Abstract
Introduction:
Cephalomedullary nailing presents several biomechanical benefits for treatment of intertrochanteric fractures, but posterior sagging (PS) of the proximal fragment occurs postoperatively in some patients despite intraoperative achievement of an adequate reduction. We investigated the risk factors for PS in those patients, with specific attention to posterior split fragment involving the greater trochanter (GT separation) as a possible significant risk factor.
Methods:
We retrospectively reviewed 50 (12 males, 38 females) patients ≥50 years old at diagnosis of an intertrochanteric fracture after low-energy trauma who underwent cephalomedullary nailing between April 2015 and February 2017 and were not lost to follow-up within 12 months postoperatively.
Results:
Thirteen (26%) patients experienced PS postoperatively. Average time to bone union was significantly longer in the PS (9.5 months) than in the non-PS (4.8 months) groups (P = .002). Three patients in the PS group experienced nonunion compared to none in the non-PS group (P = .015). Significant difference was found in postoperative level of ambulatory ability (Koval score) and deterioration of the score after the injury between 2 groups (4.2 vs 2.8, P = .043 and 2.5 vs 0.8, P = .005). On multivariate logistic regression analysis, GT separation (P = .010) was a significant risk factor for PS.
Discussion and Conclusion:
The presence of GT separation in cases of intertrochanteric fractures seems to weaken posterior stability in the proximal fragment, thus showing poor clinical outcomes.
Keywords: intertrochanteric fracture, cephalomedullary nailing, loss-of-reduction, greater trochanter, posterior sagging
Introduction
An intertrochanteric fracture generally occurs in older individuals with poor bone strength.1 Adequate bone reduction during surgery is imperative for maintaining the reduction status and promoting bone healing.2 Even though various surgical techniques have been introduced, cephalomedullary nailing currently is a common surgical treatment for intertrochanteric fractures3 because of its biomechanical benefits.4,5
Anteromedial cortical reduction has been emphasized in intertrochanteric fractures, especially in cases of unstable nature, despite lack of a definite consensus for achieving adequate reduction.6 Several surgical techniques have been introduced to establish these bone-to-bone contacts during surgery,7-9 but some patients still experience loss-of-reduction (LOR) despite such efforts. We also experienced several cases of LOR as posterior sagging (PS) of the proximal fragment after obtaining adequate reduction during cephalomedullary nailing for intertrochanteric fractures. However, few studies have evaluated the mechanism underlying PS after cephalomedullary nailing for intertrochanteric fractures.
Several authors have reported posterior split fragment involving the greater trochanter (GT separation) using 3-dimensional computed tomography (3DCT).10,11 We hypothesized that GT separation affects stability around the proximal part of the nail, which can lead to PS. We also investigated clinical outcomes and risk factors of the cases of PS after cephalomedullary nailing of an intertrochanteric fracture with specific attention to GT separation as a possible significant risk factor.
Materials and Methods
Patient Selection
After receiving approval from the institutional review board of our institute, we reviewed 70 consecutive patients who underwent cephalomedullary nailing for an intertrochanteric fracture as a part of the Proximal Femoral Nail Antirotation (Synthes) system by one senior surgeon from April 2015 to February 2017. Six patients with high-energy injuries from traffic accidents or falling from a high height, or patients <50 years were excluded. Fourteen cases who were lost to be followed up within 12 months after surgery were excluded, but the patients who were confirmed to achieve bony union and preinjury ambulatory ability were not excluded even their follow-up durations were less than 12 months. A total of 50 (12 men, 38 women; average age 77 [57-95] years) patients were included in this study. Mean follow-up duration was 9.8 (range: 3-24) months.
Surgical Technique and Postoperative Rehabilitation
Under general or spinal anaesthesia, the patient was positioned on the fracture table. Before draping, if possible, closed reduction was performed by manipulating the lower limbs with fluoroscopic guidance. We intended to establish anterior and medial cortical contacts at the fracture site with appropriate alignment by reference to the contralateral side. If closed reduction was not acceptable, percutaneous minimally invasive techniques were used. We initially attempted reduction through manipulation of additional pins, and hemostatic forceps or a ball spike pusher also were used if necessary (Figure 1).12,13 In all patients, the nail was inserted only after adequate reductions (anterior and medial cortical contacts achieved between proximal and distal fragments) were confirmed using intraoperative fluoroscopy. In cases when the anteromedial cortical contact was not maintained during reduction because the proximal head and neck fragment was engaged inward to the distal shaft, this fragment was intentionally medially extracted from the distal shaft (positive medial cortical support).14 After the nail insertion, a helical blade was inserted and tightened to subchondral bone of the femoral head, and then one distal locking screw was fixed through the interlocking hole. Adequate reduction was finally confirmed before wound closure in all cases.
