Abstract
The full scope of the impact of The Great Recession on individuals’ mental health has not been quantified to date. This study aimed to determine whether financial, job-related, and housing impacts experienced by individuals during the recession predicted changes in the occurrence of symptoms of depression, generalized anxiety, panic attacks, and problematic alcohol or other substance use. Longitudinal survey data (n = 2,530 to n = 3,293) were analyzed from the national Midlife in the United States (MIDUS) study collected before (2003–2004) and after (2012–2013) The Great Recession. The population-level trend was towards improvements in mental health over time. However, for individuals each recession impact experienced was associated with long-lasting and transdiagnostic declines in mental health. These relationships were stronger for some sociodemographic groups, suggesting the need for additional support for people who suffer marked losses during recessions and for those without a strong safety net.
Keywords: The Great Recession, Global Financial Crisis, mental health, longitudinal research
The Great Recession in the United States officially lasted from December 2007 to June 2009, resulting in the largest national reductions in employment, earnings, assets and income since the Great Depression (Hoynes, Miller & Schaller, 2012; Jacobsen & Mather, 2011). These recession impacts can broadly be conceptualized in three domains: (1) financial impacts, including bankruptcy and increased debt; (2) job-related impacts, such as job loss or reductions in pay or hours; and (3) housing impacts, such as housing loss (eviction or foreclosure). While the majority of the U.S. population was affected by The Great Recession, the economic, labor, and housing market impacts were greatest for racial and ethnic minorities, people with lower levels of education or income, men, younger adults, and single people (Engemann & Wall, 2010; Hoynes et al., 2012; Jacobsen & Mather, 2011).
Recessions and Mental Health
Reviews of the extant literature on the associations between these types of recession impacts and mental health have consistently found that they increase risk for worse mental health—particularly depression and anxiety—and harmful coping behaviors such as risky alcohol and drug use (Burgard, Ailshire & Kalousova, 2013; Catalano et al., 2011; Frasquilho et al., 2016; Haw, Hawton, Gunnell & Platt, 2015; Margerison-Zilko, Goldman-Mellor, Falconi & Downing, 2016; Mucci, Giorgi, Roncaioli, Perez & Arcangeli, 2016; Tsai, 2015). These adverse effects of recessions on mental health compound the already high costs for society, particularly in the forms of associated economic impacts via lost productivity, healthcare utilization, and increases in suicide (Burgard et al., 2013; Chang, Stuckler, Yip & Gunnell, 2013; Kessler et al., 2008; Reeves, McKee & Stuckler, 2014; World Health Organization, 2011). Of particular concern, current research suggests that The Great Recession exerted more negative effects on mental health for the U.S. population compared to previous economic downturns, and compared to other countries (Burgard et al., 2013; Reeves et al., 2012; Riumallo-Herl, Basu, Stuckler, Courtin & Avendano, 2014). This may in part be due to substantial and increasing income inequality in the U.S. (Central Intelligence Agency, 2017), which has been found to amplify the mental health impacts of economic recessions (Paul & Moser, 2009).
Further, there is some evidence that recession impacts may differentially affect the mental health of specific sociodemographic groups: Two recent reviews have concluded that economic crises tend to have stronger negative effects on the mental health of people with lower income or education, people without secure employment, and women (Glonti et al., 2015; Zivin, Paczkowski & Galea, 2011). To the extent that these groups overlap with the groups who were more likely to experience hardships during The Great Recession (e.g., lower levels of income or education), vulnerable Americans may have suffered the worst of the adverse effects of recession hardships on mental health (World Health Organization, 2011).
Research on The Great Recession in the U.S.
Aggregate-level studies on the effects of The Great Recession in the U.S. have found that suicide rates and alcohol-related suicides—visible indicators of the recession’s toll on mental health—rose in tandem with the national unemployment, foreclosure, and poverty rates (Kerr et al., 2017; Phillips & Nugent, 2014). Specifically, levels of psychological distress, symptoms of depression, chronic mental illness, and mental health care utilization were found to rise during the recession in most (Cagney, Browning, Iveniuk & English, 2014; Chen & Dagher, 2016; Lo & Cheng, 2014; Mark, Hodgkin, Levit & Thomas, 2016; Modrek, Hamad & Cullen, 2015), but not all (Dagher, Chen & Thomas, 2015) trend analyses. Population-level alcohol use often declines during recessions, but this net effect appears to mask a combination of increases in abstention from alcohol, as well as increases in binge drinking (Bor, Basu, Coutts, McKee & Stuckler, 2013).
While these aggregate-level studies tend to support the conclusion that The Great Recession adversely affected mental health in the U.S., comprehensive studies of these relationships in data on individuals’ experiences spanning the duration of the recession are lacking (Burgard et al., 2013; Catalano et al., 2011; Frasquilo et al., 2016; Zivin et al., 2011). Research in this framework has been restricted by the availability of appropriate data, and has largely focused on associations between a limited range of specific recession hardships (i.e., job loss and changes in financial well-being) and depressive outcomes in older adults (aged 50+; Pruchno, Heid & Wilson-Genderson, 2017; Riumallo-Herl et al., 2014; Wilkinson, 2016). Data from a convenience sample from Detroit also found that individuals’ exposure to foreclosure predicted subsequent symptoms of major depression and generalized anxiety (McLaughlin et al., 2011). Finally, data from the Panel Study of Income Dynamics showed that declines in housing wealth were associated with psychological distress, and that difficulties with mortgage repayments were associated with both distress and depression symptoms (Yilmazer, Babiarz & Liu, 2015). To our knowledge, these studies represent all of the individual-level analyses of how recession impacts during The Great Recession predicted changes in mental health. Notably, no studies have systematically examined the relationships among the spectrum of hardships caused by The Great Recession and corresponding changes over time in individual Americans’ mental health across the key domains of depression, anxiety, and problematic alcohol and substance use. The scope of The Great Recession’s impact on individuals’ mental health in the U.S. therefore remains largely unknown. Understanding the effects on both population- and individual-level mental health is important for policy and planning for future recessions, as well as for determining whether targeted interventions may be effective for specific types of recession impacts, mental health domains, or sociodemographic groups. These questions may be particularly pertinent given some indications that the next period of economic contraction might begin as early as 2020 (e.g., Colvin, 2018).
