Abstract
Aims
Hypertensive disorders of pregnancy (HDP) predict future cardiovascular events. We aim to investigate relations between HDP history and subsequent hypertension (HTN), myocardial structure and function, and late gadolinium enhancement (LGE) scar.
Methods and results
We evaluated a prospective cohort of women with suspected ischaemia with no obstructive coronary artery disease (INOCA) who underwent stress/rest cardiac magnetic resonance imaging (cMRI) with LGE in the Women’s Ischemia Syndrome Evaluation-Coronary Vascular Dysfunction study. Self-reported history of pregnancy and HDP (gestational HTN, pre-eclampsia, toxaemia and eclampsia) were collected at enrollment. In our cohort of 346, 20% of women report a history of HDP. HDP history was associated with 3.2-fold increased odds of HTN. Women with a history of both HDP and HTN had higher cMRI measured left ventricular (LV) mass compared with women with HDP only (99.4±2.6 g vs 87.7±3.2 g, p=0.02). While we found a similar frequency of LGE scar, we observed a trend towards increased LGE scar size (5.1±3.4 g vs 8.0±3.4 g, p=0.09) among the women with HDP history compared to women without.
Conclusion
In a high-risk cohort of women with suspected INOCA, 20% had a history of HDP. Women with HDP history were more likely to develop HTN. Our study demonstrates higher LV mass in women with HDP and concomitant HTN. Although the presence of LGE scar was not different in women with and without HDP history, we observed a trend towards larger scar size in women with HDP. Future studies are needed to better assess the relationship of HDP and cardiac morphology and LGE scarring in a larger cohort of women.
Keywords: risk factors, coronary artery disease, hypertension, MRI
Key questions.
What is already known about this subject?
Hypertensive disorders of pregnancy (HDP) are associated with increased risk of cardiovascular disease and mortality.
What does this study add?
Our study demonstrates higher left ventricular mass in women with HDP and concomitant hypertension (HTN) history and a trend towards larger LGE myocardial scar size in women with HDP. Future studies are needed to better assess the relationship of HDP and left ventricular morphology and myocardial scarring in a larger cohort of women.
How might this impact on clinical practice?
Our findings support HTN surveillance in women with HDP who may be at higher risk for abnormalities in cardiac morphology.
Introduction
Increasing evidence has led to a wider recognition of women-specific risk factors for cardiovascular disease (CVD). These include hypertensive disorders of pregnancy (HDP), such as gestational hypertension (HTN) and pre-eclampsia, which combined complicate up to 10% of pregnancies and are characterised by de novo HTN after 20 weeks gestation.1–3 Although the pathophysiology is poorly understood, large cohort studies have found that pre-eclampsia is associated with up to an eightfold higher risk of CVD and mortality compared with women with healthy normotensive pregnancies.4–8 These findings emphasise the importance of understanding women-specific risk factors for CVD.
Cardiac magnetic resonance imaging (cMRI) with late gadolinium enhancement (LGE) can be used to evaluate ventricular morphology and function, detect myocardial scar and quantify scar size with high accuracy.9 10 cMRI measures, particularly increased left ventricular (LV) mass, presence of ischaemic and non-ischaemic scar as determined by LGE imaging are independent risk factors for major adverse cardiovascular events.11–16
Research on the associations between HDP and CVD is limited. Therefore, we investigated the risk of developing HTN decades after the index pregnancy complicated by HDP and relationship of history of HDP and HTN with cMRI measured LV morphology and function, and presence and size of LGE myocardial scar in women with ischaemia with no obstructive coronary artery disease (INOCA) in the Women’s Ischemia Syndrome Evaluation-Coronary Vascular Dysfunction (WISE-CVD) cohort.17 We hypothesise that women with HDP history will have abnormalities in LV morphology and function and more likely to have LGE myocardial scar.
Methods
Study population
This investigation was part of the National Heart, Lung, and Blood Institute-sponsored prospective multicentre WISE-CVD study (URL: http://www.clinicaltrials.gov, unique identifier: NCT00832702). WISE-CVD was a prospective study of women with suspected sign and symptoms of INOCA (defined as <50% luminal diameter in any major coronary artery) on invasive angiography.18 Subjects were recruited from January 2009 to August 2015 at Cedars-Sinai Medical Center, Los Angeles, California or University of Florida, Gainesville, Florida. The protocol was approved by the Institutional Review Board at each site and all participants provided written informed consent.
