Abstract
Background and Aim
Currently, the number of patients with coronavirus disease 2019 (COVID-19) infection is increasing rapidly worldwide. In this study, we aimed to assess whether diabetes mellitus (DM) would increase the risk of severe infection and death in patients with COVID-19.
Methods
We systematically searched the PubMed, Web of Science, MedRxiv and COVID-19 academic research communication platform for studies reporting clinical severity and/or overall mortality data on DM in patients with COVID-19 published up to July 10, 2020. The primary outcome was to compare the severe infection rate and mortality rate in COVID-19 patients with and without DM, and to calculate the odds ratio (OR) and 95% confidence interval (CI).
Results
A total of 76 studies involving 31,067 patients with COVID-19 were included in our meta-analysis. COVID-19 patients with DM had higher severe infection and case-mortality rates compared with those without DM (21.4 vs. 10.6% and 28.5 vs. 13.3%, respectively, all p <0.01). COVID-19 patients with DM were at significantly elevated risk of severe infection (OR = 2.38, 95% CI: 2.05–2.78, p <0.001) and mortality (OR = 2.21, 95% CI: 1.83–2.66, p <0.001).
Conclusion
DM is associated with increased risk of severe infection and higher mortality in patients with COVID-19. Our study suggests that clinicians should pay more attention to the monitoring and treatment of COVID-19 patients with DM.
Key Words: COVID-19, Diabetes mellitus, Disease severity, Mortality, Meta-analysis
Introduction
Since first reported in December 2019, coronavirus disease 2019 (COVID-19), caused by the new corona virus SARS-CoV-2, has spread all over the world and has been defined as a global pandemic by the World Health Organization (WHO) (1). COVID-19 is now a worldwide public health concern, the number of confirmed cases is increasing exponentially worldwide (2). By July 1, 2020, there were more than ten million confirmed cases and half a million deaths from COVID-19 in more than 200 countries (3).
The clinical manifestations of patients after SARS-CoV-2 infection are heterogeneous. Mild cases are mainly characterized by flu-like symptoms, such as cough and fever. However, patients with severe cases may die due to severe pneumonia, acute respiratory distress syndrome, multiple organ failure, or sepsis (4). According to a report from the Chinese Center for Disease Control and Prevention, the case-fatality rate was 2.3% in 44,672 patients with confirmed cases of COVID-19, and all death cases were among critical patients (5). Therefore, it is very important to identify predictors of severe infection and mortality for effective treatment and therapeutic intervention.
Diabetes mellitus (DM) is a common underlying disease in patients with COVID-19. A meta-analysis including 76,993 patients with confirmed cases showed that the prevalence of DM in patients with COVID-19 was 7.87% (95% confidence interval [CI]: 6.57% - 9.28%) (6). Emerging evidence suggests that COVID-19 patients with DM have an increased risk of complications and poor prognosis (7). A recent study showed that COVID-19 patients with DM had higher levels of serum inflammation-related biomarkers and increased risk of severe pneumonia, excessive uncontrolled inflammatory responses, and hypercoagulability compared with non-diabetic patients (8). In the present study, we performed a systematic review and meta-analysis to investigate the association of DM with disease severity and mortality in patients with COVID-19 and to provide reliable evidence for improved treatment and control of COVID-19.
Methods
Our literature search was conducted in accordance with the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines (9) and was performed following the Preferred Reporting Items for Meta-Analyses (PRISMA) statement (10).
Search Strategy
We searched PubMed, the Web of Science, MedRxiv (https://www.medrxiv.org) and COVID-19 academic research communication platform (http://medjournals.cn/2019NCP/index.do) on March 31, 2020 and up-dated the search on July 10, 2020. The search was limited to papers published in English or Chinese language. The following mesh-terms and free words were used: “COVID-19”, “coronavirus disease 2019”, “novel coronavirus pneumonia”, “2019-nCoV”, “SARS-CoV-2”, “clinical characteristics”, “clinical features”, “outcome”, “severe infection”, “severe illness”, “severity”, “alive”, “death”, “mortality”, “non-survivor”, and “deceased”, alone and in combination. The title, abstract, and full text of all documents identified with the search criteria were assessed. The reference lists of all studies were also analyzed to identify additional eligible studies. Only those research articles that reported data of DM and at least one outcome of interest were included in this meta-analysis. The primary outcomes were the pooled severe infection and mortality risk in COVID-19 patients with DM. Studies were excluded if they included duplicated results, reported insufficient data, or were case reports, case series with less than 20 patients, letters, review articles, editorial comments, guidelines or studies with animals. Studies that reported only deaths or critically ill cases were excluded. When single-center studies from the same hospital reported the same outcome with the study period overlapping by at least 50%, outcome from the study with the largest number of patients was extracted.
Study Selection
Two investigators (MJS and LXS) independently scanned all the titles, abstracts and full text to identify studies that met the inclusion criteria and extracted data from these studies. Discrepancies between reviewers were resolved by discussion with a third reviewer (QLG) or by consensus. In this study, patients with severe infection were defined as those who met the diagnostic criteria of the Guidelines on the Diagnosis and Treatment of Novel Coronavirus Pneumonia (11) or were admitted to intensive care units.