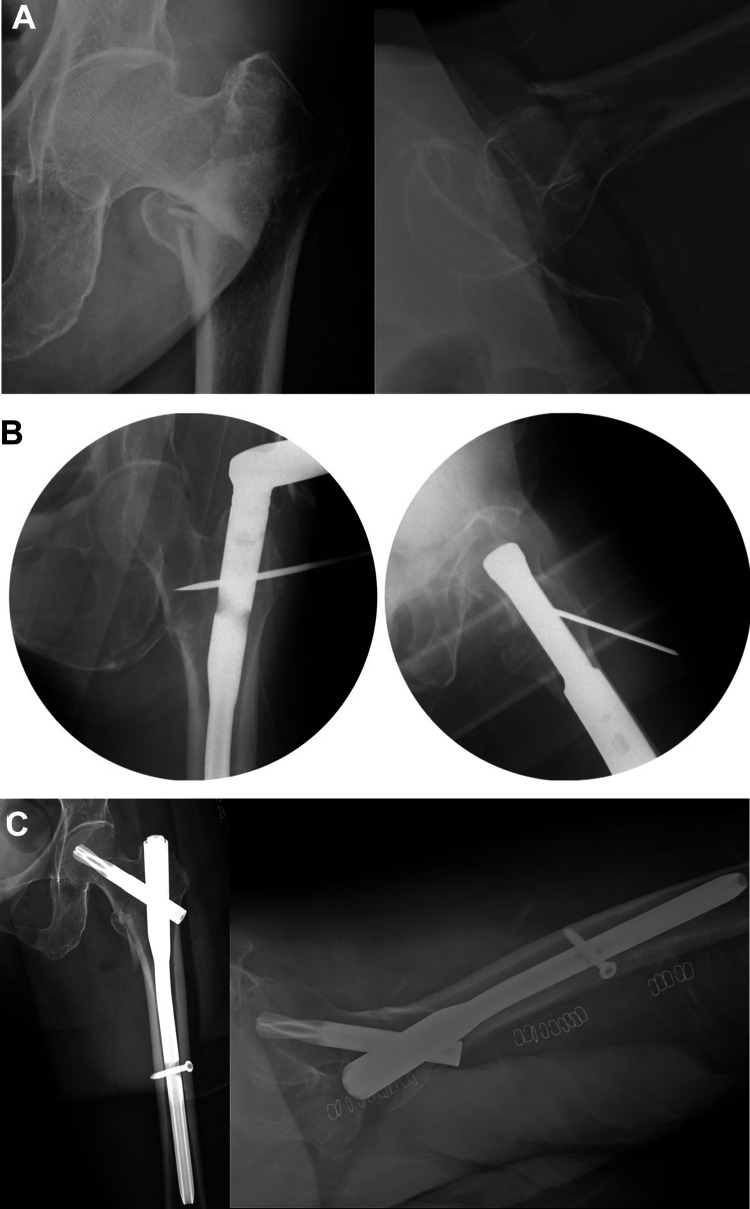
Figure 1.
A 77-year-old female patient with an intertrochanteric fracture on her left femur. A, Preoperative simple radiographs. The proximal femoral head and neck was impacted and collapsed in the varus position into a distal fragment. B, The intraoperative fluoroscopic images. After reduction by manipulation of the distal limb on the fracture table had failed, a steinmann pin was used for reducing the varus displacement by pushing the proximal part medially. The nail was inserted while maintaining the reduced state. C, The immediate postoperative simple radiographs. Direct contacts of the anterior and medial cortices were confirmed.
From the first postoperative day, the patients were encouraged to move using wheelchair and to perform tolerable muscular exercise, including straight leg raises of the affected leg. Then, ambulatory rehabilitation was performed through weight bearing within a pain-tolerable range. Walking aids were used at the initial phase in cases of a risk of falling.
Investigated Variables
Patient demographic characteristics, radiographic measurements, and clinical outcomes were investigated. All measurements were performed independently by 2 orthopedic specialists. If any discrepancies were noted, a consensus discussion was made.
Demographics
Age at operation, sex, body weight, height, body mass index, bone mineral density (BMD), osteoporosis medication, and physical status were investigated. Physical status was evaluated using the American Society of Anesthesiologists classification and Charlson comorbidity index (CCI).15,16
Radiographic measurements
We reviewed simple radiographs (anteroposterior [AP] view for both hips and a translateral view for the injured hip) obtained preoperatively, immediately postoperatively, and at each postoperative follow-up visit. All patients were examined preoperatively via 3DCT. Intraoperative reduction status was assessed via the intraoperative fluoroscopic images.
