Abstract
Coronavirus disease (COVID-19) pandemic has become a significant global public health concern. Since the announcement of the Public Health Emergency of International Concern, many countries have implemented lockdown and restrictive quarantines; therefore, routine dentistry, as well as oral medicine practise, have been suspended in several countries. However, urgent oral cares and emergencies are still operated and delivered by on-call dental practitioners. The objective of this study was to investigate the management of oral medicine emergency during a viral pandemic such as COVID-19. During the lockdown period, digital technologies, such as video conferencing with Zoom, Google Meeting or WhatsApp, are useful and efficient tools that oral medicine practitioners could consider to use for patient triage, managing emergencies, reassure, and follow patients remotely. Oral medicine emergencies can be carefully evaluated and triaged via video conferencing and sometimes phone contact, to avoid life-threatening risks while realising the limitations by both patient and clinician.
Keywords: COVID-19, Oral medicine emergency, Video conferencing
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was reported by The World Health Organization (WHO) on the 31st December 2019.1 Since the announcement of Public Health Emergency of International Concern, countries such as China, France, Italy, New Zealand, and the UK have implemented the world's largest and most restrictive mass quarantines. For example, people are instructed to stay at home, non-essential businesses and educational institutes are closed, travelling is strictly limited, and health care is limited to emergency only.2
The spectrum of the illness of COVID-19 ranges from mild (asymptomatic) to critical (respiratory failure, or multiorgan dysfunction), fortunately, most infection are not severe.3 The route of transmission is not yet fully solved. It is thought to be via respiratory droplets, similar to the spread of influenza.4 Besides respiratory droplets, SARS-CoV-2 RNA can be found in blood and stool specimens.5,6 Dental procedures using drills or ultrasonic devices can produce aerosol release, which would then increase the risk of transmission. Although the live virus can be cultured in patients' stool, according to a Chinese study, faecal-oral route transmission remains low.4
Routine dentistry has been suspended in several countries, including New Zealand. However, urgent dental care is still being operated and delivered by emergency or on-call dental teams. Therefore, dental professions should understand the modes of transmission of SARS-CoV-2, identify potential patients with COVID-19, and understand the needs of extra-protection during their practise to minimise the transmission of SARS-CoV-2 infection.7 Patient screening by a questionnaire, hand hygiene, correct use of the personal protective equipment, mouth rinse before dental procedures, rubber dam isolation, anti-retraction handpiece, disinfection of the clinic settings, correctly management of medical waste is the fundamental aspect of breaking the chain of infection in dental practice.7
Oral medicine specialists generally manage chronic oral mucosal diseases and orofacial pain. Some diseases and conditions are considered to be oral medicine emergencies such as exacerbation of pemphigus or pemphigoid, Stevens-Johnson syndrome, toxic epidermal necrolysis, mucositis and giant cell arteritis. When patients suffer from these problems, an unscheduled appointment is required to resolve the issues. However, oral medicine service is limited by the availability of oral medicine specialists, especially during the lockdown period. Furthermore, during this stressful period, some oral mucosal diseases or orofacial pain problems may represent urgencies, not true emergencies; hence digital technology such as video conferencing might be a reasonable option when evaluating these cases. This brings to the forefront of how important a good history and patient interview and even the use of clinical photographs can be in getting to a differential diagnosis under pandemic conditions.
Guidelines for dental care provision during the COVID-19 pandemic has been developed in several countries,8 however, guideline for the management of oral medicine emergency is still scarce. A brief summary and discussion on the management of oral medicine patients during COVID-19 emergency are proposed as follows, focussing on remote assistance devices and classification of emergencies.