Data Collection and Quality Assessment
Data extraction and quality assessment of the included studies were also performed by two investigators (MJS and LXS) who performed the literature search. Data were collected and entered into a spreadsheet. We extracted the following variables: first author, study period, location, sample size, patient age range, sex, the number of participants with severe infection and/or death, and the prevalence of comorbidities. We used the Newcastle-Ottawa Scale (NOS) to assess the risk of bias of the included studies, and a NOS score >7 was considered good quality (12).
Statistical Analysis
Statistical analysis was performed using the Meta package within R software (version 3.6.3). The OR and its 95% CI were used to estimate the corelation between DM and severe infection and mortality in patients with COVID-19. We used a random-effects model to synthesize data for the relevant outcomes. Heterogeneity was evaluated using the χ2 test and the I 2 statistic. For the χ2 test, the significant heterogeneity among studies was indicated with a Cochran's Q p-value of <0.10. I 2 values of 25%, 25–50%, or 50% indicated low, moderate, or high heterogeneity, respectively (13). If there was high heterogeneity, a sensitivity analysis was performed by removing each study from the meta-analysis (14). Forest plots visually showed effect estimates of the included studies. We used funnel plots, Begg's test, and Egger's test to evaluate potential publication bias. A two tailed p <0.05 was considered statistically significant.
Results
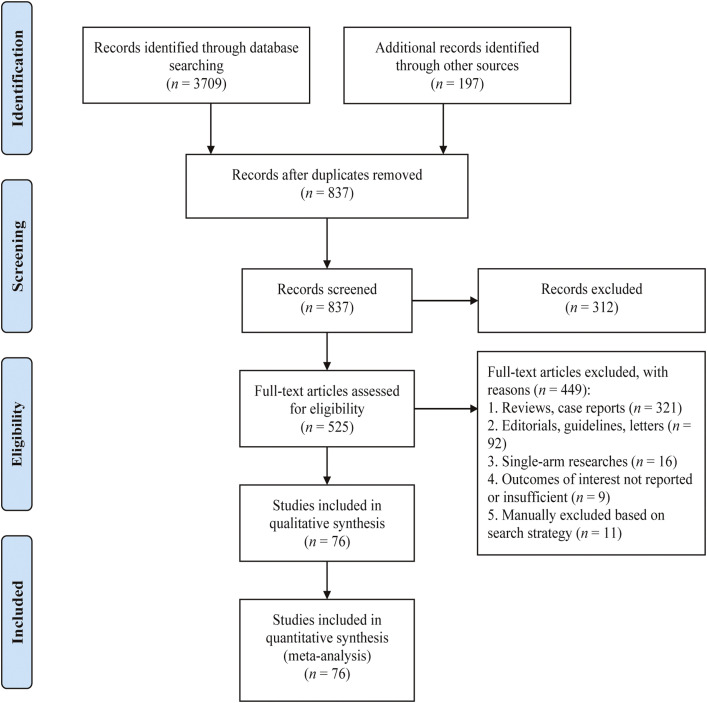
