Abstract
Churches are well positioned to promote better mental health outcomes in underserved populations, including rural adults. Mind–body (MB) practices improve psychological well-being yet are not widely adopted among faith-based groups due to conflicting religious or practice beliefs. Thus, “Harmony & Health” (HH) was developed as a culturally adapted MB intervention to improve psychosocial health in urban churchgoers and was adapted and implemented in a rural church. The purpose of this study was to explore the feasibility, acceptability, and efficacy of HH to reduce psychosocial distress in rural churchgoers. HH capitalized on an existing church partnership to recruit overweight or obese (body mass index [BMI] ≥25.0 kg/m2) and insufficiently active adults (≥18 years old). Eligible adults participated in an 8 week MB intervention and completed self-reported measures of perceived stress, depressive symptoms, anxiety, and positive and negative affect at baseline and postintervention. Participants (mean [M] age = 49.1 ± 14.0 years) were mostly women (84.8%), non-Hispanic white (47.8%) or African American (45.7%), high socioeconomic status (65.2% completed ≥bachelor degree and 37.2% reported an annual household income ≥$80,000), and obese (M BMI = 32.6 ± 5.8 kg/m2). Participants reported lower perceived stress (t = −2.399, p = .022), fewer depressive symptoms (t = −3.547, p = .001), and lower negative affect (t = −2.440, p = .020) at postintervention. Findings suggest that HH was feasible, acceptable, and effective at reducing psychosocial distress in rural churchgoers in the short-term. HH reflects an innovative approach to intertwining spirituality and MB practices to improve physical and psychological health in rural adults, and findings lend to our understanding of community-based approaches to improve mental health outcomes in underserved populations.
Keywords: Psychological well-being, Mind–body therapies, Rural health, Adults, Feasibility study
Culturally-adapted mind-body interventions are feasible, acceptable, and show promise for reducing psychosocial distress in adults residing in rural areas.
Implications.
Practice: Community-based settings, such as churches, are viable venues for reaching rural adults and for implementing behavioral health interventions to reduce psychosocial distress and improve quality of life.
Policy: Policymakers who want to reduce rural health disparities should explore the use of community-based settings, including churches, to extend services and care to adults residing in rural communities who have limited access to specialty care and mental health services.
Research: Future research is needed to test implementation strategies to improve the long-term sustainability of community-based programs to improve mental health among rural adults.
Introduction
Rural populations experience disparities in morbidity and mortality [1–4] in large part as a result of poorer health-related behaviors, such as maintaining a normal body weight and physical activity [2], and lower access to health care services [5] compared to those residing in urban or metropolitan areas. In addition to access to quality health services, rural stakeholders identified mental health as one of the most important rural priorities [5]. However, rural Americans face gross shortages in health care providers, including physicians, nurses, and specialty care providers, such as mental health professionals [6,7], despite reporting higher rates of depression, anxiety, and other mental health disorders [8]. Additionally, rural adults are less likely to perceive a need, or seek treatment, for mental health disorders [8,9]. Thus, traditional clinical treatment options may be less culturally acceptable or accessible for rural adults [10,11].
Previous studies have shown yoga to be effective for improving symptoms of depression [12,13], relieving stress and anxiety [14], and improving quality of life [15]. Yoga-based physical activity may be more sustainable and feasible and less intimidating than pharmacotherapy or psychotherapy for reducing psychosocial distress and improving quality of life in rural adults [10,16]. However, there are few studies on yoga and mind–body (MB) practices in rural or nonmetropolitan areas [17,18]. This may be due to a shortage of yoga therapists and other complementary and integrative health providers in rural areas [19] combined with a historical resistance to yoga and meditation in faith-based communities [20]. Nevertheless, rural adults are often willing to engage in MB practices, including yoga [21] and, thus, may benefit from community-based interventions that address barriers and acknowledge religious beliefs and rural cultural values [9–11].
Faith-based organizations play a key role in health promotion efforts and have the capacity to reach underserved populations, particularly rural residents and racial/ethnic minorities [22]. Thus, there is a growing trend to utilize academic-community partnerships to deliver physical and mental health programming to reduce health inequalities in underserved and hard-to-reach populations [22]. However, no study of which we are aware has explored the use of a culturally adapted MB intervention to improve psychological well-being in rural adults in a faith-based setting. “Harmony & Health” (HH), a culturally adapted MB intervention, was developed in partnership with a faith-based organization to promote physical activity, psychosocial well-being, and quality of life in metropolitan African-American adults [23]. Although HH was feasible and acceptable, it is unknown how the intervention would translate to a rural community-based setting and population and if it would remain efficacious when translated to a different setting and population.
