Abstract
Introduction: While cannabis has been medically legal in Vermont since 2004 and recreationally legal since 2018 there has been minimal published research regarding the use and practices in the adult population. This gap in understanding results in primary care providers having difficulty navigating conversations surrounding cannabinoid use. The purpose of this research was to identify current use and perceptions of cannabinoids, including Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD), in adult primary care patients in Vermont. Methods: An anonymous written survey was given to 1009 Vermont primary care patients aged 18 years and older. All measures were patient-reported and included use of CBD and THC products, perceived helpfulness for certain medical conditions, knowledge of CBD and THC, perceived knowledge of their provider, and concerns regarding cannabis legalization. Results: 45% of adult primary care patients reported using cannabinoids in the past year. Only 18% of patients reported their provider as being a good source of information regarding cannabis. Of the patients who used cannabis in the past year, a majority reported it helpful for conditions such as anxiety and depression, arthritis, pain, sleep, and nausea. Conclusions: Primary care providers need to be knowledgeable about cannabinoids to best support patient care. In addition, with a significant number of patients reporting cannabinoids helpful for medical conditions common in primary care, it is important that research continue to identify the potential benefits and harms of cannabis.
Keywords: cannabinoids, primary care, survey, rural health, medications
Background
Approximately 15% of adults in the United States self-report cannabis use in the past year, with nearly 9% reporting use within the past 30 days.1 Cannabis contains over one hundred cannabinoids with Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most frequently studied.2 THC is a potent cannabinoid known for its psychoactive properties, while CBD is generally considered safer and well-tolerated in humans.3
Medical use in the United States is limited by Drug Enforcement Agency scheduling, variability of state policies, inadequate information about risks, and limited evidence of benefit in prospective human trials. There is some evidence to suggest that cannabinoids (THC, CBD, or a combination) may be helpful for symptoms, including neuropathic pain and spasticity associated with multiple sclerosis. However, data are generally from trials with small sample sizes and are at risk of bias.4 Recent randomized trial data support the use of CBD for managing seizures related to Lennox-Gastaut syndrome.5,6 In this era of evolving evidence and public policy, it is not clear how patients are using cannabinoids to address medical symptoms or conditions. There are some recent data regarding perceptions of risks and benefits by patients using medical cannabis,7,8 however data specific to adult primary care patients are needed, especially related to use of CBD, where little data currently exist. The purpose of this research was to identify current use of cannabinoids (both CBD and THC) in adult primary care patients, including perceived helpfulness in relieving symptoms.
Methods
We conducted an anonymous survey of Vermont primary care patients about their use of cannabinoids, including both CBD and THC. The available population included patients receiving care from a convenience sample of Vermont primary care practices who agreed to allow the survey to be distributed to their adult patients. We targeted at least 1 practice in each of Vermont’s fourteen counties, to ensure geographic representation. Rural location was defined using the US Department of Agriculture Rural-Urban Commuting Area Codes.9
At the time of the survey, Vermont allowed both medical and adult use of cannabis. However, there was not a legal retail market, meaning that cannabis possession under certain limits was allowable, but there were no means to purchase whole plant cannabis or THC for adult recreational use.10 Hemp-derived CBD could be purchased in retail stores across the state. Patients registered in the Vermont Marijuana Registry could obtain whole plant cannabis, THC, or cannabis-derived CBD through a dispensary as part of the medical cannabis program.11
No validated surveys of cannabinoid use have been published to date. We created our own survey with questions adapted from existing surveys, including the Behavioral Risk Factor Surveillance System (BRFSS) and Patient-Reported Outcomes Measurement Information System (PROMIS®).12,13 Additional questions of interest to the investigators were also included. The survey was pilot-tested among a convenience sample of lay people and revised for clarity and comprehensibility. The final survey comprised 17 questions that asked patients about demographics, frequency and amount of CBD and THC use, out-of-pocket costs for CBD and THC, indications for use, and perceptions of benefit. Perceived benefits were assessed with the question “Do you use CBD for any of the following conditions, and if so, how much does it help?” Response categories were “Not helpful”, “Somewhat Helpful”, and “Very helpful”, and respondents only answered for conditions that applied to them. One open-ended question asked “What is your biggest concern regarding cannabis? (CBD, THC, or marijuana)”. The Flesch-Kincaid Grade reading level of the final survey was 7.2.
