Abstract
Objective
To describe patient preparation for routine outpatient blood work and examine the implications of surreptitious fasting on interpretation of glucose results.
Patients and Methods
We designed a survey and administered it between September 1, 2016, and April 30, 2017, to assess fasting behaviors in a convenience sample of 526 adults presenting for outpatient blood work in 2 health systems between 7 am and 12 pm. We reviewed the electronic health records to extract glucose results. We describe the frequency of clinician-directed fasting and surreptitious fasting. In those surreptitiously fasting, we describe the frequency of missed diagnoses of prediabetes and diabetes.
Results
Of 526 participants, 330 (62.7%) self-identified as fasting, and 304 (92.1%) of those fasting met American Diabetes Association fasting criteria. Only 131 (24.9%) of those fasting were told to fast by their health care team. Almost 50% (257 of 526) believed it was important to fast for every blood test. Of the 64 patients with diabetes who were taking insulin, 37 (57.8%) fasted and took their insulin as prescribed. Among the 89 patients without diabetes who fasted without knowledge of their health care team and had glucose tested, 2 (2.2%) had a missed diagnosis of diabetes and 18 (20.2%) had a missed diagnosis of prediabetes.
Conclusion
Fasting for outpatient blood work is common, and patients frequently fast without awareness of their health care team. Failure to capture fasting status at the time of glucose testing is a missed opportunity to identify undiagnosed cases of diabetes and prediabetes.
Abbreviations and Acronyms: ADA, American Diabetes Association; EHR, electronic health record; HbA1c, hemoglobin A1c
Fasting blood work is a common component of preventive examinations in outpatient medicine. However, clinician utilization of fasting laboratory tests and patient fasting practices are poorly understood. Clinicians frequently instruct patients to fast for their blood work, and patients may also fast for blood work without the knowledge of their clinician. Historically, patients were required to fast for 2 key purposes: (1) to screen for, diagnose, and monitor hyperlipidemia and (2) to screen for and diagnose prediabetes and type 2 diabetes.1, 2, 3 Multiple studies have reported that fasting has limited impact on lipid measurement and prediction of cardiovascular risk.4, 5, 6, 7 As a result, clinical guidelines no longer recommend fasting for routine lipid screening.8,9
Fasting blood glucose level remains an important criterion-standard screening and diagnostic test for type 2 diabetes and is one of the few indications for fasting laboratory tests.3 Although hemoglobin A1c (HbA1c) is a commonly ordered screening and diagnostic test because it does not require patients to fast, many clinicians continue to utilize fasting glucose level as part of their testing strategy because fasting glucose and HbA1c identify different groups of people with diabetes and prediabetes.10 Additionally, concurrent measurement of HbA1c and fasting glucose levels on the same day can confirm a diagnosis of diabetes without requiring patients to return for follow-up testing.10,11
Laboratory protocols to assess and document patients’ fasting state at the time of phlebotomy are inconsistent or nonexistent, and these data are not routinely captured in the electronic health record (EHR). Failure to capture the fasting state of patients prohibits clinicians from identifying fasting glucose values and interpreting them in accordance with diabetes screening guidelines. This failure may result in missed diagnoses of type 2 diabetes and prediabetes. Therefore, we conducted a survey and structured medical record review of patients presenting for routine outpatient laboratory testing in 2 health systems to describe utilization of fasting laboratory tests, understand patient fasting practices, and assess the implications of surreptitious fasting without clinician awareness on the interpretation of glucose values and missed diagnoses of prediabetes and type 2 diabetes.
Patients and Methods
Study Design and Participants
We conducted a cross-sectional survey to characterize patients’ beliefs about fasting blood work and their preparation for routine laboratory testing. We surveyed a convenience sample of patients presenting to the outpatient laboratory for routine ambulatory blood work at a large, academic medical center and 2 community-based clinics within an integrated safety-net health care system between September 1, 2016, and April 30, 2017. English- or Spanish-speaking adults aged 18 years or older presenting to the outpatient laboratory for routine blood work between 7:00 am and 12:00 pm were eligible for participation. At the time of this study, the outpatient laboratories included in the study did not have standardized protocols to assess and document patients’ fasting states in the EHR.
