Abstract
Psychosocial eHealth intervention programs for cancer survivors are still in their infancy, with inconsistent findings so far in the scientific literature. The aim of this study was to explore system use, usefulness, ease of use, and preliminary effects of Stress Proffen, an app-based cognitive-behavioral stress management intervention for patients with cancer. A feasibility pilot project tested the intervention with cancer survivors (N = 25). The intervention contained (a) one face-to-face introduction session, (b) 10 app-based modules with stress management educational material and exercises, and (c) one follow-up phone call. Post-intervention interviews were conducted and user log-data were extracted. Outcome measures—Perceived Stress Scale (PSS), Anxiety and Depression (Hospital Anxiety and Depression Scale [HADS]), Health-Related Quality of Life (HRQoL; SF-36), and Self-Regulatory Fatigue (SRF-18)—were completed at baseline and post-intervention. Participants were primarily women (84%), age 34–71 (mean 48) and represented a variety of cancer diagnoses (majority breast cancer: 40%). Twenty-two participants completed all (pre–post) questionnaires. Sixteen participants (67%) completed at least 7 of 10 modules within the 8-week study period. Post-intervention interviews described StressProffen as providing a new, appreciated, and easily accessible stress management tool for the cancer survivors. Dependent/paired t-tests showed significant pre–post intervention effects with significant decrease in stress (p = .008), anxiety (p = .019), and self-regulatory fatigue (p = .025), and improved HRQoL (Role Physical, General Health, Vitality, and Role Emotional, all p’s <.01). App-based stress management interventions such as StressProffen can provide appreciated support for cancer survivors, should be easy to use, can provide significant stress reduction, and improve emotional well-being. Further testing in a randomized controlled trial is warranted and is in progress.
Clinicaltrials.gov: NCT0293961.
Keywords: Stress management, Cancer, eHealth, mHealth, Psycho-oncology, User-centered design
An app-based stress-management program for patients with cancer was found to be easy to use and could provide significant stress reduction and improved emotional well-being.
Implications
Practice: Findings suggest that it is feasible to deliver an app-based stress management intervention for cancer survivors, and that it can be a highly appreciated tool for stress management for the survivors.
Policy: If found to be effective, an app-based stress management intervention can offer cancer survivors stress management techniques to be used without concern for challenges with face-to-face visits or geographical limitations.
Research: The current study provides insight into a feasibility pilot test of an app-based stress management intervention as well as preliminary intervention effects.
BACKGROUND
Globally, cancer continues to be a leading cause of death, with nearly every family worldwide touched by cancer at some point [1]. Despite improved survival rates in recent years, cancer diagnosis and ensuing treatment still carry significant physical and psychosocial challenges, including fatigue, discomfort, stress, distress, anxiety, and depression [2–4]. Increased survival is accompanied by long-term physical and psychological health challenges and many survivors struggle to cope long term [5]. Capacity to self-regulate may also be adversely affected [6, 7]. With numerous domains of function influenced, it is not surprising that quality of life (QoL) is often negatively impacted [8–10].
A number of clinical trials have shown psychosocial interventions to support well-being and adaptive coping in the face of cancer, including improved QoL and reduced stress, distress, anxiety, and depression [8,11–17]. Recent findings also suggest the potential for long-term positive effects from structured interventions for coping with cancer [18].
Unfortunately, in-person individual or group psychosocial interventions are not always an option for patients with cancer. Barriers include lack of services, lack of insurance coverage, geographical distance, or patients do not feel able or comfortable participating in face-to-face settings [16]. Cancer survivors do describe having numerous unmet needs, however, including needs for rehabilitation services, psychological counseling, and supportive group sessions [19].
Telephone-based interventions represent one way of getting around some of the challenges with face-to-face interventions. However, a systematic review examining efficacy of peer-reviewed telephone interventions in randomized controlled trials (RCTs) showed mixed results [20]. Methodological concerns were identified, positive effects on psychosocial outcomes were lacking robustness across multiple end-points, and studies reporting significant effects had no clear commonalities [20]. Also, even without required travel time, telephone interventions still require therapist time, insurance coverage, and fixed appointment times, meaning limited flexibility and availability for the cancer survivor.
If face-to-face interventions are not available, too challenging to attend or engage in for some cancer survivors, and if telephone interventions have uncertain effects, availability and flexibility, innovative new solutions are needed. eHealth solutions may provide such innovative options and could have the potential to address unmet needs, support psychological well-being, strengthen coping skills, and increase flexibility and availability for cancer survivors.
Psychosocial eHealth intervention programs for cancer survivors are still in their infancy, with inconsistent findings so far in the scientific literature. A systematic literature review examining online interventions for cancer patients found positive associations with QoL and related psychosocial factors, but inconclusive overall effect and limited duration of benefit [21]. On the other hand, a meta-review examining the effects of eHealth for patients and caregivers found positive findings in terms of perceived support and information competence, but inconclusive results related to psychological well-being and QoL [22]. More recent research has, however, shown improved physical activity and QoL for breast cancer survivors through use of an online portal [23], and improved QoL and reduced distress for newly diagnosed patients with cancer following use of a structured online stress management program guided by psychologists [24]. A systematic review and meta-analysis examining eHealth/mHealth interventions concluded that guided intervention may have better effect compared with self-guided interventions [25]. A pilot study testing a mobile application (app) for managing post-traumatic stress disorder (PTSD) symptoms in cancer survivors also indicated reduction in PTSD and distress symptoms following use of the app [26]. Given positive yet continued mixed findings, researchers have called for an increase in focus on evidence-based eHealth interventions, involvement from healthcare providers when developing technology-based psychosocial interventions, and outcome assessment to gauge intervention impact [21, 27].
