Abstract
Background
The acute kidney injury (AKI) remains a frequent complication following open thoracic aortic surgery (OTAS) and worsens the postoperative prognosis. It remains unclear that whether the predictors of AKI following OTAS are different in the patients with or without acute aortic syndrome (AAS).
Methods
Preoperative and intraoperative variables were compared between the patients with or without AKI, and were further analyzed for identifying the potential predictors of postoperative AKI. Subgroup analysis was conducted in the patients with or without AAS, respectively.
Results
AKI after OTAS occurred in 57.6% of the overall cohort, 70.1% of the patients with AAS and 46.7% of the patients without AAS. In the multivariate analysis, history of hypertension (OR 1.011, 95% CI: [1.001–1.022], p = 0.04), preoperative platelet (OR 0.995, 95% CI: [0.991–0.999], p = 0.006) and operation time (OR 1.572, 95% CI: [1.355–1.823], p < 0.001) were identified as independent predictors of postoperative AKI for the overall cohort; CPB time (OR 1.020, 95% CI: [1.009–1.031], p < 0.001) and preoperative LMR (OR 0.823, 95% CI: [0.701–0.966], p = 0.02) as independent predictors for the patients with AAS; age (OR 1.045, 95% CI: [1.015–1.076], p = 0.003), preoperative platelet (OR 0.993, 95% CI: [0.988–0.998], p = 0.04) and operation time (OR 1.496, 95% CI: [1.166–1.918], p = 0.002) as independent predictors for the patients without AAS.
Conclusions
The patients with AAS carry a higher risk for postoperative AKI compared with those without AAS. The predictive factors for postoperative AKI after OTAS are different for AAS- and non-AAS subgroups and operation time, CPB time and preoperative platelet are modifiable predictors of AKI.
Keywords: Acute aortic syndrome, Acute kidney injury, Independent predictor, Open thoracic aortic surgery
Introduction
The AKI complicates 10–70% patients undergoing OTAS, depending on the distinct definitions of AKI [1–7]. This complication predicts a dismal prognosis and increases the postoperative mortality and morbidity. Despite the recent advancements in cardiopulmonary bypass (CPB), anesthesia and intensive care, the incidence of AKI following OTAS remains high [8]. The AKI contemporarily represents a huge challenge for cardiovascular surgeons as no definite therapy has thus been developed. Though renal replacement therapy (RRT) is a feasible therapeutic option, modifying those potential risk factors could fundamentally prevent the occurrence of AKI and improves the short- and long-term outcomes [2, 9–12].
The primary objective of this retrospective cohort study was to clarify that whether different risk factors predict AKI after OTAS in the patients with or without AAS.
Materials and methods
Study design and participants
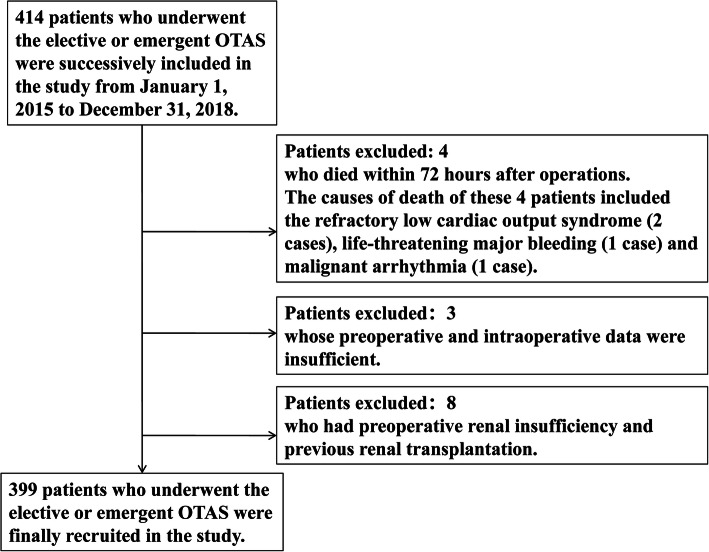
This single-center retrospective cohort study was approved by the Ethics Committee of Shandong Provincial Hospital and the written informed consent was waived due to the retrospective design. 399 consecutive patients were eventually recruited who underwent the elective or emergent OTAS between January 1, 2015 to December 31, 2018. The patients were excluded from the cohort who died within 72 h after operations or whose preoperative and intraoperative data were insufficient or who had preoperative renal insufficiency or previous renal transplantation (Fig. 1). The study was conducted following the Good Clinical Practice (GCP) as well as principles of the Declaration of Helsinki. The clinical data of those patients were carefully collected from admission to discharge. All the operations were completed by an identical surgical team. In this study, AAS represents a series of acute and catastrophic aortic lesions including acute aortic dissection, intramural hematoma, penetrating aortic ulcer, and rupture of aorta due to aortic aneurysm or trauma. Non-AAS represents the non-acute and non-catastrophic thoracic aortic lesions that require elective surgical treatment. The included 399 patients were divided into the AAS subgroup and non-AAS subgroup for further analysis. Potential demographic or perioperative variables considered associated with postoperative AKI were included on the basis of clinical experiences and literature review.
Fig. 1.
Flow chart of participants inclusion and exclusion. Figure 1 depicts the process of participants inclusion and exclusion
Definition of AKI following OTAS and postoperative outcomes
The primary outcome of this cohort study was AKI after OTAS. The diagnosis of AKI was established according to the modified Kidney Disease: Improving Global Outcomes guidelines (KDIGO) [13]. The postoperative AKI was defined as an increase of > 50% of the baseline within the first 7 days or > 0.3 mg/dL (26.5 umol/L) within the first 48 h in the postoperative serum creatinine (Scr). The baseline Scr was ascertained based on the latest preoperative tests. And the AKI was further graded as stage I, II and III according to the KDIGO classification and the patients were categorized in line with their highest levels of postoperative Scr. Besides, the postoperative outcomes attributable to AKI included RRT, length of ICU stay and ICU stay > 7 days, intubation time and time > 5 days, stroke, redo surgery and in-hospital mortality.
Surgical details
The Surgical details were summarized in the supplementary material.
Statistical analysis
Statistical analysis was performed using SPSS Statistics 25.0. Categorical variables were expressed as frequencies (n) with percentages (%). Continuous variables were expressed as mean ± standard deviation (SD) or median (quartile), depending on the data dispersion. The t-test was used if a continuous variable conformed normal distribution. And non-parametric Mann-Whitney U test was applied if a continuous variable was consistent with skewed distribution. A chi-squared or a Fisher’s exact test was used for categorical variables when necessary. The univariate and multivariate analyses were performed using binary logistic regression analysis. The candidate univariates (with a p valve less than 0.1) as well as those possible predictive variables were included in the multivariate predictive model. And the predictive model was further evaluated using the receiver operating curve (ROC) and the Hosmer-Lemeshow test. Except that the overall cohort were analyzed as above-mentioned, the subgroup analyses were additionally conducted for the patients with or without AAS. All the statistical tests were two-sided and a p valve less than 0.05 was considered statistically significant.
