Abstract
Objective:
This study examined the relationship between eating-disorder behaviors—including restrictive eating, binge eating, and purging—and suicidal ideation. We hypothesized that restrictive eating would significantly predict suicidal ideation, beyond the effects of binge eating/purging.
Methods:
Participants were 82 adolescents and young adults with low-weight eating disorders. We conducted a hierarchical logistic regression, with binge eating and purging in Step 1 and restrictive eating in Step 2, to predict suicidal ideation.
Results:
Step 1 was significant (p = .01) and explained 20% variance in suicidal ideation; neither binge eating nor purging significantly predicted suicidal ideation. Adding restrictive eating in Step 2 significantly improved the model (ΔR2 = .07, p = .009). This final model explained 27% of the variance, and restrictive eating (but not binge eating/purging) significantly predicted suicidal ideation (p = .02).
Discussion:
Restrictive eating is associated with suicidal ideation in youth with low-weight eating disorders, beyond the effects of other eating-disorder behaviors. Although healthcare providers may be more likely to screen for suicidality in patients with binge eating and purging, our findings indicate clinicians should regularly assess suicide and self-injury in patients with restrictive eating. Future research examining how individuals progress from suicidal ideation to suicidal attempts can further enhance our understanding of suicide in eating disorders.
Keywords: anorexia nervosa, eating disorders, low weight, restrictive eating, suicidal ideation
1. ∣. INTRODUCTION
Anorexia nervosa (AN) has one of the highest mortality rates of any psychiatric disorder, and suicide is the second leading cause of death among individuals with AN (Arcelus, Mitchell, Wales, & Nielsen, 2011). Compared to 15–34-year-old women in the general population, individuals with AN are approximately 5.2 times more likely to die prematurely and 18 times more likely to die by suicide specifically (Keshaviah et al., 2014). In addition to suicide death, individuals with AN report greater suicidal ideation than individuals in the general population, with 20–43% of individuals with AN endorsing current suicidal ideation (Milos, Spindler, Hepp, & Schnyder, 2004). These data are particularly concerning given epidemiological studies demonstrating that approximately one-third of individuals with suicidal ideation eventually make a suicide attempt, and approximately 60% of transitions from ideation to attempts occur in the first year after suicidal ideation onset (Nock et al., 2008).
Despite the high prevalence of suicidality in AN, the specific relationship between restrictive eating and suicidal thoughts remains unclear. Several studies comparing suicidality across eating disorder (ED) diagnostic categories have found elevated rates of suicidal thoughts and behaviors among individuals with AN binge/purge subtype (AN-BP) and bulimia nervosa (BN; Foulon et al., 2007; Stein, Lilenfeld, Wildman, & Marcus, 2004) compared to AN restricting subtype (AN-R). Clinically, this may have led to an assumption that restrictive eating is less strongly associated with suicidality than binge eating/purging. Indeed, healthcare providers are less likely to screen for suicide and self-injury among patients engaging in restrictive eating without binge eating/purging (Peebles, Wilson, & Lock, 2011). However, restrictive eating occurs across all ED diagnoses, not only AN-R. In fact, individuals with AN-BP report more frequent restrictive eating behaviors than individuals with AN-R (De Young et al., 2013). Therefore, as individuals with diagnoses characterized by binge eating/purging (e.g., AN-BP) also engage in frequent restrictive eating, conclusions about the extent to which specific ED behaviors increase risk for suicidality cannot be drawn based on the prevalence of suicidality across ED diagnostic categories alone.
Rather, data examining the relationship between suicidality and specific ED behaviors, rather than diagnoses—which conflate multiple behaviors—are needed. Indeed, recent research examining specific ED behaviors and nonsuicidal self-injury (NSSI; i.e., direct self-harm without suicidal intent, leading to tissue damage; Nock, 2010) found restrictive eating was associated with NSSI above and beyond the influence of binge eating/purging (Wang, Pisetsky, Skutch, Fruzzetti, & Haynos, 2018), despite prior research suggesting stronger links between binge-eating/purging and NSSI based on between-diagnosis comparisons (Claes et al., 2015). Preliminary work suggests restrictive eating is associated with a past history of suicide attempts (Witte et al., 2016) and is indirectly associated with suicidal thoughts (Forrest et al., 2016), but the specific, direct relationship between restrictive eating and suicidal thoughts—particularly compared to binge-eating/purging behaviors—remains unclear.
