Abstract
Objectives:
The objectives of this study were to categorize newborns in Hamilton County, Ohio by late pregnancy fetal opioid exposure status and to assess their healthcare utilization in the first year of life.
Study design:
We used a population-based cohort of 41,136 live-births from 2014-2017, and analyzed healthcare encounters in the first year of life from electronic health records. We prospectively assessed for the presence of opioids in maternal urine collected at delivery and newborn neonatal abstinence syndrome (NAS) diagnosis. At birth, infants were classified as either unexposed to opioids, exposed to opioids and diagnosed with NAS, or subclinically exposed to opioids—exposure that did not result in NAS.
Results:
The total prevalence of newborn opioid exposure was 37 per 1,000. Lengths of hospital stay at birth were significantly longer for infants with subclinical exposure than unexposed infants (10% increase; 95% confidence interval (95%CI): 7-13%) but were shorter for infants with NAS. Neither subclinical exposure nor NAS was associated with total ED visits. Subclinical exposure was associated with increased odds of having at least one hospitalization in the first year of life. However, total length of stay at hospitalizations was 82% that of the unexposed group (95%CI: 75-89%). Infants with NAS had a total length of stay 213% that of the unexposed group (95% CI: 191-237%).
Conclusions:
Subclinical and overt opioid exposure among newborns was associated with increased first year healthcare utilization. From 2014-2017, this cost the Hamilton County healthcare system an estimated $1,109,452 for longer birth encounters alone.
Keywords: pregnancy, cohort, substance abuse
Introduction
Over the last decade, the United States’ opioid epidemic has become a public health crisis, but opioid use among pregnant women remains understudied for several reasons. Self-reported illicit drug use during pregnancy is notoriously unreliable (1), and most delivery hospitals in the US only perform drug testing upon suspicion of newborn exposure (i.e., risk-based screening), as opposed to implementing a universal testing protocol (2). Others have shown that Neonatal Abstinence Syndrome (NAS) (also known as Neonatal Opioid Withdrawal Syndrome or NOWS) resulting from in utero opioid exposure leading to withdrawal in the newborn, is on the rise in the United States; between 2000 and 2013, NAS increased from 1.2 to 6 per thousand live-born infants (3–5).
Although the long-term effects of prenatal opioid exposure are not well understood, there is evidence of adverse health consequences for these children. A recent meta-analysis described associations between in utero opioid exposure and adverse neurobehavioral and visual outcomes in children under three years of age but interpreted the results with caution due to inherent limitations and biases of the included studies (6). Another review article reported associations between maternal opioid use and congenital malformations and recommended that future studies include comparison groups of truly unexposed children to form valid conclusions (7). Previous work has been unable to accurately differentiate exposed and unexposed newborns from hospital records because infants with “subclinical” exposure, who do not experience severe withdrawal and do not receive a diagnosis of NAS, are not retrospectively identifiable. Thus, infants with subclinical exposure are misclassified as unexposed controls in other studies of opioid use during pregnancy, biasing any findings of those studies.
Therefore, we conducted a population-based cohort study of infants whose mothers are universally tested for opioids at birth, allowing us to differentiate infants with subclinical opioid exposure from truly unexposed infants. The objectives of this study are to calculate the prevalence of late pregnancy fetal opioid exposure and to determine how subclinical and overt (NAS) opioid exposure are associated with healthcare utilization in the first year of life including the length of initial birth encounter, number of emergency department (ED) visits, time to first ED visit, and total length of stay during hospitalizations in the first year of life. We hypothesize that infants exposed to opioids will have increased healthcare utilization compared to their unexposed peers.
Patients and Methods
Design, setting, and participants
We examined 41,136 live births from 2014-2017 in a population-based cohort of infants with a residential address at birth within Hamilton County, Ohio, where Cincinnati is located. Each infant received newborn services from a Cincinnati Children’s Hospital Medical Center (CCHMC) physician at one of 13 regional delivery hospitals representing 94.6% of the 43,467 county resident births during the period as reported by the Ohio Department of Health (8). CCHMC physician billing records generated during newborn encounters, as well as electronic health records collected during subsequent CCHMC hospital encounters, are integrated within the Maternal and Infant Data Hub, a regional population-based perinatal research repository (9).
Of the 0-14 year-olds who receive inpatient care in Hamilton County, 99% do so at CCHMC, and 81% of 0-14 year-olds who receive emergency care do so at CCHMC, ensuring nearly complete hospital utilization data for the cohort (10). We analyzed hospital encounters, including admissions and urgent care and emergency department visits in the first year of life for each child in the study. We only excluded infants if they died in the first year of life (n=183) or had unknown health insurance type (n=7, due to difficulty modeling this covariate when these patients were included), for a final sample size of 40,966.
