Abstract
Aim
Three‐dimensional (3D) nonfluoroscopic mapping systems (NMSs) are generally used during the catheter ablation (CA) of complex arrhythmias. We evaluated the efficacy, safety, and economic advantages of using NMSs during His‐Bundle CA (HB‐CA).
Methods
A total of 124 consecutive patients underwent HB‐CA between 2012 and 2019 in our EP Laboratory. We compared two groups: 63 patients who underwent HB‐CA with fluoroscopy alone from 2012 to 2015 (Group I) and 61 patients who underwent HB‐CA with the aid of NMSs from 2016 to 2019 (Group II). Two cost‐effectiveness analyses were carried out: the alpha value (AV) (ie, a monetary reference value of the units of exposure avoided, expressed as $/man Sievert) and the value of a statistical life (VSL) (ie, the amount of money that a community would be willing to pay to reduce the risk of a person's death owing to exposure to radiation, it is not the cost value of a person's life). The cost reduction estimated by means of both these methods was compared with the real additional cost of using NMSs.
Results
The use of NMS resulted in reduced fluoroscopy time in Group II {median 1.35 min} in comparison with Group I {median 4.8 min (P < .05)}. The effective dose reduction (ΔE) was 1.16 milli‐Sievert.
Conclusion
The use of NMS significantly reduces fluoroscopy time. However, the actual reduction is modest and in our EP Laboratory this reduction is not cost‐effective. Indeed, when the ΔE is referred to country and agency tables for absolute values of AV or VLS, it is not economically advantageous in almost all cases.
Keywords: cost‐effectiveness, electroanatomic mapping system, electrophysiological procedures, His‐Bundle catheter ablation
We evaluated the efficacy, safety and economic advantages of using 3D non‐fluoroscopic mapping systems during His‐Bundle CA.The use of mapping systems significantly reduces fluoroscopy time. However, the actual reduction is modest and it is not cost‐effective.

1. INTRODUCTION
His‐bundle catheter ablation (HB‐CA) and the implantation of a pacemaker is a well‐established rate control therapy in atrial fibrillation (AF) when medications fail to control ventricular rate (Ablate and Pace Strategy). This type of procedure is relatively simple and fast, and has a low complication rate. The ESC 2016 guidelines assign a Class IIa (B) indication for HB‐CA in this type of AF patient. 1
Radiofrequency is the most commonly used energy source in catheter ablations in general, and fluoroscopy is used for catheter placement. However, exposure to radiation increases the lifetime risk of malignancies and genetic defects in patients and operators. 2
In the last 20 years, several studies have shown that the use of three‐dimensional (3D) nonfluoroscopic mapping systems (NMSs) during catheter ablation (CA) is safe and effective for the treatment of complex and simple arrhythmias in children and adults. In addition, their use permits a significant reduction in X‐Ray exposure. 3 , 4 , 5 , 6 , 7
In our previous papers, we reported that the systematic use of NMSs could dramatically reduce X‐Ray exposure during CA procedures 8 ; in our practice, however, this approach is economically advantageous only in the treatment of complex arrhythmias. 9
The literature contains no studies on the use of NMSs during HB‐CA procedures. The aim of the present study was to evaluate the efficacy, safety, radiation exposure and economic advantages of the systematic use of NMSs during HB‐CA in patients with AF refractory to medical treatment in comparison with the standard procedure, which uses fluoroscopy alone.
2. METHODS
2.1. Study population
This study was a retrospective analysis that involved 124 consecutive patients (pts) with AF refractory to medical treatment who underwent HB‐CA procedures from 2012 to 2019. We compared the fluoroscopy data from two groups: 63 pts who underwent HB‐CA with fluoroscopy (FL) alone from 2012 to 2015 (Group I) and 61 pts who underwent HB‐CA with the additional aid of NMSs (EnSite NavXTM St. Jude Medical, St Paul, MN, USA or CARTO3, Biosense‐Webster, Diamond Bar, CA, USA) from 2016 to 2019 (Group II). The baseline patient characteristics of the two groups were also analyzed (Table 1).
TABLE 1.