Practices were recruited by email and telephone by 1 co-investigator (CDM) with a goal of recruiting a broad state-wide sample that included practices organized in the prevalent payment models in the state (academic, hospital-owned, federally qualified health centers, and private practice). The practices were known to the investigators, many of which have participated in prior educational and quality improvement activities with the university and was thus a convenience sample as opposed to a systematic sample of all primary care practices in the state. Upon agreement, 1 co-investigator (NW) delivered 50 paper copies of the survey to the practice. Practices were instructed to hand out the survey to adult patients at the time of check-in, to be completed in the waiting room. There were no other inclusion or exclusion criteria. Completion of the survey implied consent.
Completed surveys were collected from participating practices. The median number of surveys returned per practice was 49, with a range of 4 to 105. While the goal was to return 50 surveys per practice, we allowed 3 weeks for data collection and not all practices were able to recruit 50 subjects, and 1 practice greatly exceed our goal with 105 surveys completed. Survey data were entered into an Excel spreadsheet and subsequently analyzed using Stata 16 (Stata Corp, College Station, TX). We used descriptive statistics to summarize results, and Chi square and t-test for comparisons, where appropriate. Free text comments were categorized using a descriptive approach. Each of the authors categorized the comments separately and the categories were refined by group consensus.
This study was approved by the University of Vermont Committees of Human Research in the Medical Sciences (CHRMS# 00000361).
Results
The survey was distributed to 24 practices in 11 of the 14 counties in Vermont between June 1, 2019 and November 1, 2019. A total of 1009 patients completed the survey. See Table 1. The median age of patients was 51 years and 63% identified as female. About half had completed college, which is higher than the 37% reported in the US Census for Vermont.14 The smoking rate of 24% was slightly higher than the 17.3% reported for the state as a whole in 2017.12 Almost 3 quarters of the patients were in practices in rural areas of Vermont.
Table 1.
Patient and Practice Characteristics (n = 1009).
| Characteristic | Median or Proportion |
|---|---|
| Age, median (range) | 51 (18-96) |
| Gender, % female | 63% |
| Education, % | |
| HS or less | 33% |
| Some college | 21% |
| College or greater | 46% |
| Smoker, % current | 24% |
| Alcohol use past month, % | 58% |
| Chronic pain self-report, % | 36% |
| Rural practice, % | 74% |
| Practice model, % | |
| Academic | 10% |
| Federally Qualified Health Center | 39% |
| Hospital-owned | 38% |
| Private | 13% |
Use of CBD and THC Products
Forty-five percent of primary care patients reported using a cannabis product in the past year, either CBD or THC. Use in the past month of CBD was 21%, and for THC was 19%, and varied considerably by age group. See Figure 1. The highest prevalence of CBD use was observed among adults up to 39 years old (over 30% use in the past month) and decreased with age for those 40 years and older. For THC, the prevalence of use was overall lower (between 10% and 20%) and was more consistent across the age groups. We did not find significant difference in use by gender. The prevalence of CBD use was 19.8% among females and 23% among males (P = .29) and the prevalence of THC use was 20.4% among females and 15.6% among males (P = .06).
Figure 1.
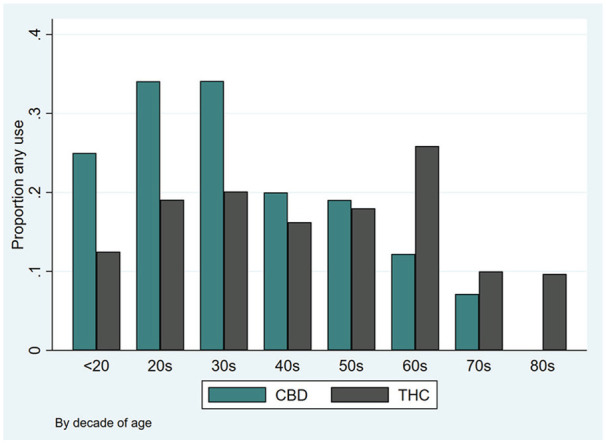
Use of CBD and THC in the past month by age.
