Abstract
Objectives
Prader-Willi syndrome (PWS) significantly impacts health-related quality of life; however, its relational and existential aspects remain unknown in Italian clinical and social debate. The project aimed to investigate the impact of PWS on illness experience through narrative medicine (NM) to understand the daily life, needs and resources of patients with PWS and their caregivers, and to furnish insights for clinical practice.
Design and setting
The project involved 10 medical centres of the Italian Network for Rare Diseases and PWS family associations and targeted underage and adult patients with PWS and their caregivers. Written interviews, composed by a sociodemographic survey and a narrative, were collected through the project’s website. Three dedicated illness plots employed evocative and open words to facilitate individual expression and to encourage reflection. Narratives were analysed through NVivo software. Researchers discussed the results with the project’s steering committee.
Participants
Twenty-one children and adolescents and 34 adults with PWS joined the project, as well as 138 caregivers. A PWS diagnosis or the caregiving of a patient with PWS older than 5 years represented the eligibility criteria, as well as the willingness to share their illness experience by writing and the ability to communicate in Italian.
Results
The analysis of narratives led to understanding the PWS social and relational issues concerning diagnosis and current management, PWS daily experiences and social contexts, PWS implications in the working sphere and participants’ future perspectives. Narratives demonstrated that PWS management affects relationships and work-life balance and that social stigma remains present.
Conclusion
The project represented the first effort to investigate the impact of PWS on illness experience in Italy through NM while considering the perspectives of patients with PWS and their caregivers. The findings indicated that a multiprofessional approach is fundamental to ensure adequate treatment and provided elements for its improvement.
Keywords: qualitative research, paediatric endocrinology, paediatric clinical genetics & dysmorphology, eating disorders
Strengths and limitations of this study.
Inclusion of patients with Prader-Willi syndrome (PWS) perspective in the project.
Narrative medicine approach.
Participants did not equally represent the geographical areas of Italy.
Among patients with PWS, researchers included only those able to write.
Introduction
Prader-Willi syndrome (PWS) is a rare genetic condition caused by an absence of functioning paternal genes on chromosome 15 in the 15q11-q13 region1: approximately 65%–70% of the cases are due to the deletion of this region, 20%–30% are caused by a maternal uniparental disomy of chromosome 15 and most of the remaining 2%–5% have an imprinting centre defect or unbalanced translocations (~1%).2 PWS occurs in approximately 1 in 10 000–30 000 births,3 affecting both sexes and all geographic areas.4
Neonatal hypotonia, poor sucking and feeding difficulties characterise PWS in early infancy; dysmorphic signs (mild craniofacial abnormalities, small hands and feet, kyphoscoliosis), multiple endocrine abnormalities (growth hormone (GH)/insulin-like growth factor-I axis dysfunction, hypogonadism, central hypothyroidism and central adrenal insufficiency) and developmental delay constitute other cardinal features of the syndrome.5–7 Learning disabilities, maladaptive behaviours and hyperphagia—leading to life-threatening obesity if uncontrolled—follow in childhood and adulthood.3 8 The mortality rate of patients with PWS is higher than in the general population,9 with a 3% annual death rate across all ages.
Behavioural issues are noticeable in PWS, including aggressive and obsessive-compulsive behaviours and skin picking,10 11 and patients present a higher risk of developing psychiatric illness in adulthood12; food-seeking behaviours are particularly complex and13 significantly affect patients and caregivers’ health-related quality of life (HRQoL). In particular, PWS caregivers—compared with other families managing children’s disability or complex condition—report a higher level of stress, more difficulties in coping with symptoms,14 a higher caregiving burden15 and a lower HRQoL.16
The clinical picture of patients with PWS substantially differs during the lifespan,3 6 and the prognosis is significantly conditioned by proactive interventions to prevent morbid weight excess.9 Currently, no treatment is available for PWS. However, early diagnosis combined with multidisciplinary care favourably influences the course of PWS17; therefore, the diagnosis should be confirmed early during the neonatal period,18 with the support of genetic testing development.19 In this context, early GH treatment has beneficial outcomes on, for example, height, body composition, endurance and sense of well-being20–22; furthermore, early treatment with recombinant GH positively affects the HRQoL of patients with PWS23 and caregivers.24 25
The social, relational, emotional and existential aspects of PWS remain profoundly unknown, and the debate within Italian clinical and social communities has been poor: the WHO has stressed the importance of researching the measurable dimensions of HRQoL and—more broadly—illness experiences in leading clinical and social practice and recommends using narrative research.26
The discipline of narrative medicine (NM), based on illness narratives,27 pursues the integration of the disease-centred approach and is concerned with clinical aspects and the illness-centred and sickness-centred approaches, which respectively focus on individual experience and the social understanding of a specific condition,28 and both have often been neglected by the scientific community. The range of applications for NM is from clinical practice to therapeutic path design, education and research.29 In research, narratives have demonstrated possible interventions on a specific condition through the integration of all perspectives involved in the pathway of care.30 31 Combining evidence-based medicine and NM provides clinicians methods to strengthen clinical practices with narrative competences.29 NM research addresses the individual’s experience when coping with distress caused by clinical conditions: it allows for the understanding of the profound experiences, needs and values of all actors involved in the care pathway.27 32 Scientific societies, healthcare facilities and patient associations have increasingly employed NM research findings to improve the organisation and efficacy of healthcare services, generating sustainability26 and fostering quality of care for patients and their social and relational contexts.27
The NM project ‘PRAXIS: Prader-Willi Excellence in Care with Story Taking’ aimed to investigate the PWS illness experience by employing the analysis of narratives (A) to understand daily life, real needs and personal resources of people with PWS and their caregivers from diagnosis to current management, and by doing so, (B) furnish insights to support a multidisciplinary and a multiprofessional perspective in PWS clinical practice.17 According to our review of the literature, no other project has addressed these issues simultaneously by considering the perspectives of underage and adult patients with PWS and their caregivers.
