Abstract
Women with Turner syndrome (TS) have a high morbidity from both medical and psychological conditions with a negative impact on quality of life (QoL). Physical activity is a modifiable behavior shown to reduce risk for these chronic medical and mental health conditions and enhance QoL in other populations. Limited research suggests that adolescents and women with TS are less likely to engage in or enjoy physical activity than peers. This mixed methods study aimed to document physical activity levels in a sample of youth with TS and explore how factors unique to TS contribute to and are affected by physical activity. A cross-sectional sample of 21 girls (12–21 years) with TS and their parents (n=21) completed standardized questionnaires to quantify habitual physical activity (3-Day Physical Activity Recall) and QoL (PROMIS) and participated in individual interviews focused on their experience with physical activity. Quantitative and qualitative results were synthesized using a phenomenological mixed methods approach. Results indicate that our sample engaged in less physical activity than peers and only 19% met recommendations for one hour per day of moderate-to-vigorous physical activity (MVPA). Parents reported significant problems with peer relationships and psychological stress, and peer relationships scores correlated with physical activity. Reported barriers to physical activity included physical and psychosocial complications related to TS as well as unique developmental considerations specific to adolescence. Quantitative and qualitative results supported that structured fitness options embedded into routines enhanced activity levels. Results were compiled into specific recommendations for clinical care and areas of future research.
Keywords: Turner syndrome, sex chromosome aneuploidy, gonadal dysgenesis, physical activity, quality of life, health behavior
1. INTRODUCTION
Turner Syndrome (TS), defined as females with a partial or complete absence of the second sex chromosome, occurs in ~1 of every 2,000 female births. TS classically manifests with short stature and ovarian insufficiency, but the missing genetic material can affect every system. Epidemiological data suggest mortality related to diabetes and cardiovascular disease (CVD) conditions is three times greater in women with TS, (Schoemaker et al., 2008; Stochholm, Juul, Juel, Naeraa, & Gravholt, 2006) and obesity, hypertension, dyslipidemia, and dysglycemia are prevalent (Gawlik, Gieburowska, & Malecka-Tendera, 2015; Mavinkurve & O’Gorman, 2015). Females with TS also have a higher risk of psychosocial deficits with half affected by anxiety (Hutaff-Lee, Bennett, Howell, & Tartaglia, 2019) and quality of life (QoL) is significantly impaired by social isolation (Amundson, Boman, Barrenas, Bryman, & Landin-Wilhelmsen, 2010). The international guidelines for the care of women and girls with TS recommend screening for CVD-related conditions and psychosocial problems starting in childhood (Gravholt et al., 2017), however there is a paucity of research on prevention of these risks in TS.
Modifiable behavioral risk factors, particularly physical activity, are inversely correlated with the development of CVD precursors in multiple populations (Abrignani et al., 2019). Physical activity intervention studies have shown positive effects on inflammatory markers, blood pressure, lipids, and insulin sensitivity in youth (Palve et al., 2014; Sirico et al., 2018). In addition to prevention of CVD and lowered risk of chronic medical conditions, there are recognized benefits of physical activity on lowering risk for anxiety and depression, improving sleep, and positively influencing QoL (Biddle & Asare, 2011; Kredlow, Capozzoli, Hearon, Calkins, & Otto, 2015; Riiser et al., 2014; Wu et al., 2017). The World Health Organization, US Department of Health and Human Services, and the National Heart, Lung, and Blood Institute Expert Panel Integrated Guidelines all recommend adolescents get a minimum of 60 minutes of moderate to vigorous physical activity (MVPA) per day (“Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report,” 2011; “WHO Guidelines Approved by the Guidelines Review Committee,” 2010).
Physical activity recommendations are particularly important for individuals at higher risk for CVD and mental health conditions, such as TS. While the international TS clinical care guidelines encourage physical activity, there is minimal research in this arena (Gravholt et al., 2017). Self-reported physical activity in Polish adolescents with TS found that only 19% were meeting the recommended level of physical activity per week. In that study, 25% were disqualified by physicians from physical education classes (likely due to cardiac restrictions) and another 30% disliked physical education classes (Sienkiewicz-Dianzenza, Milde, & Frac, 2006; Sienkiewicz-Dianzenza, Milde, Tomaszewski, & Frac, 2011). Similarly, a study from Norway reported women with TS were less likely to have enjoyed physical activity in childhood compared to controls (Naess, Bahr, & Gravholt, 2010). More recently, a study of 16 adolescents with TS found both self and parent-reported QoL was impaired in multiple domains, including physical functioning (Amedro et al., 2017). These few studies raise many more questions as to why girls with TS are not engaging in physical activity, what impact this has on their health and QoL, and how we can target improvement for this important preventative health behavior.
Based on clinical experience and the limited research in this area, we hypothesized that physical activity level would be low in adolescent girls with TS and that experiences unique to TS would both contribute to and be affected by physical activity. In this mixed methods study, we aimed to investigate these questions through quantitative assessment of physical activity levels and related domains of QoL together with a qualitative assessment of the lived experience of girls with TS. This novel approach allows for convergence of results with direct implications for clinical care.
2. METHODS
2.1. Study Design
The current study utilized a convergent parallel mixed methods design in order to both test and generate hypotheses (Creswell & Clark, 2017). A cross-sectional study of daily activity and quality of life was conducted with a sample of adolescent girls and young adults with TS and their parents. Simultaneously, participants were interviewed in a qualitative phenomenological strand of inquiry. An integration of statistical and thematic results was used to cross-validate and confirm findings (Figure 1).
Figure 1.
