Highlights
-
•
Multiple cases of re-infections/re-positive RT-PCR of COVID-19 in people with DM have been reported.
-
•
Patients with uncontrolled diabetes mellitus (DM) have impaired antibody response.
-
•
Lack of neutralizing antibodies in DM may contribute to an increased risk of reinfection.
Keywords: COVID-19, Diabetes mellitus, Reinfections
Abstract
Several cases of positive real time-polymerase chain reaction (RT-PCR) results (called “re-positives”) after recovery from COVID-19 have emerged worldwide. These cases could represent patients experiencing a “turn positive” of nucleic acid detection attributed to the high false-negative rate of RT-PCR. On the contrary, in symptomatic patients, the possibility of reactivation or true reinfection remains. We hypothesize that people with uncontrolled diabetes mellitus might be at a high risk of reinfections with COVID-19 attributed to the impaired adaptive immune response. In fact, multiple cases of re-positives/re-infections in people with diabetes mellitus have hitherto been reported.
The novel coronavirus disease (COVID-19) has affected over 17 million people, inflicting more than 668,000 casualties in over 200 nations worldwide [1]. Moreover, the World Health Organization has raised serious concerns about the possibility of a second infection with COVID-19 [2]. Reinfections have been reported with other human coronaviruses, namely, 229E, NL63, OC43, all of which generally cause milder respiratory illness. Hitherto, multiple cases of clinical recurrence of COVID-19 and/or positive real time-polymerase chain reaction (RT-PCR) results after recovery have been reported [[3], [4], [5], [6], [7], [8]]. Among 576 patients with COVID-19 discharged from hospital in Chongqing, China, 61 patients (10.6%) had positive RT-PCR test results [6]. These cases could represent patients experiencing a “turn positive” or “re-positive” of nucleic acid detection by RT-PCR after two consecutive negative results, attributed to prolonged persistence of the virus following initial infection that remained undetected due to the high false-negative rate of RT-PCR [9,10]. In fact, persistence of traces of viral RNA can be detected in respiratory samples up to 6 weeks after the onset of symptoms in clinically-cured patients [11]. However, in clinically symptomatic patients, the possibility of reactivation or true reinfection should be entertained [[3], [4], [5]].
Primary infection with a pathogen leads to the proliferation of antigen-specific T and B-lymphocytes to control the pathogen. Eventually, a memory pool of antigen-specific adaptive immune cells is left behind that establishes long-term protection for secondary encounters [12]. Re-challenge with the same/antigenically similar pathogen leads to rapid memory activation of the humoral and cellular arms of the adaptive immune system. It has also been demonstrated that in an immunocompetent host, reinfection with the same strain of the influenza virus is prevented by antibody-mediated neutralization of viral particles (sterilizing immunity) [13].
Acquired immunity after primary COVID-19 infection has been studied in rhesus monkeys. Four Chinese rhesus macaques were infected with SARS-CoV-2 and two out of the four were re-infected at 28 days post initial infection (dpi) with the same viral dose after confirming recovery. Viral loads in the swabs tested negative after reinfection. In addition, the necropsy from a reinfected monkey showed no viral replication as well as no pathognomonic histological changes. Furthermore, sera from three monkeys at 21 and 28 dpi exhibited neutralizing activity against SARS-CoV-2 in vitro, suggesting the production of protective neutralizing antibodies [14]. Similarly, COVID-19 infection in humans leads to the production of neutralizing antibodies, directed against the nucleocapsid and spike proteins of SARS-CoV-2. IgM antibodies appear as early as within 5 days after symptom onset and IgG within 5–7 days. Maximum seroconversion occurs at 2–3 weeks for IgM and 3–6 weeks for IgG [[15], [16], [17]]. The durability of the neutralizing antibody (especially IgG) is questionable; persistence up to 40 days from symptom onset has been described. Besides, not all patients develop neutralizing antibodies and studies have shown that 10–20% of COVID-19 patients have little or no detectable antibody [18]; the reason being unknown. Thus, humoral immunity, memory B-lymphocytes, and circulating neutralizing antibodies seem crucial for preventing reinfections in COVID-19.