The Present Study
The longitudinal Midlife in the United States (MIDUS) study includes broad assessment of symptoms of depression, anxiety, and problematic alcohol and substance use in a national sample before and after The Great Recession, as well as assessing a broad spectrum of financial, job-related, and housing recession impacts that these individuals experienced. These data thus provide an ideal opportunity for a first look at the relationships among a comprehensive set of recession impacts and mental health outcomes in the U.S. The objective of this study was to characterize how each domain of recession impacts predicted mental health outcomes over the course of The Great Recession. A secondary objective was to determine whether these relationships were moderated by sociodemographic characteristics—for example, whether the relationship between job-related impacts and depressive symptoms was stronger for people with lower levels of education. We did not specify hypotheses a priori, but the literature reviewed above suggested three outcomes: (1) Declines in population-level mental health over the course of the recession; (2) Recession impacts would have broad adverse associations with affected individuals’ mental health; and (3) Some sociodemographic groups (e.g., people with lower education, without secure employment, and women) may have experienced greater declines in mental health associated with recession impacts.
Method
Sample and Procedure
MIDUS is a longitudinal study of adult development that began in 1995 with a nationally representative sample of 7,108 non-institutionalized, English-speaking adults in the U.S. aged 25–75 (Radler, 2014). The initial sample at the first wave of the study (MIDUS-I) comprised a national random digit dialling sample (n = 3,487) with an oversample in select metropolitan areas (n = 757); siblings of individuals from the RDD sample (n = 950); and a national RDD sample of twins (n = 1,914). We used the data from the second (MIDUS-II) and third (MIDUS-III) waves of the core survey study—collected in 2003–2004 and 2012–2013, respectively—to focus on change in mental health from pre- to post-recession. Participants at MIDUS-II and MIDUS-III included the living respondents that could be contacted and agreed to participate. Adjusted for mortality, the retention rates for MIDUS-II and MIDUS-III were 75% and 77%, respectively. The attrition from MIDUS-I to MIDUS-II has been analyzed in detail elsewhere (Radler & Ryff, 2010) and does not fundamentally bias the representativeness of the study sample. We further examined whether attrition from MIDUS-II to MIDUS-III was related to the variables in our study (see Table S1 in the Supplemental Material available online). There were no differences between the retained and attrited samples on any study variable that exceeded a small standardized effect size.
We included participants in the analyses for each mental health outcome based on whether they had complete data for that outcome. All participants completed a 30-minute telephone interview at each wave—which included the questions regarding depression, generalized anxiety, and panic symptoms described below—and were asked to complete extensive self-administered questionnaires—which included the questions regarding alcohol and substance use described below. Descriptive statistics for the analytic sample for each outcome are provided in Table 1. Comparisons of these samples to participants without complete data for each outcome are provided in Table S1 in the Supplemental Material available online and indicated no differences exceeding a small standardized effect size for any study variables, except that the sample with complete information on their symptoms of problematic substance use had a lower mean number of financial and job-related impacts compared to other participants (M[SD] of 1.1 [1.23] versus 1.5 [1.42], d = .31; and 0.4 [0.75] versus 0.6 [1.00], d = .30, respectively). However, the proportion of people in each sample who had experienced at least one financial or job-related impact did not differ substantially (φ = .10 and φ = .12, respectively; see Table 2).
Table 1.
Descriptive statistics for the analytic samples for each mental health outcome; No.(%) or M(SD)
| Mental Health Outcome |
|||
|---|---|---|---|
| Variable | Depression, generalized anxiety, and panic symptoms (n = 3,293) |
Problems related to alcohol use (n = 2,530) |
Problems reated to other substance use (n = 2,545) |
| Sociodemographic characteristics prior to The Great Recession (range or reference category) | |||
| Age in years (30–84) a | 54·5 (11·35) | 55·6 (11·23) | 55·5 (11·21) |
| Sex (Female) b | 1810 (55·0%) | 1421 (55·8%) | 1414 (55·9%) |
| Race-ethnicity (White) c | 3026 (91·9%) | 2361 (93·1%) | 2346 (93·0%) |
| Education (No college) d | 952 (29·0%) | 751 (29·5%) | 740 (29·3%) |
| Employment status (Not in paid work) e | 646 (19·6%) | 523 (24·9%) | 523 (25·0%) |
| Marital status (Not married or cohabiting) | 760 (23·1%) | 604 (23·7%) | 601 (23·8%) |
| Income per person (0–300,000), $/year f | 41,250 (34,185·8) | 40,806 (33,490·1) | 40,840 (33,481·1) |
| Financial advantage g | |||
| Current financial situation (0–10) g | 6·6 (2·09) | 6·6 (2·08) | 6·6 (2·08) |
| Enough money to meet needs (Not enough) g | 515 (15·6%) | 450 (17·8%) | 452 (18·0%) |
| Difficult to pay bills (Somewhat or Very) g | 735 (22·3%) | 625 (24·7%) | 624 (24·8%) |
| Prevalence of mental health outcomes | |||
| Symptoms of major depression at MIDUS-II | 393 (11·9%) | 293 (11·5%) | 291 (11·5%) |
| Symptoms of major depression at MIDUS-III | 397 (12·1%) | 286 (11·2%) | 284 (11·2%) |
| Symptoms of generalized anxiety at MIDUS-II | 89 (2·7%) | 61 (2·4%) | 61 (2·4%) |
| Symptoms of generalized anxiety at MIDUS-III | 84 (2·6%) | 57 (2·2%) | 56 (2·2%) |
| Symptoms of panic disorder at MIDUS-II | 356 (10·8%) | 256 (10·1%) | 258 (10·2%) |
| Symptoms of panic disorder at MIDUS-III | 340 (10·3%) | 244 (9·6%) | 247 (9·8%) |
| Problems related to alcohol use at MIDUS-II | 614 (18·6%) | 511 (20·3%) | 514 (20·3%) |
| Problems related to alcohol use at MIDUS-III | 515 (15·6%) | 473 (18·7%) | 481 (19·0%) |
| Problems related to substance use at MIDUS-II | 158 (4·8%) | 132 (5·2%) | 136 (5·4%) |
| Problems related to substance use at MIDUS-III | 114 (3·5%) | 101 (3·4%) | 99 (3·9%) |
Age in years was divided by ten and centered at the mean for analysis so regression coefficients in subsequent analyses can be interpreted as the effect corresponding to a ten-year age difference.
Sex was self-reported as male or female.
Race-ethnicity was based on self-reported main racial origins (parents, grandparents, and other ancestors), and was classified as white or minority.
Education was based on self-reported highest grade of school or year of college completed, and classified as up to and including graduation from high school (no college) or one or more years of college.
Employment status was based on self-reported employment situation in January 2008, and classified as working or self-employed (in paid work) or not in paid work.
Income per person was calculated as total household income divided by the number of people in the household and was standardized for analysis so regression coefficients in subsequent analyses can be interpreted as the effect corresponding to a one standard deviation difference in income.
