normal’, stable skeletal base for correction of severe nasal deformities. Generally speaking, intermediate rhinoplasty is more conservative than definitive rhinoplasty techniques. Definitive rhinoplasty, frequently termed as secondary rhinoplasty, is performed after completion of maxillary and nasal growth [21]. At this point, more aggressive septoplasty, osseous reframing and grafting manoeuvres can be performed. The corrections may also be multi-staged or phased if the deformity is severe; therefore, the term ‘secondary’ rhinoplasty is a misnomer.
Prior to the 1970s, customary practice dictated the nasal correction of the cleft deformity be performed later in life, often delayed until growth was complete [12]. Gillies and Millard [22] purported in 1966 that any primary nasal correction is untenable because the deformity is so complex. They believed any such early correction, even if successful, would not avert future surgery. Cronin and Denkler [23], and Aufricht [24] believed the teenage years were the optimum time for correction of the unilateral cleft deformity. Broadbent and Woolf [25] reiterated this philosophy of not repairing noses in infancy claiming the results were not stable. Earlier reports of primary repair had fallen into disrepute because noses that looked satisfactory on the operating table had subsequently reverted to develop into the typical stigmata. These dogmas were reinforced by the works of surgeons such as Gelbke [26] who were radical in their primary repair, with extensive incisions, excisions and dissection, but with unsatisfactory results and significant growth disturbance.
Those against early attempts at correction of the cleft nose had three main concerns: (1) growth retardation of the midface and nasal complex, (2) scarring inflicted by the extensive dissection which would hamper future surgeries and (3) delicate cartilages and minimal soft tissue not being amenable to manipulation [23]. Despite the existing contrarian beliefs of the time, a handful of surgeons from across the globe began their work on primary rhinoplasty [11, 27–29]. As they started to publish their long-term results, fears of effects of early surgery on growth started to wane. McComb and Coghlan [30], Salyer et al. [28] and Anderl et al. [27] have been credited with popularising the concept of concomitant primary lip and nose repair in unilateral clefts. They have all published fairly stable, agreeable, long-term results without any apparent adverse effect of the growth of the midface [27, 28, 30, 31].
It would be prudent at this point to discuss the cartilaginous septum in the unilateral cleft deformity and the conundrum it presents in terms of timing of repair. Two schools of thought still exist in this regard: one, who believe early septal correction is unwarranted and may even adversely affect the growth of the nasal and midfacial complex [28]. This belief was mostly instilled by a number of experimental animal studies in the 1960s and 1970s that emphasised the importance of the nasal septum in facial growth. Surgical removal of all or part of the cartilaginous septum typically resulted in a deficiency in the anteroposterior growth of the maxilla and premaxilla (or snout in most cases!). Sarnat and Wexler [32] demonstrated this in normal adult rabbit. Latham [33], in 1969, suggested that the nasal septum was the primary factor in the osseous deformity that is the unilateral cleft. According to him, the septum has a downward and forward growth direction. And in the event of a unilateral cleft, the normal resistance to septal growth would be lacking on the cleft side due to the abnormal tethering of the inferior septal border [33]. Therefore, this would infer that repositioning the septum at the earliest would be ideal for optimum growth, thus laying basis for the beliefs of the second group, who prefer to correct the septum early. It is also proposed that correction of the deviated septum early is important because it provides stability and exact positioning of the lifted alar crura of the cleft side and nasal tip [34]. Proponents of early septal correction cite myriad advantages of early septal repair; they include: better anteroposterior and vertical growth, improved nasal symmetry, improved function and therefore avoidance of altered facial growth due to the mouth-breathing malady, better tip projection and a more simplified definitive secondary procedure if performed [1, 9, 27, 34]. Smahel et al. [35] conducted a radiographic growth study wherein two comparable groups were studied on the effect of primary repositioning of the nasal septum (which was performed in one group). The group with early manipulation of the septum showed more favourable nasal prominence and had better vertical growth with the anteroposterior parameters in both groups being equivocal. Therefore, current literature seems to favour repositioning of the cartilaginous septum at primary repair, with some evidence that this does not suffer from any long-term consequences.
Is There a Role for Nasoalveolar Moulding?
