Abstract
Background
Burnout syndrome (BS) is a common condition among medical professionals. It is composed of 3 different subdimensions: emotional exhaustion (EE), depersonalization (DP), and reduced personal accomplishment (PA). In the last years, interest in BS in the neurosurgical community has increased. Here we investigated burnout among neurosurgeons and residents in neurosurgery.
Methods
A systematic review with meta-analysis was performed following PRISMA guidelines. A search of bibliographic databases was conducted from study inception to February 2020. A total of 16,377 studies were found. Six articles were included in our final analysis. Their references were checked for additional studies, but none were found.
Results
From the initial 16,377 studies identified, only 6 met our inclusion criteria. These studies included a total of 3310 physicians. The general prevalence of BS was 48%. The prevalence in neurosurgeons was 51.1%, higher than that recorded in neurosurgical residents (45.4%). Regarding subdimensions, personal accomplishment seemed to be the most influential factor for burnout development among neurosurgeons (42.57%) and residents (51.56%) alike.
Conclusions
Neurosurgery is a rewarding career choice, but numerous challenges and stressors can lead to lower levels of satisfaction and dangerously increased levels of burnout. We hope that our results will generate discussion, raise awareness, stimulate further studies, and lead to programs designed to mitigate excessive stress and burnout in neurosurgeons.
Key words: Burnout, Career, Neurosurgery, Residency
Abbreviations and Acronyms: BS, Burnout syndrome; DP, Depersonalization; EE, Emotional exhaustion; MBI, Maslach Burnout Inventory; NOS, Newcastle–Ottawa Scale; PA, Personal accomplishment
Introduction
Burnout syndrome (BS) is defined as a condition of emotional exhaustion (EE), feelings of depersonalization (DP), and a lack of personal accomplishment (PA) specifically related to stress at work.1 Although interest in this topic has recently been growing in the medical community, BS has been known for decades, since its first description published by Freudenberger in 1974.2 Burnout is related to an increasing workload, typical of healthcare professionals, that leads to job stress and intense time pressure, compounded by a lack of organizational support. This stressful situation is known to be an issue for the personal mental health of healthcare workers, as well as the economy as a whole.3
The stress in the workplace, which also can be manifested with emotional exhaustion and irritability in the work environment, can tend to lead to mental health issues such as BS, which is characterized by 3 main aspects: EE, DP, and a feeling of diminished PA.4
Even in such a physical and mentally demanding field as neurosurgery, there are few published studies concerning work stress and BS. The situation appears to be dramatic. A recent US national survey on BS in the neurosurgical community found that more than one-half of the respondents showed signs of BS, and that only one-third of respondents would recommend a career in neurosurgery.5 Studies on career satisfaction and burnout are instrumental in identifying factors that precipitate psychological distress, so that reforms can be instituted to stem the tide of disgruntled physicians.
In this report, we summarize the scientific literature on BS in neurosurgery and estimate its prevalence among neurosurgery residents and neurosurgeons.
Methods
To better define the state of burnout in the neurosurgical community and the overall prevalence, we performed a systematic review and a meta-analysis, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocols.6
Data Sources and Search Strategy
A search was conducted using a combination of MeSH search terms, text words, and keywords based on each database characteristics, focusing on synonyms of BS and neurosurgery.
Keywords included “burnout,” “burnout syndrome,” “neurosurgery,” “neurosurgeon,” and “resident.” To collect all articles related to the topic of the study, several online databases were accessed, including Embase, PubMed, Scopus, and Cochrane Library. Electronic searches identified articles published between January 1974, when burnout was first described,2 and February 2020.
Quality Evaluation of the Primary Studies
An evaluation of the methodological quality/risk of bias of the primary cross-sectional studies was performed using the Newcastle–Ottawa Quality assessment scale (NOS).7 The NOS scale is an epidemiologic tool composed of 8 items used for assessing the quality of nonrandomized studies included in systematic review and/or meta-analyses. The checklist is divided into 3 sections, each focusing on a different aspect: (1) study selection, (2) group comparability, and (3) outcome of interest.