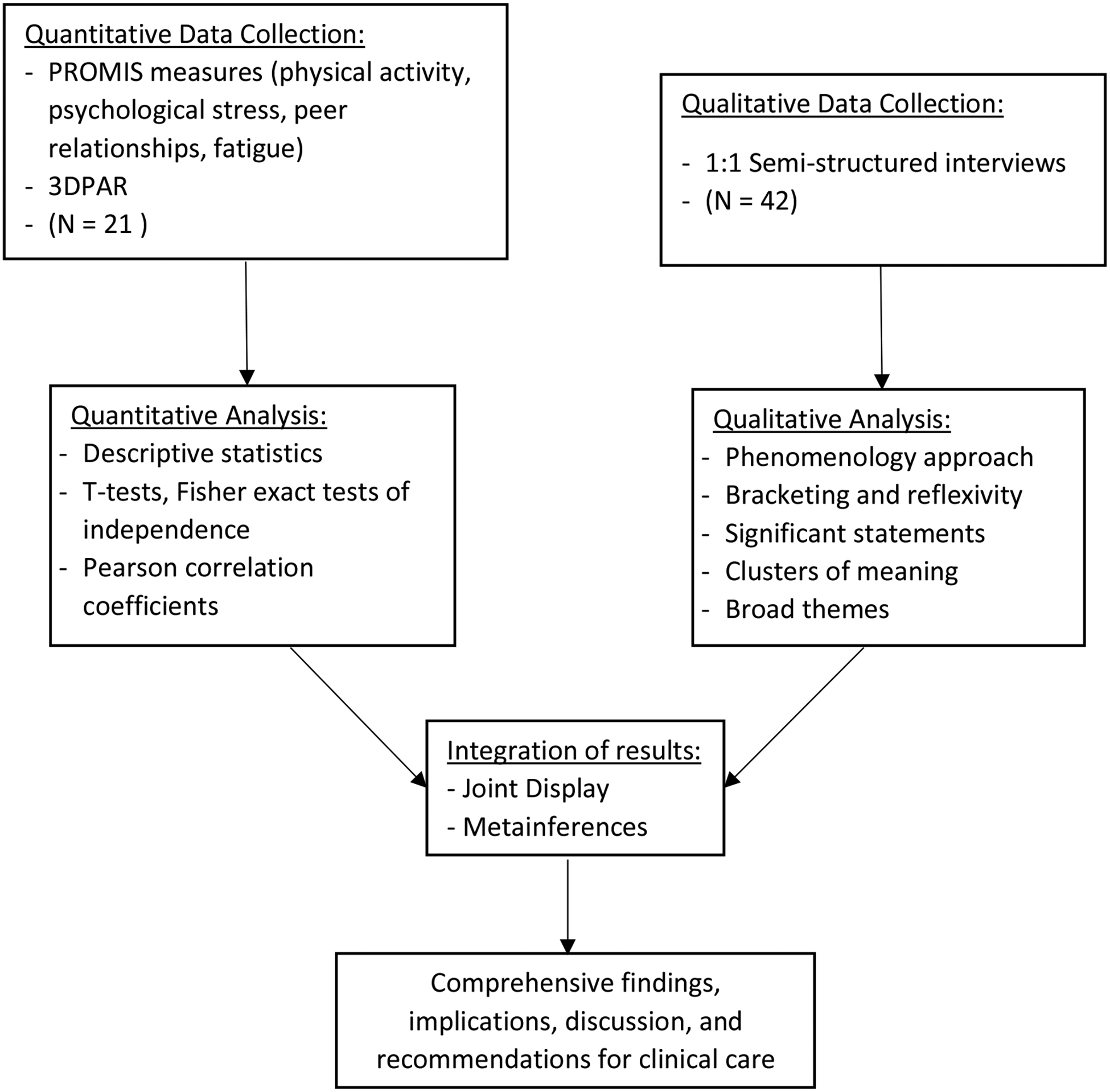
Concurrent mixed methods study design.
2.2. Participant Recruitment and Ethical Compliance
Adolescent participants were recruited from the local multidisciplinary TS clinic, endocrine clinic, and advertisement through regional parent support groups for a study of health, fitness, and quality of life at the University of Colorado from 2017 to 2018. Inclusion criteria were as follows: adolescent girls age 12–21 with TS confirmed by karyotype with at least 50% of cells tested having a TS-specific karyotype. Participants had to have had spontaneous puberty or be on estradiol replacement. The larger study protocol involved direct assessment of insulin resistance and physical fitness, therefore exclusion criteria included growth hormone treatment within the past two weeks, diagnosis of diabetes, untreated hypertension, body weight more than 300 pounds, height less than 54 inches, aortic dilation, and other cognitive, psychiatric, or physical impairment resulting in the inability to tolerate study procedures, including vigorous exercise. For each adolescent participant, one parent was invited to participate as well. All participants and/or a parent provided written consent and/or assent as appropriate for age. This study was approved by the Colorado Multiple Institutional Review Board (COMIRB #17–0142) and published on clinicaltrials.gov (NCT03181230) on June 8, 2017 prior to first participant enrollment.
2.3. Data Collection
Quantitative Procedures.
Medical history including karyotype, age of TS diagnosis, relevant chronic medical conditions, medications were collected via interview and review of medical records. Participants were asked if they currently participate in any organized physical activities, such as sports. Youth completed the 3-day physical activity recall (3DPAR) questionnaire, a validated questionnaire designed to capture the physical activity habits of adolescents. The 3DPAR has been validated in the general population of adolescent girls, showing significant correlations between self-reports of behavior and objective accelerometer assessments (r = 0.27–0.46; P < 0.05) (Pate, Ross, Dowda, Trost, & Sirard, 2003). Participants were asked to rate their behavior in terms of activity and intensity in 30-minute blocks of time between the hours of 6:00am and midnight over the previous three days. The reported activities were converted to metabolic equivalent (MET) levels using the published manual. Activities ≥4 MET were categorized as moderate-to-vigorous physical activity (MVPA). Total time spent in MVPA for each day was added together and was averaged between the three days. Participants who averaged 60 minutes/day or more of MVPA were considered to be meeting recommendations.
Parents completed parent proxy ratings and youth completed self-reporting questionnaires on domains of QoL determined to be relevant for physical activity. Four QoL domains were administered from the Patient-Reported Outcomes Measurement Information System (PROMIS): Physical Activity (v1.0 short form 8a), Fatigue (v2.0 short form 10a), Peer Relationships (v2.0 short form 8a), and Psychological Stress Experiences (v1.0 short form 4a) (Bevans et al., 2018; Dewalt et al., 2013; Lai et al., 2013; Tucker et al., 2014). The research team chose these measures based on prior TS research and a priori hypotheses that physical fatigue (potentially associated with body habitus or chronic health issues), psychological stress (anxiety), and social relationships were all vulnerable areas in girls with TS and could potentially contribute both to their level of engagement in physical activities and their experiences with physical activity. For each PROMIS domain, participants respond on a Likert scale to a series of questions representing the past week. PROMIS measures provide T-scores normed to the general population with a mean of 50 and standard deviation of 10; higher scores indicating more of the concept being measured (e.g., more fatigue or more physical activity).
Qualitative Procedures.
Three research team members conducted one-on-one semi-structured interviews with 21 adolescent girls with TS and each of their parents for a total of 42 interviews. Interviews took place during study visits at Children’s Hospital Colorado (CHCO) and lasted an average of 24 minutes (21 minutes for TS patients, 27 minutes for parents). The interview protocol (available upon request) consisted of eight open ended questions and 20 possible follow-up probes designed to elicit thoughts, perceptions, and feelings on physical activity and TS. Interviews were fluid, allowing for interviewers and interviewees to expand and elaborate on the protocol. Interviews were conducted in a private, quiet setting, the interviewer took notes during the interview, and the discussion was audio recorded.
