Abstract
Background:
Cardiovascular disease is linked to cognitive decline and disorders (e.g., dementia). The evidence is based largely on older non-Latino White cohorts.
Objective:
Examine the association between global vascular risk and cognitive function among Hispanics/Latinos in the United States.
Methods:
We used data from a large sample of stroke- and cardiovascular disease-free, middle-aged and older Hispanics/Latinos with diverse backgrounds (n=7,650) from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). We compared associations between two measures of cardiovascular risk (CVR), the Framingham Cardiovascular Risk Score (FCRS) and the multiethnic Global Vascular Risk Score (GVRS), and cognitive performance using measures of global and domain specific cognitive function, and tested for modification by sex and age.
Results:
Higher FCRS and GVRS were associated with lower global cognition and higher probability of low mental status, after covariates adjustment. Both CVR indices were associated with lower performances in learning and memory, verbal fluency, and psychomotor speed. Higher GVRS presented stronger associations with lower cognitive function compared to the FCRS. Women and younger age (45–64 years) exhibited more pronounced associations between higher CVR and worse cognition, particularly so with the GVRS.
Discussion:
CVR is also a risk for compromised cognitive function and evident in middle-age among Hispanics/Latinos. The multiethnic GVRS, tailored to specific risks based on racial/ethnic background, is feasible to use in primary care settings and can provide important insight on cognitive risk. Even modest shifts in population toward cardiovascular health in the high-risk Hispanic/Latino population can have important positive impacts on healthy cognitive aging.
Keywords: Cardiovascular risk, cognition, HCHS/SOL, Hispanics/Latinos, neuroepidemiology, neuropsychology
INTRODUCTION
By 2060 nearly 30% of the U.S. population will be Hispanic/Latino and only close to 45% will be non-Hispanic white [1]. Recent analyses by the Center for Disease Control suggests that the largest growth in Alzheimer’s disease and related dementias (ADRD), by 2060 (versus 2014), will be among Hispanics/Latinos (7.5-fold compared to 90% among non-Hispanic white) [2]. These statistics highlight the critical need for studying Hispanic/Latino populations. Compromised vascular health evokes a cascade of pathologies linked to cognitive decline, and cognitive disorders such as dementia in older age [3, 4]. Most of the evidence is based on older non-Latino Whites.
Hispanic/Latino (interchangeably used with Latino) studies on the association between cardiovascular disease (CVD) and cognition have included limited Latino groups (e.g., Dominicans). Furthermore, existing cohorts of Latino subgroups show notable variations in cognitive function and prevalence and incidence of dementias [5]. These select cohorts provided mixed evidence on the associations between vascular risk factors (e.g., diabetes) and cognitive function and disorders [6, 7]. More recently, studies using diverse Latinos indicate that cardiovascular health metrics and elevated burden are related to worse cognitive function [8, 9], and that specific cardiovascular risk (CVR) factors (e.g., compromised blood pressure) are associated with cognitive underperformance that is evident even in midlife [10, 11].
CVRs are likely to cluster in individuals [12, 13]. Independent examination of individual factors (e.g., obesity) can mask the overall impact of CVR on cognition. Composite risk indicators, such as the Framingham Cardiovascular Risk Score (FCRS), aggregate important CVR information that have been linked to deficits in cognitive performance, cognitive decline, cerebrovascular disease markers (e.g., blood flow), and dementias in Whites [14–23]. Despite wide adoption, some have challenged the applicability of the FCRS to non-Whites. Recently, a Global Vascular Risk Score (GVRS) that includes several FCRS factors, and other risk factors (e.g., anthropometry) was created and tested in a multiethnic prospective cohort of African Americans, Whites, and Caribbean Latinos (i.e., Dominicans and Puerto Ricans) [24]. The GVRS has been shown to improve prediction of cardiovascular events and stroke in minority populations [25], and was linked to successful aging (i.e., without significant cognitive decline) among older adults [24]. Middle-age Latinos are at high risk for CVD and have a disproportionately high CVD burden as a result of low levels of CVD awareness (e.g., undiagnosed hypertension) and healthcare access [26–30]. Little research to date has examined the association between global cardiovascular profile and cognition in middle-age and older Latinos, and no work has done so in a stroke and CVD event-free population.
In this study, we used data from a large sample of stroke- and CVD event-free middle-aged and older diverse Latinos in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), to examine associations between global vascular risk and cognitive function. Specifically, we examined and compared associations between two CVR measures (FCRS and GVRS) and cognitive performance. We hypothesized that higher CVR will be associated with lower cognitive performance in multiple domains (e.g., memory). We expected the associations to be stronger using the GVRS compared to FCRS, especially in the cognitive domains of verbal fluency and executive function [9, 10, 31]. Additionally, we expected these associations to be more pronounced among women, to be present in both middle-age and older adulthood, particularly for measures of memory and mental status.
METHODS
Data
HCHS/SOL is a multisite, prospective cohort study of 16,415 community-dwelling Hispanic/Latino adults (18–74 years old) from multiple background groups. The HCHS/SOL design was formulated to estimate representative baseline risk factors for overall Hispanics/Latinos as well as for specific backgrounds including Central Americans, Cubans, Dominicans, Mexicans, Puerto Ricans, and South Americans. Data were collected from field centers in four U.S. cities with substantial Hispanic/Latino population concentrations (Bronx, NY; Chicago, IL; Miami, FL; and San Diego, CA). Each field center recruited about 4,000 eligible, self-identified Hispanic/Latino adults. Detailed HCHS/SOL sampling methods have been previously published [32]. We used HCHS/SOL data from participants 45–74 years, with neurocognitive testing data, free of self-reported medical histories of: 1) stroke or transient ischemic attack, CVD events (coronary heart disease, angina, heart attack, heart failure, atrial fibrillation, and rheumatic heart disease), and without missing values for the primary exposures or the model covariables (n=7,650). Written informed consent was obtained from all included participants, and the study was reviewed and approved by the Institutional Review Boards of all participating institutions.
Cognitive outcomes included: 1) a global cognitive measure, based on a factor score generated using a confirmatory factor analysis of the cognitive tests available in HCHS/SOL (the Brief-Spanish English Verbal Learning Test sum of trials and recall, the Word Fluency (WF), and the Digit Symbol Substitution (DSS) test; and 2) high and low mental status based on the Six-Item Screener (SIS). The SIS (range 0–6) is a mental status test that was scored dichotomously with a value of 4 or lower representing “cognitive impairment” (herein referred to as low mental status). The cut-point reflects previous validation work in patients with dementia [33]. In secondary analyses, we also considered the 4-cognitive continuous cognitive tests modeled independently. The B-SEVLT is an episodic learning and memory test with two scores: 1) the summed total of correctly learned items across three learning trials (B-SEVLT-sum; range 0–45), and 2) total correctly recalled items (B-SEVLT recall; range 0–15) following an interference trial. The WF is a phonemic verbal fluency test scored as the total number of correctly generated words within 1 minute for the letters F and A. The DSS is a mental processing speed and executive function exam (range 0–90). These cognitive tests and scoring procedures have been previously described [34]. A detailed characterization and discussion of these tests as applied to HCHS/SOL data is available elsewhere [35]. All continuous measures were z-score transformed [(Score-Mean)/Standard Deviation (SD); using the tests’ probability weighted means and SDs] to facilitate score comparisons across tests using a common metric.