As previously described women with signs and symptoms of ischaemia undergoing clinically indicated coronary angiography, age ≥21 years and competent to give informed consent were included. Exclusion criteria included acute coronary syndrome (defined by the American College of Cardiology/American Heart Associationcriteria),19 acute myocardial infarction; concurrent cardiogenic shock or inotropic or intra-aortic balloon support; prior or planned percutaneous coronary intervention or coronary artery bypass graft (CABG); primary valvular heart disease clearly indicating need for valve repair or replacement; chest pain with a non-ischaemic aetiology (eg, pericarditis, pneumonia, oesophageal spasm); conditions that preclude accurate or safe testing, or prognostic follow-up, specifically contraindications to cMRI (eg, implantable cardioverter defibrillator, pacemaker, untreatable claustrophobia or known angio-oedema, severe renal impairment (estimated glomerular filtration rate (eGFR) <45 mL/min); prior non-cardiac illness with an estimated life expectancy <4 years; and obstructive coronary artery disease defined as ≥50% luminal diameter stenosis in ≥1 epicardial coronary artery, assessed visually at the time of angiography.18
Self-reported history of pregnancy, HDP and HTN were collected at time of enrollment. Questionnaires specifically collected data on history of gestational HTN, pre-eclampsia, toxaemia and eclampsia. HTN was collected based on patient-reported medical history of HTN. Among the 374 women who completed cMRI in the WISE-CVD study, we included 346 women who reported history of at least one pregnancy and completed questions on history of HDP in our analysis.
Patient and public involvement
It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting or dissemination plans of our research.
cMRI protocol and analyses
Stress and rest cMRI were performed at time of enrollment on a 1.5-Tesla MR scanner (Magnetom Avanto, Siemens Healthcare Erlangen, Germany) in the supine position with ECG gating. All subjects were asked to hold all their cardiac medications 24–48 hours prior to cMRI. A highly standardised protocol was used and included assessment of ventricular function and morphology and LGE imaging.18 In brief, LGE images were acquired in 10–12 short axis slices, one horizontal long axis slice and one vertical long axis slice in the same positions as the LV function cine images. A single shot trufi-based sequence was used with heart rate-based temporal resolution and echo time minimised at 0.98 ms. A ‘TI scout’ image was obtained followed by single shot inversion recovery TrueFISP images 10 min after last gadolinium injection.
The WISE-cMRI core lab analysed LV function and morphology using commercially available software (CAAS MRV V.3.4, PIE Medical Imaging) as previously described.20–22 Epicardial and endocardial borders of short-axis cine images were manually traced and postprocessing software was used to generate volume–time curves used for LV volumes and LV mass. Stroke volume was calculated as end-diastolic volume minus end-systolic, and ejection fraction as stroke volume divided by end-diastolic volume. LGE quantification was performed by a single experienced operator using associated postprocessing software (QMass, Medis) by defining endocardial and epicardial borders using the short-axis images and the full width at half-maximum method. LGE myocardial scar pattern was evaluated visually and defined as atypical scar pattern when mid-myocardial or epicardial scar pattern was present; and typical scar pattern when scar pattern was subendocardial or transmural and localised to a coronary artery distribution as previously described.23
Statistical analyses
The 346 women with a pregnancy history were divided into two groups: those with HDP and those without. Variables were summarised using mean and SD, or frequency and per cent if categorical, median and IQR was used to report LGE myocardial scar size. Baseline clinical and demographic variables were tested between these two groups using Pearson χ2 tests, or Fisher’s exact test for categorical variables that had low expected cell counts, or t-tests for continuous variables, unless non-normal distributions were present where a Wilcoxon rank-sum test was used.
The primary outcome assessed was HTN and secondary outcome was LV mass. A logistic regression model was used with history of HTN as the outcome, and groups with and without history of HDP as the explanatory factors, adjusting for age, body mass index (BMI), income category, diabetes and number of pregnancies. Additionally, linear regression models were used to examine the association of history of HDP and HTN with LV mass adjusting for history of HDP, history of HTN and interaction between the two. Additionally, adjusted multiple linear regression models accounting for age, BMI and systolic blood pressure (SBP) were performed. Tukey post hoc adjustment was used for pair-wise comparisons. All hypothesis tests used a significance level of 0.05. All analyses were done in SAS V.9.4 (SAS Institute, Cary, North Carolina, USA).