Prior to the advent of nasoalveolar moulding (NAM), none of the existing methods of presurgical orthopaedics attempted to address the nasal deformity. Nasoalveolar moulding, as the term implies, places considerable emphasis on the nasal component of the deformity. Among its primary objectives are: correction of nasal asymmetry, presurgical elongation of columella, correction of nasal cartilage deformity, increasing the surface area of the nasal mucosal lining and uprighting the columella [36]. Pioneered by Grayson et al. [37], and based on work by Matsuo et al. [38], the initial techniques have been extensively refined [39, 40]. Early opposition to the intervention was based on several dogmas. From being a growth hindrance to being a complete waste of time and resources, several arguments have been made: some warranted, some not. The disagreement concerning the long-term stability of the results achieved notwithstanding, existing evidence [41–43] suggests overall improvement in nasal aesthetics over the non-NAM population, with some element of relapse, especially in the early years. To counter this, a few have advocated overcorrection at the time of primary repair [44, 45]. In their comparison study assessing 5-year follow-up results, Chang et al. [44] concluded that an overcorrection of 20 per cent was necessary to maintain the nostril height. Lonic et al. [45] arrived at a similar verdict, though their results were judged at 1-year follow-up. They surmised that primary nasal overcorrection including muscle to columella base suture, alar cinch suture and the Tajima method resulted in quantitatively more symmetric alae and nostril height when compared to non-overcorrected patients. The corollary to these studies would be to infer that about 10–20% relapse can be expected even after NAM and primary nasal cartilage work. Therefore, the deformity can only be mitigated not entirely abolished.
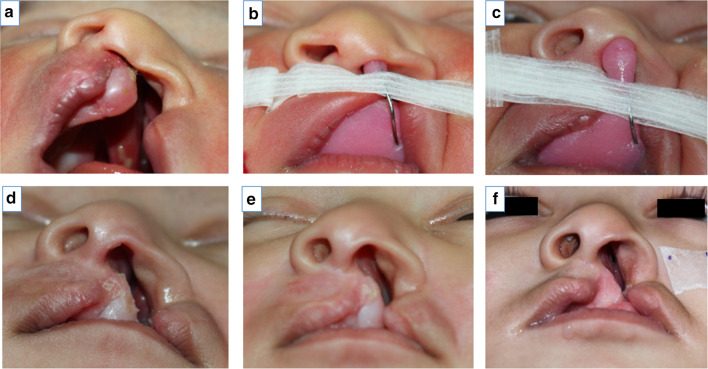
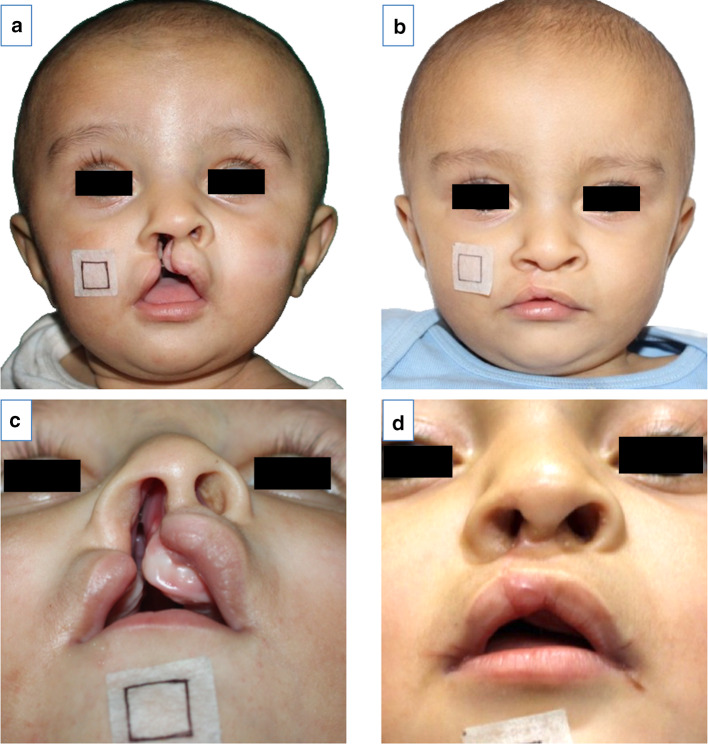
After the emergence and tentative acceptance of NAM, there was a period when primary rhinoplasty was not performed (in those that were treated with NAM) because at the end of primary cheiloplasty, the nose often looked satisfactory even without surgical intervention. For a while, some surgeons believed the NAM-treated nose without further surgical manipulation will suffice, till definitive rhinoplasty is warranted in adulthood. However, most quickly went back to primary nasal repair as results showed NAM by itself was insufficient to maintain nostril symmetry over time [41, 44] (Fig. 2).
Fig. 2.