The flow of studies through our meta-analysis is depicted in Figure 1 . A total of 76 studies with 31,067 patients were eventually included in our study (8,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89). The characteristics of the included studies are described in Supplementary Table 1. The number of confirmed COVID-19 cases in each study ranged from 41–3,841. The proportion of diabetic patients ranged from 3.3–68.5%. As outlined in Supplementary Table 2, all articles included in the meta-analysis had high quality according to the NOS tool.
Figure 1.
Flow diagram for literature selection.
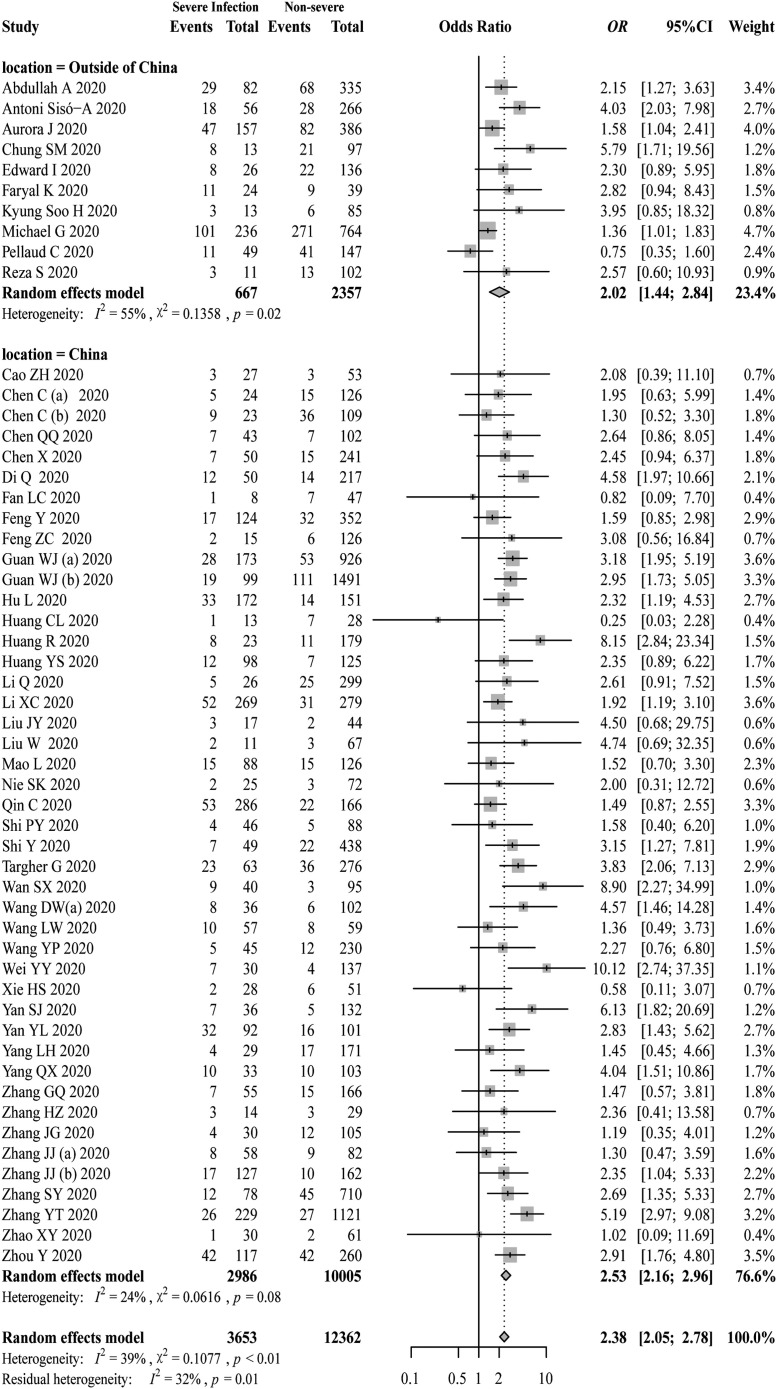
Pooled Analysis of Severe Infection
There were 54 studies reported the association between DM and severe infection in patients with COVID-19. COVID-19 patients with DM had higher severe infection rate compared with those non-diabetic patients (21.4 vs. 10.6%, p <0.01). DM was found to be associated with a significantly greater risk of severe COVID-19 infection (pooled OR = 2.38, 95% CI: 2.05–2.78, p <0.001; I 2 = 39%, p <0.01, Figure 2 ). The result remained similar for subgroup analysis according to study location (p = 0.24).
Figure 2.
Forest plot for the association of DM and disease severity in patients with COVID-19.
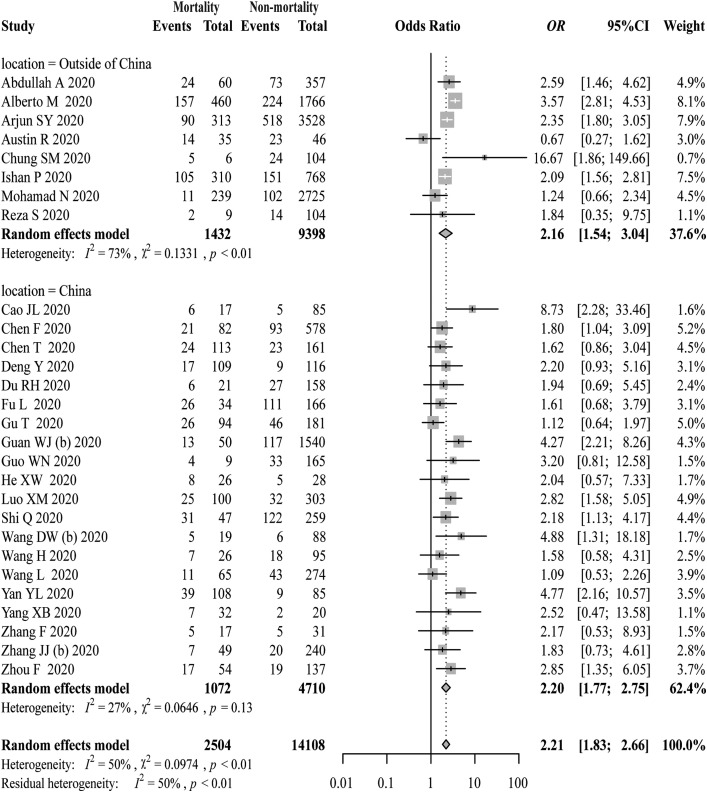
Pooled Analysis of Mortality
A total of 28 studies reported an association between DM and mortality in patients with COVID-19. COVID-19 patients with DM had higher mortality rate compared with those non-diabetic patients (28.5 vs. 13.3%, p <0.01). COVID-19 patients with DM had a higher risk of death (pooled OR = 2.21, 95% CI: 1.83–2.66, p <0.001; I 2 = 50%, p <0.01, Figure 3 ). The subgroup analyses in different locations showed similar result (p = 0.93).
Figure 3.
Forest plot for the association of DM and mortality in patients with COVID-19.