Diabetes mellitus (DM) is a known risk factor for severe disease and mortality in COVID-19. It is partly attributed to the dysfunctional immune system seen in patients with uncontrolled DM [19]. Both innate and adaptive arms of the immune system are compromised in DM. Hyperglycemia affects innate immunity by impeding the production of type I interferon that has antiviral properties. Hyperglycemia also impairs neutrophil chemotaxis, phagocytosis, degranulation, and oxidative burst. Defects in the adaptive immune system involve impaired T-lymphocyte function in people with uncontrolled DM [20,21]. Deficits in adaptive humoral immune response in DM are controversial; plasma immunoglobulin levels have been reported to be normal in some studies while reduced levels of IgG and IgM have been reported in others [22,23]. In addition, glycation of circulating immunoglobulins has been reported in people with DM [24]. The binding ability of glycated antibodies to their respective antigens is impaired, thereby compromising the immune response [25]. Besides, an animal model has shown that IgM producing B-1 lymphocyte function is impaired in the presence of hyperglycemia [26].
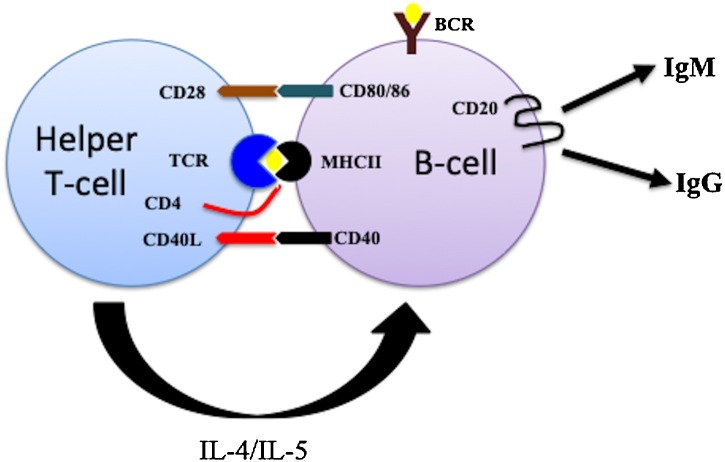
Humoral immune response and production of antigen-specific antibodies are orchestrated by B-lymphocytes. Although naïve B-lymphocytes can act as antigen-presenting cells, they require accessory signals from helper T-lymphocytes for activation into antibody-producing plasma cells [27]. Such signals include interleukins produced by helper T-lymphocytes (IL-4, IL-5, IL-6) as well as interaction between CD40L (CD40 ligand) on T-cell and CD40 on B-cell membrane (Fig. 1 ). Any abnormality in T-lymphocyte number and/or function is likely to impair B-cell activation and subsequent development of neutralizing antibodies as well. Diminished pathogen-specific memory CD4+ T-cell response had been demonstrated in people with type 2 diabetes mellitus (T2DM) in response to Streptococcus pneumoniae stimulation. The memory CD4+ T-cell response was inversely associated with fasting blood glucose and glycated hemoglobin, implying that the higher the glycemic burden, the greater is the T-cell dysfunction [21]. Impaired host defense against viral diseases due to depletion of memory CD4+ T-cells and the defective natural killer activity has also been demonstrated in type 1 diabetes mellitus (T1DM) [28]. In addition, plasma levels of sCD40L are elevated in hyperglycemic patients with T2DM that can bind to CD40 on B-cell membrane and prevent interaction between B- and T-cells [29]. Besides, hypocomplementemia seen in people with DM can further impair B-cell function and antibody generation. Genetic deficiency of C4 has been reported in 25% of patients with T1DM [28]. The possible mechanisms leading to impaired adaptive immune response in people with DM have been summarized in Table 1 . Prior studies have shown impaired antibody response in people with uncontrolled DM following influenza and hepatitis B vaccination [[30], [31], [32]]. Immunity to varicella-zoster virus is reduced in people with DM that may explain the DM-associated increased risk for developing herpes zoster [33]. However, clinicians must also be wary of the fact that SARS-CoV-2 viral clearance is delayed in people with DM and hence the chances of testing “re-positive” are expected to be higher in this subset of patients [34,35].
Fig. 1.
Showing interaction between B-lymphocyte and helper T-lymphocyte. B-cell recognizes an antigen through cell surface B-cell receptor (BCR) and presents it with major histocompatibility complex class II (MHC II) protein. Antigen-MHC II complex is recognized by T-cell receptor (TCR) on helper T-cell. Subsequent activation of B-cell requires an accessory signal mediated via interaction between CD40 ligand (CD40L) on T-cell and CD40 on B-cell. In addition, interleukin 4 and 5 (IL-4/IL-5) produced by armed helper T-cell also promote B-cell activation. Activated B-cell produces antigen-specific antibodies (IgM followed by IgG). People with uncontrolled diabetes mellitus have T-cell dysfunction that can lead to impaired B-cell activation and diminished antibody production.