Baseline characteristics of the two groups and statistically significant (P‐value) differences between Groups I and II
| Patients | Group I (fluoroscopy) | Group II (NMS) | P‐value | |
|---|---|---|---|---|
| 63 | 61 | |||
| Age | Mean [years] | 76.8 | 74.9 | P = NS |
| BMI | Mean [kg/m2] | 25.7 | 26.4 | P = NS |
| GENDER | F | 30 | 29 | P = NS |
| M | 33 | 32 | ||
| Heart disease | None | 4 | 8 | P = NS |
| Hypertensive | 11 | 9 | ||
| Valvular | 15 | 7 | ||
| Ischemic | 15 | 16 | ||
| Dilated cardiomyopathy | 9 | 12 | ||
| Other | 9 | 9 | ||
| LVEF | <35% | 21 | 16 | P = NS |
| >55% | 18 | 23 | ||
| 35%–44% | 10 | 6 | ||
| 45%–55% | 14 | 16 | ||
| NYHA | I | 6 | 8 | P = NS |
| II | 18 | 25 | ||
| III | 38 | 27 | ||
| IV | 1 | 1 | ||
| DEVICE | ICD dual chamber | 2 | 1 | P = NS |
| ICD CRT | 20 | 17 | ||
| ICD single chamber | 2 | 3 | ||
| PMK dual chamber | 15 | 18 | ||
| PMK CRT | 5 | 3 | ||
| PMK single chamber | 19 | 19 | ||
Prior to each procedure, we obtained the written informed consent of the patient. The procedures were performed as described in our previous paper. 8
2.2. Fluoroscopy and procedure data
In this study, we compared fluoroscopy time and total X‐ray exposure. Fluoroscopy time (FT) was defined as the cumulative duration of fluoroscopy during the entire procedure, whereas the patient's radiation dose was assessed as the recorded dose‐area product (DAP). Procedure Time (PT) was measured as the interval from the initial recording of intracardiac signals to the final ECG recording before the end of the procedure.
2.3. Statistical analysis
Nonparametric Mann‐Whitney tests (MW‐test) were performed to compare all continuous variables and to exam median values between the groups. The χ 2 test was used to compare categorical variables. Statistical analyses were conducted by means of R software, Version 3.4.3 10 (The R Foundation for Statistical Computing). A P < .05 was considered significant.
2.4. Economic analysis
The economic impact of the X‐ray dose reduction resulting from the use of NMSs in CA procedures was analyzed by means of two methods: the alpha‐value (AV)‐based method and the value of a statistical life (VSL)‐based method. These two methods have been well described in two of our previous papers. 9 , 11
The definitions of the methods and the final formulas are summarized below.
The AV‐based method adopts the concept of the alpha‐value (AV) parameter. AV represents a monetary reference value of units of exposure avoided and can be expressed as € or $/manSievert ($/man‐Sv). A limitation of the AV‐based method is the range of values that the AV can have in different countries. In 2018, the Information System on Occupational Exposure (ISOE) of the European Technical Centre published the latest updated survey, conducted from May to July 2017 in order to collect the different AV values used by regulatory bodies. In most cases, regulatory authorities reported that they did not recommend a monetary value of the AV, whereas only three nuclear regulatory authorities—the British Office for Nuclear Regulation, the Slovak Public Health Authority, and the Czech State Office for Nuclear Safety—reported recommendations on the use of AV. 12 In order to obtain a wider and more complete picture, we decided to consider the updated ISOE survey of 2012, which reported several AV values from regulatory bodies in different countries. This is shown in Table2 13 column entitled AV value in $(2014‐USD)/mSv). In 2016, the United States Nuclear Regulatory Commission (NRC) drew up the “dollar per person‐rem conversion factor” for use in cost‐benefit analyses of radiation exposure. Its value was updated to $5.200 (2014‐USD) per person‐rem, ie, 520 $/man‐millisievert ($/man‐mSv), as reported in Table 2. In this calculation, 1 rem is equal to 10 mSv and 1$ is equal to 1 US dollar. 14 The advantage of this method is that it enables fast and easy cost‐utility analysis, since the cost reduction related to radiation saved is obtained by simply multiplying the ED reduction (ΔE, measured in [mSv]) by the AV value.
| (1) |
where AV values are expressed in [$/mSv] instead of [$/man‐mSv], as they are related to the exposure of a single patient.
TABLE 2.
