Abstract
BACKGROUND
Patients undergoing implantable cardioverter-defibrillator (ICD) implantations have high rates of long-term device-related complications and reoperations. Whether physician specialty training is associated with differences in long-term outcomes following ICD implantation is unclear.
METHODS AND RESULTS
We linked data from the National Cardiovascular Data Registry ICD Registry with Medicare fee-for-service claims to identify physicians who performed ≥10 index ICDs from 2006 to 2009. We used data from the American Board of Medical Specialties to group the specialty of the implanting physician into mutually exclusive categories: electrophysiologists, interventional cardiologists, general cardiologists, thoracic surgeons, and other specialties. Primary outcomes were long-term device-related complications requiring reoperations or hospitalizations and reoperations for reasons other than complications. We compared the cumulative incidence rates and case-mix adjusted rates of long-term outcomes of index ICD implantations across physician specialties. Our analysis had a median follow-up of 47 months and included 107 966 index ICD implantations. Electrophysiologists had the lowest rates of incident long-term device-related complications (14.1%; interventional cardiologists, 15.3%; general cardiologists, 15.4%; thoracic surgeons, 16.4%; other specialists, 15.2%; P<0.001) and reoperations for reasons other than complications (electrophysiologists, 16.7%; interventional cardiologists, 17.0%; general cardiologists, 18.0%; thoracic surgeons, 18.4%; other specialists, 18.0%; P<0.001). Compared with patients whose ICDs were implanted by electrophysiologists, patients with implantations performed by nonelectrophysiologists were at higher risk of having long-term device-related complications (relative risk for interventional cardiologists: 1.16 [95% CI, 1.08–1.25]; general cardiologists: 1.13 [1.08 –1.18]; thoracic surgeons: 1.20 [1.06–1.37]; all P<0.001, but not other specialists: 1.08 [0.99–1.17]; P=0.07). Compared to patients with implantations performed by electrophysiologists, patients with implantations performed by general cardiologists and thoracic surgeons were at higher risk of reoperation for noncomplication causes (relative risk for general cardiologists: 1.10 [1.05–1.15]; thoracic surgeons: 1.16 [1.00–1.33]; both P<0.05).
CONCLUSIONS
Patients with ICD implantations performed by electrophysiologists had the lowest risks of having long-term device-related complications and reoperations for noncomplication causes. Consideration of physician specialty before ICD implantation may represent an opportunity to minimize long-term adverse outcomes.
Keywords: cardiac resynchronization therapy, hospitalization, incidence, reoperation, risk
Randomized controlled studies have shown that implantable cardioverter-defibrillators (ICDs) improve survival in patients at high risk of sudden cardiac death.1–5 Consequently, ICDs have become a mainstay of therapy, but there remains controversy as to whether physicians not trained as electrophysiologists should implant these devices. A prior study demonstrated that in-hospital complication rates vary by provider training such that implants performed by electrophysiologists were associated with lower rates of in-hospital complications, higher rates of optimal medical therapy, and increased use of cardiac resynchronization therapy (CRT) among eligible patients compared with those of implants performed by nonelectrophysiologist physicians.6 However, whether physician training is associated with differences in longer-term outcomes following ICD implantation is not known.
Understanding the presence and extent of differences in longer-term outcomes following ICD implantation is important as many device-related complications may not be apparent until well after hospital discharge.7 For this reason, focusing on in-hospital complications may not provide a complete picture of training-based differences in outcome. Furthermore, physician specialty may be associated with longer-term outcomes including reoperations. Understanding this relationship is important because reoperations such as device upgrades or generator changes are not without risk and avoiding such reoperations can potentially prevent a patient from undergoing unnecessary exposure to harm.8,9
To address this gap in knowledge, we linked longitudinal data from the National Cardiovascular Data Registry-ICD Registry (NCDR ICD Registry) with Medicare fee-for-service administrative claims data to assess the association of physician specialty and longer-term outcomes. Specifically, we examined the association of physician specialty with risks of ICD complications requiring acute hospitalizations or reoperations and ICD reoperations for reasons other than complications. Understanding whether long-term outcomes vary by physician specialty will inform decisions about the practice of nonelectrophysiologists implanting ICDs.
METHODS
Data Sources
The NCDR ICD registry gathers data on ICD and CRT-defibrillator (CRT-D) implantations, revisions, and replacements.10,11 From 2006 to 2018, the Center for Medicare and Medicaid services mandated submission of data in the ICD registry as a stipulation for payment for all primary prevention ICD implantations performed on Medicare patients.12 The registry collects demographics, procedural, and clinical status using standardized definitions. For this analysis, we used data from ICD implantations using Version 1.0 of the registry of the data collection form. To identify information about complications and reoperations following discharge, we linked registry data with corresponding Medicare claims data using the deterministic matching method based on patients’ age, gender, admission date or procedure date, and hospital provider number. The data and analytical methods will not be available to other researchers for the purpose of study replication.
Patient Population
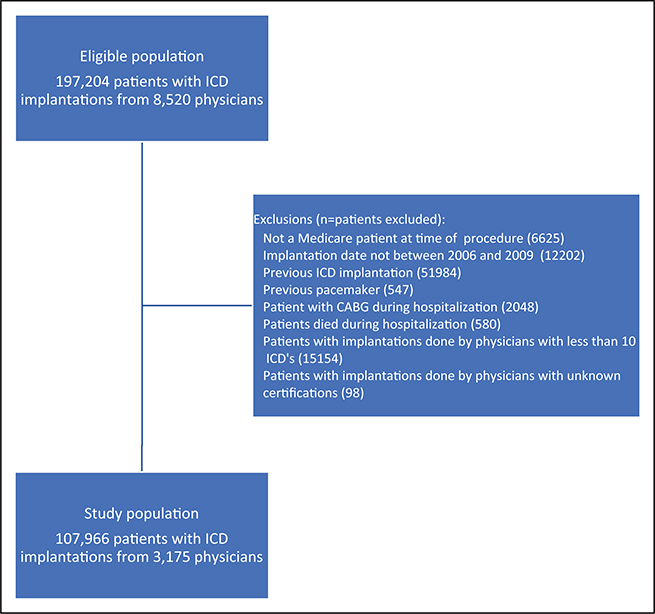
The study cohort consisted of all patients included in the ICD registry undergoing first-time device implantation between January 2006 and December 2009. To link registry data to Medicare, we restricted our cohort to patients 65 years and older and who were fee-for-service Medicare beneficiaries. We excluded patients with a previous ICD or pacemaker to ensure the index implantation was not a result of a previous device-related complication, patients with coronary artery bypass surgery during the index hospitalization as any short-term complication may be related to the surgery, and patients who died during the index hospitalization. We excluded patients whose physician had fewer than 10 ICD procedures submitted to the ICD registry given a known relationship between volume and outcomes.13 Finally, we excluded any patients that had ICDs performed by physicians for which we could not identify their specialties (Figure 1). Medicare fee-for-service data were available through December 2011. Overall, the median follow-up was 47 months (range: 23–72 months).
Figure 1. Cohort selection.
CABG indicates coronary artery bypass surgery; and ICD, implantable cardioverter-defibrillator.