Methods
Research design and setting
The project was conducted in Italy between October 2018 and July 2019, as a part of a broader research project, and targeted people with PWS and their caregivers, as well as professionals working with PWS. The professionals underwent a webinar conducted by researchers from the ‘Istituto Studi Direzionali’ (Institute of Management Studies, ISTUD) Foundation to be trained in NM and on the project’s aims and methods; moreover, a parallel chart27 33 was identified as the most suitable NM tool to collect their narratives because it constitutes a personal notebook, parallel to the clinical record, in which professionals can write their impressions and feelings in plain language as a supplement to technical and quantitative reports.27 30 33 Participants with PWS were given the possibility to express by drawing if under 5 years old or if unable to write; however, some participants over the threshold of 5 years old decided to maintain both the opportunities of expression.
The target group was people with PWS aged older than 5 years and their caregivers. Participants were recruited from 10 medical centres for paediatric and adult patients in the Italian Network for Rare Diseases (online supplementary material 1), namely six general hospitals and four scientific institutes of research, hospitalisation and healthcare: all the medical centres were macroregional, hospital-based centres that specialised in PWS treatment, and they were distributed among geographical areas (North, Central and South Italy). The Italian Prader-Willi Federation, and the Prader-Willi Association of the Lazio Region were also involved in disseminating the project; in particular, they organised three seminars—one each in the Lombardy, Lazio and Sicily regions—to provide the caregivers of those regions the opportunity to be further informed on NM and the project’s aims and methods.
bmjopen-2019-036502supp001.pdf (35.5KB, pdf)
A PWS diagnosis, determined at the reference medical centre, or a caregiver for a person older than 5 years with PWS represented the eligibility criteria, as well as the willingness to share their illness experience by writing; thus, the ability to communicate in Italian was indispensable for the inclusion in the project. Participants were informed of the possibility to view the projects (in Italian) on the project’s web page: www.medicinanarrativa.eu/praxis
Data collection
Written stories of experiences were collected anonymously through the project’s web page; next, raw and anonymous narratives were downloaded as a Microsoft Excel spreadsheet. A sociodemographic survey constituted the written narrative, together with an illness plot,34 35 namely a plot related to the illness experience: it serves to guide narratives in a chronological order to identify evolutions over time and is characterised by evocative and open words that facilitate individual expression.36
Three illness plots were designed for three different groups—underage and adult patients with PWS, and caregivers (online supplementary material 2)—while addressing common aspects: (A) diagnosis and current management of the condition, namely the strategies related to food behaviours; (B) daily living with PWS, namely the relational sphere and social context; and (C) the work experience and future perspectives.
bmjopen-2019-036502supp002.pdf (38.5KB, pdf)
The project design and the research tools were created by the project’s steering committee, which comprised three endocrinologist experts in PWS, namely one each from the Oasi Maria SS Research Institute (Troina, Italy), the Bambino Gesù Paediatric Hospital of Palidoro (Rome, Italy) and the Istituto Auxologico Italiano of Piancavallo (Oggebbio, Italy), and three researchers from the ISTUD Foundation different for academic backgrounds, to reduce the personal influence on the research.
Patient and public involvement
The research was conducted without patient involvement. Patients did not participate in developing the research design and tools and were not engaged in the interpretation and discussion of the results. Patients were not invited to contribute to the writing or editing of this document.
Ethical considerations
The project was performed according to the principles of the Declaration of Helsinki. Before the participants’ involvement, they provided written informed consent after being briefed on the project’s purpose and confidential data handling procedures, according to the Italian Law 196/2003 on Privacy and the Safeguarding of Sensitive Data37 and the General Data Protection Regulation of the European Union 2016/679.38 Involved professionals obtained written informed consent to participate from parents and tutors for underage participants during the first interview on the project’s methods and purposes. Next, the professionals briefed the underage patients on the project and obtained their verbal consent to participate. Moreover, written informed consent to participate was obtained from adult participants and/or their tutors when appropriate. The Ethical Committee of the Oasi Maria SS Research Institute (Troina, Italy) approved the project in January 2019 with the ethics approval number 2019/01/09/CE-IRCCS-OASI/19.