In response to these research recommendations, this research team has developed a cognitive-behavioral stress management eHealth intervention (called StressProffen) for patients diagnosed with cancer [28]. The development of StressProffen combines evidence-based psychosocial intervention concepts for cancer survivors [8, 11, 13, 16, 29, 30], with continuous user involvement from cancer survivors, healthcare personnel, and eHealth experts [28]. Design, development, and usability testing of the app-based StressProffen intervention program is reported elsewhere [28].
In order to successfully evaluate the effectiveness of complex interventions, the Medical Research Council recommends initial testing and refining of the intervention to ensure its feasibility [31]. The current feasibility study aimed to pilot-test system use, usefulness, ease of use, and preliminary effects of the StressProffen intervention to enable optimization and preparation for a larger RCT. Feasibility conceptualization was guided by Bowen et al. [32], exploring the following areas: Acceptability: To what extent is StressProffen judged as suitable, satisfying, or attractive to program recipients? Demand: Exploration of the actual use of the StressProffen intervention and it modules. Adaption: To what extent does an app-based stress management program perform as described by the participants in interviews? Limited efficacy testing: Does the intervention show promise of being successful with the intended population? [32].
It was hypothesized that the program would have no technical challenges and that pilot participants would evaluate the stress management program as useful and easy to use. A general, secondary hypothesis was that pilot participants would experience stable (i.e., not worsened) or potentially improved psychosocial scores in terms of stress, anxiety, depression, health-related quality of life, and self-regulatory fatigue.
METHODS
Participants and recruitment
Participants were patients diagnosed with cancer recruited at a major medical center in Northern Europe as well as through social media. Twenty-five participants with a range of cancer diagnoses were included. Eligibility criteria included the following: (a) currently or recently in cancer treatment (maximum 1 year since hospital treatment completion); (b) ≥18 years of age; (c) able to speak, read, and understand Norwegian; (d) access to smartphone or tablet; and (e) able to attend one face-to-face introduction session at the major medical center. These eligibility criteria were chosen to enhance the likelihood of effective testing in the most relevant settings (e.g., recent experiences from cancer diagnosis and treatment, and access to smartphone/tablet).
Study procedure
This study was approved by the Regional Committee for Medical and Health Research Ethics (2016/14369) and the Hospital Privacy Protection Committee (2015/10204). All participants provided written informed consent. Questionnaire data and log-data were collected electronically through a secure server using an encrypted connection.
Evaluation included (a) baseline questionnaires, (b) one face-to-face introduction session, (c) 10 app-based thematic modules, (d) one follow-up phone call 2–3 weeks after the introduction session, (e) post-intervention questionnaires (immediately post-intervention completion or maximum 8 weeks after the introduction session), and (f) voluntary face-to-face or telephone post-intervention interviews. Program completers were defined as participants completing at least 70% (7 of 10) of the sessions [30].
Description of the stress management intervention StressProffen
StressProffen was developed utilizing user-centered design methods in close collaboration between scientists, cancer survivors, psychosocial-oncology healthcare providers, and eHealth experts, and is built on evidence-based factors from well-known cognitive-behavioral stress management strategies [8, 11, 13, 15, 16]. Please see Børøsund et al. [28] for more details on StressProffen design, development, and usability testing.
The introductory session was conducted as a one-time face-to-face in-person structured individual or group session led by healthcare study personnel trained by a clinical health psychologist. The session introduced participants to the stress management concept, provided help downloading the StressProffen app from App store or Google play, and gave instructions in how to use the program.
The thematic modules 1–10 delivered through StressProffen included the following themes: (1) What is stress; (2) Stress, QoL, and planning; (3) Thoughts, feelings, and self-care; (4) Mindfulness, rational thought-replacement, and guided imagery; (5) Stress and coping; (6) Social support, humor, and meditation; (7) Anger management and conflict style awareness; (8) Assertiveness and communication; (9) Health behaviors and setting goals; and (10) Review and summary. A total of 36 different types of exercises (e.g., diaphragmatic breathing, mindfulness, challenging negative thoughts) were incorporated in the modules. Participants could at any point choose between reading or listening. Based on feedback from patients and healthcare providers in the design and development phase, the modules were divided in smaller subsections (from 9 to 14 sections) to avoid overwhelming the patients [28]. Each module would take between 35 and 50 min if completed in one setting without interruption.
To encourage content practice, each thematic module had to be open for 3 days before the next module would open. To provide structure and to allow individualization, the four first modules were sequential, while the order of modules 5–9 could be chosen. Module 10 gave a review and suggestions for “the road ahead” [28]. To motivate for continued use, participants would receive messages such as: “Very good! You have now completed Module 3 on Thoughts, feelings and self-care! Module 4 on Mindfulness, rational thought-replacement and guided imagery will soon be opened for you!” when completing a module. In addition, participants had the option to receive daily reminders from the application and could choose their own timing for receiving this reminder. The reminder was created as brief, positive messages from the application such as: “Make appointments with yourself to do something you enjoy,” “To be mindful is to focus on the here and now,” “Breathe in and out…. and repeat a million times.”