Inclusion and Exclusion Criteria
We included only articles describing the study of BS in neurosurgeons and neurosurgical residents. After a first screening, case series, editorials, case-control studies, cohort studies, retrospective studies, systematic reviews, meta-analyses, and clinical trials considering burnout syndrome in the neurosurgical community were included. All reviews were screened for possible inclusion. Non-English articles were excluded. Laboratory studies and studies involving animals were excluded. The scale used for measuring BS was not an inclusion criterion. Intervention studies were also excluded, even though there was the possibility that they would have provided additional data, but they would have been a source of heterogeneous data, and thus considering them would have been a conceptual error. Studies that considered other specialties along with neurosurgery were considered only if data related to the neurosurgical specialty could be isolated.
Data Extraction
The data were carefully evaluated and extracted independently by 2 authors (I.Z. and Y.J.). Data retrieved from the studies included author, publication year, country, specialties evaluated, population size, BS dimension, and overall burnout value.
Maslach Burnout Inventory
The Maslach Burnout Inventory (MBI) is an introspective psychological inventory consisting of 22 items about burnout.4 Currently the MBI is the most widely used test to diagnose BS. It is a psychological tool that aims to quantify the level of all the 3 dimensions of burnout: EE, the feeling of being emotionally overextended by something; DP, defined as an impersonal response toward recipients of one's service, care treatment, or instruction; and PA, feelings of competence and achievement. This test can be completed in 10–15 minutes.
Answers to each question are based on the frequency of the respondent's encountering the situation described on a 7-point scale, from “never” (0 points) to “daily” (6 points). The scores in each dimension are further graded as high, intermediate, or low (low EE, ≤18; high EE, ≥27; low DP, ≤5, high DP, ≥10; low PA, ≤33; high PA, ≥40). High scores in the EE and/or DP dimension are considered to indicate burnout.8
Statistical Analysis
The main objective of the meta-analysis was to identify quantitative studies assessing the burnout phenomena and gauge its prevalence among residents and neurosurgeons. The analysis was conducted with SPSS version 26.0 (IBM, Armonk, New York, USA) using as data input the sample size and burnout rate of each included primary study. Effect sizes were assessed through the computation of dichotomous means and the gauging of variance (z-values) to indicate the significance of the effect in the overall sample, a 95% confidence interval, a P value, and a standard error. Both a fixed-effects model and a random-effects model were used to identify a general prevalence and an effect size for both neurosurgeons and residents. Moreover, a heterogeneity analysis was conducted to test the null hypothesis and assess the q-values and τ2 values to evaluate the consistency of the results.
Results
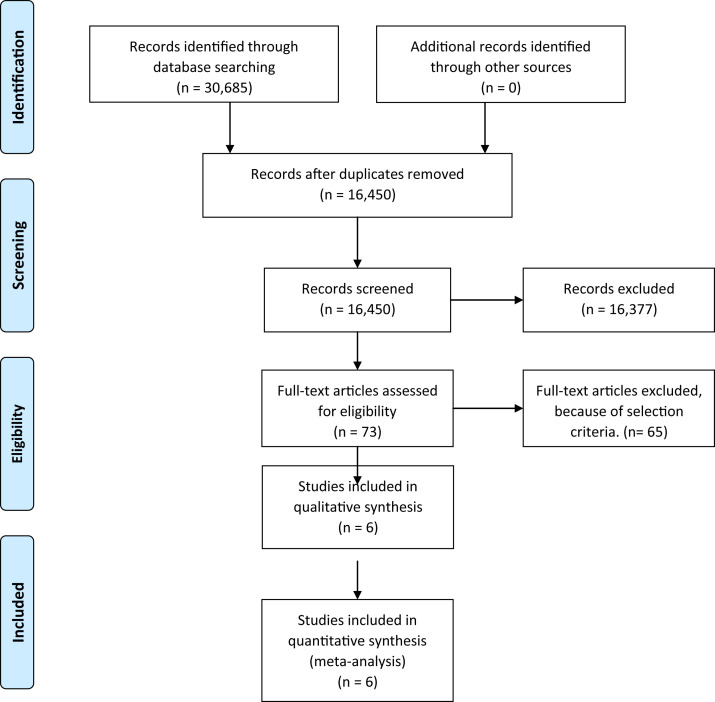
A complementary article search was performed using PubMed, SCOPUS, and Cochrane Library. The results are shown in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram (Figure 1 ).