Results
Patient characteristics
A total of 399 patients were enrolled in this retrospective cohort study and the patient characteristics of overall cohort, AAS subgroup and non-AAS subgroup were shown respectively in the supplementary material. The patients were excluded who died within 72 h after operations (n = 4), whose preoperative and intraoperative data were insufficient (n = 3) as well as who had preoperative renal insufficiency and previous renal transplantation (n = 8). The causes of death of these 4 patients included the refractory low cardiac output syndrome (n = 2), life-threatening major bleeding (n = 1) and malignant arrhythmia (n = 1). The surgical options of overall cohort were presented in the supplementary Table 1. And the surgical options of AAS subgroup and non-AAS subgroup were showed in supplementary Table 2 and supplementary Table 3, respectively.
Incidence of AKI after open thoracic aortic surgery
Postoperative AKI in the overall cohort
According to the modified KDIGO’s Criteria, the incidence of AKI after aortic operation was 57.6% (230 in 399), among whom 153 patients (38.3%) met the criteria of stage 1, 49 patients (12.3%) satisfied the criteria of stage 2, and 28 patients (7.0%) reached the stage 3 (Table 1).
Table 1.
Characteristics of the Overall Cohort
| No AKI | AKI | P1 Value* | P2 Value# | |||
|---|---|---|---|---|---|---|
| Stage 1 | Stage 2 | Stage 3 | ||||
| Patient population (n) | 169 | 153 | 49 | 28 | ||
| Demographic data | ||||||
| Age (y) | 52.0 (18.0) | 54.0 (16.5) | 50.0 (13.0) | 41.5 (17.5) | 0.9 | 0.004 |
| Sex, male (n) | 112 (66.3%) | 116 (75.8%) | 34 (69.4%) | 21 (75.0%) | 0.08 | 0.3 |
| Height (cm) | 170.0 (13.0) | 170.0 (8.5) | 170.0 (14.0) | 169.0 (10.0) | 0.7 | 1.0 |
| Weight (kg) | 70.0 (16.0) | 72.0 (18.0) | 74.0 (24.0) | 75.0 (20.0) | 0.002 | 0.02 |
| BMI (kg/m2) | 24.6 (5.1) | 25.7 (5.8) | 25.2 (4.9) | 27.4 (5.8) | 0.003 | 0.009 |
| Medical history | ||||||
| Diabetes (n) | 4 (2.4%) | 4 (2.6%) | 3 (6.1%) | 1 (3.6%) | 0.5 | 0.6 |
| Hypertension (n) | 74 (43.8%) | 85 (55.6%) | 34 (69.4%) | 23 (82.1%) | < 0.001 | < 0.001 |
| Chronic obstructive pulmonary disease (n) | 4 (2.4%) | 6 (3.9%) | 1 (2.0%) | 0 (0.0%) | 0.7 | 0.6 |
| Previous myocardial infarction (n) | 1 (0.6%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.2 | 0.7 |
| Peripheral vascular disease (n) | 13 (7.7%) | 11 (7.2%) | 5 (10.2%) | 1 (3.6%) | 0.9 | 0.8 |
| Smoking (n) | 57 (33.7%) | 59 (38.6%) | 19 (38.8%) | 12 (42.9%) | 0.3 | 0.7 |
| Preoperative laboratory tests | ||||||
| Platelet (109/L) | 197.0 (71.0) | 186.5 (71.8) | 199.0 (65.5) | 166.5 (68.3) | 0.006 | 0.01 |
| Lymphocyte (109/L) | 1.63 (0.74) | 1.58 (0.90) | 1.18 (0.72) | 1.48 (0.90) | 0.004 | 0.001 |
| Monocyte (109/L) | 0.44 (0.30) | 0.51 (0.40) | 0.79 (0.78) | 0.91 (0.70) | < 0.001 | < 0.001 |
| Neutrophil (109/L) | 4.22 (2.95) | 4.86 (4.30) | 7.51 (5.64) | 10.1 (5.3) | < 0.001 | < 0.001 |
| Hyperlipidemia (n) | 55 (34.4%) | 44 (31.0%) | 7 (14.9%) | 10 (43.5%) | 0.2 | 0.04 |
| Retinol binding protein (mg/L) | 35.7 (16.2) | 37.8 (18.7) | 26.4 (24.7) | 37.3 (22.5) | 0.7 | 0.007 |
| Urinary protein | ||||||
| +/− | 17 (11.6%) | 25 (18.8%) | 10 (23.8%) | 4 (20.0%) | 0.05 | 0.2 |
| + | 14 (9.5%) | 20 (15.0%) | 11 (26.2%) | 8 (40.0%) | 0.01 | 0.005 |
| ++ | 1 (0.7%) | 2 (1.5%) | 2 (4.8%) | 1 (5.0%) | 0.2 | 0.3 |
| INR | 1.04 (0.12) | 1.04 (0.1) | 1.09 (0.15) | 1.10 (0.2) | 0.05 | 0.02 |
| Preoperative renal function | ||||||
| Preoperative SCr (μmol/L) | 70.4 (21.79) | 73.6 (23.1) | 66.0 (26.3) | 76.0 (45.7) | 0.3 | 0.07 |
| > 106 (n) | 11 (6.5%) | 13 (8.5%) | 4 (8.2%) | 8 (28.6%) | 0.1 | 0.002 |
| eGFR(mL/min/1.73 m2) | 99.8 (22.0) | 97.2 (21.2) | 103.4 (18.2) | 94.4 (39.5) | 0.2 | 0.08 |
| Preoperative cardiovascular status | ||||||
| Marfan syndrome (n) | 14 (8.3%) | 3 (2.0%) | 1 (2.0%) | 1 (3.6%) | 0.005 | 0.04 |
| Aortic dissection (n) | 56 (33.1%) | 71 (46.4%) | 36 (73.5%) | 24 (85.7%) | < 0.001 | < 0.001 |
| Stanford type-A aortic dissection (n) | 53 (31.4%) | 71 (46.4%) | 34 (69.4%) | 24 (85.7%) | < 0.001 | < 0.001 |
| Intraoperative blood product use | ||||||
| Erythrocytes (u) | 2.0 (2.0) | 4.0 (3.9) | 4.0 (6.0) | 4.0 (4.5) | 0.001 | < 0.001 |
| Fresh frozen plasma (ml) | 400.0 (200.0) | 400.0 (150.0) | 400.0 (375.0) | 600.0 (500.0) | 0.06 | 0.002 |
| Platelets (u) | 1.0 (0.0) | 1.0 (1.0) | 1.0 (1.0) | 2.0 (1.0) | 0.002 | < 0.001 |
| Surgical details | ||||||
| Involving the aortic arch (n) | 79 (46.7%) | 97 (63.4%) | 38 (77.6%) | 26 (92.9%) | < 0.001 | < 0.001 |
| Involving the descending aorta (n) | 43 (25.4%) | 60 (39.2%) | 33 (67.3%) | 24 (85.7%) | < 0.001 | < 0.001 |
| CPB duration(min) | 133.0 (75.5) | 165.0 (79.0) | 201.0 (67.5) | 220.0 (52.0) | < 0.001 | < 0.001 |
| DHCA or MHCA (n) | 58 (34.3%) | 76 (49.7%) | 34 (69.4%) | 25 (89.3%) | < 0.001 | < 0.001 |
| Aortic cross-clamp time (min) | 86.0 (27.0) | 90.0 (31.0) | 96.0 (32.0) | 113.0 (32.0) | < 0.001 | < 0.001 |
| Operation time (h) | 6.0 (2.0) | 7.0 (2.0) | 8.5 (2.0) | 9.0 (2.5) | < 0.001 | < 0.001 |
| Combined surgery | ||||||