Results
Overall, 20% (68/346) of the women included in this analysis report history of at least one HDP. Pertinent demographics and clinical characteristics are summarised in table 1. Women with HDP history were younger (p=0.05) and had a higher mean BMI (p<0.001) compared with those without. There were no differences in coronary severity score and per cent of coronary artery stenosis on invasive coronary angiography between the group with and without HDP history. History of HDP was associated with 3.2-fold increased odds of HTN compared with women without HDP after adjusting for age, BMI, history of diabetes, number of pregnancies and income level (95% CI 1.4 to 7.3, adjusted p=0.005). cMRI LV structure and function parameters were similar between both groups (table 2).
Table 1.
Demographics and clinical characteristics of women with INOCA with and without history of HDP
| Characteristics | History of a HDP | P value | |
| No (n=278) | Yes (n=68) | ||
| Demographics | |||
| Age, years | 55.6±10.6 | 53.1±9.6 | 0.05 |
| BMI, kg/m2 | 27.4±6.6 | 31.7±7.5 | <0.001 |
| Race/ethnicity | 0.7 | ||
| White/Non-Hispanic | 207 (74.5%) | 52 (76.5%) | |
| Black/African–American | 20 (7.2%) | 7 (10.3%) | |
| Hispanic/Latin | 24 (8.6%) | 4 (5.9%) | |
| Annual income | 0.04 | ||
| US$0–US$49 000 | 84 (31.2%) | 32 (48.5%) | |
| US$50 000–US$99 000 | 71 (26.4%) | 12 (18.2%) | |
| US$100 000+ | 114 (42.4%) | 22 (33.3%) | |
| Clinical characteristics | |||
| HTN | 92 (35.3%) | 41 (65.1%) | 0.002* |
| Dyslipidaemia | 42 (18.9%) | 11 (22%) | 0.7 |
| Diabetes mellitus | 30 (11%) | 12 (18.2%) | 0.1 |
| Ever smoker | 115 (41.4%) | 25 (37.3%) | 0.6 |
| Cardiovascular medications | |||
| ACE-I or ARB | 65 (24.6%) | 22 (32.8%) | 0.2 |
| Beta blocker | 83 (31.1%) | 27 (40.3%) | 0.2 |
| Calcium channel blocker | 58 (21.9%) | 19 (28.8%) | 0.3 |
| Diuretic | 34 (12.7%) | 14 (20.9%) | 0.1 |
| Postmenopausal | 202 (72.7%) | 52 (76.5%) | 0.6 |
| Number of pregnancies | 3±2, 3 | 4±1, 4 | 0.01 |
| Coronary severity score | 9.2±4.2, 8.5 | 10.3±4.5, 9.6 | 0.1 |
| Angiographic findings | 0.8 | ||
| No CAD | 12 (6.4%) | 4 (8.3%) | |
| No obstructive CAD | 164 (87.2%) | 40 (83.3%) | |
Values are N (%), mean±SD, median (range).
No CAD defined as <20% coronary artery stenosis, no obstructive CAD defined as 20%–50% coronary artery stenosis.
Bold indicates significant p value </= 0.05
*Adjusted for age, BMI, diabetes, annual income, number of pregnancies.
ACE-I, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; BMI, body mass index; CAD, coronary artery disease; HDP, hypertensive disorders of pregnancy; HTN, hypertension; INOCA, ischaemia with no obstructive coronary artery disease.
Table 2.
cMRI haemodynamics, LV morphology and function in women with INOCA with and without history of HDP
| cMRI variables | History of a HDP | P value | |
| No (n=278) | Yes (n=68) | ||
| Heart rate (bpm) | 68.7±10.6 | 68.5±12.4 | 0.9 |
| SBP (mm Hg) | 129.7±20.8 | 134.4±18.7 | 0.1 |
| DBP (mm Hg) | 62.7±13.4 | 65.7±12.3 | 0.1 |
| Ejection fraction (%) | 68.2±6.8 | 68.3±7.6 | 0.6* |
| End-diastolic volume (mL) | 121.1±23.8 | 128.7±24.1 | 0.5* |
| End-systolic volume (mL) | 38.9±13.23 | 41.3±13.3 | 0.1 |
| Stroke volume (mL) | 82.0±16.5 | 86.3±17.6 | 0.7* |
| Mass to volume ratio | 0.8±0.1 | 0.8±0.2 | 0.6 |
| LGE % | 20 (7.2%) | 3 (4.4%) | 0.6 |
Values are mean±SD, or median (range).