Physician Specialty Identification
We identified physicians in the ICD registry using a combination of name and National Provider Identifier or unique physician identification numbers. Specialty status was obtained through information from databases of the American Board of Internal Medicine and the American Board of Medical Specialties, which contains certification information drawn from 24 Member Boards including the American Board of Internal Medicine, Surgery, and Thoracic Surgery.14,15 Physicians were grouped into mutually exclusive categories that reflected their most recently documented specialty. The specific categories were electrophysiologists, interventional cardiologists, general cardiologists, thoracic and cardiac surgeons, and other specialists. The “other” category included physicians such as internists or general surgeons that did not obtain specialty training in general cardiology or thoracic or cardiac surgery.
Outcomes
The methodology used to identify device-related events has been described previously.5 The primary outcome was the occurrence of any ICD-related complication that required reoperation, emergency department visit, observation stay, or hospitalization post-discharge. For reoperations, we used the Healthcare Common Procedure Coding System procedure codes in outpatient claims and International Classification of Diseases, Ninth Revision, Clinical Modification procedures codes in inpatient claims. We used revenue center codes from outpatient claims data to define emergency department visits and observation stays. To identify ICD complications, we used principle or secondary diagnosis codes from the International Classification of Diseases, Ninth Revision, Clinical Modification. We also grouped the ICD complications into device-related mechanical complications; infection (device-specific, systemic infection, endocarditis, and other procedural-related infections); pocket-related complications (hemorrhage or hematoma, wound disruption, foreign body left during procedure, and persistent postoperative fistula); and other complications (pneumothorax, pleural effusion, pericardial effusion, perforation, and superior vena cava obstruction/venous thromboembolism; Table I in the Data Supplement). We did not consider any ICD-related complication that did not result in an acute hospitalization or reoperation.
Secondary outcomes included all ICD reoperations that were not associated with the aforementioned complications (Table II in the Data Supplement). These reoperations include generator battery changes, lead revisions, electrode insertion, and upgrade procedures. We included these procedures as an outcome as they still remain a significant event to patients and carry an elevated risk of complications and death peri- and post-procedurally.
Statistical Analysis
We compared patient characteristics of ICD implantations across physician specialty categories using χ2 tests for categorical variables and ANOVA for continuous variables. Patient characteristics included demographics, comorbid medical conditions, and cardiac status. Because of unbalanced data among different physician categories, the ANOVA test was done using generalized linear models.
To compare ICD complications and ICD reoperations post-discharge across specialty categories, we estimated the cumulative incidence rates (the proportion of patients who experienced an outcome in our study window), taking into account the competing risk of death. We then plotted the cumulative incidence across specialty categories for ICD complications and reoperations for reasons other than complications for each ICD type placed. Given that patients may experience more than one complication or reoperation during follow-up, we included multiple occurrences of any outcomes (device-related complications or reoperations) for the same patient, except for generator changes and death. Therefore, a patient can contribute more than once to the numerator when estimating the incidence rate of our primary outcomes. Although mortality was not one of our primary outcomes, we reported and plotted all-cause mortality because of the competing risk of death with ICD complications and the high risk of death in this population, many with conditions such as congestive heart failure that have high short- and mid-term mortality rates.
To assess the relationship between certification status and outcomes, we developed hierarchical proportional hazards models with time to the first ICD complication and reoperations separately as dependent variables with a censor indicator incorporating mortality as a competing risk.16,17 We included a robust sandwich variance estimator to account for correlation within providers. In the model, we included the following covariates for adjustment: demographics (age, gender, race, and insurance payor status); cardiac status (heart failure, New York Health Association class, history of cardiac arrest, atrial fibrillation/atrial flutter, ventricular tachycardia, nonischemic dilated cardiomyopathy, ischemic heart disease, previous myocardial infarction, and previous coronary revascularization); comorbid conditions (previous valvular surgery, cerebrovascular disease, chronic lung disease, diabetes mellitus, hypertension, and end-stage renal disease); facility volume and characteristics (profit status, census region, bed size, and teaching status); physician volume; and device type. All variables except left ventricular ejection fraction had <1% missing values. For categorical variables, missing data was assumed a no response, and for continuous variables, we used the median value of the entire cohort.
We repeated all of the above analyses with stratification by specific device type (single-chamber, dual-chamber, or CRT-D). Analyses were conducted using SAS software (version 9.4; SAS Institute Inc, Cary, NC). All analyses were conducted with a significance level of 0.05 and a 2-sided null hypothesis. The Yale University Human Investigations Committee approved analyses of this limited NCDR data set.
RESULTS
The study cohort included 107 966 implants performed by 3175 physicians (Figure 1). The majority of identified physicians were electrophysiologists (63.9%), followed by general cardiologists (20.5%), interventional cardiologists (9.6%), thoracic surgeons (2.5%), and other specialties (4.5%). Similarly, the majority of ICD implantations in our study were performed by electrophysiologists (69.0%) followed by general cardiologists (19.3%), interventional cardiologists (5.8%), other specialists (4.3%), and thoracic surgeons (1.7%).
Patient and Hospital Characteristics
The mean age of patients in our cohort was 75.1 years (SD: 6.3), 27.3% were female, and 88.5% were white. The demographic characteristics of patients differed depending on physician specialty, most notably with regards to age and race. There were statistically significant but clinically modest differences across physician specialties for patient clinical characteristics and cardiac status including history of diabetes mellitus, hypertension, end-stage renal disease, chronic lung disease, cerebrovascular disease, previous percutaneous coronary intervention, previous coronary artery bypass surgery, previous pacemaker insertion, congestive heart failure, New York Health Association class, prior cardiac arrest, history of atrial fibrillation or atrial flutter, and history of ventricular tachycardia. Furthermore, there were similarly modest differences in the QRS duration, LVEF, and blood urea nitrogen level. Across physician specialties, there were modest but significant differences across specialties in the proportion of ICDs placed for primary prevention of sudden cardiac death, and larger absolute differences in the ICD type placed such that electrophysiologists proportionally performed more CRT-D device implantations than other specialties (Table 1; Table III in the Data Supplement).
Table 1.