Survey Design and Administration
Potential survey items were generated and drafted following literature review and stakeholder engagement with patients, laboratory staff, clinical staff, and clinicians. Patient and clinical stakeholders reviewed candidate questions for content and clarity. The final survey (Supplemental Appendix 1, available online at http://www.www.mcpiqojournal.org) included 11 questions assessing 3 key domains: (1) patient preparation for laboratory work, (2) instructions given for laboratory testing, and (3) understanding and perceived importance of fasting. The survey was translated into Spanish by a bilingual research assistant and pilot tested with native Spanish speakers prior to use.
Research assistants approached patients in the laboratory waiting area to assess eligibility and obtain consent for surveys and medical record reviews. All surveys were orally administered in the patients’ preferred language (English or Spanish) by a language-concordant research assistant. Following survey completion, we reviewed each participants EHR data 72 hours after completion of the laboratory visit. We extracted patient demographic characteristics and comorbidities, documentation of fasting instructions in the 30 days prior to the laboratory visit, and laboratory results (glucose, HbA1c, and lipid levels) from the day of the survey and laboratory visit. Fasting instructions were extracted from telephone encounters, patient portal messages, the physician progress notes, after-visit summaries, and patient instructions. All survey responses and extracted EHR data were entered into REDCap (Research Electronic Data Capture), a secure Web application for survey and data management.12
Statistical Analyses
We describe patient demographic characteristics, comorbidities, and fasting practices according to patient-reported fasting states using χ2 test, Fisher exact test, and t test as appropriate. Participants responding “yes” to the question, “Did you fast for your blood test today?” were considered fasting. We categorized patients as meeting the American Diabetes Association’s (ADA) criterion-standard fasting definition if they reported nothing to eat or drink except water for at least 8 hours prior to laboratory testing.13
We performed 2 subgroup analyses. First, we describe the frequency of fasting and hypoglycemia (glucose level, <70 mg/dL; to convert values to mmol/L, multiple by 0.0555) among patients with diagnosed diabetes (type 1 and type 2 diabetes). Diabetes and prediabetes were defined using patient-reported data on the survey questionnaire. Second, in patients without diagnosed dysglycemia (diabetes and prediabetes), we describe the frequency of missed dysglycemia using fasting blood glucose criteria (fasting blood glucose, ≥100 mg/dL) in patients who met ADA fasting criteria but were not instructed to fast by their clinician. All participants provided informed consent, and no incentives were provided. Data were analyzed using Stata statistical software, version 12 (StataCorp). This study was approved by the University of Texas Southwestern Medical Center Institutional Review Board.
Results
Of the 958 patients invited to participate during the study period, a total of 526 completed the survey, for a response rate of 54.9%. Most of the surveys were completed before 10 AM (371 of 526; 70.6%), at the academic center (407; 77.4%), and in English (471; 89.7%). On average, participants were 51 years old and had a body mass index (calculated as weight in kilograms divided by height in meters squared) of 30.1 kg/m2. Of the 526 participants, 342 (65.1%) were female, 229 (43.5%) were non-Hispanic white, 127 (24.1%) were Hispanic, and 100 (19.0%) were black. Common comorbidities included hypertension (235 [44.7%]), hyperlipidemia (188 [35.7%]), previously diagnosed diabetes (132 [25.1%]), and history of myocardial infarction (39 [7.4%]) (Table 1).
Table 1.