*Adjusted for age, BMI.
BMI, body mass index; cMRI, cardiac MRI; DBP, diastolic blood pressure; HDP, hypertensive disorders of pregnancy; INOCA, ischaemia with no obstructive coronary artery disease; LGE, late gadolinium enhancement; LV, left ventricular; SBP, systolic blood pressure.
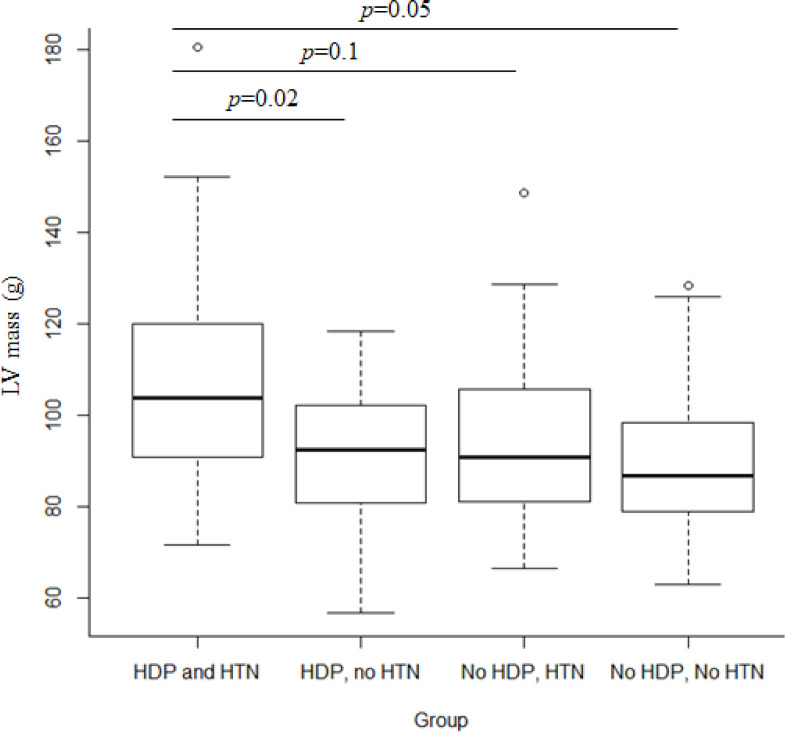
In unadjusted and adjusted models, we found an interaction between history of HDP and HTN in relation to cMRI-measured LV mass (interaction adjusted p=0.01). Women with a history of both HDP and HTN had the highest average LV mass compared with women with HDP only (HDP, no HTN), HTN only (no HDP, HTN) or neither (no HDP, no HTN, figure 1). The adjusted model showed that LV mass increased as BMI increased (by 1.3 per unit BMI, p<0.001). Women with a history of both HDP and HTN had a significantly higher LV mass compared with women with HDP only (99.4±2.6 g vs 87.7±3.2 g, p=0.02) and women with neither (99.4±2.6 g vs 91.9±1.2 g, p=0.05) after adjusting for age, BMI and SBP.
Figure 1.
Box plot of LV mass in women with history of HDP and HTN box plot showing that women with a history of both HDP and HTN have the highest average LV mass to women with HDP only (HDP, no HTN), HTN only (no HDP, HTN) or neither (no HDP, no HTN). HDP, hypertensive disorders of pregnancy; HTN, hypertension; LV, left ventricular.