Therefore, the primary aim of this study was to explore the feasibility and acceptability of HH in a church-based sample of rural, insufficiently active adults. Additionally, as a secondary aim, we tested the efficacy of the culturally adapted MB intervention to reduce psychosocial distress (e.g., perceived stress, depressive symptoms, anxiety, and positive and negative affect) and improve health-related quality of life in rural adults.
Materials and Methods
Study design and sample
HH was a faith-based, one-armed, 14-week feasibility study conducted in Centre County, PA, a medically underserved, nonmetropolitan area [24,25]. The study was conducted in two cohorts, Fall 2016 (July–October 2016) and Spring 2017 (March–July 2017). Participants were recruited to the study through an ongoing partnership with a local church in State College, PA. Participants were recruited face-to-face at church services through announcements from the pulpit and an information table and via ads placed in the church bulletin, flyers posted on church and community bulletin boards, and emails announcing the study to on- and off-campus listservs.
Interested participants completed a telephone or in-person screening to assess eligibility. Centre County residents who were at least 18 years old, overweight or obese (body mass index [BMI] ≥25.0 kg/m2), generally healthy and able to pass the Physical Activity Readiness Questionnaire (PAR-Q [26]), and insufficiently active (<120 min of physical activity per week) were eligible to participate. Participants deemed ineligible based on PAR-Q results related to the management of blood pressure or diabetes were asked to complete additional questions from the PAR-Q+ [27]. If still deemed ineligible based on PAR-Q+ results, participants had the option to provide a letter from their physician clearing them to participate in the study. This two-phased screening procedure reduced barriers to participation and ensured that adults and older adults for whom it is safe to engage in physical activity were able to participate in HH [28]. All study procedures and materials were reviewed and approved by an institutional review board, and participants provided written informed consent prior to participation.
Intervention and procedures
HH was initially developed and culturally adapted for African-American churchgoers in Houston, TX; details on the development of the intervention are available [23]. The curriculum was shared with a senior member and head pastor of a local church, who were African American and Christian, to ensure the intervention components aligned with the values of the church.
Women and men enrolled in the study attended two in-person, group-based 45 min MB intervention sessions each week for 8 weeks and were instructed to practice their stretches and relaxation activities individually at home at least twice a week. Due to inclement weather, one session was canceled in each of the cohorts for a total of 15 (instead of 16) sessions. All MB intervention sessions were held at a local church.
In-person sessions were led by a certified yoga instructor who was trained specifically for the current study. Participants practiced stretching for 30 min, followed by 15 min of guided relaxation, during which participants were instructed to relax, reflect on a biblical scripture of the day, and focus on their breath and God’s word [23]. Selected scriptures emphasized one’s mind, body, strength, faith, or peace and changed daily. Participants were provided a list of stretches, a 5 min video demonstrating the stretches, a relaxation tip sheet, and a list of the scriptures by session to aid their weekly practice at home. Research staff completed weekly reminder phone calls and sent reminder emails to encourage participants to practice their stretches and relaxation practices at home and to remind them of the date and time of the next face-to-face MB intervention session.
Data collection and measures
Participants completed in-person assessments at baseline, postintervention (8 weeks), and 6 week follow-up (14 weeks) at the Clinical Research Center on The Pennsylvania State University’s University Park campus. Participants completed a physical health assessment at each time point. Computer-based questionnaires were completed in person at the baseline assessment, and participants were given the option to complete questionnaires in-person at their postintervention or follow-up assessments or via a web-based Health Insurance Portability and Accountability Act-compliant survey platform prior to their assessments to minimize participant burden and increase retention.
Feasibility and acceptability
To assess feasibility and acceptability of the HH intervention, we measured recruitment and retention rates, intervention adherence, and satisfaction with the intervention. A priori feasibility objectives were based on our initial pilot study and collective experience [23]: 50 eligible participants consent and enroll in the study, ≥80% of enrolled participants complete the postintervention and follow-up assessments, and participants attend a minimum of 10 face-to-face MB intervention sessions. Satisfaction was assessed at the 6 week follow-up assessment using a self-report survey, which asked participants to report their satisfaction with the overall study, individual intervention components, intervention logistics (e.g., location, duration, frequency, and length of the study), and the likelihood that they would recommend HH to family and friends.
Psychosocial distress
Perceived stress, depressive symptoms, anxiety, and positive and negative affect were assessed at all time points. Perceived stress was assessed using a modified 10-item Perceived Stress Scale (PSS-10) [29,30], and scores range from 0 to 36. The 20-item Center for Epidemiological Studies Depression Scale (CES-D) was used to measure depressive symptoms [31], and scores range from 0 to 60. The 21-item Beck Anxiety Inventory (BAI) was used to measure cognitive and physiological symptoms of anxiety [32], and scores range from 0 to 63. Lastly, the 20-item Positive and Negative Affect Scale (PANAS) was used to assess positive and negative affect [33], and scores range from 10 to 50 on each scale. Higher scores on the PSS-10, CES-D, and BAI indicate greater perceived stress, greater depressive symptomology, and greater anxiety, respectively, and higher scores on the PANAS indicate higher levels of positive affect and lower scores indicate lower levels of negative affect. Cronbach’s alphas were .84 for the PSS-10, .89 for the CES-D, .90 for the BAI, .93 for positive affect, and .88 for negative affect in this sample.