The method of use was different for CBD and THC. Of the 316 subjects who reported using CBD, 21% used only topical preparations, 38% used only oral, 7.6% only smoked or vaped, and the remaining 33% used a variety of methods. Of the 303 subjects who reported using THC, less than 1% used topical only, 7.2% used oral only, 46% only smoked or vaped, and the remaining 46% used a variety of methods.
Among those reporting use of cannabis products in the past month, the median monthly spending on CBD was $30 (range 0-400) and the median monthly spending on THC was $40 (range 0-800). At the time of the survey, under Vermont law an individual 21 years of age or older was permitted to cultivate up to 2 mature and 4 immature marijuana plants for personal use,10 which could account for subjects reporting recent use but at zero cost.
Helpfulness
In our assessment of patient perception of the helpfulness of CBD and THC for common symptoms, we found that a large proportion found them to be helpful. Only 9% of the 220 patients with pain who had tried CBD found it to be not helpful, while 53% found it somewhat helpful and 38% found it very helpful. See Table 2. The three symptoms for which the greatest number of patients had tried CBD and THC were pain, depression, and insomnia, with at least 89% finding either cannabinoid product at least somewhat helpful.
Table 2.
How Helpful are CBD and THC Among Those Who Have Tried Them?
| Condition | Na | Not Helpful | Somewhat Helpful | Very Helpful |
|---|---|---|---|---|
| CBD helpfulness | ||||
| Pain | 220 | 9% | 53% | 38% |
| Depression | 187 | 11% | 55% | 34% |
| Sleep | 182 | 8% | 41% | 51% |
| Arthritis | 120 | 11% | 47% | 42% |
| Migraine | 98 | 15% | 50% | 35% |
| THC helpfulness | ||||
| Pain | 185 | 4% | 36% | 59% |
| Depression | 193 | 8% | 36% | 56% |
| Sleep | 204 | 6% | 30% | 63% |
| Arthritis | 79 | 3% | 38% | 59% |
| Migraine | 107 | 8% | 32% | 60% |
The N for each condition varies depending on self-reported data about having the listed condition and having tried CBD or THC as a treatment.
Knowledge
When asked to rate their understanding of the difference between CBD and THC, 29% of patients reported poor understanding, 34% a good understanding, and 37% a very good or excellent understanding. When asked whether their health care provider is a good source of information, we found 55% rated their provider as a good source of information about supplements in general, while only 18% rated their provider as a good source of information regarding cannabis.
Selected Patient Concerns
A total of 358 patients (35%) listed a concern. See Table 3. Common concerns related to the side effects of cannabinoids, the lack of scientific information to guide health care providers and patients, and the potential for negative consequences, such as addiction. Some of the concerns were relatively specific, such as concerns about driving safety and lack of reliable tests for impairment. Other comments were broader and expressed general concerns, both positive and negative about the societal impacts of increasing access to cannabis products. Some patients expressed concern about the lack of access to cannabis products related to cost, lack of insurance coverage, or availability.
Table 3.
Open-ended Patient Concerns Regarding Cannabis.
| Category | Selected Quote |
|---|---|
| Addiction and societal impacts |
“I feel it is habit forming and just one more (drug) especially for the younger generation.”