| Valvular surgery (n) | 94 (55.6%) | 67 (43.8%) | 10 (20.4%) | 3 (10.7%) | < 0.001 | < 0.001 |
| Outcomes | ||||||
| Renal replacement therapy (n) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 12 (42.9%) | 0.003 | < 0.001 |
| Length of ICU stay (day) | 3.0 (2.0) | 4.0 (2.5) | 5.0 (4.0) | 10.5 (11.0) | < 0.001 | < 0.001 |
| > 7 d (n) | 19 (11.2%) | 20 (13.1%) | 17 (34.7%) | 23 (82.1%) | < 0.001 | < 0.001 |
| Intubation time (h) | 15.0 (9.0) | 17.0 (27.5) | 38.0 (72.5) | 136.0 (110.3) | < 0.001 | < 0.001 |
| > 5 d (n) | 4 (2.4%) | 5 (3.3%) | 6 (12.2%) | 17 (60.7%) | < 0.001 | < 0.001 |
| Stroke (n) | 0 (0.0%) | 4 (2.6%) | 0 (0.0%) | 2 (7.1%) | 0.04 | 0.01 |
| Redo surgery (n) | 4 (2.4%) | 6 (3.9%) | 6 (12.2%) | 6 (21.4%) | 0.02 | < 0.001 |
| In-hospital mortality (n) | 2 (1.2%) | 1 (0.7%) | 1 (2.1%) | 8 (28.6%) | 0.07 | < 0.001 |
Abbreviations: BMI body mass index, INR International Normalized Ratio, SCr Serum Creatinine, eGFR Estimated Glomerular Filtration Rate, CPB Cardiopulmonary Bypass, DHCA Deep Hypothermia and Circulatory Arrest, MHCA Median Hypothermia and Circulatory Arrest
NOTE. The categorical variables in the table are presented by the number of cases (with percentage) and the continuous variables are expressed by the median (with interquartile range) or mean (with standard deviation).
*P1 Value: Compare the patients without AKI and all patients with AKI. P1 values* were the results of unpaired t-test or Mann-Whitney U test for continuous variables, and χ2 test or Fisher’s exact test for categorical variables.
#P2 Value: Compare patients within four groups (without AKI and patients with stage 1, 2 and 3 AKI). P2 values# were the results of one-way analysis of variance or KruskalWallis test for continuous variables, and χ2 test or Fisher’s exact test for categorical variables
Postoperative AKI in the patients with AAS
In the subgroup of patients with AAS, the incidence of postoperative AKI was evidently higher than that of the overall cohort (p < 0.01). 131 in 187 (70.1%) developed the postoperative AKI, among whom 71 patients (38.0%) met the criteria of stage 1, 36 patients (19.3%) satisfied the criteria for stage 2 AKI, and 24 patients (12.8%) met reached the stage 3 (Table 3).
Table 3.
Characteristics of the patients with acute aortic syndrome
| No AKI | AKI Stage | P1 Value* | P2 Value# | |||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||
| Patient population (n) | 56 | 71 | 36 | 24 | ||
| Demographic data | ||||||
| Age (y) | 48.0 (16.5) | 48.0 (15.0) | 48.0 (13.5) | 41.0 (8.3) | 0.2 | 0.07 |
| Sex, male (n) | 31 (55.4%) | 52 (73.2%) | 24 (66.7%) | 18 (75.0%) | 0.03 | 0.1 |
| Height (cm) | 170.0 (12.8) | 171.0 (7.0) | 172.0 (10.5) | 170.0 (13.0) | 0.4 | 0.5 |
| Weight (kg) | 71.9 ± 10.2 | 78.0 ± 12.6 | 77.1 ± 14.4 | 77.8 ± 13.4 | 0.003 | 0.07 |
| BMI (kg/m2) | 25.5 ± 2.8 | 25.7 ± 5.6 | 26.4 ± 3.9 | 28.2 ± 3.7 | 0.3 | 0.2 |
| Medical history | ||||||
| Diabetes (n) | 2 (3.6%) | 1 (1.4%) | 2 (5.6%) | 1 (4.2%) | 0.9 | 0.7 |
| Hypertension (n) | 38 (67.9%) | 46 (64.8%) | 30 (83.3%) | 23 (95.8%) | 0.3 | 0.009 |
| Chronic obstructive pulmonary disease (n) | 1 (1.8%) | 1 (1.4%) | 0 (0.0%) | 0 (0.0%) | 0.5 | 0.8 |
| Peripheral vascular disease (n) | 4 (7.1%) | 5 (7.0%) | 4 (11.1%) | 1 (4.2%) | 0.9 | 0.8 |
| Smoking (n) | 17 (30.4%) | 21 (29.6%) | 13 (36.1%) | 9 (37.5%) | 0.7 | 0.8 |
| Preoperative laboratory tests | ||||||
| Platelet (109/L) | 195.5 (106.0) | 191.0 (82.0) | 191.0 (83.3) | 177.0 (65.5) | 0.1 | 0.2 |
| Lymphocyte (109/L) | 1.39 (0.75) | 1.24 (0.81) | 1.13 (0.59) | 1.41 (0.99) | 0.01 | 0.03 |
| Monocyte (109/L) | 0.70 (0.56) | 0.67 (0.60) | 0.89 (0.63) | 0.92 (0.82) | 0.03 | 0.03 |
| Neutrophil (109/L) | 7.39 ± 3.60 | 7.76 ± 3.41 | 8.97 ± 3.33 | 10.52 ± 3.76 | 0.04 | 0.001 |
| Hyperlipidemia (n) | 14 (25.0%) | 16 (22.5%) | 3 (8.3%) | 9 (37.5%) | 0.6 | 0.02 |
| Retinol binding protein (mg/L) | 27.6 (24.1) | 27.9 (17.1) | 21.2 (16.4) | 37.3 (25.2) | 0.7 | 0.02 |
| Preoperative renal function | ||||||
| Dissection involving renal artery (n) | 4 (7.1%) | 6 (8.5%) | 4 (11.1%) | 5 (20.8%) | 0.4 | 0.3 |
| Preoperative SCr (μmol/L) | 65.5 (31.0) | 75.0 (24.4) | 68.5 (36.2) | 81.1 (47.9) | 0.2 | 0.2 |
| > 106 (n) | 6 (10.7%) | 10 (14.1%) | 4 (11.1%) | 7 (29.2%) | 0.3 | 0.2 |
| Surgical details | ||||||
| Involving the aortic arch (n) | 50 (89.3%) | 66 (93.0%) | 35 (97.2%) | 24 (100.0%) | 0.1 | 0.2 |
| Involving the descending aorta (n) | 43 (76.8%) | 59 (83.1%) | 33 (91.7%) | 23 (95.8%) | 0.06 | 0.1 |
| CPB duration (min) | 188.0 (38.8) | 201.0 (44.0) | 222.0 (51.8) | 235.0 (60.0) | < 0.001 | < 0.001 |
| DHCA or MHCA (n) | 48 (85.7%) | 65 (91.5%) | 34 (94.4%) | 23 (95.8%) | 0.1 | 0.4 |
| Aortic cross-clamp time (min) | 94.5 (21.8) | 99.0 (31.0) | 96.0 (32.5) | 110.0 (29.0) | 0.02 | 0.02 |
| Operation time (h) | 7.0 (1.5) | 8.0 (1.5) | 8.5 (1.9) | 9.0 (2.5) | < 0.001 | < 0.001 |
| Combined surgery | ||||||
| CABG (n) | 1 (1.8%) | 2 (2.8%) | 0 (0.0%) | 3 (12.5%) | 0.5 | 0.04 |
| Valvular surgery (n) | 8 (14.3%) | 7 (9.9%) | 1 (2.8%) | 0 (0.0%) | 0.07 | 0.1 |
| Outcomes | ||||||