Health-related quality of life
The 36-item short-form (SF-36) was used to measure health-related quality of life [34]. The SF-36 measures eight components of health status: physical functioning, role limitations due to physical health problems, role limitations due to emotional health problems, energy/fatigue, emotional well-being, social functioning, pain, and general health. Scores range from 0 to 100, with higher scores indicating better health status. Cronbach’s alpha for each of the subscales ranged from .71 to .86 in this sample.
Data analysis
The primary outcomes of this study were feasibility and acceptability of the HH intervention, and secondary outcomes included changes in psychosocial distress and health-related quality of life from baseline (T1) to postintervention (T2) and baseline (T1) to 6 week follow-up (T3). To assess feasibility and acceptability, recruitment and retention, intervention adherence, and program satisfaction were calculated. Baseline comparisons between non-Hispanic White or Other and African-American or Black demographic characteristics were performed using chi-square, Fisher’s exact tests, and independent samples t-tests. Paired samples t-tests were used to test for statistically significant changes in psychosocial distress and health-related quality of life from baseline to postintervention and from baseline to 6 week follow-up. All statistical analyses were conducted in SPSS 25.0 (IBM SPSS Statistics, Armonk, NY), and effects were tested using a nonparametric bootstrapping procedure using 5,000 resamples from the data set. Statistical significance was inferred at p < .05, and the effect was considered significant if the 95% confidence interval (CI) of the effect did not include zero.
Results
Feasibility and acceptability
Recruitment and retention
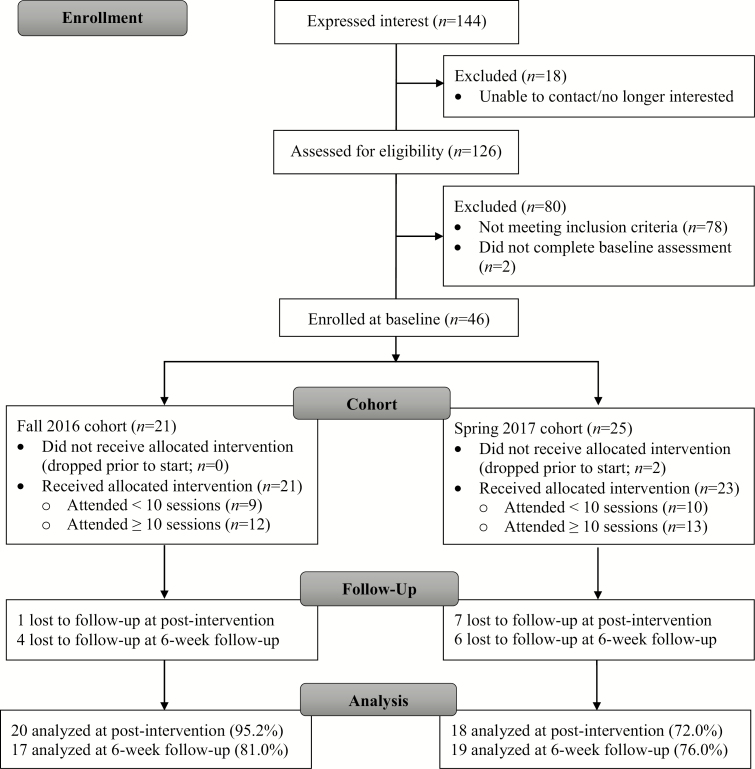
We recruited 46 eligible participants between June 2016 and January 2017, as shown in Fig. 1. Of those, 38 (82.6%) participants completed their postintervention assessment, and 36 (78.3%) returned to complete their 6 week follow-up assessment. Demographic characteristics of participants at baseline are presented in Table 1. Participant age ranged from 18.5 to 83.7 years (mean [M] = 49.1 years, standard deviation [SD] = 14.0). BMI ranged from 24.1 to 44.4 kg/m2 (M = 32.1 kg/m2, SD = 5.8), and most participants were classified as obese (n = 29, 63.0%) or overweight (n = 15, 32.6%). Most participants were women (84.8%), had obtained a bachelor’s degree or higher (65.2%), and reported an annual household income of at least $40,000 (74.4%). There were no statistically significant differences in baseline demographic characteristics, psychosocial distress, or health-related quality-of-life scores by race/ethnicity, with the exception of positive affect (M = 30.2 in non-Hispanic White or Other vs. 36.1 in African American or Black, t = −2.310, p = .026), and there were no statistically significant differences in demographic characteristics between those who completed the postintervention assessment and those who dropped out of the study, with the exception of BMI (M = 31.5 kg/m2 in completers vs. 38.0 kg/m2 in noncompleters, t = 3.200, p = .003).