Primary exposures included two composite CVR measures, the FCRS and GVRS. The FCRS is coded according to the Framingham study’s published criteria, using sex-specific equations incorporating age, total cholesterol, HDL cholesterol, systolic blood pressure and blood pressure treatment, smoking, and diabetes status [36]. The GVRS was constructed following previously published criteria based on data from the multiethnic Northern Manhattan Aging Study (NOMAS). The GVRS enriches the traditional Framingham score by using alternative functional forms of the traditional factors, and by adding anthropometric indicators (e.g., waist circumference), health behaviors (e.g., subjective physical activity levels based on the Global Physical Activity Questionnaire and moderate alcohol consumption), and peripheral vascular disease. A detailed description of the GVRS algorithm and component measures is published elsewhere [25]. Both the GVRS and FCRS yield probability estimates for 10-year CVD events. The probability values for both the FCRS and GVRS were multiplied by 100 to allow interpretation on a percentile scale. The distributions of the FCRS and GVRS and a scatter plot with a linear fit line representing their crude association are presented in Supplementary Figure 1.
Covariables in multiple regression models we included education (less than high school (<12 years, 12 years, and >12 years), Latino background, depressive symptoms (Center for Epidemiologic Studies Depression-10; CESD-10) score, and Field Center. We do not adjust for age and sex since these variables are included in the risk prediction models for both the FCRS and the GVRS. However, we do test for age group and sex modifications.
Analytic strategy
Our analyses were conducted in three steps. First, we generated descriptive statistics for the HCHS/SOL subpopulation of interest and by Hispanic/Latino background to provide detailed characteristics of the diversity of Latinos in the target population (Table 1). We used survey adjusted chi-squared tests (for categorical variables) and t-tests (for continuous variables) to examine and test variations by covariates of interests. Second, we sequentially fit survey generalized linear regression models (linear for the global cognitive measure and logistic for the mental status outcome) to model the associations between the CVR exposures and cognitive performance. In each case, we fit two models to determine the 1) crude, and 2) fully adjusted coefficients/odds ratios and standard errors/95% confidence intervals (CI; Table 2). To facilitate the interpretation of these associations we estimated and plotted the unadjusted and fully adjusted marginal cognitive performance means/probabilities (average marginal effects, AMEs) [37, 38] and their 95% CI across the CVR continua (Fig. 1). By doing so we are able to visualize the predicted average cognitive function for the target population at different values of the primary exposures (in this case the CVR scores under consideration) [39]. Estimating and plotting adjusted AMEs allows us to compare cognitive performance at prespecified values of the CVR scores continua while holding other target population characteristics, as specified in the regression model, constant [37, 39]. By plotting the crude and adjusted estimates, we are able to assess the attenuation in the associations between the CVR scores and cognitive performance resulting from adjustment for the covariates. Third, we refit the fully adjusted models while independently including interactions between both sex and a dichotomized age indicator (45–64 years; 65 + years) and the vascular risk scores to test for the hypothesized sex and age modifications (Table 3). As with step above, we estimated and plotted the marginal cognitive scores means/probabilities (AMEs) and their 95% CI by sex (Fig. 2) and age (Fig. 3) groups across the vascular risk continua. In secondary analyses the survey linear regression models were fit following step 2 and 3 above for each of the cognitive tests, independently. In sensitivity analyses, we investigated the possibility of non-linear associations between the risk scores (the FCRS and GVRS, independently) and cognitive function. We considered several polynomial forms and linear splines but found no evidence for non-linear associations in our data (available from authors). Additionally, we refit all the above specified regression models using categorical versions of the risk scores that classified individuals into low (0–<10%), intermediate (10–<20%), and high (20%+) risk. The results were qualitatively equivalent to the main findings (see Supplementary Table 1 and plotted in Supplementary Figure 2).
Table 1.
Descriptive statistics to characterize the covariates and cognitive outcomes of the HCHS/SOL target population by Hispanic/Latino background
| Dominican | CA | Cuban | Mexican | PR | SA | Other | Overall | |
|---|---|---|---|---|---|---|---|---|
| % (SE) | ||||||||
| Age 65 + y* | 13.25 (2.11) | 14.41 (2.07) | 27.00 (1.99) | 14.11 (1.20) | 21.12 (2.35) | 18.26 (2.65) | 15.90 (5.01) | 19.01 (0.83) |
| Female* | 61.34 (2.42) | 63.19 (2.39) | 49.67 (1.46) | 57.91 (1.42) | 54.41 (1.93) | 59.83 (2.61) | 48.05 (5.60) | 55.65 (0.76) |
| Education (y) * | ||||||||
| <12 | 47.70 (2.49) | 42.41 (2.38) | 26.30 (1.49) | 47.15 (2.02) | 43.06 (2.55) | 24.22 (2.72) | 22.83 (4.41) | 38.67 (1.02) |
| 12 | 18.84 (1.93) | 19.94 (1.82) | 25.47 (1.67) | 17.90 (1.11) | 22.43 (1.64) | 25.40 (2.57) | 17.91 (4.97) | 21.38 (0.74) |
| >12 | 33.45 (2.38) | 37.65 (2.28) | 48.23 (1.66) | 34.95 (1.92) | 34.51 (2.39) | 50.37 (2.94) | 59.26 (5.48) | 39.95 (0.97) |
| Field center* | ||||||||
| Bronx | 90.96 (1.77) | 16.39 (2.83) | 1.27 (0.31) | 3.85 (1.26) | 70.50 (2.51) | 25.32 (3.09) | 26.23 (4.43) | 24.28 (1.57) |
| Chicago | 1.14 (0.37) | 13.92 (1.83) | 0.65 (0.23) | 21.51 (1.81) | 20.65 (2.06) | 16.98 (2.15) | 9.10 (2.68) | 12.79 (0.88) |
| Miami | 6.69 (1.51) | 65.33 (3.50) | 97.95 (0.42) | 0.98 (0.37) | 6.37 (1.30) | 53.38 (3.60) | 43.94 (5.67) | 37.27 (2.46) |
| San Diego | 1.21 (0.85) | 4.36 (1.17) | 0.12 (0.08) | 73.66 (2.20) | 2.48 (1.00) | 4.31 (1.42) | 20.73 (4.64) | 25.67 (1.87) |
| Six item screener* | ||||||||
| Low mental status (SIS≤4) | 23.53 (2.25) | 10.70 (1.16) | 11.37 (0.86) | 12.15 (0.99) | 21.60 (2.05) | 11.68 (1.78) | 13.78 (3.67) | 14.40 (0.61) |
| Mean [SD] | ||||||||
| Age (y)* | 54.87 [8.85] | 54.96 [11.04] | 57.39 [8.23] | 54.87 [10.09] | 56.69 [10.02] | 55.74 [10.73] | 55.05 [9.96] | 55.92 [9.85] |
| CESD-10* | 7.18 [7.12] | 6.75 [8.93] | 7.47 [6.66] | 6.39 [7.23] | 9.22 [8.42] | 6.55 [7.96] | 6.98 [8.36] | 7.26 [7.75] |
| B-SEVLT recall* | 7.78 [3.56] | 8.69 [4.08] | 7.83 [2.51] | 8.86 [3.78] | 7.29 [3.84] | 8.81 [3.71] | 9.26 [3.64] | 8.22 [3.55] |
| B-SEVLT sum* | 22.78 [6.21] | 23.30 [8.31] | 21.80 [5.28] | 23.59 [7.59] | 21.14 [7.20] | 23.99 [7.22] | 25.34 [7.00] | 22.67 [6.98] |
| WF* | 16.22 [8.21] | 18.08 [10.50] | 17.54 [6.39] | 19.79 [10.33] | 17.90 [9.03] | 20.61 [9.69] | 20.08 [9.12] | 18.50 [8.99] |
| DSS* | 27.15 [13.81] | 29.87 [18.78] | 33.56 [11.89] | 37.18 [18.69] | 35.72 [16.47] | 36.12 [17.12] | 40.60 [16.00] | 34.59 [16.49] |
| Global cognition* | −0.30 [0.88] | −0.08 [1.18] | −0.06 [0.74] | 0.26 [1.17] | −0.01 [1.04] | 0.27 [1.03] | 0.44 [1.02] | 0.06 [1.03] |
Differences between groups based on survey adjusted F-tests is significant at p < 0.001; SE, standard error; SD, standard deviation; CA, Central American; PR, Puerto Rican; SA, South American; LTHS, less than high school; MTHS, more than high school; Global Cognition, Composite factor score; SIS, Six-item screener; B-SEVLT, Spanish English verbal learning test; WF, word fluency; DSS, digit symbol substitution; BMI, body mass index; CESD, Center for Epidemiologic Studies Depression Scale (CESD-10).