The AO Foundation/Orthopaedic Trauma Association classification and the presence of GT separation and posteromedial comminution were evaluated by 3DCT. As in the Nakano classification by 4-part concept, the GT was considered as one part.17 Greater trochanter separation was determined when any fragment of the GT was completely separated from the femur on preoperative 3DCT regardless of displacement. A large separation, including the GT and lesser trochanter with or without posteromedial cortex as one fragment, also was considered GT separation. In the characteristic assessment of separated GT, we referred to the method of evaluation of coronal fragments introduced by Cho et al.11 Other radiographic parameters included the neck–shaft angle, tip–apex distance, modified working length of the nail, and anterior/medial cortical contacts based on intraoperative fluoroscopic images and postoperative serial simple radiographs (Figure 2).
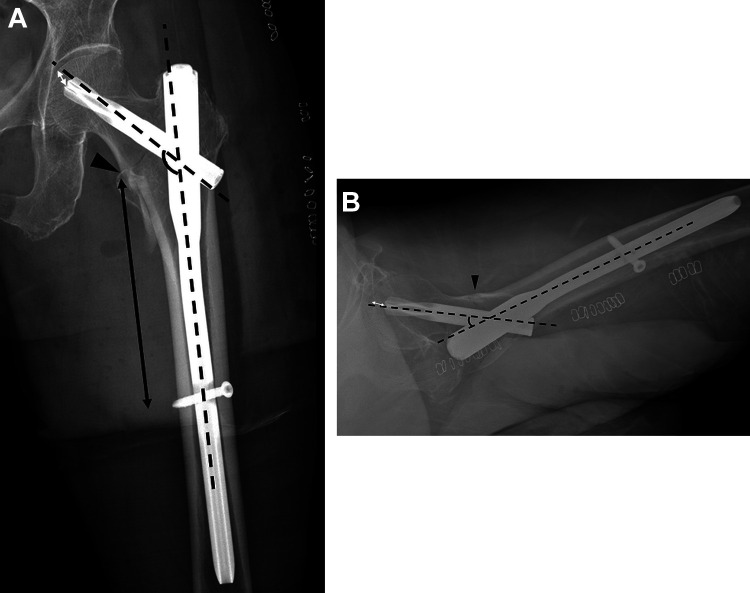
Figure 2.
Neck–shaft angle, tip–apex distance, modified working length of the nail, and anterior/medial cortical contacts were measured using simple radiographs. The neck–shaft angle was measured between the long axis of the femur shaft and the femur neck on both (A) anteroposterior (AP) and (B) translateral views, respectively (the angle between black dashed lines). The tip–apex distance was calculated by the sum of the distances between the tip of the blade and the apex of the femoral head on both AP and translateral views (white double-sided arrows on A and B).18 The modified working length of the nail was defined as the distance between the distal end of the fracture and the distal locking screw on the AP view (black double-sided arrow on A). The anterior/medial cortical contacts were determined if the cortices of the proximal and distal portions were in contact on both the AP and translateral views, respectively (black arrowheads on A and B).
Clinical outcomes
Postoperative simple radiographs and medical charts were reviewed for assessing clinical outcomes. The cases that lost anterior cortical contact with PS postoperatively in the translateral view were defined as “PS group.” Bone union also was evaluated on simple radiographs and was considered adequate when all cortices were connected and consolidated thoroughly without any gap in the AP and translateral views. Nonunion was determined after at least 9 months and was defined as a case in which no further radiologic progression during >3 months occurred in serial radiographs. For functional evaluation, Koval score was used to evaluate ambulatory ability, and the scores were given from 1 point in independent community ambulator to 7 points in nonfunctional ambulator.19 Preinjury and final Koval scores were examined, and deterioration after the injury was determined by the gap between the 2 scores.
Analysis and Statistical Methods
We divided the patients into groups those with and without PS (PS and non-PS groups, respectively). SPSS version 21.0 (SPSS, Inc) was used for statistical analysis. A χ2 test or Fisher exact test was used for comparing frequencies between the 2 groups. The t test or the Mann-Whitney U test was used for comparing means between the 2 groups. Value of P < .05 was considered a statistically significant. In addition, logistic regression analysis with univariate and multivariate analyses were performed for assessing the risk factors of PS. For eliminating confounders among the variables, the variables with a P < .15 in the univariate analysis were included in the multivariate analysis.
Results
Of the 50 patients, 13 (26%) patients experienced PS postoperatively. Compared to the reduction status before the nail insertion, immediate postoperative PS was observed in 9 patients. In the other 4 patients, the reduction status was maintained immediately postoperatively, but PS developed on the radiographs taken 2 weeks postoperatively (Figure 3). There was no additional PS case after 2 weeks postoperatively.