We aimed to address this gap by testing whether restrictive eating predicted unique variance in suicidal ideation beyond binge eating and purging. We examined this among adolescents with low-weight EDs, as both EDs and suicidal ideation have a peak age of onset during adolescence (Nock et al., 2008; Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011) and individuals with low-weight EDs such as AN are at elevated risk for suicide death compared to the general population (Keshaviah et al., 2014). We focused on suicidal ideation as an outcome given the rarity of suicide attempts in our young sample. As suicidal ideation is a precursor to suicide attempts (Nock et al., 2019), identifying specific ED behaviors associated with suicidal ideation could provide important information about intervention targets to prevent escalation to suicidal behaviors. Based on previous empirical literature examining restrictive eating and suicide attempts (Witte et al., 2016) and research comparing the influence of specific ED behaviors on NSSI (Wang et al., 2018), we hypothesized that restrictive eating would be associated with increased likelihood of suicidal ideation, even after accounting for the influence of binge-eating/purging behaviors.
2 ∣. METHODS
2.1 ∣. Participants and procedure
Participants were 82 adolescents and young adult females with low-weight EDs (Table 1 displays sample characteristics). Low weight was indicated by either: <90% median body mass index or <90% expected body weight (%EBW) for height or age based on Center for Disease Control female growth charts (Kuczmarski et al., 2000). Exclusion criteria included active suicidal intent and plan, but no participants from the sample were excluded due to active suicidality. Trained research assistants measured participants' heights on a wall-mounted stadiometer and participants' weight on an electronic scale. This study received approval from the hospital's institutional review board. Participants over 18 years old and parents of participants under 18 provided written informed consent; participants under 18 provided assent.
TABLE 1.
Demographic and clinical characteristics of the study sample
| M (SD) | Range | N (%) | |
|---|---|---|---|
| Age (years) | 18.3 (3.2) | 10.09–22.52 | |
| Body mass index (kg/m2) | 17.3 (1.5) | 13.00–20.90 | |
| % expected body mass index | 82.6 (6.5) | 67.50–96.97 | |
| Eating disorder diagnosis | |||
| Anorexia nervosa—Restricting | 29 (36.59) | ||
| Anorexia nervosa—Binge/purge | 11 (15.86) | ||
| Avoidant/restrictive food intake disorder | 16 (18.29) | ||
| OSFED—Atypical anorexia nervosa | 26 (28.04) | ||
| Eating disorder behaviors | |||
| Fasting | 0.48 (0.92) | 0–4 | 24 (29.27) |
| Binge eating | 1.42 (5.32) | 0–38.67 | 15 (18.29) |
| Purging | 2.22 (7.68) | 0–54 | 20 (24.39) |
| Suicidal ideation | 21 (25.61) | ||
| Race | |||
| White | 68 (82.93) | ||
| Asian | 12 (14.63) | ||
| Other | 2 (2.44) | ||
| Ethnicity | |||
| Hispanic | 6 (7.32) | ||
| Non-Hispanic | 76 (92.68) | ||
Note: OSFED, other specified feeding and eating disorders. Fasting is measured by the Eating Disorders Examination (EDE) avoidance of eating item; binge eating is measured as the average of EDE objective binge-eating episodes over the past 3 months; purging is measured as the average of EDE self-induced vomiting, laxative use, and diuretic use over the past 3 months.
2.2 ∣. Measures
DSM-5 diagnoses were conferred through assessment by KSADS (Kaufman et al., 2013) and confirmed via symptom count on the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993). Inter-rater reliability for these diagnoses based on a random subset of the sample (n = 10) was excellent (κ = 1.0).