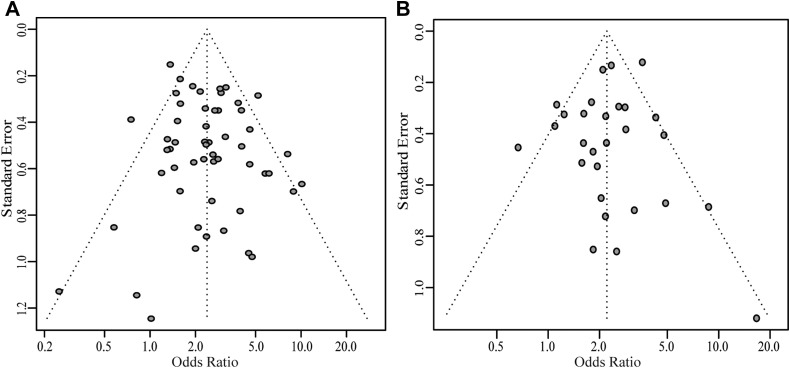
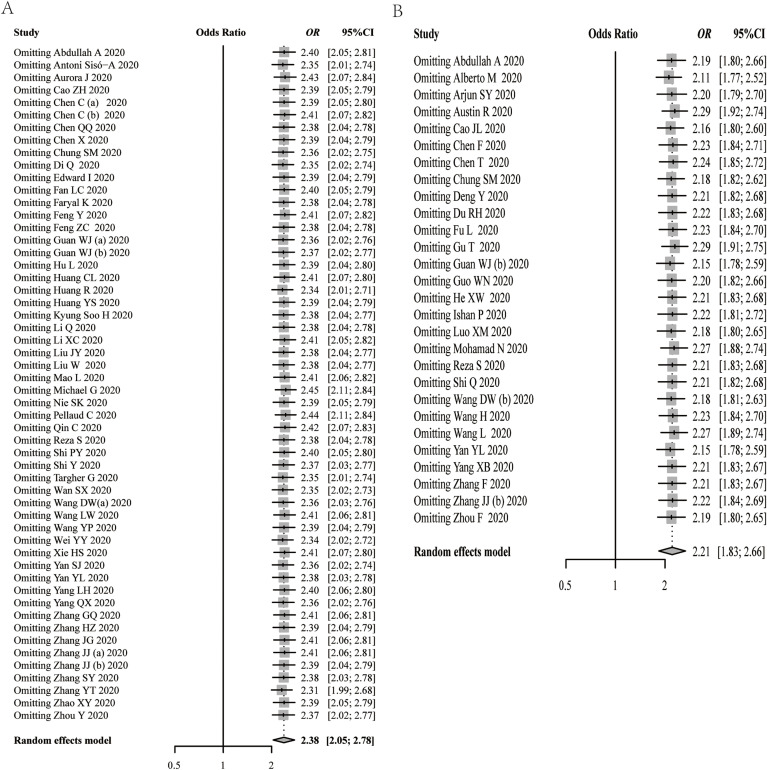
Sensitivity Analysis and Publication Bias
The sensitivity analysis showed that none of the studies remarkably affected the pooled ORs and CIs (Supplementary Figure 1). Visual inspection of the both funnel plots revealed symmetry, indicating a low risk of publication bias (Figure 4 ). The Begg's test and Egger's test for the severe infection outcome (Begg's test: p = 0.96, Egger's test: p = 0.18) and for mortality outcome (Begg's test: p = 0.25, Egger's test: p = 0.48), respectively, confirmed that there was no statistically publication bias.
Figure 4.
Funnel plot for the assessment of publication bias. (A) Outcome of severe infection; (B) Outcome of mortality.
Discussion
To our knowledge, this meta-analysis used the largest number of studies and the largest sample size so far to evaluate the correlation between DM and the risk of disease severity and death in COVID-19. Our results showed that diabetic patients with COVID-19 had higher severe infection and case-fatality rates compared with non-diabetic patients, and DM was associated with an increased risk of severe infection and mortality in patients with COVID-19.
It remains unclear whether DM would increase the risk of SARS-CoV-2 infection, however, it has been observed that DM is a common underlying disease in patients with COVID-19. An early meta-analysis of 6 studies with 1,527 patients showed that hypertension (17.1%), cardio-cerebrovascular disease (16.4%), and DM (9.7%) were the most prevalent cardiovascular metabolic comorbidities in COVID-19 patients (7). An updated meta-analysis, including 83 studies and nearly 79,000 patients with laboratory-confirmed cases of COVID-19 showed that the prevalence of DM among COVID-19 patients was 14.34% (95% CI: 12.62–16.06 %) (90). Therefore, patients with DM are suggested to pay attention to self-protection, and maintain good blood glucose control to reduce the risk of infection.
Our results showed that diabetic patients with COVID-19 had higher severe infection and case-fatality rates. A retrospective review of 25 patients with COVID-19 who died showed that all had one or more underlying diseases, of which DM accounted for 40% (91). An analysis from Italy showed that the average number of complications is 2.7 in patients who died from COVID-19, and this study suggests that the high prevalence of complications is one of the important reasons for the high mortality of COVID-19 patients in Italy (92). Our results support most of the current research conclusions (93,94) and highlight the importance of DM in the stratification of critical illness and death risk in patients with COVID-19.