Table 2.
Associations between cardiovascular risk scores and cognitive function (z-scores for continuous outcomes). Results are derived from survey generalized linear models. Results for Hispanic/Latino adults ages 45–74 years without prevalent stroke or cardiovascular events (HCHS/SOL; 2008–2011)
| Primary outcomes | ||
| M1 GC | M2 GC | |
| β (se) | β (se) | |
| FCRS | −0.019*** (0.001) | −0.014*** (0.001) |
| GVRS | −0.042*** (0.002) | −0.031*** (0.002) |
| M1 SIS ≤ 4 OR/95% CI |
M3 SIS ≤ 4 OR/95% CI |
|
| FCRS | 1.021*** [1.016;1.026] | 1.021*** [1.015;1.026] |
| GVRS | 1.052*** [1.037;1.066] | 1.048*** [1.032;1.064] |
| Secondary Outcomes | ||
| M1 SEVLT Recall β (se) |
M3 SEVLT Recall β (se) |
|
| FCRS | −0.015*** (0.001) | −0.012*** (0.001) |
| GVRS | −0.031*** (0.002) | −0.023*** (0.002) |
| M1 SEVLT Sum β (se) |
M3 SEVLT Sum β (se) |
|
| FCRS | −0.016*** (0.001) | −0.014*** (0.001) |
| GVRS | −0.034*** (0.002) | −0.025*** (0.002) |
| M1 WF β (se) |
M3 WF β (se) |
|
| FCRS | −0.009*** (0.001) | −0.006*** (0.001) |
| GVRS | −0.021*** (0.002) | −0.012*** (0.002) |
| M1 DSS β (se) |
M3 DSS β (se) |
|
| FCRS | −0.017*** (0.001) | −0.014*** (0.001) |
| GVRS | −0.043*** (0.002) | −0.034*** (0.002) |
FCRS, Framingham Cardiovascular Risk Score; GVRS, Global Vascular Risk Score.;
p<0.001;
p<0.01;
p<0.05;
Global Cognition (GC), Composite factor score; SIS, Six-item Screener; SEVLT, Spanish English verbal learning test; WF, word fluency; DSS, digit symbol substitution.; M1 = Crude; M2 = adjusted for education, Hispanic/Latino background, CESD-10, and study site adjustments.
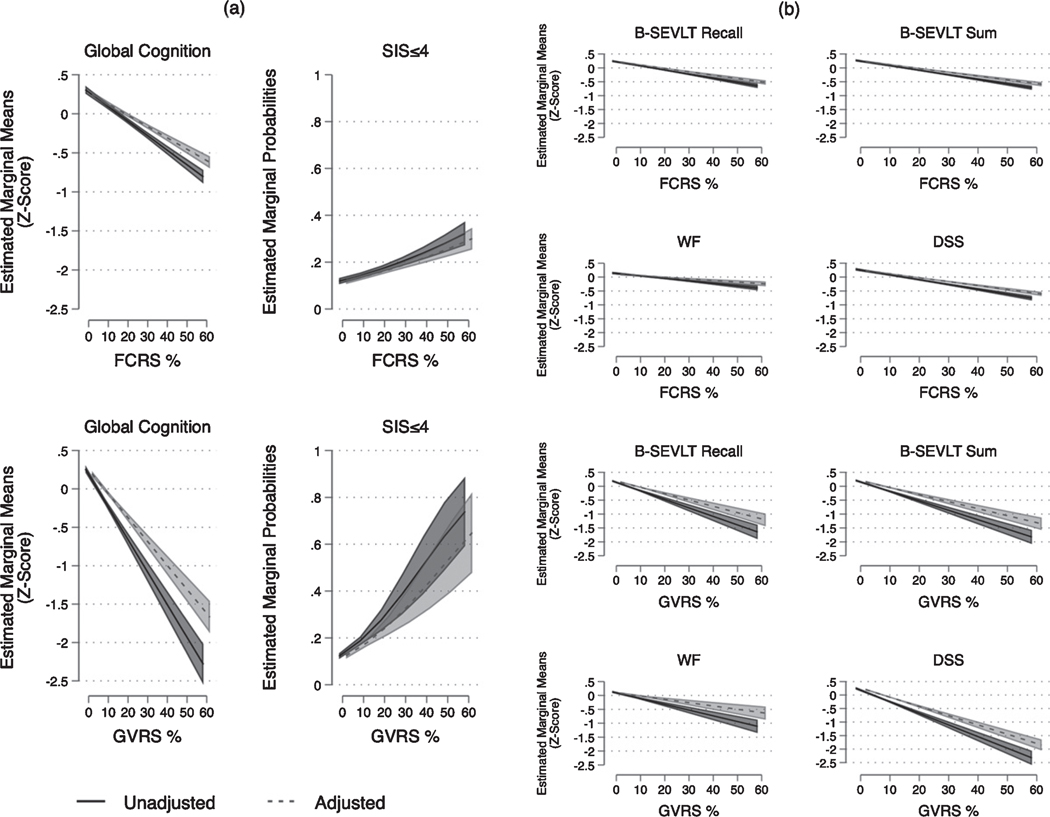
Fig. 1.
Estimated marginal means/probabilities (Average Marginal Effects; AMEs) and 95% confidence intervals for the associations between cardiovascular risk scores and cognitive function (z-scores for continuous outcomes). Results are derived from survey generalized linear models. Results for Hispanic/Latino adults ages 45–74 years without prevalent stroke or cardiovascular events (HCHS/SOL; 2008–2011). FCRS, Framingham Cardiovascular Risk Score; GVRS, Global Vascular Risk Score; Global Cognition, Composite factor score; SIS, Six-item Screener; SEVLT, Spanish English verbal learning test; WF, word fluency; DSS, digit symbol substitution. Adjusted includes education, Hispanic/Latino background, CESD-10, and study site adjustments. (a) Global cognitive outcomes (b) Domain specific cognitive function.