Fig. 1.
Flow of study participants.
Table 1.
Demographic characteristics of Harmony & Health participants by race/ethnicity
| Non-Hispanic White or Other (N = 25) | African American or Black (N = 21) | Total (N = 46) | p | |
|---|---|---|---|---|
| Age | 49.5 ± 12.8 | 48.6 ± 15.7 | 49.1 ± 14.0 | .818 |
| BMI (kg/m2) | 33.0 ± 6.3 | 32.1 ± 5.2 | 32.6 ± 5.8 | .578 |
| Gender | .601* | |||
| Female | 21 (84.0) | 18 (85.7) | 39 (84.8) | |
| Male | 7 (15.2) | |||
| Education | .190 | |||
| <Bachelor degree | 11 (44.0) | 5 (23.8) | 16 (34.8) | |
| Bachelor degree | 9 (36.0) | 7 (33.3) | 16 (34.8) | |
| >Bachelor degree | 5 (20.0) | 9 (42.9) | 14 (30.4) | |
| Annual income | .329 | |||
| <$40,000 | 8 (33.3) | 3 (15.8) | 11 (25.6) | |
| $40,000–79,999 | 7 (29.2) | 9 (20.9) | 16 (37.2) | |
| ≥$80,000 | 9 (37.5) | 7 (16.3) | 16 (37.2) | |
| Employment status | .966 | |||
| Not working | 18 (72.0) | 15 (71.4) | 13 (28.2) | |
| Working part- or full-time | 7 (28.0) | 6 (28.6) | 33 (71.7) | |
| Marital status | .189 | |||
| Not married | 9 (40.9) | 10 (62.5) | 19 (50.0) | |
| Married/living with a partner | 13 (59.1) | 6 (37.5) | 19 (50.0) | |
| Perceived stress | .896 | |||
| Low (PSS <14) | 14 (56.0) | 13 (61.9) | 27 (58.7) | |
| Moderate (PSS 14–26) | 10 (40.0) | 7 (33.3) | 17 (37.0) | |
| High (PSS ≥27) | 1 (4.0) | 1 (4.8) | 2 (4.3) | |
| Depressive symptoms | .502* | |||
| Low (CES-D <16) | 17 (68.0) | 17 (81.0) | 34 (73.9) | |
| Elevated (CES-D ≥16) | 8 (32.0) | 4 (19.0) | 12 (26.1) | |
| General health status | .431 | |||
| Excellent | 2 (8.0) | 1 (4.8) | 3 | |
| Very good | 8 (32.0) | 3 (14.3) | 11 | |
| Good | 11 (44.0) | 9 (42.9) | 20 | |
| Fair | 3 (12.0) | 6 (28.5) | 9 | |
| Poor | 1 (4.0) | 2 (9.5) | 3 |
Data are presented as the mean ± standard deviation for continuous variables (e.g., age and body mass index [BMI]) and frequency (%) for categorical variables. Demographic characteristics were compared using independent samples t-tests and chi-square (or Fisher’s exact, marked by *) tests where appropriate.
Intervention adherence
Most (n = 25, 71.4%) participants attended at least 10 of the 15 face-to-face MB intervention sessions. Of those who attended at least 10 sessions, 9 (36.0%) attended 10–12 sessions, 10 attended 13–14 sessions (40.0%), and 6 (24.0%) attended all 15 sessions. Two participants (5.0%) dropped out prior to the start of the intervention and did not attend any MB intervention sessions.
Satisfaction
All participants completed a satisfaction survey at the 6 week follow-up assessment, and nearly all participants (97.2%) were satisfied (28.6%), very satisfied (45.7%), or extremely satisfied (22.9%) with the HH study. Participants reported satisfaction with the stretching (94.1%) and guided relaxation (94.1%) elements of the MB intervention, and 88.7% were satisfied with the community-based church location where sessions were held. Most participants reported the 45 min duration (88.6%) and twice weekly frequency (74.3%) of intervention sessions were just right. Some participants felt sessions were too short (8.6%) and would prefer to meet more frequently than twice a week (25.7%). Participants felt the 8 week study period was just the right amount of time (48.6%) or too short (42.9%). Most (77.2%) found the intervention sessions to be useful in motivating them to adopt a healthy lifestyle, and 74.3% of participants reported that they learned new information from HH on how to manage their stress. Nearly all participants reported that they looked forward to attending HH sessions (42.9% agreed and 51.4% strongly agreed) and would recommend the study to their friends and family (40.0% agreed and 57.1% strongly agreed).