2.4. Analytic Strategy
Quantitative Analysis.
Data were reviewed for outliers and missing data; all questionnaires were complete with no missing data and there were no outliers excluded. Normality was evaluated visually by plotting and with the Shapiro Wilk test to determine whether to use parametric or non-parametric tests. Descriptive statistics were used to summarize data with either mean ± standard deviation (SD) or median with interquartile range (IQR) as appropriate. Fischer exact test was used to calculate the odds of meeting recommendations for MVPA depending on whether or not they participated in sports. PROMIS T-scores were compared to the normative population (theoretical median 50) by one-sample Wilcoxon rank sum tests for each domain. Adolescent and parent-proxy T-scores were compared for each domain using Wilcoxon matched-pairs rank sum test. Spearman Correlation Coefficients were used to evaluate for linear relationships between Physical Activity and the other PROMIS domains or demographic covariates; a correlation coefficient of > 0.7 signified a strong correlation, while an r value between 0.4 and 0.6 signified a moderate correlation. Significance was set at an alpha of 0.05. Statistics were conducted with Prism Graphpad v8.1.2.
Qualitative Analysis.
Interviews were audio recorded and verbatim transcribed before being uploaded into ATLAS.ti v 8.3.1 software for data management and analysis. Research team members trained in qualitative methods used a phenomenological approach to analysis (Moustakas, 1994). In phenomenology, it is critical that researchers “bracket” their personal experiences in order to understand the essence of a phenomenon from the perspective of those experiencing it (Giorgi, 2009). Therefore, team members met prior to analysis to discuss subjectivities related to their personal experiences and roles with TS (e.g., physician, genetic counselor, clinic coordinator, psychologist, affected family member). This reflexivity is critical in qualitative research in order to address any biases or personal goals that may impact interpretation (Tracy, 2010). Further, each rater listened to interview audio recordings and read through interview transcripts several times to immerse themselves in the data. Next, horizonilization was used to identify “significant statements” directly from participant responses (Creswell & Clark, 2017). Subsequently, these statements were reduced into clusters of meaning and finally into broad emergent themes describing the essence of physical activity for adolescent girls with TS. Triangulation was used to compare and contrast data from youth and parent interviews to establish trustworthiness and assure all perspectives were represented (Tracy, 2010). Raters met multiple times to assess inter-rater agreement on clusters and themes and to collectively determine nomenclature used in data representation. Any differences in interpretation of data were discussed until group consensus was met. Finally, member checking of synthesized themes was conducted with both a parent and a young adult with TS to test whether conclusions were trustworthy and transferable to the population of study (Carlson, 2010). Both readers reported that the themes accurately represented experiences of the TS community.
Mixed Methods Analysis.
After completing the quantitative and qualitative analyses separately, the research team met to review both sets of data, linking results for a more robust understanding of physical activity in TS. A joint display (interpretive matrix) was developed to compare and contrast the phenomenological themes with statistical results (Fetters, Curry, & Creswell, 2013; Guetterman, Fetters, & Creswell, 2015; Mayoh & Onwuegbuzie, 2015). Areas of congruence were highlighted; qualitative data (direct quotes from participants) were used to confirm statistical results. Qualitative results that expanded upon quantitative data were used to explain the how and why of specific quantitative constructs. Examples of discordance between data sets were noted and explored for content and methodological considerations.
3. RESULTS
3.1. Demographics
Twenty-one females 13 to 21 years of age enrolled in and completed the study (Table 1). The majority of participants were diagnosed with TS postnatally with the most common reasons for genetic testing being dysmorphic features at birth and short stature in childhood. Ultrasound anomalies led to genetic testing in 6 of the 7 girls diagnosed prenatally. Just over half had a non-mosaic 45,X, three were mosaic with a typical 46,XX cell line, and other karyotypes included 45,X/47,XXX (n=1), 45,X/46,XidicY (n=1), 45,X/46,XidicX (n=1), 46,XidicX (n=2), 46,XdelXq (n=1).
Table 1.
Characteristics of Participants
| N=21 | |
|---|---|
| Age (yrs) | 17.3 ± 5.5 |
| Height (cm) | 150.5 ± 8.1 |
| Race/Ethnicity | |
| Non-Hispanic White | 15 (72%) |
| Hispanic White | 3 (14%) |
| Other/more than one race | 3 (14%) |
| Karyotype | |
| 45,X (non-mosaic) | 12 (57%) |
| 45,X/46,XX | 3 (14%) |
| Other TS karyotype | 6 (29%) |
| Postnatal TS Diagnosis | 14 (67%) |
| Age (yrs), median (range) | 7 (0–17) |
| Post-Menarchal | 17 (81%) |
| Age of menarche (yrs) | 14.2 ± 1.5 |
| Chronic medical conditions | |
| Congenital heart disease | 8 (38%) |
| Obesity (BMI >95%ile) | 4 (19%) |
| Hypertension | 2 (10%) |
| Autoimmune condition | 4 (19%) |
| Asthma | 2 (10%) |
| Mental health diagnosis | 11 (52%) |
| Medications | |
| History of growth hormone | 18 (86%) |
| Estradiol | 19 (90%) |
| Antihypertensive | 2 (10%) |
| Antidepressant | 3 (14%) |
| Organized physical activity | 6 (29%) |
Data are mean ± SD, median (IQR), or n(%)
At the time of the study, most of the participants were on hormone replacement therapy and had reached menarche. Per the study design, no one was on growth hormone at the time of the study however almost all been on growth hormone previously and the average height corresponded to the 6th percentile for adult women. Over half of the participants had a diagnosis of a mental health condition with anxiety and attention deficit disorder being the most prevalent.
3.2. Quantitative Results
Six of the 21 participants (29%) reported being currently or recently involved in organized sports; the list of activities included martial arts, running club, tennis, cheer, gymnastics and diving. The median time spent in MVPA daily was 20 (0–51) minutes. Only four girls (19%) averaged 60 or more minutes of MVPA daily and only two (10%) had 60 minutes or more of MVPA on all three days captured. All four girls who averaged 60 minutes/day of MVPA were in organized physical activity (OR 95% CI 3.1-infinity for meeting physical activity recommendations if in sports, p=0.003). Physical Activity assessed via the PROMIS QoL instruments found significantly lower physical activity than the general population by both self and parent-proxy report (Figure 2). This assessment correlated with time spent in MVPA for both adolescent (r=0.69, p<0.001) and parent (r=0.55, p=0.009) reported physical activity, supporting measure validity. A weak-to-moderate relationship between height and physical activity approached significance (r=0.40, p=0.072 for time spent in MVPA and r=0.18, p=0.050 for parent PROMIS Physical Activity with height). Age, karyotype, race, and medical/psychiatric diagnoses were not associated with either time spent in MVPA or PROMIS Physical Activity scores.