Patient Characteristics According to Self-Reported Fasting State at the Time of Routine Outpatient Blood Worka,b
| Variable | Total population (N=526) | Fasting (n=330) | Not fasting (n=196) | P value |
|---|---|---|---|---|
| Age (y) | 51.0±16 | 51.3±15 | 50.4±17 | .56 |
| BMI (kg/m2) (N=501) | 30.1±7.4 | 30.7±7.4 | 29.2±7.4 | .028 |
| Female | 342 (65.1) | 208 (60.8) | 134 (39.2) | .23 |
| Race/ethnicity | .06 | |||
| Non-Hispanic white | 229 (43.5) | 132 (40.0) | 97 (49.5) | |
| Hispanic white | 127 (24.1) | 92 (27.9) | 35 (17.9) | |
| Black | 100 (19.0) | 60 (18.2) | 40 (20.4) | |
| Asian | 16 (3.0) | 12 (3.6) | 4 (2.0) | |
| Other/unknown | 54 (10.3) | 34 (10.3) | 20 (10.2) | |
| Prediabetes | 25 (4.8) | 17 (5.2) | 8 (4.1) | .58 |
| Diagnosis of hypertension | 235 (44.7) | 149 (45.2) | 86 (43.9) | .78 |
| Diagnosis of hyperlipidemia | 188 (35.7) | 129 (39.1) | 59 (30.1) | .04 |
| History of MI | 39 (7.4) | 22 (6.7) | 17 (8.7) | .28 |
| History of heart failure | 57 (10.8) | 36 (10.9) | 21 (10.7) | .37 |
| History of CVA | 22 (4.2) | 14 (4.2) | 8 (4.1) | .41 |
| FH diabetes | 227 (43.2) | 147 (44.4) | 81 (41.3) | .56 |
| Diagnosed DMc | 132 (25.1) | 85 (25.8) | 47 (24.0) | .57 |
| Use of insulind | 255 (48.5) | 144 (43.5) | 113 (57.5) | .13 |
| Use of oral hypoglycemicsd | 311 (59.1) | 214 (64.7) | 96 (48.9) | .08 |
| Use of statins | 182 (34.6) | 114 (34.6) | 68 (34.7) | .97 |
| Lipids checked on day of survey | 216 (41.1) | 173 (52.4) | 43 (21.9) | <.005 |
| Glucose checked on day of survey | 330 (62.7) | 221 (67.0) | 109 (55.6) | .01 |
| HbA1c checked on day of survey | 160 (30.4) | 118 (35.8) | 42 (21.4) | .001 |
BMI = body mass index; CVA = cerebrovascular accident; DM = diabetes mellitus; FH = family history; HbA1c = hemoglobin A1c; MI = myocardial infarction.
Data are presented as mean ± SD or No. (percentage) of participants.
Self-reported diabetes diagnosis.
Denominator =132 patients with diabetes.
Overall, 330 of the 526 patients (62.7%) reported fasting at the time of their blood draw. Almost all of the 330 participants who self-reported fasting (304 [92.1%]) met the criterion-standard ADA fasting criteria of nothing to eat or drink except water for at least 8 hours before testing.13 Overall, participants who reported they were fasting were similar to those who were not fasting. However, those who were fasting had a higher body mass index, were more likely to have hyperlipidemia, and were significantly more likely to have cholesterol (P<.005), glucose (P=.01), and HbA1c (P=.001) testing on the day of the survey (Table 1).
Nearly half of all participants (257 of 526 [48.9%]) believed that it was important to fast for every blood test regardless of whether or not they received instructions to fast from their health care team, and these patients were more likely to self-report fasting for laboratory tests on the day of the survey (P<.001). The criterion-standard ADA fasting definition used in this study has 2 components: (1) what patients reported eating or drinking and (2) how long they went without intake. Patient-defined fasting criteria almost universally excluded food and beverages with cream or sugar. Nearly half accurately defined fasting intake as “water only.” However, 221 (42.0%) believed that fasting meant that they were not allowed to have anything to eat or drink, including water. For the duration of fasting, the most common definitions were at least 8 hours or after midnight (Table 2).
Table 2.