Analysis
We analysed the sociodemographic survey through descriptive statistics; no question was mandatory.
We separately examined the caregivers and patients’ perspectives. Anonymous narratives were entered into NVivo software39 for coding and analysis. ISTUD researchers collectively coded 10 narratives in NVivo to assess consistency across team members. Afterwards, each narrative was coded separately by at least two researchers and then reviewed during weekly meetings and peer debriefings to reduce bias in the interpretation of texts. Open interpretive coding was employed to identify and analyse emerging topics; Kleinman’s28 classification was retrospectively applied to the analysis of narratives because the researchers considered it the most suitable to further reveal illness-related and sickness-related aspects in narratives, respectively concerning the personal and emotional experience of a condition and how it is perceived within society.
The analysis process and results were shared within the project’s steering committee to collectively address emerged topics and interpretation of data. Researchers followed the Standards for Reporting Qualitative Research reporting guidelines.40
Results
Sociodemographic aspects
Twenty-one children and adolescents and 34 adults with PWS participated in the project, as well as 138 caregivers. Table 1 summarises the sociodemographic data of these three groups; the representation includes non-responses as a separate category.
Table 1.
Sociodemographic data of participants
| Minors with PWS (n=21) |
Adults with PWS (n=34) |
PWS caregivers (n=138) |
|
| Gender (%) | |||
| Females | 6 (29) | 19 (56) | 99 (72) |
| Males | 15 (71) | 15 (44) | 37 (27) |
| Non-responses | 0 | 0 | 2 (1) |
| Age (years) | |||
| Mean (SD) | 14 (3.09) | 29 (9.72) | 48 (9.04) |
| Minimum | 7 | 19 | 20 |
| Maximum | 18 | 48 | 61 |
| Geographic residence (%) | |||
| Northern Italy | 3 (13) | 19 (58) | 29 (21) |
| Central Italy | 4 (19) | 6 (18) | 40 (29) |
| Southern Italy | 14 (69) | 9 (24) | 69 (50) |
| Non-responses | 0 | 0 | 0 |
| Education (%) | |||
| Elementary school | 10 (48) | 2 (6) | 5 (4) |
| Middle school | 5 (24) | 10 (30) | 19 (14) |
| High school | 2 (10) | 21 (64) | 76 (55) |
| University degree | 0 | 1 (1) | 19 (14) |
| Non-responses | 4 (19) | 0 | 19 (13) |
| Marital status (%) | |||
| Single | 21 (100) | 33 (97) | 3 (2) |
| Married/cohabitate | 0 | 1 (3) | 118 (86) |
| Divorced/separated | 0 | 0 | 14 (10) |
| Widowed | 0 | 0 | 3 (2) |
| Non-responses | 0 | 0 | 0 |
| Employment status (%) | |||
| Student | 21 (100) | 4 (11) | 3 (2) |
| Working | 0 | 19 (56) | 94 (68) |
| Not working | 0 | 11 (33) | 38 (28) |
| Retired | 0 | 0 | 3 (2) |
| Non-responses | 0 | 0 | 0 |
Data presented as n (%) or mean (SD) and minimum/maximum.
PWS, Prader-Willi syndrome.
Results from the analysis are presented by following the dedicated illness plots’ structure: (A) the first section concerns PWS diagnosis and current management, in which narratives’ illness-related and sickness-related aspects, caregivers’ perspectives on therapeutic path and strategies to manage food-seeking behaviours are addressed; (B) the second section focuses on living with PWS in relational and social contexts and addresses participants’ indoor and outdoor daily activities; (C) the third section concerns the narratives on the working sphere of caregivers and adult patients with PWS and participants’ future perspectives and desires.
From diagnosis to the current management of PWS
Thirty-six per cent of caregivers reported that their children were diagnosed with PWS within the first month of life (figure 1); however, 10% affirmed that the diagnosis occurred after the child’s third year of life.
Figure 1.
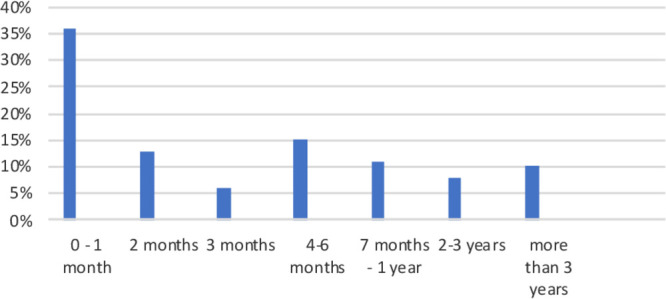
Age of children with Prader-Willi syndrome (PWS) at diagnosis.