Changes in psychosocial distress and health-related quality of life
Psychosocial distress and health-related quality-of-life Ms, SDs, and mean differences from baseline to postintervention (Δ T2 − T1) and baseline to follow-up (Δ T3 − T1) are shown in Table 2. Participants reported statistically significant decreases in perceived stress, depressive symptoms, and negative affect and improvements in energy/fatigue, emotional well-being, and social functioning. However, improvements in psychosocial distress and health-related quality of life were not sustained at 6 week follow-up.
Table 2.
Changes in psychosocial distress and health-related quality of life (mean ± standard deviation) from baseline (T1) to postintervention (T2) and baseline to follow-up (T3)
| T1 | T2 | T3 | Baseline to postintervention | Baseline to follow-up | |||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | (N = 46) | (N = 38) | (N = 36) | Δ a | 95% CI | Cohen’s d | Δ a | 95% CI | Cohen’s d |
| Psychosocial distress | |||||||||
| Perceived stress | 12.2 ± 6.7 | 10.0 ± 6.3 | 11.4 ± 7.2 | −1.5 | −2.8, −0.3 | .39 | −0.8 | −2.5, 1.0 | .14 |
| Depressive symptoms | 10.8 ± 8.8 | 7.7 ± 7.9 | 9.9 ± 10.8 | −2.2 | −3.5, −1.1 | .58 | −0.8 | −3.6, 1.9 | .10 |
| Anxiety | 7.7 ± 7.8 | 6.3 ± 6.6 | 7.5 ± 7.8 | 0.2 | −1.5, 2.0 | .04 | 1.4 | −0.7, 3.5 | .21 |
| Positive affect | 32.9 ± 9.0 | 33.6 ± 9.8 | 34.1 ± 8.8 | 0.6 | −1.2, 2.3 | .11 | 0.5 | −1.1, 2.1 | .10 |
| Negative affect | 16.7 ± 6.2 | 14.1 ± 5.4 | 15.9 ± 6.1 | −1.4 | −2.4, −0.3 | .40 | −0.2 | −1.6, 1.2 | .04 |
| Health-related quality of life | |||||||||
| Physical functioning | 84.4 ± 16.7 | 87.6 ± 13.1 | 83.7 ± 17.0 | 3.5 | −0.7, 8.1 | .26 | 0.0 | −3.9, 3.6 | .00 |
| Role limitations—physical | 83.7 ± 30.4 | 87.2 ± 29.8 | 85.4 ± 30.1 | 2.8 | −8.3, 13.2 | .08 | 2.1 | −7.1, 11.4 | .07 |
| Role limitations—emotional | 69.6 ± 35.7 | 77.5 ± 37.7 | 75.5 ± 39.7 | 7.4 | −4.6, 19.4 | .20 | 6.2 | −7.1, 20.0 | .15 |
| Energy/fatigue | 52.3 ± 19.8 | 58.0 ± 19.4 | 54.6 ± 20.5 | 3.9 | 0.3, 7.6 | .33 | 1.8 | −3.1, 6.6 | .12 |
| Emotional well-being | 73.7 ± 15.0 | 80.4 ± 13.1 | 77.2 ± 19.0 | 5.7 | 2.6, 8.8 | .59 | 2.9 | −1.1, 7.0 | .23 |
| Social functioning | 79.6 ± 23.6 | 86.8 ± 18.4 | 83.7 ± 22.7 | 5.9 | 1.7, 10.1 | .45 | 3.9 | −1.8, 9.6 | .23 |
| Pain | 80.5 ± 17.6 | 77.4 ± 19.9 | 77.3 ± 21.9 | −2.4 | −7.5, 2.6 | .15 | −3.6 | −8.1, 0.9 | .27 |
| General health | 66.5 ± 17.8 | 68.9 ± 18.9 | 67.2 ± 18.1 | 0.1 | −4.6, 5.0 | .01 | 0.0 | −4.3, 4.1 | .00 |
CI confidence interval.
aSample size for mean differences (Δ) varies by time point and is calculated using participants with complete data at T1 and T2 or T1 and T3 only.
Discussion
HH was adapted for rural adults and was implemented in a rural church-based setting. Findings support the feasibility and acceptability of the culturally adapted MB intervention, incorporating yoga-based physical activity with spirituality and religious practice, among rural adults. We extend previous findings to show preliminary efficacy of HH to reduce psychosocial distress and improve dimensions of health-related quality of life in rural adults who are at greater risk of mental health disorders and may be less likely to seek traditional treatment [9–11]. Coupled with previous findings [23], results suggest that HH is feasible, acceptable, and efficacious for improving psychosocial health and well-being in underserved populations in the short-term, but further work is needed to sustain intervention effects.