Figure 1.
PRISMA flow diagram summarizing the literature search.
In the second step of screening, 16,377 studies were excluded because the full text articles were not available or were assessed for eligibility according to the following exclusion criteria: laboratory study, animal study, or article not in English.
Among the remaining 73 articles, 65 were eliminated for several reasons: 3 studies were reviews/meta-analyses, 18 were laboratory/animal studies, 4 were non-English studies, 6 were interventional studies, 6 were letters to the editor, 5 were editorials, 4 were commentaries, and 19 were nonrelated studies (Table 1 ).
Table 1.
Summary of the Articles Considered in the Analysis
| Study | Year | Country | Population | Response, % | N | Reporting Burnout, n (%) | Males | Females | Age |
|---|---|---|---|---|---|---|---|---|---|
| Attenello et al.9 | 2018 | US | Residents | 24% | 346 | 232 (67.1) | 270 | 76 | NA |
| Fargen et al.10 | 2019 | US | Neurosurgeons | 27% | 297 | 164 (55.2) | NA | NA | NA |
| McAbee et al.5 | 2015 | US | Neurosurgeons | 24% | 783 | 425 (54.3) | NA | NA | NA |
| Shakir et al.11 | 2017 | US | Residents | 21% | 255 | 93 (36.5) | 205 | 50 | NA |
| Shakir et al.12 | 2019 | US | Residents | 31% | 427 | 141 (33) | 324 | 99 | NA |
| Yu et al.13 | 2019 | China | Neurosurgeons and residents | 16% | 1202 | 535 (44.5) | 1117 | 85 | 34.32 |
NOS Evaluation
The selected studies were submitted to the NOS evaluation to determine the risk of bias. The results are summarized in Table 1. Five of the studies included obtained 6 stars,5 , 9, 10, 11, 12 whereas 1 study gathered 5 stars.13
General Prevalence
The 6 included studies involved 3310 neurosurgeons and neurosurgical residents. The design features of the selected studies are indicated in Tables 1 and 2 . The general response rate reported for the selected studies to the MBI questionnaire ranged from 16% to 31%. Among the 3310 respondents, 1590 reported a diagnosis of BS, for a general prevalence of 48.4% in the random-effects model and 48% in the fixed-effects model. Analyzing the subdimensions identified PA (45.2%) as the most prevalent subdimension, followed by DP (37.9%) and EE (37.4%) (Table 3 ).
Table 2.
Subdimension Values in the Analyzed Studies
| Study | Emotional Exhaustion |
Depersonalization |
Personal Accomplishment |
||||||
|---|---|---|---|---|---|---|---|---|---|
| High | Moderate | Low | High | Moderate | Low | High | Moderate | Low | |
| Attenello et al.9 | 125 | 66 | 155 | 207 | 64 | 75 | 119 | 78 | 149 |
| Fargen et al.10 | 137 | NA | NA | 107 | NA | NA | NA | NA | 48 |
| McAbee et al.5 | 263 | 165 | 322 | 235 | 166 | 349 | 336 | 201 | 312 |
| Shakir et al.11 | 83 | 106 | 66 | 55 | 82 | 118 | 222 | 32 | 1 |
| Shakir et al.12 | 124 | 179 | 124 | 217 | 138 | 72 | 3 | 64 | 380 |
| Yu et al.13 | 434 | 573 | 195 | 356 | 303 | 543 | 151 | 518 | 533 |
Table 3.