In narratives, 95% of caregivers focused on PWS illness and sickness-related aspects (table 2); the remaining 5% adopted technical and clinical language28 to discuss the condition, as exemplified in the following two quotes from narratives: (A) She was hospitalised at the Neurology department for a muscle biopsy; diagnosed with congenital myopathy and 2 years later, underwent the DNA test. She was sent to a hospital in Northern Italy, and from there, we got the Prader-Willi diagnosis (Caregiver 015). (B) He underwent nine surgeries: adenoids, laryngotomy, broken arm fracture, desmoid, flat foot, strabismus. He has been taking GH since he was a child (Caregiver 063). Disbelief, displacement, anger and pain represented the most recurrent emotions expressed by caregivers when attempting to adapt to the situation and its criticalities. Patients with PWS—underage and adult—described the condition only through its illness-related and sickness-related facets.
Table 2.
Illness and sickness-related aspects: quotes from narratives
| Caregivers | Minors and adults with Prader-Willi syndrome | |
| Illness |
|
|
| Sickness |
|
|
PWS, Prader-Willi syndrome.
In table 3, a focus on therapeutic paths from the caregivers’ perspective meant addressing (A) relationships with different professionals and (B) healthcare structures, and the (C) necessary or employed treatments, beyond diet.
Table 3.
Perspectives from PWS caregivers on the therapeutic path: quotes from narratives
| Professionals |
|
| Healthcare structures |
|
| Treatments |
|
GH, growth hormone; PWS, Prader-Willi syndrome.
From caregivers’ narratives, food-seeking behaviours13 emerged as the most challenging event within the domestic context. Caregivers were aware that feeding is the first treatment for people with PWS and sought strategies to feed them. Fifty per cent declared that they had achieved a balance, and the other 50% reported a problematic relationship with food. Both underage and adult participants with PWS were aware of the importance of following a diet: positive or negative relationships with food emerged from narratives, where (A) the positive relationships also represented the result of commitment and several strategies to manage food-seeking behaviours, and (B) food seeking was related to emotions (eg, anger). Table 4 shows the main elements that emerged from the caregivers and PWS participants’ narratives.
Table 4.
Attitudes towards food-seeking behaviours: quotes from narratives
| Caregivers | Minors and adults with Prader-Willi syndrome | |
| Commitment |
|
|
| Strategies |
|
|
| Criticalities |
|
|
PWS, Prader-Willi syndrome.
Living with PWS in relationships and in social contexts
Thirty-six per cent of PWS caregivers described daily life at home as quiet; however, most (64%) reported: fatigue (21%), chaos (6%), all-encompassing assistance (20%) and using tested routines to better manage food-seeking behaviours (17%). They have attempted to maintain their hobbies, interests and outside activities, even though their sons and daughters have PWS (table 5). Relationships external to the family are difficult to preserve, imposing a radical change in social life. Indoor and outdoor activities represented an essential tool for caregivers in managing emotion patterns and food-seeking behaviours: narratives demonstrated that underage and adult participants with PWS were aware of that. Sport, mind activity games, gardening and pet therapy were some of the most helpful activities reported; furthermore, patients with PWS appeared dedicated to cleanliness and routine activities. Both relational and activity spheres revealed the influence of behavioural and emotional changes in daily life and in familiar and social contexts; moreover, narratives addressed the strong presence of caregivers, as well as situations of social inclusion or exclusion.
Table 5.
Living with Prader-Willi syndrome (PWS) in activities and relationships: quotes from narratives
| Caregivers | Minors and adults with PWS | |
| Indoor activities |
|
|
| Outdoor activities |
|
|
| Relationships |
|
|
Work and future perspectives
Sixty-two per cent of family caregivers had to change their job after the birth of their child with PWS (table 6): more than one-third left their current work, 8% changed jobs to assist the child, 8% requested a part-time job and 3% abandoned the perspective of a career. From a gender perspective, 63% of female (mothers) and 33% of male caregivers had to change their current job to adapt to the child’s condition. Forty-six per cent did not discuss PWS in the workplace or discussed PWS with only their closest colleagues; 36% reported comprehensive behaviours, and 18% declared a lower understanding of PWS management necessities than for other diseases, such as cancer. Based on the narratives, work was a positive personal resource. Fifty-six per cent of adults with PWS declared that they were working in jobs mainly characterised by low complexity and repetitive operations and conducted in social cooperatives or centres, small companies with high corporate social responsibility and family companies. Work is a source of pride and well-being and a distraction from food, but episodes of irritability and aggressive behaviours have been reported.
Table 6.
Prader-Willi syndrome and the work sphere: quotes from narratives
| Adults with PWS |
|
| PWS caregivers |
|
PWS, Prader-Willi syndrome.