Financial advantage was calculated as the sum of three standardized items: (a) “Using a scale from 0 to 10 where 0 means “the worst possible financial situation” and 10 means “the best possible financial situation,” how would you rate your financial situation these days?”; (b) “In general, would you say you (and your family living with you) have more money than you need [2], just enough for your needs [1], or not enough to meet your needs [0]?”; and (c) “How difficult is it for you (and your family) to pay your monthly bills?” rated from “very difficult” (1) to “not at all difficult” (4). This sum score was standardized for analyses so regression coefficients in subsequent analyses can be interpreted as the effect corresponding to a one standard deviation difference in financial advantage.
Note. MIDUS-II is the second wave of data from the Midlife in the United States study, collected in 2003–2004; MIDUS-III is the third wave, collected in 2012–2013.
Table 2.
Prevalence of recession impacts within the analytic sample for each mental health outcome; No. (%)
| Mental Health Outcome |
|||
|---|---|---|---|
| Recession Impact by Domain | Depression, generalized anxiety, and panic symptoms (n = 3,293) |
Problems related to alcohol use (n = 2,530) |
Problems related to other substance use (n = 2,545) |
| Financial impacts | |||
| Declared bankruptcy | 97 (2·9%) | 74 (2·9%) | 72 (2·8%) |
| Missed a credit card payment | 364 (11·1%) | 233 (9·2%) | 232 (9·1%) |
| Missed other debt payments, car/student loans | 195 (5·9%) | 114 (4·5%) | 113 (4·4%) |
| Increased credit card debt | 671 (20·4%) | 484 (19·1%) | 482 (18·9%) |
| Sold possessions to make ends meet | 449 (13·6%) | 315 (12·5%) | 311 (12·2%) |
| Cut back on your spending | 2039 (61·9%) | 1508 (59·6%) | 1514 (59·5%) |
| Exhausted unemployment benefits | 240 (7·3%) | 174 (6·9%) | 173 (6·8%) |
| At least one financial impact | 2189 (66·5%) | 1620 (64·0%) | 1626 (63·9%) |
| Job-related impacts | |||
| Lost a job | 446 (13·5%) | 301 (11·9%) | 299 (11·7%) |
| Started a new job did not like | 210 (6·4%) | 129 (5·1%) | 127 (5·0%) |
| Taken job below education/experience | 377 (11·4%) | 253 (10·0%) | 253 (9·9%) |
| Taken on an additional job | 344 (10·4%) | 228 (9·0%) | 226 (8·9%) |
| At least one job-related impact | 863 (26·2%) | 596 (23·6%) | 594 (23·3%) |
| Housing impacts | |||
| Missed a mortgage or rent payment | 232 (7·0%) | 136 (5·4%) | 135 (5·3%) |
| Been threatened with foreclosure or eviction | 165 (5·0%) | 104 (4·1%) | 103 (4·0%) |
| Sold a home for less than it cost | 148 (4·5%) | 103 (4·1%) | 102 (4·0%) |
| Lost a home to foreclosure | 69 (2·1%) | 45 (1·8%) | 45 (1·8%) |
| Lost a home to something other foreclosure | 76 (2·3%) | 50 (2·0%) | 49 (1·9%) |
| Family/friends moved in to save money | 407 (12·4%) | 298 (11·8%) | 296 (11·6%) |
| Moved in with family/friends to save money | 151 (4·6%) | 106 (4·2%) | 104 (4·1%) |
| At least one housing-related impact | 762 (23·1%) | 526 (20·8%) | 523 (20·6%) |
The MIDUS protocol was reviewed and approved by ethics committees at all participating institutions and the research was carried out in accordance with the provisions of the World Medical Association Declaration of Helsinki. Participants provided informed consent and monetary incentives were offered to compensate for respondent burden. Preparation of this article followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Assessment
Sociodemographic characteristics including financial resources were assessed at MIDUS-II prior to The Great Recession, as shown in Table 1.
Financial, job-related, and housing impacts experienced during the Great Recession were assessed at MIDUS-III based on “yes” (1) or “no” (0) responses to each item shown in Table 2. Each impact was asked about specifically regarding respondents’ experiences with the recession, and the number of impacts in each domain was used as the primary predictor of mental health outcomes (Kirsch & Ryff, 2016).
Mental health outcomes during the past 12 months were assessed at both waves. The World Health Organization’s Composite International Diagnostic Interview Short Form (CIDI-SF; Kessler, Andrews, Mroczek, Ustun & Wittchen, 1998) was included in the phone interview to assess clinically significant symptoms of major depression, generalized anxiety, and panic disorder. Clinically significant symptoms of depression in the past 12 months included at least two weeks in a row of (1) either feeling sad, blue, or depressed or losing interest in most things (e.g., hobbies, work, or usually pleasurable activities) most of the day, nearly every day, and (2) at least one other symptom (low energy, change in appetite, sleep difficulties, concentration difficulties, guilt, or suicidality) during the same period. Clinically significant symptoms of generalized anxiety in the past 12 months included (1) worrying a lot more than most people, most days, and (2) worrying about more than one thing or having multiple worries at once, and (3) at least one other symptom (i.e., restless, on edge, irritable, trouble falling or staying asleep, trouble concentrating or remembering things, low energy, feeling tired, having sore or aching muscles) due to worry most days during the same period. Clinically significant symptoms of panic in the past 12 months included (1) a spell or attack of feeling afraid or anxious or of physiological arousal not due to a physical cause, and (2) the attack happened when not in danger or the center of attention, and (3) at least one other symptom (i.e., pounding heart, discomfort in chest or stomach, sweating, shaking, hot flashes, or chills, feeling or unreality) during the attacks. Problems related to alcohol and other substance use were assessed in the self-administered questionnaires based on items inquiring about abuse or dependence symptoms experienced in the past 12 months, including using larger amounts of alcohol or other substances than intended; being under the influence of alcohol or other substances at work, school, or while caring for children; using substances in hazardous situations; experiencing emotional or psychological problems as a result of alcohol or other substance use; having a strong desire to use alcohol or other substances; spending a lot of time using alcohol or other substances or recovering from the effects; and needing to use more alcohol or other substances than usual to get the same effect. For each outcome, symptoms were coded as present (1) or absent (0) at each wave.a
Statistical Analyses
As described above, participants were included in the analyses if they had complete data for the mental health outcome being analysed. Missing data for other variables were imputed, and reported results are based on pooled estimates across 20 multiple imputation data sets. Population-level changes in mental health were represented by the descriptive aggregate-level results for observed changes in prevalence over time for each mental health outcome. To examine individual-level change, preliminary multiple linear regression analyses were used to quantify the relationships among recession impacts and sociodemographic characteristics in our sample. The primary analyses were then conducted using multiple logistic regressions to calculate the odds of each mental health outcome at MIDUS-III as a function of the number of each type of recession impacts experienced, controlling for extant symptoms of the mental health outcome at MIDUS-II. After examining these unconditional relationships in Step 1, Step 2 also controlled for the sociodemographic variables. Step 3 included interaction terms between the recession impact and sociodemographic variables to test whether the relationships in Steps 1 and 2 varied as a function of sociodemographic characteristics (e.g., whether the relationship between job-related impacts and depressive symptoms was stronger for people with lower levels of education, compared to those with higher education). To test whether these results related to each symptom domain specifically, or to the patterns of overlap between symptom domains, we also examined these relationships in a transdiagnostic latent variable indirect effects modelling framework (Muthén & Muthén, 1998-2018). Specifically, we modelled the variance shared among depression, generalized anxiety, and panic symptoms in a transdiagnostic internalizing latent variable, and the variance shared between problems related to alcohol and other substances in a substance use latent variable (Kotov et al., 2017). We then examined the proportion of the total effects for each symptom domain in Steps 1 and 2 above that was accounted for by the corresponding higher-order latent variable, and what proportion was unique to each symptom domain. We also tested whether any sociodemographic variables moderated the associations between recession impacts and the two transdiagnostic dimensions.