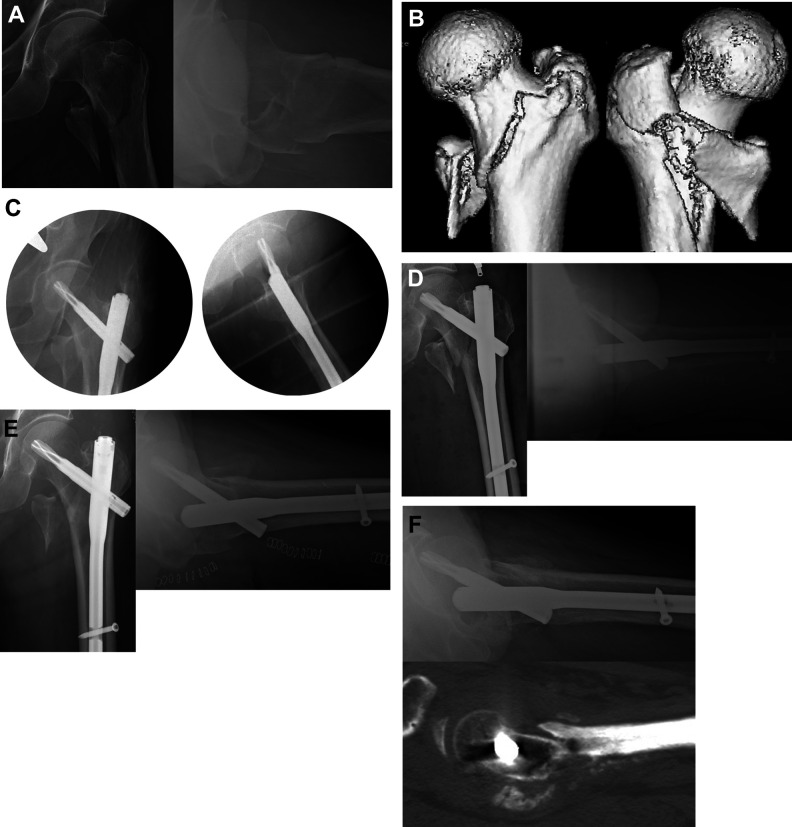
Figure 3.
A 79-year-old male patient. The (A) simple radiographs and (B) 3-dimensional computed tomography (3DCT) images show an intertrochanteric fracture with greater trochanter (GT) separation. The contacts of both medial and anterior cortices were confirmed on both (C) intraoperative fluoroscopic images and (D) immediate postoperative simple radiographs. (E) However, 2 weeks postoperatively, the proximal femoral head and neck was translated posteriorly with loss of cortical contact. (F) This is clearly confirmed by computed tomography (CT) scan taken 5 months after the surgery owing to persistent pain.
Statistically significant differences were noted between the PS and non-PS groups in the prevalence of GT separation, CCI, and mean age (P = .003, .043, and .015, respectively; Table 1). Average time to bone union also was significantly different (4.8 [2-10] and 9.5 [4-14] months in the non-PS and PS groups, respectively; P = .002). Nonunion occurred in 0 and 3 patients in the non-PS and PS groups, respectively (P = .015; Figure 4). In the 3 nonunion patients, their ambulatory ability was poor with Koval score of 6 or 7 points caused by hip pain and frailty. We didn’t perform any additional operations on them because of their medical comorbidities and their reluctance for the operation. There was no cutout, metal failure, and postoperative infection in either group.
Table 1.
Comparison Between the PS Group and the Non-PS Group.
| PS group (n = 13) | Non-PS group (n = 37) | P value | |
|---|---|---|---|
| Demographic characteristics | |||
| Mean age (range, years) | 72.7 (66 to 79) | 78.5 (57 to 95) | .015 |
| Sex | .256 | ||
| Male (%) | 5 (38.5) | 7 (18.9) | |
| Female (%) | 8 (61.5) | 30 (81.1) | |
| Height (range, cm) | 157.6 (135 to 171) | 153.4 (140 to 173) | .141 |
| Weight (range, kg) | 61.9 (49 to 74) | 55 (38 to 90) | .069 |
| BMI (range, kg/m2) | 24.9 (19.5 to 30.7) | 23.3 (16.4 to 37.5) | .229 |
| BMD, trochanter (range) | −2.1 (−3.1 to −0.3, n = 9) | −2.0 (−5.2 to 0.1, n = 23) | .783 |
| BMD, total (range) | −2.5 (−3.7 to −0.7, n = 9) | −2.7 (−5.6 to −1.2, n = 23) | .625 |
| Preoperative osteoporosis medicationa (%) | 2 (15.4) | 2 (5.4) | .275 |
| Postoperative teriparatide injection (%) | 6 (46.2) | 17 (45.9) | .990 |
| ASA | 2.3 (2 to 3) | 2.1 (1 to 3) | .276 |
| CCI | 3.1 (1 to 7) | 1.6 (0 to 9) | .043 |
| Radiographic measurements | |||
| AO/OTA classification; A1/2/3 (%) | 0/10/3 (0/76.9/23.1) | 7/24/6 (18.9/64.9/16.2) | .257 |
| GT separation (%) | 12 (92.3) | 16 (43.2) | .003 |
| PM comminution (%) | 6 (46.2) | 19 (51.4) | 1.000 |
| Modified working length (range, mm) | 84.5 (75 to 96) | 96.4 (58 to 272) | .403 |
| N-S angle in AP view (range, degree) | 129.5 (121 to 142) | 130.3 (119 to 142) | .999 |
| N-S angle in translateral view (range, degree) | 21.1 (10 to 32) | 20.7 (5 to 43) | .893 |
| TAD (range, mm) | 17.3 (13 to 27) | 16.3 (12 to 25) | .568 |
| Bone union | |||
| Time to union (months) | 9.5 (4 to 14, n = 10) | 4.8 (2 to 10) | .002 |
| Nonunion (%) | 3 (23.1) | 0 (0) | .015 |
| Ambulatory ability | |||
| Preinjury Koval score | 1.6 (1 to 6) | 2.1 (1 to 4) | .239 |
| Final Koval score | 4.2 (1 to 7) | 2.8 (1 to 7) | .043 |
| Deterioration after the injury | 2.5 (0 to 5) | 0.8 (0 to 5) | .005 |
Abbreviations: AO/OTA,The AO Foundation/Orthopaedic Trauma Association; ASA, American Society of Anesthesiologists classification; BMI, body mass index; BMD, bone mineral density; CCI, Charlson comorbidity index; GT, greater trochanter, N-S, neck-shaft; PM, posteromedial; PS, posterior sagging; TAD, tip-apex distance.