However, so far, the mechanism leading to worse clinical outcomes in COVID-19 patients with DM has not been fully clarified. One possible reason is that DM is related to the activation of the renin-angiotensin system, and patients with DM are often treated with angiotensin-converting enzyme inhibitors (ACEIs) and/or angiotensin receptor blockers (ARBs), which may both lead to the increased expression of ACE2 in tissues, promoting virus absorption and increasing the risk of severe infection in patients with DM (95). Secondly, DM may induce the hypercoagulable state in patients with COVID-19, resulting in worse outcomes of these patients. Studies have reported that diabetic patients with COVID-19 had increased risk of hypercoagulability, and many severe and fatal patients with COVID-19 seemed to eventually die of small pulmonary embolism (96). Futhermore, DM patients are in a state of chronic inflammation. Inflammatory markers such as C-reactive protein, erythrocyte sedimentation rate and interleukin-6 are elevated in diabetic patients with COVID-19, which may contribute to a cytokine storm and in turn, lead to severe pneumonia and the eventual death outcome (97).
At present, experts from all over the world are providing advice on the management of diabetic patients with COVID-19. The suggestion from the Chinese Diabetes Society points out that hospitalized COVID-19 patients with DM should receive individualized blood glucose control goals and treatment strategies according to their condition (98). Klonoff DC, et al. (99) pointed out the importance of careful use of glucocorticoids, strengthened blood glucose monitoring, strengthened contacts with health-care staff, and cautious cessation of ACEIs or ARBs. Advice from China called for the “Seven Treasures” policy for DM management, including health education, balanced nutrition, physical activity, standardized medication, blood glucose monitoring, regular schedule, and care for mental health (100). The European Society of Endocrinology also suggested that endocrinologists provide online/email/phone consultation services and closely monitor glycemic control in patients with DM during the COVID-19 pandemic (101). However, in view of the pandemic state of COVID-19, the evidence available at present is still limited. More studies are needed to determine the best treatment for COVID-19 patients with DM in the future, and the current clinical management should be revised promptly according to the latest evidence.
This study has several limitations. First, while we excluded some studies manually to avoid including any duplicate studies, it is still possible that some overlapping patients were included in our meta-analysis, which might have some slight impact on our results. Second, the patients with COVID-19 in our meta-analysis had a high case-fatality rate, which may be due to these included studies during the early stages of the outbreak involving a higher proportion of severely ill patients. Therefore, the relationship between DM and mortality risk in mildly ill patients still needs to be evaluated. Third, different studies have different definitions of severe infection; at the same time, most studies were not adjusted for various confounding factors, such as data on diabetic medications, which might both cause bias in the results. Forth, the majority of the included studies in our meta-analysis were retrospective case-control studies, as the disease spreads around the world, it is hoped that other cohort studies and randomized studies will report more clinical data to verify our results, and further examine the effect of DM type, DM duration, presence of DM-related complications and glycaemic controls on prognosis of COVID-19.
In conclusion, DM is related to a higher risk of severe infection and mortality. Therefore, it is needed to protect DM population from COVID-19 infection. Meanwhile, special care and monitoring are required in COVID-19 patients with DM to improve prognosis.
Conflicts of Interest
All authors report no conflicts of interest related to this manuscript.
Acknowledgments
This study was supported by National Key R&D Program of China (Grant number: 2016YFC0900905). We thank AJE (American Journal Experts) and “HOME for Researchers” for linguistic assistance.
Funding: National Key R&D Program of China (2016YFC0900905).
(ARCMED_2020_603)
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.arcmed.2020.07.005.
Supplementary data
Supplementary Figure.
References
- 1.Cucinotta D., Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahn D.-G., Shin H.-J., Kim M.-H. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19) J Microbiol Biotechnol. 2020;30:313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Coronavirus disease (COVID-2019) situation report - 163. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- 4.Li L.-Q., Huang T., Wang Y.-Q. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92:577–583. doi: 10.1002/jmv.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z., McGoogan J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 6.Emami A., Javanmardi F., Pirbonyeh N. Prevalence of Underlying Diseases in Hospitalized Patients with COVID-19: a Systematic Review and Meta-Analysis. Arch Acad Emerg Med. 2020;8:e35. [PMC free article] [PubMed] [Google Scholar]
- 7.Li B., Yang J., Zhao F. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo W., Li M., Dong Y. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020:e3319. doi: 10.1002/dmrr.3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stroup D.F., Berlin J.A., Morton S.C. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 10.Moher D., Liberati A., Tetzlaff J. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 11.National Health Commission of China . 2020. Diagnosis and treatment protocol for novel coronavirus pneumonia (7rd interim edition.http://www.nhc.gov.cn/jkj/s3577/202003/4856d5b0458141fa9f376853224d41d7/files/4132bf035bc242478a6eaf157eb0d979.pdf [Google Scholar]
- 12.Wells G., Shea B., O’Connell D. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Ottawa Hospital Research Institute.