| Renal replacement therapy (n) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 11 (45.8%) | 0.03 | < 0.001 |
| Length of ICU stay (day) | 5.0 (3.8) | 5.0 (2.0) | 5.0 (4.0) | 12.0 (11.5) | 0.02 | < 0.001 |
| > 7 d (n) | 17 (30.4%) | 16 (22.5%) | 13 (36.1%) | 22 (91.7%) | 0.3 | < 0.001 |
| Intubation time (h) | 19.0 (20.0) | 24.0 (32.0) | 40.5 (75.8) | 147.5 (81.0) | < 0.001 | < 0.001 |
| > 5 d (n) | 4 (7.1%) | 4 (5.6%) | 5 (13.9%) | 17 (70.8%) | 0.03 | < 0.001 |
| Redo surgery (n) | 2 (3.6%) | 2 (2.8%) | 5 (13.9%) | 6 (25.0%) | 0.1 | 0.002 |
| In-hospital mortality (n) | 1 (1.8%) | 1 (1.4%) | 0 (0.0%) | 7 (29.2%) | 0.2 | < 0.001 |
Abbreviations: BMI body mass index, SCr Serum Creatinine, CPB Cardiopulmonary Bypass, DHCA Deep Hypothermia and Circulatory Arrest, MHCA Median Hypothermia and Circulatory Arrest, CABG Coronary Artery Bypass Graft
NOTE. The categorical variables in the table are presented by the number of cases (with percentage) and the continuous variables are expressed by the median (with interquartile range) or mean (with standard deviation)
*P1 Value: Compare the patients without AKI and all patients with AKI. P1 values* were the results of unpaired t-test or Mann-Whitney U test for continuous variables, and χ2 test or Fisher’s exact test for categorical variables
#P2 Value: Compare patients within four groups (without AKI and patients with stage 1, 2 and 3 AKI). P2 values# were the results of one-way analysis of variance or KruskalWallis test for continuous variables, and χ2 test or Fisher’s exact test for categorical variables
Postoperative AKI in the patients without AAS
Compared with the AAS subgroup, the incidence of postoperative AKI was markedly reduced in the non-AAS subgroup (p < 0.001). Of 212 patients in the non-AAS subgroup, 99 (46.7%) patients developed the postoperative AKI. 82 patients (38.7%) met the criteria of stage 1, 13 patients (6.1%) reached the criteria for stage 2, 4 patients (1.9%) were in stage 3 (Table 5).
Table 5.
Characteristics of the patients without acute aortic syndrome
| No AKI | AKI Stage | P1 Value* | P2 Value# | |||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||
| Patient population (n) | 113 | 82 | 13 | 4 | ||
| Demographic data | ||||||
| Age (y) | 53.0 (17.5) | 60.0 (11.0) | 52.0 (14.0) | 55.0 (19.5) | 0.002 | 0.01 |
| Sex, male (n) | 81 (71.7%) | 64 (78.0%) | 10 (76.9%) | 3 (75.0%) | 0.3 | 0.8 |
| Height (cm) | 170.0 (14.0) | 168.0 (10.5) | 165.0 (15.0) | 166.5 (4.5) | 0.1 | 0.3 |
| Weight (kg) | 67.0 (16.0) | 69.1 (15.6) | 66.0 (15.0) | 62.0 (17.0) | 0.6 | 0.2 |
| BMI (kg/m2) | 24.2 (5.3) | 25.0 (5.7) | 22.9 (5.0) | 22.8 (5.6) | 0.09 | 0.09 |
| Medical history | ||||||
| Diabetes (n) | 2 (1.8%) | 3 (3.7%) | 1 (7.7%) | 0 (0.0%) | 0.3 | 0.6 |
| Hypertension (n) | 36 (31.9%) | 39 (47.6%) | 4 (30.8%) | 0 (0.0%) | 0.08 | 0.05 |
| Chronic obstructive pulmonary disease (n) | 3 (2.7%) | 5 (6.1%) | 1 (7.7%) | 0 (0.0%) | 0.2 | 0.6 |
| Previous myocardial infarction (n) | 1 (0.9%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.3 | 0.8 |
| Peripheral vascular disease (n) | 9 (8.0%) | 6 (7.3%) | 1 (7.7%) | 0 (0.0%) | 0.8 | 0.9 |
| Smoking (n) | 40 (35.4%) | 38 (46.3%) | 6 (46.2%) | 3 (75.0%) | 0.08 | 0.2 |
| Preoperative laboratory tests | ||||||
| Platelet (109/L) | 197.0 (57.5) | 183.0 (58.0) | 203.0 (54.5) | 137.5 (109.3) | 0.03 | 0.09 |
| Preoperative renal function | ||||||
| eGFR(mL/min/1.73 m2) | 99.8 (16.1) | 95.9 (18.1) | 101.7 (16.4) | 97.2 (37.6) | 0.04 | 0.02 |
| Preoperative cardiovascular status | ||||||
| Previous cardiovascular surgery (n) | 2 (1.8%) | 1 (1.2%) | 0 (0.0%) | 1 (25.0%) | 0.9 | 0.008 |
| LVEF (%) | 58.0 (8.0) | 60.0 (4.5) | 52.5 (17.8) | 59.0 (11.8) | 0.2 | 0.08 |
| Marfan syndrome (n) | 11 (9.7%) | 2 (2.4%) | 1 (7.7%) | 0 (0.0%) | 0.05 | 0.2 |
| Intraoperative blood product use | ||||||
| Erythrocytes (u) | 2.0 (3.0) | 2.0 (4.0) | 3.0 (3.0) | 4.0 (6.0) | 0.2 | 0.07 |
| Fresh frozen plasma (ml) | 400.0 (0.0) | 400.0 (0.0) | 400.0 (300.0) | 650.0 (450.0) | 0.2 | 0.02 |
| Platelets (u) | 1.0 (1.0) | 1.0 (1.0) | 1.0 (1.0) | 2.0 (0.8) | 0.5 | 0.004 |
| Surgical details | ||||||
| Involving the aortic arch (n) | 29 (25.7%) | 31 (37.8%) | 3 (23.1%) | 2 (50.0%) | 0.09 | 0.2 |
| Involving the descending aorta (n) | 0 (0.0%) | 1 (1.2%) | 0 (0.0%) | 1 (25.0%) | 0.1 | < 0.001 |
| CPB duration(min) | 117.5 (43.0) | 131.0 (50.5) | 137.0 (52.5) | 187.5 (34.8) | 0.005 | 0.003 |
| DHCA or MHCA (n) | 10 (8.8%) | 11 (13.4%) | 0 (0.0%) | 2 (50.0%) | 0.3 | 0.03 |
| Aortic cross-clamp time (min) | 81.0 (27.8) | 83.0 (31.3) | 94.0 (32.5) | 122.0 (42.8) | 0.08 | 0.04 |
| Operation time (h) | 5.0 (1.0) | 6.0 (1.5) | 7.0 (2.3) | 8.5 (2.5) | < 0.001 | < 0.001 |
| Combined surgery | ||||||
| CABG (n) | 8 (7.1%) | 11 (13.4%) | 2 (15.4%) | 1 (25.0%) | 0.09 | 0.3 |
| Outcomes | ||||||
| Renal replacement therapy (n) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (25.0%) | 0.3 | < 0.001 |
| ICU length of stay (day) | 3.0 (1.0) | 3.0 (2.0) | 5.0 (5.0) | 4.0 (7.5) | < 0.001 | < 0.001 |
| > 7 d (n) | 2 (1.8%) | 4 (4.9%) | 4 (30.8%) | 1 (25.0%) | 0.02 | < 0.001 |