Prevalence of BS in the Different Groups
| Population Considered | Fixed-Effects Model, % | Random-Effects Model, % |
|---|---|---|
| General | 48 | 48.4 |
| Neurosurgeons | 49.3 | 51.1 |
| Neurosurgery Residents | 45.1 | 45.4 |
Prevalence Among Neurosurgeons
The prevalence of burnout among neurosurgeon was calculated separately. The prevalence was 49.3% according to the fixed-effects model and 51.1% according to the random effects model. The most frequently reported subdimension was PA (42.57%), followed by EE (35.1%) and DP (29.77%) (Table 3).
Prevalence Among Neurosurgical Residents
The prevalence of BS was calculated separately for the residents. The prevalence was similar when calculated according to the fixed-effects and random-effects model (45.1% vs. 45.4%). The results for the subdimensions differed from those in neurosurgeons, with PA still the most important factor (51.56%) but DP (46.6%) more important than EE (32.3%). Of note, in an analysis of BS among US neurosurgical residents, Shakir et al.11 reported a significantly lower prevalence rate of 36.5% (Table 3).
Discussion
Study Findings
Both in the general population and among physicians, neurosurgery is considered a stressful yet rewarding profession.5 This meta-analysis attempted to quantify the stress associated with the field by analyzing prevalence rates in published studies addressing the presence of burnout in neurosurgeons and neurosurgical residents.
Our findings show that the general prevalence of BS is higher in the neurosurgical community compared with other medical specialties. A recent systematic review focused on estimating burnout among different medical residency specialties found an overall prevalence of burnout in all specialties of 35.1% (95% confidence interval, 26.8% to 43.5%) and a higher prevalence of burnout in general surgery, anesthesiology, obstetrics and gynecology, and orthopedics, with an average prevalence of 42.5%.3
Burnout
Several previous studies have identified BS as one of the main drivers of medical errors,14 , 15 early retirement,16 an increase in malpractice suits,17 and diminished satisfaction.18 It is widely known that surgeons are under especially high levels of stress, which is increasing the rate of burnout.19
The MBI consists of 22 items scored from 0 to 6 that include 9 items related to EE, 5 items related to DP, and 8 items relating to PA. Individuals with a high score on EE and DP or a low score on PA are considered to have symptoms of burnout.20 However, because the PA score is considered less important for determining whether surgeons or residents exhibit burnout,21 all the primary studies included in our analysis characterized burnout mainly through high scores on EE and DP.
Because our results depends on the data available in the selected literature, it was not feasible to conduct a moderator analysis to identify the impact of such factors as age, sex, marital status, medical experience, workload, and work characteristics to identify any significant correlations with burnout in neurosurgeons and neurosurgical residents. In fact, most of the studies that met our inclusion criteria focused primarily on submission of the MBI test, and when other factors were considered, it was not done in a standardized way, making comparisons statistically incorrect and forcing the exclusion of several studies. Even if it was not possible to analyze these factors, the literature has already considered them and have shown some correlations.22 Personal characteristics do not appear to have as much influence on burnout as the characteristics of employment, in both neurosurgeons and neurosurgical residents.13
In contrast, certain characteristics of neurosurgical practice correlate with the development of BS, especially work-life imbalance, residents' duties, provision of emergency services, and weekly workload.13 , 22 Interestingly enough, a recent Chinese study published by Yu et al.13 found that academic neurosurgeons have a significantly low (P < 0.01) rate of burnout even if they have to work a long hours; this could be explained by the high sense of personal accomplishment, and possibly by the high salaries (P < 0.01).13
For neurosurgical residents, personal characteristics, including age, marital status, and involvement in sports activities or leisure, showed less influence on the development of burnout.9 However, several factors affecting the stress level of neurosurgical residents have been identified, including inadequate exposure to the operating room, hostile faculty, hostile coresidents, and feeling underappreciated by patients or staff, poor control over one's schedule, and co-resident attrition.9
In general, a high prevalence of burnout was found in neurosurgical residents (45.4%) and neurosurgeons (51.1%), especially compared with other medical specialties.3 Regardless, given that burnout is correlated with high probabilities of medical errors and other work-related issues, such as an increased risk of work–home conflicts and a greater predisposition to depression,3 , 20 it is has been emphasized that an early and regular assessment of burnout among neurosurgeons and residents is essential to reverse this phenomenon.20
