Abstract
Oesophageal cancer (OC) is an aggressive neoplasm that manifests in the gastrointestinal tract and is the result of numerous factors that can contribute to the development of the disease. These may include old age, nutritional deficiencies, oesophageal obstruction and food ingestion difficulties. Environmental factors serve a large role in increasing the risk of developing OC. Two factors that serve an increasing risk of developing OC are the use of tobacco and the consumption of alcohol. Genetic factors also exhibit a large effect on the risk of developing OC, for example, the causative genes in Black Africans differ from other races. OC is 3–4 times more common among men than women. OC has been previously reported in >450 000 individuals worldwide, and its incidence is increasing. The current review compares OC in low to middle-income countries with developed countries. The incidence of OC, particularly squamous cell carcinoma (SCC) is high in low and middle-income countries. In developed countries, the incidence of SCC is low compared with adenocarcinoma. The majority of OC cases are diagnosed in the late stages of the disease, leading to high mortality rates. The current review aimed to discuss factors that contribute to the development of this disease in different geographical areas and genetic mechanisms governing these findings. The current review also aims to discuss the preventative treatment options for the disease, and also discusses the diagnosis and surveillance in five LMICs, including South Africa, China, Tanzania, India and Brazil.
Keywords: esophageal cancer, squamous cell carcinoma, adenocarcinoma, Barrett's esophagus, low to middle income countries, South Africa, Tanzania, China, India, Brazil
1. Introduction
Oesophageal cancer (OC) is an aggressive neoplasm with its effect manifested in the gastrointestinal tract as a result of late diagnosis, old age and nutritional abnormalities which results from oesophageal obstruction and impossibility of proper food ingestion (1). The disease is more frequent in old age male individuals (2,3). Oesophageal cancer is usually 3 to 4 times more common among men than women (1,4). Oesophageal cancer is a disease that is reported in more than 450,000 individuals worldwide and its incidence is increasing. Squamous cell carcinoma (SCC) is the histological type that is predominant as compared to adenocarcinoma (AC) form. However, in well-developed countries a shift is observed where adenocarcinoma (AC) is predominant. This includes countries such as Australia, United Kingdom, United States of America and some Western European countries such as Finland, France and the Netherlands. The five-year survival of oesophageal patients ranges from 15 to 25% (5–7). Greater than 490,000 new cases of OC were reported in 2005 and the prevalence of oesophageal cancer (OC) is expected to increase by 14% while other types of cancers incidence are expected to decrease by 2025 (8,9). Oesophageal cancer (OC) accounted for >400 000 mortalities worldwide in 2000 (8), OC is considered as the eighth most common cancer and the sixth highest cause of cancer related mortalities worldwide with developing countries accounting >80% of total cases and deaths (8,10). Various risk factors are reported to be involved in the genesis of oesophageal tumours. The highest OC risk areas are found in Eastern Asia and Eastern and Southern Africa, Brazil, India and Kenya. The lowest OC risk areas are found in Western Africa (4). The aims of the current review are to compare oesophageal cancer in low to middle income countries, as an example, China, Brazil, India and South Africa to developed countries. According to the National Cancer Institute in the United States, approximately 17,990 new cases of OC cases were reported and 15,210 deaths occurred due to OC in 2013 (9). The five-year survival rate for all oesophageal cancers in the United States of America is 43% in those individuals where the cancer has not spread. This drops to between 4 and 23% if the cancer spreads to different parts of the body.
The current review also focusses on the oesophageal cancer burden; risk factors, molecular epidemiology; genetic factors; diagnosis; prevention and treatment challenges of the disease in low and middle countries such as South Africa, China, India, Brazil and Tanzania compared to developed countries such as the United States.
In developing countries oesophageal cancer makes up approximately 80% of total cases and deaths (11,12). Oesophageal cancer histological type and its incidence differs depending on geographic locations. The incidence is directly proportional to the related risk factors and economic development in variable countries. This variation in incidence is assumed to be based on usage or consumption of tobacco and alcohol as contributing risk factors (12). Table I (4,13) shows the estimated new oesophageal cancer cases and deaths worldwide by sex. This data indicates that males are more affected than females in both well-developed and developing countries. The relative risk factors for developing oesophageal cancer depend on geographic locations as well as variations in histological types (Table II) (11,13).
Table I.
Estimated new oesophageal cancer cases and deaths worldwide (Torre, 2016 #264).
| Variable | Estimated new cases | Estimated deaths |
|---|---|---|
| Worldwide | ||
| Male | 323,000 | 281,200 |
| Female | – | 119,000 |
| Developed countries | ||
| Male | – | 56,100 |
| Female | – | – |
| Developing countries | ||
| Male | 255,300 | 255,100 |
| Female | 114,400 | 103,700 |
-, no data.
Table II.
Relative risk factors for oesophageal cancer (13).
| Risk factor | Squamous cell carcinoma | Adenocarcinoma |
|---|---|---|
| First or second hand smoke | +++ | + |
| Alcohol consumption | +++ | – |
| Red meat consumption | + | + |
| Barrett's oesophagus | – | ++++ |
| Reflux symptoms | – | +++ |
| Overweight | – | ++ |
| Poverty | ++ | – |
| Caustic injury to the oesophagus | ++++ | – |
| History of head and neck cancer | ++++ | – |
| History of radiotherapy | +++ | +++ |
| Frequent consumption of hot drinks | + | – |
-, no effect; +, suspicious effect; ++, positive effect; +++ and ++++, strong positive effect.
2. Methods
Literature searches were performed in PubMed using the following search terms; oesophageal cancer epidemiology; adenocarcinoma epidemiology; squamous cell carcinoma epidemiology; esophageal cancer incidence rate developed countries; esophageal cancer incidence rate low and muddle income countries, oesophageal cancer mortality developed countries, oesophageal cancer mortality low and muddle income countries, oesophageal cancer Biomarkers and oesophageal cancer treatment. In order to obtain country specific data the search term oesophageal cancer and the countries or geographical area name were used (USA, Europe, Asia, Africa's oesophageal cancer corridor, Brazil, China, India, South Africa and Tanzania). In addition to this the following search terms were used; oesophageal cancer geographic distribution, oesophageal cancer ethnicity, oesophageal cancer socioeconomic distribution, oesophageal cancer international trends. The name of the country was used in combination with the search term oesophageal cancer environmental risk factors, to obtain references for the risk factors for the population of these countries. Information on the genetic factors contributing to oesophageal cancer in each country was obtained by combining the country name and the following search terms; oesophageal cancer Genome-wide association study, oesophageal cancer non-coding mRNA and oesophageal cancer Genetic polymorphisms. Cancer statistics for oesophageal cancer were obtained from publications by the Surveillance, Epidemiology, and End Results (SEER) program and the World Health Organization) WHO). Data was also obtained from the GLOBOCAN database International Association of Cancer Registries (IACR). The ethnicity terms used are taken from the data sources that were searched and referenced.
3. Oesophageal cancer risk factors
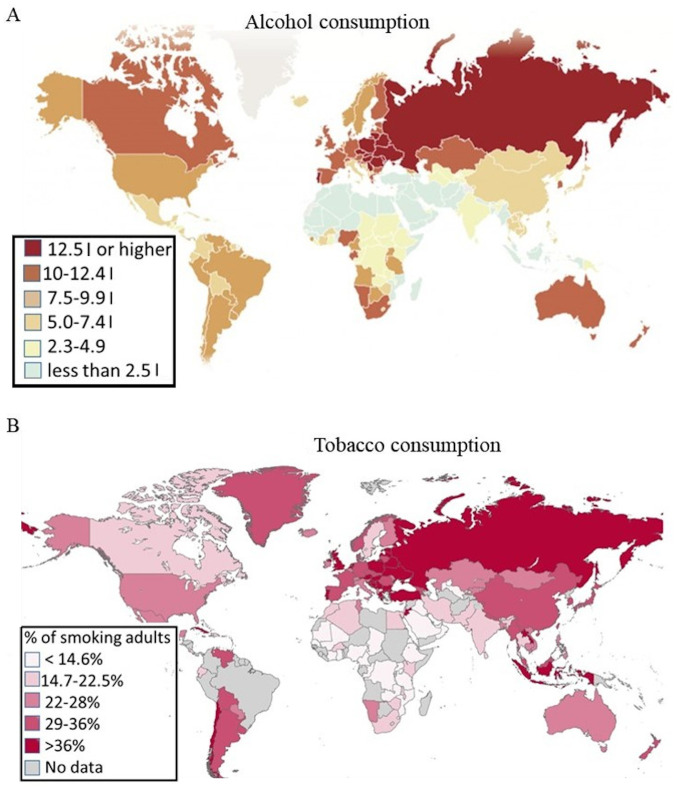
The risk of developing oesophageal cancer increases with age with squamous cell carcinoma (SCC) occurring equally in the middle or lower oesophagus. The highest risk of oesophageal cancer has been indicated in individuals with ages that ranges between 45 and 70. According to Daly et al (2000) oesophageal cancer incidence is three times higher in black Africans as compared to their white counterparts (14) while Das et al (2015) indicated that the chance of black Africans developing OC is thought to be twice that for white individuals (5). There are major risk factors that have played an important role in these two subtypes of oesophageal cancer, depending on the area where the oesophageal cancer subtype occurred (14). As previously stated, two of the greatest risk factors are alcohol consumption and tobacco use (Fig. 1) (15,16). Alcohol consumption is reported as the primary risk factor while alcohol consumption and tobacco use together have a synergistic effect and may increase the relative risk (9). Table II presents risk factors for oesophageal cancer and the histological type that each relative risk factor affects. One of the main reasons for males having a higher incidence of oesophageal cancer is that males have higher rates of alcohol and tobacco use (17). Smoking is an important risk factor for both AC and SCC while alcohol is a significant factor for SCC (18). Alcohol and tobacco use in combination leads to a substantial increase in the risk of oesophageal cancer. Users of both tobacco and alcohol have a relative risk of 35.4 in white males and 149.2 in African males as compared to the men of the same race and areas who neither smoke nor consume alcohol (19). The mechanism behind this increased risk by dual alcohol and tobacco use is because alcohol decreases or reduces metabolic activity within the cell, resulting in a reduction in the activity of detoxification enzymes, while promoting oxidation. This results in increased damage to DNA and increased sensitivity to other environmental toxins (20). Tobacco carcinogens penetrate the oesophageal epithelium (21). Carcinogens in tobacco include aromatic amines, nitrosamines, polycyclic aromatic hydrocarbons, aldehydes and phenols (21,22). Another risk factor for adenocarcinoma (AC) is obesity. This occurs in individuals with a predominately abdominal centered fat distribution. Hypertrophied adipocytes and inflammatory cells within fat deposits cause a low grade inflammation environment and promote tumour development through the release of adipokines and cytokines (23). In the tumour microenvironment, adipocytes supply energy production and support tumour growth and progression (24). Obesity is associated with an increased risk for adenocarcinoma (18), which may explain the increase in AC relative risk reportedly affecting individuals in developed countries like the United States and the United Kingdom, where alcohol and tobacco use is relatively lower than in developing countries. It has also been found that poor socio-economic status in low and middle developed countries results in a lower intake of fruits and vegetables. Fruits, vegetables and fish have been reported to play a major role in reducing the risk of development of oesophageal cancer (25). Regular, repeated consumption of hot beverages may cause chronic esophagitis and is strongly associated with a high risk of oesophageal cancer (26). Raw food contaminated by N-necrosis-compounds are also suspected risk factors for the development of oesophageal cancer. Foods rich in these compounds include salted tea, which has a high methylation activity, leading to the endogenous formation of nitrosamines (27–29).