AV values, expressed as $(2014‐USD)/mSv, in different countries, and corresponding Cost Reduction values, expressed in $(2014‐USD), Cost‐Effectiveness, expressed as Yes or No on adopting the AV method
| Country a | AV value in $(2014‐USD)/mSv | HB‐CA cost reduction $(2014‐USD) | HB‐CA cost‐effectiveness |
|---|---|---|---|
| Canada | 108 | 125 | No |
| Czech Republic (min value) | 28 | 33 | No |
| Czech Republic (max value) | 137 | 159 | No |
| Finland | 105 | 122 | No |
| Korea | 84 | 98 | No |
| Netherlands | 619 | 719 | No |
| Romania | 777 | 903 | No |
| Slovakia | 45 | 52 | No |
| Sweden (min value) | 76 | 88 | No |
| Sweden (max value) | 386 | 449 | No |
| Switzerland | 3384 | 3932 | Yes |
| United Kingdom (min value) | 17 | 20 | No |
| United Kingdom (max value) | 171 | 199 | No |
| United States | 210 | 244 | No |
| United States b | 520 | 604 | No |
ISOE European Technical Center (2012) Man‐Sievert Monetary Value Survey (2012 Update). ISOE Information Sheet No. 55, General Distribution November 2012.
Office of Nuclear Reactor Regulation (2016) Reassessment of NRC's Dollar Per Person‐Rem Conversion Factor Policy. Final Report. NUREG‐1530, Revision 1, Manuscript Completed: September 2016.
The Value of a Statistical Life (VSL) ‐based method aims to overcome some limitations of the AV‐based method. It is based on the concept of the willingness to pay for a specific level of risk reduction. The VSL does not represent the cost value of a person's life, but the amount that a community would be willing to pay to reduce the risk of one person's death. This risk assessment can be made by using the coefficients reported in the recent (2011) report of the United States Environmental Protection Agency (EPA) EPA 402‐R‐11‐001. 15 This document estimates cancer incidence risk and cancer mortality risk as a result of low doses of ionizing radiation in the US population.
The coefficient used to convert ED into the attributable lifetime risk of cancer mortality was estimated on the basis of the risk models described in EPA 402‐R‐11‐001. 15 The EPA’s cancer risk model was also adopted by the NRC in its dollar‐per‐person‐rem conversion factor reassessment. 16
The lifetime risk (LR) of cancer mortality is strongly related to the age and gender of the patients exposed. We therefore assumed that, for HB‐CA, LR had an average value of 2.44%/Sv in adult males and females aged 75 years.
The VSL estimates differ across countries and also among agencies within the same country. In 2011, the Organization for Economic Co‐operation and Development (OECD) published the VSL values. 16 In OECD countries, the recommended VSL range is $1.45‐4.35 million (2005‐USD), with a base value of $2.9 million (2005‐USD), whereas in EU‐27 countries, the recommendation is between $1.75‐5.25 million (2005‐USD), with a base value of $3.5 million (2005‐USD) (see Table 3, column entitled VSL values in millions $(2014‐USD)).
TABLE 3.
VSL values, expressed as millions $(2014‐USD), in different countries and United States Agencies, and corresponding Cost Reduction values, expressed in $(2014‐USD), Cost‐Effectiveness, expressed as Yes or No on adopting the VSL method
| OECD b | VSL values in millions $(2014‐USD) | HB‐CA cost reduction $(2014‐USD) | HB‐CA cost‐effectiveness |
|---|---|---|---|
| OECD countries | 3.5 | 99 | No |
| OECD EU‐27 | 4.2 | 119 | No |
| United States Agencies a | VSL values in millions $(2014‐USD) | HB‐CA cost reduction $(2014‐USD) | HB‐CA cost‐effectiveness |
|---|---|---|---|
| Environmental Protection Agency (EPA) | 8.7 | 247 | No |
| Department of Transportation (DOT) | 9.3 | 264 | No |
| Department of Homeland and Security (DHS) | 8.6 | 244 | No |
| Food and Drug Administration (FDA) | 8.6 | 244 | No |
| Occupational Safety and Health Administration (OSHA) | 9.0 | 255 | No |
| Office of Management and Budget (OMB) (min value) | 1.3 | 37 | No |
| Office of Management and Budget (OMB) (max value) | 13.2 | 374 | No |
Office of Nuclear Reactor Regulation (2016) Reassessment of NRC's Dollar Per Person‐Rem Conversion Factor Policy. Final Report. NUREG‐1530, Revision 1, Manuscript Completed: September 2016
OECD (2011), “Valuing Mortality Risk Reductions in Regulatory Analysis of Environmental, Health and Transport Policies: Policy Implications”, OECD, Paris, www.oecd.org/env/policies/vsl
Even in the same country, values differ; in the United States, for example, the Office of Management and Budget (OMB) concluded that the majority of VSL studies across regulatory agencies suggested a value ranging from $1 million to $10 million (2001‐USD) per statistical life in 2001, 17 updated to $1.2 million and $12.2 million (2010‐USD) in 2010. 18
The NRC staff estimates are presented in Table 3. 16
Hence, for a single procedure, and on adopting the VSL‐based method, the cost reduction can be estimated by means of Equation (1):
| (2) |
LARR is the Lifetime Attributable Risk Reduction, which is the product of the Lifetime Risk (LR) of cancer incidence related to X‐ray exposure and the ED Reduction (ΔE).