Similar to our previous work in urban African-American churchgoers [23], our target population expressed strong interest in the HH study, and 87.5% of those interested in the study were screened for eligibility. However, only 36.5% of those screened were eligible to participate and enrolled in the study. Common reasons for ineligibility included self-reporting being sufficiently active (≥120 min per week), having a BMI ≥45.0 kg/m2, or unable to get their physician’s clearance to participate. This enrollment rate is similar to a previous study that enrolled rural breast cancer survivors in a lifestyle intervention and used multiple recruitment methods [35]. Despite using strategies to enhance recruitment in rural adults [36], such as building trust with church partners and community stakeholders and minimizing participant burden via the utilization of a community-based location and web-based surveys, we fell short of our recruitment goal of 50 rural adults. This may be due to the fact that fewer eligible participants live in rural areas [37] and supports the need to lower the threshold for participant involvement in rural communities [38].
Despite moderate recruitment success initially, we successfully retained 82.6% of participants at postintervention and met retention goals. More participants in the spring cohort were lost to follow-up at postintervention and 6 week follow-up due to spring/summer vacations and schedule conflicts. However, participants reported high satisfaction with HH, including the stretching and guided relaxation intervention components, the format and duration of the intervention, and the community-based church location. Findings from this study further support the use of community-based settings, such as churches, to deliver physical and mental health programming aimed at reducing health disparities and promoting health equity in rural populations [22].
Although the primary aim of this study was to assess feasibility and acceptability, our results extend findings previously reported [23] and demonstrate the preliminary efficacy of HH for reducing psychosocial distress and improving dimensions of health-related quality of life in rural adults. Namely, participants reported modest reductions in perceived stress, depressive symptomology, and negative affect along with improvements in energy, emotional well-being, and social functioning over the 8 week intervention period. These findings are similar to trends seen in urban African-American adults who participated in HH [23]. However, improvements in distress and quality of life were not maintained at the 6 week follow-up assessment. Thus, additional research is needed to increase the maintenance of intervention effects and to explore opportunities to increase the sustainability of physical and mental health programs, similar to HH, within rural faith-based settings as a means to reduce barriers to access and availability and stigma related to mental health disorders and treatment [10,11,16,22].
Strengths of this study include the use of HH, a culturally adapted MB intervention that intertwined spirituality with MB practices and physical activity to reduce psychosocial distress in rural churchgoers, the innovative implementation of the study in a rural faith-based setting, and the inclusion of a racially/ethnically diverse rural sample. However, there are several limitations that must be considered when interpreting findings from this study. First, this was a feasibility study with a small sample size. Thus, we employed a pre–post study design and were not statistically powered to detect statistically significant and clinical effects of the intervention. However, results offer preliminary evidence that HH may reduce psychosocial distress and improve quality of life in rural adults. Next steps include confirming efficacy by conducting a randomized trial and later testing the effectiveness of HH in a larger, statistically powered randomized controlled trial in faith-based settings. Second, this study used survey-based assessments of stress, depressive symptoms, anxiety, affect, and quality of life, which are subject to self-reporting and social desirability biases, and participants reported low psychosocial distress at baseline, which may limit our ability to detect an intervention effect. Additionally, given daily fluctuations in affective states related to mental health and well-being [39], the simple pre–post measurement of psychosocial distress and quality of life may reduce ecologic validity of findings. Future studies could assess physiological patterns of stress from wearables and use intensive longitudinal designs, such as ecological momentary assessment or daily diaries [39–41]. Third, we saw statistically significant differences in BMI at baseline between completers and noncompleters. Although this is in line with previous studies [42,43], it may contribute to selection bias and skew findings. Additional work is needed to explore adaptations needed to recruit and retain adults with obesity who are at higher risk of disease. Finally, this study included predominantly female, non-Hispanic white and African-American adults with moderate-high socioeconomic status who were relatively psychologically healthy and motivated to engage in a relaxation study. Thus, findings may not be generalizable to rural adults from other racial/ethnic groups who face greater physical and mental health disparities [44,45]. Additional formative research is needed to inform community-based intervention strategies to engage rural men and adults from other racial/ethnic groups that align with cultural values related to rurality and race/ethnicity.
Translational next steps
HH effectively engaged rural adults within a community-based setting to participate in a culturally adapted MB intervention that intertwined spirituality with yoga-based light-intensity physical activity. Results demonstrate preliminary efficacy for improving mental health among rural adults, including reducing psychosocial distress and improving health-related quality of life. However, improvements in psychosocial distress and quality of life were not sustained at follow-up. Further work is needed to explore the mechanism through which HH impacts mental health in rural adults and to test strategies that promote maintenance of effects. Immediate next steps include confirming the efficacy of HH for improving mental health in a randomized controlled trial. Additionally, implementation strategies to retain adults with obesity and sustain effects of community-based interventions must be tested to facilitate the maintenance of effects. One possible strategy is to use lay health workers or community leaders to lead recruitment and retention efforts and lead MB sessions in diverse community settings, thereby extending services and care in rural settings and reducing rural health disparities.