Figure 1.
Alcohol and Tobacco consumption worldwide. (A) Alcohol consumption in liters of pure ethanol per person and (B) tobacco usage in percentage of adults smoking (28,29).
4. Epidemiology of oesophageal cancer
Oesophageal cancer has two histological subtypes: Squamous cell carcinomas (SCC) and adenocarcinomas (AC). SCC develops mostly in flat cell linings whereas AC arises from cells located in the lower third of the oesophagus and originate predominantly from Barrett mucosa (30). SCC and Barrett's develop from high-grade dysplastic pre-cancerous tissue. AC develops from the progression of Barrett's oesophagus from metaplastic to dysplastic tissue and invasive carcinoma (31). SCC incidence rates are high in countries that fall into two geographical regions. One region is named the ‘Asian oesophageal cancer belt’ and stretches from northern China to the Middle East (32). Another area is known as the East Africa oesophageal cancer corridor and stretches from South Africa to Somalia. This indicates that oesophageal cancer incidence and its histological type differs depending on risks factors on those particular geographic areas (9,18).
5. Oesophageal cancer in low to middle countries compared to developed countries
Low socioeconomic conditions are associated with higher incidence and mortality of oesophageal cancer in specific areas around the world, with the exception of China (33,34). It is important to analyse changes in the incidence and mortality rate of oesophageal cancer in the context of territorial socioeconomic disparities, this is especially true in countries affected by inequalities in healthcare. Fig. 1 llustrates the higher prevalence of SCC in low and middle-income countries.
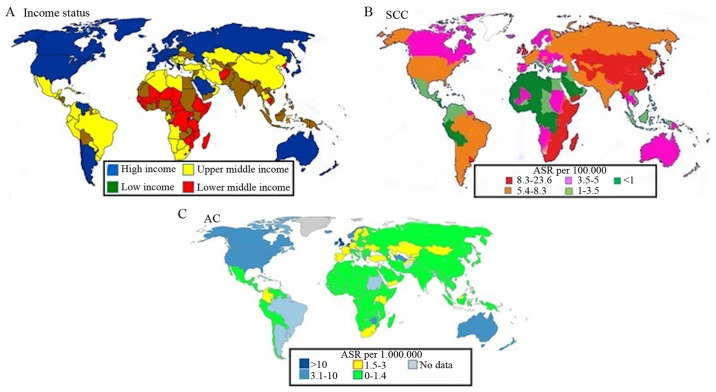
Countries in the oesophageal cancer corridor. The regions with the highest number of cases and most deaths are the south and the east of Africa, central Asia, Turkey, Iran, Kazakhstan and China (Fig. 2) (35,36). The Southern Africa region has the highest incidence of oesophageal cancer worldwide (4). Oesophageal cancer is a rare disease in Western Africa, with incidence rates of 0.8 and 0.4 in males and females respectively (4). This may be because they have not changed their life style, for example their diet, drastically in the last few decades. Fig. 1 illustrates the prevalence of AC in well-developed countries. India also falls within the Asian oesophageal-cancer belt and has a high incidence rate of oesophageal cancer (26).
Figure 2.
Oesophageal cancer incidence and income status of countries. (A) Countries divided into high, high middle, low middle and low income based on their GDP (145). (B) ASR per 100,000 for SCC. (C) Age-standardised incidence rate (ASR) per 100,000 for Adenocarcinoma (AC) (37,146). SCC, Squamous cell carcinoma; ASR, Age-standardised incidence rate.
South Africa
In South Africa oesophageal cancer is the eighth most common cancer in men and the eleventh in woman. In the early 20th century esophageal cancer was an uncommon disease in South Africa (37). From the 1940s, there was a rapid rise in the number of EC cases until esophageal cancer became the third most commonly diagnosed cancer in Black South Africans (38–40). In the African population group the ASR was 22.3 per 100,000 in males and 11.7 per 100,000 in females (41). In the African or mixed ancestry population group EC is the fourth highest cause of death in males (42). The area with the highest incidence is the Transkei region (43) with an ASR of 46.7/100,000 for males and 19.2/100,000 for females (44). When this disease is defined by sex and race, a slightly different picture emerges. A decrease in both SCC and AC becomes evident, especially when comparing African males and females with their non-African counterparts (37,45). However, other studies have found that there has only been a decrease in the prevalence of AC in South Africa (8). The areas in South Africa with the highest incidence of OC include the former Transkei region. This area was then a homeland settlement, with limited healthcare resources.
The increased incidence of EC in South Africa over the last decades is largely due to changes in lifestyle, diet, and the exposure to carcinogens (43). EC rates are highest in the 60 to 70-year age group. The two most important risk factors include cigarette fuming and extreme alcohol use (46). Approximately 17.6%, of adult South Africans use tobacco, 29.2% of males and 7.3% in females (47). South Africans consume >53 g of ethanol per day, which leads to a 5 times greater risk of developing esophageal cancer in comparison to non-drinkers. Smoking and drinking together lead to an 8.5 times greater risk of developing oesophageal cancer (48). Most of the studies on oesophageal cancer in South Africa have been performed in large urban areas like Johannesburg and Cape Town. Investigations performed amongst rural populations in South Africa, is more challenging hence, such data from is limited in South African databases.
Other risk factors include exposure to environmental smoke (cooking fires) (49), HPV infection (43) and diet. Helicobacteraceae infection may be related to OC risk as it was discovered in roughly 50% of South African patients with oesophageal carcinoma (50). Dietary risk factors include the use of wild herbs such as Solanum nigrum, the brewing and consumption of traditional maize based beer brewed with maize that may contain fungal mycotoxins or nitrosamines (37), and most importantly the shift to a Western diet. This diet is defined by an increase in the consumption of fats and animal protein (37). High-risk individuals in both the Transkei and KwaZulu-Natal province, are typically poorer with inadequate diets, and consume some class of alcohol and tobacco (51–53). In the Eastern Cape and Transkie, high risk of oesophageal cancer is associated with a diet low in green leafy vegetables and fruit (54). and is associated with low plasma concentrations of vitamins A, E, B12, folic acid and selenium (55). The increased consumption of maize compared to a more traditional diet which is based on other grains such as sorghum, may present additional risks. The maize-rich diet leads to increased levels of prostaglandin E2 (PGE2) in gastric fluid, an enzyme which increases Wnt signaling and proliferation (56).
Tanzania
Like all countries in the Eastern and Southern Africa cancer corridor, Tanzania has a high incidence of esophageal cancer. The age-standardized rate of EC incidence in Tanzania is 9.2 per 10,0000 (57). Generally esophageal carcinoma affects people at a young age in Tanzania, approximately 40 years and older. This is twenty years younger than the average seen in most developed countries (58). The region of Tanzania with the highest number of EC patients is the Kilimanjaro region, with the eastern and central parts of the country having a higher incidence rate of EC compared to the western parts (57). The control of esophageal cancer in Tanzania is hampered by the lack of educational and screening programs as well as a lack of facilities capable of diagnosing and treating the disease (58). There is only one specialized cancer treatment facility in Tanzania, the Ocean Road Cancer Institute (ORCI), located in Dar es Salaam (57). A study of patient numbers being diagnosed at ORCi compared with those receiving treatment showed that over 20% of EC patients did not receive treatment due to a lack of resources (57). As in other countries, the consumption of hot beverages has been linked to esophageal cancer in Tanzania. In this, case the consumption of hot milky tea (59). Oesophageal cancer in Kenya, especially in the regions bordering Tanzania, is a major health problem. In Kenya oesophageal cancer is more prevalent amongst people living in low socio-economic conditions, and is affected by the level of education and general living conditions (60).
India
OC is also a major health problem in India; particularly in snow-capped Kashmir valley and North-eastern states and is associated with peculiar food and drinking habits such as the drinking of hot salted tea which contains carcinogenic compounds like nitrosamines (29,61,62). Besides salted tea, tobacco smoking (Hukkah or water-pipe), sun dried vegetables are also very common in Kashmir valley and has been shown to be a potential risk factors for increased incidence of OC. In addition, high risk HPV type infection has also been reported form areas of OC cases in India (63,64).
China
China is also included in the oesophageal c cancer corridor. China accounts for more than half of all new cases of oesophageal cancer and is the fourth most frequently diagnosed cancer (65). The highest incidence is found in the rural areas (66). Certain areas of China, in Central North China, have the highest oesophageal cancer incidence rate in the world (over 100 per 100 000) (67,68). In China, oesophageal cancer occurs 20–30 times more than in the United States (69). SCC is the major type of oesophageal cancer and more than half of the global SCC cases occur in China (13). Oesophageal cancer is the fourth leading cause of cancer related death in China (65). The Chinese, government is still trying to improve the quality of the cancer registration data in rural areas (13). Like developed countries, an increase in the number of AC cases and a decrease in the number of SSC cases has been observed in China. The rise in the incidence of AC in China was reported in both urban and rural areas (70).
Apart from alcohol consumption and tobacco use is a high risk factors for oesophageal cancer in China include nutritional factors such as the consumption of fatty meat, salted and pickled vegetables and mouldy food as well as nutritional deficiencies. The populations from many of the areas in China with high oesophageal cancer rates were found to have a diet lacking in selenium, zinc, folate, riboflavin, and vitamins A, C, E, and B12 (71). These areas also contained high levels of nitrates and nitrosamines in local sources of drinking water and samples of food from local suppliers (72). A relationship also exists between the consumption of hot green tea and the risk of developing oesophageal cancer (73). Lifestyle factors include passive smoking, oesophageal lesions, and infection with Helicobacter pylori, low socioeconomic status and poor oral hygiene. However, a family history of cancer is also an important risk factor associated with increased risk of ESCC (52) and this points to a genetic component. Gastric atrophy, the replacement of dying of gastric cells with intestinal tissues, was also found to be an indication of increased risk for developing oesophageal cancer in Chines populations (74).
Tobacco use amongst Chinese males is currently estimated to be approximately 49.2–56.1% while it is estimated that only between 2.2–2.6% of Chinese females smokes (75). Alcohol is a Group 1 carcinogen and the body relies on alcohol dehydrogenases (ADHs) to convert alcohol into acetaldehyde, which is then converted to acetic acid by aldehyde dehydrogenase-2 (ALDH2). Mutations and polymorphisms in either of the genes encoding these two enzymes may decrease the ability to detoxify ethanol leading to cells being exposed to high levels of carcinogens (76). These mutations and polymorphisms are frequently found in individuals that originate from East Asia. ALDH2 mutations lead to the development of a rash or flush response when they consume alcohol. These individuals are at an increased risk of developing oesophageal cancer. A study performed in China, in the Shanxi Province, gave one of the strongest indications that genetics and familial history play a role in oesophageal cancer. This study showed that families with a history of oesophageal cancer were more likely to report a new case within ten years of the first case (77).