Figure 2.
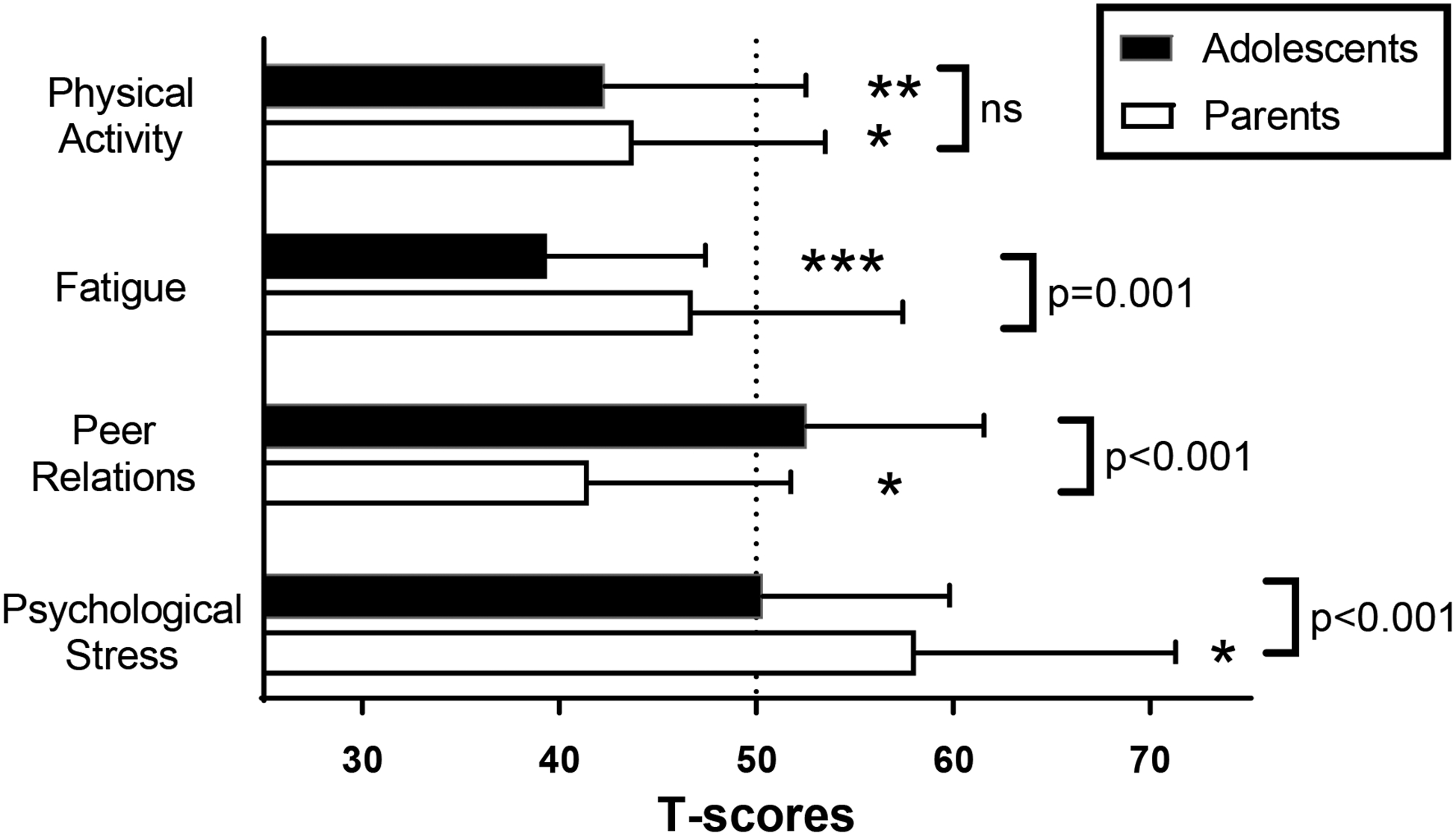
PROMIS quality of life (QoL) domains for self-report by adolescents (black) and proxy-report by parents (white). Asterisks represent a difference compared to a normative population (T score of 50) by one-sided Wilcoxon signed rank test at a significance level of *p<0.01, **p<0.001, ***p<0.0001. Brackets represent the comparison between adolescent and parent-report within a given domain by Wilcoxon matched-pairs signed rank test.
Results for the PROMIS QoL questionnaires are displayed in Figure 2. Adolescent self-report and parent-proxy report were discordant for all domains measured aside from Physical Activity. Parents were more likely to report their daughters had problems in the domains of Peer Relationships and Psychological Stress Experiences, but neither adolescents nor parents reported difficulties with Fatigue. In fact, girls with TS reported significantly lower levels of fatigue than the normative PROMIS sample. PROMIS Physical Activity T-scores had a moderate correlation with Peer Relationships (r=0.44, p=0.045), but not with measures of Fatigue and Psychological Stress Experiences (p>0.05 for all).
3.3. Qualitative Findings
Raters identified over 600 significant statements in the interview transcripts, which were then reduced into seven clusters of meaning and finally three broad overarching themes: “Differences in motivation for physical activity”, “Barriers to physical activity in TS”, and “Structured fitness options facilitate physical activity.” See Table 2 for examples of significant statements that exemplify each theme.
Table 2.
Broad Themes, Clusters of Meaning, Significant Statements.