“My parents did way too much of it” |
| Driving safety | “concerned about people driving under the influence and no clear way of testing yet.” |
| Lack of consumer knowledge | “I’d like to know more about how the body uses CBD to assist pain, anxiety, etc. . .” |
| Lack of insurance coverage and cost | “It would be very helpful if cannabis THC and CBD were covered by insurance, especially for people that are on disability.” |
| Legal issues | “THC is still illegal at the federal level and as a green card holder I cannot break any federal law or risk deportation.” |
| Side effects and lack of scientific knowledge | “Unforeseen negative health effects for those who take it medicinally. For a terminal illness or chronic illness, maybe benefits outweigh the risks.” |
| Uncertainty regarding potency and dosing | “with the unregulation [sic] I worry about products not being what they say they are.” |
Discussion
Overall, we found 45% of Vermont primary care adult patients surveyed reported using cannabinoids in the past year. This study’s reported use of THC in the past month (19%) was very similar to the 15% past-month use reported by the Vermont Behavioral Risk Factor Surveillance System (BRFSS),12 but considerably higher than national estimates of marijuana use of 10.5%.15 The differences in these estimates may be related to differences in use patterns, including state versus national estimates and unselected versus primary care populations, as well as differences in survey terminology (THC vs marijuana).
We found a relatively steep decline in the reported use of CBD starting at age 40, but a steady plateau of reported THC use through the 6th decade. There was a recent Gallup poll that reported 14% of US adults “use CBD products.”16 While the relative declines in CBD use with age from our study are similar to those in the Gallup poll, our THC findings are in contrast to national estimates of marijuana use, which decline steadily from 22% (ages 18-25), to 12.8% (ages 26-49), to 6.8% (ages 50-64), to 2.5% (age 65+).15 This highlights the need to screen all primary care patients for cannabinoid use, including both CBD and THC.
Patients report using cannabinoids for a variety of medical conditions and symptoms. Zaki et al surveyed Canadian subjects before and after the initiation of medical cannabis and found that 70% or more of patients reported improvements in anxiety, post-traumatic stress disorder (PTSD), insomnia, and pain.17 Sexton et al also found patients reported benefits in pain, anxiety, and depression, among other conditions.7 The patients in our study reported similarly high level of helpfulness for a wide variety of symptoms. This perception of the positive effects of CBD and THC are in contrast to the paucity of evidence from well-designed clinical trials supporting the effectiveness of cannabinoids.4,18-21 This may be due to selection bias. High perceived benefit may also be due to placebo effect.
Patients in our study did not perceive their primary care providers to be good sources of information regarding cannabis. Given the large proportion of patients using cannabinoids, primary care providers likely need more education about the potential risks and benefits. We suggest that providers initiate an open dialogue about cannabinoid use with all patients in order to create a safe space for patients to ask questions and monitor use. A recent survey of primary care providers found that 45% were not ready to answer questions about medical cannabis and 77% were interested in learning more information about medical cannabis.22 Our Vermont Department of Health-funded Vermont Academic Detailing Program, operated by the University of Vermont Office of Primary Care (www.vtad.org) offers individual and small group primary care provider education sessions to help close the gaps between patients’ expectations and providers’ knowledge about cannabinoids. Recent articles also attempt to close this knowledge gap.23 In addition, it is important to include cannabis education in health professions curricula to expose students to this topic during their training. A 2017 study demonstrated that only 9% of medical schools currently have medical cannabis included in their curricula.24
The patient-reported comments from our survey represented a range of patient concerns, both positive and negative, regarding cannabinoids. The concerns about the lack of scientific knowledge are well-founded, as are the concerns regarding driving safety.25-27 Given the variability in regulation of CBD and THC among states and in contrast to federal policy, the uncertainties about potency and dosing, as well as access to cannabis, the concerns about addiction and societal impacts are also understandable. We are hopeful that the concerns raised in these comments will help future research as our laws continue to evolve.
This study has several limitations. We conducted our survey in a single state, and while this may limit generalizability to other states or regions, it offers an in-depth look at the particular circumstances in a jurisdiction that permits medical marijuana, has decriminalized recreational use, but has not established a retail marketplace. Vermont is among the most rural and racially homogeneous states in the country, so our findings may not generalize to more urban or diverse parts of the country.14 Our recruitment strategy was a convenience sample of primary care practices in the state. Given that the practices were recruited in part because of past participation in educational and quality improvement activities offered by the academic medical center, they may have been more open to research initiatives. While this may introduce an element of participation bias on the part of the practice, it is not likely that the patients in these practices are systematically different from those in other practices. Given that the survey was offered to patients arriving for primary care office visits, it possible that there was a selection bias among those who were offered the survey by office staff. For example, it is possible that patients with more severe symptoms may not have been offered the survey. Finally, we did not perform formal validation testing of the survey instrument.