Exposure, outcome, and covariates
Exposure to opioids was assessed for every newborn by maternal urine testing using immunoassay. Urine samples were collected immediately upon admission to labor and delivery to avoid the detection of medications administered during the labor process. If opioids were detected by immunoassay, confirmation was obtained with mass spectrometry.
All infants were assessed for NAS as part of the standard of care during their birth encounter, and NAS diagnoses were recorded using the International Classification of Diseases, Ninth or Tenth Revision (ICD-9/10) codes (ICD9: 779.5; ICD 10 P96.1). Further, the assignment of the NAS diagnosis was standardized within the region and only represents infants who receive pharmacologic treatment (including a stringent pharmacologic weaning protocol) for the management of severe opioid withdrawal symptoms (11). If maternal urine tested positive for opioids, infants were automatically held for 72-96 hours for observation. Infants managed exclusively with non-pharmacologic measures such as swaddling, skin-to-skin care, or breastfeeding were labeled sub-clinically exposed to opioids and were not diagnosed with NAS. We classified infants into three mutually-exclusive groups: unexposed infants, opioid exposed infants without NAS (subclinical exposure), and opioid exposed infants with NAS diagnosis (NAS).
Health care utilization outcomes were abstracted from hospital billing data. We assessed 1) length of the birth encounter (including any hospital transfers before homebound discharge), 2) total ED visits in the first year of life, 3) time to first ED visit in the first year of life, which began after discharge from the birth encounter, and 4) total inpatient length of stay in the first year of life, which did not include the birth encounter.
To address possible confounding pathways, we selected covariates a priori using a directed acyclic graph (DAG) based on the defined levels of opioid exposure and hospital utilization outcomes (Figure 1, online). DAGs are used to visually represent causal pathways between an exposure and outcome and aid in the selection of model covariates to prevent over- or under-adjustment and collider stratification bias (12). We adjusted statistical models for infant race, ethnicity, term status (full-term: ≥37 weeks, late pre-term: <37 weeks - ≥34 weeks, or pre-term: <34 weeks), insurance type, presence of a complex chronic condition, and presence of neonatal intensive care unit (NICU) admission during the initial birth encounter. Complex chronic condition was defined based on ICD-10 codes and the Pediatric Complex Chronic Condition Classification System Version 2 (13). For the total ED visits and time to first