| Theme 1: Differences in motivation for physical activity | |
|---|---|
| Youth: Social motivation | Parents: Health benefits |
| Youth: “I prefer more people because it motivates me. I’m just by myself, then I’m just like there’s no one to push me or keep me going.” | Parent: “I know that TS sets her up for being predisposed to a lot more health problems than a typical girl her age would have. So I feel like it’s even more important for her because if she doesn’t stay physically active she is going to deteriorate at a much earlier age and have lots more health issues.” |
| Youth: “If I go with a friend it would be really exciting, and then I look forward to [exercise].” | |
| Parent: “She’s a social girl and she wants to do that. It’s just hard to find those girls in this age group - nice girls.” | Parent: “The benefits that I’ve been promoting are her mental health. To find this motivation, to help her understand that it’s not just about losing weight… that physical activity makes you feel good.” |
| Youth: “I don’t know what the feeling of just exercising alone does, I just don’t like the feeling. I like having someone there with me.” | |
| Theme 2: Barriers to physical activity in TS | ||
|---|---|---|
| Physical factors of TS | Psychosocial factors of TS | Developmental considerations |
| Youth: “It’s just the general fatigue. So, if I did maybe like a five-minute or a little less than five-minute workout every day I think I’d be fine.” | Youth: “I would probably go more often, but I would think about it and I would stress out and I would not go by myself because of my anxiety.” | Youth: “Just time and how young I am. I can’t go somewhere by myself and just [exercise] which makes it kind of hard. Not having the time because I have to run around all the time. With school and everything, like homework.” |
| Youth: “I don’t mind sports, but the main reason I’m not in any sports is because I feel I would pummeled. It’s kind of hard to make sure you don’t get really really hurt and be this small.” | Parent: “Learning to get on that bike was weeks of preparing her mentally to get on the bike because there was 400 reasons of why she was going to die or whatever. Just a lot of tapes in her head going about everything.” | Parent: “Since everyone was struggling at the beginning, it was really nice for her. They all kind of learned together. She learned a lot of gymnastics type stuff as a kid. Then it took a turn where everyone got better and she kind of peaked and flattened out.” |
| Youth: “Since I’m a little bit shorter it’s kind of hard to keep up with everyone else.” | Parent: “She just couldn’t quite grasp what to do or how to move.” | |
| Parent: “I have my own anxiety about her heart exploding and dying.” | ||
| Theme 3: Structured options facilitate physical activity | |
|---|---|
| Embedding activity into a routine | Desire for clear recommendations from doctors |
| Parent: So because it was part of her schedule, it made it easier for her to do it. As opposed to getting home, that’s like her leisure time, being at home. So I think that’s what it was. It was made to be a part of her routine.” | Parent: “If the doctor would just say, ‘Here, okay. Since you have Turner syndrome, I want you exercising three days a week, and this is what I would like you to do. A light aerobic.’ Or whatever. And just come up with a plan.” |
| Youth: “I usually go to the gym one or two times a week for classes or meeting with a personal trainer. That’s usually when I exercise.” | Youth: “I mean, maybe helping the patient find a good activity that fits them and their lifestyle and their home life and stuff.” |
Differences in motivation for physical activity.
Girls with TS and their parents differed in opinions on the benefits of exercise. Adolescent interviews revealed a strong preference for engaging in exercise with others (peers and family members) to make the work more fun and to avoid feelings of loneliness. While a few of the girls admitted to feeling awkward or inadequate when exercising with peers, most reported that they were more likely to be physically active with social encouragement and as an opportunity to spend time with others. Social physical activities included hiking with family on the weekends, biking with siblings, working out at the gym with a friend, being a part of a sports team, or taking a fitness class.
Parents were more likely to describe the physical and mental health benefits of exercise. Many parents referred to documented physical and psychological risks associated with TS as the reason they most wanted their daughters to increase activity levels. Specifically, parents reported the hope that exercise could mediate the risk of heart problems, reduce weight gain, combat stress and anxiety, and build self-esteem and confidence.
Barriers to physical activity in TS.
Interviewees described three major barriers to physical activity. First, physical limitations related to TS were frequently cited by both girls and their parents. Short stature was listed as a challenge associated with running and trying to keep up with taller peers and siblings. Several parents mentioned clumsiness and motor coordination problems related to TS that made it difficult for their daughters to learn new exercise routines or skilled sports. In contrast with the quantitative results, fatigue was the most frequently reported physical limitation, with many parents and girls describing their exhaustion after a long day at school or work and a tendency to tire easily during physical activity.
Second, psychosocial aspects of TS that interfered with physical activity were also reported by a number of parents and occasionally by the girls themselves. Specifically, anxiety was cited as interfering with motivation to try new activities (e.g., learning to bike, starting a new exercise class, working out alone) or engage in competitive sports. Further, specific cognitive deficits in visual spatial reasoning were also reported by parents as contributing to physical problems with motor coordination.
Finally, participants described several developmental considerations for physical activity in adolescence. Most girls and parents reported they engaged in significantly more physical activity in childhood through organized, recreational sports and daily unstructured, physical play with friends. As the girls grew older, sports became more competitive and the gap in skills widened between teens with TS and their peers, with recreational options being less available. Further, adolescence is marked by higher demands in school and work, which the girls and their parents often described as difficult to balance with a commitment to physical activity. Several parents noted that visual spatial deficits precluded their daughters from learning to drive, and that a lack of transportation interfered with their ability to participate in some activities. Finally, parents and some girls cited transitioning off growth hormone and/or starting estrogen may compound the typical physical and emotional changes that are occurring during puberty and this may pose challenges to physical activity unique to TS during this critical stage of development.
Structured fitness options facilitate physical activity.
Girls and their parents reported that adding structure encouraged more physical activity. Physical movement embedded into a daily routine was mentioned by many parents as a strategy to promote activity. For example, parents reported making daily walks a part of the family routine, parking farther away from a destination than necessary to encourage more walking, and purchasing a family gym membership with regularly scheduled family workout sessions. Youth with TS also reported the importance of routine daily movement, for example an active work environment/job setting, walking the family dog as an evening chore, working with a personal trainer each week, and intentionally registering for physical education classes in school.
Both youth and parents described a desire for clear and individualized exercise recommendations and support from the medical community, around which they could structure their activity plans with confidence. Fear of potential harm from overdoing exercise was reported by several participants, as was a need for clarification on what types of exercise were the most helpful for a patient with TS. Recommendations for doctors also included suggestions to create pamphlets or videos encouraging exercise and affirming positive body image concepts as well as creating exercise groups, classes, or monitoring programs for girls with TS.
3.4. Mixed Methods Results
Data sets were analyzed to assess confirmation, expansion, or discordance of qualitative findings with statistical results. The linked data sets provided 11 key, clinically relevant meta-inferences (Johnson, Onwuegbuzie, & Turner, 2007). Figure 3 depicts a joint display of the data and the relationships between quantitative constructs and qualitative themes.
Figure 3.