Digital technologies for managing health care emergency
For the present study, video conferencing is defined as the use of communication video devices to hold discussions such as consultation, diagnosis, treatment planning and follow up via electronic transmission between participants in different locations.9 Electronic databases were searched to identify relevant articles. Searches were limited to the English language and publication date from the earliest available date for each database to April 2020. In this study, researchers conducted searches PubMed/MEDLINE, Cochrane Library and Web of Science for articles published until April 2020. The search strategies included subject headings and subheadings (if available) combined with keyword searching. The research terms were video conferencing or video conferencing software in health. Studies were included if they were designed as an interventional, used quantitative or qualitative approaches, and presented findings related to video conferencing. There were no restrictions for age or care setting, such as home, community or facility. Studies were excluded if they included other digital technologies, such as telemonitoring devices, telecare devices, electronic health care records, telepresence devices, digital pen and paper technology, and audit feedback. Studies were also excluded if they provided insufficient information to allow adequate interpretation of the study design, measures or results, or if they were only found in abstract form, in abstracts or posters from conference proceedings. Total of 492 references were found, PubMed/MEDLINE (365), Web of Science (124) and Cochrane Library (3). Within 492 references, Zoom Video Communications (27) and WhatsApp (14) were the most referenced video conferencing software. Most of the references did not name the video conferencing software.
A number of digital technologies have been used for health care, such as telemonitoring devices, telecare devices, teleconferencing, electronic health care records, telepresence devices, digital pen and paper technology, and teleconferencing and audit feedback.10 This article focused on one type of digital technology – video conferencing, which has been considered to be a useful and efficient tool for continuous quality improvement, education, and patient care when the in-person discussion is not possible because of geographic and schedule constraints.11
Video Communications has been found to be feasible and effective in chronic diseases management;12 however, security and patient confidentiality are paramount when choosing the software. There are many video conferencing software in the market, such as Zoom Video Communications and WhatsApp. Zoom Video Communications is an American remote conferencing services company headquartered in San Jose, California. It provides a remote conferencing service that combines video conferencing, online meetings, chat, and mobile collaboration, and the service started in early 2013. Its use has significantly increased in the world due to the COVID-19 pandemic, as teaching and meetings have shifted to online platforms. In addition to teaching and meetings, Zoom Video Communications has been used in many health care settings, including multidisciplinary hospital meeting, cardiology, and mental health.11,13 WhatsApp Messenger is an American freeware, cross-platform messaging and Voice over IP (VoIP) service owned by Facebook. It has been suggested to be used in the management of orthodontic emergencies during COVID-19.14 The national cybersecurity centre of New Zealand suggested care when using video conferencing software.15
Security and patient confidentiality are two big concerns, and patient consent is important in this context. The oral health practitioners should take extra care to ensure that patient privacy is not compromised by unauthorised entities. However, patients should be made aware that their information is to be transmitted electronically. It is possible that their information will be intercepted, despite maximum efforts to maintain security.16 The concerns of a proper method of informing patients about the potential transmission of their data also may arise. Informed consent in video conferencing should be recorded and cover everything that exists in a standard, traditional consent form.17 The patient should be informed of the inherent risk of the lack of totally accurate triage, diagnosis and/or treatment due to failure of the technology involved and not being able to physically examine the patient.18 As well, medicolegal such as licensure, jurisdiction, and malpractice, have not been definitively decided by legislative or judicial branches of various governments.17,19 Nevertheless, there is still a drive to use digital technology creatively in the provision of health care.20 It is recommended that to ensure an appropriate level of security and privacy is maintained, setting up a password, activating the verification and changing some of the default configurations for the meeting may be necessary.
Several guidelines have developed for the video conferencing, including Australian Dental Association Guidelines for Teledentistry,21 and however, most of them are hard tissue focused. There is no mention of soft tissue or oral-facial pain emergency. In this COVID-19 situation, it is important to identify and prioritise who requires urgent intervention. An accurate triage decision helps patients receive the emergency service in the most appropriate time, but with limited numbers of oral medicine specialist and resource, this might be difficult to achieve. It is recommended for large centres to have their oral medicine specialists and video conferencing software available for triaging and remote assistance during COVID-19 period. Besides, video conferencing could be used to review low-risk diseases or well-controlled conditions. Repeated medication, routine blood tests could be prescribed via video conferencing software with electronic ID and signature. Oral medicine specialists should be more proactive to use their technology to take care of small centres or areas that do not have an oral medicine specialist during this period. However, we must stress that the clinicians and patients alike need to be aware of the limitations of remote and video consultations.