Baseline Patient Cohort Characteristics Stratified by Physician Specialty
| Description | Total | Physician Specialty | P Value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Electrophysiologist | Interventional Cardiologist | General Cardiologist | Thoracic Surgeon | Other Specialist | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| All | 107966 | 100 | 74 505 | 100 | 6219 | 100 | 20 795 | 100 | 1790 | 100 | 4657 | 100 | |
| Admission characteristics | 69.0 | 5.8 | 19.3 | 1.7 | 4.3 | ||||||||
| Age, mean (SD) | 75.1 | 6.3 | 75.03 | 6.2 | 74.98 | 6.4 | 75.11 | 6.3 | 75.94 | 6.5 | 75.12 | 6.2 | <0.001 |
| Female | 29 420 | 27.2 | 20 342 | 27.3 | 1658 | 26.7 | 5668 | 27.3 | 496 | 27.7 | 1256 | 27.0 | 0.814 |
| Race | |||||||||||||
| White | 95 587 | 88.5 | 65 902 | 88.5 | 5557 | 89.4 | 18 550 | 89.2 | 1615 | 90.2 | 3963 | 85.1 | <0.001 |
| Black | 8196 | 7.6 | 5864 | 7.9 | 382 | 6.1 | 1499 | 7.2 | 74 | 4.1 | 377 | 8.1 | |
| Other | 4183 | 3.9 | 2739 | 3.7 | 280 | 4.5 | 746 | 3.6 | 101 | 5.6 | 317 | 6.8 | |
| History and risk factors | |||||||||||||
| Family history sudden death | 3753 | 3.5 | 2655 | 3.6 | 150 | 2.4 | 685 | 3.3 | 56 | 3.1 | 207 | 4.4 | <0.001 |
| Congestive heart failure | 87 018 | 80.6 | 60 446 | 81.1 | 4919 | 79.1 | 16 584 | 79.7 | 1400 | 78.2 | 3669 | 78.8 | <0.001 |
| NYHA class—current status | <0.001 | ||||||||||||
| Class I | 10 685 | 9.9 | 7502 | 10.1 | 558 | 9.0 | 1988 | 9.6 | 188 | 10.5 | 449 | 9.6 | |
| Class II | 35 639 | 33.0 | 24 943 | 33.5 | 1899 | 30.5 | 6838 | 32.9 | 534 | 29.8 | 1425 | 30.6 | |
| Class III | 57 125 | 52.9 | 39 347 | 52.8 | 3381 | 54.4 | 10 921 | 52.5 | 908 | 50.7 | 2568 | 55.1 | |
| Class IV | 4517 | 4.2 | 2713 | 3.6 | 381 | 6.1 | 1048 | 5.0 | 160 | 8.9 | 215 | 4.6 | |
| Cardiac arrest | <0.001 | ||||||||||||
| No arrest | 99 580 | 92.2 | 68 579 | 92.0 | 5800 | 93.3 | 19 248 | 92.6 | 1658 | 92.6 | 4295 | 92.2 | |
| Brady arrest | 1100 | 1.0 | 739 | 1.0 | 72 | 1.2 | 217 | 1.0 | 25 | 1.4 | 47 | 1.0 | |
| Tachy arrest | 7286 | 6.7 | 5187 | 7.0 | 347 | 5.6 | 1330 | 6.4 | 107 | 6.0 | 315 | 6.8 | |
| Atrial fibrillation/atrial flutter | 42 788 | 39.6 | 29 732 | 39.9 | 2275 | 36.6 | 8154 | 39.2 | 728 | 40.7 | 1899 | 40.8 | <0.001 |
| Ventricular tachycardia | |||||||||||||
| No | 70 640 | 65.4 | 48 231 | 64.7 | 4421 | 71.1 | 13 992 | 67.3 | 1218 | 68.0 | 2778 | 59.7 | <0.001 |
| Yes-VT, nonsustained | 25 714 | 23.8 | 17 902 | 24.0 | 1319 | 21.2 | 4747 | 22.8 | 427 | 23.9 | 1319 | 28.3 | |
| Yes-monomorphic sustained VT | 9435 | 8.7 | 6800 | 9.1 | 398 | 6.4 | 1675 | 8.1 | 118 | 6.6 | 444 | 9.5 | |
| Yes-polymorphic sustained VT | 2177 | 2.0 | 1572 | 2.1 | 81 | 1.3 | 381 | 1.8 | 27 | 1.5 | 116 | 2.5 | |
| Ischemic heart disease | 77 700 | 72.0 | 53 311 | 71.6 | 4616 | 74.2 | 15 118 | 72.7 | 1308 | 73.1 | 3347 | 71.9 | <0.001 |
| Previous CABG | 44 346 | 41.1 | 30 377 | 40.8 | 2654 | 42.7 | 8619 | 41.4 | 777 | 43.4 | 1919 | 41.2 | 0.005 |
| Previous PCI | 37 543 | 34.8 | 25 501 | 34.2 | 2417 | 38.9 | 7317 | 35.2 | 586 | 32.7 | 1722 | 37.0 | <0.001 |
| Pacemaker insertion | 16 448 | 15.2 | 11 114 | 14.9 | 924 | 14.9 | 3326 | 16.0 | 351 | 19.6 | 733 | 15.7 | <0.001 |
| Cerebrovascular disease | 18 884 | 17.5 | 12 639 | 17.0 | 1174 | 18.9 | 3868 | 18.6 | 403 | 22.5 | 800 | 17.2 | <0.001 |
| Chronic lung disease | 26 711 | 24.7 | 17 890 | 24.0 | 1640 | 26.4 | 5362 | 25.8 | 538 | 30.1 | 1281 | 27.5 | <0.001 |
| Diabetes mellitus | 40 954 | 37.9 | 28 015 | 37.6 | 2443 | 39.3 | 7952 | 38.2 | 679 | 37.9 | 1865 | 40.0 | 0.001 |
| Hypertension | 86 173 | 79.8 | 59 167 | 79.4 | 5004 | 80.5 | 16 748 | 80.5 | 1456 | 81.3 | 3798 | 81.6 | <0.001 |
| Renal failure-dialysis | 4327 | 4.0 | 2944 | 4.0 | 259 | 4.2 | 806 | 3.9 | 91 | 5.1 | 227 | 4.9 | 0.002 |
| Diagnostics | |||||||||||||
| %EF, mean (SD) | 27.72 | 9.9 | 27.84 | 10.0 | 27.29 | 9.4 | 27.55 | 9.7 | 25.98 | 8.8 | 27.76 | 9.9 | <0.001 |
| QRS duration, mean (SD) | 131.64 | 34.5 | 132.00 | 34.5 | 129.83 | 34.0 | 130.96 | 34.4 | 131.32 | 35.8 | 131.45 | 34.9 | <0.001 |
| ICD procedure(s) | |||||||||||||
| ICD indication: primary prevention | 90 550 | 83.9 | 62 600 | 84.0 | 5242 | 84.3 | 17 390 | 83.6 | 1511 | 84.4 | 3807 | 81.7 | 0.001 |
| ICD type | |||||||||||||
| Missing | 151 | 0.1 | 112 | 0.2 | 8 | 0.1 | 24 | 0.1 | 1 | 0.1 | 6 | 0.1 | <0.001 |
| Single chamber | 19 135 | 17.7 | 13 034 | 17.5 | 1237 | 19.9 | 3925 | 18.9 | 286 | 16.0 | 653 | 14.0 | |
| Dual chamber | 41 118 | 38.1 | 27 602 | 37.0 | 2500 | 40.2 | 8206 | 39.5 | 817 | 45.6 | 1993 | 42.8 | |
| Biventricular | 47 562 | 44.1 | 33 757 | 45.3 | 2474 | 39.8 | 8640 | 41.5 | 686 | 38.3 | 2005 | 43.1 | |
CABG indicates coronary artery bypass graft; EF, ejection fraction; ICD, implantable cardioverter-defibrillator; NYHA, New York Health Association; PCI, percutaneous coronary intervention; and VT, ventricular tachycardia.