Developing countries outside of the OC cancer corridor
Brazil
Brazil is a good example of a country with social and healthcare inequalities across geographic regions. Parts of Brazil have the highest incidence of oesophageal cancer in the Western hemisphere. As in other countries alcohol and tobacco consumption are the main factors contributing to this high incidence rate. In the South of Brazil the consumption of hot mate (78). The incidence of oesophageal cancer in Brazil ranges from one to 18 per 100,000 inhabitants and is higher in the southern part of Brazil where it ranges from nine to 18 per 100 000 (79). The incidence of oesophageal cancer is intermediate in the central western and North Eastern regions where it ranges from 4 to 9 per 100,000 and is low in the Northern region, where it ranges from 1 to 2 per 100,000 (80). In Brazil cases are mainly diagnosed in individuals over the age of 30, which is similar to what is seen in Asian countries (81).
Western countries: The United States
The pattern of oesophageal cancer is rapidly changing worldwide. In Western countries, adenocarcinoma of the lower oesophagus has overtaken the previously more prevalent squamous cell carcinoma (82). Adenocarcinoma is the predominant type in Western countries (82). In the US, adenocarcinoma of the oesophagus is reported to be the most common malignancy with the fastest growing incidence, having increased six times in three decades (82,83). This contrasts with studies from the US in which adenocarcinoma accounted for 81% and squamous cell carcinoma for 17% (84). In another study among Asian/Pacific Islanders in the US, the rate of oesophageal squamous cell carcinoma was 81% higher than in white populations (85).
The characteristics of oesophageal cancer differ between Asian and western populations (Table III). These differences have been reported to play an important role in the disease (86). In future, studies and clinical practices must consider these ethnic and histological differences and molecular epidemiologic studies may will be helpful in investigating high-risk populations.
Table III.
The incidence rates of oesophageal cancer by World area and sex (Torre, 2016 #264).
| Country | Male (ASR of 100,000) | Female (ASR of 100,000) |
|---|---|---|
| Eastern Asia | 16.9 | 5.4 |
| Southern Africa | 17.7 | 6.7 |
| Eastern Africa | 11.9 | 7.8 |
| Northern Europe | 8.1 | 2.7 |
| South America | 7.0 | 2.0 |
| Western Europe | 6.8 | 1.6 |
| South-Central Asia | 6.5 | 3.9 |
| Central and Eastern Europe | 5.6 | 0.8 |
| Northern America | 5.4 | 1.1 |
| Australia/New-Zealand | 5.4 | 1.7 |
| Caribbean | 4.6 | 1.2 |
| Middle Africa | 4.2 | 2.0 |
| Melanesia | 3.6 | 1.4 |
| South-Eastern Asia | 3.6 | 1.0 |
| Southern Europe | 3.2 | 0.6 |
| Western Asia | 2.9 | 2.1 |
| Northern Africa | 2.4 | 1.5 |
| Central America | 1.7 | 0.6 |
| Western Africa | 0.8 | 0.4 |
AGR, age standardized rate.
6. Molecular epidemiology of oesophageal cancer
The risk of OC may be increased by environmental and behavioural factors, of which only a few cases exposed to risk factors develop oesophageal cancer. This indicates that there is a role played by genetics, which may increase the susceptibility of an individual to developing oesophageal disease. The role played by genetic factors has been demonstrated by immigrant epidemiology studies that both genetics and environmental factors are important components that affects oesophageal cancer risk (87,88). TP53 point mutations are common in both adenocarcinoma and ESCC, occurring in approximately 50% of cases. The mutations in p53 are detectable in the early stages of cancer development, being detectable in early metaplastic precancerous lesions (89).
The molecular profiles of both adenocarcinoma and SCC have been used to classify theses cancers into further subtypes. ESCC can be divided into three classes. The first class is characterised by genomic alterations in the NRF2 pathway, the second class is characterised by mutations in NOTCH1, ZNF750, KDM6A, KDM2D, PTEN and PIK3R1. Finally the third class is characterized by Phosphoinositide 3-kinase (PI3K) pathway disruption (90). Many of the genetic alterations identified in oesophageal squamous cell cancers are associated with cell cycle progression, apoptosis, DNA repair mechanisms and growth factor receptors. Epidermal growth factor receptor (EGFR) is overexpressed in 50% of ESCCs, mutations in p53 is found in 92% of ESCCs, while mutations in NOTCH1 and NOTCH3 are found in 25–33% of ESCCs. Another pathway that is commonly mutated is the Wnt pathway (91). The mutational profile of ESCC more closely resembles other squamous cell carcinomas than it does other adenocarcinoma[, with complex deletions and translocations being the dominant genetic variations (89). Mutations were also identified in the PI3KCA gene and showed overexpression of the mTOR protein (89).
Adenocarcinoma can also be classified using its molecular characteristics. The first subgroup has many C>A/T mutations. A second group us characterised by defective homologous recombination/chromosome segregation. A final group has a high number of T>G mutations mutation with high mutation burden (90). In addition to p53, adenocarcinomas also have a mutated in the tumor suppressor gene p16/CDKN2A. In adenocarcinoma additional genes that are regularly mutated include mediators of the Rho family ELMO1 and DOCK2 (mutated in 17% of cases). Mutation of these genes lead to an enhancement of cellular motility and an increase in invasion TP53 point mutations are common in both adenocarcinoma and ESCC, occurring in approximately 50% of cases. The mutations in p53 are detectable in the early stages of cancer development, being detectable in early metaplastic precancerous lesions (89). Other mutated genes are the chromatin-remodeling genes, ARID1A, SMARCA4 and ARID2. Adenocarcinoma is dominated by copy number alterations with frequent large-scale rearrangements, with a larger number of genes being rearranged, amplified or deleted than were affected by point mutations or insertions/deletions (92).
Many genes mutated in adenocarcinoma were also mutated in Barrett's oesophagus. However, p53 mutations are not common in Barrett's oesophagus (39%) (89). Genes involved in the development of Barrett's oesophagus included genes playing a role in oesophageal development FOXF1[18], FOXSP1 and transcription factors such as CREB, b BARX1 (93). Those that progress from Barret's oesophagus to adenocarcinoma, showing signs of chromosome instability with gene losses and gains. Non-progressors show signs of small localised deletions (89). The molecular epidemiology of ESCC is similar in different population groups, with a population of sub-Saharan ESCC patients showing similar genetic aberrations as those reported in Asian and North American cohorts (55,94). Chinese populations showed a ESCC mutation signature that seems to be linked to mutations in alcohol-metabolizing enzymes. This may help to explain the contribution made by alcohol consumption to ESCC (95).
Genetic risk factors such as single nucleotide polymorphisms (SNPs) are the most common genetic modification that affects the risk of an individual to develop cancer (96). SNPs may influence the risks, outcome and responses to treatment of oesophageal cancer (29). Therefore, it is important to identify genetic markers of oesophageal cancer as they could be used to develop personalised medicine. These markers can also be used as diagnostic biomarkers that can be screened to detect OC at the early stages (97).
Genetic factors
Literature on SC particularly SCC identified candidate genes that are involved in alcohol metabolism, detoxification of carcinogens, DNA repair, apoptosis and cell proliferation (98,99), but their results are not consistent across different populations. This lack in consistency indicates the role played by environmental differences between populations, differences in the level of exposure to different carcinogens as well as differences in sample sizes (98). Genome wide association studies (GWAS) successfully founded hundreds of genetic polymorphisms that are associated with complex diseases including cancer (96). SCC GWAS were conducted in four Asian populations, three in Chinese population and one in a Japanese population (100–103). Two SCC associated single nucleotide polymorphisms (SNPs) were identified in the Japanese study. These were SNPs in alcohol dehydrogenase 1B (rs1229984) and aldehyde dehydrogenase 2 (rs671) gene. These genes encode for metabolic enzymes that are involved in the metabolism of alcohol. Un-metabolised or partially metabolised alcohol is a carcinogen associated with altered SCC risk. The study also indicated gene environmental interactions of rs1229984 and rs671 with alcohol drinking and in the case of rs671, with smoking (101). Two of the Chinese genome association studies reported two susceptibility loci rs2274223 in phospholipase C and rs13042395 in chromosome 20 (104). In a larger GWAS of 2043 cases and 2063 controls in Chinese Han individuals, three new SNPs associated with SCC were identified. These were, rs10052657 in phosphodiesterase 4D, rs2014300 in runt related transcription factor 1and rs10484761 close to unc5 homolog C (100). No SNP has been identified that plays a larger role than environmental factors. SNPs have been identified in different population groups in South Africa that are associated with increased risk for developing oesophageal cancer. These studies targeted black Africans and mixed ancestry populations of South Africa and investigated the occurrence of 12 SNPs and one insertion/deletion variant from 8 genes, known to be associated with oesophageal cancer. These studies have indicated that several genetic variants in alcohol metabolism and DNA repair genes are known to contribute to genetic susceptibility to SCC in mixed ancestry populations but not in black South African populations of South Africa or Brazil. This shows that the differences in genetic variants may be explained by genetic history and different environmental exposures (97). This indicates that in low and middle countries more investigations are required that will involve more black populations than white and mixed ancestries populations, since caucasians and those of a mixed ancestry share some genetic history. Mixed population composition differs in genetic, epidemiological and socio demographical characteristics and these may result in association variation between smoking and different types of cancer (105). These differences in different populations are demonstrated in Table III, which shows different incidence rates of OC in different countries with different genetic history and environmental factors.
7. Diagnosis and prognosis of oesophageal cancer
Mortality in cancer patients ranged from 15 to 20% despite many advances in diagnosis and treatment (35). OC prognosis depends on local invasion and spread to regional and distant structures of the body. This type of cancer spread along the body using a variety of pathways such as direct extension, through the lymphatic system and haematogenous metastasis. The lack of an oesophageal wall allows the primary tumour to migrate rapidly into the adjacent structures of the neck and thorax such as the thyroid gland, trachea, larynx, lung, pericardium, aorta and diaphragm (106). The lymphatic drainage of the oesophagus drained by two individual lymphatic plexuses. One lymphatic plexuses develop within the mucosal layer and a second plexus develops within muscular layer. The lymphatic fluid of the oesophagus is able to flow to and communicate with any other part of the oesophagus and migrate in any direction and spread to the intra-thorax or intra-abdominal lymph nodes (107). In order for OC to spread to the liver, lungs, adrenalin glands, bones, kidney and brain, it must spread hematogenously (9,108). The lack of early symptoms complicates diagnosis, while the lack of a hereditary form of the disease makes population based screening impossible unless the screening takes place in high risk areas (35,109). Barrett's oesophagus can develop into cancer. This is because Barrett's oesophagus displays both low and high-grade dysplasia. Patients displaying high-grade dysplasia progress to cancer in approximately 1% of cases, while those displaying low-grade dysplasia progress to cancer in approximately 0.5 percent of patients. The best way to monitor these patients is through the use of endoscopy (109). However, the use of this screening method has been questioned since high numbers of individuals with reflux symptoms do not develop OC and 40% of these patients do not have reflux symptoms. This led to the endoscopic screening to be done in two steps, the detection of an abnormal area through changes in relief, color or in the course of superficial capillaries. This is then followed by morphological characterisation of the lesion (13,110).