Oral medicine emergency, video conferencing triage and management
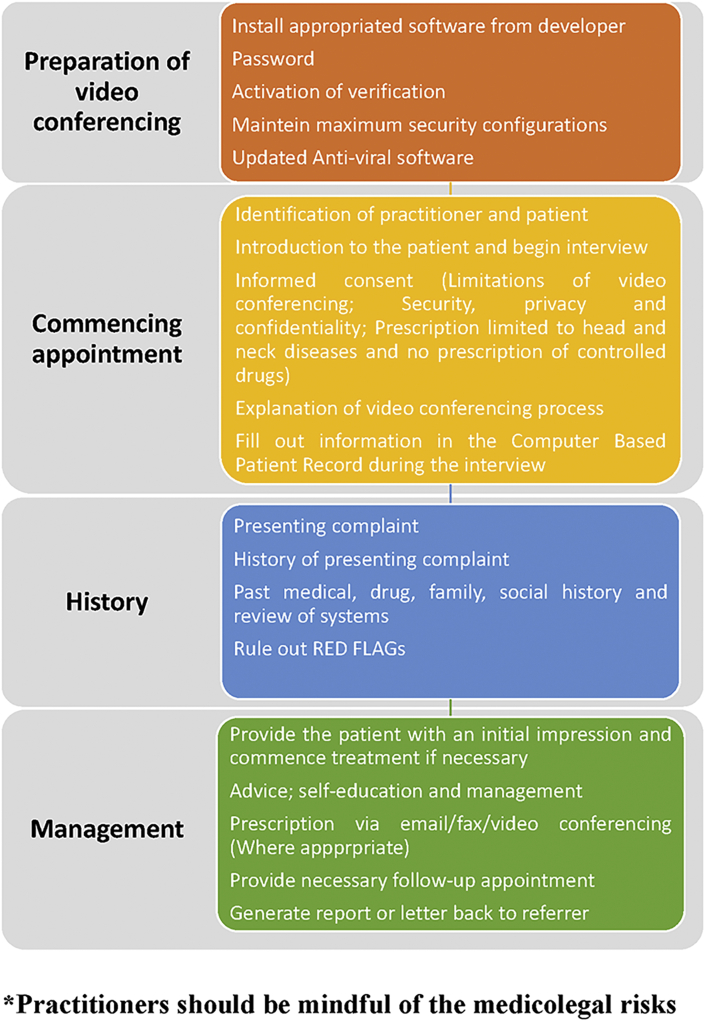
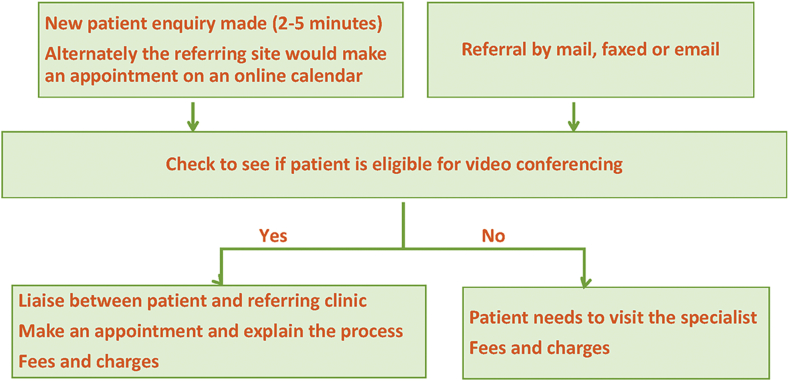
Video conferencing has been successfully used in oral medicine.20 The most common oral medicine emergencies usually include severe vesiculobullous lesions and giant cell arteritis. The video conferencing triage and management of these emergencies are summarised in Table 1. We also proposed a guideline for the practitioners, and it is based on the New Zealand Dental Association “COVID-19 Safety Standards”, and Australian Dental Association Guidelines for Teledentistry (Figure 1, Figure 2).21,22
Table 1.