The characteristics of hospitals varied significantly across physician specialties. Electrophysiologists were less likely than nonelectrophysiologist cardiologists, thoracic surgeons, and other specialists to be implanting an ICD in private/community and rural hospitals. On the other hand, electrophysiologists were more likely to be implanting in hospitals with larger number of patient beds, classified as teaching hospitals, and with larger ICD volume (Table 2).
Table 2.
Facility Characteristics Stratified by Physician Specialty
| Description | Total | Physician Specialty | P Value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Electrophysiologist | Interventional Cardiologist | General Cardiologist | Thoracic Surgeon | Other Specialist | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| All | 107 966 | 100 | 74 505 | 100 | 6219 | 100 | 20 795 | 100 | 1790 | 100 | 4657 | 100 | |
| Profit type: private/community | 93 330 | 86.4 | 62 816 | 84.3 | 5854 | 94.1 | 19 158 | 92.1 | 1526 | 85.3 | 3976 | 85.4 | <0.001 |
| Census region: rural | 13 032 | 12.1 | 7017 | 9.4 | 1596 | 25.7 | 3484 | 16.8 | 354 | 19.8 | 581 | 12.5 | <0.001 |
| Patient beds >450 | 52 086 | 48.2 | 39 892 | 53.5 | 1451 | 23.3 | 8201 | 39.4 | 551 | 30.8 | 1991 | 42.8 | <0.001 |
| Teaching hospital | 59 725 | 55.3 | 44 443 | 59.7 | 2110 | 33.9 | 9976 | 48.0 | 742 | 41.5 | 2454 | 52.7 | <0.001 |
| Annual ICD volume >220 | 50 361 | 46.6 | 38 417 | 51.6 | 886 | 14.2 | 8477 | 40.8 | 525 | 29.3 | 2056 | 44.1 | <0.001 |
ICD indicates implantable cardioverter-defibrillator.
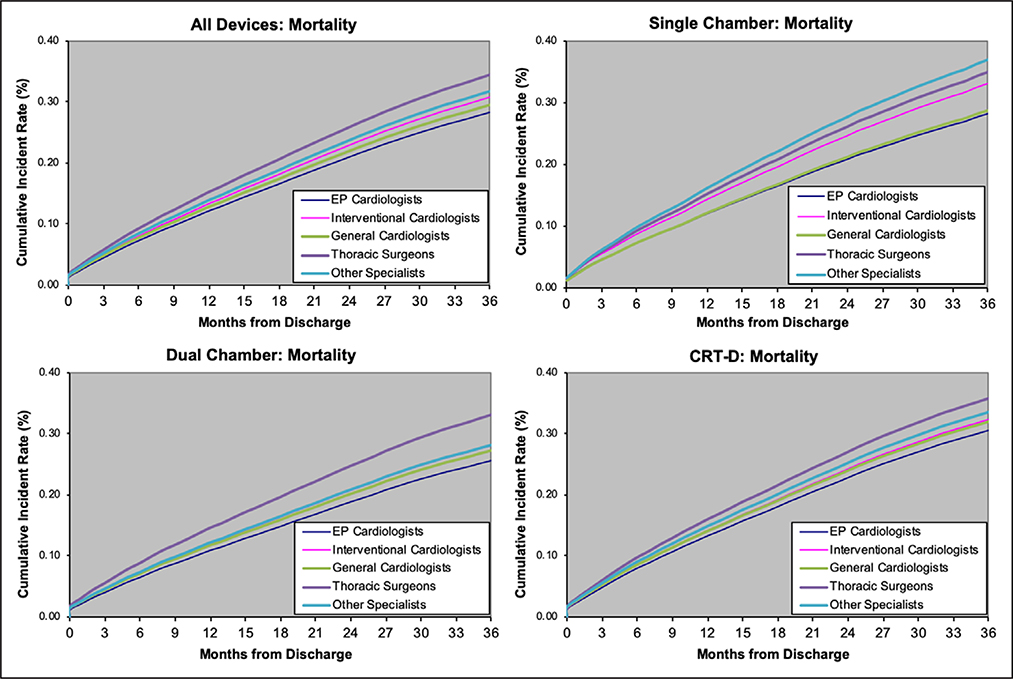
Mortality
Overall, 40 418 (37.4%) patients died in our study window. Mortality rates were lowest among electrophysiologists (36.8%) and highest among thoracic surgeons (43.3%) (Table 3). Electrophysiologists also had the lowest cumulative rate of mortality, and this trend was consistent across different ICD types including single-chamber, dual-chamber, and CRT-D (Figure 2). In multivariable analyses, the adjusted risk of death was significantly higher among patients whose implants had been performed by interventional cardiologists, general cardiologists, thoracic surgeons, and other specialties as compared to patients with implantations performed by electrophysiologists (Table 4).
Table 3.
Complications Stratified by Physician Specialty
| Description | Total | Physician Specialty | P Value | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Electrophysiologist | Interventional Cardiologist | General Cardiologist | Thoracic Surgeon | Other Specialist | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | ||
| All patients | |||||||||||||
| Any death | 40 418 | 37.4 | 27 409 | 36.8 | 2414 | 38.8 | 7945 | 38.2 | 775 | 43.3 | 1875 | 40.3 | <0.001 |
| Any complications | 15 685 | 14.5 | 10 536 | 14.1 | 950 | 15.3 | 3199 | 15.4 | 294 | 16.4 | 706 | 15.2 | <0.001 |
| Mechanical complications | 10 479 | 9.7 | 7024 | 9.4 | 653 | 10.5 | 2141 | 10.3 | 199 | 11.1 | 462 | 9.9 | <0.001 |
| Infection | 2360 | 2.2 | 1505 | 2.0 | 177 | 2.8 | 516 | 2.5 | 54 | 3.0 | 108 | 2.3 | <0.001 |
| Pocket-related complication | 2484 | 2.3 | 1691 | 2.3 | 147 | 2.4 | 479 | 2.3 | 43 | 2.4 | 124 | 2.7 | 0.002 |
| Other | 1955 | 1.8 | 1355 | 1.8 | 98 | 1.6 | 384 | 1.8 | 32 | 1.8 | 86 | 1.8 | 0.003 |
| Reoperation for reasons other than complications | 18 376 | 17.0 | 12 414 | 16.7 | 1058 | 17.0 | 3739 | 18.0 | 329 | 18.4 | 836 | 18.0 | <0.001 |
| ICD type: single chamber | |||||||||||||
| Any death | 7321 | 38.3 | 4881 | 37.4 | 517 | 41.8 | 1499 | 38.2 | 126 | 44.1 | 298 | 45.6 | <0.001 |
| Any complications | 2486 | 13.0 | 1621 | 12.4 | 172 | 13.9 | 545 | 13.9 | 41 | 14.3 | 107 | 16.4 | <0.001 |
| Mechanical complications | 1615 | 8.4 | 1046 | 8.0 | 112 | 9.1 | 372 | 9.5 | 24 | 8.4 | 61 | 9.3 | 0.001 |
| Infection | 329 | 1.7 | 197 | 1.5 | 33 | 2.7 | 76 | 1.9 | 8 | 2.8 | 15 | 2.3 | <0.001 |
| Pocket-related complication | 431 | 2.3 | 296 | 2.3 | 29 | 2.3 | 82 | 2.1 | 5 | 1.7 | 19 | 2.9 | 0.027 |
| Other | 342 | 1.8 | 226 | 1.7 | 16 | 1.3 | 72 | 1.8 | 8 | 2.8 | 20 | 3.1 | 0.002 |