Moreover, it is suggested that preventive actions can be adopted to reduce the occurrence of burnout among neurosurgeons and residents in neurologic surgery. In general, the present literature showed that unstable routine work, high hourly workloads, and reduced time for family and leisure, in addition to the great difficulty to seek professional help are some of the most influential factors responsible for a predisposition to developing burnout6, 7, 8, 9 Thus, changes in habits among neurosurgeons, residents, and medical institutions are required so that standardization of hourly workloads may be set, as this seems to be a more effective protective factor against burnout.23 , 24
Creating support groups is important to allow neurosurgeons and residents to exchange experiences, receive information from experts that will help them recognize the signs and symptoms of burnout besides strategies that help deal with severe burnout, as well as the foundation of wellness programs.25, 26, 27, 28 Furthermore, the implementation of frequent interviews and psychological assessments can also be used as a good tool for screening and prevention of burnout among neurosurgeons and residents in neurosurgery.29 There are already several studies discussing the implementation of wellness programs for neurosurgical residents and attendings that have been shown to positively impact the personal life and professional life of the participants.27, 28, 29, 30
Future Studies
To safely and reliably provide for the needs of the increasing patient population, it is essential to create institutional programs to diminish the potential stressors that can lead to unhealthy levels of stress and burnout in the neurosurgical community.31 , 32 Such programs could be tailored to practice types (academic vs. private vs. hospital-based) based on research that would further clarify the predictors of burnout.
Some researchers have already begun work on programs to reduce stress and burnout.33, 34, 35 An intervention involving facilitated physician discussion groups around mindfulness, reflection, shared experience, and small-group learning has shown increased empowerment and engagement at work, decreased rates of depersonalization, and decreased overall burnout among participating physicians.34 Another intervention that offered an educational course on mindfulness meditation, self-awareness, and meaningful clinical narratives was shown to improve scores for mindfulness, burnout, depersonalization, personal accomplishment, and empathy.33 Finally, it would be interesting to repeat this study in the future to ascertain the full impact of health care reform.
Study Limitations
Despite all the efforts deployed, this study has several limitations. There are, in fact, some limitations in the methodology used. The inclusion of only articles written in English could have excluded some relevant articles from non-English speaking countries. An important limitation is related to the study topic itself; currently, BS remains a pathological entity in need of a better definition.32 It is important then to keep in mind that the authors could have used different criteria to study the syndrome. Heterogeneity is a potential problem, both in terms of populations included (since the selected papers analyze residents in neurosurgery and neurosurgeons) and of scales used to measure burnout, even though most of them used the MBI scale. It is important to mention that all data collection methods have significant inherent biases and limitations, including sampling error and selection bias. These limitations are further confounded at the meta-analysis level, because the included studies are not independent samples. For example, the 3 studies of US neurosurgery residents9 , 11 , 12 included 1028 subjects. There are approximately 1200 neurosurgery residents in the US11; therefore, it is almost certain that the meta-analysis includes the at least most of the residents in the 3 studies. Another limitation is that the scales measuring burnout have been designed for an enduring state and thus are relatively insensitive to minor fluctuations.
Furthermore, owing to the novelty of the topic and the limited empirical scientific literature, the analysis suffers from a limited data input sample size, requiring additional primary studies to improve the statistical robustness of the meta-analysis. An augmented pool of empirical studies will allow the design of a moderator analysis enabling the assessment of subvariables that may influence and have a high correlation with burnout levels in neurosurgeons and residents.
Conclusions
BS is a condition that affects all medical and surgical specialties. According to the literature, neurosurgery is the most affected specialty (48.4%); these results held when neurosurgeons (51.1%) and neurosurgical residents (45.4%) were analyzed separately. Given the severe consequences of BS, institutions and departments should be encouraged to develop and improve wellness programs. We hope that these results will raise awareness, stimulate further studies, and lead to programs designed to mitigate excessive stress and burnout within neurosurgery.