Acknowledgements:
The authors wish to thank Ms. Tracey Jackson and Pastor Harold McKenzie for their support of and assistance with the Harmony & Health study. We would also like to thank Dr. Brandi Rollins, Ms. Grace Emmerling, Ms. Hannah T. Jones, and Ms. Cassandra Kennedy for their assistance with the Harmony & Health study at The Pennsylvania State University.
Funding:
This study was funded by an American Cancer Society Institutional Research Grant (124171-IRG-13-043-01, PI: Mama) from the Penn State Cancer Institute. S.K.M. is supported by a career development award from the National Cancer Institute (K07 CA222335, PI: Mama), and E.J.L. is partially supported by a grant from the National Center for Advancing Translational Sciences, National Institutes of Health (UL1 TR002014; PI: Sinoway).
Compliance with Ethical Standards
Conflicts of Interest: Scherezade K. Mama, Nishat Bhuiyan, Melissa J. Bopp, Lorna H. McNeill, Eugene J. Lengerich, and Joshua M. Smyth declare that they have no conflicts of interest.
Authors’ Contributions: S.K.M. conceived the study, collected data, completed data analyses, and led data interpretation and manuscript writing; N.B. assisted with data collection and manuscript preparation; M.J.B., L.H.M., E.J.L., and J.M.S. contributed toward study design, data interpretation, and critical review of the manuscript.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All study procedures and materials were reviewed and approved by the Institutional Review Board at The Pennsylvania State University (protocol ID: STUDY00004310). This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. O’Connor A, Wellenius G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public Health. 2012;126(10):813–820. [DOI] [PubMed] [Google Scholar]
- 2. Matthews KA, Croft JB, Liu Y, et al. Health-related behaviors by Urban-Rural County Classification—United States, 2013. MMWR Surveill Summ. 2017;66(5):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Long AS, Hanlon AL, Pellegrin KL. Socioeconomic variables explain rural disparities in US mortality rates: Implications for rural health research and policy. SSM Popul Health. 2018;6:72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moy E, Garcia MC, Bastian B, et al. Leading xauses of death in nonmetropolitan and metropolitan areas—United States, 1999-2014. MMWR Surveill Summ. 2017;66(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bolin JN, Bellamy GR, Ferdinand AO, et al. Rural healthy people 2020: new decade, same challenges. J Rural Health. 2015;31(3):326–333. [DOI] [PubMed] [Google Scholar]
- 6. Douthit N, Kiv S, Dwolatzky T, et al. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. [DOI] [PubMed] [Google Scholar]
- 7. Davis MM, Spurlock M, Dulacki K, et al. Disparities in alcohol, drug use, and mental health condition prevalence and access to care in rural, isolated, and reservation areas: Findings from the south dakota health survey. J Rural Health. 2016;32(3):287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):629–640. [DOI] [PubMed] [Google Scholar]
- 9. Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Barriers to mental health treatment in rural older adults. Am J Geriatr Psychiatry. 2015;23(11):1172–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Snell-Rood C, Hauenstein E, Leukefeld C, et al. Mental health treatment seeking patterns and preferences of Appalachian women with depression. Am J Orthopsychiatry. 2017;87(3):233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haynes TF, Cheney AM, Sullivan JG, et al. Addressing mental health needs: Perspectives of African Americans living in the rural south. Psychiatr Serv. 2017;68(6):573–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cramer H, Lauche R, Langhorst J, et al. Yoga for depression: A systematic review and meta-analysis. Depress Anxiety. 2013;30(11):1068–1083. [DOI] [PubMed] [Google Scholar]
- 13. Duan-Porter W, Coeytaux RR, McDuffie JR, et al. Evidence map of yoga for depression, anxiety, and posttraumatic stress disorder. J Phys Act Health. 2016;13(3):281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li AW, Goldsmith CA. The effects of yoga on anxiety and stress. Altern Med Rev. 2012;17(1):21–35. [PubMed] [Google Scholar]
- 15. Desveaux L, Lee A, Goldstein R, et al. Yoga in the management of chronic disease: a systematic review and meta-analysis. Med Care. 2015;53(7):653–661. [DOI] [PubMed] [Google Scholar]
- 16. Stewart H, Jameson JP, Curtin L. The relationship between stigma and self-reported willingness to use mental health services among rural and urban older adults. Psychol Serv. 2015;12(2):141–148. [DOI] [PubMed] [Google Scholar]
- 17. Hamrick I, Mross P, Christopher N, et al. Yoga’s effect on falls in rural, older adults. Complement Ther Med. 2017;35:57–63. [DOI] [PubMed] [Google Scholar]
- 18. Smith PD, Mross P, Christopher N. Development of a falls reduction yoga program for older adults—A pilot study. Complement Ther Med. 2017;31:118–126. [DOI] [PubMed] [Google Scholar]