| Reoperation for reasons other than complications | 2481 | 13.0 | 1653 | 12.7 | 168 | 13.6 | 533 | 13.6 | 38 | 13.3 | 89 | 13.6 | 0.019 |
| ICD type: dual chamber | |||||||||||||
| Any death | 14 181 | 34.5 | 9318 | 33.8 | 921 | 36.8 | 2881 | 35.1 | 344 | 42.1 | 717 | 36.0 | <0.001 |
| Any complications | 5540 | 13.5 | 3597 | 13.0 | 363 | 14.5 | 1184 | 14.4 | 124 | 15.2 | 272 | 13.6 | 0.003 |
| Mechanical complications | 3668 | 8.9 | 2382 | 8.6 | 243 | 9.7 | 775 | 9.4 | 83 | 10.2 | 185 | 9.3 | 0.018 |
| Infection | 782 | 1.9 | 482 | 1.7 | 60 | 2.4 | 179 | 2.2 | 21 | 2.6 | 40 | 2.0 | 0.004 |
| Pocket-related complication | 856 | 2.1 | 562 | 2.0 | 58 | 2.3 | 172 | 2.1 | 19 | 2.3 | 45 | 2.3 | 0.133 |
| Other | 744 | 1.8 | 499 | 1.8 | 46 | 1.8 | 158 | 1.9 | 13 | 1.6 | 28 | 1.4 | 0.089 |
| Reoperation for reasons other than complications | 6016 | 14.6 | 3934 | 14.3 | 388 | 15.5 | 1266 | 15.4 | 118 | 14.4 | 310 | 15.6 | 0.013 |
| ICD type: CRT-D | |||||||||||||
| Any death | 18 862 | 39.7 | 13 169 | 39.0 | 973 | 39.3 | 3556 | 41.2 | 305 | 44.5 | 859 | 42.8 | <0.001 |
| Any complications | 7638 | 16.1 | 5305 | 15.7 | 413 | 16.7 | 1465 | 17.0 | 129 | 18.8 | 326 | 16.3 | 0.004 |
| Mechanical complications | 5182 | 10.9 | 3588 | 10.6 | 296 | 12.0 | 991 | 11.5 | 92 | 13.4 | 215 | 10.7 | 0.003 |
| Infection | 1245 | 2.6 | 823 | 2.4 | 84 | 3.4 | 260 | 3.0 | 25 | 3.6 | 53 | 2.6 | <0.001 |
| Pocket-related complication | 1195 | 2.5 | 832 | 2.5 | 60 | 2.4 | 225 | 2.6 | 19 | 2.8 | 59 | 2.9 | 0.075 |
| Other | 867 | 1.8 | 629 | 1.9 | 36 | 1.5 | 153 | 1.8 | 11 | 1.6 | 38 | 1.9 | 0.056 |
| Reoperation for reasons other than complications | 9848 | 20.7 | 6804 | 20.2 | 501 | 20.3 | 1934 | 22.4 | 173 | 25.2 | 436 | 21.7 | <0.001 |
CRT-D indicates cardiac resynchronization therapy-defibrillator; and ICD, implantable cardioverter-defibrillator.
Figure 2. Cumulative incidence curves by physician specialties of mortality rates.
CRT-D indicates cardiac resynchronization therapy-defibrillator; and EP, electrophysiology.
Table 4.
Adjusted Cox Regression Model of Complication and Reoperation Rates by Physician Specialties*
| Description | Interventional Cardiologist | General Cardiologist | Thoracic Surgeon | Other Specialist | ||||
|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | |
| All patients | ||||||||
| Mortality | 1.09 (1.03–1.15) | 0.002 | 1.05 (1.01–1.09) | 0.007 | 1.16 (1.05–1.28) | 0.003 | 1.15 (1.09–1.21) | <0.001 |
| Any complication | 1.16 (1.07–1.26) | <0.001 | 1.13 (1.07–1.19) | <0.001 | 1.20 (1.04–1.39) | 0.01 | 1.08 (0.97–1.19) | 0.16 |
| Reoperation | 1.10 (0.99–1.23) | 0.07 | 1.10 (1.05–1.15) | 0.003 | 1.16 (1.00–1.34) | 0.05 | 1.10 (0.98–1.24) | 0.10 |
| ICD type: single chamber | ||||||||
| Mortality | 1.19 (1.06–1.32) | 0.002 | 1.03 (0.95–1.11) | 0.46 | 1.22 (0.98–1.53) | 0.07 | 1.34 (1.18–1.53) | <0.001 |
| Any complication | 1.26 (1.06–1.50) | 0.009 | 1.19 (1.07–1.33) | 0.002 | 1.26 (0.88–1.81) | 0.20 | 1.34 (1.08–1.67) | 0.008 |
| Reoperation | 1.15 (0.92–1.44) | 0.23 | 1.10 (0.97–1.25) | 0.13 | 1.17 (0.77–1.77) | 0.46 | 1.04 (0.80–1.35) | 0.78 |
| ICD type: dual chamber | ||||||||
| Mortality | 1.04 (0.96–1.13) | 0.37 | 1.05 (0.99–1.10) | 0.09 | 1.17 (1.02–1.34) | 0.02 | 1.13 (1.04–1.22) | 0.005 |
| Any complication | 1.19 (1.05–1.35) | 0.007 | 1.14 (1.05–1.24) | 0.002 | 1.20 (0.99–1.46) | 0.06 | 1.06 (0.92–1.21) | 0.42 |
| Reoperations | 1.13 (0.98–1.31) | 0.09 | 1.07 (0.99–1.16) | 0.12 | 0.97 (9.78–1.20) | 0.78 | 1.09 (0.94–1.26) | 0.24 |
| ICD type: CRT-D | ||||||||
| Mortality | 1.07 (0.98–1.17) | 0.11 | 1.06 (1.00–1.12) | 0.26 | 1.11 (0.97–1.28) | 0.11 | 1.11 (1.00–1.24) | 0.05 |
| Any complication | 1.11 (0.98–1.26) | 0.10 | 1.10 (1.01–1.18) | 0.015 | 1.17 (0.98–1.42) | 0.85 | 1.03 (0.89–1.18) | 0.73 |
| Reoperations | 1.05 (0.90–1.21) | 0.56 | 1.12 (1.02–1.24) | 0.016 | 1.34 (1.11–1.62) | 0.002 | 1.12 (0.95–1.31) | 0.17 |
Reference: electrophysiologist. CRT-D indicates cardiac resynchronization therapy-defibrillator; HR, hazard ratio; and ICD, implantable cardioverter-defibrillator.