Correction of nasal asymmetry, presurgical elongation of columella, correction of nasal cartilage deformity, increasing the surface area of the nasal mucosal lining and uprighting the columella. As nasoalveolar moulding progresses (pictures ‘a’ through ‘e’); the desired changes are apparent
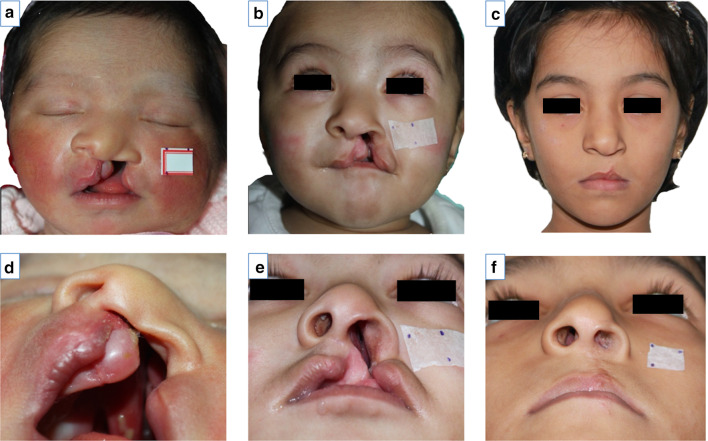
Regardless of the use of NAM, the goals of primary unilateral cleft rhinoplasty remain fairly consistent among different centres [9, 28, 44, 46]. (1) Releasing, undermining and repositioning the lower lateral cartilage (LLC) to provide better contour, symmetry and projection of the nasal tip, (2) centralising the antero-caudal septum, (3) elevating the medial crus of the LLC, and (4) medialising and securing the alar base. Lengthening the hemi-columella with a C-flap [9] and correcting vestibular webbing [46] are also often added to this list. The approach to achieving these goals varies significantly (Fig. 3).
Fig. 3.
Results of NAM without primary rhinoplasty. At one week of age prior to NAM (a, d). At 4 months of age, after NAM and just prior to primary surgery (b, e). Postoperative views at the age of 5 years (c, f)
Goals, Approaches and Techniques of Repair
Primary cleft rhinoplasties can broadly be classified into open, semi-open and closed types. Though less extensive than the definitive adult rhinoplasty, the so-called open-tip cleft rhinoplasties involve significant dissection and tissue manipulation and are therefore not very popular [47, 48]. There is also minimal evidence of its superiority over other less invasive techniques, especially when combined with NAM. Closed primary rhinoplasties are termed as those who do not have separate nasal incisions for cartilage manipulation [9, 15, 28]. The lower nasal structures are accessed via the medial and lateral lip incisions and the dissection is blind and by ‘feel’ only. Subsequent to dissection, the cartilage is repositioned with different methods of ‘suspension suturing’, to the extent where this might be called a suspension rhinoplasty (Figs. 4, 5).
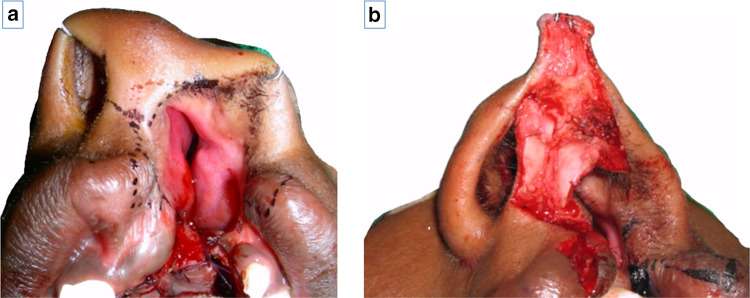
Fig. 4.
Primary open rhinoplasty—direct visualisation of the LLCs, via a trans-columellar incision incorporated into the cheiloplasty incision. Incision markings (a), after exposure (b)
Fig. 5.
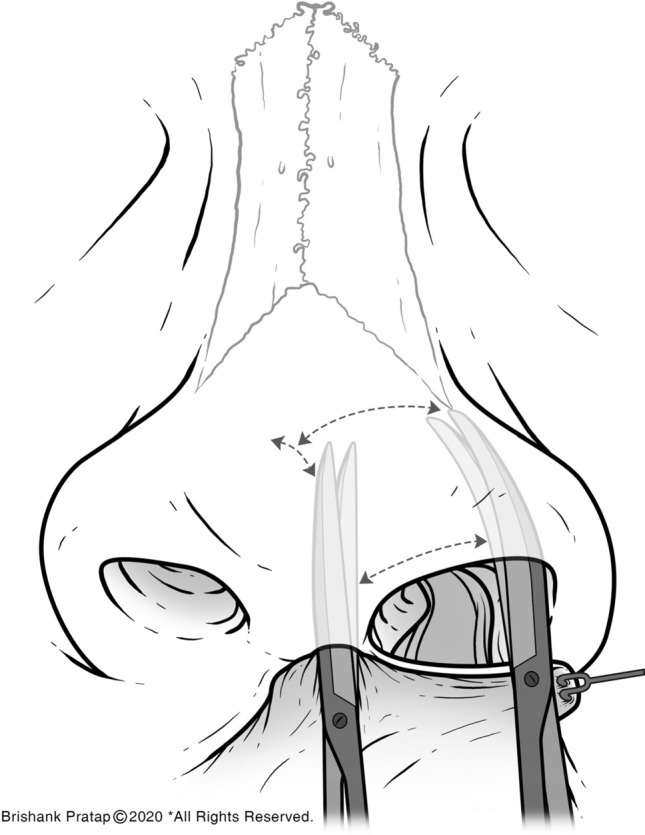
Closed primary rhinoplasty involves ‘blind’ dissection of the LLCs through the medial and lateral cheiloplasty incisions
Semi-open primary rhinoplasty involves minimal incisions on the nose with cartilage work and suspension suturing, the premise being better access to the LLC and therefore a more thorough dissection of aberrant tethering of cartilage and better control of the sutures techniques used [44, 49] (Figs. 6, 7).