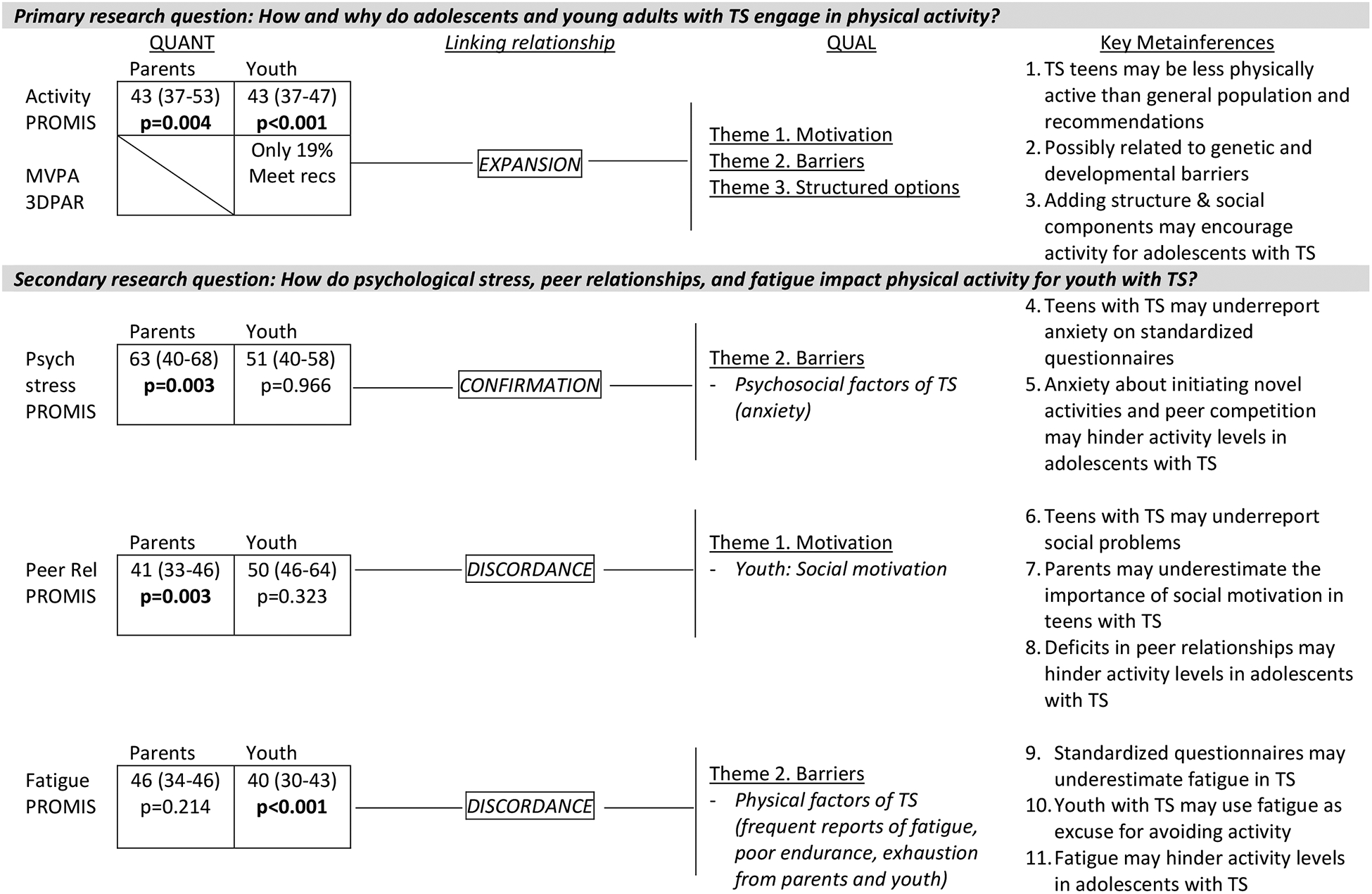
Joint Display synergizing quantitative with qualitative findings. Results for all PROMIS measures are the median (IQR) of T-scores, with 50 being normal. Bold indicates significant results.
4. DISCUSSION
The current study is the first to demonstrate lower levels of physical activity in adolescents with TS by both parent and child report and to investigate reasons for reduced activity levels through qualitative methods. These data are critical to addressing the high morbidity and mortality from CVD and other chronic conditions in TS through the preventative measure of increasing physical activity. These findings can be used by researchers and providers to guide clinical care recommendations and ultimately improve quality of life for individuals with TS.
Results indicate that parents and youth report significantly less physical activity than a normative sample on standardized questionnaires, and that a minority of adolescents with TS were meeting recommendations for MVPA, the type of physical activity known to have the greatest benefits on physical and mental health outcomes (Kraus et al., 2019; Sogut et al., 2019; “WHO Guidelines Approved by the Guidelines Review Committee,” 2010). These results confirm prior research in Europe indicating that fewer than 20% of adolescents with TS meet recommended activity levels (Sienkiewicz-Dianzenza et al., 2006), but are at odds with the much higher rates of physical activity found in a sample of girls with TS attending summer camp (Sienkiewicz-Dianzenza et al., 2011). Previous studies have not explored possible reasons for decreased activity in the TS population. A thorough understanding of the reasons why youth with TS may lead a more sedentary lifestyle is required in order to develop meaningful and relevant clinical care recommendations.
Reported barriers to physical activity for youth with TS included physical and psychosocial complications related to TS (e.g., short stature, fatigue, anxiety, visual-spatial deficits) as well as developmental considerations that arise in adolescence (e.g., widening of gap with peer skill levels, transition off growth hormone, increased time demands from school and work, fewer opportunities for noncompetitive recreation.) Parents and youth described that structured fitness options embedded into a routine enhanced their activity levels. Congruent with this was the finding that girls who participated in organized physical activities were the only ones who met recommendations for MVPA, and suggests that finding organized physical activity opportunities may combat some of the barriers to engaging in physical activity. Many expressed a desire for clear and individualized exercise plans and increased support from the medical community. Importantly, several parents reported confusion over the safety of physical activity for their daughter as it related to her heart, which is supported by Sienkiewicz-Dianzenza et al., who reported physicians excluded 1 in 4 adolescents with TS from participating in school physical education classes (Sienkiewicz-Dianzenza et al., 2006). Although the risk of aortic dissection is higher in TS than the general population, the consensus is that moderate intensity physical activity is safe for the vast majority of girls with TS (Gravholt et al., 2017) and may be beneficial even among individuals with thoracic aortic disease according to a recent systematic review (Thijssen et al., 2019). Clinical implications and recommendations based on key meta-inferences from mixed methods joint analysis are listed in Table 3.
Table 3.