ED visit models, we created partially adjusted models that excluded demographic covariates (race, ethnicity, and insurance type) to assess for the effect of physiologic variables only. We created another DAG considering socioeconomic status (SES) factors as our exposure and determined that we could adjust for the same confounders in order to estimate the direct effect of these SES factors on ED utilization (Figure 2, online). The model for length of birth encounter additionally included the delivery route (vaginal vs. caesarian-section) as a covariate. The final variables included in models were obtained from the Cincinnati Maternal and Infant Data Hub.
Figure 1:
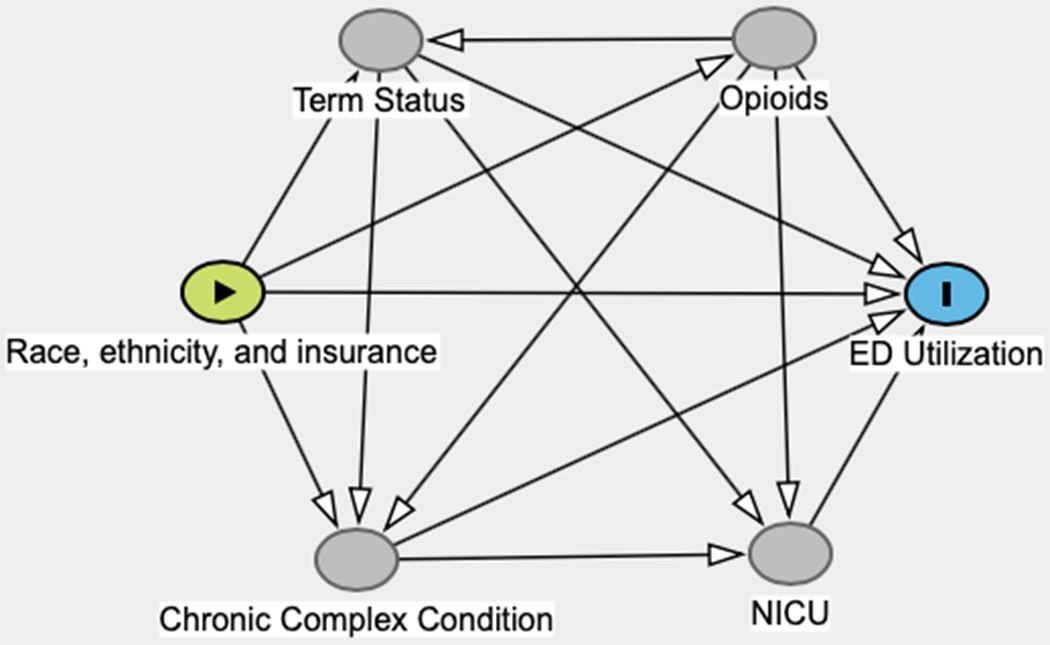
Directed acyclic graph for potential confounders in the relationship between opioid exposure and healthcare utilization
Figure 2:
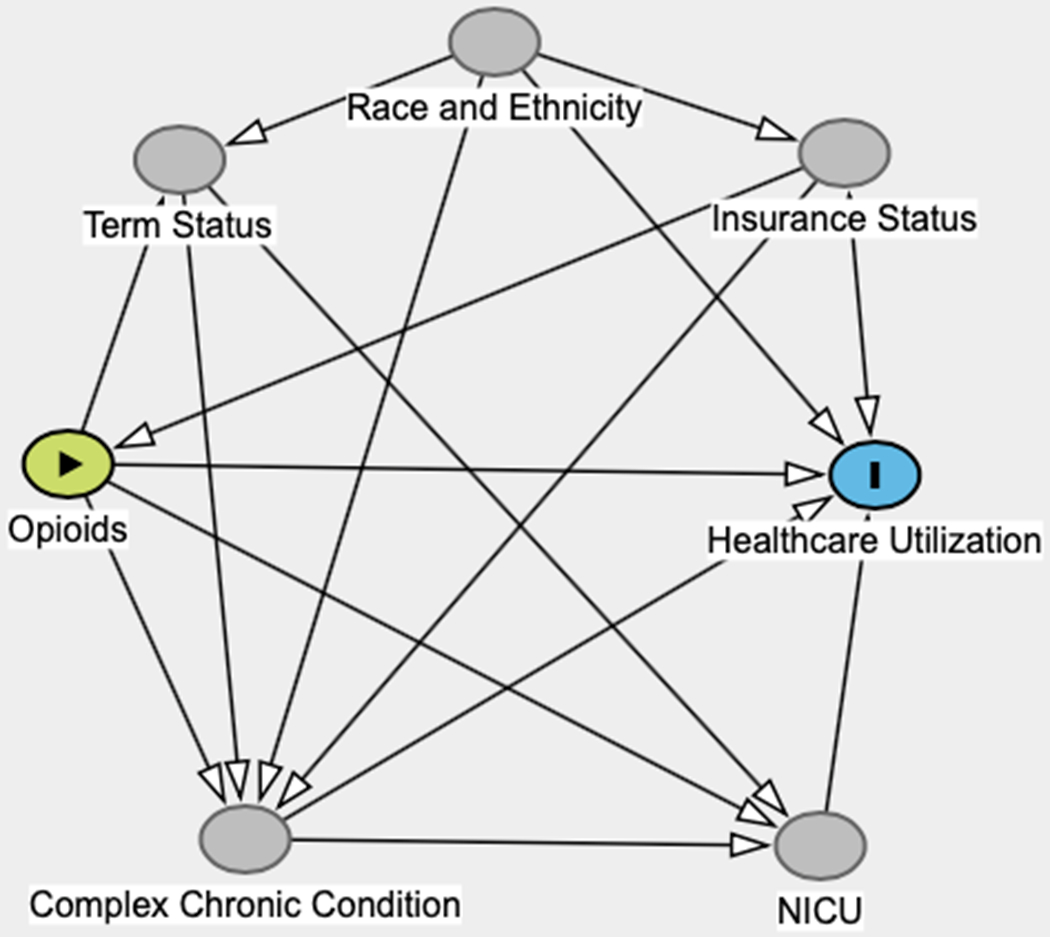
Directed acyclic graph for the relationship between socioeconomic factors and emergency department (ED) utilization with potential confounders.
Statistical Methods
Univariate differences between the three exposure groups were tested using the Kruskall-Wallis test. We used multivariable Poisson regression to model the length of the initial birth encounter, and multivariable Cox proportional hazards regression to model the time to the first ED visit. For total ED visits and total length of inpatient stay, we used multivariable zero-inflated Poisson (ZIP) regression models to account for the large number of infants with zero ED visits or inpatient stays. The zero-inflated assumption was verified using Vuong non-nested tests (14). ZIP models assume that the data is generated through two distinct distributions. The first is whether a count is zero or non-zero, and it is modeled using a logistic distribution. The second is the magnitude of all of the non-zero counts, modeled using a Poisson distribution. Thus, a ZIP model produces both an odds ratio for a zero count and a risk ratio for the multiplicative change in the non-zero count.
Since we considered opioid exposure as a non-ordered categorical variable with three levels (no exposure, subclinical exposure, NAS-level exposure), we were able to extract separate odds ratios for “subclinical exposure” and “NAS-level exposure,” both comparing to the baseline of “no exposure.” As polysubstance exposures and genetic factors are believed to play a crucial role in the presentation and severity of NAS, the type, extent, and duration of in-utero opioid exposure alone cannot fully predict infant withdrawal severity (15). Models were fitted using only non-missing covariate data, and a previous study of this cohort showed that race and ethnicity data were missing completely at random (16).