Fig. 6.
Our approach to semi-open primary rhinoplasty involves a reverse-U (Tajima) incision on the cleft side and a marginal incision on the non-cleft side. Incision marking on cleft side (a), Tajima incision (b), dissection over the cartilage plane and release of fibrofatty tissue (c), approximation of LLCs with inter-domal stitches using 4-0 polydioxanone suture (d), excision of skin over the cleft side ala and closure of nasal incisions (e)
Fig. 7.
After NAM and prior to primary surgery (a, c), one year after cheiloplasty and semi-open rhinoplasty (b, d)
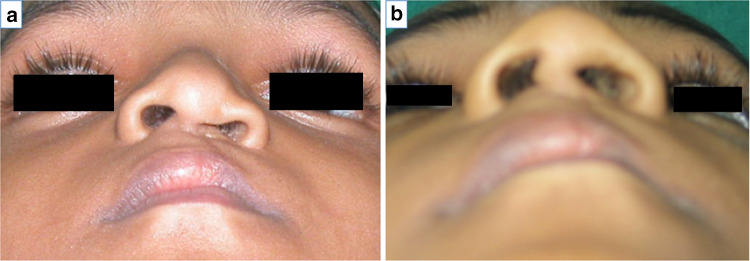
With the primary rhinoplasty, invariably there will be some residual deformities [1]. Either uncorrected, poorly corrected, or perhaps excellently corrected at primary repair but relapsed to some degree, these deformities may cause some distress to the parent or to the child herself. There are also those children that present in early childhood with an untouched cleft nasal deformity [46]. These can be re-evaluated and repaired at the time of the ‘intermediate rhinoplasty’. This is a term given to nasal procedures that are performed after the primary lip repair but prior to completion of facial growth [1, 46]. The objectives of this surgery are not expansive; it is largely agreed that it should focus on improvements of the lower third of the nose [46], i.e. repositioning of the antero-inferior cartilaginous septum, evaluation and repositioning of the LLC, adjusting the alar base and elimination of any lateral vestibular webbing that occurs. The goal is to achieve the said objectives with as conservative an approach as possible, the idea being to set the stage for a simpler, successful definitive rhinoplasty after cessation of growth (Fig. 8).
Fig. 8.
‘Preschool rhinoplasty’ primarily focuses on improving the lower third of the nasal structure, and mitigation of the deformity, setting the stage for secondary or definitive rhinoplasty. Preoperative (a) and postoperative (b) basal views. (Picture courtesy—The Charles Pinto Centre for Cleft Lip and Palate, Thrissur, Kerala)
Definitive rhinoplasty or adult cleft rhinoplasty aims to correct the residual deformity (or the primary deformity itself, in untreated cases). Factors contributing to the secondary unilateral cleft nasal deformity can be described as a sum of the following: residual deformities if any, deformities brought forth by previous surgeries (i.e. iatrogenic), combined with growth-related changes that may occur. [1, 46].
The agenda, beginning from infancy, should be achieving a nose at skeletal maturity, primed for definitive rhinoplasty, with the following attributes [1]:
Untouched upper 2/3rds.
A well-balanced skeletal base; this includes a maxilla that has its cleft alveolus treated. Any orthognathic maxillary procedure should ideally precede definitive cleft rhinoplasty.
Cleft side ala with minimal to moderate slumping (if at all).
Minimal to no cartilaginous injury from prior procedures.
Negligible or inconspicuous external scarring.
Such a cleft nose would be the ideal, where nasoalveolar moulding and primary rhinoplasty have achieved all their objectives. But in the real world, this often is not the case. And a significant number of adult cleft noses have not had any previous surgeries and therefore the deformity may be significant.