- 13.Higgins J.P., Thompson S.G., Deeks J.J. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Viechtbauer W., Cheung M.W. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. 2010;1:112–125. doi: 10.1002/jrsm.11. [DOI] [PubMed] [Google Scholar]
- 15.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang D., Hu B., Hu C. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J.J., Dong X., Cao Y.Y. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730–1741. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 18.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guan W.J., Ni Z.Y., Hu Y. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu W., Tao Z.W., Wang L. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J (Engl) 2020;133:1032–1038. doi: 10.1097/CM9.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen C., Chen C., Yan J.T. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E008. doi: 10.3760/cma.j.cn112148-20200225-00123. [Article in Chinese] [DOI] [PubMed] [Google Scholar]
- 22.Qin C., Zhou L., Hu Z. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;71:762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.He X.W., Lai J.S., Cheng J. Impact of complicated myocardial injury on the clinical outcome of severe or critically ill COVID-19 patients. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E011. doi: 10.3760/cma.j.cn112148-20200228-00137. [Article in Chinese] [DOI] [PubMed] [Google Scholar]
- 25.Shi Y., Yu X., Zhao H. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24:108. doi: 10.1186/s13054-020-2833-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wan S., Xiang Y., Fang W. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020;92:797–806. doi: 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deng Y., Liu W., Liu K. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 in Wuhan, China: a retrospective study. Chin Med J (Engl) 2020;133:1261–1267. doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen T., Wu D., Chen H. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guan W.J., Liang W.H., Zhao Y. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55:2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang L., Li X., Chen H. Coronavirus Disease 19 Infection Does Not Result in Acute Kidney Injury: An Analysis of 116 Hospitalized Patients from Wuhan, China. Am J Nephrol. 2020;51:343–348. doi: 10.1159/000507471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cao J., Tu W.J., Cheng W. Clinical Features and Short-term Outcomes of 102 Patients with Corona Virus Disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71:748–755. doi: 10.1093/cid/ciaa243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xie H., Zhao J., Lian N. Clinical characteristics of non-ICU hospitalized patients with coronavirus disease 2019 and liver injury: A retrospective study. Liver Int. 2020;40:1321–1326. doi: 10.1111/liv.14449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang L., He W., Yu X. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80:639–645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Du R.H., Liang L.R., Yang C.Q. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55:2000524. doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Feng Y., Ling Y., Bai T. COVID-19 with Different Severities: A Multicenter Study of Clinical Features. Am J Respir Crit Care Med. 2020;201:1380–1388. doi: 10.1164/rccm.202002-0445OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li X., Xu S., Yu M. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wei Y.Y., Wang R.R., Zhang D.W. Risk factors for severe COVID-19: Evidence from 167 hospitalized patients in Anhui, China. J Infect. 2020;81:e89–e92. doi: 10.1016/j.jinf.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang G., Hu C., Luo L. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127:104364. doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y.T., Deng A.P., Hu T. Clinical outcomes of COVID-19 cases and influencing factors in Guangdong province. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:E057. doi: 10.3760/cma.j.cn112338-20200318-00378. [Article in Chinese] [DOI] [PubMed] [Google Scholar]
- 40.Chen Q., Zheng Z., Zhang C. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection. 2020 doi: 10.1007/s15010-020-01432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhao X.Y., Xu X.X., Yin H.S. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis. 2020;20:311. doi: 10.1186/s12879-020-05010-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yan Y., Yang Y., Wang F. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care. 2020;8:e001343. doi: 10.1136/bmjdrc-2020-001343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nikpouraghdam M., Jalali Farahani A., Alishiri G. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: A single center study. J Clin Virol. 2020;127:104378. doi: 10.1016/j.jcv.2020.104378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang D., Yin Y., Hu C. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit Care. 2020;24:188. doi: 10.1186/s13054-020-02895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hu L., Chen S., Fu Y. Risk Factors Associated with Clinical Outcomes in 323 COVID-19 Hospitalized Patients in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Itelman E., Wasserstrum Y., Segev A. Clinical Characterization of 162 COVID-19 patients in Israel: Preliminary Report from a Large Tertiary Center. Isr Med Assoc J. 2020;22:271–274. [PubMed] [Google Scholar]
- 47.Huang R., Zhu L., Xue L. Clinical findings of patients with coronavirus disease 2019 in Jiangsu province, China: A retrospective, multi-center study. PLoS Negl Trop Dis. 2020;14:e0008280. doi: 10.1371/journal.pntd.0008280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hong K.S., Lee K.H., Chung J.H. Clinical Features and Outcomes of 98 Patients Hospitalized with SARS-CoV-2 Infection in Daegu, South Korea: A Brief Descriptive Study. Yonsei Med J. 2020;61:431–437. doi: 10.3349/ymj.2020.61.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shi Q., Zhang X., Jiang F. Clinical Characteristics and Risk Factors for Mortality of COVID-19 Patients With Diabetes in Wuhan, China: A Two-Center, Retrospective Study. Diabetes Care. 2020;43:1382–1391. doi: 10.2337/dc20-0598. [DOI] [PubMed] [Google Scholar]