a All medications were bisphosphonates.
Statistically significant different values (p<0.05) were indicated as bold-faced value.
Figure 4.
A 66-year-old female patient. The (A) simple radiograph and (B) 3-dimensional computed tomography (3DCT) images show an intertrochanteric fracture with greater trochanter (GT) separation. (C) She was treated using a cephalomedullary nail, and intraoperative fluoroscopic images showed adequate reduction (direct contacts of both anterior and medial cortices). (D) However, posterior sagging of the proximal head and neck fragment with a fracture site gap were observed in the translateral view of simple radiographs performed at 2 weeks postoperatively. (E) Seven months later, sliding of blade had occurred, and the gap still remained without evidence of radiologic union.
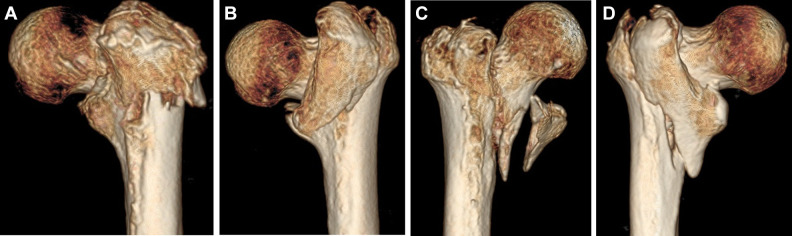
For the subgroup analysis according to the patterns of GT separation, 2 of 28 patients with GT separation had whole lateral wall separation, and the other 26 had coronal split with a posteriorly extended fracture line. In all patients with GT separation, the fracture line extended posteriorly (posterior extension, Figure 5). There were no statistically significant differences for PS among the subgroups (Table 2).
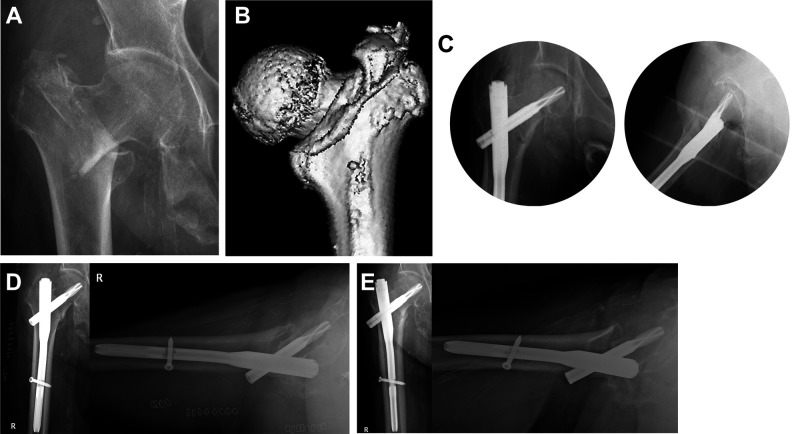
Figure 5.
Greater trochanter (GT) separation showed various patterns in posterior view. For example, there were GT separation with (A) whole lateral wall breakage, (B) coronally separated GT, (C) coronally separated GT and lesser trochanter (LT), and (D) coronally separated as one big fragment involving GT, LT, and posteromedial cortex. All patterns have in common posteriorly extended fracture line.
Table 2.