Regarding future perspectives, PWS family caregivers hope to have long lives so that they can care for their sons and daughters as long as possible, and they were particularly concerned with what would happen to their children without familial support (table 7). Caregivers also addressed social inclusion, such as social changes and openness, rather than clinical solutions to PWS. Adult participants with PWS demonstrated self-realisation through work (27%)—as underage participants did—and the desire to have a family (46%), recover from PWS (10%) and generally live well (14%).
Table 7.
Living with Prader-Willi syndrome and future thoughts: quotes from narratives
| Minors with PWS |
|
| Adults with PWS |
|
| PWS caregivers |
|
PWS, Prader-Willi syndrome.
Discussion
The PRAXIS project represents the first effort to investigate the PWS illness experience in Italy through NM by simultaneously considering the perspectives of underage and adult patients with PWS and their caregivers. The project first aimed to understand their daily life, real needs and personal resources. Fifty-five participants, namely children, adolescents and adults with PWS, reported joy and pride in sharing their stories, also suggesting that using evocative and open words36 in structuring illness plots can be crucial to helping people to express themselves. Moreover, the collection of 138 caregiving stories suggested a strong dedication to the survey and the need for caregivers to be listened to: they described writing as liberating, demonstrating its potential (A) to have a therapeutic effect27 33 and (B) to be a safe space from the attitude of passing,41 namely handling information considered discrediting or critical for the self to avoid social stigma.
Talking about PWS emerged as a ‘taboo’. In illness-centred and sickness-centred narratives,28 caregivers encountered significant difficulties in socialising the challenges PWS imposes in daily life, as well as the pain of having a child ‘different’ from social imagery: we identify this as a social pain that also concerns caregivers when performing familiar criticalities. Furthermore, caregivers considered the project a chance to invite society to integrate people with PWS and to denounce the stigma41 that surrounds them.
If the literature demonstrates cognitive impairment in people with PWS,6 we would like to enrich the evidence by suggesting the consideration of the multiple intelligences42 these people demonstrate in their everyday experience. In line with Gardner’s42 reflection, revealing alternatives to the standard forms of intelligence (the logical-mathematical and linguistic ones), the narratives demonstrated the constant use of visuospatial, musical, interpersonal, existential and introspective talents, resources and capabilities. In this regard, patients with PWS have been reported to show above-average performance in several tasks implying visuospatial skills,43 which in the general population are linked with higher math abilities.44 In particular, the importance of multiple intelligences emerged in food-control strategies and activities, consequently suggesting that considering them may positively influence the overall illness experience.
Considering the second purpose of the project, specific elements emerged from the analysis of therapeutic paths. PWS diagnosis mostly occurred up to the child’s second year of life, but in some cases, a significant delay remained, particularly for those people living away from specialised centres. Because timing is essential in PWS treatment,9 training for neonatologists, geneticists and general paediatricians on PWS might improve early diagnosis. Moreover, the other professionals involved also must develop or strengthen specific PWS competencies to appropriately address this condition.
The narratives demonstrated some peculiar clinical PWS characteristics, such as irritability, aggressive and obsessive-compulsive behaviour10 11 and food-seeking13 behaviours. The last resulted in the most challenges for the people with PWS and their caregivers: food management strategies,45 and indoor and outdoor activities46 and school or work schedules,47 48 can help people with PWS and their caregivers improve their relationships with food and family members, enhancing overall daily life.
Diet management and strategies, early GH therapy, clinical and psychiatric treatments, activities in specialised or social centres and the different professional roles involved demonstrated that a mutiprofessional approach that integrates the factors of hospital and territory is fundamental to ensure adequate treatment of PWS17 47 49 and to mitigate the burden of caregiving reported in the narratives and the literature.14–16 In particular, two related topics emerged: (A) mostly women (mothers) changed or retired from work to become a caregiver; (B) family caregivers stated their concerns regarding what will happen to their sons and daughters if no family members are available—a topic already addressed by Italian Law 112/2016, on the social inclusion and autonomy of people with disabilities. These considerations also suggest, on the one hand, that social centres and services are crucial but need to be implemented in areas that have insufficient support for people with PWS and their caregivers, and on the other hand, a focus on work policies to create autonomy and social inclusion. Overcoming economic, legal and social barriers and improving the current service provision still represent a challenge; patient organisations and scientific societies may have a crucial role in addressing these issues. Furthermore, although a national plan for rare diseases50 has been developed in Italy since 2013, its application in daily practice remains demanding. One possible intervention strategy to reduce medical barriers requires universities and scientific societies to develop specific educational programmes; in particular, creating a PWS national register may help interface with similar international tools.51
The acknowledgement of the importance of multiple intelligences42 in everyday experiences may also improve the daily and relational life of people with PWS or their caregivers, together with ameliorating the social stigma of PWS and enhancing social inclusion. Multiple intelligences might also become a tool in clinical practice to better evaluate people with PWS; moreover, an evolving model for PWS care should include modern technologies, for example, video visits, remote monitoring and electronic health records.52
The participants in the project did not equally represent the different geographical areas in Italy because of the local distribution of expert centres in the management of care for PWS, and this could be a selection bias. Furthermore, the results are specific because of (A) the voluntary nature of the project and (B) the critical difference among Italian regional healthcare systems; therefore, further analysis is required. For people with PWS, the inclusion criterion of being able to write represented another bias.