Table 3.
Sex and age modifications in the associations between cardiovascular risk scores and cognitive function (z-scores for continuous outcomes). Results are derived from survey generalized linear models. Results for Hispanic/Latino adults ages 45–74 years without prevalent stroke or cardiovascular events (HCHS/SOL; 2008–2011)
| ΔSlope* | 95% CI |
p | ||
|---|---|---|---|---|
| LL | UL | |||
| Sex modification | ||||
| Female versus Male* | ||||
| Contrasts | ||||
| FCRS | ||||
| Primary Outcomes | ||||
| Global Cognition | 0.009 | 0.006 | 0.013 | 0.000 |
| SIS≤4 | −0.002 | −0.004 | 0.000 | 0.011 |
| Secondary Outcomes | ||||
| SEVLT-Recall | 0.006 | 0.002 | 0.009 | 0.002 |
| SEVLT-Sum | 0.007 | 0.004 | 0.011 | 0.000 |
| WF | 0.005 | 0.002 | 0.009 | 0.003 |
| DSS | 0.009 | 0.006 | 0.012 | 0.000 |
| GVRS | ||||
| Primary Outcomes | ||||
| Global Cognition | 0.023 | 0.015 | 0.031 | 0.000 |
| SIS≤4 | −0.005 | −0.008 | −0.001 | 0.011 |
| Secondary Outcomes | ||||
| SEVLT-Recall | 0.017 | 0.008 | 0.025 | 0.000 |
| SEVLT-Sum | 0.015 | 0.007 | 0.023 | 0.000 |
| WF | 0.012 | 0.004 | 0.020 | 0.005 |
| DSS | 0.023 | 0.015 | 0.031 | 0.000 |
| Age modification | ||||
| Age 45–64 versus 65+* Contrasts | ||||
| FCRS | ||||
| Primary Outcomes | ||||
| Global Cognition | 0.006 | 0.002 | 0.010 | 0.001 |
| SIS≤4 | 0.000 | −0.002 | 0.002 | 0.738 |
| Secondary Outcomes | ||||
| SEVLT-Recall | 0.003 | −0.001 | 0.007 | 0.109 |
| SEVLT-Sum | 0.003 | 0.000 | 0.007 | 0.063 |
| WF | 0.000 | −0.005 | 0.004 | 0.889 |
| DSS | 0.009 | 0.006 | 0.013 | <0.001 |
| GVRS | ||||
| Primary Outcomes | ||||
| Global Cognition | 0.021 | 0.011 | 0.031 | <0.001 |
| SIS≤4 | −0.004 | −0.009 | 0.001 | 0.091 |
| Secondary Outcomes | ||||
| SEVLT-Recall | 0.016 | 0.007 | 0.026 | 0.001 |
| SEVLT-Sum | 0.013 | 0.002 | 0.023 | 0.015 |
| WF | 0.002 | −0.009 | 0.014 | 0.681 |
| DSS | 0.028 | 0.019 | 0.036 | <0.001 |
FCRS, Framingham Cardiovascular Risk Score; GVRS, Global Vascular Risk Score; Global Cognition, Composite factor score; SIS, Six-item Screener; SEVLT, Spanish English verbal learning test; WF, word fluency; DSS, digit symbol substitution; CI, confidence intervals (LL lower limit; and UL upper limit).; Models are adjusted for education, Hispanic/Latino background, CESD-10, and study site.;
Calculated group differences in slopes (Slope Males – Slope Females; Slope age 65+– Slope age 45–64 years) per 1% increase in cardiovascular risk score.
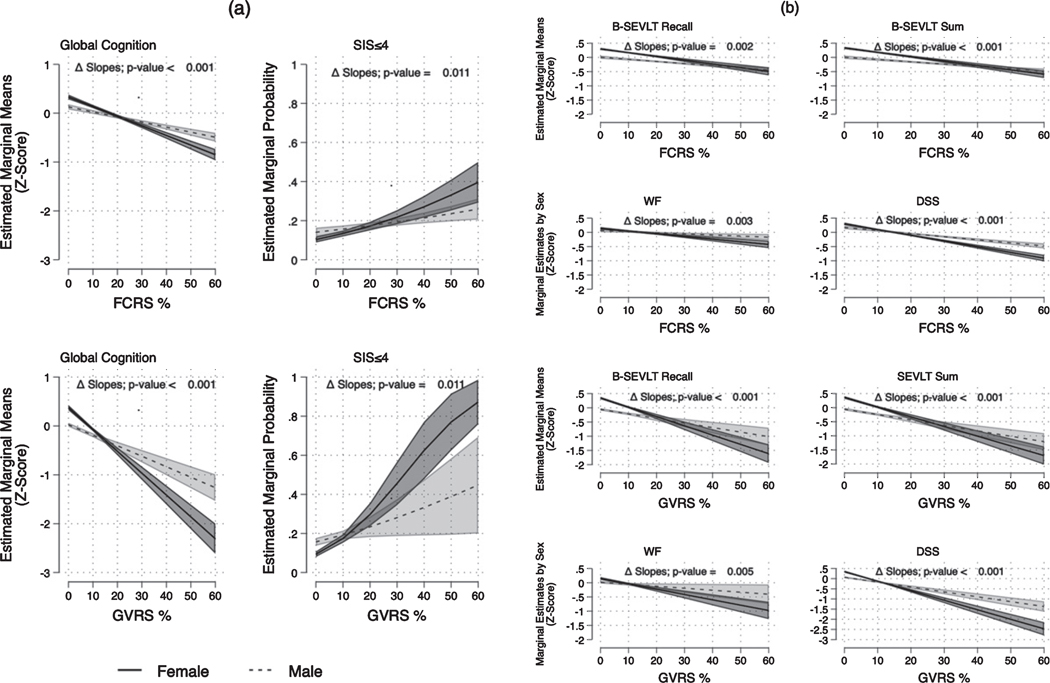
Fig. 2.
Estimated marginal means/probabilities (Average Marginal Effects; AMEs) and 95% confidence intervals for sex modifications in the associations between cardiovascular risk scores and cognitive function (z-scores for continuous outcomes). Results are derived from survey generalized linear models. Results for Hispanic/Latino adults ages 45–74 years without prevalent stroke or cardiovascular events (HCHS/SOL; 2008–2011). FCRS, Framingham Cardiovascular Risk Score; GVRS, Global Vascular Risk Score; Global Cognition, Composite factor score; SIS, Six-item Screener; B-SEVLT, Spanish English verbal learning test; WF, word fluency; DSS, digit symbol substitution. Models are adjusted for education, Hispanic/Latino background, CESD-10, and study site adjustments. (a) Global cognitive outcomes (b) Domain specific cognitive function.