| Intubation time (h) | 13.0 (8.0) | 14.0 (9.0) | 20.0 (28.5) | 28.5 (28.5) | 0.03 | 0.001 |
| > 5 d (n) | 0 (0.0%) | 1 (1.2%) | 1 (7.7%) | 0 (0.0%) | 0.1 | 0.06 |
| In-hospital mortality (n) | 1 (0.9%) | 0 (0.0%) | 1 (7.7%) | 1 (25.0%) | 0.5 | < 0.001 |
Abbreviations: BMI body mass index, INR International Normalized Ratio, eGFR Estimated Glomerular Filtration Rate, LVEF Left Ventricular Ejection Fraction, CPB Cardiopulmonary Bypass, DHCA Deep Hypothermia and Circulatory Arrest, MHCA Median Hypothermia and Circulatory Arrest, CABG Coronary Artery Bypass Graft
NOTE. The categorical variables in the table are presented by the number of cases (with percentage) and the continuous variables are expressed by the median (with interquartile range) or mean (with standard deviation)
*P1 Value: Compare the patients without AKI and all patients with AKI. P1 values* were the results of unpaired t-test or Mann-Whitney U test for continuous variables, and χ2 test or Fisher’s exact test for categorical variables
#P2 Value: Compare patients within four groups (without AKI and patients with stage 1, 2 and 3 AKI). P2 values# were the results of one-way analysis of variance or KruskalWallis test for continuous variables, and χ2 test or Fisher’s exact test for categorical variables
Risk factors of postoperative AKI after open thoracic aortic surgery
Risk factors of postoperative AKI for the overall cohort
Demographic and perioperative data of patients grouped by the severity of the KDIGO classification were present in Table 1. There were significant statistical differences in a series of variables including age, weight, BMI, history of hypertension, preoperative platelet, lymphocyte, monocyte, neutrophil and several other laboratory variables, Marfan syndrome, aortic dissection (as well as the Stanford type-A aortic dissection), intraoperative infusion of erythrocytes, fresh frozen plasma and platelets, combined valvular surgery and all the surgical data (Table 1).
The incidences of CRRT, ICU stay > 7 days, intubation time > 5 days, stroke, redo surgery and in-hospital mortality were all significantly higher among the patients with AKI than those without AKI. The time of ICU stay and intubation also markedly increased in the patients with AKI compared those without AKI (Table 1).
In the univariate analysis of risk factors for the overall cohort, body weight, history of hypertension, Marfan syndrome, preoperative platelet, lymphocyte, monocyte and neutrophil, neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), preoperative urinary protein positive (+,++), Marfan syndrome, aortic dissection (Stanford type-A aortic dissection), intraoperative fresh frozen plasma use, intraoperative involvement of aortic arch and descending aorta, CPB time, aortic cross-clamp time, operation time, DHCA or MHCA and concurrent valve surgery were candidate variables (Table 2).
Table 2.
Univariate Analysis of Risk Factors for the Overall Cohort
| Variable | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Age (y) | 1.01 | 0.99–1.02 | 0.6 |
| Sex, male | 1.48 | 0.95–2.28 | 0.08 |
| Weight | 1.02 | 1.01–1.04 | 0.006 |
| Hypertension | 2.07 | 1.38–3.10 | < 0.001 |
| Preoperative platelet | 1.00 | 0.99–1.00 | 0.006 |
| Preoperative lymphocyte | 0.64 | 0.46–0.88 | 0.007 |
| Preoperative monocyte | 3.76 | 2.02–7.00 | < 0.001 |
| Preoperative neutrophil | 1.16 | 1.08–1.23 | < 0.001 |
| NLR | 1.17 | 1.10–1.25 | < 0.001 |
| LMR | 0.88 | 0.81–0.96 | 0.003 |
| Preoperative urinary protein + or ++ | 2.43 | 1.30–4.53 | 0.005 |
| Marfan syndrome | 0.25 | 0.09–0.70 | 0.008 |
| Aortic dissection | 2.67 | 1.77–4.04 | < 0.001 |
| Standford type-A aortic dissection | 2.80 | 1.84–4.24 | < 0.001 |
| Intraoperative fresh frozen plasma use | 1.00 | 1.00–1.00 | 0.01 |
| Involving the aortic arch | 2.66 | 1.76–4.02 | < 0.001 |
| Involving the descending aorta | 3.03 | 1.97–4.67 | < 0.001 |
| CPB duration | 1.01 | 1.01–1.02 | < 0.001 |
| DHCA or MHCA | 2.72 | 1.80–4.11 | < 0.001 |
| Aortic cross-clamp time | 1.02 | 1.01–1.02 | < 0.001 |
| Operation time | 1.63 | 1.41–1.89 | < 0.001 |
| Combined valvular surgery | 0.43 | 0.28–0.64 | < 0.001 |
Abbreviations: NLR Neutrophil to Lymphocyte Ratio, LMR Lymphocyte to Monocyte Ratio, SCr Serum Creatinine, CPB Cardiopulmonary Bypass, DHCA Deep Hypothermia and Circulatory Arrest, MHCA Median Hypothermia and Circulatory Arrest
Risk factors of postoperative AKI for the patients with AAS
For the subgroup of patients with AAS, there existed significant statistical differences in those variables including male gender, weight, history of hypertension, preoperative lymphocyte, monocyte and neutrophil and several other laboratory variables, CPB time, aortic cross-clamp time, operation time and combined CABG (Table 3).
Similarly as above, the proportions of CRRT, ICU stay > 7 days, intubation time > 5 days, stroke, redo surgery and in-hospital mortality were all higher in the AKI group. Consistently, the durations of ICU stay and intubation were evidently increased in the patients with AKI in comparison with those without AKI (Table 3).