Patient Beliefs About Fasting According to Self-Reported Fasting Statusa
| Patient beliefs | Total population, No. (%) (N=526) | Fasting, No. (%) (n=330) | Not fasting, No. (%) (n=196) |
|---|---|---|---|
| Fasting important for every blood test | 257 (48.9) | 160 (62.4) | 97 (37.6) |
| Intake allowed while fasting | |||
| Nothing to eat or drink | 221 (42.0) | 132 (40.0) | 89 (45.6) |
| Water only | 250 (47.5) | 160 (48.5) | 90 (45.9) |
| Black coffee or tea | 50 (9.5) | 33 (10.0) | 15 (7.5) |
| Coffee or tea with cream/sugar | 5 (0.9) | 3 (0.9) | 0 (0) |
| Eating allowed | 1 (0.1) | 2 (0.6) | 2 (1.0) |
| Time required for fasting (h) | |||
| 0-3 | 23 (4.4) | 8 (2.5) | 20 (10.4) |
| 4-8 | 22 (4.2) | 11 (3.4) | 13 (6.6) |
| >8 | 258 (49.1) | 175 (53.1) | 72 (36.8) |
| After midnight | 222 (42.3) | 135 (41.0) | 91 (46.2) |
Although 330 (62.7%) of the 526 participants in our survey self-reported fasting, only 131 (24.9%) were told to fast by their health care team. Of the 131 who were told to fast, only 84 (64.1%) reported receiving specific instructions for fasting, and only 14 (11.3%) had documentation of fasting instructions in the EHR recorded between their most recent clinic visit and the date of the laboratory visit. When fasting instructions were documented, all were instructed to avoid food intake for at least 8 hours or after midnight. Drinking instructions varied from water only, black coffee or tea, or nothing to drink. We found no documentation of instructions regarding medication administration while fasting.
Of the 132 patients with diagnosed diabetes, 78 (59.1%) were prescribed an oral diabetes medication and 64 (48.5%) were prescribed insulin. Of the 78 taking oral diabetes medications, 63 (81.4%) reported taking their medications as prescribed in the preceding 24 hours and 56 (71.8%) were fasting at the time of the blood draw. Of the 64 patients taking insulin, 59 (91.5%) reported taking their insulin as prescribed in the preceding 24 hours and 37 (57.8%) were fasting at the time of their blood draw. Nearly 30% (19) of participants taking insulin had a concurrent lipid panel and were told to fast by their health care team. The frequency of hypoglycemia (glucose <70 mg/dL) in patients with diagnosed diabetes was low (n=2).
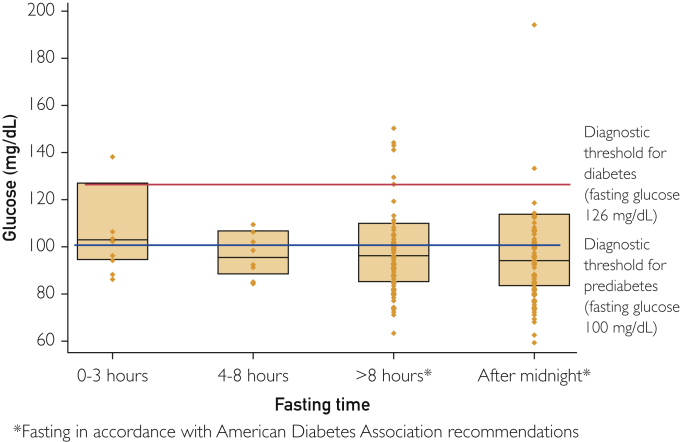
Among the 228 patients without previously diagnosed prediabetes or diabetes who had glucose tested, most satisfied the ADA fasting definition (Figure). Of the 181 patients who met the ADA criterion-standard fasting definition, the overall yield of fasting glucose was 9 (5.0%) for diabetes and 51 (28.2%) for prediabetes. Of these 181 patients, 89 (49.2%) fasted without being told to do so by their health care team. These tests represent missed criterion-standard diabetes screening tests that went unrecognized because the health care team was not aware that the patient was fasting. Interpreting the test results of these 89 patients who fasted without awareness of their health care team according to ADA glucose fasting criteria, 2 (2.2%) had a missed diagnosis of diabetes (fasting blood glucose ≥126 mg/dL) and 18 (20.2%) had prediabetes (fasting blood glucose, 100-125 mg/dL). None of these patients had an HbA1c or oral glucose tolerance test on the same day as the fasting glucose test.