In conclusion, this NM project provides new insights into the individual and social experiences related to PWS and provides elements for improving multidisciplinary and multiprofessional perspectives on this condition: the social, relational and emotional aspects of PWS crucially influence the illness experience and narratives that can foster the relationship between PWS professionals, patients, families and the community.
Supplementary Material
Acknowledgments
The authors wish to thank all participants in the project, the Italian Prader-Willi Federation and the Prader-Willi Association of Lazio Region for their active contribution. Acknowledgements are extended also to the researchers of the Healthcare Area of ISTUD Foundation for their useful role throughout this project and to Enago (www.enago.com) for the English language review.
Footnotes
Contributors: Conceptualisation: LRagusa, AC, GG, LReale, MGM. Analysis: LReale, AF. Investigation: LRagusa, AC, GG, LReale, AF, MRL, MFF, MW, MD, AF, IR, PF, DC, GC, DG, MC, MS, ST, MGM. Methodology: LReale, MGM. Project administration: LReale, LRagusa, AC, GG, MGM. Report visualisation: LRagusa, AC, GG, LReale, AF, MRL, MFF, MW, MD, AF, IR, PF, DC, GC, DG, MC, MS, ST, MGM. Writing: AF, LRagusa, AC, GG, LReale, MGM. Editing: AF.
Funding: Sandoz unconditionally supported the ISTUD Foundation for the realisation of the project.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Comitato Etico dell’IRCCS Associazione Oasi Maria SS (number ID 2019/01/09/CE-IRCCS-OASI/19). The study was approved on 9 January 2019.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. All data relevant to the project are included in the present manuscript. Original narratives are available in Italian upon request at the email areasanita@istud.it.
References
- 1.Butler MG, Hartin SN, Hossain WA, et al. Molecular genetic classification in Prader-Willi syndrome: a multisite cohort study. J Med Genet 2019;56:149–53. 10.1136/jmedgenet-2018-105301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irizarry KA, Miller M, Freemark M, et al. Prader Willi syndrome: genetics, metabolomics, hormonal function, and new approaches to therapy. Adv Pediatr 2016;63:47–77. 10.1016/j.yapd.2016.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cassidy SB, Schwartz S, Miller JL, et al. Prader-Willi syndrome. Genet Med 2012;14:10–26. 10.1038/gim.0b013e31822bead0 [DOI] [PubMed] [Google Scholar]
- 4.Vogels A, Van Den Ende J, Keymolen K, et al. Minimum prevalence, birth incidence and cause of death for Prader-Willi syndrome in Flanders. Eur J Hum Genet 2004;12:238–40. 10.1038/sj.ejhg.5201135 [DOI] [PubMed] [Google Scholar]
- 5.Heksch R, Kamboj M, Anglin K, et al. Review of Prader-Willi syndrome: the endocrine approach. Transl Pediatr 2017;6:274–85. 10.21037/tp.2017.09.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Angulo MA, Butler MG, Cataletto ME. Prader-Willi syndrome: a review of clinical, genetic, and endocrine findings. J Endocrinol Invest 2015;38:1249–63. 10.1007/s40618-015-0312-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crinò A, Di Giorgio G, Livieri C, et al. A survey on Prader-Willi syndrome in the Italian population: prevalence of historical and clinical signs. J Pediatr Endocrinol Metab 2009;22:883–93. 10.1515/JPEM.2009.22.10.883 [DOI] [PubMed] [Google Scholar]
- 8.Hartley SL, Maclean WE, Butler MG, et al. Maladaptive behaviors and risk factors among the genetic subtypes of Prader-Willi syndrome. Am J Med Genet A 2005;136:140–5. 10.1002/ajmg.a.30771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manzardo AM, Loker J, Heinemann J, et al. Survival trends from the Prader-Willi syndrome association (USA) 40-year mortality survey. Genet Med 2018;20:24–30. 10.1038/gim.2017.92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guinovart M, Coronas R, Caixàs A. Psychopathological disorders in Prader-Willi syndrome. Endocrinol Diabetes Nutr 2019;66:579–87. 10.1016/j.endinu.2019.03.004 [DOI] [PubMed] [Google Scholar]
- 11.Sinnema M, Einfeld SL, Schrander-Stumpel CTRM, et al. Behavioral phenotype in adults with Prader-Willi syndrome. Res Dev Disabil 2011;32:604–12. 10.1016/j.ridd.2010.12.014 [DOI] [PubMed] [Google Scholar]