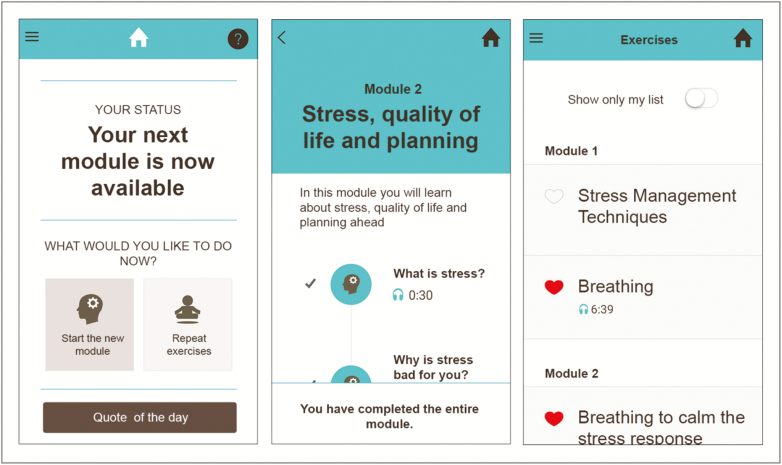
Participants received a follow-up phone call from study staff 2–3 weeks after the introduction session. Program progress was monitored by the research team through app activity. To ensure availability, the program could also be used while the participants were offline. Progress was then automatically uploaded when the participants were online again. Participants could contact the study staff on weekdays for questions through a project phone number. All contact with participants was logged. Emergency issues or non-study-related questions should be addressed to the patient’s own primary care team or the nearest hospital/urgent care treatment unit. Selected StressProffen screenshots are shown in Fig. 1.
Fig. 1.
StressProffen screenshots.
Data collection and outcome measures
Outcome measures were collected prior to the introduction session and immediately post-intervention completion or at maximum 8 weeks post-introductory session if the intervention was not yet completed by then.
Sociodemographic and disease-related measures
A study-specific questionnaire was distributed at baseline (see Table 1).
Table 1.
Baseline demographic and clinical characteristics of cancer survivors included in the app-based stress management intervention (N = 25)
| Characteristics | Cancer survivors (N = 25) | |||
|---|---|---|---|---|
| Median | Range | n | % | |
| Age (years) | 46 | 34–71 | ||
| Months since diagnosis | 18 | 0.5–78 | ||
| Gender | ||||
| Female | 21 | 84 | ||
| Male | 4 | 16 | ||
| Marital status | ||||
| Married/cohabitating | 18 | 84 | ||
| Single/divorced | 7 | 16 | ||
| Education | ||||
| Elementary/high school | 5 | 20 | ||
| University/college ≤4 years | 8 | 32 | ||
| University/college >4 years | 12 | 48 | ||
| Employment status | ||||
| Full-time/part-time work | 8 | 32 | ||
| Sick leave/disability benefits | 14 | 56 | ||
| Retired/other | 3 | 12 | ||
| Diagnosis | ||||
| Breast cancer | 10 | 40 | ||
| Othera (see below) | 15 | 60 | ||
| Metastatic disease | ||||
| Yes | 8 | 32 | ||
| No | 17 | 68 | ||
| Treatment | ||||
| Operation | 18 | 72 | ||
| Chemotherapy | 16 | 64 | ||
| Hormone therapy | 10 | 40 | ||
| Radiation | 9 | 36 | ||
| Immune therapy | 1 | 4 |
aOther includes: cancer of bladder, cervix, ovary, fallopian tube, colon, pancreas, peritoneal, lung, prostate, endometriosis sarcoma, melanoma, chronic myelogenous leukemia, leukemia, and brain tumor.
System use
To explore actual use of the StressProffen intervention and its modules (Demand) [32], system use log-data including details of use and program progress were extracted from user logs stored on a secure research server.
Usefulness and ease of use
To explore Acceptability (i.e., to what extent the intervention is judged as satisfying or attractive to the recipients) of the intervention [32], participants completed a six-item study-specific questionnaire post-intervention. The first three items, inspired by Davis [33], gauged participants’ program perception: (1) The program was easy to use, (2) The exercises were easy to understand, and (3) The program was useful. Response options ranged from 1 – “totally agree” to 5 – “totally disagree.” Based on previous experience with developing eHealth applications in the research group, the next three items were open-ended questions designed to gather as much information as possible related to program usefulness and ease of use: (4) What did you like best? (5) What did you like the least? (6) Suggestions for improvement?
Interviews
Participants were invited to a post-intervention interview to further explore Acceptability of the intervention and to what extent the StressProffen program performed as described (Adaption) [32]. Interviews were conducted by two research team members using a semi-structured interview guide capturing the following areas: (a) experiences using the intervention, (b) features regarded as useful, and (c) suggestions for app improvements. Based on participant preference, interviews were face-to-face or by telephone with 30–60-min duration. All interviews were recorded, reviewed, and analyzed by the first author and three co-authors using content analysis [34]. Topics and impressions were discussed and notes were recorded. Issues considered important by participants, including things they found interesting, easy, challenging, liked, or disliked were recorded.
Psychosocial outcome measures
To explore whether StressProffen shows promise of being successful with the intended population (Limited efficacy testing) [32], gauging preliminary effects, participants completed the following outcome measures:
Perceived stress
The Perceived Stress Scale (PSS-14) is a 14-item scale measuring feelings and thoughts over the last month [35]. It is widely used for measuring the perception of stress, measuring the degree to which situations in one’s life are appraised as stressful. Chronbach’s alpha coefficient at baseline for the current study sample was .88.
Anxiety and depression
Anxiety and depression were measured with the Hospital Anxiety and Depression Scale (HADS) [36], a 14-item measure of anxiety and depression, validated as a unidimensional measure of distress. Chronbach’s alpha coefficient for the current study sample at baseline was .88 for HADS – Anxiety and .80 for HADS – Depression.