Unlike aesthetic nasal procedures, cleft rhinoplasty is rarely accomplished with an endonasal approach [1, 19, 46]. The open approach is often chosen, for it offers better visualisation and access. Irrespective of the plan of care adopted, patient evaluation prior to definitive repair should be comprehensive, including functional and aesthetic concerns and expectations of the patient. It is paramount to elicit a detailed history with regard to previous nasal/facial surgeries to best prepare for possible findings intraoperatively, and the effect they may have on the final outcome. Various combinations of trans-columellar incisions coupled with rim, marginal or infra-cartilaginous incisions are used to gain access. Typically, adult unilateral cleft nose reconstruction includes manipulation of the bony pyramid and septal work, with placement of cartilage grafts for support and reinforcement being a major component of the operation [19, 46]. It may involve:
Procedure to improve function—inferior turbinate reduction, septal resection/repositioning.
Bony vault correction—possible nasal bone osteotomies and infractures.
Lower third manipulation—centralisation of cartilaginous septum, chondromucosal V–Y advancement, vestibular web corrections, alar base and nostril repositioning.
Cartilage grafts harvested from the septum, auricle or rib are necessary to reshape, reconstruct, reinforce and hold the structural framework in position with minimal relapse. They may include some or all of the following [50, 51]:
Dorsal (spreader/augmentation) grafts to straighten or increase height of the dorsum and/or improve internal valve cross section (and consequently the airway).
Columellar strut grafts to reinforce the medial and middle crura. These are essential to provide extra support to the alar cartilage and support the nasal tip against scar-tissue forces in the postoperative period.
Caudal septal extension grafts for septal structural support.
Invisible (non-projecting) tip grafts to support the nasal tip and visible ones/cap grafts to add projection and give shape to the tip. They may be shaped and smoothed cartilages from the septum, ear or rib. They are often heart or shield shaped and are stabilised by suturing to the adjacent alar cartilages.
Crural grafts to shape the lateral crura and support the vestibule. They are inserted under the lateral crus to straighten the ala and correct its slump, thus opening the airway.
Batten grafts to correct the pinched nasal tip.
Premaxillary grafts can move the base of the nose forward and make the lip–nose angle less acute (Fig. 9).
Fig. 9.
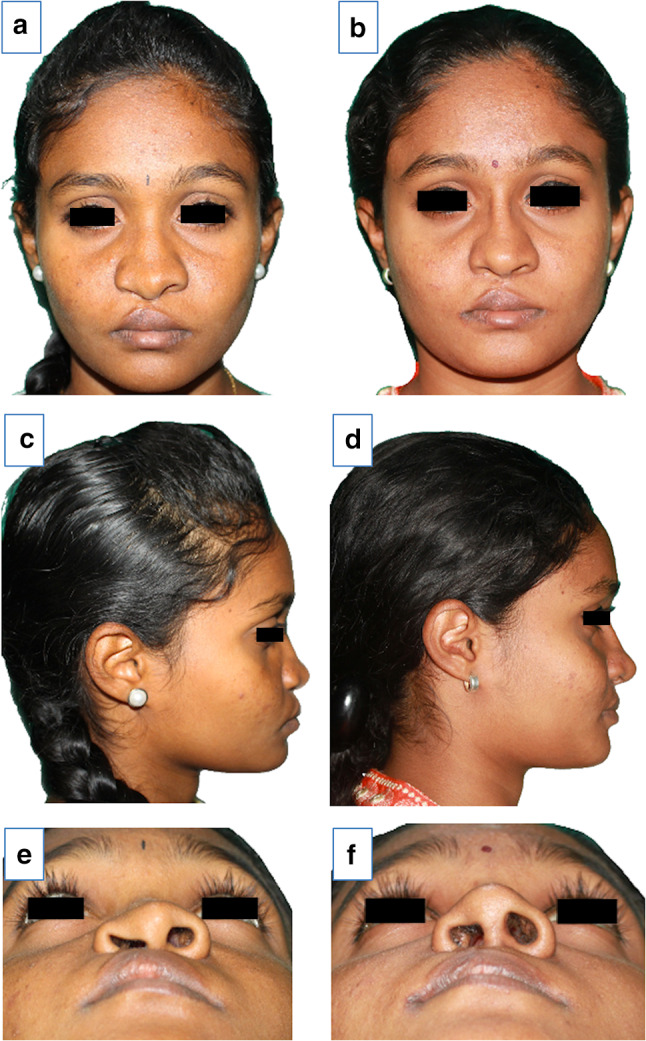
Adult unilateral cleft nose reconstruction includes manipulation of the bony pyramid and septal work with placement of cartilage grafts for support and reinforcement. Preoperative views prior to maxillary advancement and definitive rhinoplasty (a, c, e), and post-Le Fort 1 advancement and definitive rhinoplasty (b, d, f). (Picture courtesy—Mr N.A. Nasser)
In terms of long-term complications of unilateral cleft rhinoplasties, the most common will invariably be residual asymmetry. A bulbous, downturned tip is another. Septal deviation can also recur, or it may be residual septal deviation caused by the magnitude of the initial deformity [12]. Wound dehiscence, skin necrosis, exposure and migration of grafts are rare after meticulous repair. Subtle nostril size differences and a residual deformity apparent in the basal or worm’s eye view are a potential outcome that the patient should be made aware of.