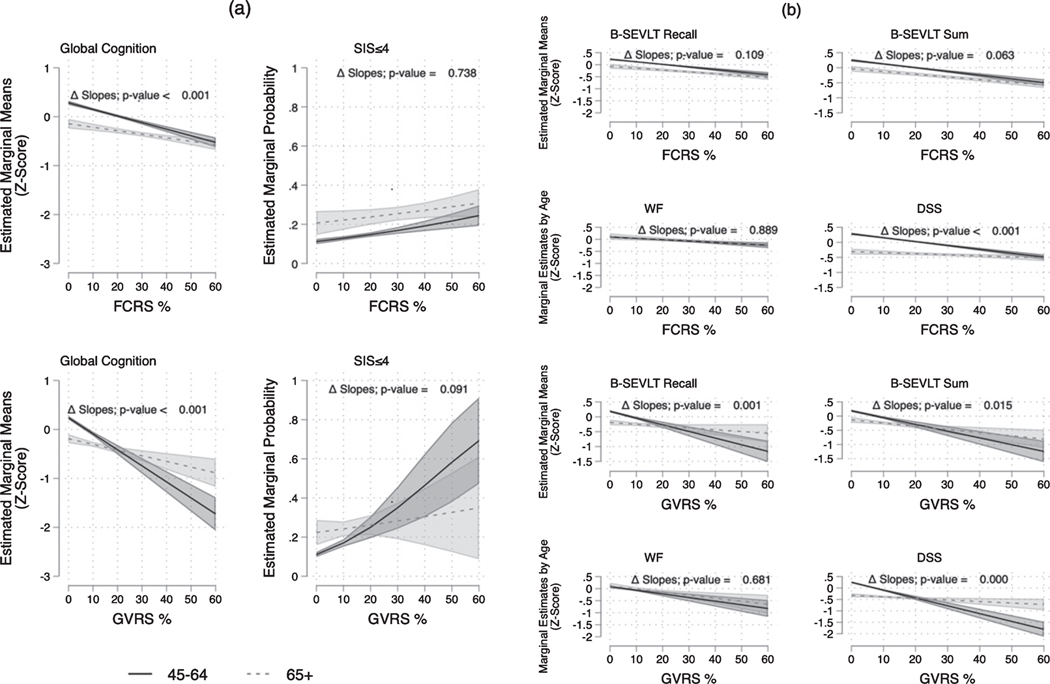
Fig. 3.
Estimated marginal means/probabilities (Average Marginal Effects; AMEs) and 95% confidence intervals for age modifications in the associations between cardiovascular risk scores and cognitive function (z-scores for continuous outcomes). Results are derived from survey generalized linear models. Results for Hispanic/Latino adults ages 45–74 years without prevalent stroke or cardiovascular events (HCHS/SOL; 2008–2011). FCRS, Framingham Cardiovascular Risk Score; GVRS, Global Vascular Risk Score; Global Cognition, Composite factor score; SIS, Six-item Screener; B-SEVLT, Spanish English verbal learning test; WF, word fluency; DSS, digit symbol substitution. Models are adjusted for education, Hispanic/Latino background, CESD-10, and study site adjustments. (a) Global cognitive outcomes (b) Domain specific cognitive function.
We used statistical procedures specific to complex survey sample designs in the Stata software package (15.1) for all study analyses. Specifically, we used Taylor Series Linearization to compute variance estimates and derive adjusted standard errors for statistical inferences [40]. All models accounted for the probability weighting, clustering, and stratification underlying the HCHS/SOL design [32].
RESULTS
Target population characteristics
Survey weighted descriptive characteristics for the HCHS/SOL target population are included in Table 1. About half of the target population was female (55.6%), and its mean age was 56 years (SD=9.9). Two-fifths of the target population (38.7%) had <12 years of education. The average CESD-10 score was 7.3 (SD=7.75; range 0–30). The estimated means for the cognitive tests were: B-SEVLT Sum, 22.7 (SD=7.0), B-SEVLT Recall, 8.2 (SD=3.5), WF, 18.5 (SD=9.0), DSS, 34.6 (SD=16.5). Additionally, 14.4% of the target population satisfied criteria for low mental status on the SIS (≤4). The overall means for FCRS and GVRS were 15.3 (SD=15.9) and 5.75 (SD=7.5), respectively. Latino groups varied significantly on all considered cognitive outcomes, cardiovascular risk measures, and covariates (Table 1).
Crude associations
We found that both the FCRS and GVRS had consistent (1) inverse linear associations with global cognition (βFCRS=−0.019 [SE=0.001] p < 0.001; βGVRS=−0.042 [SE=0.003] p < 0.001; per 1% increase in risk score) and (2) higher odds ratios of low mental status (ORFCRS 1.021 95%CI=1.016–1.026]; −ORGVRS=1.025, 95%CI=1.037–1.066]; p < 0.001 for both) (Table 2). Additionally, both the FCRS and GVRS were negatively linked (Table 2) to all examined domain-specific measures of learning and memory (SEVLT-sum and SEVLT-Recall), verbal fluency (WF), and psychomotor speed and executive function (DSS).
Adjusted associations
Adjusting the regression models for the covariates attenuated the estimated crude association between the FCRS (β--FCRS=−0.014 [SE=0.001] p < 0.001; per 1% increase in risk score) and the GVRS (β—GVRS=−0.031 [SE=0.002] p < 0.001; per 1% increase in risk score) and global cognition by close to a quarter. Adjustments for the covariates also attenuated the estimated log odds of low mental status classification for the GVRS by close to 8% (−ORGVRS=1.048 [95%CI=1.032–1.064]; p < 0.001). The majority of the attenuations in the estimated coefficients resulted from controlling for educational attainment. We found similar attenuation trends when examining the associations between the risk scores and the individual cognitive domains (Table 2). The estimated crude coefficients for the FCRS decreased by 20%, 12.5%, 33%, and 18% for the B-SEVLT Recall, B-SEVLT Sum, WF, and DSS, respectively. The estimated crude coefficients for the GVRS decreased by 26%, 27%, 43%, and 21% for the B-SEVLT Recall, B-SEVLT Sum, WF, and DSS, respectively. Importantly, after adjusting for covariates, the inverse associations between the GVRS and each of the considered cognitive measures were more than double the magnitude of the associations reported for the FCRS (Table 2). The adjusted marginal means/probabilities, and their 95% confidence intervals, for each risk score for the primary outcomes of global cognitive function and low mental status, and secondary domain specific cognitive outcomes, are presented in Figure 1.
Age and sex modifications
Tests of interactions for both CVR scores with sex provided evidence for modification (Table 3) such that women had more pronounced associations between higher CVR and worse cognition (Fig. 2). These findings were consistent for global cognition and mental status, as well as domain-specific measures of memory, verbal fluency, and executive function. Modification by age was evident with the GVRS with respect to global cognition (p < 0.001), low mental status (p=0.091), episodic and learning memory (p=0.001 and p=0.015 for B-SEVLT Recall and B-SEVLT Sum, respectively), and executive function (p < 0.001) (Table 3). Age only modified the association between the FCRS and global cognition (p=0.001) and executive function (p < 0.001). Younger individuals (<65 years) had more pronounced associations between higher CVR and worse cognition. The survey adjusted F-tests and p-values for the interactions (and group differences in slopes) are presented in Table 3. Plots of the estimated slopes by sex and age groups, for the cognitive outcomes, as detailed in our regression results above, are plotted in Figures 2 and 3, respectively.