- 50.Targher G., Mantovani A., Wang X.B. Patients with diabetes are at higher risk for severe illness from COVID-19. Diabetes Metab. 2020 doi: 10.1016/j.diabet.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yang Q., Xie L., Zhang W. Analysis of the clinical characteristics, drug treatments and prognoses of 136 patients with coronavirus disease 2019. J Clin Pharm Ther. 2020;45:609–616. doi: 10.1111/jcpt.13170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang L., Liu J., Zhang R. Epidemiological and clinical features of 200 hospitalized patients with corona virus disease 2019 outside Wuhan, China: A descriptive study. J Clin Virol. 2020;129:104475. doi: 10.1016/j.jcv.2020.104475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chen F., Sun W., Sun S. Clinical characteristics and risk factors for mortality among inpatients with COVID-19 in Wuhan, China. Clin Transl Med. 2020;10:e40. doi: 10.1002/ctm2.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Khamis F., Al-Zakwani I., Al Naamani H. Clinical characteristics and outcomes of the first 63 adult patients hospitalized with COVID-19: An experience from Oman. J Infect Public Health. 2020;13:906–913. doi: 10.1016/j.jiph.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shahriarirad R., Khodamoradi Z., Erfani A. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infect Dis. 2020;20:427. doi: 10.1186/s12879-020-05128-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cao Z., Li T., Liang L. Clinical characteristics of Coronavirus Disease 2019 patients in Beijing, China. PLoS One. 2020;15:e0234764. doi: 10.1371/journal.pone.0234764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang Y., Liao B., Guo Y. Clinical Characteristics of Patients Infected With the Novel 2019 Coronavirus (SARS-Cov-2) in Guangzhou, China. Open Forum Infect Dis. 2020;7:ofaa187. doi: 10.1093/ofid/ofaa187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chung S.M., Lee Y.Y., Ha E. The Risk of Diabetes on Clinical Outcomes in Patients with Coronavirus Disease 2019: A Retrospective Cohort Study. Diabetes Metab J. 2020;44:405–413. doi: 10.4093/dmj.2020.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang S.Y., Lian J.S., Hu J.H. Clinical characteristics of different subtypes and risk factors for the severity of illness in patients with COVID-19 in Zhejiang, China. Infect Dis Poverty. 2020;9:85. doi: 10.1186/s40249-020-00710-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Morrison A.R., Johnson J.M., Griebe K.M. Clinical characteristics and predictors of survival in adults with coronavirus disease 2019 receiving tocilizumab. J Autoimmun. 2020 doi: 10.1016/j.jaut.2020.102512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang J.J., Cao Y.Y., Tan G. Clinical, radiological and laboratory characteristics and risk factors for severity and mortality of 289 hospitalized COVID-19 patients. Allergy. 2020 doi: 10.1111/all.14496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pellaud C., Grandmaison G., Pham Huu Thien H.P. Characteristics, comorbidities, 30-day outcome and in-hospital mortality of patients hospitalised with COVID-19 in a Swiss area - a retrospective cohort study. Swiss Med Wkly. 2020;150:w20314. doi: 10.4414/smw.2020.20314. [DOI] [PubMed] [Google Scholar]
- 63.Borobia A.M., Carcas A.J., Arnalich F. A cohort of patients with COVID-19 in a major teaching hospital in Europe. Preprint at medRxiv. 2020 doi: 10.1101/2020.04.29.20080853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Huang Y., Lyu X., Li D. A cohort study of 223 patients explores the clinical risk factors for the severity diagnosis of COVID-19. Preprint at medRxiv. 2020 doi: 10.1101/2020.04.18.20070656. [DOI] [Google Scholar]
- 65.Zhou Y., Yang Z., Guo Y. A New Predictor of Disease Severity in Patients with COVID-19 in Wuhan, China. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.24.20042119. [DOI] [Google Scholar]
- 66.Luo X., Xia H., Yang W. Characteristics of patients with COVID-19 during epidemic ongoing outbreak in Wuhan, China. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.19.20033175. [DOI] [Google Scholar]
- 67.Argenziano M.G., Bruce S.L., Slater C.L. Characterization and clinical course of 1000 Patients with COVID-19 in New York: retrospective case series. Preprint at medRxiv. 2020 doi: 10.1101/2020.04.20.20072116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Alshukry A., Ali H., Ali Y. Clinical characteristics of Coronavirus Disease 2019 (COVID-19) patients in Kuwait. Preprint at medRxiv. 2020 doi: 10.1101/2020.06.14.20131045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yan S., Song X., Lin F. Clinical Characteristics of Coronavirus Disease 2019 in Hainan, China. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.19.20038539. [DOI] [Google Scholar]
- 70.Paranjpe I., Russak A., De Freitas J.K. Clinical Characteristics of Hospitalized Covid-19 Patients in New York City. Preprint at medRxiv. 2020 doi: 10.1101/2020.04.19.20062117. [DOI] [Google Scholar]
- 71.Shi P., Ren G., Yang J. Clinical characteristics of imported and second-generation COVID-19 cases outside Wuhan, China: A multicenter retrospective study. Preprint at medRxiv. 2020 doi: 10.1101/2020.04.19.20071472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yadaw A.S., Li Y-C, Bose S. Clinical predictors of COVID-19 mortality. Preprint at medRxiv. 2020 doi: 10.1101/2020.05.19.20103036. [DOI] [Google Scholar]
- 73.Jurado A., Martin M.C., Abad-Molina C. COVID-19: age, Interleukin-6, C-Reactive Protein and lymphocytes as key clues from a multicentre retrospective study in Spain. Preprint at medRxiv. 2020 doi: 10.1101/2020.05.13.20101345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Feng Z., Yu Q., Yao S. Early Prediction of Disease Progression in 2019 Novel Coronavirus Pneumonia Patients Outside Wuhan with CT and Clinical Characteristics. Preprint at medRxiv. 2020 doi: 10.1101/2020.02.19.20025296. [DOI] [Google Scholar]