Conclusion
Understanding the underlying mechanisms of this complex malformation is essential, so is acceding to the reality that despite our best efforts, there can be no ‘one-size-fits-all’ surgical panacea to this intricate problem. Primary intervention may mitigate the condition and lend the child a modicum of facial normalcy during childhood. But it would be prudent to be mindful that one might have to revisit the problem in the future. Intermediate rhinoplasty may not always be indicated and when it is, it should be performed to improve symmetry and function in a manner that does not further aggravate the deformity or inflict undue scarring. Definitive rhinoplasty should be the final step in the process, bearing in mind that nasal cartilages have notoriously potent memory, with a tendency to revert to its original state. Therefore, thorough dissection, use of robust grafts and meticulous planning of the skin drape is most critical.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Krishnamurthy Bonanthaya, Email: kbonanthaya@gmail.com.
Jazna Jalil, Email: jazna.jalil@gmail.com.
References
- 1.Fisher MD, Fisher DM, Marcus JR. Correction of the cleft nasal deformity: from infancy to maturity. Clin Plast Surg. 2014;41:283–299. doi: 10.1016/j.cps.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Blair VP, Brown JB. Nasal abnormalities, fancied and real. Int J Orthod Oral Surg Radiogr. 1932;18:363–401. doi: 10.1016/s0099-6963(32)80076-1. [DOI] [Google Scholar]
- 3.Huffman WC, Lierle DM. Studies on the pathologic anatomy of the unilateral harelip nose. Plast Reconstr Surg. 1949;4:225–234. doi: 10.1097/00006534-194905000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Fisher DM, Sommerlad BC. Cleft lip, cleft palate, and velopharyngeal insufficiency. Plast Reconstr Surg. 2011;128:342–360. doi: 10.1097/PRS.0b013e3182268e1b. [DOI] [PubMed] [Google Scholar]
- 5.Boo-Chai K, Tange I. The Origami cleft lip. Br J Plast Surg. 1970;23:248–253. doi: 10.1016/s0007-1226(70)80049-2. [DOI] [PubMed] [Google Scholar]
- 6.Hogan VM. The tilted tripod: a theory of unilateral cleft lip nasal deformity. In: Heuston JT, editor. Transactions of the Fifth International congress of plastic and reconstructive surgery. Melbourne: Butterworths; 1971. p. 382. [Google Scholar]
- 7.Fisher DM, Mann RJ. A model for the cleft lip nasal deformity. Plast Reconstr Surg. 1998;101:1448–1456. doi: 10.1097/00006534-199805000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Bardach J, Cutting C. Multidisciplinary management of cleft lip and palate. In: Bardach J, Morris HL, editors. Multidisciplinary management of cleft lip and palate. Philadelphia: Saunders; 1990. pp. 154–158. [Google Scholar]
- 9.Narayanan P, Adenwalla H. Primary rhinoplasty at the time of unilateral cleft lip repair: a review and our protocol. J Cleft Lip Palate Craniofac Anom. 2015;2:92. doi: 10.4103/2348-2125.162961. [DOI] [Google Scholar]
- 10.Lo LJ. Primary correction of the unilateral cleft lip nasal deformity: achieving the excellence. Chang Gung Med J. 2006;29:262–267. [PubMed] [Google Scholar]
- 11.McComb H. Treatment of the unilateral cleft lip nose. Plast Reconstr Surg. 1975;55:596–601. doi: 10.1097/00006534-197505000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Guyuron B. MOC-PS(SM) CME article: late cleft lip nasal deformity. Plast Reconstr Surg. 2008;121:1–11. doi: 10.1097/01.prs.0000305955.67554.40. [DOI] [PubMed] [Google Scholar]
- 13.LaRossa D, Donath G. Primary nasoplasty in unilateral and bilateral cleft nasal deformity. Clin Plast Surg. 1993;20:781–791. doi: 10.1016/S0094-1298(20)32384-1. [DOI] [PubMed] [Google Scholar]
- 14.Atherton JD. A descriptive anatomy of the face in human fetuses with unilateral cleft lip and palate. Cleft Palate J. 1967;4:104–114. [PubMed] [Google Scholar]