In China, several screening methods have been performed and tested in the high-risk areas. These methods includes balloon cytology with smears (111–114), liquid-based balloon cytology (115), occult blood detection (116,117) and endoscopic examination with Lugol's iodine staining and biopsy (111,118). As a result of these studies, endoscopic examinations with iodine staining indicated a sensitive and specificity for the diagnosis of SCC (119,120). None of these studies indicated that any diagnostic method was associated with a reduction in OC incidence or mortality (121).
OC has a poor prognosis. The prognosis of cancer is performed through platelet count, as these are the integral component of the inflammation processes. However, platelet counts are known to be inversely related to cancer prognosis, higher platelet count correlates to a poorer prognosis. The cut off for platelet count as a prognosis factor has been contested. Tumour length is utilized as a prognostic factor in SCC but the length cut off in predicting survival has been debated (122). OC is normally only diagnosed at late stages of tumour development, resulting in higher mortality.
Oesophageal cancer prevention
The prevention of OC differs depending on cell type. The best way to prevent oesophageal cancer is to avoid exposure to environmental risks. In the case of SCC, it is important to reduce or quit tobacco usage and alcohol consumption. Reports indicated that no particular risk factor is responsible for the rise of OC incidence and several strategies are under investigations using agents such as nonsteroidal anti-inflammatory drugs, selenium, alpha-di-fluoro-methyl-ornithine, and retinoids (123). Vegetable and fruit intake are reported to be important preventive strategies, in the case of obesity, which is reported as a risk factor for AC). Follow up of patients with precancerous lesions is recommended. Surveillance, endoscopic screening and surgical resection are important approaches that are suggested to prevent the progression of high-grade dysplasia patients (9). Monitoring the weight of obese patients is also an important strategy of prevention. In Asian and African countries such as China and South Africa, there are preventive approaches of cancer related diseases and OC is one of them, which are under investigation such as using medicinal plant extracts to induce apoptosis. Both China and African countries have a history of using traditional herbs to treat diseases. These plants are currently being assessed scientifically for their medicinal value. This involves the extraction and purification of crude plant extracts. The purified compounds can then be tested for their ability to treat diseases. For instance, the effectiveness of these compounds in cancer treatment can be assessed by exposing cancer cells to these compounds. This is one of the important strategies required to treat OC in low and middle countries such as China, India, Brazil and South Africa. These compounds may serve as lead targets for the development of new drugs for the treatment of SCC or even AC in developed countries. Table III, indicates that low and middle-income countries are having high incidence of OC (124).
8. Oesophageal cancer treatment
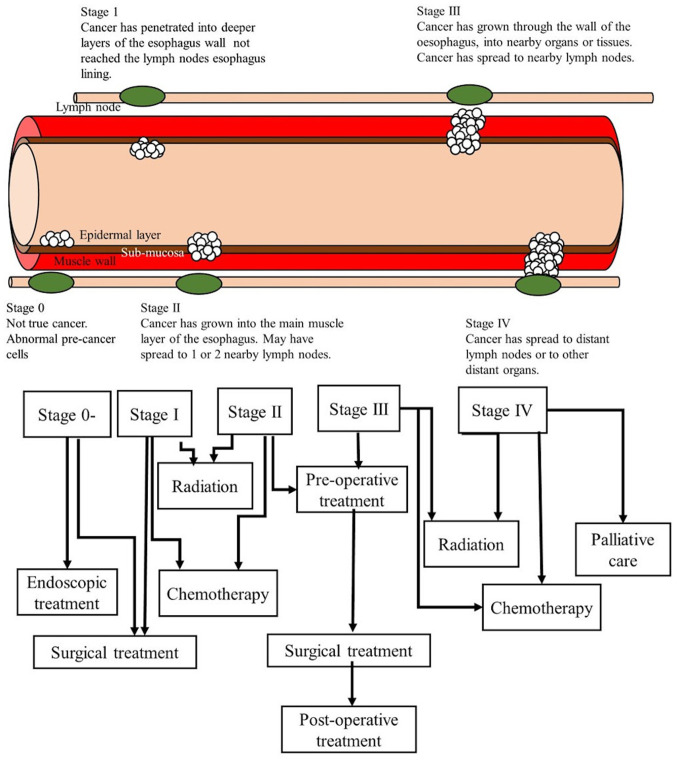
The choice of treatment strategy depends on the stage of the cancer (Fig. 3) (125). There are two broad approaches to treat OC, surgical or non-surgical. The appropriate use of surgical approach is determined by the resect ability of the cancer. OC tumours that are locally advanced are good candidates for surgical intervention. Non-surgical approaches are meant for patients with tumours that cannot be surgically removed due to them spreading to various locations in the body or being in-operable due to location (35,126–128).
Figure 3.
Treatment of oesophageal cancer at different stages (130).
Surgical treatment
Surgical treatment is divided into six types, endoscopic procedures, resection, lymph-node dissection, and minimally invasive oesophagectomy, neoadjuvant chemotherapy with surgical resection, neoadjuvant chemoradiotherapy surgery, and surgery with adjuvant chemotherapy, radiation or chemoradiation (128). OC may require surgical resection, which includes traditional oesophagostomy and transthoracic approaches (127,128). This surgical option depends on the location of the tumour and the preference of the surgeon (35). Lymph-node dissection surgery is required for patients with oesophageal carcinoma that may be prone to spreading. An oesophagostomy targets the abdominal lymph nodes and the thoracic lymph nodes. This type of dissection is commonly performed in Japan, where incidence of SCC is high (129). It has been noticed that a mortality rate of 1–23% is associated with oesophagostomy. In order, to reduce the morbidity and mortality associated with oesophagostomy, minimally invasive oesophagostomy was introduced (130).
Immunotherapy
Avoiding the immune system is one of the hallmarks of cancer. Inducing or sustaining the immune system to act against cancer cells, is a promising therapeutic strategy. This has led to the development of immunotherapies to treat oesophageal cancer. Different classes of compounds have shown promising results. These include cancer vaccines and immune checkpoint inhibitors (ICI) (131). The development of cancer vaccines is based on the identification of immunogenic cancer antigens (ICA) Cancer vaccines work by initiating antigen specific cytotoxiv T lymphocyte killing of cancer cells. One approach is to use dendritic cells loaded with multiple Tumor specific antigens, leading to the activation of multiple population of T cells (131). Novel ICAs for ESCC have been identified which match the criteria for being good UCAs as they hive high expression levels in ESCC. They are also essential molecules for the survival of the cancer cells/Despite this, no cancer vaccine has been approved for the treatment of ESCC yet.
As mentioned previously, another type of immunotherapy is the use of immune checkpoint inhibitors. The response of T cells to cancer cells is regulated by immune checkpoints. This checkpoints are regulated through the binding of inhibitory or stimulatory molecules to receptors, examples of which include Cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and programmed cell death protein 1 (PD-1) (131). Both of these checkpoint receptors are expressed on T cells and act to inhibit T cells by inhibiting the activity of receptors such as CD28, which activate T cells (131) An ICI named ipilimumab is an anti-CTLA-4 mAb, that is able to treat metastatic melanoma. PD-1 binds to the death-ligand receptor 1 (PD-L1) on cancer cells to induce apoptosis in T cells. PD-L1 is, therefore, an inhibitory B7 family member and is up-regulated in ESCC. Four anti-PD1 mAbs, nivolumab, avelumab, pembrolizumab and atezolizumab are used to treat cancer. Anti-CTLA-4 mAb (ipilimumab) and anti-PD-1 mAb (nivolumab), have both demonstrated the ability to decrease in tumor size (131,132).
Combination therapies
It was suggested that the spread of OC could be controlled by the combination of both chemotherapy and surgery (133). This type of surgery has encountered some problems since patients with SCC or adenocarcinoma shown conflicting results. However, a UK Medical Research Council Oesophageal cancer Working Group study tested the effectiveness of surgery combined with chemotherapy. This study identified a significant improvement in 3-year survival compared with surgery alone (134).
Neoadjuvant chemoradiotherapy and surgery is commonly used in the USA for locally advanced oesophageal cancer. Most randomised studies of this surgery have shown non-significant results. Two studies performed indicated significant survival benefit of this commination treatment (135,136). It has been predicted that adjuvant chemotherapy treated with primary resection might be beneficial especial in patients with node-positive disease (133,137–139). In several randomised trials performed by the Japanese Clinical Oncology Group compared surgery with or without chemotherapy in SCC patients (137,138). In one study, 5-year disease-free survival indicated that combined therapy was favoured (137).
Non-surgical treatment
Non-surgical treatment are divided into six treatment approaches, namely: Radiotherapy; concurrent definitive chemoradiation; salvage oesophagectomy after definitive chemoradiation; advanced metastatic or recurrent disease; biological and targeted therapies; and endoscopic treatment. It is well known that external beam radiotherapy played an important role in the management of un-resectable oesophageal carcinoma. Sustained remission and long-term survival are rarely achieved, although radiotherapy is used in palliative treatment for dysphagia. The preferred approach is chemo-radiotherapy for patients suitable for combined therapy as it provides better palliation than radiotherapy alone and improves the likelihood of long-term progression-free survival (140). Radiotherapy against chemo-radiotherapy was assessed with cisplatin and fluorouracil in patients with 90% SCC. Chemo-radiotherapy group had an estimated 5-year survival of 27% and there was no 5-year survival observed in those patients who received radiotherapy alone. It was suggested that although chemo-radiotherapy without surgery is accepted as a SCC treatment, local control is improved when performed with surgery (141).
Salvage oesophagostomy has a higher morbidity and mortality than regular oesophagostomy performed in neoadjuvant methods. A 5-year survival estimation of 25% in selected patients has shown an increase in perioperative risks. So Salvage oesophagostomy was suggested to be considered for selected patients. It is only an option for patients that respond to chemo-radiotherapy. In most cases by the time of diagnosis of oesophageal carcinoma. The tumour has already started to spread and metasasise (142). Combined short-acting and long-acting narcotics and local radiotherapy are used to treat pain. The effectiveness of chemotherapy or chemo-radiation is observed in approximately 50% of patients; however, management of pain is effective in almost all patients. Cisplatin and fluoroucil combination play a vital role as supportive care in SCC patients (143). Agents consisting of small molecules and antibodies were created and incorporated into multimodal therapies for tumours (144). The commonly used agents include the angiogenesis inhibitor bevacizumab and the inhibitors of epidermal growth factor receptor; panitumumab; cetuximab; and erlotinib (23).
Endoscopic therapies are used to treat advanced or inoperative cancers and have been suggested as curative approaches for early-stage oesophageal carcinomas. Barrett's oesophagus and early stage cancer might be treatable endoscopically with resection or ablation. Nonsurgical treatment seem to be less reliable than surgical treatment. These treatment options are also more common in well-developed countries. In low and middle countries due to lack of funds and experienced personnel (23).