Analyses were conducted separately for each type of recession impact and mental health outcome, and the Benjamini-Hochberg procedure (Benjamini & Hochberg, 1995) was used to account for multiple comparisons in significance testing, allowing for a paper-wide false discovery rate of 5%. A clustering variable was included in all regression analyses to account for non-independence of observations within families, given the presence of twin and sibling participants in the sample, and maximum likelihood estimation with robust standard errors was used to account for the non-independence of observations over time (Field & Wilcox, 2017). All analyses were conducted in MPlus version 8.
Results
Population-Level Change
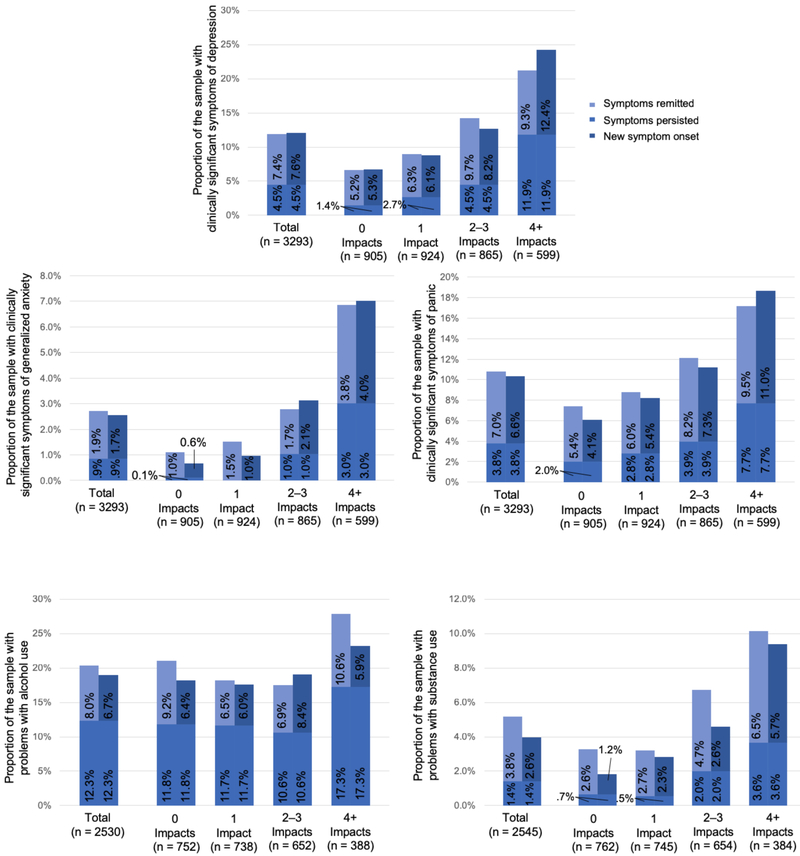
To understand population-level change over time, we examined the change in prevalence of each mental health outcome from before the recession (2003–2004) to after the recession (2012–2013) for the total sample, as well as stratified by quartiles of the total number of recession impacts experienced (see Figure 1). In the full sample the prevalence of each mental health outcome generally remained stable or decreased over time. However, the group of people who had experienced the greatest number of recession impacts (four or more) had the highest prevalence of all outcomes before and after the recession. Further, this group had the greatest proportions of individuals with symptoms that persisted between both waves for all outcomes (3–17%; 1·5–30 times greater than people who did not experience any recession impacts), and the greatest proportions of individuals with symptom onset after the recession for all outcomes except problems with alcohol (4–12%; 2·3–6·7 times greater than people who did not experience any recession impacts). These stratified results indicated that individuals’ experiences of recession impacts may be differentially associated with mental health, but that these patterns of association are obscured in the population-level change.
Figure 1.
Change in the prevalence of each mental health outcome from MIDUS-II (left-hand bar in each pair) to MIDUS-III (right-hand bar in each pair) for the total sample, and stratified by quartiles of total number of recession impacts experienced—(a) symptoms of depression; (b) symptoms of generalized anxiety; (c) symptoms of panic; (d) problems with alcohol use; (e) problems with other substance use. The prevalence at each wave is decomposed into persistent symptoms (i.e., respondents with symptoms at both waves) versus remitted and new onset of symptoms (i.e., respondents with symptoms at only MIDUS-II or MIDUS-III, respectively).
Individual-Level Change in Specific Mental Health Outcomes
Preliminary analyses
Holding all other sociodemographic characteristics constant, younger people and people with more financial disadvantage experienced more financial, job-related, and housing impacts, on average (see Table S2 in the Supplemental Material available online). People with higher education also experienced marginally more job-related impacts, on average.
Step 1: Associations between recession impacts and mental health outcomes
Each recession impact—regardless of the specific domain of impact—was associated with 1.3 to 1.5 times higher odds of symptoms of depression, generalized anxiety, panic, and problems associated with substance use after The Great Recession, controlling for the presence of those symptoms before The Great Recession (see Table 3). These relationships were all statistically significant, with the exception of the association between job-related impacts and symptoms of generalized anxiety. In contrast, the associations between each recession impact and problematic alcohol use were all small (ORrange = 1.0–1.1) and not statistically significant.
Table 3.