The Fracture Characteristic Around GT in Cases of GT Separation.
| n = 28 | Coronal split fracture pattern (n = 26) | Whole lateral wall breakage (n = 2) | |||
|---|---|---|---|---|---|
| GT | GLPC | GT/LT | GT/LPC | ||
| PS (n = 12) | 7 | 0 | 0 | 3 | 2 |
| Non-PS (n = 16) | 4 | 4 | 4 | 4 | 0 |
Abbreviations: GLPC, one fragment including greater trochanter, lesser trochanter, and posteromedial cortex; GT, greater trochanter; GT/LT, separated 2 fragments of greater trochanter and lesser trochanter; GT/LPC, separated 2 fragments of greater trochanter and lesser trochanter with posteromedial cortex; PS, posterior sagging.
On multivariate logistic regression analysis that evaluated risk factors for PS, GT separation was a significant risk factor (P = .010; Table 3).
Table 3.
Logistic Regression Model to Identify Risk Factors for PS.a
| Characteristics | N | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Sex | .164 | ||||
| Female | 38 | 0.373 (0.093-1.495) | |||
| Male | 12 | 1 (Reference) | |||
| Laterality | .408 | ||||
| Right | 22 | 1.711 (0.479-6.109) | |||
| Left | 28 | 1 (Reference) | |||
| Age | .072 | .090 | |||
| 77 years or more | 30 | 0.300 (0.081-1.114) | 0.248 (0.049-1.242) | ||
| Less than 77 years | 20 | 1 (Reference) | 1 (Reference) | ||
| ASA | .441 | ||||
| 3 | 15 | 1.687 (0.445-6.395) | |||
| 1 or 2 | 35 | 1 (Reference) | |||
| CCI | .137 | .403 | |||
| 5 or more | 7 | 6.133 (1.032-36.449) | .046 | 4.317 (0.516-36.138) | .177 |
| 2-4 | 15 | 1.673 (0.374-7.484) | .501 | 1.489 (0.252-8.783) | .660 |
| 0-1 | 28 | 1 (Reference) | 1 (Reference) | ||
| BMI | 1.096 (0.943-1.274) | .231 | |||
| AO classification | .582 | ||||
| 3 | 9 | 1.550 (0.326-7.365) | |||
| 1 or 2 | 41 | 1 (Reference) | |||
| GT separation | .012 | .010 | |||
| Presence | 28 | 15.750 (1.851-134.023) | 21.374 (2.098-217.722) | ||
| Absence | 22 | 1 (Reference) | 1 (Reference) | ||
| Posteromedial comminution | .747 | ||||
| Presence | 25 | 0.812 (0.229-2.882) | |||
| Absence | 25 | 1 (Reference) | |||
| BMD (trochanter) | 1.119 (0.520-2.409) | .774 | |||
| BMD (total) | 1.228 (0.555-2.715) | .613 | |||
| Preoperative osteoporosis medication | .274 | ||||
| User | 4 | 3.182 (0.400-25.310) | |||
| Nonuser | 46 | 1 (Reference) | |||
| Postoperative teriparatide injection | .990 | ||||
| User | 23 | 1.008 (0.284-3.583) | |||
| Nonuser | 27 | 1 (Reference) | |||
| Intentional medialization of PHNF | .195 | ||||
| Presence | 15 | 0.336 (0.064-1.749) | |||
| Absence | 35 | 1 (Reference) | |||
| Modified working lengthb | 0.431 (0.967-1.014) | .431 | |||
| N-S angle in AP viewb | 1.000 (0.886-1.129) | .999 | |||
| N-S angle in translateral viewb | 1.005 (0.932-1.084) | .890 | |||
| Tip-apex distanceb | 1.119 (0.907-1.381) | .292 | |||
Abbreviations: AP, anteroposterior; ASA, American Society of Anesthesiologists classification; BMD, bone mineral density, BMI body mass index; CCI, Charlson comorbidity index; GT, greater trochanter; N-S, neck-shaft; PHNF, proximal head and neck fragment; PS, posterior sagging.
a Odds ratios (OR) >1 implies more risk of PS. The variables that P < .15 in univariate analysis were included in multivariate analysis.
b Measurements in immediately postoperative radiographs.
The values of p<0.15 are indicated in bold.
Discussion
Various techniques exist for reducing or maintaining the reduced status of an intertrochanteric fracture during cephalomedullary nailing, such as provisional pin fixation or hook leverage techniques.7-9 Loss-of-reductions still occasionally are reported despite the adequate reduction achieved by those techniques.7
In the present study, we also experienced 13 cases with postoperative LOR in the form of PS even though such reduction-maintaining procedures were used. Provided that LOR is an important factor associated with nonunion, it would be meaningful to investigate the risk factors for LOR.20 Pursuant to these concerns and under the hypothesis that mechanical factors are associated with postoperative PS in patients with intertrochanteric fracture, we attempted to investigate the association between PS and the fracture patterns and patient bone characteristics.