Table 1.
Mechanisms underlying impaired adaptive immune response in people with uncontrolled diabetes mellitus.
| 1. Diminished pathogen-specific memory CD4+ T-cell response [21,28] |
| 2. Impaired B-cell function as B-cells require T-cells for activation into antibody-producing plasma cells [27] |
| 3. Reduced levels of circulating IgG and IgM [22,23] |
| 4. Elevated plasma levels of sCD40L [29] |
| 5. Glycation of circulating immunoglobulins [24,25] |
| 6. Low levels of circulating complements [28] |
Zhou et al. has reported that COVID-19 patients who “relapse” after discharge are usually elderly, have poor immune function, and have more comorbidities [36]. Accordingly, multiple cases of clinical recurrences of COVID-19 and/or re-positives of SARS-CoV-2 RT-PCR have been reported in patients with DM [[3], [4], [5], [6], [7], [8]]. Amongst 61 patients who had turned re-positive after being discharged from the hospital, 5 had DM [6]. In a series of 11 patients with clinical recurrences of COVID-19 after recovery, 2 had DM, one of who did not have anti-SARS-CoV-2 antibody response even 53 days after the onset of the first episode [5]. Two preliminary studies have shown no difference in the prevalence of DM in re-positives vs. non-re-positives. However, the number of re-positives included in these two studies was only 17 and 20, respectively, hence, validated conclusions are difficult to be drawn. In addition, data on glycemic control in the cohorts were not available [8,37].
Considering the fact that adaptive immunity and immunological memory is impaired in people with uncontrolled DM, patients with poor glycemic control at the time of initial diagnosis of COVID-19 might be considered to be at a high risk of re-infections. Large-scale studies involving a significant number of patients who have had clinical recurrence and/or positive RT-PCR results after complete recovery might help resolve the issue. In addition, a comparison of neutralizing anti-SARS-CoV-2 antibody titers in COVID-19 patients with and without DM (and also between people with well-controlled and uncontrolled DM) may provide some clues. Till further data is available, it would be prudent to recommend that COVID-19 survivors with DM do not consider themselves immune and continue adhering to government advisories of social distancing, hand hygiene and ensure good glycemic control. In case of any reappearance of symptoms, a possibility of clinical recurrence should be kept and medical advice should be sought immediately.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The Authors declare that there is no conflict of interest.
Acknowledgement
None.
References
- 1.Coronavirus disease (COVID-19) Situation Report – 193. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200731-covid-19-sitrep-193.pdf?sfvrsn=42a0221d_4.
- 2.“Immunity passports” in the context of COVID-19 [Internet]. [cited 2020 May 24]. Available from: https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19.
- 3.Lafaie L., Célarier T., Goethals L., Pozzetto B., Sylvain G., Ojardias E. Recurrence or relapse of COVID-19 in older patients: a description of three cases. J. Am. Geriatr. Soc. 2020 doi: 10.1111/jgs.16728. https://onlinelibrary.wiley.com/doi/abs/10.1111/jgs.16728 [cited 2020 Aug 1]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ravioli S., Ochsner H., Lindner G. Reactivation of COVID-19 pneumonia: a report of two cases. J. Infect. 2020;81:e72–3. doi: 10.1016/j.jinf.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Batisse D., Benech N., Botelho-Nevers E., Bouiller K., Collarino R., Conrad A. Clinical recurrences of COVID-19 symptoms after recovery: viral relapse, reinfection or inflammatory rebound? J. Infect. 2020 doi: 10.1016/j.jinf.2020.06.073. https://linkinghub.elsevier.com/retrieve/pii/S0163445320304540 [cited 2020 Aug 1]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deng W., Guang T., Yang M., Li J., Jiang D., Li C. Positive results for patients with COVID-19 discharged form hospital in Chongqing, China. BMC Infect. Dis. 2020 doi: 10.1186/s12879-020-05151-y. https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-05151-y [cited 2020 Aug 1];20. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dou C., Xie X., Peng Z., Tang H., Jiang Z., Zhong Z. A case presentation for positive SARS-CoV-2 RNA recurrence in a patient with a history of type 2 diabetes that had recovered from severe COVID-19. Diabetes Res. Clin. Pract. 2020;166 doi: 10.1016/j.diabres.2020.108300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu H., Fu L., Jin Y., Shao J., Zhang S., Zheng N. Clinical features of COVID‐19 convalescent patients with re‐positive nucleic acid detection. J. Clin. Lab. Anal. 2020 doi: 10.1002/jcla.23392. https://onlinelibrary.wiley.com/doi/abs/10.1002/jcla.23392 [cited 2020 Aug 1];34. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiao A.T., Tong Y.X., Zhang S. False-negative of RT-PCR and prolonged nucleic acid conversion in COVID-19: rather than recurrence. J. Med. Virol. 2020 doi: 10.1002/jmv.25855. http://doi.wiley.com/10.1002/jmv.25855 [cited 2020 May 26]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang H., Wang Y., Tong Z., Liu X. Retest positive for SARS-CoV-2 RNA of “recovered” patients with COVID-19: persistence, sampling issues, or re‐infection? J. Med. Virol. 2020 doi: 10.1002/jmv.26114. https://onlinelibrary.wiley.com/doi/abs/10.1002/jmv.26114 [cited 2020 Aug 1]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao A.T., Tong Y.X., Zhang S. Profile of RT-PCR for SARS-CoV-2: a preliminary study from 56 COVID-19 patients. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa460. https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa460/5822175 [cited 2020 Aug 1]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Francis M., King M., Kelvin A. Back to the future for influenza preimmunity—looking back at influenza virus history to infer the outcome of future infections. Viruses. 2019;11:122. doi: 10.3390/v11020122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chiu C., Ellebedy A.H., Wrammert J., Ahmed R. B cell responses to influenza infection and vaccination. In: Oldstone M.B.A., Compans R.W., editors. Influenza Pathogenesis and Control — Volume II [Internet] Springer International Publishing; Cham: 2014. pp. 381–398.http://link.springer.com/10.1007/82_2014_425 [cited 2020 May 27] (Current Topics in Microbiology and Immunology; vol. 386). Available from: [Google Scholar]
- 14.Deng W., Bao L., Liu J., Xiao C., Liu J., Xue J. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science. 2020 doi: 10.1126/science.abc5343. eabc5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu W., Liu L., Kou G., Zheng Y., Ding Y., Ni W. Evaluation of Nucleocapsid and Spike Protein-based ELISAs for detecting antibodies against SARS-CoV-2. J. Clin. Microbiol. 2020 doi: 10.1128/JCM.00461-20. http://jcm.asm.org/lookup/doi/10.1128/JCM.00461-20 [cited 2020 May 24]; Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.To K.K.-W., Tsang O.T.-Y., Leung W.-S., Tam A.R., Wu T.-C., Lung D.C. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect. Dis. 2020;20:565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sun B., Feng Y., Mo X., Zheng P., Wang Q., Li P. Kinetics of SARS-CoV-2 specific IgM and IgG responses in COVID-19 patients. Emerg. Microbes Infect. 2020;9:940–948. doi: 10.1080/22221751.2020.1762515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altmann D.M., Douek D.C., Boyton R.J. What policy makers need to know about COVID-19 protective immunity. Lancet. 2020;395:1527–1529. doi: 10.1016/S0140-6736(20)30985-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pal R., Bhansali A. COVID-19, diabetes mellitus and ACE2: the conundrum. Diabetes Res. Clin. Pract. 2020;162 doi: 10.1016/j.diabres.2020.108132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peleg A.Y., Weerarathna T., McCarthy J.S., Davis T.M.E. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes Metab. Res. Rev. 2007;23:3–13. doi: 10.1002/dmrr.682. [DOI] [PubMed] [Google Scholar]
- 21.Martinez P.J., Mathews C., Actor J.K., Hwang S.-A., Brown E.L., De Santiago H.K. Impaired CD4+ and T-helper 17 cell memory response to Streptococcus pneumoniae is associated with elevated glucose and percent glycated hemoglobin A1c in Mexican Americans with type 2 diabetes mellitus. Transl. Res. 2014;163:53–63. doi: 10.1016/j.trsl.2013.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geerlings S.E., Hoepelman A.I.M. Immune dysfunction in patients with diabetes mellitus (DM) FEMS Immunol. Med. Microbiol. 1999;26:259–265. doi: 10.1111/j.1574-695X.1999.tb01397.x. [DOI] [PubMed] [Google Scholar]