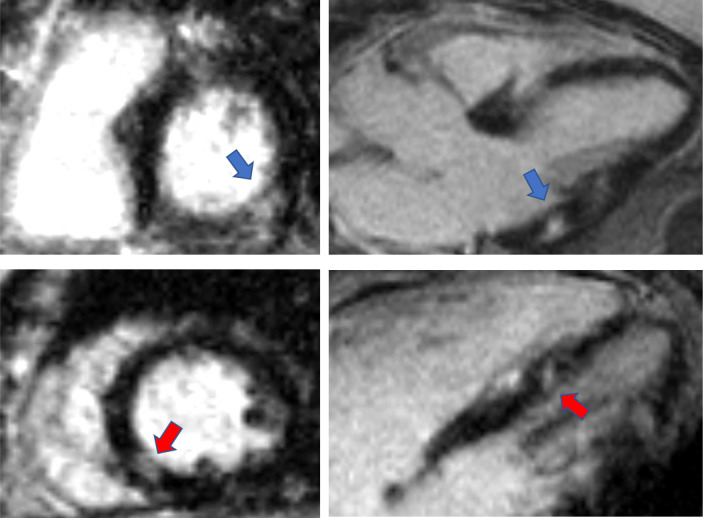
While there was a relatively similar frequency of cMRI LGE myocardial scar, we observed a trend towards increased LGE myocardial scar size (5.1±3.4 g, 4.0 (1.9, 18.0) vs 8.0±3.4 g, 8.3 (4.5, 11.2), p=0.09) in women with history of HDP compared with women withouttable 2. Among the women with history of HDP with LGE myocardial scar, 67% had typical scar pattern (vascular pattern consistent with coronary distribution) and 33% had atypical scar pattern (non-vascular pattern). Among women without history of HDP, 78% had typical pattern and 22% had atypical pattern. Sample case of a participant with INOCA and history of HDP showed inferolateral transmural LGE myocardial scar and inferoseptal subendocardial LGE myocardial scar (figure 2).
Figure 2.
Myocardial scar in woman with ischaemia with no obstructive CAD and HDP sample case of a participant with INOCA and history of HDP disorder of pregnancy showing inferolateral subepicardial LGE myocardial scar (blue arrow) and inferoseptal subendocardial LGE myocardial scar (red arrow). CAD, coronary artery disease; HDP, hypertensive disorders of pregnancy; INOCA, ischaemia with no obstructive coronary artery disease; LGE, late gadolinium enhancement.
Discussion
Studies assessing cardiac structure and function in women with history of HDP are limited, to our knowledge our study is the first to use advanced imaging with LGE to evaluate myocardial scar in a high-risk group of women with history of HDP. In our cohort of women with signs and symptoms of INOCA, 20% had a history of HDP. Our study confirms that women with HDP are more likely to go on to develop HTN. We also found that HDP history is related to cMRI-determined higher LV mass in women with concomitant HTN. Although LGE myocardial scar was not different in women with and without HDP history, we observed a a trend towards larger scar size in women with HDP.
In accordance with prior studies, we find that women with HDP history have 3.2-fold increase risk of developing HTN later in life.24 During pregnancies complicated by HDP there is a pronounced increase in LV mass in response to the increased LV workload from the sudden development of HTN that leads to abnormal cardiac remodelling.25 26 Unlike healthy pregnancies, in which the physiologic increase in LV mass and dimensions reverses a few weeks post partum, studies have shown that in HDP abnormal cardiac remodelling can persist up to 2 years post partum.26–28 However, the extent to which these abnormalities in cardiac remodelling persist decades later remains unclear. We found that the combination of HDP and HTN was associated with higher LV mass similar to Scantlebury et al who found that history of HDP was a risk factor for LV hypertrophy mediated by HTN using echocardiography.28 Further, Ghossein-Doha et al showed that increased LV mass at 10 months post partum was a predictor for the development of HTN in women whose blood pressure had normalised after a pregnancy complicated by HDP.25 Our study supports this inter-relationship between HDP, adverse cardiac remodelling and HTN and suggests that both HDP and HTN may lead to adverse cardiac remodelling decades later.
The Danish cohort is the only other cohort that has used cMRI with gadolinium to evaluate for myocardial scar with LGE in otherwise healthy women with history of HDP; however, they did not find evidence of myocardial scar in the 28 women with history of HDP.29 In our cohort, 23 had LGE with similar frequency in those with and without history of HDP, this difference is likely due to the fact that our cohort is composed of high-risk women with suspected INOCA. Our trend towards larger LGE myocardial scar in women with history of HDP leads us to hypothesise that HDP history may contribute to irreversible myocardial injury that needs further evaluating in future larger studies. The mechanisms are unknown, and could be via HTN, abnormal cardiac remodelling, myocardial infarction or other comorbidities.