2.2.1 ∣. ED behaviors
We used the EDE to assess restrictive eating, binge eating, and purging. First, we used the EDE avoidance of eating item (“Have you gone for periods of eight or more waking hours without eating anything?”) to assess fasting, one form of restrictive eating, over the past 28 days. We chose to use this item rather than the entire EDE restraint subscale as other items on this subscale assess cognitive restraint (e.g., “deliberately trying to limit the amount of food you eat, whether or not you have succeeded?) rather than restriction. Second, we used the EDE objective binge episodes item to assess average objective binge eating over the past 3 months. Finally, we used a composite score of the EDE self-induced vomiting, laxative use, and diuretic use items to assess average purging over the past 3 months. Inter-rater reliability for ED behaviors were excellent (ICCs = 1 for all behaviors).
2.2.2 ∣. Suicidal ideation
We used the suicide item from the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996) for participants over 18 years old and the Child Depression Inventory (CDI; Kovacs, 2001) for participants under 18 to assess suicidal ideation over the past 2 weeks. Participants were categorized as endorsing suicidal ideation if they selected a response of “I have thoughts of killing myself, but I would not carry them out” or “I would like to kill myself” on the BDI-II, and a response of “I think about killing myself but I would not do it” on the CDI; no participants endorsed active suicidal intent.
2.3 ∣. Data analysis
We first used descriptive statistics to examine the frequency of restrictive eating (fasting), binge eating, purging, and suicidal ideation. We next conducted a hierarchical logistic regression to test whether restrictive eating was associated with increased likelihood of suicidal ideation, above and beyond the effects of binge eating and purging. We also included %EBW, diagnosis, and age in the model to rule out the possibility that any detected association between restrictive eating and suicidal ideation could be accounted for by these variables. Step 1 in the model included binge eating, purging, and %EBW/diagnosis/age, and Step 2 included restrictive eating.
3 ∣. RESULTS
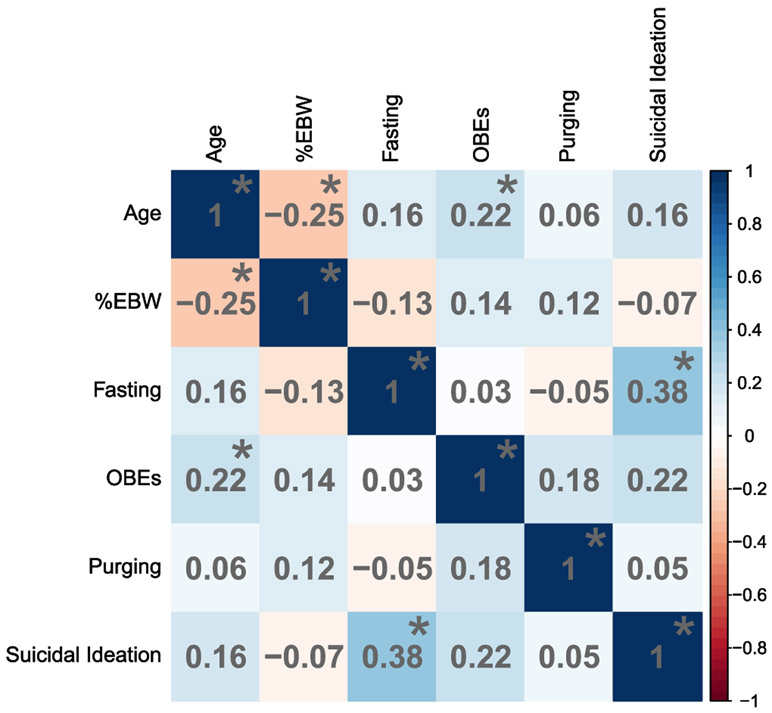
Table 1 summarizes participant characteristics and Figure 1 displays correlations among variables. A total of 24 participants endorsed fasting, 15 endorsed binge eating, and 20 participants endorsed purging. Over one quarter of the sample (n = 21) endorsed suicidal ideation.
FIGURE 1.
Correlation matrix among demographics and clinical characteristics. %EBW, percent expected body weight; OBEs, objective binge episodes. Darker blue colors indicate stronger, more positive correlations and darker red colors indicate stronger, more negative correlations. Significant correlations are indicated by an asterisk
Table 2 summarizes the hierarchical logistic regression. Step 1, which examined the relationship between binge eating, purging, and controlled for %EBW/diagnosis/age, was significant (McFadden's pseudo-R2 = .20, X2 = 18.34, p = .01). The model fit improved with the addition of restrictive eating, ΔMcFadden's pseudo-R2 = .07, ΔX2 = 6.72, p = .009. In this final model, restrictive eating predicted suicidal ideation (B = 0.78, p = .02), but binge eating and purging did not (ps = .55 and .13, respectively). Variance inflation factors were low (ranging from 1.12 to 1.3.91), demonstrating no problematic multicollinearity between predictors.