DISCUSSION
We found that higher CVR scores were associated with notably lower cognitive performance, across multiple domains of cognition including memory and executive function. These findings extend the evidence base on the negative links between CVR and lower cognitive performance, and increased risk of cognitive impairment [3, 4, 44–47] using the first diverse Hispanic/Latino cohort. Additionally, existing findings derive largely from older cohorts and the evidence base on vascular risk and cognition in younger cohorts remains limited. Our results complement recent work by Joosten and colleagues using data from the PREVEND cohort that showed that the association of cardiovascular risk with poorer cognitive function is already present in early middle age adults [48]. Consistent pre/subclinical deficits in cognitive function can herald the onset of cognitive disorders by several decades. Targeting cardiovascular risks for modification and enhancing clinical access can be particularly impactful on cognitive disease course and progression among Latinos given their lower disease awareness and access to healthcare resources [49, 50].
We found that the GVRS exhibited stronger links to lower cognitive function compared to the FCRS. Sacco and colleagues [25] have argued that many of the existing tools to predict cardiovascular events have been limited by “use of single index, lack of racial diversity, or endpoints that are limited to either heart disease or stroke alone.” The FCRS is derived from a largely non-Latino white population and recent work has challenged its sensitivity to population differences in the mix of risk factors outside of non-Latino white populations. The differences between the GVRS and FCRS scores could be attributed to several issues. A primary weakness of the FCRS is that it does not include behavioral variables or anthropometric indexes. The GVRS improves prediction by including behavioral risk factors such as alcohol consumption, physical activity, and waist circumference. As such, our findings could reflect the GVRS’ strength in accounting for such factors that are relevant to and differentially expressed among Latinos. Second, the GVRS was developed with applicability to diverse populations in mind and was derived from the NOMAS cohort, which had a significant proportion of Hispanic samples. Our results support the suggestion that models tailored to specific subgroup risks and built using multiethnic samples can provide better insight into the role of CVR in cognitive health. The GVRS is feasible to use in primary care settings because all the factors that are included are recorded or easy to obtain through simple self-reported questionnaires.
The relationships between CVR and cognitive function were consistently modified by sex for both the FCRS and GVRS. We expected evidence of modification particularly with the GVRS given its incorporation of behavioral and obesity risk factors. Middle-aged and older Latinas (45 years and older) have a much higher likelihood of abdominal obesity relative to men and are more likely to satisfy criteria for metabolic abnormalities [51]. The role of sex in the relationship between CVD and cognition is complex and requires additional investigation.
The negative association between higher CVR and lower cognition was more pronounced in middle adulthood. Cardiovascular burden accumulates in middle age and differentially so across racial/ethnic groups. The accumulation of risk factors in young adulthood and middle age accelerates cardiovascular disease onset and the insidious buildup of biological risks (e.g., brain lesions). Epidemiological work indicates that the prevalence of advanced atherosclerotic arterial plaques is high even at young ages. McGill and colleagues, for example, used data from autopsied decedents ages 30–34 to show that one in four men had advanced lesions and pronounced atherosclerotic stenosis in their brain [52]. Paul and colleagues [53] using data from asymptomatic young to middle age (24–43 years old) Black and White adults showed that having multiple cardiovascular risk factors (3+) was associated with close to a 5-fold increase in the odds of classification in the highest 5th percentile of having carotid intima-media thickness. Our results provide further support to scientific calls for increased focus on midlife interventions with modifiable risks when these risks are likely to emerge. Interventions aimed at improving the CVR profiles of Latinos can be particularly significant. Doing so has the potential to provide an early buffer for cognitive function and could reduce the severity of change in cognitive status to levels that are less insidious.
Study strengths
This study has several strengths. First it uses HCHS/SOL data, including the most detailed characterization of biomarkers and multiple cognitive measures from the largest cohort of diverse Latinos in the United States (US). Second, we adopted an analytic plan that allowed us to directly compare the associations of the risk measures. Third, we were able to link cognitive underperformance to higher vascular risk in a relatively young population that was free of cardiovascular disease or stroke. This provides evidence that the influence of vascular risks on brain aging are likely to begin years before clinical symptoms manifest. Our results indicate that CVR has the potential to affect cognitive performance, slow processing speed, and alter executive function, thus initiating and likely accelerating the cascade of cognitive decline into older age. Our results also emphasize the importance of synergistic associations between risk components in cardiovascular disease-free individuals, which could be missed or underestimated by focusing on single components.
Limitations
Several limitations are worth mentioning. First, we were unable to ascertain cognitive change or cognitive disease status (e.g., dementia). Second, the study’s baseline did not include individuals over age 74 years, which limited our ability to generalize to older Latino population. However, the strength of this study is our ability to link these competing risk scores to cognitive function at a younger age where intervention to improve modifiable risks for cardiovascular disease and stroke events and ultimately brain disease is feasible. This said, we also did not have cognitive data on individuals aged < 45 years in HCHS/SOL and therefore could not test our hypotheses in younger age groups. Given the more pronounced effects observed at middle age in this study as well as previous published work in other younger cohorts (e.g., Coronary Artery Risk Development in Young Adults Study) relating cardiovascular risk to brain health in early adulthood, future work should focus on collecting data among younger Hispanics/Latinos and other minorities to investigate these earlier age risks for cognitive impairment and ADRDs. Third, although AMEs mimic the counterfactual logic of quasi-experimental observational studies and permit us to assess and visualize cognitive function over the continua of the CVR scores, the slopes and interpretation of the relationships should be considered in the context of observational cross-sectional data. As such, no causal links can be inferred from the generated estimates and plotted slopes. Fourth, the evidence base suggests a high variability in educational quality among under-represented minority groups in the US. Adjusting for education alone might not have been sufficient to control for the effects of education. Uncovering and accounting for residual confounding through more precise measures of educational quality and its conceptual proxies are needed in future work. Fifth, we did not account for genetic risk, including APOE4, in this study. Future work should consider examining the role of APOE4 in the pathway between CVD risk and cognition. Sixth, we did not have access to MRI markers in our cohort. Enriching the HCHS/SOL cohort with MRI markers offers valuable resources and future directions for work in Hispanic/Latino samples. Lastly, we only considered the FCRS and GVRS. Both scores can potentially underestimate the risk of all adverse cardiovascular events and thus can be less sensitive to cognitive problems. Other competing risk scores should also be examined.
Conclusion
Cardiovascular disease risks are also risks for lower cognitive function in middle age and early older adulthood. Cardiovascular disease interventions are therefore promising avenues for reducing vascular contributions to cognitive impairment and dementia. Even modest shifts in population cardiovascular health may have important positive impacts on healthy cognitive aging, which has the potential to enhance quality of life, health expenditures, and stress on health resources in the US. This is particularly important given the continued ascendance of cognitive disorders and their vascular subtypes in the US. Future work that examines the association between CVR and longitudinal cognitive outcomes including cognitive impairment and dementia are warranted, especially in Latinos with high cardiovascular disease risk.