- 15.McComb H. Primary correction of unilateral cleft lip nasal deformity: a 10-year review. Plast Reconstr Surg. 1985;75:791–799. doi: 10.1097/00006534-198506000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Li A-Q, Sun Y-G, Wang G-H, et al. Anatomy of the nasal cartilages of the unilateral complete cleft lip nose. Plast Reconstr Surg. 2002;109:1835–1838. doi: 10.1097/00006534-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Kim YS, Cho HW, Park B-YY, Jafarov M. A comparative study of the medial crura of alar cartilages in unilateral secondary cleft nasal deformity: the validity of medial crus elevation. Ann Plast Surg. 2008;61:404–409. doi: 10.1097/SAP.0b013e318168db1c. [DOI] [PubMed] [Google Scholar]
- 18.Fisher DM, Lo LJ, Chen YR, Noordhoff MS. Three-dimensional computed tomographic analysis of the primary nasal deformity in 3-month-old infants with complete unilateral cleft lip and palate. Plast Reconstr Surg. 1999;103:1826–1834. doi: 10.1097/00006534-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Kaufman Y, Buchanan E, Wolfswinkel E, et al. Cleft nasal deformity and rhinoplasty. Semin Plast Surg. 2012;26:184–190. doi: 10.1055/s-0033-1333886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang TD. Secondary rhinoplasty in unilateral cleft nasal deformity. Clin Plast Surg. 2010;37:383–387. doi: 10.1016/j.cps.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 21.Wang TD. Secondary rhinoplasty in unilateral cleft nasal deformity. Facial Plast Surg. 2007;23:123–127. doi: 10.1055/s-2007-979281. [DOI] [PubMed] [Google Scholar]
- 22.Gillies H, Millard DR. The principles and art of plastic surgery. Boston: Little, Brown; 1966. [Google Scholar]
- 23.Cronin TD, Denkler KA. Correction of the unilateral cleft lip nose. Plast Reconstr Surg. 1988;82(3):419–432. doi: 10.1097/00006534-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Aufricht G (1955) Presentation at the annual meeting of the American Society of maxillo-facial surgeons, Philadelphia
- 25.Broadbent TR, Woolf RM. Cleft lip nasal deformity. Ann Plast Surg. 1984;12:216–234. doi: 10.1097/00000637-198403000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Gelbke H. The nostril problem in unilateral harelips and its surgical management. Plast Reconstr Surg. 1956;1946(18):65–75. doi: 10.1097/00006534-195607000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Anderl H, Hussl H, Ninkovic M. Primary simultaneous lip and nose repair in the unilateral cleft lip and palate. Plast Reconstr Surg. 2008;121:959–970. doi: 10.1097/01.prs.0000299942.84302.16. [DOI] [PubMed] [Google Scholar]
- 28.Salyer KE, Genecov ER, Genecov DG. Unilateral cleft lip-nose repair: a 33-year experience. J Craniofac Surg. 2003;14:549–558. doi: 10.1097/00001665-200307000-00030. [DOI] [PubMed] [Google Scholar]
- 29.Velazquez JM, Ortiz-Monasterio F. Primary simultaneous correction of the lip and nose in the unilateral cleft lip. Plast Reconstr Surg. 1974;54:558–563. doi: 10.1097/00006534-197411000-00006. [DOI] [PubMed] [Google Scholar]
- 30.McComb HK, Coghlan BA. Primary repair of the unilateral cleft lip nose: completion of a longitudinal study. Cleft Palate Craniofac J. 1996;33:21–23. doi: 10.1597/1545-1569_1996_033_0023_protuc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 31.Haddock NT, McRae MH, Cutting CB. Long-term effect of primary cleft rhinoplasty on secondary cleft rhinoplasty in patients with unilateral cleft lip-cleft palate. Plast Reconstr Surg. 2012;129:740–748. doi: 10.1097/PRS.0b013e3182402e8e. [DOI] [PubMed] [Google Scholar]
- 32.Sarnat BG, Wexler MR. Rabbit snout growth after resection of central linear segments of nasal septal cartilage. Acta Otolaryngol. 1967;63:467–478. doi: 10.3109/00016486709128781. [DOI] [PubMed] [Google Scholar]
- 33.Latham RA. The pathogenesis of the skeletal deformity associated with unilateral cleft lip and palate. Cleft Palate J. 1969;6:404–414. [PubMed] [Google Scholar]
- 34.Gosla-Reddy S, Nagy K, Mommaerts MY, et al. Primary septoplasty in the repair of unilateral complete cleft lip and palate. Plast Reconstr Surg. 2011;127:761–767. doi: 10.1097/PRS.0b013e318200a97a. [DOI] [PubMed] [Google Scholar]