Health-Related Quality of Life (HRQoL)
HRQoL was measured with the non-commercial SF-36-item Short-Form Health Survey (RAND-36 version) [37, 38], a 36-item measure of physical, role, emotional, cognitive, and social functions, as well as physical health and general and global health/HRQoL. The RAND-36 is validated and cross-culturally tested in cancer patients. Chronbach’s alpha coefficients at baseline for the current study sample ranged from .76 to .90 on the different subscales at baseline.
Self-regulation
Self-regulation was measured with the Self-Regulatory Fatigue-18 (SRF-18) [39], an 18-item self-report scale gauging capacity to regulate cognitive, emotional, and behavioral components of self-regulation and includes eight items that are phrased positively (e.g., “It’s easy for me to set goals”) and 10 items that are phrased negatively (e.g., “I find it difficult to exercise as much as I should”). Items are scored on a 5-point Likert scale (1 to 5). Higher numbers reflect higher SRF. The SRF-18 has acceptable internal consistency and reliability [39], and the Chronbach’s alpha coefficient at baseline in the current study sample was .88.
Statistical analyses
Statistical analyses were completed using the Statistical Package for the Social Sciences (release 21; SPSS Inc., Chicago, IL). Data on baseline characteristics and usefulness/ease of use are presented as medians and range for continuous variables and as proportions with percentages for categorical variables. Dependent paired t-tests were used to analyze pre–post intervention changes. To explore potential group differences on outcome measures, demographics, and app program progress, a bivariate correlation analysis was conducted. A standard alpha level of .05 was used for all statistical analyses.
RESULTS
Sample description
Participants (N = 25) were median 46 (range: 34–71) years old at inclusion. Cancer diagnosis varied, with breast cancer diagnosis being the largest classification (40%). Time since diagnosis was median 18 months (range: 0.5–78 months). All participants were Caucasian (100%) and mainly female (84%) (see Table 1 for details).
System use
All participants (N = 25) completed baseline questionnaires. One participant was not able to attend the face-to-face introduction group due to disease progression, and 24 participants therefore received the app-based intervention. Sixteen participants completed at least 7 of the 10 modules within the 8-week study period, yielding a 67% intervention completion rate. Thirteen (54%) participants completed all modules and used median 46 (range 27–56) days on completion. The intervention “non-completers” (less than seven modules) on average completed four modules. The follow-up call from the study staff 2–3 weeks after the introductory session appeared to prompt an increase in use. There were no reports of technical problems during the pilot period.
The top three exercises repeated most during the 8 weeks were progressive muscle relaxation (58 repetitions, exercise duration: 8 min and 22 s), autogenic relaxation (48 repetitions, exercise duration: 10 min and 22 s), and guided imagery (25 repetitions, exercise duration: 9 min and 34 s). Exercises that required use of pen and paper were not repeated often (e.g., setting goals = no repetitions).
Usefulness and ease of use
Twenty-two participants (88%) completed the post-intervention questionnaires. The intervention was rated as useful (i.e., “totally agree” or “agree”; 19/22, 87%) and easy to use (21/22, 95%), with easily understandable exercises (100%). Participants reported appreciating easy access, being able to choose between listening and reading, the variation in types of exercises, brief modules, and being able to mark their own favorite areas.
Interview data
Twenty-one participants agreed to be interviewed about their use and experience. Several participants described having obtained a broader understanding of distress and that StressProffen had provided them with many new stress management techniques for everyday use. Some described changes in own behavior, also noted by their support network. One participant stated: “Several people asked whether I had done something to change, saying that I am calmer now… I keep repeating these exercises and I think it’s really good for me.”
The easy accessibility was highly appreciated as the intervention could be used anytime and anywhere without having to involve or “bother” anyone. One participant stated: “I really liked the content and the exercises. Something you can do on your own. I think, no matter your life situation, breathing is good for you. Don’t need a disease to benefit from that. You have a tool in your own pocket. Don’t need to go to a physician or therapist for that, you can use it when it suits you.”
Participants described the face-to-face introduction group and phone call as experiencing “a human contact” behind the app.
When asked for suggestions or advice for StressProffen improvements, participants expressed a need for even easier navigation, for example, being able to find previously completed exercises and information more easily. The 3-day delay before a new module could be opened received mixed feedback. Eleven participants thought this was too long to wait. One woman said: “When you have fatigue, you want to do what you can when you can. It is easy to delay it if you have to wait, you may even forget about the app”. The other 10 liked the 3-day delay, and one participant said: “I think it’s a good thing. I don’t feel the pressure to do it all at once.”
Pre–post intervention results
A statistically significant change from baseline to post-intervention was noted in several of the outcome measures (see Table 2). Participants reported a significant decrease in perceived stress level (p = .008), anxiety (p = .019), and in the anxiety–depression total score (p = .024). There was no significant change in level of depression alone.
Table 2.