The results of our research pose important questions that should be investigated in the future. Considering patients feel that their providers may not be an adequate source of information regarding cannabinoids, it would be interesting to explore the perceived knowledge and perceptions of cannabinoids by primary care providers, to identify opportunities for improvement. Amidst the opioid epidemic, providers are being urged to discuss non-opioid alternatives for chronic pain. A survey of self-reported cannabis users in Washington found that respondents reported using cannabis as an alternative to opioids and other prescriptions for pain medications.7 Further research should consider how to assist primary care providers in having informed conversations about the risks and benefits of cannabis, especially in the setting of chronic pain. Investigating the use of cannabinoids has both patient-centered and public health implications.
Conclusion
Cannabinoids are used by a significant proportion of adult primary care patients. Our findings indicate the importance of asking all patients about cannabis use. Although there is limited research, primary care providers should be aware of the currently available information about potential risks and benefits of CBD and THC to help patients make informed decisions. Monitoring cannabinoid use and trends across states with varying laws may provide valuable insights to guide policy.
Supplemental Material
Supplemental material, Cannabis_survey_2019_06_11_IRB_approved_updates_2019.06.30 for Use and Reported Helpfulness of Cannabinoids Among Primary Care Patients in Vermont by Nicole Wershoven, Amanda G. Kennedy and Charles D. MacLean in Journal of Primary Care & Community Health
Acknowledgments
The authors wish to thank the Vermont primary care practices involved with this study for their willingness to participate. The authors also wish to thank the Larner College of Medicine Office of Primary Care and the AHEC Scholars Program.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Health Resources and Services Administration (U77HP03624). The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
ORCID iD: Amanda G. Kennedy  https://orcid.org/0000-0002-7540-4961
https://orcid.org/0000-0002-7540-4961
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Steigerwald S, Wong PO, Cohen BE, et al. Smoking, vaping, and use of edibles and other forms of Marijuana among U.S. Adults. Ann Intern Med. 2018;169:890-892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bonini SA, Premoli M, Tambaro S, et al. Cannabis sativa: a comprehensive ethnopharmacological review of a medicinal plant with a long history. J Ethnopharmacol. 2018;227:300-315. [DOI] [PubMed] [Google Scholar]
- 3. Campos AC, Fogaça MV, Scarante FF, et al. Plastic and neuroprotective mechanisms involved in the therapeutic effects of cannabidiol in psychiatric disorders. Front Pharmacol. 2017;8:269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313:2456-2473. [DOI] [PubMed] [Google Scholar]
- 5. Devinsky O, Patel AD, Cross JH, et al. Effect of cannabidiol on drop seizures in the lennox-gastaut syndrome. N Engl J Med. 2018;378:1888-1897. [DOI] [PubMed] [Google Scholar]
- 6. Thiele EA, Marsh ED, French JA, et al. Cannabidiol in patients with seizures associated with Lennox-Gastaut syndrome (GWPCARE4): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391:1085-1096. [DOI] [PubMed] [Google Scholar]
- 7. Sexton M, Cuttler C, Finnell JS, Mischley LK. A cross-sectional survey of medical cannabis users: patterns of use and perceived efficacy. Cannabis Cannabinoid Res. 2016;1:131-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Webb CW, Webb SM. Therapeutic benefits of cannabis: a patient survey. Hawaii J Med Public Health. 2014;73:109-111. [PMC free article] [PubMed] [Google Scholar]
- 9. USDA. US Department of Agriculture 2010. Rural-Urban Commuting Area (RUCA) Codes. 2019. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. Accessed April 24, 2020.