- 35.Smahel Z, Mullerova Z, Nejedly A. Effect of primary repositioning of the nasal septum on facial growth in unilateral cleft lip and palate. Cleft Palate Craniofac J. 1999;36:310–313. doi: 10.1597/1545-1569_1999_036_0310_eoprot_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 36.Grayson BH, Maull D. Nasoalveolar molding for infants born with clefts of the lip, alveolus, and palate. Clin Plast Surg. 2004;31:149–158. doi: 10.1016/S0094-1298(03)00140-8. [DOI] [PubMed] [Google Scholar]
- 37.Grayson BH, Santiago PE, Brecht LE, Cutting CB. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft palate-craniofacial. J Off Publ Am Cleft Palate-Craniofac Assoc. 1999;36:486–498. doi: 10.1597/1545-1569_1999_036_0486_pnmiiw_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 38.Matsuo K, Hirose T, Otagiri T, Norose N. Repair of cleft lip with nonsurgical correction of nasal deformity in the early neonatal period. Plast Reconstr Surg. 1989;83:25–31. doi: 10.1097/00006534-198901000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Gomez DF, Donohue ST, Figueroa AA, Polley JW. Nasal changes after presurgical nasoalveolar molding (PNAM) in the unilateral cleft lip nose. Cleft Palate Craniofac J. 2012;49:689–700. doi: 10.1597/11-007. [DOI] [PubMed] [Google Scholar]
- 40.Subramanian CS, Prasad NKKK, Chitharanjan AB, Liou EJW. A modified presurgical orthopedic (nasoalveolar molding) device in the treatment of unilateral cleft lip and palate. Eur J Dent. 2016;10:435–438. doi: 10.4103/1305-7456.184146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liou EJW, Subramanian M, Chen PKT, Huang CS. The progressive changes of nasal symmetry and growth after nasoalveolar molding: a three-year follow-up study. Plast Reconstr Surg. 2004;114:858–864. doi: 10.1097/01.PRS.0000133027.04252.7A. [DOI] [PubMed] [Google Scholar]
- 42.Singh GD, Levy-Bercowski D, Yanez MA, Santiago PE. Three-dimensional facial morphology following surgical repair of unilateral cleft lip and palate in patients after nasoalveolar molding. Orthod Craniofac Res. 2007;10:161–166. doi: 10.1111/j.1601-6343.2007.00390.x. [DOI] [PubMed] [Google Scholar]
- 43.Barillas I, Dec W, Warren SM, et al. Nasoalveolar molding improves long-term nasal symmetry in complete unilateral cleft lip-cleft palate patients. Plast Reconstr Surg. 2009;123:1002–1006. doi: 10.1097/PRS.0b013e318199f46e. [DOI] [PubMed] [Google Scholar]
- 44.Chang CS, Por YC, Liou EJW, et al. Long-term comparison of four techniques for obtaining nasal symmetry in unilateral complete cleft lip patients: a single surgeon’s experience. Plast Reconstr Surg. 2010;126:1276–1284. doi: 10.1097/PRS.0b013e3181ec21e4. [DOI] [PubMed] [Google Scholar]
- 45.Lonic D, Morris DE, Lo L-J. Primary overcorrection of the unilateral cleft nasal deformity: quantifying the results. Ann Plast Surg. 2016;77(Suppl 1):S25–S29. doi: 10.1097/SAP.0000000000000708. [DOI] [PubMed] [Google Scholar]
- 46.Allori AC, Mulliken JB. Evidence-based medicine: secondary correction of cleft lip nasal deformity. Plast Reconstr Surg. 2017;140:166e–176e. doi: 10.1097/PRS.0000000000003475. [DOI] [PubMed] [Google Scholar]
- 47.Trott JA, Mohan N. A preliminary report on one stage open tip rhinoplasty at the time of lip repair in bilateral cleft lip and palate: the Alor Setar experience. Br J Plast Surg. 1993;46:215–222. doi: 10.1016/0007-1226(93)90171-7. [DOI] [PubMed] [Google Scholar]
- 48.Thomas C, Mishra P. Open tip rhinoplasty along with the repair of cleft lip in cleft lip and palate cases. Br J Plast Surg. 2000;53:1–6. doi: 10.1054/bjps.1999.3248. [DOI] [PubMed] [Google Scholar]
- 49.Mulliken JB, Martinez-Perez D. The principle of rotation advancement for repair of unilateral complete cleft lip and nasal deformity: technical variations and analysis of results. Plast Reconstr Surg. 1999;104:1247–1260. doi: 10.1097/00006534-199910000-00003. [DOI] [PubMed] [Google Scholar]
- 50.Burget GC. Secondary cleft surgery. In: Losee JE, Kirschner RE, editors. Comprehensive cleft care. 2. Stuttgart: Georg Thieme; 2016. pp. 1063–1069. [Google Scholar]
- 51.Hsieh T, Dedhia R, Del Toro D, Tollefson TT. Cleft septorhinoplasty: form and function. Facial Plast Surg Clin North Am. 2017;25:223–238. doi: 10.1016/j.fsc.2016.12.011. [DOI] [PubMed] [Google Scholar]