We used R version 3.6.1 for all data analysis (17), including packages pscl (18,19) for ZIP models, survival (20) for Cox proportional hazards models, and survminer (20) for the generation of survival curves.
Results
Cohort Information
Of the 40,966 infants born 2014-2017, 96.3% (n=39,469) were unexposed to opioids, 2.6% (n=1,066) had subclinical opioid exposure, and 1.1% (n=431) had NAS. Of the 183 excluded patients who died in the first year of life, 96.2% were unexposed (n=176), 3.3% had subclinical opioids exposure (n=6), and 0.5% were diagnosed with NAS (n=1). All 7 patients excluded due to unknown insurance type were unexposed.
Table 1 shows the hospital utilization outcomes and sociodemographic factors of the cohort by exposure status. There were statistically significant differences between exposure groups for all outcome variables and covariates except for infant sex. Infants with subclinical exposure and NAS were more likely to have public insurance, to be admitted to the NICU, and to have a complex chronic condition. Infants with subclinical exposure were more likely to be pre-term or late pre-term, and infants with NAS were much more likely to be late pre-term than either unexposed or subclinically exposed infants (both P < 0.001). Compared to national statistics, our population-based cohort had a higher proportion of black mothers, a lower proportion of Hispanic mothers, and mothers were more likely not to have health insurance.
Table 1:
Cohort outcomes and sociodemographic information by exposure group, 2014-2017.
| Unexposed % (n) | Subclinical % (n) | NAS % (n) | p-value | US Births in 2017§, % (n) | |
|---|---|---|---|---|---|
| Total infants | 96.3 (39,469) | 2.6 (1,066) | 1.1 (431) | (3,855,500) | |
| Percentage with total LOS >0† | 8.1 | 12.5 | 19.0 | <0.001 | |
| Length of birth encounter (days) | <0.001 | ||||
| 25th Percentile | (2) | (3) | (11) | ||
| Median | (2) | (4) | (15) | ||
| 75th Percentile | (3) | (5) | (21) | ||
| Percentage with total ED visits >0 | 40.1 | 48.5 | 46.9 | <0.001 | |
| Time to first ED visit* (days) | 0.024 | ||||
| 25th percentile | (44) | (38) | (48) | ||
| Median | (122) | (97) | (118) | ||
| 75th percentile | (227) | (212) | (220) | ||
| Female | 48.8 | 50.6 | 50.1 | 0.46 | 48.8 |
| Race | <0.001 | ||||
| White | 26.1 | 22.9 | 5.8 | 51.7 | |
| Black | 12.0 | 12.7 | 12.3 | 14.5 | |
| Other | 22.1 | 22.4 | 21.6 | 33.8 | |
| Unknown | 39.8 | 42.0 | 60.3 | -- | |
| Ethnicity | <0.001 | ||||
| Hispanic | 6.0 | 2.8 | 3.3 | 23.3 | |
| Non-Hispanic | 84.8 | 88.5 | 90.0 | 76.7 | |
| Unknown ethnicity | 9.2 | 8.7 | 6.7 | -- | |
| Term status | <0.001 | ||||
| Full-term | 86.4 | 79.8 | 74.7 | 90 | |
| Late pre-term | 7.5 | 12.3 | 19.3 | 7.2 | |
| Pre-term | 2.9 | 5.7 | 4.9 | 2.8 | |
| Unknown | 3.2 | 2.2 | 1.2 | -- | |
| Health insurance | <0.001 | ||||
| Public | 46.5 | 75.8 | 75.4 | 46.4 | |
| Private | 43.8 | 12.9 | 7.4 | 49.1 | |
| Self-pay | 9.7 | 11.4 | 17.2 | 4.1 | |
| Delivery method | 0.10 | ||||
| Vaginal | 68.5 | 65.7 | 74.5 | 68.2 | |
| Cesarean-Section | 31.5 | 34.3 | 25.5 | 31.8 | |
| NICU stay | <0.001 | ||||
| Yes | 8.0 | 20.3 | 67.5 | -- | |
| Unknown | 1.1 | 1.1 | 4.2 | -- | |
| Complex chronic condition | 18.6 | 24.1 | 26.5 | <0.001 | -- |
National Vital Statistics Reports, Vol. 67, No. 8, November 7, 2018
Total LOS does not include initial hospitalization at birth
Only patients with an ED visit in the first year of life are included in these calculations. NAS=neonatal abstinence syndrome; LOS=length of stay; ED=emergency department; NICU=neonatal intensive care unit
Length of Stay at Birth
Subclinical exposure to opioids was associated with a 10% longer stay after birth compared to infants without opioids exposure (95% CI: 7-13%, p<0.001). NAS was associated with a 94% longer stay (95% CI: 88-101%, p<0.001).