Figure.
Distribution of glucose values by fasting time in patients without diagnosed diabetes or prediabetes.
Discussion
In this cross-sectional survey of patients presenting for routine outpatient laboratory testing, we found that over 60% of patients fasted for blood work despite infrequently receiving fasting instructions from their health care team. Nearly all patients who reported fasting met the ADA fasting definition, suggesting that improved processes to capture and indicate fasting status for routine laboratory testing could improve interpretation of glucose values and identification of prediabetes and type 2 diabetes in clinical practice. Standardized patient instructions for fasting laboratory tests—including instructions for medication administration and water intake—are needed to improve patient safety and acceptability of fasting. Partnership with laboratory personnel to establish clear protocols for fasting assessment and documentation are needed to allow accurate interpretation of glucose values and decrease missed diagnoses of prediabetes and diabetes.
Despite rarely receiving instructions from their health care team, patients frequently fast for laboratory work on their own accord because they perceive that it is important. This issue may reflect a legacy effect from the era when patients were routinely told to fast for lipid testing. Over 40% of patients defined fasting according to the common procedural or surgical instructions of nothing to eat or drink after midnight. Overall, patient understanding of the duration of fasting is high, although nearly half believed that fasting meant nothing to eat or drink at all—including water. The lack of guidance from the health care team helps perpetuate patient misconceptions of fasting, resulting in care that is not patient centered and unnecessarily inconveniences patients.
Patients who fast without instructions from their health care team have the potential for medication-related adverse health events. Among those with diagnosed type 2 diabetes, we found that over 90% taking insulin and over 80% taking oral hypoglycemics took their medications as prescribed on the day of their labwork, and 58% of those taking insulin and 72% of those taking oral hypoglycemics reported fasting. Although we only found 2 cases of hypoglycemia on medical record review, as many as 25% of patients with diabetes report hypoglycemic events while preparing for fasting blood work.14,15 In our study, laboratory personnel reported frequent hypoglycemic events requiring treatment while patients were waiting for phlebotomy, which may contribute to the low rate of hypoglycemia observed in our study. Such events can be easily avoided in patients with diagnosed diabetes because they have no clear indication to fast since nonfasting lipid levels are suitable for clinical decision making.4,7,9 Thus, for patients with diagnosed diabetes, fasting is a high-risk practice with no clinical indication or benefit.
In patients without diagnosed diabetes or prediabetes, surreptitious fasting without clinician awareness contributes to missed opportunities to diagnose prediabetes and type 2 diabetes. Most patients who fasted in our study satisfied the ADA fasting criteria. Thus, their glucose measurements were true fasting glucose values and diabetes screening tests even though this information was not collected by the laboratory team or indicated in the EHR with the laboratory result. Therefore, unless physicians in this study specifically contacted patients after laboratory testing to inquire about fasting status at the time of testing, they would be unaware that glucose values were true fasting glucose values and assume patients were not fasting. Improved detection of undiagnosed diabetes and prediabetes is necessary for adequate population health management because 25% of US adults with diabetes and 90% with prediabetes have yet to be diagnosed.16 Among patients in our study without diagnosed diabetes who had glucose measured, 2.2% had a missed diagnosis of diabetes, which is similar to the overall prevalence of undiagnosed diabetes in the United States.17 An additional 20.2% had a missed diagnosis of prediabetes, which is similar to reported rates of undiagnosed prediabetes in clinical practice.18 The 22.4% overall diagnostic error rate for glycemic abnormalities in our study is much higher than the 5% diagnostic error rate reported for colorectal and lung cancer screening.19 Clinical consequences associated with diagnostic errors for prediabetes and type 2 diabetes include missed opportunities for counseling on lifestyle modification and diabetes prevention interventions for those with prediabetes and a delay in diabetes treatment and screening for diabetes-related complications. The failure to capture fasting status at the time of glucose testing also limits the ability of clinical researchers and population health teams to accurately identify patients with prediabetes for diabetes surveillance and targeting preventive interventions.