- 12.Yang L, Zhan G-dong, Ding J-jie, et al. Psychiatric illness and intellectual disability in the Prader-Willi syndrome with different molecular defects--a meta analysis. PLoS One 2013;8:e72640. 10.1371/journal.pone.0072640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller JL, Lynn CH, Driscoll DC, et al. Nutritional phases in Prader-Willi syndrome. Am J Med Genet A 2011;155A:1040–9. 10.1002/ajmg.a.33951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanfranchi S, Vianello R. Stress, locus of control, and family cohesion and adaptability in parents of children with Down, Williams, fragile X, and Prader-Willi syndromes. Am J Intellect Dev Disabil 2012;117:207–24. 10.1352/1944-7558-117.3.207 [DOI] [PubMed] [Google Scholar]
- 15.Kayadjanian N, Schwartz L, Farrar E, et al. High levels of caregiver burden in Prader-Willi syndrome. PLoS One 2018;13:e0194655. 10.1371/journal.pone.0194655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mazaheri MM, Rae-Seebach RD, Preston HE, et al. The impact of Prader-Willi syndrome on the family's quality of life and caregiving, and the unaffected siblings' psychosocial adjustment. J Intellect Disabil Res 2013;57:861–73. 10.1111/j.1365-2788.2012.01634.x [DOI] [PubMed] [Google Scholar]
- 17.Crinò A, Fintini D, Bocchini S, et al. Obesity management in Prader-Willi syndrome: current perspectives. Diabetes Metab Syndr Obes 2018;11:579–93. 10.2147/DMSO.S141352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gunay-Aygun M, Schwartz S, Heeger S, et al. The changing purpose of Prader-Willi syndrome clinical diagnostic criteria and proposed revised criteria. Pediatrics 2001;108:e92. 10.1542/peds.108.5.e92 [DOI] [PubMed] [Google Scholar]
- 19.Hartin SN, Hossain WA, Francis D, et al. Analysis of the Prader–Willi syndrome imprinting center using droplet digital PCR and next‐generation whole‐exome sequencing. Mol Genet Genomic Med 2019;7:e00575 10.1002/mgg3.575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grugni G, Marzullo P. Diagnosis and treatment of GH deficiency in Prader-Willi syndrome. Best Pract Res Clin Endocrinol Metab 2016;30:785–94. 10.1016/j.beem.2016.11.003 [DOI] [PubMed] [Google Scholar]
- 21.Deal CL, Tony M, Höybye C, et al. GrowthHormone research Society workshop summary: consensus guidelines for recombinant human growth hormone therapy in Prader-Willi syndrome. J Clin Endocrinol Metab 2013;98:E1072–87. 10.1210/jc.2012-3888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanchez-Ortiga R, Klibanski A, Tritos NA. Effects of recombinant human growth hormone therapy in adults with Prader-Willi syndrome: a meta-analysis. Clin Endocrinol 2012;77:86–93. 10.1111/j.1365-2265.2011.04303.x [DOI] [PubMed] [Google Scholar]
- 23.Moix Gil E, Giménez-Palop O, Caixàs A. Treatment with growth hormone in the Prader-Willi syndrome. Endocrinol Diabetes Nutr 2018;65:229–36. 10.1016/j.endinu.2018.01.006 [DOI] [PubMed] [Google Scholar]
- 24.Bakker NE, Siemensma EPC, van Rijn M, et al. Beneficial effect of growth hormone treatment on health-related quality of life in children with Prader-Willi syndrome: a randomized controlled trial and longitudinal study. Horm Res Paediatr 2015;84:231–9. 10.1159/000437141 [DOI] [PubMed] [Google Scholar]
- 25.Bertella L, Mori I, Grugni G, et al. Quality of life and psychological well-being in GH-treated, adult PWS patients: a longitudinal study. J Intellect Disabil Res 2007;51:302–11. 10.1111/j.1365-2788.2006.00878.x [DOI] [PubMed] [Google Scholar]
- 26.Greenhalgh T. Cultural contexts of health: the use of narrative research in the health sector. Copenhagen: who regional office for Europe; 2016, health evidence network (hen) synthesis report 49. Available: http://www.euro.who.int/__data/assets/pdf_file/0004/317623/HEN-synthesis-report-49.pdf [Accessed 26 Feb 2020]. [PubMed]
- 27.Marini MG. Narrative medicine: bridging the gap between evidence-based care and medical humanities. London: Springer International Publishing, 2016. [Google Scholar]
- 28.Kleinman A. The illness narrative, suffering and healing the human condition. New York: Basic Book, 1989. [Google Scholar]
- 29.Greenhalgh T, Hurwitz B. Narrative based medicine: why study narrative? BMJ 1999;318:48–50. 10.1136/bmj.318.7175.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Banfi P, Cappuccio A, Latella ME, et al. Narrative medicine to improve the management and quality of life of patients with COPD: the first experience applying parallel chart in Italy. Int J Chron Obstruct Pulmon Dis 2018;13:287–97. 10.2147/COPD.S148685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marini MG, Chesi P, Mazzanti L, et al. Stories of experiences of care for growth hormone deficiency: the CRESCERE project. Future Sci OA 2016;2:FSO82. 10.4155/fso.15.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Vincentis G, Monari F, Baldari S, et al. Narrative medicine in metastatic prostate cancer reveals ways to improve patient awareness & quality of care. Future Oncol 2018;14:2821–32. 10.2217/fon-2018-0318 [DOI] [PubMed] [Google Scholar]