Our study has limitations. Our findings are limited to a high-risk cohort of women with suspected INOCA that is not representative of the general population. History of HDP and HTN were collected through self-report, which is subject to recall bias.30–33Although maternal recall of HDP has a high specificity, its modest predictive value is a limitation of our study as it is for most studies on HDP conducted decades after pregnancy period.30 33 We were unable to account for presence of HTN prior to pregnancy or duration of HTN postpregnancy as this data were not collected. Additionally, we were underpower to assess the relationship between HDP and cardiovascular outcomes.
Conclusions
In summary, in our cohort of women with signs and symptoms of INOCA, 20% had a history of HDP. Our study is consistent with prior work and confirms that women with HDP are more likely to go on to develop HTN. We also found higher LV mass in women with concomitant history of HDP and HTN, supporting the current guidelines on increased HTN surveillance in women with history of HDP. Although the presence of LGE myocardial scar was not different in women with and without HDP history, we observed a trend towards larger LGE myocardial scar size in women with HDP. Future studies are needed to better assess the relationship of HDP and LV morphology and function and LGE myocardial scarring in a larger cohort of women.
Footnotes
OQ and KP contributed equally.
Contributors: NBM and OQ are responsible for the overall content of this article including the planning, conduct and reporting of the work described.
Funding: This work was supported by contracts from the National Heart, Lung and Blood Institutes (grant numbers N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, U0164829, U01 HL649141, U01 HL649241, K23HL105787, K23HL125941, T32HL69751, R01 HL090957); the National Institute on Aging (grant number 1R03AG032631); National Center for Research Resources General Clinical Research Center (GCRC, grant number MO1-RR00425); the National Center for Advancing Translational Sciences (grant number UL1TR000124 and UL1TR000064); grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, and QMED, Inc, Laurence Harbor, NJ, the Edythe L. Broad and the Constance Austin Women’s Heart Research Fellowships, Cedars-Sinai Medical Center, Los Angeles, California, the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles, The Society for Women’s Health Research (SWHR), Washington, DC, The Linda Joy Pollin Women’s Heart Health Program, the Erika J. Glazer Women’s Heart Research Initiative, and the Adelson Family Foundation, Cedars-Sinai Medical Center, Los Angeles, California. Dr Pepine was also supported by National Institute of Health (grant numbers HL33610, HL56921, UM1 HL087366); the Gatorade Trust through funds distributed by the University of Florida, Department of Medicine; NIH NCATS—University of Florida Clinical and Translational Science (grant number UL1TR001427); and PCORnet-OneFlorida Clinical Research Consortium (grant number CDRN-1501-26692). This work is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or National Institutes of Health.
Competing interests: Dr Bairey Merz reports personal fees from iRhythm, other from Sanofi, other from Abbott Diagnostics, during the conduct of the study. Dr Handberg reports grants from NIH/NHLBI, during the conduct of the study; grants from Aastom Biosciences, Amgen, Amorcyte, AstraZeneca, Biocardia, Boehringer Ingelheim, Brigham and Women’s Hospital, Capricor, Cytori Therapeutics, Department of Defense, Direct Flow Medical, Duke Clinical Research Institute, East Carolina University, Everyfit Inc, Gilead, Ionis, Medtronic, Merck grants from NIH/NCATS, grants from BioCardia BC-14-001-02; Mesoblast, Inc MSB-MPC-CHF001; Ventrix, Inc; Athersys Inc. AMI MultiStem; Verily Life Sciences LLC-Project Baseline OSMB; Ironwood MSB-MPC-CHF00-DMC, Imbria Pharmaceuticals Inc; Milestone Pharmaceuticals Inc; Caladrius Biosciences, Inc; Gatorade Trust; and McJunkin Family Foundation, outside the submitted work. Dr Minissian reports consulting with Amgen, Medical Advisory Board; honorarium NACCME, LLC Co-Chair for CME; Vox Media; Medtelligence; Minneapolis Heart Institute; Primed; Good Samaritan Hospital, Los Angeles, California; Cardiometabolic Health Congress; American Heart Association; National Lipid Association; Preventive Cardiovascular Nurses Association; American College of Cardiology. All other authors have no disclosures to report.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author, NBM, upon reasonable request.