- 23.Guo X., Meng G., Liu F., Zhang Q., Liu L., Wu H. Serum levels of immunoglobulins in an adult population and their relationship with type 2 diabetes. Diabetes Res. Clin. Pract. 2016;115:76–82. doi: 10.1016/j.diabres.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Lapolla A., Tonani R., Fedele D., Garbeglio M., Senesi A., Seraglia R. Non-enzymatic glycation of IgG: an in vivo study. Horm. Metab. Res. 2002;34:260–264. doi: 10.1055/s-2002-32140. [DOI] [PubMed] [Google Scholar]
- 25.Pampati P.K., Suravajjala S., Dain J.A. Monitoring nonenzymatic glycation of human immunoglobulin G by methylglyoxal and glyoxal: a spectroscopic study. Anal. Biochem. 2011;408:59–63. doi: 10.1016/j.ab.2010.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jennbacken K., Ståhlman S., Grahnemo L., Wiklund O., Fogelstrand L. Glucose impairs B-1 cell function in diabetes: glucose impairs B-1 cell function. Clin. Exp. Immunol. 2013;174:129–138. doi: 10.1111/cei.12148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pierce S.K., Morris J.F., Grusby M.J., Kaumaya P., Buskirk A.V., Srinivasan M. Antigen-presenting function of B lymphocytes. Immunol. Rev. 1988;106:149–180. doi: 10.1111/j.1600-065x.1988.tb00778.x. [DOI] [PubMed] [Google Scholar]
- 28.Moutschen M.P., Scheen A.J., Lefebvre P.J. Impaired immune responses in diabetes mellitus: analysis of the factors and mechanisms involved. Relevance to the increased susceptibility of diabetic patients to specific infections. Diabete Metab. 1992;18:187–201. [PubMed] [Google Scholar]
- 29.Toniolo A., Cassani G., Puggioni A., Rossi A., Colombo A., Onodera T. The diabetes pandemic and associated infections: suggestions for clinical microbiology. Rev. Med. Microbiol. 2019;30:1–17. doi: 10.1097/MRM.0000000000000155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diepersloot R.J.A., Bouter K.P., Beyer W.E.P., Hoekstra J.B.L., Masurel N. Humoral immune response and delayed type hypersensitivity to influenza vaccine in patients with diabetes mellitus. Diabetologia. 1987;30:397–401. doi: 10.1007/BF00292541. [DOI] [PubMed] [Google Scholar]
- 31.Smith S.A., Poland G.A. Use of influenza and pneumococcal vaccines in people with diabetes. Diabetes Care. 2000;23:95–108. doi: 10.2337/diacare.23.1.95. [DOI] [PubMed] [Google Scholar]
- 32.Volti S.L., Caruso-Nicoletti M., Biazzo F., Sciacca A., Mandara G., Mancuso M. Hyporesponsiveness to intradermal administration of hepatitis B vaccine in insulin dependent diabetes mellitus. Arch. Dis. Child. 1998;78:54–57. doi: 10.1136/adc.78.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Okamoto S., Hata A., Sadaoka K., Yamanishi K., Mori Y. Comparison of varicella-zoster virus–specific immunity of patients with diabetes mellitus and healthy individuals. J. Infect. Dis. 2009;200:1606–1610. doi: 10.1086/644646. [DOI] [PubMed] [Google Scholar]
- 34.Chen X., Hu W., Ling J., Mo P., Zhang Y., Jiang Q. 2020. Hypertension and Diabetes Delay the Viral Clearance in COVID-19 Patients.http://medrxiv.org/lookup/doi/10.1101/2020.03.22.20040774 [cited 2020 Aug 1]. Available from: [Google Scholar]
- 35.Mazucanti C.H., Egan J.M. SARS-CoV-2 disease severity and diabetes: why the connection and what is to be done? Immun. Ageing. 2020 doi: 10.1186/s12979-020-00192-y. https://immunityageing.biomedcentral.com/articles/10.1186/s12979-020-00192-y [cited 2020 Aug 2]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhou L., Liu K., Liu H.G. Cause analysis and treatment strategies of “recurrence” with novel coronavirus pneumonia (COVID-19) patients after discharge from hospital. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:281–284. doi: 10.3760/cma.j.cn112147-20200229-00219. [DOI] [PubMed] [Google Scholar]
- 37.Yuan B., Liu H.-Q., Yang Z.-R., Chen Y.-X., Liu Z.-Y., Zhang K. Recurrence of positive SARS-CoV-2 viral RNA in recovered COVID-19 patients during medical isolation observation. Sci. Rep. 2020 doi: 10.1038/s41598-020-68782-w. http://www.nature.com/articles/s41598-020-68782-w [cited 2020 Aug 1]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]