Pre–post intervention changes in perceived stress, anxiety, depression, HRQoL, and self-regulation (n = 22)
| Baseline (n = 22) | Post-intervention (n = 22) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Psychosocial outcomes | Mean | SD | Mean | SD | Mean diff. | 95% CI of diff. | SD diff. | d | p |
| Perceived stress (PSS-14) | 25.7 | 7.7 | 21.8 | 7.1 | 4.0 | 1.1–6.8 | 6.4 | 0.62 | .008 |
| Anxiety (HADS-A) | 8.1 | 4.2 | 6.4 | 3.5 | 1.7 | 0.3–3.1 | 3.2 | 0.54 | 019 |
| Depression (HADS-D) | 6.1 | 3.9 | 5.3 | 3.6 | 0.7 | −0.3 to 1.7 | 2.3 | 0.32 | .148 |
| Anxiety and depression (HADS Total) |
14.2 | 7.4 | 11.7 | 6.9 | 2.5 | 0.4–4.6 | 4.7 | 0.52 | .024 |
| HRQoL (SF-36)a | |||||||||
| Physical Functioning | 73.9 | 21.6 | 42.0 | 31.2 | 31.8 | 15.7–48.0 | 36.4 | 0.87 | .001 |
| Role Physical | 29.5 | 39.1 | 80.2 | 22.8 | −50.7 | −69.3 to −32.1 | 42.0 | 1.21 | <.001 |
| Bodily Pain | 59.7 | 25.1 | 39.8 | 39.8 | 19.9 | 2.0–37.8 | 40.4 | 0.49 | .031 |
| General Health | 46.8 | 22.7 | 66.5 | 22.7 | −19.7 | −32.8 to −6.5 | 29.6 | 0.67 | .005 |
| Vitality | 39.3 | 19.5 | 53.9 | 21.8 | −14.5 | −24.0 to −5.1 | 21.3 | 0.68 | .004 |
| Social Functioning | 50.6 | 27.7 | 44.5 | 17.6 | 6.0 | −5.0 to 17.1 | 24.9 | 0.24 | .270 |
| Role Emotional | 34.8 | 37.8 | 65.9 | 25.9 | −31.1 | −50.4 to −11.7 | 43.7 | 0.71 | .003 |
| Mental Health | 64.4 | 17.1 | 75.8 | 37.3 | −11.4 | −25.2 to 2.4 | 31.1 | 0.37 | .101 |
| SRF-18 | 51.6 | 11.2 | 48.1 | 10.4 | 3.6 | 0.5–6.7 | 7.0 | 0.52 | .025 |
CI confidence interval; d, Cohen’s d; HADS Hospital Anxiety and Depression Scale; HRQoL Health-Related Quality of Life; PSS Perceived Stress Scale; SF-36 Short-Form Health Survey; SRF-18 18-item Self-Regulatory Fatigue.
aHigher scores indicate better function.
Results related to HRQoL varied, as changes from baseline to post-intervention indicated statistically significant improvement for the scales Role Physical (problems with work or other daily activities as a result of physical health problems; p < .001), General Health (p = .005), Vitality (energy/fatigue; p = .004), Role Emotion (problems with work or other daily activities as a result of emotional problems; p = .003), and significant worsening for Physical Functioning (p = .001) and Bodily Pain (p = .031).
There was a statistically significant improvement in self-regulatory capacity (i.e., decrease in reported self-regulatory fatigue; p = .025).
Program completion and baseline psychosocial findings
Bivariate correlation analysis indicated that in this sample, being an intervention completer (completed seven or more modules) was associated with lower baseline perceived stress score and higher baseline scores on the HRQoL – General Health subscale. Please see Table 3 for demographics, baseline psychosocial outcome measures, and app progression correlation details.
Table 3.
Correlations of intervention completer status, selected background variables, and baseline psychosocial measures (N = 25)
| Completer status | Age | Gender | Education | Metastasis | Months since diagnosis | PSS | HADS – Anxiety | HADS – Depression | HRQoL – Physical Functioning | HRQoL – Role Physical | HRQoL – Bodily Pain | HRQoL – General Health | HRQoL – Vitality | HRQoL – Social Functioning | HRQoL – Role Emotional | HRQoL – Mental Health | SRF | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention completer status | 1 | |||||||||||||||||
| Age | .27 | 1 | ||||||||||||||||
| Gender | −.13 | .12 | 1 | |||||||||||||||
| Education | .16 | .11 | .12 | 1 | ||||||||||||||
| Metastasis | −.16 | .00 | −.17 | −.08 | 1 | |||||||||||||
| Months since diagnosis | −.00 | −.29 | −.27 | −.21 | −.16 | 1 | ||||||||||||
| Perceived stress (PSS) | −.40* | −.21 | −.08 | −.47* | .07 | .10 | 1 | |||||||||||
| HADS – Anxiety | −.15 | −.10 | .00 | −.44* | .02 | .16 | .76** | 1 | ||||||||||
| HADS – Depression | −.12 | .01 | .05 | −.39 | −.17 | .10 | .54** | .62** | 1 | |||||||||
| HRQoL – Physical Functioning | .02 | −.47* | .23 | .06 | −.02 | −.21 | .10 | .06 | −.09 | 1 | ||||||||
| HRQoL – Role Physical | .05 | −.24 | .02 | .16 | .16 | −.12 | −.23 | −.18 | −.31 | .30 | 1 | |||||||
| HRQoL – Bodily Pain | −.09 | −.08 | .11 | .02 | .24 | −.26 | −.29 | −.39 | −.26 | .14 | .56** | 1 | ||||||
| HRQoL – General Health | .48* | .40* | .09 | .26 | .13 | −.26 | −.43* | −.35 | −.48* | −.01 | .28 | .11 | 1 | |||||
| HRQoL – Vitality | .27 | .14 | .25 | .46* | −.20 | −.22 | −.68** | −.66** | −.57** | .26 | .24 | .20 | .61** | 1 | ||||
| HRQoL – Social Functioning | −.07 | −.24 | .25 | .36 | .05 | −.13 | −.27 | −.49* | −.47* | .56** | .58** | .44* | .38 | .49* | 1 | |||
| HRQoL – Role Emotional | .10 | .21 | −.02 | .35 | .02 | .17 | −.59** | −.65** | −.33 | −.14 | .14 | .20 | .39 | .65** | .,41* | 1 | ||
| HRQoL – Mental Health | .02 | −.04 | .05 | .46* | .02 | −.06 | −.59** | −.74** | −.64** | −.03 | .22 | .31 | .43* | .53** | .64** | .57** | 1 | |
| SRF | −.29 | −.31 | −.14 | −.40* | .22 | .29 | .75** | .65** | .50* | .23 | −.16 | −.19 | −.32 | −.69** | −.09 | −.58** | −.40* | 1 |
HADS Hospital Anxiety and Depression Scale; HRQoL Health-Related Quality of Life; PSS Perceived Stress Scale; SRF Self-Regulatory Fatigue.