ED Utilization
To assess the association between prenatal opioid exposure and ED utilization, we created multivariable ZIP and Cox-proportional hazards models for total ED visits and time to first ED visit, respectively (Table 2). Neither the logistic nor the Poisson portions of the fully adjusted ZIP model showed significant associations between in utero opioid exposure and number of ED visits in the first year of life. In the fully adjusted time to first ED visit model, there was a significantly increased hazard for subclinical exposure (hazard ratio (HR): 1.11, 95% confidence interval (CI): 1.01-1.21, p=0.02).
Table 2:
Total ED visits in first year of life (zero-inflated Poisson model) results and time to first ED visit (Cox-proportional hazards model) results. Reference is unexposed infants. Fully adjusted model infant race, ethnicity, term status, insurance type, complex chronic condition, and NICU stay. Partially adjusted models include term status, complex chronic condition, and NICU stay, and do not include demographic covariates race, ethnicity, or insurance type.
| Total ED visits | Time to first ED visit | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Odds of having at least one ED visit | Number of non-zero ED visits | |||||||||
| Odds Ratio | 95% CI | P-value | Rate Ratio | 95% CI | P-value | Hazard Ratio | 95% CI | P-value | ||
| Fully adjusted | Subclinical | 1.18 | 0.98-1.48 | 0.09 | 0.99 | 0.92-1.06 | 0.66 | 1.11 | 1.01-1.21 | 0.02 |
| NAS | 1.00 | 0.73-1.38 | 0.997 | 1.04 | 0.91-1.18 | 0.57 | 0.99 | 0.83-1.17 | 0.90 | |
| Unadjusted | Subclinical | 1.43 | 1.23-1.64 | <0.001 | 1.05 | 0.98-1.12 | 0.17 | 1.31 | 1.21-1.44 | <0.001 |
| NAS | 0.95 | 0.73-1.25 | 0.70 | 0.97 | 0.85-1.10 | 0.58 | 0.95 | 0.80-1.11 | 0.50 | |
| Partially adjusted | Subclinical | 1.37 | 1.18-1.59 | <0.001 | 1.03 | 0.96-1.10 | 0.48 | 1.26 | 1.16-1.38 | <0.001 |
| NAS | 0.93 | 0.70-1.25 | 0.66 | 0.97 | 0.85-1.10 | 0.59 | 0.93 | 0.79-1.10 | 0.40 | |
Before adjusting for any covariates, subclinical exposure was associated with increased odds of having at least one ED visit in the first year of life compared to the unexposed group (odds ratio (OR): 1.43, 95% CI: 1.23-1.64, p<0.001), and increased hazard for time to first ED visit (HR: 1.31, 95% CI 1.21-1.44, p<0.001). NAS was not significantly associated with these outcomes. When the models were adjusted with a partial set of covariates (term status, complex chronic condition, and NICU stay), results were very similar to the unadjusted models, indicating that these variables do not account for the difference between the simple and fully adjusted models (Table 2). Figure 3 shows the unadjusted survival curves for time to first ED visit. In the unexposed group, 40.1% had an ED visit in the first year of life; in the subclinical exposure group, 48.5% had an ED visit in the first year of life; and in the NAS group, 46.9% had an ED visit in the first year of life.
Figure 3:
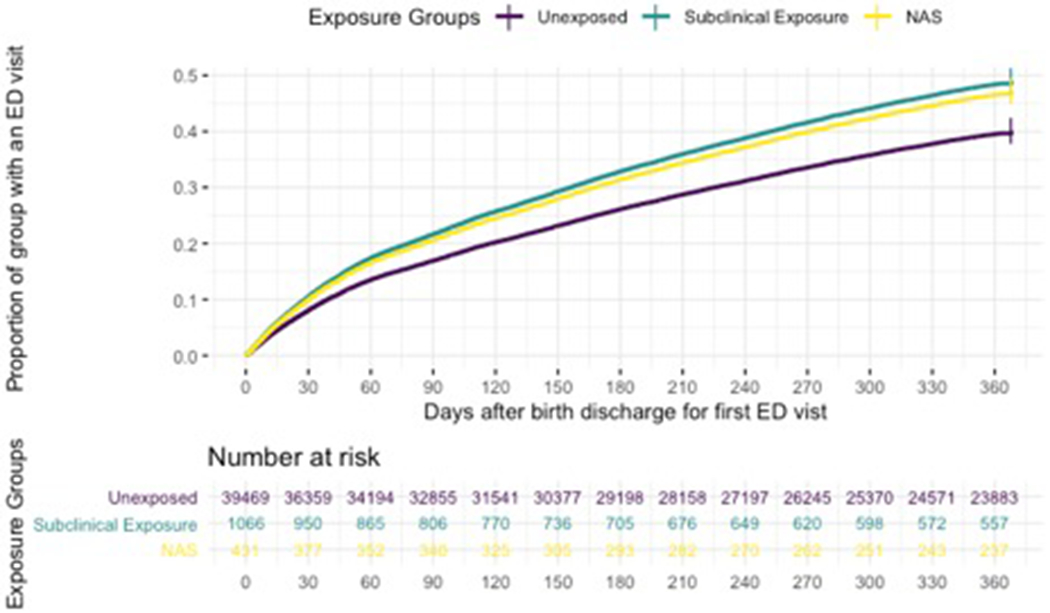
Unadjusted survival curves of time to first emergency department (ED) visit by exposure group. NAS: neonatal abstinence syndrome
Total Hospitalization Length of Stay
To assess associations between in utero opioid exposure and hospitalization in the first year of life, we used a ZIP model. In the logistic portion of the adjusted model, subclinical exposure was associated with 30% increased odds of having at least one hospital admission (95% CI: 6-59%, p=0.01) compared to unexposed infants, and NAS exposure was associated with 28% increased odds (p=0.13). From the Poisson portion of the adjusted model, we expect the total length of stay among the subclinical exposure group to be 82% of the unexposed group (95% CI: 75-89%, p<0.001) and the NAS group to be 213% of the unexposed group (95% CI: 191-237%, p<0.001).