References
- 1.Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol 2009;33:130–7. 10.1053/j.semperi.2009.02.010 [DOI] [PubMed] [Google Scholar]
- 2.Brown HL, Warner JJ, Gianos E, et al. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and Gynecologists: a presidential Advisory from the American heart association and the American College of obstetricians and Gynecologists. Circulation 2018;137:e843–52. 10.1161/CIR.0000000000000582 [DOI] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy . Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol 2013;122:1122–31. 10.1097/01.AOG.0000437382.03963.88 [DOI] [PubMed] [Google Scholar]
- 4.Cirillo PM, Cohn BA. Pregnancy complications and cardiovascular disease death: 50-year follow-up of the child health and development studies pregnancy cohort. Circulation 2015;132:1234–42. 10.1161/CIRCULATIONAHA.113.003901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Männistö T, Mendola P, Vääräsmäki M, et al. Elevated blood pressure in pregnancy and subsequent chronic disease risk. Circulation 2013;127:681–90. 10.1161/CIRCULATIONAHA.112.128751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu P, Haththotuwa R, Kwok CS, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2017;10:1–3. 10.1161/CIRCOUTCOMES.116.003497 [DOI] [PubMed] [Google Scholar]
- 7.Bellamy L, Casas J-P, Hingorani AD, et al. Pre-Eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 2007;335:974. 10.1136/bmj.39335.385301.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown MC, Best KE, Pearce MS, et al. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol 2013;28:1–19. 10.1007/s10654-013-9762-6 [DOI] [PubMed] [Google Scholar]
- 9.Kim RJ, Fieno DS, Parrish TB, et al. Relationship of MRI delayed contrast enhancement to irreversible injury, infarct age, and contractile function. Circulation 1999;100:1992–2002. 10.1161/01.CIR.100.19.1992 [DOI] [PubMed] [Google Scholar]
- 10.Ricciardi MJ, Wu E, Davidson CJ, et al. Visualization of discrete microinfarction after percutaneous coronary intervention associated with mild creatine kinase-MB elevation. Circulation 2001;103:2780–3. 10.1161/hc2301.092121 [DOI] [PubMed] [Google Scholar]
- 11.Bluemke DA, Kronmal RA, Lima JAC, et al. The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (multi-ethnic study of atherosclerosis) study. J Am Coll Cardiol 2008;52:2148–55. 10.1016/j.jacc.2008.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haider AW, Larson MG, Benjamin EJ, et al. Increased left ventricular mass and hypertrophy are associated with increased risk for sudden death. J Am Coll Cardiol 1998;32:1454–9. 10.1016/S0735-1097(98)00407-0 [DOI] [PubMed] [Google Scholar]
- 13.Jain A, McClelland RL, Polak JF, et al. Cardiovascular imaging for assessing cardiovascular risk in asymptomatic men versus women: the multi-ethnic study of atherosclerosis (MESA). Circ Cardiovasc Imaging 2011;4:8–15. 10.1161/CIRCIMAGING.110.959403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuruvilla S, Adenaw N, Katwal AB, et al. Late gadolinium enhancement on cardiac magnetic resonance predicts adverse cardiovascular outcomes in nonischemic cardiomyopathy: a systematic review and meta-analysis. Circ Cardiovasc Imaging 2014;7:250–8. 10.1161/CIRCIMAGING.113.001144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kwong RY, Chan AK, Brown KA, et al. Impact of unrecognized myocardial scar detected by cardiac magnetic resonance imaging on event-free survival in patients presenting with signs or symptoms of coronary artery disease. Circulation 2006;113:2733–43. 10.1161/CIRCULATIONAHA.105.570648 [DOI] [PubMed] [Google Scholar]
- 16.Ganesan AN, Gunton J, Nucifora G, et al. Impact of late gadolinium enhancement on mortality, sudden death and major adverse cardiovascular events in ischemic and nonischemic cardiomyopathy: a systematic review and meta-analysis. Int J Cardiol 2018;254:230–7. 10.1016/j.ijcard.2017.10.094 [DOI] [PubMed] [Google Scholar]