*p <.05, **p <.01.
DISCUSSION
The current study supported the hypotheses that the app-based cognitive-behavioral stress management intervention program StressProffen [28] would have no technical challenges and that StressProffen would be easy to use and useful. The study also supported the secondary hypothesis and documented preliminary evidence of efficacy when delivered in a blended healthcare delivery model (preceded by a single face-to-face consultation and accompanied by telephone support).
System use, usefulness, ease of use, and user feedback
The StressProffen app-based intervention was rated as useful (87%) and easy to use (95%), with easily understandable exercises (100%), which indicates that the intervention was regarded as acceptable by the participants [32]. Interview findings where participants described learning new stress management techniques, as well as the appreciation of easy accessibility of StressProffen, also supported the acceptability of the intervention. The fact that this program was developed by scientists in close collaboration with user representatives and healthcare personnel is likely contributing to this finding [40]. User input contributed to design features such as easy access, being able to choose between reading or listening, brevity in modules, and the option of marking and easily finding back to favorite areas.
Findings suggest that lower perceived stress level and higher HRQoL – General Health subscale at baseline may have positively impacted program completion rates. Approximately two-thirds (67%) of the participants completed the program (at least 7 out of 10 modules) within the study period of eight weeks (Demand) [32]. This is a somewhat lower completion rate compared to face-to-face interventions [13, 17, 30], and may reflect the attrition challenge experienced by eHealth interventions [41, 42]. As high attrition rates have emerged as one of the major challenges to the efficacy of eHealth programs, support and follow-up are, therefore, important to strengthen adherence [43]. Given the variety of challenges posed by a cancer diagnosis and subsequent treatment, these findings may indicate that flexibility in time use can be necessary for cancer survivors to fully benefit from such a program. The repeated use of multiple stress management exercises in the program also suggests that a variety of exercises and types of exercises is beneficial to support use. Given the repeated use, it is also possible that participants may have committed some exercises to memory and to some extent continued use without the app. However, as module completion in eHealth therapy programs reportedly correlates to psychological outcomes [41], efforts to encourage and stimulate intervention adherence are of essence. Feasibility testing and intervention adjustments based on user feedback, prior to a large scale testing, can likely contribute to such increased adherence.
In the post-intervention interviews, participants described having obtained a broader understanding of stress and that using StressProffen had provided them with many new stress management techniques. They also described appreciating being able to have a support tool “anytime and anywhere,”, without having to rely on or “bother” others. This suggests that the StressProffen intervention performed as intended in the target group, and as such had an acceptable Adaption [32].
Preliminary StressProffen effect indications
Although not the primary goal of this study, the preliminary intervention effect findings are promising. For the participants completing both pre- and post-intervention questionnaires, a significant decrease in perceived stress was reported. There was also a significant decrease in anxiety. This indicates that app-based stress management interventions may have positive effects similar to those of face-to-face individual or group interventions [8, 11–15]. This needs to be verified through larger-scale RCTs, however.
The pilot study also suggest that use of StressProffen may have positive impact on HRQoL, as pre- to post-intervention improvements were found for the HRQoL subscales Role Physical, General Health, Vitality, and Role Emotion. There was, however, no significant change for Social Functioning and Mental Health. The fact that a significant worsening was found for Physical Functioning and Bodily Pain is intriguing, as it could suggest that the positive psychosocial impact in this study was achieved despite a worsening picture with regard to physical function and pain. As these are preliminary results, it is difficult to accurately interpret these findings and larger-scale studies are needed to further investigate and clarify. It is, however, encouraging to see that several HRQoL factors may be positively impacted by an app-based intervention such as the StressProffen.
Findings also indicated a positive impact on self-regulatory capacity in terms of a significant decrease in self-regulatory fatigue. To our knowledge, this is the first study to suggest that self-regulatory capacity can be improved through an app-based stress management intervention. The finding gives great promise as self-regulatory fatigue in patients with cancer and chronic pain has been shown to significantly impact choice of coping strategies, HRQoL, health behaviors, and adherence to medical recommendations [6, 7, 44, 45]. The indication needs to be verified by future research in a larger-scale setting, however. It should also be noted that most effect sizes were small to medium, with the exception of the HRQoL subscales Role Physical and Physical Functioning. This is, however, not uncommon for psychosocial interventions in cancer, and the potential clinical impact of small to medium effect sizes in this setting should not be underestimated [12, 14].
Preparation for efficacy testing
Participant feedback was used to prioritize app changes, preparing for an upcoming RCT. For example, a “My top three exercises” function was created based on individual user patterns. As the 3-day delay between modules received mixed feedback, modules 1 and 2 were opened simultaneously. Module 1 and the face-to-face introduction session had overlapping features and this change allowed users more exercises to practice and repeat initially. As increased app use was observed around the time of the follow-up phone call, a second follow-up phone call was included in the RCT protocol.