Supplementary Material
ACKNOWLEDGMENTS
Drs. Tarraf, González, and Vásquez, and Mr. Chai are supported by R01-AG48642 (National Institute of Aging). Drs. Tarraf and González previously received support was from NHLBI HC-65233. The Hispanic Community Health Study/Study of Hispanic/Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following Institutes/Centers/Offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Institute on Minority Health and Health Disparities, National Institute on Deafness and Other Communication Disorders, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute of Neurological Disorders and Stroke, NIH Institution-Office of Dietary Supplements.
Footnotes
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/19-0830r1).
SUPPLEMENTARY MATERIAL
The supplementary material is available in the electronic version of this article: http://dx.doi.org/10.3233/jad-190830.
REFERENCES
- [1].Colby LS, Ortman MJ (2015) Projections of the size and composition of the US population: 2014 to 2060, Current Population Reports, P25–1143, U.S. Census Bureau, Washington, DC: https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf [Google Scholar]
- [2].Matthews KA, Xu W, Gaglioti AH, Holt JB, Croft JB, Mack D, McGuire LC (2019) Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged>/=65 years. Alzheimers Dement 15, 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Qiu CX, Fratiglioni L (2015) A major role for cardiovascular burden in age-related cognitive decline. Nat Rev Cardiol 12, 267–277. [DOI] [PubMed] [Google Scholar]
- [4].Iadecola C (2013) The pathobiology of vascular dementia. Neuron 80, 844–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mehta KM, Yeo GW (2017) Systematic review of dementia prevalence and incidence in US race/ethnic populations. Alzheimers Dement 13, 72–83. [DOI] [PubMed] [Google Scholar]
- [6].Luchsinger J, Reitz C, Patel B, Tang M, Manly JJ, Mayeux R (2007) Relation of diabetes to mild cognitive impairment. Arch Neurol 64, 570–575. [DOI] [PubMed] [Google Scholar]
- [7].Wu JH, Haan MN, Liang J, Ghosh D, Gonzalez HM, Herman WH (2003) Impact of diabetes on cognitive function among older Latinos: a population-based cohort study. J Clin Epidemiol 56, 686–693. [DOI] [PubMed] [Google Scholar]
- [8].Gonzalez HM, Tarraf W, Gouskova N, Rodriguez CJ, Rundek T, Grober E, Pirzada A, Gonzalez P, Lutsey PL, Camacho A, Daviglus ML, Wright C, Mosley TH (2016) Life’s simple 7’s cardiovascular health metrics are associated with Hispanic/Latino neurocognitive function: HCHS/SOL results. J Alzheimers Dis 53, 955–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lamar M, Durazo-Arvizu RA, Sachdeva S, Pirzada A, Perreira KM, Rundek T, Gallo LC, Grober E, DeCarli C, Lipton RB (2019) Cardiovascular disease risk factor burden and cognition: Implications of ethnic diversity within the Hispanic Community Health Study/Study of Latinos. PloS One 14, e0215378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Tarraf W, Rodríguez CJ, Daviglus ML, Lamar M, Schneiderman N, Gallo L, Talavera GA, Kaplan RC, Fornage M, Conceicao A (2017) Blood pressure and Hispanic/Latino cognitive function: Hispanic Community Health Study/Study of Latinos results. J Alzheimers Dis 59, 31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lamar M, Wu D, Durazo-Arvizu RA, Brickman AM, Gonzalez HM, Tarraf W, Daviglus ML (2017) Cognitive associates of current and more intensive control of hypertension: findings from the Hispanic Community Health Study/Study of Latinos. Am J Hypertens 30, 624–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Anderson KM, Odell PM, Wilson PWF, Kannel WB (1991) Cardiovascular disease risk profiles. Am Heart J 121, 293–298. [DOI] [PubMed] [Google Scholar]
- [13].Sacco RL, Khatri M, Rundek T, Xu Q, Gardener H, Boden-Albala B, Di Tullio MR, Homma S, Elkind MSV, Paik MC (2009) Improving global vascular risk prediction with behavioral and anthropometric factors: The Multiethnic NOMAS (Northern Manhattan Cohort Study). J Am Coll Cardiol 54, 2303–2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Harrison SL, de Craen AJ, Kerse N, Teh R, Granic A, Davies K, Wesnes KA, den Elzen WP, Gussekloo J, Kirkwood TB, Robinson L, Jagger C, Siervo M, Stephan BC (2017) Predicting risk of cognitive decline in very old adults using three models: The Framingham Stroke Risk Profile; the Cardiovascular Risk Factors, Aging, and Dementia Model; and oxi-inflammatory biomarkers. J Am Geriatr Soc 65, 381–389. [DOI] [PubMed] [Google Scholar]
- [15].Jefferson AL, Hohman TJ, Liu D, Haj-Hassan S, Gifford KA, Benson EM, Skinner JS, Lu Z, Sparling J, Sumner EC, Bell S, Ruberg FL (2015) Adverse vascular risk is related to cognitive decline in older adults. J Alzheimers Dis 44, 1361–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Harrison SL, Ding J, Tang EY, Siervo M, Robinson L, Jagger C, Stephan BC (2014) Cardiovascular disease risk models and longitudinal changes in cognition: a systematic review. PLoS One 9, e114431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Joosten H, van Eersel ME, Gansevoort RT, Bilo HJ, Slaets JP, Izaks GJ (2013) Cardiovascular risk profile and cognitive function in young, middle-aged, and elderly subjects. Stroke 44, 1543–1549. [DOI] [PubMed] [Google Scholar]
- [18].Dregan A, Stewart R, Gulliford MC (2013) Cardiovascular risk factors and cognitive decline in adults aged 50 and over: a population-based cohort study. Age Ageing 42, 338–345. [DOI] [PubMed] [Google Scholar]
- [19].Pase MP, Grima NA, Stough CK, Scholey A, Pipingas A (2012) Cardiovascular disease risk and cerebral blood flow velocity. Stroke 43, 2803–2805. [DOI] [PubMed] [Google Scholar]
- [20].Unverzagt FW, McClure LA, Wadley VG, Jenny NS, Go RC, Cushman M, Kissela BM, Kelley BJ, Kennedy R, Moy CS, Howard V, Howard G (2011) Vascular risk factors and cognitive impairment in a stroke-free cohort. Neurology 77, 1729–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Glodzik L, Rusinek H, Brys M, Tsui WH, Switalski R, Mosconi L, Mistur R, Pirraglia E, de Santi S, Li Y, Goldowsky A, de Leon MJ (2011) Framingham cardiovascular risk profile correlates with impaired hippocampal and cortical vasoreactivity to hypercapnia. J Cereb Blood Flow Metab 31, 671–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Debette S, Seshadri S, Beiser A, Au R, Himali JJ, Palumbo C, Wolf PA, DeCarli C (2011) Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology 77, 461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Llewellyn DJ, Lang IA, Xie J, Huppert FA, Melzer D, Langa KM (2008) Framingham Stroke Risk Profile and poor cognitive function: a population-based study. BMC Neurol 8, 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Warsch JR, Rundek T, Paik MC, Elkind MS, Sacco RL, Wright CB (2013) Association between northern Manhattan study global vascular risk score and successful aging. J Am Geriatr Soc 61, 519–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Sacco RL, Khatri M, Rundek T, Xu Q, Gardener H, Boden-Albala B, Di Tullio MR, Homma S, Elkind MSV, Paik MC (2009) Improving global vascular risk prediction with behavioral and anthropometric factors: The Multiethnic NOMAS (Northern Manhattan Cohort Study). J Am Coll Cardiol 54, 2303–2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Daviglus ML, Pirzada A, Talavera GA (2014) Cardiovascular disease risk factors in the Hispanic/Latino population: lessons from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prog Cardiovasc Dis 57, 230–236. [DOI] [PubMed] [Google Scholar]