Development of standardized patient instructions for patients when fasting is clearly indicated, and deemphasizing fasting blood work to patients when it is not indicated can improve the patient centeredness of routine laboratory testing. When fasting is indicated, instructions should clearly define a time period and emphasize that water intake is allowed. Additionally, the instructions should recommend that most medications, with the exception of insulin and oral hypoglycemics, should be taken as prescribed. By avoiding fasting laboratory tests when not clearly indicated, clinicians help reduce the risk of hypoglycemia in patients with diagnosed diabetes and can increase patient flexibility and convenience for laboratory testing. Development of laboratory protocols to routinely assess fasting status and documentation in the EHR are needed to allow clinicians to accurately interpret glucose values on routine testing. Given the high frequency of surreptitious patient fasting, assessing the fasting state of all patients with a single yes/no question such as, “Have you had anything to eat or drink besides water in the past 8 hours?” is preferable to the use of fasting orders in the EHR that identify fasting laboratory tests. Fasting orders capture the intent of the order but not the patient’s fasting state unless laboratory personnel routinely assess and document it in the EHR.
Our study has several strengths, including surveying patients in 2 different health systems and review of the EHR for fasting instructions and laboratory results. However, our study is not without limitations. First, we required documentation of fasting instructions, which likely underestimates the frequency of instructions provided to patients in clinical settings. However, by asking patients if they received fasting instructions from their health care team, we captured the actual patient receipt and retention of instructions, which is more important than providing instructions in verbal or written format. Second, our findings likely underestimate the frequency of hypoglycemia because symptomatic patients may have been treated for hypoglycemic episodes prior to phlebotomy. Lastly, our study may overestimate the rate of missed diagnoses of prediabetes and diabetes because we did not interview physicians about their interpretation of the test results or conduct a medical record review of future clinic visits to capture subsequent diagnoses.
Conclusion
Patients commonly fast for routine blood work without receiving instructions to do so from their health care team, and many fast according to recommended ADA fasting instructions for diabetes screening. However, clinician unawareness of patient fasting and lack of standardized clinic and laboratory processes to assess and document fasting practices contribute to diagnostic errors in interpreting glucose values. These factors result in substantial rates of missed diagnoses of diabetes and prediabetes. Development of standardized fasting instructions and laboratory protocols for assessment and documentation of fasting practices are needed to improve the patient experience and minimize errors. Furthermore, we propose that clinicians deemphasize the need for fasting blood work unless it is clinically indicated and the documentation of fasting behaviors are available to allow accurate interpretation of test results.
Acknowledgments
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Grant Support: This work was supported in part by Dr. Bowen was supported by the National Institutes of Health NIDDK K23 DK104065, UT Health System Patient Safety Research Grant OGC 150272, the University of Texas Southwestern CTSA NIH Grant UL1TR001105, and the Dedman Family Scholars in Clinical Care (M.E.B.) It was also supported by the Community Health Fellowship Program This grant utilized resources from the University of Texas Southwestern CTSA NIH Grant UL1-RR024982 (J.T.).
Potential Competing Interests: The authors report no competing interests.