9. Conclusions
The epidemiological differences in the incidence rates of oesophageal cancer, in terms of differences between sexes and economic status of countries, means that very different strategies for diagnosis, treatment and prevention need to be adopted in different areas and for different population groups. Developed countries, with higher rates of AC, have more treatment options due to available resources. Developing countries, with the higher rates of SCC, still rely on surgery. These countries also show far higher incidence of oesophageal cancer, due to high levels of tobacco and alcohol use, poorer nutrition and exposure to other environmental hazards such as cooking fires and nitrosamine contamination of foods. Environmental factors or race have a vital functional role in oesophageal cancer due to genetic factors, for example where causative genes in black Africans differ from other races. Diagnosis of the disease is challenging since the disease cannot be detected at early stages or early ages. People need to be taught how to prevent this disease and how are these preventions going to help them so that the incidence decrease in these countries. Treatment for oesophageal cancer does not seem reliable; more research is required to improve the diagnosis, risk factors and treatment in this disease.
Acknowledgements
Not applicable.
Glossary
Abbreviations
- AC
adenocarcinoma
- ADHs
alcohol dehydrogenases
- ALDH2
aldehyde dehydrogenase-2
- ASR
age-standardised incidence rate
- GWAS
genome wide association studies
- OC
oesophageal cancer
- ORCI
Ocean Road Cancer Institute
- PGE2
prostaglandin E2
- SCC
squamous cell carcinoma
- SNPs
nucleotide polymorphisms
Funding
The authors would like to thank the Medical Research Council of South Africa for funding this research.
Availability of data and materials
Not applicable.
Authors' contributions
ZD was responsible for the acquisition of funding and writing of the manuscript. RH, MM, RM and ZMK were responsible for the collection of data. RH, MM, TM, RM and ZMK were responsible for writing the manuscript. RH, TM, RM, ZMK, CH, SMW, RMR, SH, GK and DOB were responsible for editing/revising the manuscript. ZD was also responsible for supervising the research group.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
Authors declare that they have no competing interests.
References
- 1.Henry MA, Lerco MM, Ribeiro PW, Rodrigues MA. Epidemiological features of esophageal cancer. Squamous cell carcinoma versus adenocarcinoma. Acta Cir Bras. 2014;29:389–393. doi: 10.1590/S0102-86502014000600007. [DOI] [PubMed] [Google Scholar]
- 2.Cook MB, Chow WH, Devesa SS. Oesophageal cancer incidence in the United States by race, sex, and histologic type, 1977–2005. Br J Cancer. 2009;101:855–859. doi: 10.1038/sj.bjc.6605246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosetti C, Levi F, Ferlay J, Garavello W, Lucchini F, Bertuccio P, Negri E, La Vecchia C. Trends in oesophageal cancer incidence and mortality in Europe. Int J Cancer. 2008;122:1118–1129. doi: 10.1002/ijc.23232. [DOI] [PubMed] [Google Scholar]
- 4.Torre LA, Siegel RL, Ward EM, Jemal A. Global cancer incidence and mortality rates and trends-an update. Cancer Epidemiol Biomarkers Prev. 2016;25:16–27. doi: 10.1158/1055-9965.EPI-15-0578. [DOI] [PubMed] [Google Scholar]
- 5.Das M, Saikia BJ, Sharma SK, Sekhon GS, Mahanta J, Phukan RK. p16 hypermethylation: A biomarker for increased esophageal cancer susceptibility in high incidence region of North East India. Tumour Biol. 2015;36:1627–1642. doi: 10.1007/s13277-014-2762-7. [DOI] [PubMed] [Google Scholar]
- 6.Hongo M, Nagasaki Y, Shoji T. Epidemiology of esophageal cancer: Orient to Occident. Effects of chronology, geography and ethnicity. J Gastroenterol Hepatol. 2009;24:729–735. doi: 10.1111/j.1440-1746.2009.05824.x. [DOI] [PubMed] [Google Scholar]
- 7.Launay L, Dejardin O, Pornet C, Morlais F, Guittet L, Launoy G, Bouvier V. Influence of socioeconomic environment on survival in patients diagnosed with esophageal cancer: A population-based study. Dis Esophagus. 2012;25:723–730. doi: 10.1111/j.1442-2050.2011.01312.x. [DOI] [PubMed] [Google Scholar]
- 8.Lambert R, Hainaut P. Esophageal cancer: Cases and causes (part I) Endoscopy. 2007;39:550–555. doi: 10.1055/s-2007-966589. [DOI] [PubMed] [Google Scholar]
- 9.Napier KJ, Scheerer M, Misra S. Esophageal cancer: A review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol. 2014;6:112–120. doi: 10.4251/wjgo.v6.i5.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herszényi L, Tulassay Z. Epidemiology of gastrointestinal and liver tumors. Eur Rev Med Pharmacol Sci. 2010;14:249–258. [PubMed] [Google Scholar]
- 11.Zhang L, Ma W, Li Y. Huge primary malignant melanoma of the esophagus: A case report and literature review. Thorac Cancer. 2013;4:479–483. doi: 10.1111/1759-7714.12063. [DOI] [PubMed] [Google Scholar]
- 12.Gupta V, Coburn N, Kidane B, Hess KR, Compton C, Ringash J, Darling G, Mahar AL. Survival prediction tools for esophageal and gastroesophageal junction cancer: A systematic review. J Thorac Cardiovasc Surg. 2018;156:847–856. doi: 10.1016/j.jtcvs.2018.03.146. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013;19:5598–5606. doi: 10.3748/wjg.v19.i34.5598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daly JM, Fry WA, Little AG, Winchester DP, McKee RF, Stewart AK, Fremgen AM. Esophageal cancer: Results of an American College of Surgeons Patient Care Evaluation Study. J Am Coll Surg. 2000;190:562–573. doi: 10.1016/S1072-7515(00)00238-6. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organisation. Global status report on alcohol and health, 2014. https://www.who.int/substance_abuse/publications/global_alcohol_report/en/ [Feb 15;2020 ]; [Google Scholar]
- 16.World Health Organisation. Prevalence of tobacco smoking, 2015. https://www.who.int/gho/tobacco/use/en/ [Nov 18;2018 ]; [Google Scholar]
- 17.Akbari MR, Malekzadeh R, Shakeri R, Nasrollahzadeh D, Foumani M, Sun Y, Pourshams A, Sadjadi A, Jafari E, Sotoudeh M, et al. Candidate gene association study of esophageal squamous cell carcinoma in a high-risk region in Iran. Cancer Res. 2009;69:7994–8000. doi: 10.1158/0008-5472.CAN-09-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart BW, Kleihues P, editors. IARC Press; Lyon: 2003. World Cancer Report. [Google Scholar]
- 19.Brown LM, Hoover RN, Greenberg RS, Schoenberg JB, Schwartz AG, Swanson GM, Liff JM, Silverman DT, Hayes RB, Pottern LM. Are racial differences in squamous cell esophageal cancer explained by alcohol and tobacco use? J Natl Cancer Inst. 1994;86:1340–1345. doi: 10.1093/jnci/86.17.1340. [DOI] [PubMed] [Google Scholar]
- 20.Muwonge R, Ramadas K, Sankila R, Thara S, Thomas G, Vinoda J, Sankaranarayanan R. Role of tobacco smoking, chewing and alcohol drinking in the risk of oral cancer in Trivandrum, India: A nested case-control design using incident cancer cases. Oral Oncol. 2008;44:446–454. doi: 10.1016/j.oraloncology.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Blot W, McLaughlin J, Fraumeni J Jr, editors. Oxford University Press Oxford; 2006. Esophageal cancer. [DOI] [Google Scholar]
- 22.Blot W, Tarone R. Esophageal cancer. In: Thun M, Linet M, Cerhan L, Haiman C, Schottenfeld D, editors. Cancer epidemiology and prevention. Oxford University Press; Oxford: 2006. pp. 579–592. [Google Scholar]
- 23.Blot W, McLaughlin J, Fraumeni JJ., Jr . Esophageal Cancer. In: Thun M, Linet M, Cerhan J, Haiman C, Schottenfeld D, editors. Cancer Epidemiology and Prevention. 4th. Oxford University Press; Oxford: 2006. pp. 697–707. [DOI] [Google Scholar]
- 24.Nieman DR, Peters JH. Treatment strategies for esophageal cancer. Gastroenterol Clin North Am. 2013;42:187–197. doi: 10.1016/j.gtc.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Wang KK, Sampliner RE, Practice Parameters Committee of the American College of Gastroenterology Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus. Am J Gastroenterol. 2008;103:788–797. doi: 10.1111/j.1572-0241.2008.01835.x. [DOI] [PubMed] [Google Scholar]
- 26.Khan NA, Teli MA, Mohib-Ul Haq M, Bhat GM, Lone MM, Afroz F. A survey of risk factors in carcinoma esophagus in the valley of Kashmir, Northern India. J Cancer Res Ther. 2011;7:15–18. doi: 10.4103/0973-1482.80431. [DOI] [PubMed] [Google Scholar]
- 27.Islami F, Kamangar F, Nasrollahzadeh D, Aghcheli K, Sotoudeh M, Abedi-Ardekani B, Merat S, Nasseri-Moghaddam S, Semnani S, Sepehr A, et al. Socio-economic status and oesophageal cancer: Results from a population-based case-control study in a high-risk area. Int J Epidemiol. 2009;38:978–988. doi: 10.1093/ije/dyp195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siddiqi M, Kumar R, Kaul D, Spiegelhalder B, Preussmann R. Salivary nitrate and nitrite concentrations from a sample population of children and adults in high risk area for esophageal and gastric cancers in Kashmir, India. Cancer Lett. 1992;64:133–136. doi: 10.1016/0304-3835(92)90073-5. [DOI] [PubMed] [Google Scholar]
- 29.Gupta B, Kumar N. Worldwide incidence, mortality and time trends for cancer of the oesophagus. Eur J Cancer Prev. 2017;26:107–118. doi: 10.1097/CEJ.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 30.Hussain S, M Y, Thakur N, Salam I, Singh N, Mir MM, Bhat MA, Siddiqi MA, Das BC, Bharadwaj M. Association of cyclin D1 gene polymorphisms with risk of esophageal squamous cell carcinoma in Kashmir Valley: A high risk area. Mol Carcinog. 2011;50:487–498. doi: 10.1002/mc.20732. [DOI] [PubMed] [Google Scholar]
- 31.Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003;349:2241–2252. doi: 10.1056/NEJMra035010. [DOI] [PubMed] [Google Scholar]