- 19. Sullivan M, Leach M, Snow J, et al. The North American yoga therapy workforce survey. Complement Ther Med. 2017;31:39–48. [DOI] [PubMed] [Google Scholar]
- 20. Middleton KR, Magaña López M, Haaz Moonaz S, et al. A qualitative approach exploring the acceptability of yoga for minorities living with arthritis: “Where are the people who look like me?”. Complement Ther Med. 2017;31:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Oldendick R, Coker AL, Wieland D, et al. Population-based survey of complementary and alternative medicine usage, patient satisfaction, and physician involvement. South Carolina complementary medicine program baseline research team. South Med J. 2000;93(4):375–381. [PubMed] [Google Scholar]
- 22. Schoenberg NE. Enhancing the role of faith-based organizations to improve health: A commentary. Transl Behav Med. 2017;7(3):529–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mama SK, Bhuiyan N, Chaoul A, et al. Feasibility and acceptability of a faith-based mind-body intervention among African American adults. Transl Behav Med. 2018;XX:XX–XX. doi:10.1093/tbm/iby114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Health Resources & Services Administration. Medically underserved areas and populations (MUA/Ps) 2016. Available at https://bhw.hrsa.gov/shortage-designation/muap. Accessibility verified February 17, 2019.
- 25. The Center for Rural Pennsylvania. Demographics—rural urban definitions 2014. Available at http://www.rural.palegislature.us/demographics_rural_urban.html. Accessibility verified February 17, 2019.
- 26. Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can J Sport Sci. 1992;17(4):338–345. [PubMed] [Google Scholar]
- 27. Warburton DE, Gledhill N, Jamnik VK, et al. Evidence-based risk assessment and recommendations for physical activity clearance: consensus document 2011. Appl Physiol Nutr Metab. 2011;36 (Suppl 1):S266–S298. [DOI] [PubMed] [Google Scholar]
- 28. Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47(11):2473–2479. [DOI] [PubMed] [Google Scholar]
- 29. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 30. Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, eds. The Social Psychology of Health. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 31. Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 32. Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. [DOI] [PubMed] [Google Scholar]
- 33. Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. [DOI] [PubMed] [Google Scholar]
- 34. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 35. Befort CA, Bennett L, Christifano D, et al. Effective recruitment of rural breast cancer survivors into a lifestyle intervention. Psychooncology. 2015;24(4):487–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Anuruang S, Davidson PM, Jackson D, et al. Strategies to enhance recruitment of rural-dwelling older people into community-based trials. Nurse Res. 2015;23(1):40–43. [DOI] [PubMed] [Google Scholar]
- 37. Bergeron CD, Foster C, Friedman DB, et al. Clinical trial recruitment in rural South Carolina: A comparison of investigators’ perceptions and potential participant eligibility. Rural Remote Health. 2013;13(4):2567. [PubMed] [Google Scholar]
- 38. Miyamoto S, Henderson S, Young H, et al. Recruiting rural participants for a telehealth intervention on diabetes self-management. J Rural Health. 2013;29(1):69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Scott SB, Sliwinski MJ, Zawadzki M, et al. A coordinated analysis of variance in affect in daily life. Assessment. 2018; doi: 10.1177/1073191118799460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Smets E, Velazquez ER, Schiavone G, et al. Large-scale wearable data reveal digital phenotypes for daily-life stress detection. npj Digital Med. 2018;1(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smets E, Schiavone G, Velazquez ER, et al. Comparing task-induced psychophysiological responses between persons with stress-related complaints and healthy controls: A methodological pilot study. Health Sci Rep. 2018;1(8):e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bayley A, Stahl D, Ashworth M, et al. Response bias to a randomised controlled trial of a lifestyle intervention in people at high risk of cardiovascular disease: A cross-sectional analysis. BMC Public Health. 2018;18(1):1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Craike M, Wiesner G, Hilland TA, et al. Interventions to improve physical activity among socioeconomically disadvantaged groups: An umbrella review. Int J Behav Nutr Phys Act. 2018;15(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hall JE, Moonesinghe R, Bouye K, et al. Racial/ethnic disparities in mortality: contributions and variations by rurality in the United States, 2012–2015. Int J Environ Res Public Health. 2019;16(3):436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. James CV, Moonesinghe R, Wilson-Frederick SM, et al. Racial/ethnic health disparities among rural adults—United States, 2012-2015. MMWR Surveill Summ. 2017;66(23):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]