Discussion
Key Results
In this population-based cohort of 40,966 infants born 2014-2017 in Hamilton County, Ohio, 37 per 1,000 were born exposed to opioids; this is roughly five times greater than a previous national estimate for 2014 based on ICD code diagnoses of 6.5-8 per 1,000 for NAS alone (3,4).
After adjustment for factors that covary with opioid exposure, subclinical opioid exposure among newborns was associated with a 10% increased length of stay during the birth encounter, and infants with overt signs of opioid withdrawal who were diagnosed with NAS had a 94% increased length of stay during the birth encounter. During the four-year study period, the increased length of birth encounters directly attributable to in utero opioid exposure translated to an additional 1,024 days of hospitalization across Hamilton County.
When maternal urine tested positive for opioids in our cohort, it triggered a 72-96 hour mandatory hospital observation period for the infant for observation of opioid withdrawal. The unadjusted median length of stay at the birth encounter for infants with subclinical exposure was four days (compared to two days for unexposed infants), so most of their observed additional stay was likely due to the mandatory observation. Infants with NAS had an unadjusted median length of stay of 15 days; additional medical needs complicated their birth encounters. The observed median length of stay for infants with NAS in our cohort is similar to those previously reported in the United States (21) and Canada (22).
Opioid exposure was not associated with differences in total ED encounters in fully adjusted models, but the subclinical exposure group had an 11% increased time to first ED encounter in the first year of life. We are unable to explain why subclinical exposure, but not NAS exposure, is associated with increased time to first ED encounter. However, we hope that future research on this understudied group of infants with subclinical opioid exposure will help elucidate our results.
In the unadjusted ZIP model, subclinical exposure was associated with a 43% increased odds of having at least one ED visit in the first year of life. To test the hypothesis that SES factors were driving the unadjusted ED utilization results, we created a partially adjusted ZIP model that did not include race, ethnicity, or insurance type and compared this partially adjusted model to the unadjusted model. As the estimates from the unadjusted and the partially adjusted models were very similar, we can conclude that SES variables were driving the association that we saw in the unadjusted ED utilization results. Others have also explored the relationship between ED utilization and SES. Schlinchting et al. explored trends in ED utilization rates and found that children with public insurance had 55% increased odds of visiting the ED compared to those with private insurance, and that non-Hispanic white children were less likely to visit the ED than children of other races/ethnicities (23).
Subclinical exposure at birth was associated with increased odds of hospitalization in the first year of life, but for the subgroup of infants that did experience hospitalization, there was a decreased total length of stay compared to unexposed infants with at least one hospital stay. A longer length of stay among unexposed infants may be due to a higher proportion of hospitalizations for low-acuity illness in the subclinical exposure group than the unexposed group. Since the subclinical exposure group is more likely to experience hospitalization, they may be experiencing different types of illnesses than their unexposed peers.
Patrick et al. followed infants born with NAS in New York and observed that infants with NAS were 149% more likely to be readmitted within 30 days of discharge than their uncomplicated full-term peers after adjusting for covariates (24). In contrast, we found that NAS was not associated with increased odds of hospitalization. However, we considered the entire first year of life. Additionally, we were able to study subclinical exposure, which was associated with increased odds of hospitalization, and we considered the total length of stay experienced by each exposure group in the first year of life.
Limitations
Although we are confident that we have correctly identified our exposed and unexposed groups due to the universal maternal testing in Hamilton County, these classifications do not represent the full gestational period. Our drug testing likely only captured a window of several days prior to delivery, so we cannot consider earlier exposure. However, we speculate that a positive test result at delivery is more likely to represent exposure during pregnancy than a negative test result, which could occur in mothers who used opioids earlier in pregnancy and stopped before delivery.