TABLE 2.
Hierarchical logistic regression examining the relationship between eating disorder behaviors and suicidal ideation
| Pseudo-R2 | χ2(df) | AIC | BIC | Log-likelihood | B | SE | OR [95% CI] | |
|---|---|---|---|---|---|---|---|---|
| Step 1 | .20 | 18.34(7)* | 89.16 | 107.91 | −36.58 | |||
| %EBW | −0.07 | 0.07 | 0.93 [0.81, 1.08] | |||||
| Diagnosis: AN-BP | −0.57 | 0.94 | 0.57 [0.09, 3.55] | |||||
| Diagnosis: ARFID | −17.57 | 1,664.94 | 0.00 [0.00, Inf] | |||||
| Diagnosis: Atypical AN | 0.49 | 1.05 | 1.64 [0.21, 12.94] | |||||
| Age | −0.02 | 0.11 | 0.98 [0.79, 1.23] | |||||
| OBEs | 0.01 | 0.05 | 1.01 [0.91, 1.12] | |||||
| Purging | 0.05 | 0.04 | 1.05 [0.98, 1.13] | |||||
| Step 2 | .27 | 25.05(8)** | 84.44 | 105.53 | −33.22 | |||
| %EBW | −0.04 | 0.08 | 0.96 [0.82, 1.13] | |||||
| Diagnosis: AN-BP | −1.10 | 1.03 | 0.33 [0.04, 2.54] | |||||
| Diagnosis: ARFID | −17.28 | 1,679.08 | 0.00 [0.00, Inf] | |||||
| Diagnosis: Atypical AN | −0.02 | 1.16 | 0.98 [0.10, 9.49] | |||||
| Age | −0.03 | 0.12 | 0.97 [0.77, 1.24] | |||||
| OBEs | 0.03 | 0.05 | 1.03 [0.93, 1.15] | |||||
| Purging | 0.06 | 0.04 | 1.06 [0.98, 1.15] | |||||
| Restrictive eating | 0.78* | 0.34 | 2.10 [1.12, 4.28] |
Note:
p < .05,
p < .01. Reported pseudo-R2 is McFadden's pseudo-R2. AIC, Akaike information criterion; BIC, Bayesian information criterion; %EBW, percent expected body weight; OR, odds ratio; OBEs, objective binge episodes. Reference category for diagnosis is anorexia nervosa-restrictive eating subtype.
4 ∣. DISCUSSION
This study demonstrates suicidal ideation is common among adolescents and young adults with low-weight EDs, and that fasting, a specific type of restrictive eating, was associated with increased likelihood of suicidal ideation. This association was significant beyond the effects of objective binge episodes and purging, suggesting restrictive eating may increase risk of suicidal ideation even beyond risk associated with other ED behaviors. These findings extend a growing body of literature on the significance of restrictive eating in predicting self-injurious thoughts and behaviors (e.g., Forrest et al., 2016; Wang et al., 2018), and also shed light on the specific influence of fasting on suicidal ideation among a clinical sample of individuals with low-weight EDs.
Notably, our findings stand in contrast to the hypothesis that restrictive eating is less strongly linked to suicidal ideation and other self-injurious behaviors because of the seemingly “passive” nature of restricting food intake (Jacobson & Luik, 2014, p. 23). Importantly, this hypothesis has been derived from previous data comparing frequency of self-injurious thoughts and behaviors across ED diagnostic categories. However, as restrictive eating occurs across all ED diagnoses, data demonstrating higher rates of self-injurious thoughts and behaviors in disorders characterized by binge eating/purging (e.g., BN) are unable to rule out the possibility of this relationship being driven by heightened restrictive eating—either in addition to, or instead of, binge eating/purging. This seems particularly plausible in light of evidence suggesting individuals with AN-BP engage in more frequent restrictive eating than those with AN-R (De Young et al., 2013). By directly comparing ED behaviors, the current study allowed for interpretation of the specific effects of individual behaviors, finding that fasting was uniquely associated with suicidal ideation.