Clinical recommendations for supporting adolescents with TS in physical activity
| Clinical Recommendations | Justification† |
|---|---|
| For Medical Providers | |
| Assess habitual physical activity levels in adolescent patients with TS. | 1, 2 |
| Provide families and schools with a letter stating clear and specific individualized recommendations for physical activity including goals and any restrictions. | 1, 2, 3 |
| Recognize the tendency for adolescents with TS to underreport psychosocial concerns; multiple sources (e.g., clinical interviewing, parent/teacher surveys, standardized rating forms) provide more accurate assessment of current functioning. | 4, 6, 9, 10 |
| Utilize motivational interviewing to support well-being and encourage patient-initiated behavior change toward increased physical activity. | 1, 2, 5 |
| Screen for and treat mental health conditions, including anxiety and social isolation, that may interfere with an adolescent’s ability to participate in physical activity. | 2, 5, 10 |
| For Girls and Families | |
| Create an active lifestyle by embedding physical activity into daily routine (e.g., add PE coursework to daily school schedule, participate in walking/running fundraisers to support causes of interest, assign chores that encourage movement, volunteer in childcare or other active settings, help coach young children’s sports teams). | 3, 11 |
| Implement positive behavior supports such as self-monitoring and positive reinforcement for physical activity (e.g., visible daily checklists for physical activity for all family members with social/group rewards upon completion of preset goals). Goals should be measurable (e.g., minutes spent in activity, steps per day as measured by personal tracking device, heartrate levels during exercise), starting small with incremental growth to assure early success. | 3, 5 |
| Consider online exercise communities to address the juxtaposition of social motivation and social anxiety/peer relationship problems surrounding exercise in TS, in addition to transportation, financial, and other barriers to in-person group classes. | 3, 5, 6, 7, 8 |
| Make a plan for how to recover if goals are not met (e.g., encourage positive self-talk, reset goals, implement novel reinforcement strategies, identify barriers). Develop family mottos such as: “Some physical activity is better than none” and “Health, not perfection, is the goal.” Seek psychological/counseling support as needed. | 2, 5 |
| Downplay competition between family members and/or peers and encourage girls to feel empowered by meeting their personalized goals for daily movement. | 5, 7, 8 |
| Be proactive at bringing up physical activity with medical providers, particularly if goals or limitations are unclear. | 2 |
| Support trying new activities and get help for anxiety, if present. | 4, 5 |
| For Educators and Therapists | |
| Early and continuous occupational therapy targeting areas of vulnerability in TS, in particular visual-spatial and motor planning skills, may reduce barriers for physical activity in adolescents. | 1, 2 |
| Physical education teachers and school counselors should play an active role in school support plans (IEP or 504 Plan) for youth with TS. They should be informed of the unique features and needs surrounding physical activity in TS and assist annually in developing a coursework plan with any required accommodations for physical activity at school. | 1, 2, 3 |
| Occupational and physical therapists should consider a push-in model and/or consultation-based services to partner with physical education teachers in order to understand what sports and skills are covered in the curriculum, to provide suggestions for how to support girls with TS as they learn new skills, and to address any appropriate accommodations or modifications necessary for participation. | 2, 5 |
| Provide explicit motor learning for sports/exercise routines (e.g., verbally mediated instructions and feedback for motor learning). | 2, 5 |
| School-based mental health providers should be made aware of issues with anxiety related to physical activity in students with TS and provide school-based supports as necessary (e.g., positive behavior support plans for participation, teach strategies to manage anxiety at school). | 2, 5, 8, 10 |
Numbers indicate key metainferences from MM joint analysis (see Figure 3)
A mixed methods approach provided novel insights about the impact of the TS psychosocial phenotype on activity levels. Specifically, parents reported significant psychological stress and troubled peer relationships on PROMIS questionnaires, and the Peer Relationships domain had a moderate linear relationship with physical activity levels. Although youth participants rated themselves in the typical range for psychological stressors and peer relationships on the surveys, in the open-ended interviews some reported that anxiety interfered with their participation in physical activities. Further, youth expressed a clear social motivation for participating in exercise, indicating a complicated relationship between the variables of physical activity, peer relationships, and stress symptoms; whereby compromised social skills and peer relationships may negatively impact physical activity if it is a socially motivated behavior. Future research is needed to test this hypothesis and to further examine social relationship problems in TS during adolescence, as it is unclear whether parent reported problems are attributed to underlying social skill deficits in TS or are a result of social rejection from peers who fail to accept differences in girls with TS during a life stage where fitting in is a primary objective. Additionally, although youth and parents reported typical levels of fatigue on the PROMIS questionnaires, fatigue was frequently reported as a barrier to exercise in the open-ended interview strand of data collection (42% of youth, 19% of parent interviews). Possible reasons for the fatigue discrepancies between data strands are 1) social desirability bias in survey responses(Van de Mortel, 2008) versus a more open and informal interview setting, 2) the PROMIS fatigue assessment may not accurately capture the fatigue associated with physical activity in this population, and 3) youth may use fatigue as an excuse for a more complicated or sensitive barrier to exercise (e.g. lack of exercise partners, mood problems/depression, anxiety about performing difficult new physical movements).
There has been minimal research into preventions or interventions in TS aside from hormone treatments. This study investigates the level of engagement and barriers to engagement for physical activity, a promising preventative health behavior that is grossly understudied in TS but has proven efficacious in other populations with similar comorbidities, including those at risk for CVD, osteoporosis, and mental health conditions (Bullard et al., 2019; Quirk, Blake, Tennyson, Randell, & Glazebrook, 2014). Use of a convergent parallel mixed methods design has provided unique multidimensional perspectives to examining physical activity engagement in TS and has generated both immediate recommendations for clinical practice (Table 3) as well as future research questions. The greatest limitation to this study is the generalizability as all of the participants were willingly participating in a study that involved an exercise portion and had height and medical restrictions, therefore findings may be different (or more expansive) in girls with TS who did not participate. Further, this study used tools to report, rather than directly measure, physical activity. While these instruments are shown to correlate, there is a great deal of variability (Pate et al., 2003), and future studies should include direct measure of physical activity. Due in part to recruitment difficulties, quantitative analyses were underpowered to test a model for multiple predictors of physical activity levels, however our sample size was adequate for the analyses conducted and our qualitative themes reached saturation. With these limitations in mind, this study adds to the existing literature for physical activity and QoL in adolescents with TS.
In conclusion, girls with TS do not engage in adequate physical activity due to multiple barriers. Recognizing and targeting these barriers early and systemically may improve physical activity engagement in girls with TS, ultimately preventing comorbidities such as CVD and mental health disorders. Immediate recommendations for clinical practice were generated from this study but additional translational research is needed to implement these findings and test generated hypotheses.
ACKNOWLEDGEMENTS
The authors wish to thank all the participants, Turner Syndrome Global Alliance for providing funding for this study, Turner Syndrome Colorado for advertising, and support from the eXtraOrdinarY Kids Turner Syndrome multidisciplinary clinic and research team. We also want to acknowledge Marybel Good and Isani Singh for their contributions to this manuscript. Dr. Davis is supported on a Career Development Award through the NICHD (K23HD092588-01).