The extra cost of using an NMS during every HB‐CA procedure has been calculated as €2,500{$3,454 ($2014‐USD)} in our context.
3. RESULTS
3.1. Total population
Our study considered a total number of 124 pts (Groups I and II) affected by AF refractory to medical therapy who underwent HB‐CA procedures. The baseline characteristics of the two groups are summarized in Table 1. There were no significant differences between the two groups.
3.2. Fluoroscopy and procedure data
The use of an NMS resulted in reduced fluoroscopy time in Group II {median value 1.35 min} in comparison with Group I {median value 4.8 min (MW‐test, P < .05)}. Accordingly, total X‐ray exposure was higher in Group I (8.76 Gy*cm2) than in Group II (2.95 Gy*cm2) (MW‐test, P < .05) (Figure 1). The effective dose reduction (ΔE) was estimated to be 1.16 milli‐Sievert. The reduction in X‐ray exposure was obtained at the cost of prolonging the PT: median values of 40 min in Group I and 50 min in Group II (MW‐test, P < .05) (Figure 1).
FIGURE 1.
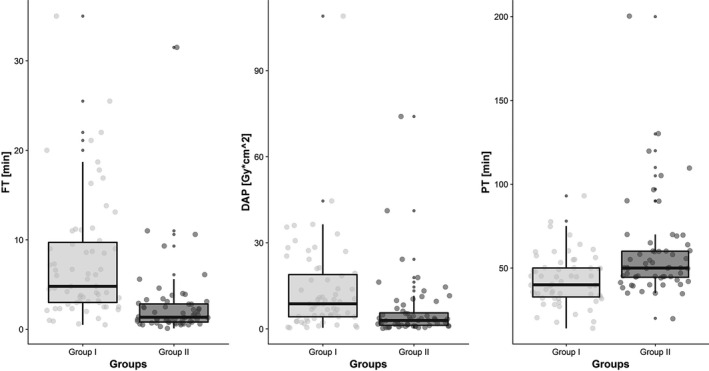
The Box and Whisker Plots show the trends in the median values of Fluoroscopy Time (FT), expressed in minutes [min], Dose Area Product (DAP), expressed in [Gy*cm2], and Procedure Time (PT), expressed in minutes [min]
No complications were reported in both groups. The HB‐CA was similarly effective in both groups, although pacemaker dependency was observed in fewer Group II patients (30 (48%) in Group I vs 19 (31%) in Group II, P = .061). In all patients, no regression of atrioventricular block was reported at 12‐month visit.
3.3. Economic results
The reduction in the detriment (cost reduction) is caused by the reduced radiation dose when an NMS is used during the HB‐CA procedure.
On applying the AV method, the cost‐effectiveness of HB‐CA procedures is strongly related to the AV values adopted in each country. Table 2 reports the countries considered in this study, their adopted AV values in $(2014‐USD as reference), HB‐CA cost‐reduction, and whether the use of an NMS is advantageous (Yes) or not (No).
In all the countries considered, with the exception of Switzerland, the dose reduction related to the use of NMSs during HB‐CA was not advantageous. The economic threshold reference for HB‐CA procedures in our EP Laboratory is $3,454.
For example, in the Netherlands, applying Equation (1) will result in:
| (3) |
On applying the VSL method, the cost‐effectiveness of the HB‐CA procedures is also strongly related to the VSL values adopted by each country or organization. Table 3 reports the countries and agencies considered in this study, their adopted VSL values in millions $(2014‐USD as reference), HB‐CA cost reduction, and whether the use of NMSs is advantageous (Yes) or not (No). The economic threshold adopted for HB‐CA procedures in our EP Laboratory is $3,454 (2014‐USD).
For example, with regard to the VLS proposed by the Food and Drug Administration (FDA), applying Equation (4) will result in:
| (4) |
4. DISCUSSION
Today, the use of NMSs during the catheter ablation of complex arrhythmias 19 , 20 is standard practice; moreover, their use in the ablation of simple arrhythmias in adults and children is increasingly frequent.