Oral medicine emergency, video conferencing triage and management.
| Oral medicine emergency | Video conferencing triage | Management |
|---|---|---|
| Oral mucosal diseases | ||
| Pemphigus vulgaris (Severe) | Generally middle aged 50–60; Sore mouth; Widespread bullae formation on the skin and oral mucosa; Skin are fragile and break down rapidly to form crusted, eroded lesion. |
Hospital admission immediately; Assessment of volume status and resuscitation; Removal of possible triggers, such as drugs; Ocular assessment; Systemic corticosteroid according to the guideline; Consider other immune suppressive drugs such as azathioprine, mycophenolate mofetil, cyclophosphamide and rituximab. |
| Mucous membrane pemphigoid (Severe) | Generally over 60 years; Sore mouth; Widespread bullae formation on the skin and oral mucosa; Intact bullae may be present. |
Hospital admission immediately; Assessment of volume status and resuscitation; Removal of possible triggers, such as drugs; Ocular assessment; Systemic corticosteroid according to the guideline; Consider other immune suppressive drugs such as azathioprine, mycophenolate mofetil, cyclophosphamide. |
| Erythema multiforme | History of herpes simplex virus, or mycoplasma pneumonia infection; Target-like lesions on the skin; Sore lips; Lips erosion often accompanied by crusting and bleeding. |
Evaluation by oral medicine specialist; Supportive care; Patient review via video conferencing. |
| Stevens-Johnson syndrome and toxic epidermal necrolysis | Extensive necrosis and detachment of the epidermis. | Hospital admission immediately; Management similar to burn; ICU care. |
| Oral mucositis (Severe) | Cancer patients undergoing chemotherapy or radiotherapy; Widespread ulcers with extensive erythema; Patient cannot swallow food. |
Hospital admission immediately; Management should be consulted with oncologist. |
| Orofacial pain | ||
| Giant cell arteritis | Patient over age of 50 years with new headaches, abrupt onset of visual disturbances, jaw claudication, tenderness of temporalis muscles to palpation | Hospital admission immediately; Consider steroids prior to temporal artery biopsy; Ophthalmologist evaluation; If the patient is in the remote area, a course of high dose prednisone should be given to prevent possible ophthalmic complication. |
| Other chronic maxillofacial pain conditions | Pain history, medical history, personal history, treatment history and family history; Ruling out red flags or warning signals. Systemic signs (fever, myalgias, weight loss, history of malignancy or AIDS) Neurologic signs or symptoms Onset sudden Older age (older than 50) Pattern change from previous headaches |
Trigeminal autonomic cephalalgias - Medication as per diagnosis; Trigeminal Neuralgia- Oxcarbazepine/Carbamazepine, Gabapentin, Pregabalin; Temporomandibular joint dysfunction- Non-surgical self-help, CBT online, pain medications |
Figure 1.
Video conferencing guideline in oral medicine.
Figure 2.
Administration flowchart.
Management of oral mucosal disease emergencies
Exacerbation or acutely presentation of vesiculobullous diseases, such as pemphigus vulgaris, mucous membrane pemphigoid, erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis could be potentially life-threatening.