CRediT authorship contribution statement
Ismail Zaed: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Youssef Jaaiddane: Formal analysis, Writing - original draft. Salvatore Chibbaro: Formal analysis, Writing - review & editing, Visualization. Benedetta Tinterri: Methodology, Writing - original draft, Writing - review & editing.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.IsHak W.W., Lederer S., Mandili C., et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1:236–242. doi: 10.4300/JGME-D-09-00054.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freudenberger H.J. Staff burnout. J Soc Issues. 1974;30:159–165. [Google Scholar]
- 3.Rodrigues H., Cobucci R., Oliveira A., et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018;13:e0206840. doi: 10.1371/journal.pone.0206840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maslach C., Jackson S.E. The measurement of experienced burnout. J Occup Behav. 1981;2:99–113. [Google Scholar]
- 5.McAbee J.H., Ragel B.T., McCartney S., et al. Factors associated with career satisfaction and burnout among US neurosurgeons: results of a nationwide survey. J Neurosurg. 2015;123:161–173. doi: 10.3171/2014.12.JNS141348. [DOI] [PubMed] [Google Scholar]
- 6.Moher D., Shamseer L., Clarke M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 8.Klimo P., Jr., DeCuypere M., Ragel B.T., McCartney S., Couldwell W.T., Boop F.A. Career satisfaction and burnout among U.S. neurosurgeons: a feasibility and pilot study. World Neurosurg. 2013;80:e59–e68. doi: 10.1016/j.wneu.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 9.Attenello F.J., Buchanan I.A., Wen T., Donoho D.A., McCartney S., Cen S.Y. Factors associated with burnout among US neurosurgery residents: a nationwide survey. J Neurosurg. 2018;129:1349–1363. doi: 10.3171/2017.9.JNS17996. [DOI] [PubMed] [Google Scholar]
- 10.Fargen K.M., Arthur A.S., Leslie-Mazwi T., et al. A survey of burnout and professional satisfaction among United States neurointerventionalists. J Neurointerv Surg. 2019;11:1100–1104. doi: 10.1136/neurintsurg-2019-014833. [DOI] [PubMed] [Google Scholar]
- 11.Shakir H.J., McPheeters M.J., Shallwani H., Pittari J.E., Reynolds R.M. The prevalence of burnout among US neurosurgery residents. Neurosurgery. 2018;83:582–590. doi: 10.1093/neuros/nyx494. [DOI] [PubMed] [Google Scholar]
- 12.Shakir H.J., Cappuzzo J.M., Shallwani H., et al. Relationship of grit and resilience to burnout among US neurosurgery residents. World Neurosurg. 2020;134:e224–e236. doi: 10.1016/j.wneu.2019.10.043. [DOI] [PubMed] [Google Scholar]
- 13.Yu J., Gao J., Chen J., Sun Y. Academic versus non-academic neurosurgeons in China: a national cross-sectional study on workload, burnout and engagement. BMJ Open. 2019;9:e028309. doi: 10.1136/bmjopen-2018-028309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shanafelt T.D., Balch C.M., Bechamps G., et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 15.West C.P., Huschka M.M., Novotny P.J., et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296:1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 16.Campbell D.A., Jr., Sonnad S.S., Eckhauser F.E., Campbell K.K., Greenfield L.J. Burnout among American surgeons. Surgery. 2001;130:696–705. doi: 10.1067/msy.2001.116676. [DOI] [PubMed] [Google Scholar]
- 17.Jones J.W., Barge B.N., Steffy B.D., Fay L.M., Kunz L.K., Wuebker L.J. Stress and medical malpractice: organizational risk assessment and intervention. J Appl Psychol. 1988;73:727–735. doi: 10.1037/0021-9010.73.4.727. [DOI] [PubMed] [Google Scholar]
- 18.Linn L.S., Brook R.H., Clark V.A., Davies A.R., Fink A., Kosecoff J. Physician and patient satisfaction as factors related to the organization of internal medicine group practices. Med Care. 1985;23:1171–1178. doi: 10.1097/00005650-198510000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Balch C.M., Shanafelt T.D., Sloan J.A., Satele D.V., Freischlag J.A. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg. 2011;254:558–568. doi: 10.1097/SLA.0b013e318230097e. [DOI] [PubMed] [Google Scholar]