- 75.Chen X., Zheng F., Qing Y. Epidemiological and clinical features of 291 cases with coronavirus disease 2019 in areas adjacent to Hubei, China: a double-center observational study. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.03.20030353. [DOI] [Google Scholar]
- 76.Qi D., Yan X., Tang X. Epidemiological and clinical features of 2019-nCoV acute respiratory disease cases in Chongqing municipality, China: a retrospective, descriptive, multiple-center study. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.01.20029397. [DOI] [Google Scholar]
- 77.Gu T., Chu Q., Yu Z. History of coronary heart disease increases the mortality rate of COVID-19 patients: a nested case-control study. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.23.20041848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fu L., Fei J., Xiang H.-X. Influence factors of death risk among COVID-19 patients in Wuhan, China: a hospital-based case-cohort study. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.13.20035329. [DOI] [Google Scholar]
- 79.Fan L., Liu C., Li N. Medical treatment of 55 patients with COVID-19 from seven cities in northeast China who fully recovered: a single-center, retrospective, observational study. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.28.20045955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nie S., Zhao X., Zhao K. Metabolic disturbances and inflammatory dysfunction predict severity of coronavirus disease 2019 (COVID-19): a retrospective study. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.24.20042283. [DOI] [Google Scholar]
- 81.Zhang J., Ding D., Cao C. Myocardial characteristics as the prognosis for COVID-19 patients. Preprint at medRxiv. 2020 doi: 10.1101/2020.05.06.20068882. [DOI] [Google Scholar]
- 82.Zhang F., Yang D., Li J. Myocardial injury is associated with in-hospital mortality of confirmed or suspected COVID-19 in Wuhan, China: A single center retrospective cohort study. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.21.20040121. [DOI] [Google Scholar]
- 83.Mao L., Wang M., Chen S. Neurological Manifestations of Hospitalized Patients with COVID-19 in Wuhan, China: a retrospective case series study. Preprint at medRxiv. 2020 doi: 10.1101/2020.02.22.20026500. [DOI] [Google Scholar]
- 84.Liu J., Liu Y., Xiang P. Neutrophil-to-Lymphocyte Ratio Predicts Severe Illness Patients with 2019 Novel Coronavirus in the Early Stage. Preprint at medRxiv. 2020 doi: 10.1101/2020.02.10.20021584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhang H., Wang X., Fu Z. Potential Factors for Prediction of Disease Severity of COVID-19 Patients. Preprint at medRxiv. 2020 doi: 10.1101/2020.03.20.20039818. [DOI] [Google Scholar]
- 86.Sisó-Almirall A., Kostov B., Mas-Heredia M. Prognostic Factors In Spanish Covid-19 Patients: A Case Series From Barcelona. Preprint at medRxiv. 2020 doi: 10.1101/2020.06.18.20134510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang H., Lu Y., Lv Q. Progression, recovery and fatality in patients with SARS-CoV-2 related pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Preprint at medRxiv. 2020 doi: 10.1101/2020.05.12.20099739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen C., Yi Z.J., Chang L. The characteristics and death risk factors of 132 COVID-19 pneumonia patients with comorbidities: a retrospective single center analysis in Wuhan, China. Preprint at medRxiv. 2020 doi: 10.1101/2020.05.07.20092882. [DOI] [Google Scholar]
- 89.Q L., Y L., J Z. Clinical Characteristics of SARS-CoV-2 Infections Involving 325 Hospitalized Patients outside Wuhan. Preprint at Research Square. 2020 doi: 10.21203/rs.3.rs-18699/v1. [DOI] [Google Scholar]
- 90.Mantovani A., Byrne C.D., Zheng M.H. Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: A meta-analysis of observational studies. Nutr Metab Cardiovasc Dis. 2020;30:1236–1248. doi: 10.1016/j.numecd.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Li X., Wang L., Yan S. Clinical characteristics of 25 death cases with COVID-19: a retrospective review of medical records in a single medical center, Wuhan, China. Int J Infect Dis. 2020;94:128–132. doi: 10.1016/j.ijid.2020.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Onder G., Rezza G., Brusaferro S. Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 93.Fadini G.P., Morieri M.L., Longato E. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020;43:867–869. doi: 10.1007/s40618-020-01236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Villabona C.V. Commentary: COVID-19 and diabetes. Diabetes Res Clin Pract. 2020;162:108138. doi: 10.1016/j.diabres.2020.108138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ma R.C.W., Holt R.I.G. COVID-19 and diabetes. Diabet Med. 2020;37:723–725. doi: 10.1111/dme.14300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Maddaloni E., Buzzetti R. Covid-19 and diabetes mellitus: unveiling the interaction of two pandemics. Diabetes Metab Res Rev. 2020:e33213321. doi: 10.1002/dmrr.3321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Society C.D. Management suggestions for patients with diabetes and novel coronavirus pneumonia. Chin J Diabetes Mellitus. 2020;12:73–75. [Article in Chinese] [Google Scholar]
- 99.Klonoff D.C., Umpierrez G.E. COVID-19 in patients with diabetes: risk factors that increase morbidity. Metabolism. 2020;108:154224. doi: 10.1016/j.metabol.2020.154224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang W., Lu J., Gu W. Care for diabetes with COVID-19: Advice from China. J Diabetes. 2020;12:417–419. doi: 10.1111/1753-0407.13036. [DOI] [PubMed] [Google Scholar]
- 101.Puig-Domingo M., Marazuela M., Giustina A. COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine. 2020;68:2–5. doi: 10.1007/s12020-020-02294-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.