When it comes to the univariate analysis of risk factors for the AAS cohort, male gender, weight, preoperative lymphocyte, monocyte, neutrophil, NLR, LMR, CPB time, aortic cross-clamp time and operation time were included in the list of plausible variables (Table 4).
Table 4.
Univariate Analysis of Risk Factors for the patients with acute aortic syndrome
| Variable | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Age (y) | 0.98 | 0.95–1.01 | 0.2 |
| Sex, male | 2.05 | 1.07–3.92 | 0.03 |
| Weight | 1.04 | 1.01–1.07 | 0.009 |
| Preoperative platelet | 1.00 | 0.99–1.00 | 0.06 |
| Preoperative lymphocyte | 0.61 | 0.37–1.01 | 0.05 |
| Preoperative monocyte | 2.42 | 1.10–5.36 | 0.03 |
| Preoperative neutrophil | 1.10 | 1.01–1.21 | 0.04 |
| NLR | 1.16 | 1.06–1.28 | 0.002 |
| LMR | 0.77 | 0.64–0.93 | 0.007 |
| Preoperative NYHA class III or IV | 0.39 | 0.14–1.03 | 0.06 |
| Involving the descending aorta | 2.17 | 0.97–4.89 | 0.06 |
| CPB duration | 1.02 | 1.01–1.03 | < 0.001 |
| DHCA or MHCA | 2.26 | 0.82–6.20 | 0.1 |
| Aortic cross-clamp time | 1.02 | 1.00–1.04 | 0.01 |
| Operation time | 1.63 | 1.26–2.10 | < 0.001 |
| Combined valvular surgery | 0.39 | 0.14–1.1 | 0.08 |
Abbreviations: NLR Neutrophil to Lymphocyte Ratio, LMR Lymphocyte to Monocyte Ratio, CPB Cardiopulmonary Bypass, DHCA Deep Hypothermia and Circulatory Arrest, MHCA Median Hypothermia and Circulatory Arrest
Risk factors of postoperative AKI for the patients without AAS
For the non-AAS subgroup, those variables reached statistical significance that include age, history of hypertension, preoperative platelet and eGFR, previous cardiovascular surgery, Marfan syndrome, intraoperative perfusion of fresh frozen plasma and platelets, operation involving the descending aorta, CPB time, aortic cross-clamp time, DHCA or MHCA and operation time (Table 5).
For the patients in the non-AAS subgroup, the rates of CRRT, ICU stay > 7 days, intubation time > 5 days and in-hospital mortality were evidently enhanced when compared to those without AKI. And the ICU length of stay also elevated in the patients with AKI (Table 5).
As for the univariate analysis of risk factors for the non-AAS cohort, several potential risk factors have been identified that consist of age, preoperative platelet and platelet to lymphocyte ratio (PLR), CPB time and operation time (Table 6).
Table 6.
Univariate Analysis of Risk Factors for the patients without acute aortic syndrome
| Variable | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Age (y) | 1.05 | 1.02–1.08 | < 0.001 |
| Sex, male | 1.38 | 0.74–2.59 | 0.3 |
| Hypertension | 1.64 | 0.94–2.88 | 0.08 |
| Smoking | 1.65 | 0.95–2.86 | 0.08 |
| Preoperative platelet | 0.99 | 0.99–1.00 | 0.02 |
| PLR | 0.99 | 0.99–1.00 | 0.05 |
| Preoperative eGFR | 0.98 | 0.97–1.00 | 0.06 |
| Marfan syndrome | 0.29 | 0.08–1.07 | 0.06 |
| Involving the aortic arch | 1.66 | 0.92–2.98 | 0.09 |
| CPB duration | 1.01 | 1.00–1.02 | 0.01 |
| Operation time | 1.56 | 1.22–1.99 | < 0.001 |
Abbreviations: PLR Platelet to Lymphocyte Ratio, eGFR Estimated Glomerular Filtration Rate, CPB Cardiopulmonary Bypass
The establishment of predictive model for postoperative AKI
Predictive model for postoperative AKI in the overall cohort
Those independent predictors of postoperative AKI after OTAS included history of hypertension (OR 1.011, 95% CI: [1.001–1.022], p = 0.04), preoperative platelet (OR 0.995, 95% CI: [0.991–0.999], p = 0.006) and operation time (OR 1.572, 95% CI: [1.355–1.823], p < 0.001). The equation obtained by binary Logistic regression analysis was as follows: Y = 0.011 × history of hypertension-0.005 × preoperative platelet+ 0.452 × operation time-4.814. The predictive model was evaluated by the ROC curve. The area under a curve (AUC) of the ROC curve was 0.750 (p < 0.001, 95%CI: 0.702–0.798) (Fig. 2). When the maximum value of the Youden index was 0.409, at this time Y = 0.031, the sensitivity of the model was 76.0% and the specificity was 64.9%.
Fig. 2.
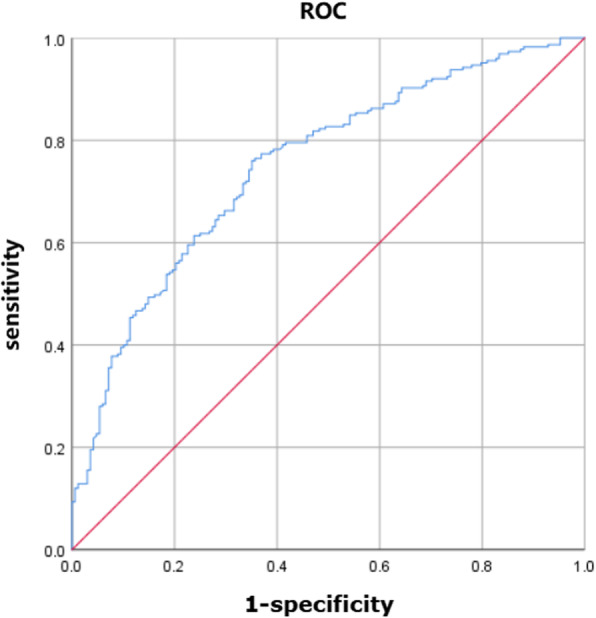
ROC curves of predictive models of acute kidney injury in the overall cohort. Figure 2 shows the ROC curves of predictive models of acute kidney injury in the overall cohort
Predictive model for postoperative AKI in the patients with AAS
For the patients with AAS, CPB time (OR 1.020, 95% CI: [1.009–1.031], p < 0.001) and preoperative LMR (OR 0.823, 95% CI: [0.701–0.966], p = 0.02) independently predicted the incidence of postoperative AKI. The equation obtained by binary Logistic regression analysis was: Y = 0.020 × CPB time-0.195 × LMR-5.601. The AUC of ROC curve was 0.784 (p < 0.001, 95% CI: 0.714–0.855) (Fig. 3). When the maximum value of the Youden index reached 0.467, at this time Y = 1.056, the sensitivity of the model was 66.7% and the specificity was 80.0%.
Fig. 3.