- 17.Thomson LEJ, Wei J, Agarwal M, et al. Cardiac magnetic resonance myocardial perfusion reserve index is reduced in women with coronary microvascular dysfunction. A national heart, lung, and blood Institute-sponsored study from the women's ischemia syndrome evaluation. Circ Cardiovasc Imaging 2015;8. 10.1161/CIRCIMAGING.114.002481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quesada O, AlBadri A, Wei J, et al. Design, methodology and baseline characteristics of the women's ischemia syndrome Evaluation-Coronary vascular dysfunction (WISE-CVD). Am Heart J 2020;220:224–36 https://doi.org/ 10.1016/j.ahj.2019.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braunwald E, Antman EM, Beasley JW, et al. ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction. A report of the American College of Cardiology/American heart association Task force on practice guidelines (Committee on the management of patients with unstable angina). J Am Coll Cardiol 2000;36:970–1062. 10.1016/s0735-1097(00)00889-5 [DOI] [PubMed] [Google Scholar]
- 20.Cain PA, Ahl R, Hedstrom E, et al. Age and gender specific normal values of left ventricular mass, volume and function for gradient echo magnetic resonance imaging: a cross sectional study. BMC Med Imaging 2009;9:2. 10.1186/1471-2342-9-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maceira AM, Prasad SK, Khan M, et al. Normalized left ventricular systolic and diastolic function by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2006;8:417–26. 10.1080/10976640600572889 [DOI] [PubMed] [Google Scholar]
- 22.Nelson MD, Szczepaniak LS, Wei J, et al. Diastolic dysfunction in women with signs and symptoms of ischemia in the absence of obstructive coronary artery disease: a hypothesis-generating study. Circ Cardiovasc Imaging 2014;7:510–6. 10.1161/CIRCIMAGING.114.001714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei J, Bakir M, Darounian N, et al. Myocardial scar is prevalent and associated with subclinical myocardial dysfunction in women with suspected ischemia but no obstructive coronary artery disease: from the women's ischemia syndrome Evaluation-Coronary vascular dysfunction study. Circulation 2018;137:874–6. 10.1161/CIRCULATIONAHA.117.031999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Garovic VD, August P. Preeclampsia and the future risk of hypertension: the pregnant evidence. Curr Hypertens Rep 2013;15:114–21. 10.1007/s11906-013-0329-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ghossein-Doha C, Peeters L, van Heijster S, et al. Hypertension after preeclampsia is preceded by changes in cardiac structure and function. Hypertension 2013;62:382–90. 10.1161/HYPERTENSIONAHA.113.01319 [DOI] [PubMed] [Google Scholar]
- 26.Simmons LA, Gillin AG, Jeremy RW. Structural and functional changes in left ventricle during normotensive and preeclamptic pregnancy. Am J Physiol Heart Circ Physiol 2002;283:H1627–33. 10.1152/ajpheart.00966.2001 [DOI] [PubMed] [Google Scholar]
- 27.Melchiorre K, Sutherland GR, Liberati M, et al. Preeclampsia is associated with persistent postpartum cardiovascular impairment. Hypertension 2011;58:709–15. 10.1161/HYPERTENSIONAHA.111.176537 [DOI] [PubMed] [Google Scholar]
- 28.Scantlebury DC, Kane GC, Wiste HJ, et al. Left ventricular hypertrophy after hypertensive pregnancy disorders. Heart 2015;101:1584–90. 10.1136/heartjnl-2015-308098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ersbøll AS, Bojer AS, Hauge MG, et al. Long-Term cardiac function after peripartum cardiomyopathy and preeclampsia: a Danish nationwide, clinical follow-up study using maximal exercise testing and cardiac magnetic resonance imaging. J Am Heart Assoc 2018;7:e008991. 10.1161/JAHA.118.008991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carter EB, Stuart JJ, Farland LV, et al. Pregnancy complications as markers for subsequent maternal cardiovascular disease: validation of a maternal recall questionnaire. J Womens Health 2015;24:702–12. 10.1089/jwh.2014.4953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Colditz GA, Martin P, Stampfer MJ, et al. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol 1986;123:894–900. 10.1093/oxfordjournals.aje.a114319 [DOI] [PubMed] [Google Scholar]
- 32.Martin LM, Leff M, Calonge N, et al. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med 2000;18:215–8. 10.1016/s0749-3797(99)00158-0 [DOI] [PubMed] [Google Scholar]
- 33.Stuart JJ, Bairey Merz CN, Berga SL, et al. Maternal recall of hypertensive disorders in pregnancy: a systematic review. J Womens Health 2013;22:37–47. 10.1089/jwh.2012.3740 [DOI] [PubMed] [Google Scholar]