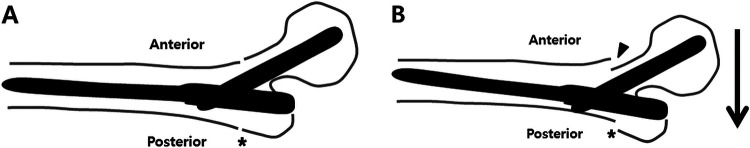
The presence of GT separation showed significant value in predicting postoperative PS. In the treatment of intertrochanteric fractures, the GT is important for supporting the stability of the proximal part of the nail, because it is almost the only point that has cortical contact with the nail in the proximal fragment. The association between GT condition and stability has been reported by Tan et al,21 who mentioned a highly unstable intertrochanteric fracture that had a coronal plane fracture extending from the GT and GT comminution with loss of the support. Therefore, GT separation can result in weak bony support around the proximal part of the nail. All of our patients with GT separation had posterior extension of the fracture line. We theoretically suggested that posteriorly extended GT separation primarily produces posterior instability (Figure 6). Notably, all of our patients with LOR had PS pattern in which a proximal fragment was displaced posteriorly with the loss of anterior cortical contact on the translateral view, which supported our hypothesis. The loss of anterior cortical contact would have caused uncontrolled fracture impaction. Although further research including a biomechanical analysis is necessary, we suggested that the condition of the GT has an important role in maintaining the reduction status because it determines the stability of the proximal area.
Figure 6.
The schematic illustration shows the mechanism of posterior sagging of the proximal fragment in greater trochanter (GT) separation. Each image is shown as the translateral view of simple radiograph. A, An intertrochanteric fracture with posteriorly extended GT separation (asterisk) is reduced and fixed with a cephalomedullary nail. B, However, posterior weak support can cause posterior sagging (arrow) postoperatively, which leads to the loss of anterior cortical contact (arrowhead).
Some studies have reported on GT separation in intertrochanteric fractures,11,22 but to our knowledge none has evaluated its clinical relevance, such as the association with postoperative PS. Ito et al22 especially reported the increased AP diameter of the GT at 2 weeks postoperatively if there was preoperative GT separation. This seems to support our results (Figure 6). In the present study, PS group indicated poor clinical outcomes in terms of bone union and ambulatory ability.
The hip is a common area for osteoporotic fractures, and hip fractures occur more commonly in female and elderly patients.23 The bony trabeculae of the proximal femur are reduced as osteoporosis progresses.24 Poor bone strength in the trochanteric area in the senile population may be attributable to PS. A weak cancellous structure may disrupt stable and tight fitting of the nail in the proximal femur. In our study, no significant difference was noted in terms of BMD and osteoporosis medication. This could be possible because BMD was not performed on all patients and was low enough to correspond to osteoporosis criteria in almost patients in both groups. Although we failed to achieve statistical significances regarding this issue, more systematic studies are necessary to analyse the relationship between bone strength and stable fixation for intertrochanteric fractures.
There are several considerations in our study. First, our results are limited by its small sample size. For example, although the presence of GT separation was a significant risk factor for PS, the subgroup analysis according to its patterns failed to reach statistical significance. However, the prevalence of PS may vary depending on the patterns of GT separation, and these differences may have significant implications for additional surgical procedures. Further research with a large cohort is needed. Second, we evaluated the reduction status using fluoroscopic images intraoperatively and simple radiographs postoperatively. There may be a discrepancy between the 2 methods. In addition, as evaluating the contact of cortical bone only by 2-dimensional radiographs, there may be differences in actual conditions. To reduce this bias, we tried to get consistent radiographs with the patella forward position, and we evaluated by comparing serial radiographs throughout whole period. Moreover, the decision was made through the consensus of all authors if there were discrepancies in the measurements. Finally, the retrospective nature also limits the present results. Most of our patients were elderly, had medical and social problems, which caused them to have much difficulty visiting the clinic regularly. Therefore, there may be more risk for bias than the retrospective studies targeting other patient group.