Another limitation of this study is that we are unable to differentiate between illicit and prescribed opioids (including medication-assisted treatment) exposure. We expect these mothers to have different healthcare utilization behaviors, and there may be residual confounding by type of opioid use (25). For example, in utero exposure to illicit opioids may have different physiological effects on the infants than prescribed opioids (26), but mothers with illicit use may also be less likely to seek prenatal care (27). Other drugs of abuse, when detected by our universal testing protocols, were not differentiated in billing records; this precluded analysis of these exposures as additional confounding factors.
While this study assumes that all children in the cohort remain in the study area for the first year of life, we were unable to verify that apparent non-utilization was not due to residential mobility out of Hamilton County. However, another study of Cincinnati children found that residential mobility was low, with only 6.5% moving in the first year of life, and that families tended to move only about two miles from their previous residence (28). While this study was only able to assess healthcare encounters in the first year of life that occurred at CCHMC, this represents 90% of all encounters in the county and 99% of hospitalizations.
Interpretation and generalizability
This study indicates that infants born exposed to opioids in Hamilton County, Ohio have an increased length of stay during the hospital birth encounter, increased odds of hospitalization, and an increased length of stay during hospitalizations in the first year of life. Opioid exposure was not associated with number of ED visits or time to first ED visit in the first year of life after adjusting for demographic confounders.
To estimate the opioid cost burden to the county health care system from the increased length of the birth encounter, we calculated the additional length of stay from adjusted risk estimates and assumed a $1,084 cost per day (21). During the four year study period, opioid exposure in newborns was associated with increased healthcare utilization in the first year of life, which cost the county healthcare system a total of $1,109,452.
The universal maternal drug testing program in Hamilton County allowed us to distinguish infants who were exposed to opioids but did not have clinically significant NAS, a group that has previously been difficult to identify and study. We showed that infants with subclinical exposure to opioids had increased healthcare utilization in the first year of life compared to unexposed infants, suggesting that this population may require closer observation either in the delivery hospital or through primary care. We are not aware of any other literature that has assessed healthcare utilization among this group. While our results may be generalizable to areas with similar population demographics and opioid use rates, it is difficult to fully consider differences in culture and healthcare access, as well as other unmeasured confounders that may exist between study areas. Therefore, our results should be interpreted with caution until they can be replicated in other locations. Further research is also needed to follow long-term health outcomes for infants with subclinical opioid exposure.
Acknowledgments
Funding: The patient cohort was obtained from the Cincinnati regional Maternal and Infant Data Hub supported by the National Center for Advancing Translational Sciences of the National Institutes of Health through the Center for Clinical and Translational Science and Training at the University of Cincinnati [5UL1TR001425-02]. This work was also supported by the University of Cincinnati Medical Scientist Training Program Grant supported by the National Institutes of Health 2T32GM063483-1.
Abbreviations:
- NAS
neonatal abstinence syndrome
- ED
emergency department
- CCHMC
Cincinnati Children’s Hospital Medical Center
- HER
electronic health record
- DAG
directed acyclic graph
- NICU
neonatal intensive care unit
- SES
socioeconomic status
- ZIP
zero-inflated Poisson
- HR
hazard ratio
- CI
confidence interval
- OR
odds ratio
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Chiandetti A, Hernandez G, Mercadal-Hally M, Alvarez A, Andreu-Fernandez V, Navarro-Tapia E, et al. Prevalence of prenatal exposure to substances of abuse: Questionnaire versus biomarkers. Reprod Health. 2017;14:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wexelblatt SL, Ward LP, Torok K, Tisdale E, Meinzen-Derr JK, Greenberg JM. Universal maternal drug testing in a high-prevalence region of prescription opiate abuse. J Pediatr [Internet]. 2015;166:582–6. Available from: 10.1016/j.jpeds.2014.10.004 [DOI] [PubMed] [Google Scholar]