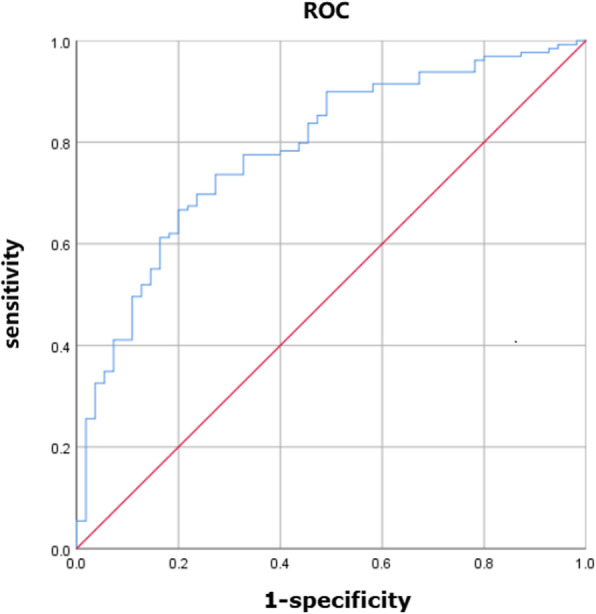
ROC curves of predictive models of acute kidney injury in the AAS subgroup. Figure 3 shows the ROC curves of predictive models of acute kidney injury in the AAS subgroup
Predictive model for postoperative AKI in the patients without acute aortic syndrome
For the patients without AAS, age (OR 1.045, 95% CI: [1.015–1.076], p = 0.003), preoperative platelet (OR 0.993, 95% CI: [0.988–0.998], p = 0.04) and operation time (OR 1.496, 95% CI: [1.166–1.918], p = 0.002) independently predicted the incidence of postoperative AKI. The equation obtained by binary Logistic regression analysis was: Y = 0.044 × age-0.006 × preoperative platelet+ 0.403 × operation time-3.751. The AUC of ROC curve (see Fig. 4) was 0.719 (P < 0.001, 95% CI: 0.651–0.787). When the maximum value of the Youden index reached 0.467, at this time Y = 1.0564, the sensitivity of the model was 81.4% and the specificity was 52.2%.
Fig. 4.
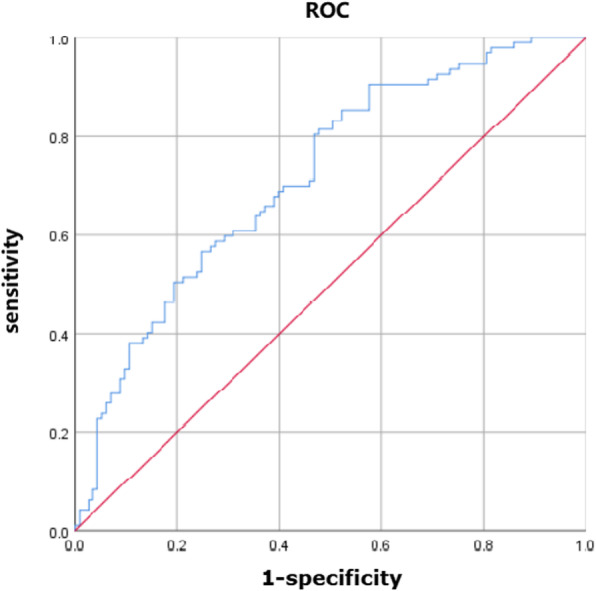
ROC curves of predictive models of acute kidney injury in the non-AAS subgroup. Figure 4 shows the ROC curves of predictive models of acute kidney injury in the non-AAS subgroup
Discussion
Prospective or retrospective studies have previously found that the incidence of AKI after thoracic aortic surgery is approximately 18–67%, depending on the definition of AKI [1–7]. Some of these prior papers recruited a highly heterogeneous group of patients, regardless of disease types and surgical options. And the other papers were designed to study on a specific group of patients, such as the patients undergoing elective or emergent OTAS, overweight patients who underwent total aorta replacement (TAR) combined with frozen elephant trunk (FET) implantation, patients receiving surgical treatment for type A aortic dissection and so on. We believe that the deviation of AKI incidence and predictive factors from various studies on OTAS was to a large extent attributable to the heterogeneity of recruited subjects including ethnicity, disease types and surgical procedures and etc.
According to our search result, the incidence of postoperative AKI following OTAS has been rarely studied in the patients with AAS and our work was among the first to focus on this special subgroup. The definition of AAS comprises of a series of acute and catastrophic aortic lesions including acute aortic dissection, intramural hematoma, penetrating aortic ulcer, and rupture of aorta due to aortic aneurysm or trauma [14]. For most heart centers across the globe including ours, emergency aortic surgery is indicated for the patients with AAS. Even for the patients at advanced age and with co-morbidities, urgent surgery is highly recommended, and for the most circumstances is not surgically contraindicated. Of note, the patients with AAS are theoretically under a higher risk of postoperative AKI than the overall cohort and non-AAS group. First, the patients with AAS are more likely to develop into a serious situation of single- or multi-organ dysfunction including cardiac, hepatic and respiratory failure, which is tightly associated with renal dysfunction and even failure. Second, acute aortic lesion could lead to the sudden disruption of normal blood supply to renal, which inevitably results in the occurrence of AKI. Third, the systemic inflammation response syndrome (SIRS) and ischemia-reperfusion injury could further deteriorate the status of renal function and worsen the AKI. Other preoperative risk factors among AAS patients compared to non-AAS patients might include hypertension, obesity, preoperative renal injury and repeated contrast agents used in CT or MRI scan. Fourth, a majority of patients with AAS will undergo the aortic arch repair and reconstruction, which signifies the prolonged operation time, CPB time and DHCA or MHCA. Especially in China, the patients with AAS have a younger average age at disease onset than the patients in the western countries [15]. And the Chinese patients prefer to undergo a more radical surgical operation (such as Sun’s procedure) for only once because of limited financial support and medical insurance. Therefore, the patients with AAS should be separately analyzed for the incidence and risk factors of postoperative AKI following OTAS. Our results revealed that compared to the non-AAS subgroup, an extra of 15% more patients with AAS will experience the AKI following OTAS. And the prolonged CPB time and reduced preoperative LMR were independently associated with the occurrence of AKI in the AAS subgroup. As expected, the predictive models for AKI were different between the AAS and non-AAS subgroups. Our results were consistent with several previous studies that CPB time instead of DHCA time were statistically linked with postoperative AKI [7, 15]. It is hypothesized by Sun and this team that DHCA could significantly extend the CPB time, which is likely to be counterbalanced by the protective effects of DHCA on renal function. Additionally, the preoperative LMR might also function as a novel bio-marker for predicting postoperative AKI following OTAS, and such report has not been published so far and it awaits further investigation.
Our team also analyzed the data from the non-AAS subgroup in whom elective OTAS were performed. Englberger and his colleagues carried out a retrospective study with a larger sample size on elective OTAS [2]. However, our work was the first to investigate the AKI following elective OTAS in Chinese ethnicity though the sample size was relatively small. Besides, the results of diagnostic test suggested that our predictive model for AKI after OTAS has a good predictive ability, with its sensitivity and specificity to be further improved in the future.