Model adjustment: (1) demographics (age, gender, race, and payor status); (2) clinical comorbidities (congestive heart failure, New York Heart Association Class—current status, cardiac arrest, atrial fibrillation/atrial flutter, ventricular tachycardia, nonischemic dilated cardiomyopathy, ischemic heart disease, previous myocardial infarction, previous revascularization, previous valvular surgery, cerebrovascular disease, chronic lung disease, diabetes mellitus, hypertension, and renal failure-dialysis); (3) left ventricular ejection fraction, QRS duration, blood urea nitrogen, ICD type; (4) facility characteristics (profit status, census region, bed size, and teaching status); and (5) physician volume. Model accounts for competing risk of death.
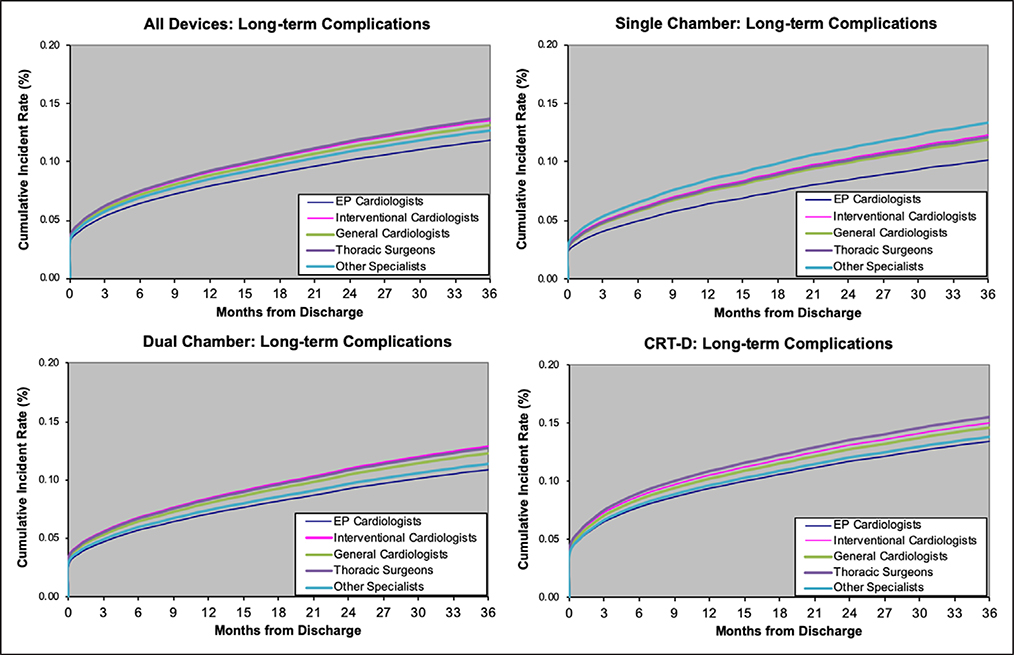
ICD-Related Complications
There were significant differences in the crude rates of ICD-related complications across physician specialties. Electrophysiologists had the lowest rates of complications at 14.1%, whereas thoracic surgeons had the highest rates at 16.4%. Complication rates varied significantly according to the type of ICD device ranging from 13.0% for single-chamber to 16.1% in CRT-D devices. Device-related mechanical complications and infection rates were consistently lowest among electrophysiologists. For most of the other individual complications, there were statistically significant but clinically modest differences across physician specialties (Table 3). Electrophysiologists had the lowest cumulative rate of complications both overall and when stratified by specific device type (Figure 3). In multivariable analyses, compared with electrophysiologists, the adjusted risk of any complication was higher in interventional cardiologists, general cardiologists, thoracic surgeons, and other specialists. After stratification for ICD device type, for several subgroups (other specialists implanting dual chamber and CRT-D devices; and thoracic surgeons implanting single-chamber and CRT-D devices) the 95% CI crossed the line of unity (Table 4).
Figure 3. Cumulative incidence curves by physician specialties of long-term complication rates.
CRT-D indicates cardiac resynchronization therapy-defibrillator; and EP, electrophysiology.
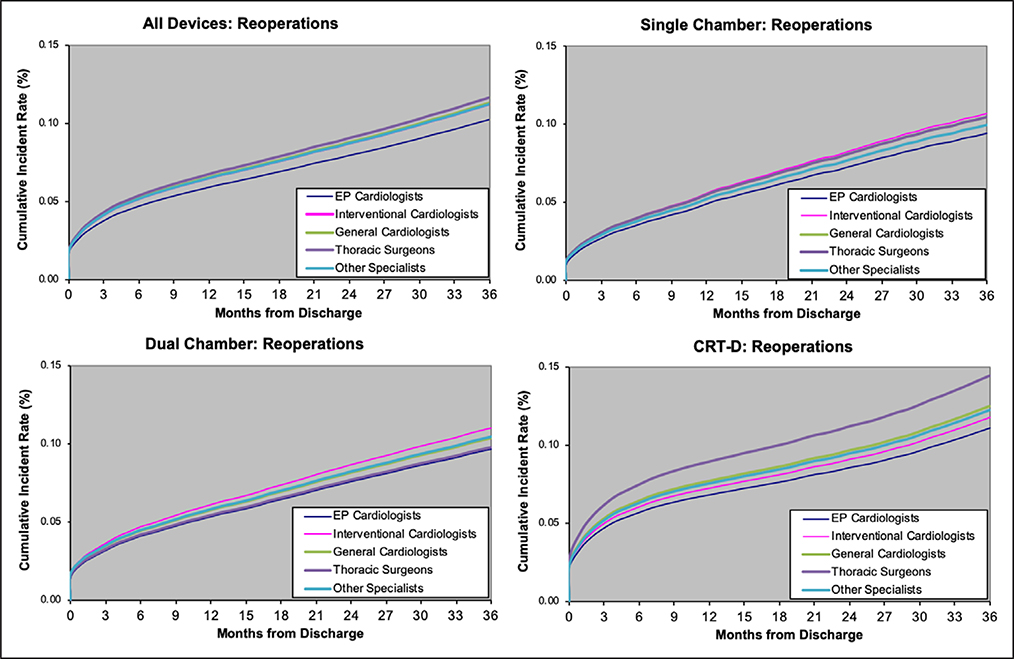
Reoperations for Reasons Other Than Complications
Over the follow-up period, 17.0% of patients had a reoperation for reasons other than complications. In analyses stratified by ICD device type, electrophysiologists consistently had the lowest rates and cumulative incidence of reoperations (Figure 4). In adjusted analysis, compared to electrophysiologists, general cardiologists and thoracic surgeons had significantly higher adjusted risks of reoperation for reasons other than complications. When stratified by device type, there were no statistical differences in the reoperation rates for single-chamber and dual-chamber devices across specialties. General cardiologists and thoracic surgeons were associated with higher risk of reoperations for CRT-D devices. Across all 3 device types, electrophysiologists were associated with the lowest risk of reoperation rates (Table 4).
Figure 4. Cumulative incidence curves by physician specialties of reoperation for reasons other than complication rates.
CRT-D indicates cardiac resynchronization therapy-defibrillator; and EP, electrophysiology.
DISCUSSION
In this nationwide study of patients undergoing ICD implantations, we found that rates of long-term complications and reoperations for reasons other than complications varied by the specialty and training of the implanting physician. Our findings demonstrate that patients with ICD implantations performed by nonelectrophysiologists had higher rates of long-term complications and rehospitalizations for reasons other than complications. Given that nearly a third of implantations were done by physicians without electrophysiology training, our findings suggest that a focus on appropriate training for those implanting ICDs may represent an opportunity to minimize long-term risks of ICD implantations.