Pemphigus vulgaris is characterised by the development of autoantibodies to antigens on the keratinocytes, commonly affect patients between the ages of 40 and 60. The clinical feature in pemphigus vulgaris is of widespread bullae formation on the skin and oral mucosa. As the bullae are intraepithelial, they are fragile and break down rapidly. Patient can potentially develop severe dehydration, infection and leads to multiorgan failure due to extensive loss of surface epithelium. Systemic corticosteroid remains the first-line treatment for Pemphigus vulgaris.23 Once remission is induced and maintained with the healing of the majority of lesions, the dose can be tapered down. Other immune suppressive drugs such as azathioprine, mycophenolate mofetil, cyclophosphamide and rituximab may be used off-label to reduce the dose of steroids.23
Mucous membrane pemphigoid is characterised by the formation of subepidermal bullae and the presence of autoantibodies at the basement membrane. While most patients have oral lesions, there are subgroup of patients with skin involvement. Severe dehydration and electrolyte abnormalities could be seen in patients with lesions covering a large surface area, and assessment of volume status and resuscitation are important. The approach to the treatment of mucous membrane pemphigoid is influenced by the site(s) of mucosal involvement and the severity of the disease. Multidisciplinary management, such as oral medicine specialist, dermatologist, ophthalmologist, gynaecologist and ENT specialist, is often required to minimise risk for adverse sequelae of this disease. Patients with severe, refractory mucous membrane pemphigoid may benefit from more aggressive therapy, such as 1 mg/kg/day of prednisone.24 Other immune suppressive drugs such as azathioprine, mycophenolate mofetil, cyclophosphamide can be used in combination with systemic corticosteroid.24,25 In mild case (patchy, localised involvement of the oral mucosa), management and review could be guided by the oral medicine specialist via video conferencing.
Erythema multiforme is an acute, immune-mediated condition characterised by the appearance of distinctive target-like lesions on the skin. This disorder may be induced by infection, such as herpes simplex virus, or mycoplasma pneumonia. The main feature of an attack is the sudden development of the oral mucosa, especially the lip. The erosion of the lips is often accompanied by crusting and bleeding; therefore, patients often seek for urgent advice. The clinical course of erythema multiforme is usually self-limiting, resolving within weeks without significant sequelae. The management relies on supportive care.26,27 However, in some cases of erythema multiforme, this disease may be managed by relatively high dose of prednisolone.28 Once the diagnosis is confirmed by the oral medicine specialist, video conferencing can be used for patient's review and guidance of the supportive care.
Stevens-Johnson syndrome and toxic epidermal necrolysis are severe mucocutaneous conditions suggested to be different from erythema multiforme.29 They are mostly triggered by medications such as antibiotic, anti-convulsant, NSAIDs, and allopurinol, and characterised by extensive necrosis and detachment of the epidermis.30 Stevens-Johnson syndrome is less severe, and the skin detachment is less than 10% of the body surface; however, toxic epidermal necrolysis involves more than 30% of the body surface and considered more severe.31,32 The management of Stevens-Johnson syndrome and toxic epidermal necrolysis are similar to the major burns. It includes wound care, fluid and electrolyte management, nutritional support, temperature management, pain control, and monitoring or treatment of infections.33 Patient should be admitted to the hospital immediately.
Oral mucositis is probably the most common, debilitating complication of cancer treatments, particularly chemotherapy and radiation. If the patients develop widespread ulcers with extensive erythema, and they are unable to tolerate food to fluids. They should be admitted to the hospital immediately. The management should be consulted with an oncologist.
Oral squamous cell carcinomas might develop from oral potentially malignant disorders, such as leukoplakia or erythroplakia. The malignant transformation rate varies from less than 1% to more than 50%.34 However, they are asymptomatic. These disorders may represent urgencies, not true emergencies. Removal of the risk factors, such as drinking and smoking, and review the patients would be the first step. Whether the patients require immediately biopsy for the diagnosis, is dependent on practitioner decision.