- 32.Arnold M, Soerjomataram I, Ferlay J, Forman D. Global incidence of oesophageal cancer by histological subtype in 2012. Gut. 2015;64:381–387. doi: 10.1136/gutjnl-2014-308124. [DOI] [PubMed] [Google Scholar]
- 33.Eslick GD. Epidemiology of esophageal cancer. Gastroenterol Clin North Am. 2009;38:17–25. doi: 10.1016/j.gtc.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 34.Thuler FP, Forones NM, Ferrari AP. Advanced esophageal cancer: Still a delayed diagnosis. Arq Gastroenterol. 2006;43:206–211. doi: 10.1590/S0004-28032006000300010. [DOI] [PubMed] [Google Scholar]
- 35.Barrios E, Sierra MS, Musetti C, Forman D. The burden of oesophageal cancer in Central and South America. Cancer Epidemiol. 2016;44(Suppl 1):S53–S61. doi: 10.1016/j.canep.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 36.Pennathur A, Gibson MK, Jobe BA, Luketich JD. Oesophageal carcinoma. Lancet. 2013;381:400–412. doi: 10.1016/S0140-6736(12)60643-6. [DOI] [PubMed] [Google Scholar]
- 37.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 38.Segal I, Reinach SG, de Beer M. Factors associated with oesophageal cancer in Soweto, South Africa. Br J Cancer. 1988;58:681–686. doi: 10.1038/bjc.1988.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Higginson J, Oettle AG. Cancer incidence in the Bantu and ‘Cape Colored’ races of South Africa: Report of a cancer survey in the Transvaal (1953–55) J Natl Cancer Inst. 1960;24:589–671. doi: 10.1093/jnci/24.3.589. [DOI] [PubMed] [Google Scholar]
- 40.Oettl AJSAMJ. An epidemic of oesophageal carcinoma in Africa. 1963;37:435. [Google Scholar]
- 41.Rose EF. Esophageal cancer in the Transkei: 1955–69. J Natl Cancer Inst. 1973;51:7–16. doi: 10.1093/jnci/51.1.7. [DOI] [PubMed] [Google Scholar]
- 42.Jemal A, Bray F, Forman D, O'Brien M, Ferlay J, Center M, Parkin DM. Cancer burden in Africa and opportunities for prevention. Cancer. 2012;118:4372–4384. doi: 10.1002/cncr.27410. [DOI] [PubMed] [Google Scholar]
- 43.Blot WJ. Esophageal cancer trends and risk factors. Semin Oncol. 1994;21:403–410. [PubMed] [Google Scholar]
- 44.Sammon AM. Carcinogens and endemic squamous cancer of the oesophagus in Transkei, South Africa. Environmental initiation is the dominant factor; tobacco or other carcinogens of low potency or concentration are sufficient for carcinogenesis in the predisposed mucosa. Med Hypotheses. 2007;69:125–131. doi: 10.1016/j.mehy.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 45.Makaula AN, Marasas WF, Venter FS, Badenhorst CJ, Bradshaw D, Swanevelder S. Oesophageal and other cancer patterns in four selected districts of the Transkei, Southern Africa: 1985–1990. Afr J Health Sci. 1996;3:11–15. [PubMed] [Google Scholar]
- 46.Bizos D, Morgan H, Motha N, Makda M, Domingo A, Tiedt S, Wing J, Munanga M, Tembo J, Hale M, Bizos D. Comparison of the incidence of oesophageal cancer in two 6-year periods from selected hospitals in and around Gauteng Province, South Africa. South Afr J Surg. 2015;53:55–58. doi: 10.7196/sajsnew.7857. [DOI] [Google Scholar]
- 47.Lagergren J, Bergström R, Lindgren A, Nyrén O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–831. doi: 10.1056/NEJM199903183401101. [DOI] [PubMed] [Google Scholar]
- 48.Reddy P, Zuma K, Shisana O, Jonas K, Sewpaul R. Prevalence of tobacco use among adults in South Africa: Results from the first South African National Health and Nutrition Examination Survey. S Afr Med J. 2015;105:648–655. doi: 10.7196/SAMJnew.7932. [DOI] [PubMed] [Google Scholar]
- 49.Sewram V, Sitas F, O'Connell D, Myers J. Tobacco and alcohol as risk factors for oesophageal cancer in a high incidence area in South Africa. Cancer Epidemiol. 2016;41:113–121. doi: 10.1016/j.canep.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 50.Dlamini Z, Bhoola K. Esophageal cancer in African blacks of Kwazulu Natal, South Africa: An epidemiological brief. Ethn Dis. 2005;15:786–789. [PubMed] [Google Scholar]
- 51.Schandl L, Malfertheiner P, Ebert MP. Prevention of gastric cancer by Helicobacter pylori eradication? Dig Dis. 2002;20:18–22. doi: 10.1159/000063157. [DOI] [PubMed] [Google Scholar]
- 52.Lin Y, Totsuka Y, Shan B, Wang C, Wei W, Qiao Y, Kikuchi S, Inoue M, Tanaka H, He Y. Esophageal cancer in high-risk areas of China: Research progress and challenges. Ann Epidemiol. 2017;27:215–221. doi: 10.1016/j.annepidem.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 53.Long N, Moore MA, Chen W, Gao CM, Lai MS, Mizoue T, Oyunchimeg D, Park S, Shin HR, Tajima K, et al. Cancer epidemiology and control in north-East Asia-past, present and future. Asian Pac J Cancer Prev. 2010;11(Suppl 2):S107–S148. [PubMed] [Google Scholar]
- 54.Wang AH, Sun CS, Li LS, Huang JY, Chen QS. Relationship of tobacco smoking CYP1A1 GSTM1 gene polymorphism and esophageal cancer in Xi'an. World J Gastroenterol. 2002;8:49–53. doi: 10.3748/wjg.v8.i1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sewram V, Sitas F, O'Connell D, Myers J. Diet and esophageal cancer risk in the Eastern Cape Province of South Africa. Nutr Cancer. 2014;66:791–799. doi: 10.1080/01635581.2014.916321. [DOI] [PubMed] [Google Scholar]
- 56.Jaskiewicz K. Oesophageal carcinoma: Cytopathology and nutritional aspects in aetiology. Anticancer Res. 1989;9:1847–1852. [PubMed] [Google Scholar]
- 57.Pink RC, Bailey TA, Iputo JE, Sammon AM, Woodman AC, Carter DR. Molecular basis for maize as a risk factor for esophageal cancer in a South African population via a prostaglandin E2 positive feedback mechanism. Nutr Cancer. 2011;63:714–721. doi: 10.1080/01635581.2011.570893. [DOI] [PubMed] [Google Scholar]
- 58.Gabel JV, Chamberlain RM, Ngoma T, Mwaiselage J, Schmid KK, Kahesa C, Soliman AS. Clinical and epidemiologic variations of esophageal cancer in Tanzania. World J Gastrointest Oncol. 2016;8:314–320. doi: 10.4251/wjgo.v8.i3.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McHembe MD, Rambau PF, Chalya PL, Jaka H, Koy M, Mahalu W. Endoscopic and clinicopathological patterns of esophageal cancer in Tanzania: Experiences from two tertiary health institutions. World J Surg Oncol. 2013;11:257. doi: 10.1186/1477-7819-11-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Munishi MO, Hanisch R, Mapunda O, Ndyetabura T, Ndaro A, Schüz J, Kibiki G, McCormack V. Africa's oesophageal cancer corridor: Do hot beverages contribute? Cancer Causes Control. 2015;26:1477–1486. doi: 10.1007/s10552-015-0646-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Patel K, Wakhisi J, Mining S, Mwangi A, Patel R. Esophageal cancer, the topmost cancer at MTRH in the Rift Valley, Kenya, and its potential risk factors. ISRN Oncol. 2013;2013:503249. doi: 10.1155/2013/503249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Khuroo MS, Zargar SA, Mahajan R, Banday MA. High incidence of oesophageal and gastric cancer in Kashmir in a population with special personal and dietary habits. Gut. 1992;33:11–15. doi: 10.1136/gut.33.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Murphy G, McCormack V, Abedi-Ardekani B, Arnold M, Camargo MC, Dar NA, Dawsey SM, Etemadi A, Fitzgerald RC, Fleischer DE, et al. International cancer seminars: A focus on esophageal squamous cell carcinoma. Ann Oncol. 2017;28:2086–2093. doi: 10.1093/annonc/mdx279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Katiyar S, Hedau S, Jain N, Kar P, Khuroo MS, Mohanta J, Kumar S, Gopalkrishna V, Kumar N, Das BC. p53 gene mutation and human papillomavirus (HPV) infection in esophageal carcinoma from three different endemic geographic regions of India. Cancer Lett. 2005;218:69–79. doi: 10.1016/j.canlet.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 65.Salam I, Hussain S, Mir MM, Dar NA, Abdullah S, Siddiqi MA, Lone RA, Zargar SA, Sharma S, Hedau S, et al. Aberrant promoter methylation and reduced expression of p16 gene in esophageal squamous cell carcinoma from Kashmir valley: A high-risk area. Mol Cell Biochem. 2009;332:51–58. doi: 10.1007/s11010-009-0173-7. [DOI] [PubMed] [Google Scholar]
- 66.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 67.Chen M, Huang J, Zhu Z, Zhang J, Li K. Systematic review and meta-analysis of tumor biomarkers in predicting prognosis in esophageal cancer. BMC Cancer. 2013;13:539. doi: 10.1186/1471-2407-13-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guo W, Blot WJ, Li JY, Taylor PR, Liu BQ, Wang W, Wu YP, Zheng W, Dawsey SM, Li B, et al. A nested case-control study of oesophageal and stomach cancers in the Linxian nutrition intervention trial. Int J Epidemiol. 1994;23:444–450. doi: 10.1093/ije/23.3.444. [DOI] [PubMed] [Google Scholar]
- 69.Parkin DM, Stjernsward J, Muir CS. Estimates of the worldwide frequency of twelve major cancers. Bull World Health Organ. 1984;62:163–182. [PMC free article] [PubMed] [Google Scholar]
- 70.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 71.Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2005;97:142–146. doi: 10.1093/jnci/dji181. [DOI] [PubMed] [Google Scholar]
- 72.Taylor PR, Li B, Dawsey SM, Li JY, Yang CS, Guo W, Blot WJ. Prevention of esophageal cancer: The nutrition intervention trials in Linxian, China. Linxian Nutrition Intervention Trials Study Group. Cancer Res. 1994;54(Suppl 7):2029S–2031S. [PubMed] [Google Scholar]
- 73.Yang CS. Research on esophageal cancer in China: A review. Cancer Res. 1980;40:2633–2644. [PubMed] [Google Scholar]
- 74.Wu M, Liu AM, Kampman E, Zhang ZF, Van't Veer P, Wu DL, Wang PH, Yang J, Qin Y, Mu LN, et al. Green tea drinking, high tea temperature and esophageal cancer in high- and low-risk areas of Jiangsu Province, China: A population-based case-control study. Int J Cancer. 2009;124:1907–1913. doi: 10.1002/ijc.24142. [DOI] [PubMed] [Google Scholar]