Supplemental material can be found online at http://www.mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. [PubMed] [Google Scholar]
- 2.International Expert Committee International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–1334. doi: 10.2337/dc09-9033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2018. Diabetes Care. 2018;41(suppl 1):S13–S27. doi: 10.2337/dc18-S002. [DOI] [PubMed] [Google Scholar]
- 4.Langsted A., Freiberg J.J., Nordestgaard B.G. Fasting and nonfasting lipid levels: influence of normal food intake on lipids, lipoproteins, apolipoproteins, and cardiovascular risk prediction. Circulation. 2008;118(20):2047–2056. doi: 10.1161/CIRCULATIONAHA.108.804146. [DOI] [PubMed] [Google Scholar]
- 5.Martin S.S., Blaha M.J., Elshazly M.B., et al. Friedewald-estimated versus directly measured low-density lipoprotein cholesterol and treatment implications. J Am Coll Cardiol. 2013;62(8):732–739. doi: 10.1016/j.jacc.2013.01.079. [DOI] [PubMed] [Google Scholar]
- 6.Mora S., Rifai N., Buring J.E., Ridker P.M. Fasting compared with nonfasting lipids and apolipoproteins for predicting incident cardiovascular events. Circulation. 2008;118(10):993–1001. doi: 10.1161/CIRCULATIONAHA.108.777334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mora S., Chang C.L., Moorthy M.V., Sever P.S. Association of nonfasting vs fasting lipid levels with risk of major coronary events in the Anglo-Scandinavian Cardiac Outcomes Trial-Lipid Lowering Arm. JAMA Intern Med. 2019;179(7):898–905. doi: 10.1001/jamainternmed.2019.0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farukhi Z., Mora S. Is it time to abandon fasting for routine lipid testing? Cleve Clin J Med. 2017;84(12):919–922. doi: 10.3949/ccjm.84a.16135. [DOI] [PubMed] [Google Scholar]
- 9.Grundy S.M., Stone N.J., Bailey A.L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary; a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in J Am Coll Cardiol. 2019;73(24):3234-3237] J Am Coll Cardiol. 2019;73(24):3168–3209. doi: 10.1016/j.jacc.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Cowie C.C., Rust K.F., Ford E.S., et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006 [published correction appears in Diabetes Care. 2011;34(10):2338] Diabetes Care. 2009;32(2):287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Selvin E., Wang D., Matsushita K., Grams M.E., Coresh J. Prognostic implications of single-sample confirmatory testing for undiagnosed diabetes: a prospective cohort study. Ann Intern Med. 2018;169(3):156–164. doi: 10.7326/M18-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Diabetes Association 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(suppl 1):S13–S28. doi: 10.2337/dc19-S002. [DOI] [PubMed] [Google Scholar]
- 14.Aldasouqi S., Corser W., Abela G.S., et al. Fasting for laboratory tests poses a high risk of hypoglycemia in patients with diabetes: a pilot prevalence study in clinical practice. Int J Clin Med. 2016;7(10):653–667. [Google Scholar]
- 15.Aldasouqi S., Sheikh A., Klosterman P., et al. Hypoglycemia in patients with diabetes on antidiabetic medications who fast for laboratory tests [published correction appears in Diabetes Care. 2011;34(8):1887] Diabetes Care. 2011;34(5):e52. doi: 10.2337/dc10-2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention National Diabetes Statistics Report, 2017: Estimates of Diabetes and Its Burden in the United States. Centers for Disease Control and Prevention website. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf Accessed February 25, 2020.
- 17.Menke A., Casagrande S., Geiss L., Cowie C.C. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021–1029. doi: 10.1001/jama.2015.10029. [DOI] [PubMed] [Google Scholar]
- 18.O'Brien M.J., Lee J.Y., Carnethon M.R., et al. Detecting dysglycemia using the 2015 United States Preventive Services Task Force screening criteria: a cohort analysis of community health center patients. PLoS Med. 2016;13(7):e1002074. doi: 10.1371/journal.pmed.1002074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh H., Meyer A.N., Thomas E.J. The frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving US adult populations. BMJ Qual Saf. 2014;23(9):727–731. doi: 10.1136/bmjqs-2013-002627. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.