The significant reduction in fluoroscopy exposure was an unexpected effect of this use, and this advantage has been validated in several papers based on randomized 21 , 22 and nonrandomized studies in adults 23 , 24 and pediatric populations. 25 However, the effect of the regular use of an NMS during HB‐CA procedures has not been investigated in terms of efficacy, safety, and economic advantages.
In our previous paper, we analyzed these aspects in adults 8 , 9 and children 25 and our final conclusions were as follows: first, the use of NMS enables fluoroscopy exposure to be considerably reduced; second, the economic advantage depends on the specific situation of the EP Laboratory and is directly related to the amount of the effective dose reduction.
In the present study, we demonstrated that performing HB‐CA in patients with AF refractory to medical treatment with the aid of an NMS is safe, feasible, and effective in comparison with the use of fluoroscopy alone; moreover, it seems to be more precise in defining the target ablation area, with less frequent induction of pacemaker dependency.
To determine whether the systematic use of NMSs during HB‐CA procedures in our EP Laboratory was economically advantageous or not, we applied two cost‐benefit methods (AV and VLS). During the analysis, we encountered the same problem as in our previous studies: the two methods show a very large range of parameters; indeed, the values adopted differ not only from one country to another but also even among the various agencies within the same country. Given these limitations, the main conclusion of our study is that, in HB‐CA patients, the effective dose reduction obtained through the use of NMSs is very low and therefore not economically advantageous according to the majority of AV and VSL values. Moreover, owing to the short fluoroscopy time and the limited X‐ray exposure required to accomplish these simple procedures with the standard approach, a significant cost‐effectiveness was not achievable with NMSs at the current cost of NMS use in our Laboratory.
4.1. Study limitations
In our opinion, the limitations of this study can be summarized as follows:
The number of patients in the study was low.
The study was a retrospective analysis and not a prospective randomized study.
Adopting the EPA’s models for the quantification of cancer mortality risk, we did not consider the additional cost associated with nonfatal cancers. Thus, the monetized benefit is underestimated.
The costs of NMS use are not standardized among institutions; thus, the results may not be applicable to other centers.
The reduction in fluoroscopic time with NMSs might prolong the longevity of fluoroscopic machine and positively contribute to economic cost‐effectiveness. This aspect was not evaluated with the current model.
We did not take into account the positive effect of the X‐ray reduction on the health of EP Laboratory workers, which is no minor issue. 2 However, as we did not record worker doses, this analysis was not possible.
5. CONCLUSIONS
Our retrospective analysis compared the use of an NMS during HB‐CA with the traditional system, which uses fluoroscopy alone. We found that the use of an NMS during HB‐CA was safe and effective and reduced fluoroscopy time and total X‐ray exposure. However, in our practice, this reduction did not prove economically advantageous.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
DISCLOSURE
The present study was performed as part of the employment of the authors at their hospital institutions.
ACKNOWLEDGMENT
We would like to thank Mr B. Patrick for proofreading and correcting the English of the study.
Marini M, Ravanelli D, Martin M, et al. Is the systematic use of mapping systems during His Bundle catheter ablation cost‐effective? A single‐center experience. J Arrhythmia. 2020;36:720–726. 10.1002/joa3.12387
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author upon request.