Management of orofacial pain emergency
The importance of a good pain history cannot be stressed and will be valuable in distinguishing between the different orofacial pain conditions. This can even be diagnostic for Trigeminal Autonomic Cephalagias (TACs), Trigeminal Neuralgias and less so with Temporomandibular Disorders (TMD) especially myogenous. However, TMDs are more common than the other chronic facial pain conditions and reassurance and patient education and self-help advice as well as blood tests where required can be carried out remotely.35
Giant cell arteritis is a systemic vasculitides that affects the orofacial region,36 although not as common as TMD, should be included in the differential diagnoses. The diagnosis of giant cell arteritis should be considered in a patient over the age of 50 years with symptoms or signs of new headaches, abrupt onset of visual disturbances, jaw claudication, tenderness of temporalis muscles to palpation, unexplained fever or anaemia, and high erythrocyte sedimentation rate and/or high serum C-reactive protein.36 Giant cell arteritis could affect the ophthalmic artery and its branches, including the posterior ciliary arteries and the central retinal artery.37 All acute ophthalmic manifestations of giant cell arteritis are medical emergencies, given the risk for progressive and permanent damage.37,38 Inflammation of these arteries could lead to optic neuropathy (arteritic anterior ischaemic), which is often severe and irreversible, and it is the most common cause of giant cell arteritis associated blindness.39 High-dose glucocorticoids are the mainstay of initial treatment of giant cell arteritis patients with visual symptoms.40,41 Patients with suspicious of giant cell arteritis during video conferencing triage need to be referred to hospital immediately for further evaluation. If the patient is in the remote area, a course of high dose prednisone should be given to prevent possible ophthalmic complication of giant cell arteritis.
The most common condition seen by oral medicine specialists is chronic facial pain, of which temporomandibular joint dysfunction is most prevalent. Temporomandibular joint dysfunction with myogenous and/or arthrogenous pain may have a central sensitisation component. Often these patients may have other comorbidities, including anxiety among other problems. These conditions may exacerbate during stressful events like a pandemic requiring lockdown, and as with COVID-19 the risk of death could weigh on a patient's mind. Mostly these patients can be managed by non-surgical methods, reassurance and sometimes with the use of neuropathic pain medications,35 all of which to some degree be carried out remotely.
In the authors' experience during the New Zealand lockdown, the most common oral medicine cases have been chronic facial pain, such as temporomandibular joint dysfunction and exacerbations of vesiculobullous lesions. However, the conditions listed in Table 1 may act as a guideline as lockdown periods are extended for longer periods. These initial guidelines are likely to evolve further as more information and data come to hand. We suggest these guidelines mainly for the New Zealand sector where the current situation may be slightly different from other countries, however the general principles can still apply to other countries.
Conclusion
During the lockdown period of a pandemic, while adhering to the “stay at home and save lives” proposal, video conferencing is a useful technology and platform that could be used in patient triage, managing emergencies, provide reassurance, and allow follow-up of patients remotely. Oral medicine emergencies can be carefully evaluated and triaged via video conferencing and sometimes phone contact, to avoid life-threatening risks while realising the limitations by both patient and clinician.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgments
We thank for Anhui Provincial Higher Education Talent Project, gxyq2018010 and Natural Science Research Project of Anhui Higher Education Institutions, KJ2017A830, for the support of the publication cost.
References