Odds ratios (95% Confidence Intervals) for the association between recession impacts in each domain and mental health outcomes
| Domain of Recession Impact |
|||
|---|---|---|---|
| Mental Health Outcome | Financial OR (95%CI) |
Job-related OR (95%CI) |
Housing OR (95%CI) |
| Symptoms of major depression (n = 3293) | |||
| Step 1 | 1·3 (1·23–1·42) | 1·4 (1·23–1·53) | 1·4 (1·29–1·58) |
| Step 2 | 1·2 (1·14–1·35) | 1·3 (1·14–1·45) | 1·3 (1·18–1·48) |
| Symptoms of generalized anxiety (n = 3293) | |||
| Step 1 | 1·5 (1·32–1·72) | 1·3 (1·05–1·56) | 1·5 (1·30–1·79) |
| Step 2 | 1·3 (1·09–1·61) | 1·1(0·89–1·40) | 1·3 (1·04–1·59) |
| Symptoms of panic disorder (n = 3293) | |||
| Step 1 | 1·3 (1·18–1·37) | 1·3 (1·14–1·46) | 1·3 (1·15–1·44) |
| Step 2 | 1·2 (1·09–1·32) | 1·2 (1·05–1·37) | 1·2 (1·05–1·34) |
| Problems related to alcohol use (n = 2530) | |||
| Step 1 | 1·0 (0·92–1·10) | 1·1 (0·97–1·30) | 1·0 (0·90–1·20) |
| Step 2 | 1·0 (0·88–1·08) | 1·0 (0·89–1·21) | 1·0 (0·89–1·20) |
| Problems related to other substance use (n =2545) | |||
| Step 1 | 1·4 (1·18–1·58) | 1·4 (1·10–1·75) | 1·5 (1·24–1·81) |
| Step 2 | 1·2 (1·00–1·43) | 1·2 (0·94–1·57) | 1·3 (1·07–1·64) |
Note. The odds ratios in Step 1 are controlled for baseline levels of the mental health outcome. The odds ratios in Step 2 are also controlled for all sociodemographic characteristics listed in Table 1. Statistically significant associations (adjusting for a paper-wide false discovery rate of 5%) are presented in bold.
Step 2: Controlling for sociodemographic characteristics
The magnitude of the associations for depression and panic symptoms was largely robust after controlling for the sociodemographic variables (ΔOR ≤ .1; see Table 3). Accounting for sociodemographic variables attenuated the associations of recession impacts with generalized anxiety symptoms and problematic substance use more so (ΔORrange = .17–24), although the specific associations between financial impacts and generalized anxiety symptoms, and between housing impacts and problematic substance use remained statistically significant (see Table 3).
Step 3: Interactions between recession impacts and sociodemographic characteristics
The complete results for Step 3 are provided in the supplementary materials (see Table S3 in the Supplemental Material available online). After constraining the paper-wide false discovery rate to 5%, there were four substantive and statistically significant moderation effects that highlighted a stronger association between recession impacts and mental health outcomes for specific sociodemographic groups:
People without a college-level education were 1.8 (95%CI 1.31 to 2.60) times more likely to have generalized anxiety symptoms associated with each job-related impact, compared to people with a college-level education.
People with greater financial advantage were more likely to have generalized anxiety symptoms associated with each housing impact, compared to people with less financial advantage, such that a one standard deviation increase in financial advantage was associated with 1.3 (95%CI 1.09 to 1.50) times higher odds of symptoms.
Similarly, people with greater financial advantage were more likely to have problems related to substance use associated with each financial impact, compared to people with less financial advantage, such that a one standard deviation increase in financial advantage was associated with 1.3 (95%CI 1.14 to 1.57) times higher odds of problematic substance use.
People who were not married or cohabiting with a partner were 1.7 (95%CI 1.21 to 2.36) times more likely to have problems related to substance use associated with each housing impact experienced.
Specificity versus generality of associations between recession impacts and mental health outcomes
We next examined the proportion of the total effects for each symptom domain in Steps 1 and 2 above that was accounted for by transdiagnostic latent variables. Specifically, we used a transdiagnostic internalizing latent variable to model the variance shared among depression, generalized anxiety, and panic symptoms, and a substance use latent variable to model the variance shared between problems related to alcohol and other substances. We then controlled for the corresponding latent variable in the analyses in Steps 1 and 2 above, and calculated the proportion of the total effect for each symptom domain that was accounted for by the corresponding latent variable (i.e., the direct effect for each symptom domain after controlling for the corresponding latent variable was divided by the total effect for the symptom domain).
An internalizing latent variable accounted for an average of 97.2% (range 82.0-100%) of the associations between the recession impacts and symptom domains in Steps 1 and 2 above, indicating that these relationships were largely at the level of the transdiagnostic internalizing variable, rather than specific to the individual symptom domains. The proportions were similar across the three internalizing symptom domains: an average of 97.5% (range 91.4-100%) for symptoms of major depression, 99.9% (99.5%-100%) for generalized anxiety, and 94.3% (82.0-100%) for panic. The negligible associations found for problematic alcohol use in Steps 1 and 2 were also wholly accounted for a substance use latent variable. By contrast, the substance use latent variable accounted for a smaller proportion (average of 67.3%, range 33.4–100%) of the associations between recession impacts and symptoms of problematic substance use in Steps 1 and 2 above, indicating that these associations tended to be both specific to problematic substance use and related to the overlap between problems related to alcohol and other substance use.
Individual-Level Change in Transdiagnostic Mental Health Outcomes
Given the internalizing and substance use latent variables tended to account for substantial proportions of the associations between recession impacts and mental health outcomes, we also examined these latent variables as mental health outcomes in the same analytic framework described above for the symptom domains (Step 1–Step 3), holding strict measurement invariance between waves.b Each recession impact—regardless of the specific domain of impact—was associated with small to moderate standardized increases in internalizing, controlling for levels of internalizing before The Great Recession (see Table 4). These associations were somewhat attenuated but remained statistically significant after controlling for the sociodemographic variables (Δβrange = .03–.04; see Table 4). In contrast, the associations for each recession impact with the substance use latent variable were very small and not statistically significant—both before and after controlling for sociodemographic variables (see Table 4). There was only one example of moderation by sociodemographic characteristics: People who were not in paid employment had an additional 0.11 standard deviation increase on internalizing associated with each financial impact they experienced, compared to people who were in paid employment.
Table 4.