- 10. 18 V.S.A. Chapter 86. H.511. An act relating to eliminating penalties for possession of limited amounts of marijuana by adults 21 years of age or older. 2018. https://legislature.vermont.gov/Documents/2018/Docs/ACTS/ACT086/ACT086%20As%20Enacted.pdf. Accessed April 24, 2020.
- 11. 18 V.S.A. Chapter 86, Therapeutic Use of Cannabis. 2019. https://legislature.vermont.gov/statutes/chapter/18/086. Accessed April 24, 2020.
- 12. Vermont Department of Health. Vermont behavioral risk factor surveillance system adult health survey. 2020. https://www.healthvermont.gov/health-statistics-vital-records/population-health-surveys-data/brfss. Accessed April 24, 2020.
- 13. PROMIS® (Patient-Reported Outcomes Measurement Information System). http://www.healthmeasures.net/explore-measurement-systems/promis. Accessed April 24, 2020.
- 14. US Census. QuickFacts Vermont. 2019. https://www.census.gov/quickfacts/VT. Accessed April 24, 2020.
- 15. Substance Abuse and Mental Health Services Administration. 2018. National Survey of Drug Use and Health (NSDUH) Releases. 2018. http://www.samhsa.gov/data/release/2018-national-survey-drug-use-and-health-nsduh-releases. Accessed April 24, 2020.
- 16. Brenan M. 14% of Americans say they use CBD products. Gallup. https://news.gallup.com/poll/263147/americans-say-cbd-products.aspx. Accessed April 24, 2020.
- 17. Zaki P, O’Hearn S, Wolt A, et al. The use of medical cannabis in common medical conditions excluding cancer. J Pain Manag. 2017;10:363-374. [Google Scholar]
- 18. Aviram J, Samuelly-Leichtag G. Efficacy of cannabis-based medicines for pain management: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2017;20:E755-E796. [PubMed] [Google Scholar]
- 19. Hill KP. Medical Marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313:2474-2483. [DOI] [PubMed] [Google Scholar]
- 20. Mücke M, Phillips T, Radbruch L, Petzke F, Häuser W. Cannabis-based medicines for chronic neuropathic pain in adults. Cochrane Database Syst Rev. 2018;3:Cd012182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nugent SM, Morasco BJ, O’Neil ME, et al. The effects of cannabis among adults with chronic pain and an overview of general harms: a systematic review. Ann Intern Med. 2017;167:319-331. [DOI] [PubMed] [Google Scholar]
- 22. Philpot LM, Ebbert JO, Hurt RT. A survey of the attitudes, beliefs and knowledge about medical cannabis among primary care providers. BMC Fam Pract. 2019;20:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Slawek D, Meenrajan SR, Alois MR, Comstock Barker P, Estores IM, Cook R. Medical cannabis for the primary care physician. J Prim Care Community Health. 2019;10:2150132719884838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Evanoff AB, Quan T, Dufault C, Awad M, Bierut LJ. Physicians-in-training are not prepared to prescribe medical marijuana. Drug Alcohol Depend. 2017;180:151-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Micallef J, Dupouey J, Jouve E, et al. Cannabis smoking impairs driving performance on the simulator and real driving: a randomized, double-blind, placebo-controlled, crossover trial. Fundam Clin Pharmacol. 2018;32:558-570. [DOI] [PubMed] [Google Scholar]
- 26. Ogourtsova T, Kalaba M, Gelinas I, Korner-Bitensky N, Ware MA. Cannabis use and driving-related performance in young recreational users: a within-subject randomized clinical trial. CMAJ Open. 2018;6:E453-E462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tank A, Tietz T, Daldrup T, et al. On the impact of cannabis consumption on traffic safety: a driving simulator study with habitual cannabis consumers. Int J Legal Med. 2019;133:1411-1420. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Cannabis_survey_2019_06_11_IRB_approved_updates_2019.06.30 for Use and Reported Helpfulness of Cannabinoids Among Primary Care Patients in Vermont by Nicole Wershoven, Amanda G. Kennedy and Charles D. MacLean in Journal of Primary Care & Community Health