- 75.Kamangar F, Diaw L, Wei WQ, Abnet CC, Wang GQ, Roth MJ, Liu B, Lu N, Giffen C, Qiao YL, Dawsey SM. Serum pepsinogens and risk of esophageal squamous dysplasia. Int J Cancer. 2009;124:456–460. doi: 10.1002/ijc.23918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Li Q, Hsia J, Yang G. Prevalence of smoking in China in 2010. N Engl J Med. 2011;364:2469–2470. doi: 10.1056/NEJMc1102459. [DOI] [PubMed] [Google Scholar]
- 77.Salaspuro M. Acetaldehyde and gastric cancer. J Dig Dis. 2011;12:51–59. doi: 10.1111/j.1751-2980.2011.00480.x. [DOI] [PubMed] [Google Scholar]
- 78.Kollarova H, Machova L, Horakova D, Janoutova G, Janout V. Epidemiology of esophageal cancer-an overview article. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2007;151:17–20. doi: 10.5507/bp.2007.003. [DOI] [PubMed] [Google Scholar]
- 79.Ribeiro Pinto LF, Teixeira Rossini AM, Albano RM, Felzenszwalb I, de Moura Gallo CV, Nunes RA, Andreollo NA. Mechanisms of esophageal cancer development in Brazilians. Mutat Res. 2003;544:365–373. doi: 10.1016/j.mrrev.2003.06.021. [DOI] [PubMed] [Google Scholar]
- 80.Mota OM, Curado MP, Oliveira JC, Martins E, Cardoso DM. Risk factors for esophageal cancer in a low-incidence area of Brazil. Sao Paulo Med J. 2013;131:27–34. doi: 10.1590/S1516-31802013000100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gao Y, He Y, Xu J, Xu L, Du J, Zhu C, Gu H, Ma H, Hu Z, Jin G, et al. Genetic variants at 4q21, 4q23 and 12q24 are associated with esophageal squamous cell carcinoma risk in a Chinese population. Hum Genet. 2013;132:649–656. doi: 10.1007/s00439-013-1276-5. [DOI] [PubMed] [Google Scholar]
- 82.Vioque J, Barber X, Bolumar F, Porta M, Santibáñez M, de la Hera MG, Moreno-Osset E, PANESOES Study Group Esophageal cancer risk by type of alcohol drinking and smoking: a case-control study in Spain. BMC Cancer. 2008;8:221. doi: 10.1186/1471-2407-8-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pun C, Aryal G, Basyal R, Shrestha S, Pathak T, Bastola S, Neupane S, Shrestha BM, Thakur BK, Lee MC. Histological pattern of esophageal cancer at BP Koirala memorial cancer hospital in Nepal: A three year retrospective study. J Pathol Nepal. 2012;2:277–281. doi: 10.3126/jpn.v2i4.6877. [DOI] [Google Scholar]
- 84.Ali A, Ersumo T, Johnson O. Oesophageal carcinoma in Tikur Anbessa Hospital, Addis Ababa. East Afr Med J. 1998;75:590–593. [PubMed] [Google Scholar]
- 85.Schlansky B, Dimarino AJ, Jr, Loren D, Infantolino A, Kowalski T, Cohen S. A survey of oesophageal cancer: Pathology, stage and clinical presentation. Aliment Pharmacol Ther. 2006;23:587–593. doi: 10.1111/j.1365-2036.2006.02782.x. [DOI] [PubMed] [Google Scholar]
- 86.Cherian JV, Sivaraman R, Muthusamy AK, Jayanthi V. Carcinoma of the esophagus in Tamil Nadu (South India): 16-year trends from a tertiary center. J Gastrointestin Liver Dis. 2007;16:245–249. [PubMed] [Google Scholar]
- 87.Fan YJ, Song X, Li JL, Li XM, Liu B, Wang R, Fan ZM, Wang LD. Esophageal and gastric cardia cancers on 4238 Chinese patients residing in municipal and rural regions: A histopathological comparison during 24-year period. World J Surg. 2008;32:1980–1988. doi: 10.1007/s00268-008-9674-x. [DOI] [PubMed] [Google Scholar]
- 88.Gomez SL, Le GM, Clarke CA, Glaser SL, France AM, West DW. Cancer incidence patterns in Koreans in the US and in Kangwha, South Korea. Cancer Causes Control. 2003;14:167–174. doi: 10.1023/A:1023046121214. [DOI] [PubMed] [Google Scholar]
- 89.Stellman SD, Wang QS. Cancer mortality in Chinese immigrants to New York City. Comparison with Chinese in Tianjin and with United States-born whites. Cancer. 1994;73:1270–1275. doi: 10.1002/1097-0142(19940215)73:4<1270::AID-CNCR2820730423>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 90.Testa U, Castelli G, Pelosi E. Esophageal Cancer: Genomic and molecular characterization, stem cell compartment and clonal evolution. Medicines (Basel) 2017;4:E67. doi: 10.3390/medicines4030067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tomczak K, Czerwinska P, Wiznerowicz M. The Cancer Genome Atlas (TCGA): An immeasurable source of knowledge. Contemp Oncol (Pozn) 2015;19:A68–A77. doi: 10.5114/wo.2014.47136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Agrawal N, Jiao Y, Bettegowda C, Hutfless SM, Wang Y, David S, Cheng Y, Twaddell WS, Latt NL, Shin EJ, et al. Comparative genomic analysis of esophageal adenocarcinoma and squamous cell carcinoma. Cancer Discov. 2012;2:899–905. doi: 10.1158/2159-8290.CD-12-0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Secrier M, Li X, de Silva N, Eldridge MD, Contino G, Bornschein J, MacRae S, Grehan N, O'Donovan M, Miremadi A, et al. Mutational signatures in esophageal adenocarcinoma define etiologically distinct subgroups with therapeutic relevance. Nat Genet. 2016;48:1131–1141. doi: 10.1038/ng.3659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Levine DM, Ek WE, Zhang R, Liu X, Onstad L, Sather C, Lao-Sirieix P, Gammon MD, Corley DA, Shaheen NJ, et al. A genome-wide association study identifies new susceptibility loci for esophageal adenocarcinoma and Barrett's esophagus. Nat Genet. 2013;45:1487–1493. doi: 10.1038/ng.2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sawada G, Niida A, Uchi R, Hirata H, Shimamura T, Suzuki Y, Shiraishi Y, Chiba K, Imoto S, Takahashi Y, et al. Genomic landscape of esophageal squamous cell carcinoma in a Japanese population. Gastroenterology. 2016;150:1171–1182. doi: 10.1053/j.gastro.2016.01.035. [DOI] [PubMed] [Google Scholar]
- 96.Chang J, Tan W, Ling Z, Xi R, Shao M, Chen M, Luo Y, Zhao Y, Liu Y, Huang X, et al. Genomic analysis of oesophageal squamous-cell carcinoma identifies alcohol drinking-related mutation signature and genomic alterations. Nat Commun. 2017;8:15290. doi: 10.1038/ncomms15290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Manolio TA. Genomewide association studies and assessment of the risk of disease. N Engl J Med. 2010;363:166–176. doi: 10.1056/NEJMra0905980. [DOI] [PubMed] [Google Scholar]
- 98.Zhang J, Bowers J, Liu L, Wei S, Gowda GA, Hammoud Z, Raftery D. Esophageal cancer metabolite biomarkers detected by LC-MS and NMR methods. PLoS One. 2012;7:e30181. doi: 10.1371/journal.pone.0030181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bye H, Prescott NJ, Matejcic M, Rose E, Lewis CM, Parker MI, Mathew CG. Population-specific genetic associations with oesophageal squamous cell carcinoma in South Africa. Carcinogenesis. 2011;32:1855–1861. doi: 10.1093/carcin/bgr211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lao-Sirieix P, Caldas C, Fitzgerald RC. Genetic predisposition to gastro-oesophageal cancer. Curr Opin Genet Dev. 2010;20:210–217. doi: 10.1016/j.gde.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 101.Abnet CC, Freedman ND, Hu N, Wang Z, Yu K, Shu XO, Yuan JM, Zheng W, Dawsey SM, Dong LM, et al. A shared susceptibility locus in PLCE1 at 10q23 for gastric adenocarcinoma and esophageal squamous cell carcinoma. Nat Genet. 2010;42:764–767. doi: 10.1038/ng.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cui R, Kamatani Y, Takahashi A, Usami M, Hosono N, Kawaguchi T, Tsunoda T, Kamatani N, Kubo M, Nakamura Y, Matsuda K. Functional variants in ADH1B and ALDH2 coupled with alcohol and smoking synergistically enhance esophageal cancer risk. Gastroenterology. 2009;137:1768–1775. doi: 10.1053/j.gastro.2009.07.070. [DOI] [PubMed] [Google Scholar]
- 103.Wang Y, Adachi Y, Imsumran A, Yamamoto H, Piao W, Li H, Ii M, Arimura Y, Park MY, Kim D, et al. Targeting for insulin-like growth factor-I receptor with short hairpin RNA for human digestive/gastrointestinal cancers. J Gastroenterol. 2010;45:159–170. doi: 10.1007/s00535-009-0151-6. [DOI] [PubMed] [Google Scholar]
- 104.Wu C, Hu Z, He Z, Jia W, Wang F, Zhou Y, Liu Z, Zhan Q, Liu Y, Yu D, et al. Genome-wide association study identifies three new susceptibility loci for esophageal squamous-cell carcinoma in Chinese populations. Nat Genet. 2011;43:679–684. doi: 10.1038/ng.849. [DOI] [PubMed] [Google Scholar]
- 105.Abnet CC, Wang Z, Song X, Hu N, Zhou FY, Freedman ND, Li XM, Yu K, Shu XO, Yuan JM, et al. Genotypic variants at 2q33 and risk of esophageal squamous cell carcinoma in China: A meta-analysis of genome-wide association studies. Hum Mol Genet. 2012;21:2132–2141. doi: 10.1093/hmg/dds029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Moura MA, Bergmann A, Aguiar SS, Thuler LC. The magnitude of the association between smoking and the risk of developing cancer in Brazil: A multicenter study. BMJ Open. 2014;4:e003736. doi: 10.1136/bmjopen-2013-003736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Postlethwait RW. Carcinoma of the thoracic esophagus. Surg Clin North Am. 1983;63:933–940. doi: 10.1016/S0039-6109(16)43094-X. [DOI] [PubMed] [Google Scholar]
- 108.Mandard AM, Chasle J, Marnay J, Villedieu B, Bianco C, Roussel A, Elie H, Vernhes JC. Autopsy findings in 111 cases of esophageal cancer. Cancer. 1981;48:329–335. doi: 10.1002/1097-0142(19810715)48:2<329::AID-CNCR2820480219>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 109.Quint LE, Hepburn LM, Francis IR, Whyte RI, Orringer MB. Incidence and distribution of distant metastases from newly diagnosed esophageal carcinoma. Cancer. 1995;76:1120–1125. doi: 10.1002/1097-0142(19951001)76:7<1120::AID-CNCR2820760704>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 110.Mao WM, Zheng WH, Ling ZQ. Epidemiologic risk factors for esophageal cancer development. Asian Pac J Cancer Prev. 2011;12:2461–2466. [PubMed] [Google Scholar]
- 111.Lambert R. Endoscopy in screening for digestive cancer. World J Gastrointest Endosc. 2012;4:518–525. doi: 10.4253/wjge.v4.i12.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Dawsey SM, Wang GQ, Weinstein WM, Lewin KJ, Liu FS, Wiggett S, Nieberg RK, Li JY, Taylor PR. Squamous dysplasia and early esophageal cancer in the Linxian region of China: Distinctive endoscopic lesions. Gastroenterology. 1993;105:1333–1340. doi: 10.1016/0016-5085(93)90137-2. [DOI] [PubMed] [Google Scholar]