REFERENCES
- 1. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962. [DOI] [PubMed] [Google Scholar]
- 2. Andreassi MG, Piccaluga E, Guagliumi G, Del Greco M, Gaita F, Picano E. Occupational health risks in cardiac catheterization laboratory workers. Circulat: Cardiovasc Intervent. 2016;9(4):e003273. [DOI] [PubMed] [Google Scholar]
- 3. Sporton SC, Earley MJ, Nathan AW, Schilling RJ. Electroanatomic versus fluoroscopic mapping for catheter ablation procedures: a prospective randomized study. J Cardiovasc Electrophysiol. 2004;15(3):310–5. [DOI] [PubMed] [Google Scholar]
- 4. Earley MJ, Showkathali R, Alzetani M, et al. Radiofrequency ablation of arrhythmias guided by non‐fluoroscopic catheter location: a prospective randomized trial. Eur Heart J. 2006;27:1223–9. [DOI] [PubMed] [Google Scholar]
- 5. Stabile G, Scaglione M, del Greco M, De Ponti R, Bongiorni MG, Zoppo F, et al. Reduced fluoroscopy exposure during ablation of atrial fibrillation using a novel electroanatomical navigation system: a multicentre experience. Europace. 2012;14(1):60–5. [DOI] [PubMed] [Google Scholar]
- 6. Casella M, Dello Russo A, Pelargonio G, Del Greco M, Zingarini G, Piacenti M, et al. Near‐zero fluoroscopic exPosure during catheter ablation of supRavenTricular arrhYthmias: the NO‐PARTY multicenter randomized trial. Europace. 2016;18(10):1565–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Giaccardi M, Del Rosso A, Guarnaccia V, Ballo P, Mascia G, Chiodi L, et al. Near‐zero x‐ray in arrhythmia ablation using a 3‐dimensional electroanatomic mapping system: a multicenter experience. Heart Rhythm. 2016;13(1):150–6. [DOI] [PubMed] [Google Scholar]
- 8. Marini M, Martin M, Ravanelli D, et al. Extensive use of 3D non‐fluoroscopic mapping system for reducing radiation exposure during catheter ablation procedures: an analysis of 10 years of activity. Biomed Res Int. 2019;10:4217076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marini M, Ravanelli D, Martin M, et al. An economic analysis of systematic use of mapping system during catheter ablation procedures: single‐center experience. Biomed Res Int. 2019;20:2427015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. R Core Team . R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. https://www.R‐project.org [Google Scholar]
- 11. Marini M, Ravanelli D, Guarracini F, et al. A cost‐effectiveness analysis of systematically using mapping systems during catheter ablation procedures in children and teenagers. Pediatr Cardiol. 2018;39:1581–9. [DOI] [PubMed] [Google Scholar]
- 12. ISOE European Technical Center . Survey on the values and uses of the monetary value of the man.sievert (in 2017). ISOE Information Sheet No. 61, General Distribution March 2018; 2018.
- 13. ISOE European Technical Center . Man‐Sievert Monetary Value Survey (2012 Update). ISOE Information Sheet No. 55, General Distribution November 2012; 2012.
- 14. Office of Nuclear Reactor Regulation . Reassessment of NRC's Dollar Per Person‐Rem Conversion Factor Policy. Final Report. NUREG‐1530, Revision 1, Manuscript Completed: September 2016; 2016.
- 15. Environmental Protection Agency . EPA radiogenic cancer risk models and projections for the US Population. EPA 402‐R‐11‐001. Washington, DC.
- 16. OECD . Valuing Mortality Risk Reductions in Regulatory Analysis of Environmental, Health and Transport Policies: Policy Implications. OECD, Paris. www.oecd.org/env/policies/vsl
- 17. Office of Management and Budget . Circular A‐4. September 17, 2003.
- 18. Office of Management and Budget, Office of Information and Regulatory Affairs . 2014 Draft Report to Congress on the Benefits and Costs of Federal Regulations and Unfunded Mandates on State, Local, and Tribal Entities; 2014.
- 19. Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14:e445–e494. [DOI] [PubMed] [Google Scholar]
- 20. Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Heart Rhythm. 2020;17:e2–e154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Scaglione M, Biasco L, Caponi D, Anselmino M, Negro A, Di Donna P, et al. Visualization of multiple catheters with electroanatomical mapping reduces X‐ray exposure during atrial fibrillation ablation. Europace. 2011;13(7):955–62. [DOI] [PubMed] [Google Scholar]
- 22. Hindricks G, Willems S, Kautzner J, De chillou C, Wiedemann M, Schepel S, et al. Effect of electroanatomically guided versus conventional catheter ablation of typical atrial flutter on the fluoroscopy time and resource use: a prospective randomized multicenter study. J Cardiovasc Electrophysiol. 2009;20(7):734–40. [DOI] [PubMed] [Google Scholar]
- 23. Fernández‐gómez JM, Moriña‐vázquez P, Morales EDR, Venegas‐gamero J, Barba‐pichardo R, Carranza MH, et al. Exclusion of fluoroscopy use in catheter ablation procedures: six years of experience at a single center. J Cardiovasc Electrophysiol. 2014;25:638–44. [DOI] [PubMed] [Google Scholar]
- 24. Casella M, Dello Russo A, Russo E, Catto V, Pizzamiglio F, Zucchett M, et al. X‐Ray exposure in cardiac electrophysiology: a retrospective analysis in 8150 patients over 7 years of activity in a modern, large‐volume laboratory. J Am Heart Assoc. 2018;22(7):e008233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marini M, Del Greco M, Ravanelli D, et al. The benefit of a general, systematic use of mapping system during electrophysiological procedures in children and teenagers: the experience of an adult EP laboratory. Pediatr Cardiol. 2016;37(4):802–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