- 1.Zhang Y., Xu J., Li H., Cao B. A novel coronavirus (COVID-19) outbreak: a call for action. Chest. 2020;157:e99–e101. doi: 10.1016/j.chest.2020.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.New Zealand Government . 2020. COVID-19 alert system.https://covid19.govt.nz/alert-system/covid-19-alert-system/#level-4-eliminate Available at: [Google Scholar]
- 3.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han Y., Yang H. The transmission and diagnosis of 2019 novel coronavirus infection disease (COVID-19): a Chinese perspective. J Med Virol. 2020;92:639–644. doi: 10.1002/jmv.25749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang A., Tong Z.D., Wang H.L. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis. 2020;26:1337–1339. doi: 10.3201/eid2606.200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen W., Lan Y., Yuan X. Detectable 2019-nCoV viral RNA in blood is a strong indicator for the further clinical severity. Emerg Microbes Infect. 2020;9:469–473. doi: 10.1080/22221751.2020.1732837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alharbi A., Alharbi S., Alqaidi S. Guidelines for dental care provision during the COVID-19 pandemic. Saudi Dent J. 2020;32:181–186. doi: 10.1016/j.sdentj.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen J.W., Hobdell M.H., Dunn K., Johnson K.A., Zhang J. Teledentistry and its use in dental education. J Am Dent Assoc. 2003;134:342–346. doi: 10.14219/jada.archive.2003.0164. [DOI] [PubMed] [Google Scholar]
- 10.Newbould L., Mountain G., Hawley M.S., Ariss S. Videoconferencing for health care provision for older adults in care homes: a review of the research evidence. Int J Telemed Appl. 2017:1–7. doi: 10.1155/2017/5785613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen G.I. A practical guide to graphic communication for quality assurance, education, and patient care in echocardiography. Echocardiography. 2019;36:1747–1754. doi: 10.1111/echo.14464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallow J.A., Petitte T., Narsavage G. The use of video conferencing for persons with chronic conditions: a systematic review. E-Health Telecommun Syst Netw. 2016;5:39–56. doi: 10.4236/etsn.2016.52005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McCarty C.A., Zatzick D., Hoopes T., Payne K., Parrish R., Rivara F.P. Collaborative care model for treatment of persistent symptoms after concussion among youth (CARE4PCS-II): study protocol for a randomized, controlled trial. Trials. 2019;20:1–14. doi: 10.1186/s13063-019-3662-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caprioglio A., Pizzetti G.B., Zecca P.A., Fastuca R., Maino G., Nanda R. Management of orthodontic emergencies during 2019-NCOV. Prog Orthod. 2020;21:10. doi: 10.1186/s40510-020-00310-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Cyber Security Centre New Zealand . 2020. Zoom security advice from the GCISO (Updated)https://www.ncsc.govt.nz/newsroom/zoom-security-advice-for-public-servants/ Available at: [Google Scholar]
- 16.Chang S.W., Plotkin D.R., Mulligan R., Polido J.C., Mah J.K., Meara J.G. Teledentistry in rural California: a USC initiative. J Calif Dent Assoc. 2003;31:601–608. [PubMed] [Google Scholar]
- 17.Jampani N.D., Nutalapati R., Dontula B.S., Boyapati R. Applications of teledentistry: a literature review and update. J Int Soc Prev Community Dent. 2011;1:37–44. doi: 10.4103/2231-0762.97695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golder D.T., Brennan K.A. Practicing dentistry in the age of telemedicine. J Am Dent Assoc. 2000;131:734–744. doi: 10.14219/jada.archive.2000.0272. [DOI] [PubMed] [Google Scholar]
- 19.Sanders J.H., Bashshur R.L. Challenges to the implementation of telemedicine. Telemed J. 1995;1:115–123. doi: 10.1089/tmj.1.1995.1.115. [DOI] [PubMed] [Google Scholar]
- 20.Bradley M., Black P., Noble S., Thompson R., Lamey P.J. Application of teledentistry in oral medicine in a community dental service, N. Ireland. Br Dent J. 2010;209:399–404. doi: 10.1038/sj.bdj.2010.928. [DOI] [PubMed] [Google Scholar]
- 21.Australian Dental Association . 2020. Australian dental association guidelines for Teledentistry.https://www.ada.org.au/Dental-Professionals/Policies/Dental-Practice?page=3 Available at: [Google Scholar]
- 22.New Zealand Dental Association . 2020. COVID-19 safety standards.https://www.nzda.org.nz/assets/files/Standards__Guidelines/COVID-19_Safety_Standards.pdf Available at: [Google Scholar]