One of the explicit goals of the NCDR ICD registry was to inform our understanding of the association of physician subspecialty training and ICD outcomes.11,12 Our results build on prior work demonstrating that in-hospital outcomes varied depending on the training of the implanting physician.6 While in both studies, patients with implantations performed by electrophysiologists had the lowest complication rates, we found that the differences across physician specialties become even more prominent over longer follow-up. The larger absolute differences in our study further emphasize the potential benefits of subspecialty training, as long-term ICD complications are not benign and carry a significant risk of morbidity and mortality.7,18
These data cannot determine the underlying reasons for observed differences in long-term complication rates among specialties. Different subspecialty training may reflect differences in experience, clinical knowledge, and technical skill. Prior work has also shown that a sizable minority of ICD implantations performed are not evidence-based and that patients with nonevidence-based ICD implantations had significantly worse outcomes.19 Importantly, nonelectrophysiologist cardiologists, thoracic surgeons, and other specialties were more likely to place a non-evidence-based ICD. Another possible mechanism is the known increased use of remote patient monitoring among electrophysiologists, which has been associated with improved outcomes and mortality.20 Nevertheless, elucidating potential mechanisms for discrepancies among physician specialties for complications and reoperations for reasons other than complications may provide an opportunity for improved outcomes of patients with ICD implantations.
Our finding of increased reoperations in patients with ICD implantations performed by nonelectrophysiologist physicians, particularly in CRT-D devices, is of importance for several reasons. Improving battery service life of ICDs can also result in reduced morbidity and mortality for patients, as generator changes are not benign and carry associated risks including pocket infection, pocket hematoma, and death.8,21,22 Electrophysiologists may have more experience in tailoring ICD programming beyond out of the box settings and adapting to patient-specific and device-specific characteristics, leading to improved generator battery life. In addition to battery generator changes, difference in rates of potentially preventable device upgrades may contribute to variations in rate reoperations for reasons other than complications across physician specialties. Previous studies have shown that nonelectrophysiologists are less likely to implant CRT-D devices in patients with appropriate indications.6 Although speculative, our observed differences in rates of device upgrades may be driven by patients that would benefit from CRT-D devices receiving a single-chamber or dual-chamber device and thus requiring a potentially avoidable upgrade procedure in the future.
Although our analyses highlight the significant association of physician specialty with long-term complications in patients receiving ICD implantations, the overall differences were clinically modest. Furthermore, there is likely heterogeneity within physician training groups such that there are nonelectrophysiologist implanters who achieve excellent outcomes and electrophysiologist implanters with below-average results. Nevertheless, our findings provide information relevant to patients when they have a choice of implanting physician, especially as Medicare recently mandated shared decision-making with the patient before ICD implantation.12
Limitations
Our study should be interpreted in the context of several limitations. Our study included only Medicare beneficiaries aged 65 years or older. Although younger patients may have higher overall nonfatal outcome because of lower competing risk of death, the effect on rates of complications and rehospitalizations for reasons other than complications should be comparable across physician specialties. We also used Medicare claims data to identify long-term complications. Administrative claims data lack the clinical complexity as compared to information extracted from chart review. However, Medicare data is the only available nationwide source of data with information of longitudinal outcomes on a large cohort of patients. Furthermore, we were not able to distinguish between appropriate versus inappropriate device upgrades or premature versus normal battery generator changes. Moreover, residual confounding is a limitation of observational studies and may explain some of the observed differences in long-term ICD outcomes across physician specialties. While our models adjusted for a robust number of clinical and demographic variables validated within NCDR, there are additional clinical characteristics of our cohort, we could not capture including the severity and duration of our clinical covariates. Last, our observational study cannot establish a cause and effect relationship between physician specialties and long-term ICD device mortality or complication rates.
Conclusions
In summary, we found that patients with ICD implantations performed by nonelectrophysiologist clinicians were at increased risk of long-term complications and reoperations for reasons other than complications. Our findings emphasize the value of subspecialty training for ICD implantation and suggest that consideration of physician specialty before ICD implantation may minimize long-term complications and reoperations.
Supplementary Material
WHAT IS KNOWN
Recent studies have shown that there are high rates of long-term device-related complications and reoperations after implantable cardioverter-defibrillator (ICD) implantations.
In-hospital procedural complication rates are known to vary by physician specialties.
However, it is not known if physician training is associated with differences in long-term outcomes following ICD implantation.
WHAT THE STUDY ADDS
There are observed differences in long-term ICD outcomes across physician specialties.
ICD implantations by electrophysiologists had the lowest risk of having long-term device-related ICD complications and reoperations.
Acknowledgments
The National Cardiovascular Data Registry (NCDR) Implantable Cardioverter-Defibrillator Registry is an initiative of the American College of Cardiology Foundation with partnering support from the Heart Rhythm Society. The views expressed in this article are those of the authors and do not necessarily represent the official views of the NCDR or its associated professional societies (identified at https://cvquality.acc.org/NCDR). The authors thank Gloria Ho for her assistance in manually abstracting physician certifications from online databases.
Sources of Funding
This analysis was funded by the American College of Cardiology Foundations’ National Cardiovascular Data Registry.
Disclosures
Dr Chui receives salary support from the VA Health Services Research and Development (IIR 12-118 and CIN 13-407). Dr Ranasinghe is supported by a National Heart Foundation of Australia Future Leader Fellowship (ID 101186). Dr Lampert receives research grants (significant) from Medtronic and St Jude/Abbott and modest advisory board compensation/honoraria from Medtronic. Dr Curtis has a contract with the American College of Cardiology for his role as Senior Medical Officer, National Cardiovascular Data Registry (NCDR); receives salary support from the American College of Cardiology, NCDR; receives funding from the Centers for Medicare & Medicaid Services to develop and maintain performance measures that are used for public reporting; and holds equity interest in Medtronic. The other authors report no conflicts.
Footnotes
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCOUTCOMES.118.005374.
Contributor Information
Philip W. Chui, Section of Internal Medicine, VA Connecticut Healthcare System, West Haven; Department of Internal Medicine, Yale University School of Medicine, New Haven, CT.
Yongfei Wang, Center for Outcomes Research and Evaluation, Yale New Haven Hospital, CT; Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, CT.
Isuru Ranasinghe, Discipline of Medicine, University of Adelaide, South Australia, Australia.
Teferi Y. Mitiku, Department of Cardiology, UC Irvine School of Medicine, Orange, CA.
Arnold H. Seto, Department of Cardiology, UC Irvine School of Medicine, Orange, CA; Department of Medicine, VA Long Beach Health Care System, CA.
Lindsey Rosman, Section of Internal Medicine, VA Connecticut Healthcare System, West Haven; Department of Internal Medicine, Yale University School of Medicine, New Haven, CT.
Rachel Lampert, Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, CT.
Karl E. Minges, Center for Outcomes Research and Evaluation, Yale New Haven Hospital, CT.