Clinical implications
Given the large positive body of evidence for clinical effects from face-to-face psychosocial interventions for cancer survivors, the preliminary indication that an app-based cognitive-behavioral stress management intervention may have similar effects gives reason for optimism. The current study utilized a single face-to-face introduction to launch the intervention and at least one phone call to support use. This type of blended delivery eHealth intervention has the potential to enhance availability of psychosocial interventions to a broader group of survivors, perhaps at a lower cost. The preliminary findings suggested by this pilot need to be confirmed through larger-scale studies, but the future potential is promising in terms of outreach and easy accessibility.
Study limitations and future directions
This study has several limitations. First of all, this is a non-randomized single-arm pilot study with a small sample size focusing on system use, usefulness, and ease of use. All effect indications should be regarded as preliminary indications. Secondly, even though a wide variety of cancer diagnoses are represented in the study, the majority was female and breast cancer survivors. Future studies should strive to include larger and more heterogenic cancer survivor populations to improve external validity, clinical utility, and generalizability. Third, time since diagnosis varies in the study and this should be controlled for in future larger studies. Also, indications of a potential link between psychological well-being at baseline and program completion should be further explored. Finally, in order to examine actual effect from app-based interventions such as StressProffen, larger-scale RCTs are needed.
CONCLUSIONS
Despite consistent positive effects, face-to-face delivery of evidence-based psychosocial interventions is not always available, or of interest, to cancer survivors. App-based stress management interventions such as StressProffen can provide a low-threshold support given their easy access, easy use, and preliminary promising indications of being effective in reducing perceived stress and anxiety, and in improving HRQoL and self-regulatory capacity. Further testing in a large-scale RCT is warranted and is in progress.
Acknowledgements
The authors would like to thank the many patients with cancer who volunteered their time for this study, the Psychosocial-Oncology team at Oslo University Hospital, and all the participating healthcare providers for contribution in the recruitment of study participants. Finally, the authors thank the Center for Shared Decision Making and Collaborative Care Research design/development team for their exceptional effort throughout the entire project process. This study was funded by the Norwegian Cancer Society (# 4602492-2013 (Principal Investigator: L.S.N.) and additional funds from the Center for Shared Decision Making and Collaborative Care Research at the Oslo University Hospital. The findings reported in this article have not been previously published, and this manuscript is not being simultaneously submitted elsewhere. Selected subparts of the results have been presented at the 39th Annual Meeting & Scientific Sessions of the Society of Behavioral Medicine in New Orleans, LA (April 2018) and at the 15th APOS Annual Conference, Tucson, AZ (February 2018). The authors have full control of all the primary data and agree to allow the journal to review their data if requested.
Compliance with Ethical Standards
Conflict of Interest: None declared.
Ethical Approval: All procedures performed involving human study participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the South East Regional Committee for Medical and Health Research Ethics in Norway (2016/14369) and the Oslo University Hospital Privacy Protection Committee/Institutional Review Board (2015/10204).
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. Word Health Organization. Cancer fact sheet 2018. http://www.who.int/news-room/fact-sheets/detail/cancer. Accessibility verified January 19, 2019.
- 2. Stanton AL. Psychosocial concerns and interventions for cancer survivors. J Clin Oncol. 2006;24(32):5132–5137. [DOI] [PubMed] [Google Scholar]
- 3. Perczek RE, Burke MA, Carver CS, Krongrad A, Terris MK. Facing a prostate cancer diagnosis: who is at risk for increased distress? Cancer. 2002;94(11):2923–2929. [DOI] [PubMed] [Google Scholar]
- 4. Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10(1):19–28. [DOI] [PubMed] [Google Scholar]
- 5. Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112(Suppl. 11):2577–2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Solberg Nes L, Ehlers SL, Patten CA, Gastineau DA. Self-regulatory fatigue in hematologic malignancies: impact on quality of life, coping, and adherence to medical recommendations. Int J Behav Med. 2013;20(1):13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Solberg Nes L, Ehlers SL, Patten CA, Gastineau DA. Self-regulatory fatigue, quality of life, health behaviors, and coping in patients with hematologic malignancies. Ann Behav Med. 2014;48(3):411–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clark MM, Rummans TA, Atherton PJ, et al. . Randomized controlled trial of maintaining quality of life during radiotherapy for advanced cancer. Cancer. 2013;119(4):880–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Holland J. Textbook of Psycho-Oncology. The Role of Psychosocial Factors in the Development of Cancer. New York: Oxford University Press; 1998. [Google Scholar]
- 10. Solberg Nes L, Liu H, Patten CA, et al. . Physical activity level and quality of life in long term lung cancer survivors. Lung Cancer. 2012;77(3):611–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Andersen BL. Psychological interventions for cancer patients to enhance the quality of life. J Consult Clin Psychol. 1992;60(4):552–568. PMID:1506503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Andersen BL, Farrar WB, Golden-Kreutz DM, Glaser R, Emery CF, Crespin TR et al. . Psychological, behavioral, and immune changes after a psychological intervention: a clinical trial. J Clin Oncol. 2004;22(17):3570–3580. PMID:15337807. doi:10.1200/jco.2004.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Antoni MH, Lehman JM, Kilbourn KM, et al. . Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001;20(1):20–32. [DOI] [PubMed] [Google Scholar]