Standardized regression coefficients (95% Confidence Intervals) for the association between recession impacts in each domain and transdiagnostic latent variables.
| Transdiagnostic Domain | Domain of Recession Impact |
||
|---|---|---|---|
| Financial | Job-related | Housing | |
| Internalizing (n = 3293) | |||
| Step 1 | 0·22 (0·17–0·27) | 0·14 (0·09–0·19) | 0·17 (0·13–0·22) |
| Step 2 | 0·18 (0·11–0·24) | 0·11 (0·05–0·16) | 0·14 (0·09–0·19) |
| Substance use (n = 3062) | |||
| Step 1 | 0·02 (−0.02–0.07) | 0·05 (−0.01–0.10) | 0·02 (−0.02–0.07) |
| Step 2 | 0·00 (−0.06–0.06) | 0·01 (−0.05–0.06) | 0·02 (−0.03–0.08) |
Note. The regression coefficients in Step 1 are controlled for baseline levels of the transdiagnostic latent variable. The regression coefficients in Step 2 are also controlled for all sociodemographic characteristics listed in Table 1. Statistically significant associations (adjusting for a paper-wide false discovery rate of 5%) are presented in bold.
Discussion
To our knowledge, this is the first study that has examined how a comprehensive set of recession impacts predicted individuals’ mental health outcomes over the course of The Great Recession. Interestingly, between 2003 and 2013, the population-level trend was towards improving mental health. However, individuals who had experienced even a single financial, job-related, or housing impact during the recession still had higher odds of symptoms of depression, generalized anxiety, panic, and problematic substance use three to four years after recession had ended. The magnitude of these associations was largely consistent regardless of demographic characteristics and financial resources—with a few notable exceptions discussed below. Taken together, these results suggest that the impacts of The Great Recession were associated with lasting and transdiagnostic declines in individuals’ mental health.
As mentioned above, it is noteworthy that the population-level prevalence of depression, generalized anxiety, panic, and problematic substance use decreased over the course of the study. This is a positive finding, given the nation-wide impact of The Great Recession, but it obscured the experiences of individuals who were hit hardest: The group of individuals who experienced four or more recession impacts had the highest rates of symptom persistence and new symptom onset for all mental health outcomes except problems related to alcohol use. In line with these findings, analyses focusing on individuals’ experiences showed broad adverse associations between recession impacts and mental health, as expected. These contradictory individual-versus group-level effects are a reminder of the ecological fallacy associated with using aggregate-level data when trying to understand impacts on individuals (Burgard et al., 2013) and highlight the importance of analysing longitudinal data that track specific individuals over time, as we were able to do here.
The remarkable consistency in the results for symptoms of depression, generalized anxiety, and panic could be parsimoniously accounted for by a transdiagnostic internalizing variable. Correspondingly, each recession impact was associated with increases in individuals’ level of internalizing. By contrast, problems with alcohol and other substances tended to operate relatively more independently from one another, as recession impacts predicted individuals’ problems associated with substance use, but not alcohol use. The null results for problems with alcohol use were the one exception to the pattern of transdiagnostic relationships among recession impacts and worse mental health. These results are broadly consistent with past population-level findings that alcohol consumption does not increase during recessions (Freeman, 1999; Ruhm, 1995), but are at odds with findings that binge drinking increases (Bor et al., 2013; Dee, 2001). Our aggregate-level findings indicated that the prevalence of problems with alcohol use declined over time for all groups; while 7% of the sample reported new onset of problems with alcohol, a larger proportion (8%) reported that their problems with alcohol remitted. Combined with the non-significant individual-level results, these findings may support the hypothesis that the effects of recession impacts on problematic alcohol use are more acute, whereas associations with depression, anxiety, and problematic substance use are more robust and/or longer lasting (Catalano et al., 2011).
Our secondary objective was to determine whether recession impacts differentially affected the mental health of specific sociodemographic groups. For example, the extant literature suggested that economic crises tend to have stronger negative effects on the mental health of people with lower education, without secure employment, and women (Glonti et al., 2015; Zivin et al., 2011). We found several examples of moderation effects that highlighted this vulnerability of less privileged groups: People with lower education were more likely to develop symptoms of generalized anxiety in response to job-related impacts; people not living with a partner were more likely to develop problematic substance use in response to housing impacts; and people not in paid employment experienced greater increases in internalizing associated with each financial impact they experienced. These associations are in line with the expectation that vulnerable groups would suffer particularly adverse effects due to recession impacts (World Health Organization, 2011), likely reflecting the relative lack of safety net available to people in the job market with fewer qualifications, and who rely on a single income.
There was also some indication that age was a vulnerability factor for mental health during The Great Recession, as younger people experienced more of all types of recession impacts and had higher odds of all adverse mental health outcomes following the recession. While the strength of the associations between recession impacts and mental health did not vary by age, these findings suggest that younger adults in particular may still be suffering the consequences of the recession. Our sample was limited to respondents aged 30 years and over at baseline, so these relationships may be stronger still in younger age groups; for example, people aged 18–29 during the recession have experienced particularly slow job market recovery (Bureau of Labor Statistics, 2017). This is an important avenue for future research.
However, the stronger associations between recession impacts and adverse mental health outcomes were not exclusive to vulnerable sociodemographic groups, but were also evident in privileged groups who were less likely to experience hardships due to the recession. For example, people with less financial advantage (e.g., not having enough money to meet one’s needs) were more likely to experience all types of recession impacts. However, it was people with more financial advantage who reported higher odds of generalized anxiety symptoms and problematic substance use related to housing and financial impacts, respectively. This is in line with McInerney et al.’s (2013) finding that older adults with higher levels of stock holdings before the recession experienced the largest increases in feelings of depression during the recession, corresponding to their larger losses in assets. Similarly, when reported by people with financial advantage, the recession impacts examined here likely reflect a marked loss of assets. For example, moving in with friends or family to save money—or selling possessions to make ends meet—likely reflect a level of hardship further removed from pre-recession life for those who were previously living comfortably.
Limitations and Future Directions
While the use of a large, longitudinal national sample was a key strength of this study, it also means interpretation of the results is constrained by the limitations of observational research. For example, causality cannot be inferred. Further, without information on the experience of the various financial, job-related, and housing impacts prior to the recession, we were not able to measure how change in the impacts predicted change in the mental health outcomes. Instead, we controlled for pre-recession sociodemographic status and financial advantage as an index of pre-recession life. However, this means that we cannot fully disentangle the recession impacts experienced during the recession from the mental health outcomes. For example, being depressed during the recession may well have led an individual to miss credit card payments or to dislike a new job. We controlled for the presence of symptoms in each domain prior to the recession to focus on changes in mental health, but it is important to acknowledge the potential for criterion contamination in the mental health outcomes used here. Further, the assessment of mental health outcomes was broad, but not comprehensive; we used the presence or absence of clinically significant symptoms in each mental health domain as our observed variables of mental health outcomes. This decision maximized sensitivity to population-level changes in mental health and corresponding impairment of psychosocial function, but does not directly measure impairment associated with these symptoms, or diagnostic status. Future research could examine how specific recession impacts related to individual symptoms or symptom clusters and associated impairment. Finally, these findings are likely specific to the U.S. context, but their concordance with other research on recession impacts in the U.S. suggests that the findings would generalize to future recessions.