- 23.Harman K.E., Brown D., Exton L.S. British Association of Dermatologists' guidelines for the management of pemphigus vulgaris 2017. Br J Dermatol. 2017;177:1170–1201. doi: 10.1111/bjd.15930. [DOI] [PubMed] [Google Scholar]
- 24.Kourosh A.S., Yancey K.B. Therapeutic approaches to patients with mucous membrane pemphigoid. Dermatol Clin. 2011;29:637–641. doi: 10.1016/j.det.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 25.Chan L.S., Ahmed A.R., Anhalt G.J. The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol. 2002;138:370–379. doi: 10.1001/archderm.138.3.370. [DOI] [PubMed] [Google Scholar]
- 26.Zoghaib S., Kechichian E., Souaid K., Soutou B., Helou J., Tomb R. Triggers, clinical manifestations, and management of pediatric erythema multiforme: a systematic review. J Am Acad Dermatol. 2019;81:813–822. doi: 10.1016/j.jaad.2019.02.057. [DOI] [PubMed] [Google Scholar]
- 27.de Risi-Pugliese T., Sbidian E., Ingen-Housz-Oro S., Le Cleach L. Interventions for erythema multiforme: a systematic review. J Eur Acad Dermatol Venereol. 2019;33:842–849. doi: 10.1111/jdv.15447. [DOI] [PubMed] [Google Scholar]
- 28.Michaels B. The role of systemic corticosteroid therapy in erythema multiforme major and stevens-johnson syndrome: a review of past and current opinions. J Clin Aesthet Dermatol. 2009;2:51–55. [PMC free article] [PubMed] [Google Scholar]
- 29.Roujeau J.C. Stevens-Johnson syndrome and toxic epidermal necrolysis are severity variants of the same disease which differs from erythema multiforme. J Dermatol. 1997;24:726–729. doi: 10.1111/j.1346-8138.1997.tb02524.x. [DOI] [PubMed] [Google Scholar]
- 30.Stern R.S., Divito S.J. Stevens-Johnson syndrome and toxic epidermal necrolysis: associations, outcomes, and pathobiology - thirty years of progress but still much to be done. J Invest Dermatol. 2017;137:1004–1008. doi: 10.1016/j.jid.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bastuji-Garin S., Rzany B., Stern R.S., Shear N.H., Naldi L., Roujeau J.C. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol. 1993;129:92–96. [PubMed] [Google Scholar]
- 32.Sousa-Pinto B., Araújo L., Freitas A., Correia O., Delgado L. Stevens-Johnson syndrome/toxic epidermal necrolysis and erythema multiforme drug-related hospitalisations in a national administrative database. Clin Transl Allergy. 2018;8:1–10. doi: 10.1186/s13601-017-0188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwartz R.A., McDonough P.H., Lee B.W. Toxic epidermal necrolysis: Part II. Prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. J Am Acad Dermatol. 2013;69:187. doi: 10.1016/j.jaad.2013.05.002. e1-16. [DOI] [PubMed] [Google Scholar]
- 34.Mortazavi H., Baharvand M., Mehdipour M. Oral potentially malignant disorders: an overview of more than 20 entities. J Dent Res Dent Clin Dent Prospects. 2014;8:6–14. doi: 10.5681/joddd.2014.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Polonowita A.D., Thomson W.M., Thorburn D.N. Clinical efficacy of a simplified approach to managing chronic temporomandibular disorders: evidence from a 1-year case series. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128:227–234. doi: 10.1016/j.oooo.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 36.Kale N., Eggenberger E. Diagnosis and management of giant cell arteritis: a review. Curr Opin Ophthalmol. 2010;21:417–422. doi: 10.1097/ICU.0b013e32833eae8b. [DOI] [PubMed] [Google Scholar]
- 37.Vodopivec I., Rizzo J.F., III Ophthalmic manifestations of giant cell arteritis. Rheumatology. 2018;57:ii63–ii72. doi: 10.1093/rheumatology/kex428. [DOI] [PubMed] [Google Scholar]
- 38.Danesh-Meyer H.V. Giant cell arteritis: a medical emergency. N Z Med J. 2008;121:10–13. [PubMed] [Google Scholar]
- 39.Biousse V., Newman N.J. Ischemic optic neuropathies. N Engl J Med. 2015;372:2428–2436. doi: 10.1056/NEJMra1413352. [DOI] [PubMed] [Google Scholar]
- 40.Bienvenu B., Ly K.H., Lambert M. Management of giant cell arteritis: recommendations of the French study group for large vessel vasculitis (GEFA) Rev Med Interne. 2016;37:154–165. doi: 10.1016/j.revmed.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 41.Mukhtyar C., Guillevin L., Cid M.C. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2009;68:318. doi: 10.1136/ard.2008.088351. [DOI] [PubMed] [Google Scholar]