- 20.Ribeiro R.V.E., Martuscelli O.J.D., Vieira A.C., Vieira C.F. Prevalence of burnout among plastic surgeons and residents in plastic surgery: a systematic literature review and meta-analysis. Plast Reconstr Surg Glob Open. 2018;6:e1854. doi: 10.1097/GOX.0000000000001854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shanafelt T.D., Balch C.M., Bechamps G.J., et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463–471. doi: 10.1097/SLA.0b013e3181ac4dfd. [DOI] [PubMed] [Google Scholar]
- 22.Tang O.Y., Dunn K.A., Yoon J.S., Ponce F.A., Sonntag V.K.H., Lawton M.T. Neurosurgery resident wellness and recovery from burnout: a 39-year single institution experience. World Neurosurg. 2020;138:e72–e81. doi: 10.1016/j.wneu.2020.01.236. [DOI] [PubMed] [Google Scholar]
- 23.Shanafelt T.D., Balch C.M., Dyrbye L., et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146:54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 24.Haik J., Brown S., Liran A., et al. Burnout and compassion fatigue: prevalence and associations among Israeli burn clinicians. Neuropsychiatr Dis Treat. 2017;13:1533–1540. doi: 10.2147/NDT.S133181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fargen K.M., Spiotta A.M., Turner R.D., Patel S. Operation La Sierra: a novel wellness initiative for neurological surgery residents. J Grad Med Educ. 2016;8:457–458. doi: 10.4300/JGME-D-15-00641.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamade Y.J., Aoun R.J.N., Zimmerman R.S., Bendok B.R. The modern neurosurgical leader as a cure for team burnout. Neurosurgery. 2015;77:N13. doi: 10.1227/01.neu.0000467292.26010.c3. [DOI] [PubMed] [Google Scholar]
- 27.Buchholz A.L., Henderson F., Jr., Lowe S., et al. Perspectives from a residency training program following the implementation of a wellness initiative. World Neurosurg. 2018;119:e947–e955. doi: 10.1016/j.wneu.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 28.Spiotta A.M., Fargen K.M., Patel S., Larrew T., Turner R.D. Impact of a residency-integrated wellness program on resident mental health, sleepiness, and quality of life [Erratum in Neurosurgery 2019;84:E334-E344] Neurosurgery. 2019;84:341–346. doi: 10.1093/neuros/nyy112. [DOI] [PubMed] [Google Scholar]
- 29.Wolfe S.Q., West J.L., Hunt M.A., et al. A comparison of the existing wellness programs in neurosurgery and institution champion's perspectives. Neurosurgery. 2019;84:1149–1155. doi: 10.1093/neuros/nyy418. [DOI] [PubMed] [Google Scholar]
- 30.Zaed I., Tinterri B. Letter to the Editor: How is COVID-19 going to affect education in neurosurgery? a step toward a new era of educational training. World Neurosurg. 2020;140:481–483. doi: 10.1016/j.wneu.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bianchi R., Schonfeld I.S., Laurent E. Burnout-depression overlap: a review. Clin Psychol Rev. 2015;36:28–41. doi: 10.1016/j.cpr.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 32.Krasner M.S., Epstein R.M., Beckman H., et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 33.West C.P., Dyrbye L.N., Rabatin J.T., et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med. 2014;174:527–533. doi: 10.1001/jamainternmed.2013.14387. [DOI] [PubMed] [Google Scholar]
- 34.Zaed I., Menna G., Caccavella V.M., et al. Italian neurosurgical residents' experience with research activities: a national survey. https://doi.org/10.1016/j.wneu.2020.06.105 [e-pub ahead of print]. World Neurosurg. accessed June 22, 2020. [DOI] [PubMed]
- 35.Zaed I. COVID-19 consequences on medical students interested in neurosurgery: an Italian perspective. https://doi.org/10.1080/02688697.2020.1777260 [e-pub ahead of print]. Br J Neurosurg. accessed July 6, 2020. [DOI] [PubMed]