Conclusion
This study provides the first comprehensive look at how Americans’ mental health changed as a function of hardships during The Great Recession. While population-level mental health generally improved over the course of the study, each recession hardship experienced by an individual was associated with higher odds of long-lasting and transdiagnostic declines in mental health. These relationships were stronger for some sociodemographic groups, suggesting the need for additional support for people who suffer marked losses during recessions and for those without a strong safety net. The transdiagnostic findings and the similarity of effects across financial, job-related, and housing impacts also indicate that broadband public health interventions—rather than targeted interventions for specific symptom domains or recession impacts—may be an effective approach to providing mental health support for individuals who experience hardships during recessions. Ultimately, the adverse effects of The Great Recession on individuals’ mental health likely compounded and prolonged its economic costs. These findings thus highlight that government-funded mental health support in future recessions would not only ease individuals’ burdens, but could be a sound financial investment that may act to stimulate faster economic recovery.
Supplementary Material
Acknowledgments
Financial Support: The work of M.K.F. on this research was supported by a National Institute on Drug Abuse training grant (T320A037183), by the Australian Research Council under grant FL150100096, and by a Macquarie University Research Fellowship. The MIDUS study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development and by National Institute on Aging Grants AG020166 and AG051426, including support for the work of R.F.K. on this project. The funding bodies that supported this research did not have any role in the study design; collection, analysis or interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Declaration of Conflicting Interests: The authors declare no conflicts of interest with respect to the authorship or the publication of this article.
We also examined the association between the recession impacts and the CIDI-SF binary diagnostic variables for DSM-III major depressive episode, generalized anxiety disorder, and panic disorder (i.e., not including sub-threshold cases). The associations in Step 1 did not differ substantively from the analyses presented here (ΔOR < .1), so we included sub-threshold cases in our criterion variables to maximize sensitivity to population-level changes in mental health, to align with the alcohol and substance use outcomes, and to capture the fact that individual symptoms—not just meeting diagnostic criteria—predict impairment of psychosocial function (e.g., Fried and Nesse, 2014).
We tested measurement invariance for the internalizing and substance use latent variables separately, based on the recommended MPlus defaults for binary indicators and maximum likelihood estimation. Given the use of multiple imputation in the present study, we compared model fit for configural, metric, and scalar invariance models based on the sample size-adjusted Bayesian information criterion: Each additional set of constraints improved model fit by > 2 points.
Contributor Information
Miriam K. Forbes, Departments of Psychiatry and Psychology, University of Minnesota, USA, 55454 Centre for Emotional Health, Department of Psychology, Macquarie University, Australia, 2109.
Robert F. Krueger, Department of Psychology, University of Minnesota—Twin Cities, USA, 55455.
References
- Benjamini Y & Hochberg Y (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol, 57, 289–300. doi: 10.2307/2346101 [DOI] [Google Scholar]
- Bor J, Basu S, Coutts A, McKee M, & Stuckler D (2013). Alcohol use during the great recession of 2008-2009. Alcohol Alcohol, 48, 343–348. doi: 10.1093/alcalc/agt002 [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. (2017). Labor force statistics including the national unemployment rate. [Google Scholar]
- Burgard SA, Ailshire JA, & Kalousova L (2013). The Great Recession and Health. Ann Am Acad Pol Soc Sci, 650, 194–213. doi: doi: 10.1177/0002716213500212 [DOI] [Google Scholar]
- Cagney KA, Browning CR, Iveniuk J, & English N (2014). The onset of depression during the Great Recession: foreclosure and older adult mental health. Am J Public Health, 104, 498–505. doi: 10.2105/ajph.2013.301566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano R, Goldman-Mellor S, Saxton K, Margerison-Zilko C, Subbaraman M, LeWinn K, & Anderson E (2011). The health effects of economic decline. Annu Rev Public Health, 32, 431–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Central Intelligence Agency. (2017). Distribution of family income - Gini index. [Google Scholar]
- Chang S-S, Stuckler D, Yip P, & Gunnell D (2013). Impact of 2008 global economic crisis on suicide: time trend study in 54 countries. Br Med J, 347, f5239. doi: 10.1136/bmj.f5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, & Dagher R (2016). Gender and race/ethnicity differences in mental health care use before and during the Great Recession. The Journal of Behavioral Health Services & Research, 43(2), 187–199. [DOI] [PubMed] [Google Scholar]
- Colvin G (2018, July 19). The end is near for the economic boom. Fortune. Retrieved from http://fortune.com/longform/economic-expansion-end-is-near/ [Google Scholar]
- Dagher RK, Chen J, & Thomas SB (2015). Gender differences in mental health outcomes before, during, and after the Great Recession. PLoS One, 10, e0124103. doi: 10.1371/journal.pone.0124103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dee TS (2001). Alcohol abuse and economic conditions: evidence from repeated cross-sections of individual-level data. Health Econ, 10, 257–270. doi: 10.1002/hec.588 [DOI] [PubMed] [Google Scholar]
- Engemann K & Wall HJ (2010). The effects of recessions across demographic groups. Fed. Reserve Bank St. Louis Rev, 92, 1–26. [Google Scholar]
- Field AP & Wilcox RR (2017). Robust statistical methods: A primer for clinical psychology and experimental psychopathology researchers. Behav Res Ther. doi: 10.1016/j.brat.2017.05.013 [DOI] [PubMed] [Google Scholar]
- Frasquilho D, Matos MG, Salonna F, Guerreiro D, Storti CC, Gaspar T, & Caldas-de-Almeida JM (2016). Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health, 16, 115. doi: 10.1186/s12889-016-2720-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman DG (1999). A note on 'Economic conditions and alcohol problems'. J Health Econ, 18, 661–670. [DOI] [PubMed] [Google Scholar]