Conclusions
The patients with AAS have a higher risk of developing postoperative AKI after OTAS compared with those without AAS. The predictive factors for postoperative AKI following OTAS vary between AAS and non-AAS subgroups. Operation time, CPB time and preoperative platelet are modifiable predictors of AKI.
Supplementary information
Additional file 2. Supplementary Table 1 Surgical options of the overall cohort
Additional file 3. Supplementary Table 2 Surgical options of AAS patient
Additional file 4. Supplementary Table 3 Surgical options of non-AAS patients
Acknowledgements
Not applicable.
Abbreviations
- AKI
Acute kidney injury
- OTAS
Open thoracic aortic surgery
- AAS
Acute aortic syndrome
- CPB
Cardiopulmonary bypass
- RRT
Renal replacement therapy
- GCP
Good Clinical Practice
- KDIGO
Kidney Disease: Improving Global Outcomes guidelines
- Scr
Serum creatinine
- SD
Standard deviation
- ROC
Receiver operating curve
- NLR
Neutrophil to lymphocyte ratio
- LMR
Lymphocyte to monocyte ratio
- PLR
Platelet to lymphocyte ratio
- TAR
Total aorta replacement
- FET
Frozen elephant trunk
- SIRS
Systemic inflammation response syndrome
Authors’ contributions
YC and XM designed the research. XM, JL, YY, DZ, SC and HM analyzed the data. XM, JL and YY wrote the paper. ZW, HZ and CZ were responsible for data collection. All authors read and approved the final manuscript.
Funding
The current work was supported by grants from The National Nature Science Foundation of China (grant no. 81600222 to YC and 81800255 to MX), Young experts of Taishan Scholar Program of Shandong Province to YC (tsqn201812142) and Natural Science Foundation of Shandong Province (ZR2018BH002 to MX). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This single-center retrospective cohort study was approved by the Ethics Committee of Shandong Provincial Hospital and the written informed consent was waived due to the retrospective design.
Consent for publication
Consents for publication were obtained from all individuals involved in our study.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaochun Ma, Jinzhang Li and Yan Yun contributed equally to this work.
Contributor Information
Xiaochun Ma, Email: mxcmxc2008@163.com.
Yuqi Cui, Email: cuiyu@health.missouri.edu.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13019-020-01257-1.
References
- 1.Ko T, Higashitani M, Sato A, Uemura Y, Norimatsu T, Mahara K, et al. Impact of acute kidney injury on early to long-term outcomes in patients who underwent surgery for type a acute aortic dissection. Am J Cardiol. 2015;116(3):463–468. doi: 10.1016/j.amjcard.2015.04.043. [DOI] [PubMed] [Google Scholar]
- 2.Englberger L, Suri RM, Greason KL, Burkhart HM, Sundt TM, 3rd, Daly RC, et al. Deep hypothermic circulatory arrest is not a risk factor for acute kidney injury in thoracic aortic surgery. J Thorac Cardiovasc Surg. 2011;141(2):552–558. doi: 10.1016/j.jtcvs.2010.02.045. [DOI] [PubMed] [Google Scholar]
- 3.Zhao H, Pan X, Gong Z, Zheng J, Liu Y, Zhu J, et al. Risk factors for acute kidney injury in overweight patients with acute type a aortic dissection: a retrospective study. J Thorac Dis. 2015;7(8):1385–1390. doi: 10.3978/j.issn.2072-1439.2015.07.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim WH, Lee JH, Kim E, Kim G, Kim HJ, Lim HW. Can we really predict postoperative acute kidney injury after aortic surgery? Diagnostic accuracy of risk scores using gray zone approach. Thorac Cardiovasc Surg. 2016;64(4):281–289. doi: 10.1055/s-0034-1396082. [DOI] [PubMed] [Google Scholar]
- 5.Roh GU, Lee JW, Nam SB, Lee J, Choi JR, Shim YH. Incidence and risk factors of acute kidney injury after thoracic aortic surgery for acute dissection. Ann Thorac Surg. 2012;94(3):766–771. doi: 10.1016/j.athoracsur.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 6.Mori Y, Sato N, Kobayashi Y, Ochiai R. Acute kidney injury during aortic arch surgery under deep hypothermic circulatory arrest. J Anesth. 2011;25(6):799–804. doi: 10.1007/s00540-011-1210-8. [DOI] [PubMed] [Google Scholar]
- 7.Nota H, Asai T, Suzuki T, Kinoshita T, Ikegami H, Takashima N. Risk factors for acute kidney injury in aortic arch surgery with selective cerebral perfusion and mild hypothermic lower body circulatory arrest. Interact Cardiovasc Thorac Surg. 2014;19(6):955–961. doi: 10.1093/icvts/ivu241. [DOI] [PubMed] [Google Scholar]
- 8.Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, et al. Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation. 2009;119(18):2444–2453. doi: 10.1161/CIRCULATIONAHA.108.800011. [DOI] [PubMed] [Google Scholar]
- 9.D'Onofrio A, Cruz D, Bolgan I, Auriemma S, Cresce GD, Fabbri A, et al. RIFLE criteria for cardiac surgery-associated acute kidney injury: risk factors and outcomes. Congest Heart Fail. 2010;16(Suppl 1):S32–S36. doi: 10.1111/j.1751-7133.2010.00170.x. [DOI] [PubMed] [Google Scholar]
- 10.Arnaoutakis GJ, Bihorac A, Martin TD, Hess PJ, Jr, Klodell CT, Ejaz AA, et al. RIFLE criteria for acute kidney injury in aortic arch surgery. J Thorac Cardiovasc Surg. 2007;134(6):1554–1560. doi: 10.1016/j.jtcvs.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 11.Kowalik MM, Lango R, Klajbor K, Musial-Swiatkiewicz V, Kolaczkowska M, Pawlaczyk R, et al. Incidence- and mortality-related risk factors of acute kidney injury requiring hemofiltration treatment in patients undergoing cardiac surgery: a single-center 6-year experience. J Cardiothorac Vasc Anesth. 2011;25(4):619–624. doi: 10.1053/j.jvca.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Bove T, Calabro MG, Landoni G, Aletti G, Marino G, Crescenzi G, et al. The incidence and risk of acute renal failure after cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18(4):442–445. doi: 10.1053/j.jvca.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 13.Kellum JA, Lameire N, Group KAGW Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1) Crit Care. 2013;17(1):204. doi: 10.1186/cc11454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erbel R, Aboyans V, Boileau C, Bossone E, Di Bartolomeo R, Eggebrecht H, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases. Kardiol Pol. 2014;72(12):1169–1252. doi: 10.5603/KP.2014.0225. [DOI] [PubMed] [Google Scholar]
- 15.Zhou H, Wang G, Yang L, Shi S, Li J, Wang M, et al. Acute kidney injury after Total arch replacement combined with frozen elephant trunk implantation: incidence, risk factors, and outcome. J Cardiothorac Vasc Anesth. 2018;32(5):2210–2217. doi: 10.1053/j.jvca.2018.02.026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 2. Supplementary Table 1 Surgical options of the overall cohort
Additional file 3. Supplementary Table 2 Surgical options of AAS patient
Additional file 4. Supplementary Table 3 Surgical options of non-AAS patients
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.