Alan D. Enriquez, Section of Internal Medicine, VA Connecticut Healthcare System, West Haven; Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, CT.
Jeptha P. Curtis, Center for Outcomes Research and Evaluation, Yale New Haven Hospital, CT; Section of Cardiovascular Medicine, Department of Internal Medicine, Yale University School of Medicine, New Haven, CT.
REFERENCES
- 1.Kuck KH, Cappato R, Siebels J, Rüppel R. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: the Cardiac Arrest Study Hamburg (CASH). Circulation. 2000;102:748–754. [DOI] [PubMed] [Google Scholar]
- 2.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML; Multicenter Automatic Defibrillator Implantation Trial II Investigators. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474 [DOI] [PubMed] [Google Scholar]
- 3.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399 [DOI] [PubMed] [Google Scholar]
- 4.Connolly SJ, Gent M, Roberts RS, Dorian P, Roy D, Sheldon RS, Mitchell LB, Green MS, Klein GJ, O’Brien B. Canadian implantable defibrillator study (CIDS): a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation. 2000;101:1297–1302. [DOI] [PubMed] [Google Scholar]
- 5.Bradley DJ, Bradley EA, Baughman KL, Berger RD, Calkins H, Goodman SN, Kass DA, Powe NR. Cardiac resynchronization and death from progressive heart failure: a meta-analysis of randomized controlled trials. JAMA. 2003;289:730–740. [DOI] [PubMed] [Google Scholar]
- 6.Curtis JP, Luebbert JJ, Wang Y, Rathore SS, Chen J, Heidenreich PA, Hammill SC, Lampert RI, Krumholz HM. Association of physician certification and outcomes among patients receiving an implantable cardioverter-defibrillator. JAMA. 2009;301:1661–1670. doi: 10.1001/jama.2009.547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ranasinghe I, Parzynski CS, Freeman JV, Dreyer RP, Ross JS, Akar JG, Krumholz HM, Curtis JP. Long-term risk for device-related complications and reoperations after implantable cardioverter-defibrillator implantation: an observational cohort study. Ann Intern Med. 2016;165:20–29. [DOI] [PubMed] [Google Scholar]
- 8.Poole JE, Gleva MJ, Mela T, Chung MK, Uslan DZ, Borge R, Gottipaty V, Shinn T, Dan D, Feldman LA, Seide H, Winston SA, Gallagher JJ, Langberg JJ, Mitchell K, Holcomb R; REPLACE Registry Investigators. Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation. 2010;122:1553–1561. doi: 10.1161/CIRCULATIONAHA.110.976076 [DOI] [PubMed] [Google Scholar]
- 9.Kramer DB, Kennedy KF, Spertus JA, Normand SL, Noseworthy PA, Buxton AE, Josephson ME, Zimetbaum PJ, Mitchell SL, Reynolds MR. Mortality risk following replacement implantable cardioverter-defibrillator implantation at end of battery life: results from the NCDR. Heart Rhythm. 2014;11:216–221. doi: 10.1016/j.hrthm.2013.10.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kremers MS, Hammill SC, Kadish AH, Kadish AH, Stevenson LW, Heidenreich PA, Lindsay BD, Mirro MJ, Radford MJ, McKay C, Wang Y, Lang CM, Pontzer K, Rumsfeld J, Phurrough SE, Curtis JP, Brindis RG. Review of the ICD Registry’s third year, expansion to include lead data and pediatric ICD procedures, and role for measuring performance. Heart Rhythm. 2009;6:1394–1401. [DOI] [PubMed] [Google Scholar]
- 11.Hammill S, Phurrough S, Brindis R. The National ICD Registry: now and into the future. Heart Rhythm. 2006;3:470–473. doi: 10.1016/j.hrthm.2006.01.019 [DOI] [PubMed] [Google Scholar]
- 12.Center for Medicare and Medicaid Services. Decision Memo for Implantable Defibrillators (CAG-00157R3). https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=148. Accessed April 21, 2018.
- 13.Freeman JV, Wang Y, Curtis JP, Heidenreich PA, Hlatky MA. Physician procedure volume and complications of cardioverter-defibrillator implantation. Circulation. 2012;125:57–64. doi: 10.1161/CIRCULATIONAHA.111.046995 [DOI] [PubMed] [Google Scholar]
- 14.Certification Matters. American Board of Medical Specialties. 2018. http://www.certificationmatters.org/?utm_source=www.abms.org-verify-certification. Accessed April 19, 2018.
- 15.American Board of Internal Medicine. Check a Physician’s Certification. http://www.abim.org/verify-physician.aspx. Accessed April 19, 2018.
- 16.So Y, Lin G, Johnston G. Using the PHREG procedure to analyze competing-risks data. Paper Presented at: the SAS Global Forum; March 23–26, 2014; Washington, DC http://support.sas.com/rnd/app/stat/papers/2014/competingrisk2014.pdf. Accessed March 11, 2019. [Google Scholar]
- 17.Guo C, So Y. Cause-specific analysis of competing risks using the PHREG procedure. Paper Presented at: the SAS Global Forum; April 8–11, 2018; Denver CO. https://www.sas.com/content/dam/SAS/support/en/sas-global-forum-proceedings/2018/2159-2018.pdf. Accessed March 11, 2019. [Google Scholar]
- 18.Hawkins NM, Grubisic M, Andrade JG, Huang F, Ding L, Gao M, Bashir J. Long-term complications, reoperations and survival following cardioverter-defibrillator implant. Heart. 2018;104:237–243. doi: 10.1136/heartjnl-2017-311638 [DOI] [PubMed] [Google Scholar]
- 19.Al-Khatib SM, Hellkamp A, Curtis J, Mark D, Peterson E, Sanders GD, Heidenreich PA, Hernandez AF, Curtis LH, Hammill S. Non-evidence based ICD implantations in the United States. Results from the NCDR-ICD registry. JAMA. 2011;305:43–49. doi: 10.1001/jama.2010.1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akar JG, Bao H, Jones P, Wang Y, Chaudhry SI, Varosy P, Masoudi FA, Stein K, Saxon LA, Curtis JP. Use of remote monitoring of newly implanted cardioverter-defibrillators: insights from the patient related determinants of ICD remote monitoring (PREDICT RM) study. Circulation. 2013;128:2372–2383. doi: 10.1161/CIRCULATIONAHA.113.002481 [DOI] [PubMed] [Google Scholar]
- 21.Gould PA, Gula LJ, Champagne J, Healey JS, Cameron D, Simpson C, Thibault B, Pinter A, Tung S, Sterns L, Birnie D, Exner D, Parkash R, Skanes AC, Yee R, Klein GJ, Krahn AD. Outcome of advisory implantable cardioverter-defibrillator replacement: one-year follow-up. Heart Rhythm. 2008;5:1675–1681. doi: 10.1016/j.hrthm.2008.09.020 [DOI] [PubMed] [Google Scholar]
- 22.Kapa S, Hyberger L, Rea RF, Hayes DL. Complication risk with pulse generator change: implications when reacting to a device advisory or recall. Pacing Clin Electrophysiol. 2007;30:730–733. doi: 10.1111/j.1540-8159.2007.00742.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.