- Fried EI & Nesse RM (2014). The impact of individual depressive symptoms on impairment of psychosocial functioning. PLOS ONE, 9, e90311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glonti K, Gordeev VS, Goryakin Y, Reeves A, Stuckler D, McKee M, & Roberts B (2015). A systematic review on health resilience to economic crises. PLoS One, 10, e0123117. doi: 10.1371/journal.pone.0123117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haw C, Hawton K, Gunnell D, & Platt S (2015). Economic recession and suicidal behaviour: Possible mechanisms and ameliorating factors. Int J Soc Psychiatry, 61, 73–81. doi: doi: 10.1177/0020764014536545 [DOI] [PubMed] [Google Scholar]
- Hoynes H, Miller DL, & Schaller J (2012). Who suffers during recessions? J Econ Perspect, 26, 27–47. [Google Scholar]
- Jacobsen LA & Mather M (2011). A post-recession update on US social and economic trends. Population Bulletin Update, 12, 1–8. [Google Scholar]
- Kerr WC, Kaplan MS, Huguet N, Caetano R, Giesbrecht N, & McFarland BH (2017). Economic Recession, Alcohol, and Suicide Rates: Comparative Effects of Poverty, Foreclosure, and Job Loss. Am J Prev Med, 52, 469–475. doi: 10.1016/j.amepre.2016.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, & Wittchen H-U (1998). The World Health Organization Composite International Diagnostic Interview short-form (CIDI-SF). Int J Methods Psychiatr, 7, 171–185. doi: 10.1002/mpr.47 [DOI] [Google Scholar]
- Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, … Zaslavsky AM (2008). Individual and Societal Effects of Mental Disorders on Earnings in the United States: Results From the National Comorbidity Survey Replication. Am J Psychiatry, 165, 703–711. doi: 10.1176/appi.ajp.2008.08010126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsch JA & Ryff CD (2016). Hardships of the Great Recession and health: Understanding varieties of vulnerability. Health Psychol Open, 3, 2055102916652390. doi: 10.1177/2055102916652390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J Abnorm Psychol, 126, 454–477. doi: 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Lo CC & Cheng TC (2014). Race, unemployment rate, and chronic mental illness: a 15-year trend analysis. Soc Psychiatry Psychiatr Epidemiol, 49, 1119–1128. doi: 10.1007/s00127-014-0844-x [DOI] [PubMed] [Google Scholar]
- Margerison-Zilko C, Goldman-Mellor S, Falconi A, & Downing J (2016). Health Impacts of the Great Recession: a Critical Review. Curr Epidemiol Rep, 3, 81–91. doi: 10.1007/s40471-016-0068-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark TL, Hodgkin D, Levit KR, & Thomas CP (2016). Growth in spending on and use of services for mental and substance use disorders after the Great Recession among individuals with private insurance. Psychiatr Serv, 67, 504–509. doi: 10.1176/appi.ps.201500034 [DOI] [PubMed] [Google Scholar]
- McInerney M, Mellor JM, & Nicholas LH (2013). Recession depression: Mental health effects of the 2008 stock market crash. J Health Econ, 32, 1090–1104. doi: 10.1016/j.jhealeco.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Nandi A, Keyes KM, Uddin M, Aiello AE, Galea S, & Koenen KC (2011). Home foreclosure and risk of psychiatric morbidity during the recent financial crisis. Psychol Med, 42, 1441–1448. doi: 10.1017/S0033291711002613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modrek S, Hamad R, & Cullen MR (2015). Psychological well-being during the great recession: Changes in mental health care utilization in an occupational cohort. American Journal of Public Health, 105(2), 304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucci N, Giorgi G, Roncaioli M, Perez JF, & Arcangeli G (2016). The correlation between stress and economic crisis: a systematic review. Neuropsychiatr Dis Treat, 12, 983–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998-2018).Mplus User’s Guide. (Eighth Edition. ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Paul KI & Moser K (2009). Unemployment impairs mental health: Meta-analyses. J Vocat Behav, 74, 264–282. doi: 10.1016/j.jvb.2009.01.001 [DOI] [Google Scholar]
- Phillips JA & Nugent CN (2014). Suicide and the Great Recession of 2007-2009: the role of economic factors in the 50 U.S. states. Soc Sci Med, 116, 22–31. doi: 10.1016/j.socscimed.2014.06.015 [DOI] [PubMed] [Google Scholar]
- Pruchno R, Heid AR, & Wilson-Genderson M (2017). The Great Recession, life events, and mental health of older adults. Int J Aging Hum Dev, 84, 294–312. doi: doi: 10.1177/0091415016671722 [DOI] [PubMed] [Google Scholar]
- Radler BT (2014). The Midlife in the United States (MIDUS) series: A National longitudinal study of health and well-being. Open health data, 2, e3. doi: 10.5334/ohd.ai [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radler BT & Ryff CD (2010). Who participates? Longitudinal retention in the MIDUS National study of health and well-being. J Aging Health, 22, 307–331. doi: 10.1177/0898264309358617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves A, McKee M, & Stuckler D (2014). Economic suicides in the great recession in Europe and North America. The British Journal of Psychiatry, 205(3), 246–247. [DOI] [PubMed] [Google Scholar]
- Reeves A, Stuckler D, McKee M, Gunnell D, Chang S-S, & Basu S (2012). Increase in state suicide rates in the USA during economic recession. The Lancet, 380, 1813–1814. doi: 10.1016/S0140-6736(12)61910-2 [DOI] [PubMed] [Google Scholar]
- Riumallo-Herl C, Basu S, Stuckler D, Courtin E, & Avendano M (2014). Job loss, wealth and depression during the Great Recession in the USA and Europe. Int J Epidemiol, 43, 1508–1517. doi: 10.1093/ije/dyu048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruhm CJ (1995). Economic conditions and alcohol problems. J Health Econ, 14, 583–603. [DOI] [PubMed] [Google Scholar]
- Tsai AC (2015). Home foreclosure, health, and mental health: a systematic review of individual, aggregate, and contextual associations. PLoS One, 10, e0123182. doi: 10.1371/journal.pone.0123182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson LR (2016). Financial strain and mental health among older adults during the Great Recession. J Gerontol B Psychol Sci Soc Sci, 71, 745–754. doi: 10.1093/geronb/gbw001 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2011). Impact of economic crises on mental health Impact of economic crises on mental health. Copenhagen Ø, Denmark: WHO Regional Office for Europe. [Google Scholar]
- Yilmazer T, Babiarz P, & Liu F (2015). The impact of diminished housing wealth on health in the United States: Evidence from the Great Recession. Soc Sci Med, 130, 234–241. doi: 10.1016/j.socscimed.2015.02.028 [DOI] [PubMed] [Google Scholar]
- Zivin K, Paczkowski M, & Galea S (2011). Economic downturns and population mental health: research findings, gaps, challenges and priorities. Psychol Med, 41, 1343–1348. doi: 10.1017/s003329171000173x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.