- 33.Charon R. The patient-physician relationship. narrative medicine: a model for empathy, reflection, profession, and trust. JAMA 2001;286:1897–902. 10.1001/jama.286.15.1897 [DOI] [PubMed] [Google Scholar]
- 34.Marini MG. Languages of care in narrative medicine. words, space and time in the healthcare ecosystem. London: Springer International Publishing, 2019. [Google Scholar]
- 35.Reid K, Soundy A. A qualitative study examining the illness narrative master plots of people with head and neck cancer. Behav Sci 2019;9:110. 10.3390/bs9100110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peeters B, Marini M. Narrative medicine across languages and cultures: using minimal English for increased comparability of patients’ narratives : Goddard C, Minimal English for a global world: improved communication using fewer words. Basingstoke, UK: Palgrave Macmillan, 2018: 259–86. [Google Scholar]
- 37.Personal data code protection. Legislat. decree No. 196 of 30 June 2003. published on the Italian official Journal N. 174, July 29, 2003, supplementary N. 123. Available: https://www.camera.it/parlam/leggi/deleghe/Testi/03196dl.htm [Accessed 15 Jun 2020].
- 38.Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing directive 95/46/EC (General data protection regulation. published on the official Journal of the European Union L 119, may 4, 2016. Available: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32016R0679 [Accessed 15 Jun 2020].
- 39.Bazeley P, Jackson K. Qualitative data analysis with NVivo. London: SAGE, 2013. [Google Scholar]
- 40.O'Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245–51. 10.1097/ACM.0000000000000388 [DOI] [PubMed] [Google Scholar]
- 41.Goffman E. Stigma. London: Penguin, 1963. [Google Scholar]
- 42.Gardner H. Frames of mind: the theory of multiple Intelligences. New York: Basic Books, 1983. [Google Scholar]
- 43.Semenza C, Pignatti R, Bertella L, et al. Genetics and mathematics: evidence from Prader-Willi syndrome. Neuropsychologia 2008;46:206–12. 10.1016/j.neuropsychologia.2007.07.017 [DOI] [PubMed] [Google Scholar]
- 44.Fanari R, Meloni C, Massidda D. Visual and spatial working memory abilities predict early math skills: a longitudinal study. Front Psychol 2019;10:2460. 10.3389/fpsyg.2019.02460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mackenzie ML, Triador L, Gill JK, et al. Dietary intake in youth with Prader-Willi syndrome. Am J Med Genet A 2018;176:2309–17. 10.1002/ajmg.a.40491 [DOI] [PubMed] [Google Scholar]
- 46.Rubin DA, Wilson KS, Dumont-Driscoll M, et al. Effectiveness of a parent-led physical activity intervention in youth with obesity. Med Sci Sports Exerc 2019;51:805–13. 10.1249/MSS.0000000000001835 [DOI] [PubMed] [Google Scholar]
- 47.Duis J, van Wattum PJ, Scheimann A, et al. A multidisciplinary approach to the clinical management of Prader-Willi syndrome. Mol Genet Genomic Med 2019;7:e514. 10.1002/mgg3.514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vogels A, Scheermeyer E. Coordination of the multidisciplinary treatment efforts : Hoybye C, Prader–Willi syndrome. New York: Nova Science Publishers, 2013: 229–54. [Google Scholar]
- 49.Mackay J, McCallum Z, Ambler GR, et al. Requirements for improving health and well-being of children with Prader-Willi syndrome and their families. J Paediatr Child Health 2019;55:1029–37. 10.1111/jpc.14546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Italian Ministry of Health Piano Nazionale delle Malattie rare 2013-2016. Rome: Ministry of health, 2013. Available: http://www.europlanproject.eu/DocumentationAttachment/Italian%20National%20Plan%20for%20Rare%20Diseases%202013-2016%20-%20eng%20(en)%20%20%5Bunofficial%20version%20by%20EUROPLAN%5D.pdf [Accessed 26 Feb 2020].
- 51.Ali SR, Bryce J, Cools M, et al. The current landscape of European registries for rare endocrine conditions. Eur J Endocrinol 2019;180:89–98. 10.1530/EJE-18-0861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Augustine EF, Dorsey ER, Saltonstall PL. The care continuum: an evolving model for care and research in rare diseases. Pediatrics 2017;140:e20170108. 10.1542/peds.2017-0108 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-036502supp001.pdf (35.5KB, pdf)
bmjopen-2019-036502supp002.pdf (38.5KB, pdf)