Conclusion
The presence of GT separation was significantly associated with postoperative PS in patients with intertrochanteric fracture. Greater trochanter separation seems to weaken posterior stability in the proximal fragment caused by inadequate bony support around the proximal part of the nail, thus showing poor clinical outcomes.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Michael Seungcheol Kang, MD, PhD  https://orcid.org/0000-0002-0172-2721
https://orcid.org/0000-0002-0172-2721
References
- 1. Lauritzen JB. Hip fractures: incidence, risk factors, energy absorption, and prevention. Bone. 1996;18(1):65S–75S. [DOI] [PubMed] [Google Scholar]
- 2. Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990;72(1):26–31. [DOI] [PubMed] [Google Scholar]
- 3. Anglen JO, Weinstein JN. American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008;90(4):700–707. doi:10.2106/JBJS.G.00517 [DOI] [PubMed] [Google Scholar]
- 4. Flahiff CM, Nelson CL, Gruenwald JM, Hollis JM. A biomechanical evaluation of an intramedullary fixation device for intertrochanteric fractures. J Trauma. 1993;35(1):23–27. [DOI] [PubMed] [Google Scholar]
- 5. Kuzyk PR, Lobo J, Whelan D, Zdero R, McKee MD, Schemitsch EH. Biomechanical evaluation of extramedullary versus intramedullary fixation for reverse obliquity intertrochanteric fractures. J Orthop Trauma. 2009;23(1):31–38. doi:10.1097/BOT.0b013e318190ea7d [DOI] [PubMed] [Google Scholar]
- 6. Carr JB. The anterior and medial reduction of intertrochanteric fractures: a simple method to obtain a stable reduction. J Orthop Trauma. 2007;21(7):485–489. doi:10.1097/BOT.0b013e31804797cf [DOI] [PubMed] [Google Scholar]
- 7. Kim Y, Dheep K, Lee J, et al. Hook leverage technique for reduction of intertrochanteric fracture. Injury. 2014;45(6):1006–1010. doi:10.1016/j.injury.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 8. Cho JW, Kim HJ, Kim J, Tae WC, Dong JC, Keon OJ. Provisional pin fixation can maintain reduction in A3 intertrochanteric fractures. Arch Orthop Trauma Surg. 2016;136(7):945–955. doi:10.1007/s00402-016-2476-y [DOI] [PubMed] [Google Scholar]
- 9. Jain MJ, Mavani KJ, Patel D. Role of provisional fixation of fracture fragments by Steinmann-pin and technical tips in proximal femoral nailing for intertrochanteric fracture. J Clin Diagn Res. 2017;11(6):RC01–RC05. doi:10.7860/JCDR/2017/25755.10117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shoda E, Kitada S, Sasaki Y, et al. Proposal of new classification of femoral trochanteric fracture by three-dimensional computed tomography and relationship to usual plain X-ray classification. J Orthop Surg (Hong Kong). 2017;25(1):2309499017692700 doi:10.1177/2309499017692700 [DOI] [PubMed] [Google Scholar]
- 11. Cho JW, Kent WT, Yoon YC, et al. Fracture morphology of AO/OTA 31-A trochanteric fractures: A 3D CT study with an emphasis on coronal fragments. Injury. 2017;48(2):277–284. doi:10.1016/j.injury.2016.12.015 [DOI] [PubMed] [Google Scholar]
- 12. Park J, Yang KH. Correction of malalignment in proximal femoral nailing—reduction technique of displaced proximal fragment. Injury. 2010;41(6):634–638. doi:10.1016/j.injury.2010.01.114 [DOI] [PubMed] [Google Scholar]
- 13. Pape HC, Tarkin IS. Intraoperative reduction techniques for difficult femoral fractures. J Orthop Trauma. 2009;23(5 suppl):S6–S11. doi:10.1097/BOT.0b013e31819f2754 [DOI] [PubMed] [Google Scholar]
- 14. Chang SM, Zhang YQ, Ma ZQing, Li, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015;135(6):811–818. doi:10.1007/s00402-015-2206-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. ASA House of Delegates. ASA Physical Status Classification system. 2014. Accessed October 23, 2019 https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system
- 16. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 17. Nakano T. Proximal femoral fracture [in Japanese] Seikeigeka (Orthopaedics). 2014;65:842–850. [Google Scholar]
- 18. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. [DOI] [PubMed] [Google Scholar]
- 19. Koval KJ, Skovron ML, Aharonoff GB, Meadows SE, Zuckerman JD. Ambulatory ability after hip fracture. A prospective study in geriatric patients. Clin Orthop Relat Res. 1995;310:150–159. [PubMed] [Google Scholar]
- 20. Niikura T, Lee SY, Sakai Y, Nishida K, Kuroda R, Kurosaka M. Causative factors of fracture nonunion: the proportions of mechanical, biological, patient-dependent, and patient-independent factors. J Orthop Sci. 2014;19(1):120–124. doi:10.1007/s00776-013-0472-4 [DOI] [PubMed] [Google Scholar]
- 21. Tan BY, Lau AC, Kwek EB. Morphology and fixation pitfalls of a highly unstable intertrochanteric fracture variant. J Orthop Surg (Hong Kong). 2015;23(2):142–145. doi:10.1177/230949901502300204 [DOI] [PubMed] [Google Scholar]
- 22. Ito R, Obara S, Atsumi T. Radiographic analysis of preoperative and postoperative 3DCT images of trochanteric femoral fractures. Showa Univ J Med Sci. 2014;26(4):271–282. [Google Scholar]
- 23. Burge R, Hughes BD, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465–475. doi:10.1359/jbmr.061113 [DOI] [PubMed] [Google Scholar]
- 24. Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am. 1970;52(3):457–467. [PubMed] [Google Scholar]