- 14. Manne SL, Andrykowski MA. Are psychological interventions effective and accepted by cancer patients? II. Using empirically supported therapy guidelines to decide. Ann Behav Med. 2006;32(2):98–103. [DOI] [PubMed] [Google Scholar]
- 15. Gudenkauf LM, Ehlers SL. Psychosocial interventions in breast cancer survivorship care. Breast. 2018;38:1–6. [DOI] [PubMed] [Google Scholar]
- 16. Rummans TA, Clark MM, Sloan JA, et al. . Impacting quality of life for patients with advanced cancer with a structured multidisciplinary intervention: a randomized controlled trial. J Clin Oncol. 2006;24(4):635–642. [DOI] [PubMed] [Google Scholar]
- 17. Antoni MH, Wimberly SR, Lechner SC, et al. . Reduction of cancer-specific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiatry. 2006;163(10):1791–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stagl JM, Bouchard LC, Lechner SC, et al. . Long-term psychological benefits of cognitive-behavioral stress management for women with breast cancer: 11-year follow-up of a randomized controlled trial. Cancer. 2015;121(11):1873–1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thorsen L, Gjerset GM, Loge JH, et al. . Cancer patients’ needs for rehabilitation services. Acta Oncol. 2011;50(2):212–222. [DOI] [PubMed] [Google Scholar]
- 20. Okuyama S, Jones W, Ricklefs C, Tran ZV. Psychosocial telephone interventions for patients with cancer and survivors: a systematic review. Psychooncology. 2015;24(8):857–870. [DOI] [PubMed] [Google Scholar]
- 21. McAlpine H, Joubert L, Martin-Sanchez F, Merolli M, Drummond KJ. A systematic review of types and efficacy of online interventions for cancer patients. Patient Educ Couns. 2015;98(3):283–295. [DOI] [PubMed] [Google Scholar]
- 22. Slev VN, Mistiaen P, Pasman HR, Verdonck-de Leeuw IM, van Uden-Kraan CF, Francke AL. Effects of eHealth for patients and informal caregivers confronted with cancer: a meta-review. Int J Med Inform. 2016;87:54–67. [DOI] [PubMed] [Google Scholar]
- 23. Kuijpers W, Groen WG, Oldenburg HS, Wouters MW, Aaronson NK, van Harten WH. eHealth for breast cancer survivors: use, feasibility and impact of an interactive portal. JMIR Cancer. 2016;2(1):e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Urech C, Grossert A, Alder J, et al. . Web-based stress management for newly diagnosed patients with cancer (STREAM): a randomized, wait-list controlled intervention study. J Clin Oncol. 2018;36(8):780–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Seiler A, Klaas V, Tröster G, Fagundes CP. eHealth and mHealth interventions in the treatment of fatigued cancer survivors: a systematic review and meta-analysis. Psychooncology. 2017;26(9):1239–1253. [DOI] [PubMed] [Google Scholar]
- 26. Smith SK, Kuhn E, O’Donnell J, et al. . Cancer distress coach: pilot study of a mobile app for managing posttraumatic stress. Psychooncology. 2018;27(1):350–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Giunti G, Giunta DH, Guisado-Fernandez E, Bender JL, Fernandez-Luque L. A biopsy of Breast Cancer mobile applications: state of the practice review. Int J Med Inform. 2018;110:1–9. [DOI] [PubMed] [Google Scholar]
- 28. Børøsund E, Mirkovic J, Clark MM, et al. . A stress management app intervention for cancer survivors: design, development, and usability testing. JMIR Form Res. 2018;2(2):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Antoni MH, Lechner S, Diaz A, et al. . Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain Behav Immun. 2009;23(5):580–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Werneburg BL, Herman LL, Preston HR, et al. . Effectiveness of a multidisciplinary worksite stress reduction programme for women. Stress Health. 2011;27(5):356–364. [Google Scholar]
- 31. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M; Medical Research Council Guidance Developing and evaluating complex interventions: the new Medical Research Council guidance. Br Med J. 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bowen DJ, Kreuter M, Spring B, et al. . How we design feasibility studies. Am J Prev Med. 2009;36(5):452–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly. 1989;13(3):319–340. [Google Scholar]
- 34. Krippendorff K. Content Analysis. An Introduction to Its Methodology. 3rd ed. Thousand Oaks, CA: Sage; 2012. [Google Scholar]
- 35. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 36. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. [DOI] [PubMed] [Google Scholar]
- 37. Hays RD, Sherbourne CD, Mazel RM. The RAND 36-item Health Survey 1.0. Health Econ. 1993;2(3):217–227. [DOI] [PubMed] [Google Scholar]
- 38. Ware JE Jr, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 39. Nes LS, Ehlers SL, Whipple MO, Vincent A. Self-regulatory fatigue in chronic multisymptom illnesses: scale development, fatigue, and self-control. J Pain Res. 2013;6:181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Yardley L, Morrison L, Bradbury K, Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. 2015;17(1):e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. J Med Internet Res. 2011;13(3):e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Eysenbach G. The law of attrition. J Med Internet Res. 2005;7(1):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JE. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14(6):e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Nes LS, Ehlers SL, Whipple MO, Vincent A. Self-regulatory fatigue: a missing link in understanding fibromyalgia and other chronic multisymptom illnesses. Pain Pract. 2017;17(4):460–469. [DOI] [PubMed] [Google Scholar]
- 45. Solberg Nes L, Carlson CR, Crofford LJ, de Leeuw R, Segerstrom SC. Self-regulatory deficits in fibromyalgia and temporomandibular disorders. Pain. 2010;151(1):37–44. [DOI] [PubMed] [Google Scholar]