- 3.Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid Use Disorder Documented at Delivery Hospitalization-United States, 1999-2014. Morb Mortal Wkly Rep [Internet]. 2018;67:845–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30091969%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC6089335%0Ahttps://www.cdc.gov/mmwr/cme/conted_info.html#weekly. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW. Incidence and Costs of Neonatal Abstinence Syndrome Among Infants With Medicaid: 2004 – 2014. Pediatrics. 2018;141:e20173520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patrick SW, Davis MM, Lehman CU, Cooper WO. Increasing Incidence and Geographic Distribution of Neonatal Abstinence Syndrome: United States 2009-2012. J Perinatol. 2015;35:650–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Monnelly VJ, Hamilton R, Chappell FM, Mactier H, Boardman JP. Childhood neurodevelopment after prescription of maintenance methadone for opioid dependency in pregnancy: a systematic review and meta-analysis. Dev Med Child Neurol. 2018;1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lind JN, Interrante JD, Ailes EC, Gilboa SM, Khan S, Frey MT, et al. Maternal Use of Opioids During Pregnancy and Congenital Malformations: A Systematic Review. Pediatrics. 2018;139:1–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohio Department of Health. Ohio Public Health Information Warehouse: Ohio Live Births. 2019. Available from: http://publicapps.odh.ohio.gov/EDW/DataBrowser/Browse/OhioLiveBirths
- 9.Hall ES, Greenberg JM, Muglia LJ, Divekar P, Zahner J, Gholap J, et al. Implementation of a Regional Perinatal Data Repository from Clinical and Billing Records. Matern Child Health J. 2018;22:485–93. Available from: 10.1007/s10995-017-2414-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beck AF, Riley CL, Taylor SC, Brokamp C, Kahn RS. Pervasive Income-Based Disparities In Inpatient Bed-Day Rates Across Conditions And Subspecialties. Health Aff. 2018;37:551–9. Available from: https://www.jstor.org/stable/1912557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hall ES, Wexelblatt SL, Crowley M, Grow JL, Jasin LR, Klebanoff MA, et al. A multicenter cohort study of treatments and hospital outcomes in neonatal abstinence syndrome. Pediatrics. 2014;134:527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: Updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vuong QH. Likelihood Ratio Tests for Model Selection and Non-Nested Hypotheses. Econometrica [Internet]. 1989;57:307–33. Available from: https://www.jstor.org/stable/1912557 [Google Scholar]
- 15.Logan BA, Brown MS, Hayes MJ. Neonatal abstinence syndrome: Treatment and pediatric outcomes. Clin Obstet Gynecol. 2013;56:186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brokamp C, Beck AF, Goyal NK, Ryan P, Greenberg JM, Hall ES. Material community deprivation and hospital utilization during the first year of life: an urban population–based cohort study. Ann Epidemiol. 2019;30:37–43. Available from: 10.1016/j.annepidem.2018.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.R Core Team. R: A language and environment for statistical computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2019. Available from: https://www.r-project.org/ [Google Scholar]
- 18.Zeileis A, Kleiber C, Jackman S. Regression Models for Count Data in R. J Stat Softw [Internet]. 2008;27 Available from: http://www.jstatsoft.org/v27/i08/. [Google Scholar]
- 19.Jackman S. pscl: Classes and Methods for R Developed in the Political Science Computational Laboratory [Internet]. Sydney, New South Wales, Australia: United States Studies Centre, University of Sydney; 2017. Available from: https://github.com/atahk/pscl/ [Google Scholar]
- 20.Therneau TM. A Package for Survival Analysis in S. 2015. Available from: https://cran.r-project.org/package=survival
- 21.Corr TE, Hollenbeak CS. The economic burden of neonatal abstinence syndrome in the United States. Addiction. 2017;112:1590–9. [DOI] [PubMed] [Google Scholar]
- 22.Filteau J, Coo H, Dow K. Trends in incidence of neonatal abstinence syndrome in Canada and associated healthcare resource utilization. Drug Alcohol Depend. 2018;185:313–21. Available from: 10.1016/j.drugalcdep.2017.12.019 [DOI] [PubMed] [Google Scholar]
- 23.Schlichting LE, Rogers ML, Gjelsvik A, Linakis JG, Vivier PM. Pediatric Emergency Department Utilization and Reliance by Insurance Coverage in the United States. Acad Emerg Med. 2017;24:1483–90. [DOI] [PubMed] [Google Scholar]
- 24.Patrick SW, Burke JF, Biel TJ, Auger KA, Goyal NK, Cooper WO. Risk of Hospital Readmission Among Infants With Neonatal Abstinence Syndrome. Hosp Pediatr. 2015;5:513–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jansson LM, Velez ML, McConnell K, Spencer N, Tuten M, Jones H, et al. Maternal buprenorphine treatment and infant outcome. Drug Alcohol Depend. 2017;180:56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hulse GK, Milne H, English DR, Holman CDJ. The relationship between maternal use of heroin and methadone and infant birth weight. Addiction. 1997;92:1571–9. [PubMed] [Google Scholar]
- 27.Chen CY, Wang IA, Fang SY, Huang N, Tsay JH, Chang SH. Inadequate prenatal care utilization among women with and without methadone-treated opioid use disorders in Taiwan. Int J Drug Policy [Internet]. 2019;67:1–8. Available from: 10.1016/j.drugpo.2019.01.024 [DOI] [PubMed] [Google Scholar]
- 28.Brokamp C, Lemasters GK, Ryan PH. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J Expo Sci Environ Epidemiol [Internet]. 2016;26:428–34. Available from: 10.1038/jes.2016.10 [DOI] [PMC free article] [PubMed] [Google Scholar]