These results also support recent work investigating self-harming intentions underlying ED behaviors. Although ED behaviors are typically conceptualized as functioning to control weight/shape, emerging research suggests individuals also engage in these behaviors with at least some intention to hurt themselves physically in the moment and in the long run (Fox et al., 2019). Notably, compared to binge eating and purging, individuals report restricting with a greater intent to cause long-term physical harm, a higher hope and knowledge of dying sooner as a consequence of restrictive eating, and greater thoughts of restricting to kill oneself (Fox et al., 2019). Although the current study did not assess motivations underlying fasting beyond controlling shape/weight, our findings, considered in concert with previous research by Fox et al. (2019), suggest one possible reason for the stronger association between suicidal ideation and restrictive eating (compared to binge eating/purging) may be self-harming and suicidal motivations underlying restrictive eating behaviors.
Limitations of this study include the cross-sectional design, as well as relatively small sample size of only females in a limited age range. Because the sample was recruited based on low weight, more participants endorsed fasting than binge eating and purging, and these smaller numbers may have limited our ability to detect statistically significant associations of these behaviors with suicidal ideation. In addition, our binary assessment of suicidal ideation (single BDI/CDI item) may not have fully captured participants' suicidal ideation, and no participants endorsed suicide plans or intent. Similarly, we focused only on fasting, and other forms of restrictive eating may show different relationships with suicidal ideation. To address these limitations, future research should aim to use longitudinal and experimental methodology, as well as more objective and comprehensive measures (e.g., Eating Pathology Symptom Inventory) to determine if and how multiple forms of restrictive eating predicts the onset or escalation of suicidal ideation over time in larger samples with more diversity in gender, age, and weight.
This study contributes new information about the association between ED behaviors and suicidal ideation among adolescents and young adults with low-weight EDs. Our findings have significant clinical applications by highlighting the importance of screening for suicidal ideation among patients with EDs, particularly those engaging in fasting. Moreover, as many individuals who make a suicide attempt do so in the first year following suicidal ideation onset (Nock et al., 2008), our results suggest reducing extreme restrictive eating may be important to reduce risk of heightened suicidal ideation or attempts, although further investigation is necessary. Future research elucidating mechanisms of the relationship between restrictive eating and suicidal ideation, as well as utilizing more complex prediction algorithms in larger samples, will continue to advance our understanding and prediction of suicidality in EDs, which could have important treatment and prevention implications for these dangerous and destructive thoughts and behaviors.
ACKNOWLEDGMENTS
This study was supported by Grant Number R01MH103402 from the National Institute of Mental Health (PIs: Misra/Lawson/Eddy). Shirley B. Wang is supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-1745303. Kendra R. Becker is supported by the National Institute of Mental Health of the National Institutes of Health under F32MH111127. Franziska Plessow is supported by the Charles A. King Trust Postdoctoral Research Fellowship Program, Bank of America, N.A., and Co-Trustees through a Charles A. King Trust Fellowship. Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funding agencies.
Funding information Division of Graduate Education, Grant/Award Number: DGE-1745303; National Institute of Mental Health, Grant/Award Numbers: F32MH111127, R01MH103402
Footnotes
DATA AVAILABILITY STATEMENT
Data Availability Statement: The data that support the findings will be available through the National Institutes of Mental Health National Database for Autism Research following an embargo period through the end of the study.