- 113.Roth MJ, Liu SF, Dawsey SM, Zhou B, Copeland C, Wang GQ, Solomon D, Baker SG, Giffen CA, Taylor PR. Cytologic detection of esophageal squamous cell carcinoma and precursor lesions using balloon and sponge samplers in asymptomatic adults in Linxian, China. Cancer. 1997;80:2047–2059. doi: 10.1002/(SICI)1097-0142(19971201)80:11<2047::AID-CNCR3>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 114.Shen O, Liu SF, Dawsey SM, Cao J, Zhou B, Wang DY, Cao SG, Zhao HZ, Li GY, Taylor PR, et al. Cytologic screening for esophageal cancer: Results from 12,877 subjects from a high-risk population in China. Int J Cancer. 1993;54:185–188. doi: 10.1002/ijc.2910540204. [DOI] [PubMed] [Google Scholar]
- 115.Shu YJ. Cytopathology of the esophagus. An overview of esophageal cytopathology in China. Acta Cytol. 1983;27:7–16. [PubMed] [Google Scholar]
- 116.Pan QJ, Roth MJ, Guo HQ, Kochman ML, Wang GQ, Henry M, Wei WQ, Giffen CA, Lu N, Abnet CC, et al. Cytologic detection of esophageal squamous cell carcinoma and its precursor lesions using balloon samplers and liquid-based cytology in asymptomatic adults in Llinxian, China. Acta Cytol. 2008;52:14–23. doi: 10.1159/000325430. [DOI] [PubMed] [Google Scholar]
- 117.Qin DX, Wang GQ, Yuan FL, Tang MZ, Li MS, Zhang ZL. Screening for upper digestive tract cancer with an occult blood bead detector. Investigation of a normal north China population. Cancer. 1988;62:1030–1034. doi: 10.1002/1097-0142(19880901)62:5<1030::AID-CNCR2820620533>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 118.Qin DX, Wang GQ, Zuo JH, Zhang XH, Yuan FL, Li MS, Wu CR, Ju CL. Screening of esophageal and gastric cancer by occult blood bead detector. Cancer. 1993;71:216–218. doi: 10.1002/1097-0142(19930101)71:1<216::AID-CNCR2820710133>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 119.Dawsey SM, Lewin KJ, Liu FS, Wang GQ, Shen Q. Esophageal morphology from Linxian, China. Squamous histologic findings in 754 patients. Cancer. 1994;73:2027–2037. doi: 10.1002/1097-0142(19940415)73:8<2027::AID-CNCR2820730803>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 120.Dawsey SM, Fleischer DE, Wang GQ, Zhou B, Kidwell JA, Lu N, Lewin KJ, Roth MJ, Tio TL, Taylor PR. Mucosal iodine staining improves endoscopic visualization of squamous dysplasia and squamous cell carcinoma of the esophagus in Linxian, China. Cancer. 1998;83:220–231. doi: 10.1002/(SICI)1097-0142(19980715)83:2<220::AID-CNCR4>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 121.Muto M, Minashi K, Yano T, Saito Y, Oda I, Nonaka S, Omori T, Sugiura H, Goda K, Kaise M, et al. Early detection of superficial squamous cell carcinoma in the head and neck region and esophagus by narrow band imaging: A multicenter randomized controlled trial. J Clin Oncol. 2010;28:1566–1572. doi: 10.1200/JCO.2009.25.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wei WQ, Chen ZF, He YT, Feng H, Hou J, Lin DM, Li XQ, Guo CL, Li SS, Wang GQ, et al. Long-Term Follow-up of a community assignment, One-time endoscopic screening study of esophageal cancer in China. J Clin Oncol. 2015;33:1951–1957. doi: 10.1200/JCO.2014.58.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Feng JF, Huang Y, Lu WS, Chen QX. Preoperative platelet count in esophageal squamous cell carcinoma: Is it a prognostic factor? Langenbeck's Arch Surg. 2013;398:1115–1122. doi: 10.1007/s00423-013-1111-4. [DOI] [PubMed] [Google Scholar]
- 124.Almhanna K, Meredith KL, Hoffe SE, Shridhar R, Coppola D. Targeting the human epidermal growth factor receptor 2 in esophageal cancer. Cancer Control. 2013;20:111–116. doi: 10.1177/107327481302000204. [DOI] [PubMed] [Google Scholar]
- 125.Ying J, Zhang M, Qiu X, Lu Y. The potential of herb medicines in the treatment of esophageal cancer. Biomed Pharmacotherapy. 2018;103:381–390. doi: 10.1016/j.biopha.2018.04.088. [DOI] [PubMed] [Google Scholar]
- 126.Krasna MJ. Stage-specific therapy for cancer of the oesophagus: A new ‘cancer of the elderly’. Drugs Aging. 2009;26:185–194. doi: 10.2165/00002512-200926030-00001. [DOI] [PubMed] [Google Scholar]
- 127.Hagen JA, DeMeester SR, Peters JH, Chandrasoma P, DeMeester TR. Curative resection for esophageal adenocarcinoma: Analysis of 100 en bloc esophagectomies. Ann Surg. 2001;234:520–531. doi: 10.1097/00000658-200110000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Pennathur A, Luketich JD. Resection for esophageal cancer: Strategies for optimal management. Ann Thoracic Surg. 2008;85(Suppl):S751–S756. doi: 10.1016/j.athoracsur.2007.11.078. [DOI] [PubMed] [Google Scholar]
- 129.Pennathur A, Zhang J, Chen H, Luketich JD. The ‘best operation’ for esophageal cancer? Ann Thorac Surg. 2010;89(Suppl):S2163–S2167. doi: 10.1016/j.athoracsur.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nishihira T, Hirayama K, Mori S. A prospective randomized trial of extended cervical and superior mediastinal lymphadenectomy for carcinoma of the thoracic esophagus. Am J Surg. 1998;175:47–51. doi: 10.1016/S0002-9610(97)00227-4. [DOI] [PubMed] [Google Scholar]
- 131.Birkmeyer JD, Sun Y, Goldfaden A, Birkmeyer NJ, Stukel TA. Volume and process of care in high-risk cancer surgery. Cancer. 2006;106:2476–2481. doi: 10.1002/cncr.21888. [DOI] [PubMed] [Google Scholar]
- 132.Mimura K, Yamada L, Ujiie D, Hayase S, Tada T, Hanayama H, Thar Min AK, Shibata M, Momma T, Saze Z, et al. Immunotherapy for esophageal squamous cell carcinoma: A review. Fukushima J Med Sci. 2018;64:46–53. doi: 10.5387/fms.2018-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vrana D, Matzenauer M, Neoral Č, Aujeský R, Vrba R, Melichar B, Rušarová N, Bartoušková M, Jankowski J. From Tumor immunology to immunotherapy in gastric and esophageal cancer. Int J Mol Sci. 2018;20:E13. doi: 10.3390/ijms20010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pennathur A, Luketich JD, Landreneau RJ, Ward J, Christie NA, Gibson MK, Schuchert M, Cooper K, Land SR, Belani CP. Long-term results of a phase II trial of neoadjuvant chemotherapy followed by esophagectomy for locally advanced esophageal neoplasm. Ann Thorac Surg. 2008;85:1930–1937. doi: 10.1016/j.athoracsur.2008.01.097. [DOI] [PubMed] [Google Scholar]
- 135.Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, Scarffe JH, Lofts FJ, Falk SJ, Iveson TJ, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355:11–20. doi: 10.1056/NEJMoa055531. [DOI] [PubMed] [Google Scholar]
- 136.Tepper J, Krasna MJ, Niedzwiecki D, Hollis D, Reed CE, Goldberg R, Kiel K, Willett C, Sugarbaker D, Mayer R. Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol. 2008;26:1086–1092. doi: 10.1200/JCO.2007.12.9593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Walsh TN, Noonan N, Hollywood D, Kelly A, Keeling N, Hennessy TP. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med. 1996;335:462–467. doi: 10.1056/NEJM199608153350702. [DOI] [PubMed] [Google Scholar]
- 138.Ando N, Iizuka T, Ide H, Ishida K, Shinoda M, Nishimaki T, Takiyama W, Watanabe H, Isono K, Aoyama N, et al. Surgery plus chemotherapy compared with surgery alone for localized squamous cell carcinoma of the thoracic esophagus: A Japan Clinical Oncology Group Study-JCOG9204. J Clin Oncol. 2003;21:4592–4596. doi: 10.1200/JCO.2003.12.095. [DOI] [PubMed] [Google Scholar]
- 139.Ando N, Ozawa S, Kitagawa Y, Takeuchi H, Kitajima M. Salvage surgery for the T4 esophageal cancer following downstaging by neoadjuvant chemoradiotherapy. Nihon Geka Gakkai Zasshi. 1997;98:767–772. (In Japanese) [PubMed] [Google Scholar]
- 140.Armanios M, Xu R, Forastiere AA, Haller DG, Kugler JW, Benson AB, III, Eastern Cooperative Oncology Group Adjuvant chemotherapy for resected adenocarcinoma of the esophagus, gastro-esophageal junction, and cardia: Phase II trial (E8296) of the Eastern Cooperative Oncology Group. J Clin Oncol. 2004;22:4495–4499. doi: 10.1200/JCO.2004.06.533. [DOI] [PubMed] [Google Scholar]
- 141.Kleinberg L, Forastiere AA. Chemoradiation in the management of esophageal cancer. J Clin Oncol. 2007;25:4110–4117. doi: 10.1200/JCO.2007.12.0881. [DOI] [PubMed] [Google Scholar]
- 142.Stahl M, Wilke H, Stuschke M, Walz MK, Fink U, Molls M, Siewert JR, Schroeder M, Makoski HB, Schmidt U, et al. Clinical response to induction chemotherapy predicts local control and long-term survival in multimodal treatment of patients with locally advanced esophageal cancer. J Cancer Res Clin Oncol. 2005;131:67–72. doi: 10.1007/s00432-004-0604-5. [DOI] [PubMed] [Google Scholar]
- 143.Polednak AP. Trends in survival for both histologic types of esophageal cancer in US surveillance, epidemiology and end results areas. Int J Cancer. 2003;105:98–100. doi: 10.1002/ijc.11029. [DOI] [PubMed] [Google Scholar]
- 144.Homs MY, Steyerberg EW, Eijkenboom WM, Siersema PD. Predictors of outcome of single-dose brachytherapy for the palliation of dysphagia from esophageal cancer. Brachytherapy. 2006;5:41–48. doi: 10.1016/j.brachy.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 145.Shah MA, Ramanathan RK, Ilson DH, Levnor A, D'Adamo D, O'Reilly E, Tse A, Trocola R, Schwartz L, Capanu M, et al. Multicenter phase II study of irinotecan, cisplatin, and bevacizumab in patients with metastatic gastric or gastroesophageal junction adenocarcinoma. J Clin Oncol. 2006;24:5201–5206. doi: 10.1200/jco.2006.24.18_suppl.4020. [DOI] [PubMed] [Google Scholar]
- 146.Batouli A, Jahanshahi P, Gross CP, Makarov DV, Yu JB. The global cancer divide: Relationships between national healthcare resources and cancer outcomes in high-income vs. middle- and low-income countries. J Epidemiol Glob Health. 2014;4:115–124. doi: 10.1016/j.jegh.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.