- [27].Schneiderman N, Llabre M, Cowie CC, Barnhart J, Carnethon M, Gallo LC, Giachello AL, Heiss G, Kaplan RC, LaVange LM, Teng Y, Villa-Caballero L, Avilés-Santa ML (2014) Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care 37, 2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Daviglus ML, Pirzada A, Durazo-Arvizu R, Chen J, Allison M, Aviles-Santa L, Cai J, Gonzalez HM, Kaplan RC, Schneiderman N, Sorlie PD, Talavera GA, Wassertheil-Smoller S, Stamler J (2016) Prevalence of low cardiovascular risk profile among diverse Hispanic/Latino adults in the United States by age, sex, and level of acculturation: The Hispanic Community Health Study/Study of Latinos. J Am Heart Assoc 5, e003929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Sorlie PD, Allison MA, Aviles-Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, Lavange LM, Raij L, Schneiderman N, Wassertheil-Smoller S, Talavera GA (2014) Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens 27, 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gonzalez HM, Tarraf W, Rodriguez CJ, Gallo LC, Sacco RL, Talavera GA, Heiss G, Kizer JR, Hernandez R, Davis S, Schneiderman N, Daviglus ML, Kaplan RC (2016) Cardiovascular health among diverse Hispanics/Latinos: Hispanic Community Health Study/Study of Latinos (HCHS/SOL) results. Am Heart J 176, 134–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].González HM, Tarraf W, Gouskova N, Rodríguez CJ, Rundek T, Grober E, Pirzada A, González P, Lutsey PL, Camacho A (2016) Life’s simple 7’s cardiovascular health metrics are associated with Hispanic/Latino neurocognitive function: HCHS/SOL results. J Alzheimers Dis 53, 955–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Lavange LM, Kalsbeek WD, Sorlie PD, Aviles-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP (2010) Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 20, 642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC (2002) Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 40, 771–781. [DOI] [PubMed] [Google Scholar]
- [34].González HM, Tarraf W, Gouskova N, Gallo LC, Penedo FJ, Davis SM, Lipton RB, Argüelles W, Choca JP, Catellier DJ, Mosley TH (2015) Neurocognitive function among middle-aged and older Hispanic/Latinos: results from the Hispanic Community Health Study/Study of Latinos. Arch Clin Neuropsychol 30, 68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Gonzalez HM, Tarraf W, Gouskova N, Gallo LC, Penedo FJ, Davis SM, Lipton RB, Arguelles W, Choca JP, Catellier DJ, Mosley TH (2015) Neurocognitive function among middle-aged and older Hispanic/Latinos: results from the Hispanic Community Health Study/Study of Latinos. Arch Clin Neuropsychol 30, 68–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB (2008) General cardiovascular risk profile for use in primary care. Circulation 117, 743–753. [DOI] [PubMed] [Google Scholar]
- [37].Williams R (2012) Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J 12, 308–331. [Google Scholar]
- [38].Bartus T (2005) Estimation of marginal effects using margeff. Stata J 5, 309–329. [Google Scholar]
- [39].Mitchell MN (2012) Interpreting and visualizing regression models using Stata. Stata Press Books. [Google Scholar]
- [40].Heeringa SG, West BT, Berglund PA (2010) Applied survey data analysis. CRC Press. [Google Scholar]
- [41].Jack CR Jr., Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, Shaw LM, Vemuri P, Wiste HJ, Weigand SD, Lesnick TG, Pankratz VS, Donohue MC, Trojanowski JQ (2013) Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol 12, 207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Jack CR Jr, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, Petersen RC, Trojanowski JQ (2010) Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol 9, 119–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].O’Bryant SE, Johnson L, Reisch J, Edwards M, Hall J, Barber R, Devous MD Sr., Royall D, Singh M (2013) Risk factors for mild cognitive impairment among Mexican Americans. Alzheimers Dement 9, 622–631 e621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Polidori MC, Pientka L, Mecocci P (2012) A review of the major vascular risk factors related to Alzheimer’s disease. J Alzheimers Dis 32, 521–530. [DOI] [PubMed] [Google Scholar]
- [45].Baumgart M, Snyder HM, Carrillo MC, Fazio S, Kim H, Johns H (2015) Summary of the evidence on modifiable risk factors for cognitive decline and dementia: A population-based perspective. Alzheimers Dement 11, 718–726. [DOI] [PubMed] [Google Scholar]
- [46].Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, Launer LJ, Laurent S, Lopez OL, Nyenhuis D, Petersen RC, Schneider JA, Tzourio C, Arnett DK, Bennett DA, Chui HC, Higashida RT, Lindquist R, Nilsson PM, Roman GC, Sellke FW, Seshadri S, American Heart Association Stroke Council, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on Cardiovascular Radiology and Intervention, and Council on Cardiovascular Surgery and Anesthesia (2011) Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the american heart association/american stroke association. Stroke 42, 2672–2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Debette S (2013) Vascular risk factors and cognitive disorders. Rev Neurol (Paris) 169, 757–764. [DOI] [PubMed] [Google Scholar]
- [48].Joosten H, van Eersel MEA, Gansevoort RT, Bilo HJG, Slaets JPJ, Izaks GJ (2013) Cardiovascular risk profile and cognitive function in young, middle-aged, and elderly subjects. Stroke 44, 1543–1549. [DOI] [PubMed] [Google Scholar]
- [49].Sorlie PD, Allison MA, Avilés-Santa ML, Cai J, Daviglus ML, Howard AG, Kaplan R, LaVange LM, Raij L, Schneiderman N, Wassertheil-Smoller S, Talavera GA (2014) Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens 27, 793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Rodriguez CJ, Daviglus ML, Swett K, González HM, Gallo LC, Wassertheil-Smoller S, Giachello AL, Teng Y, Schneiderman N, Talavera GA, Kaplan RC (2014) Dyslipidemia patterns among Hispanics/Latinos of diverse background in the United States. Am J Med 127, 1186–1194.e1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Heiss G, Snyder ML, Teng Y, Schneiderman N, Llabre MM, Cowie C, Carnethon M, Kaplan R, Giachello A, Gallo L, Loehr L, Aviles-Santa L (2014) Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diabetes Care 37, 2391–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].McGill HC, McMahan CA, Zieske AW, Tracy RE, Malcom GT, Herderick EE, Strong JP (2000) Association of coronary heart disease risk factors with microscopic qualities of coronary atherosclerosis in youth. Circulation 102, 374–379. [DOI] [PubMed] [Google Scholar]
- [53].Paul TK, Srinivasan SR, Chen W, Li S, Bond MG, Tang R, Berenson GS (2005) Impact of multiple cardiovascular risk factors on femoral artery intima-media thickness in asymptomatic young adults (the Bogalusa Heart Study). Am J Cardiol 95, 469–473. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.