REFERENCES
- Arcelus J, Mitchell AJ, Wales J, & Nielsen S (2011). Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry, 68(7),724–731. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78(2), 490–498. [Google Scholar]
- Claes L, Islam MA, Fagundo AB, Jimenez-Murcia S, Granero R, Agüera Z, … Fernández-Aranda F (2015). The relationship between non-suicidal self-injuryand the UPPS-P impulsivity facets in eating disorders and healthycontrols. PLoS One, 10(5), e0126083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Young KP, Lavender JM, Steffen K, Wonderlich SA, Engel SG, Mitchell JE, … Crosby RD (2013). Restrictive eating behaviors are a nonweight-based marker of severity in anorexia nervosa. International Journal of Eating Disorders, 46(8), 849–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, & Cooper Z (1993). The eating disorder examination In Fairburn CG, & Wilson GT (Eds.), Binge eating: Nature, assessment, and treatment. New York: Guilford Press. [Google Scholar]
- Forrest LN, Bodell LP, Witte TK, Goodwin N, Bartlett ML, Siegfried N, … Smith AR (2016). Associations between eating disorder symptoms and suicidal ideation through thwarted belongingness and perceived burdensomeness among eating disorder patients. Journal of affective disorders, 195, 127–135. [DOI] [PubMed] [Google Scholar]
- Foulon C, Guelfi JD, Kipman A, Ades J, Romo L, Houdeyer K, … Gorwood P (2007). Switching to the bingeing/purging subtype of anorexia nervosa is frequently associated with suicidal attempts. European Psychiatry, 22(8), 513–519. [DOI] [PubMed] [Google Scholar]
- Fox KR, Wang SB, Boccagno C, Haynos AF, Kleiman E, & Hooley JM (2019). Comparing self-harming intentions underlying eating disordered behaviors and NSSI: Evidence that distinctions are less clear than assumed. International Journal of Eating Disorders, 52(5),564–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson CM, & Luik CC (2014). Epidemiology and sociocultural aspects of non-suicidal self-injury and eating disorders In Non-suicidal self-injury in eating disorders (pp. 19–34). Heidelberg: Springer Berlin Heidelberg. [Google Scholar]
- Kaufman J, Birmaher B, Axelson D, Perepletchikova F, Brent D, & Ryan N (2013). Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime Version 2013: Working Draft (KSADS-PL). [Google Scholar]
- Keshaviah A, Edkins K, Hastings ER, Krishna M, Franko DL, Herzog DB, … Eddy KT (2014). Re-examining premature mortality in anorexia nervosa: A meta-analysis redux. Comprehensive Psychiatry, 55(8), 1773–1784. [DOI] [PubMed] [Google Scholar]
- Kovacs M (2001). Children's depression inventory manual Multi health systems. North Tonawanda: Multi Health Systems, NY. [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, … Johnson GL (2000). CDC growth charts for the United States: Methods and development. Vital and Health Statistics, 11(246), 1–190. [PubMed] [Google Scholar]
- Milos G, Spindler A, Hepp U, & Schnyder U (2004). Suicide attempts and suicidal ideation: Links with psychiatric comorbidity in eating disorder subjects. General Hospital Psychiatry, 26(2), 129–135. [DOI] [PubMed] [Google Scholar]
- Nock MK (2010). Self-injury. Annual review of clinical psychology, 6, 339–363. [DOI] [PubMed] [Google Scholar]
- Nock MK, Boccagno C, Kleiman EM, Ramirez F, Wang SB (2019). Suicidal and nonsuicidal self-injury In Prinstein MJ, Youngstrom EA, Mash EJ, & Barkley RA (Eds.), Treatment of Childhood Disorders, Fourth Edition. New York, NY: Guilford Publications. [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, … De Graaf R (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry, 192(2), 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peebles R, Wilson JL, & Lock JD (2011). Self-injury in adolescents with eating disorders: Correlates and provider bias. Journal of Adolescent Health, 48(3), 310–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein D, Lilenfeld LR, Wildman PC, & Marcus MD (2004). Attempted suicide and self-injury in patients diagnosed with eating disorders. Comprehensive Psychiatry, 45(6), 447–451. [DOI] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, & Merikangas KR (2011). Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 68(7), 714–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SB, Pisetsky EM, Skutch JM, Fruzzetti AE, & Haynos AF (2018). Restrictive eating and nonsuicidal self-injury in a nonclinical sample: Co-occurrence and associations with emotion dysregulation and interpersonal problems. Comprehensive Psychiatry, 82, 128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte TK, Zuromski KL, Gauthier JM, Smith AR, Bartlett M, Siegfried N, … Goodwin N (2016). Restrictive eating: Associated with suicide attempts, but not acquired capability in residential patients with eating disorders. Psychiatry Research, 235, 90–96. [DOI] [PubMed] [Google Scholar]