FUNDING:
Turner Syndrome Global Alliance (TSGA) Fellow Award; NICHD K23HD092588-01
Footnotes
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
References
- Abrignani MG, Luca F, Favilli S, Benvenuto M, Rao CM, Di Fusco SA, … Gulizia MM (2019). Lifestyles and Cardiovascular Prevention in Childhood and Adolescence. Pediatr Cardiol, 40(6), 1113–1125. doi: 10.1007/s00246-019-02152-w [DOI] [PubMed] [Google Scholar]
- Amedro P, Tahhan N, Bertet H, Jeandel C, Guillaumont S, Mura T, & Picot MC (2017). Health-related quality of life among children with Turner syndrome: controlled cross-sectional study. J Pediatr Endocrinol Metab, 30(8), 863–868. doi: 10.1515/jpem-2017-0026 [DOI] [PubMed] [Google Scholar]
- Amundson E, Boman UW, Barrenas ML, Bryman I, & Landin-Wilhelmsen K (2010). Impact of growth hormone therapy on quality of life in adults with turner syndrome. J Clin Endocrinol Metab, 95(3), 1355–1359. doi: 10.1210/jc.2009-1754 [DOI] [PubMed] [Google Scholar]
- Bevans KB, Gardner W, Pajer KA, Becker B, Carle A, Tucker CA, & Forrest CB (2018). Psychometric Evaluation of the PROMIS(R) Pediatric Psychological and Physical Stress Experiences Measures. J Pediatr Psychol, 43(6), 678–692. doi: 10.1093/jpepsy/jsy010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle SJ, & Asare M (2011). Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med, 45(11), 886–895. doi: 10.1136/bjsports-2011-090185 [DOI] [PubMed] [Google Scholar]
- Bullard T, Ji M, An R, Trinh L, Mackenzie M, & Mullen SP (2019). A systematic review and meta-analysis of adherence to physical activity interventions among three chronic conditions: cancer, cardiovascular disease, and diabetes. BMC Public Health, 19(1), 636. doi: 10.1186/s12889-019-6877-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson JA (2010). Avoiding traps in member checking. The Qualitative Report, 15(5), 1102—1113. [Google Scholar]
- Creswell JW, & Clark VLP (2017). Designing and conducting mixed methods research: Sage UNDER publications. [Google Scholar]
- Dewalt DA, Thissen D, Stucky BD, Langer MM, Morgan Dewitt E, Irwin DE, … Varni JW (2013). PROMIS Pediatric Peer Relationships Scale: development of a peer relationships item bank as part of social health measurement. Health Psychol, 32(10), 1093–1103. doi: 10.1037/a0032670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. (2011). Pediatrics, 128 Suppl 5, S213–256. doi: 10.1542/peds.2009-2107C [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fetters MD, Curry LA, & Creswell JW (2013). Achieving integration in mixed methods designs—principles and practices. Health services research, 48(6pt2), 2134–2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawlik A, Gieburowska J, & Malecka-Tendera E (2015). [Cardiometabolic risk factors in Turner syndrome]. Pediatr Endocrinol Diabetes Metab, 20(2), 69–74. doi: 10.18544/pedm-20.02.0005 [DOI] [PubMed] [Google Scholar]
- Giorgi A (2009). The descriptive phenomenological method in psychology: A modified Husserlian approach: Duquesne University Press. [Google Scholar]
- Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO, … International Turner Syndrome Consensus G (2017). Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur J Endocrinol, 177(3), G1–G70. doi: 10.1530/EJE-17-0430 [DOI] [PubMed] [Google Scholar]
- Guetterman TC, Fetters MD, & Creswell JW (2015). Integrating quantitative and qualitative results in health science mixed methods research through joint displays. The Annals of Family Medicine, 13(6), 554–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutaff-Lee C, Bennett E, Howell S, & Tartaglia N (2019). Clinical developmental, neuropsychological, and social-emotional features of Turner syndrome. Am J Med Genet C Semin Med Genet, 181(1), 126–134. doi: 10.1002/ajmg.c.31687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RB, Onwuegbuzie AJ, & Turner LA (2007). Toward a definition of mixed methods research. Journal of Mixed Methods Research, 1(2), 112–133. [Google Scholar]
- Kraus WE, Powell KE, Haskell WL, Janz KF, Campbell WW, Jakicic JM, … Piercy KL (2019). Physical Activity, All-Cause and Cardiovascular Mortality, and Cardiovascular Disease. Med Sci Sports Exerc, 51(6), 1270–1281. doi: 10.1249/mss.0000000000001939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kredlow MA, Capozzoli MC, Hearon BA, Calkins AW, & Otto MW (2015). The effects of physical activity on sleep: a meta-analytic review. J Behav Med, 38(3), 427–449. doi: 10.1007/s10865-015-9617-6 [DOI] [PubMed] [Google Scholar]
- Lai JS, Stucky BD, Thissen D, Varni JW, DeWitt EM, Irwin DE, … DeWalt DA (2013). Development and psychometric properties of the PROMIS((R)) pediatric fatigue item banks. Qual Life Res, 22(9), 2417–2427. doi: 10.1007/s11136-013-0357-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mavinkurve M, & O’Gorman CS (2015). Cardiometabolic and vascular risks in young and adolescent girls with Turner syndrome. BBA Clin, 3, 304–309. doi: 10.1016/j.bbacli.2015.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayoh J, & Onwuegbuzie AJ (2015). Toward a Conceptualization of Mixed Methods Phenomenological Research. Journal of Mixed Methods Research, 9(1), 91–107. doi: 10.1177/1558689813505358 [DOI] [Google Scholar]
- Moustakas C (1994). Phenomenological research methods: Sage. [Google Scholar]
- Naess EE, Bahr D, & Gravholt CH (2010). Health status in women with Turner syndrome: a questionnaire study on health status, education, work participation and aspects of sexual functioning. Clin Endocrinol (Oxf), 72(5), 678–684. doi: 10.1111/j.1365-2265.2009.03715.x [DOI] [PubMed] [Google Scholar]
- Palve KS, Pahkala K, Magnussen CG, Koivistoinen T, Juonala M, Kahonen M, … Raitakari OT (2014). Association of physical activity in childhood and early adulthood with carotid artery elasticity 21 years later: the cardiovascular risk in Young Finns Study. J Am Heart Assoc, 3(2), e000594. doi: 10.1161/jaha.113.000594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pate RR, Ross R, Dowda M, Trost SG, & Sirard JR (2003). Validation of a 3-day physical activity recall instrument in female youth. Pediatric Exercise Science, 15 (3), 257–265. [Google Scholar]
- Quirk H, Blake H, Tennyson R, Randell TL, & Glazebrook C (2014). Physical activity interventions in children and young people with Type 1 diabetes mellitus: a systematic review with meta-analysis. Diabet Med, 31(10), 1163–1173. doi: 10.1111/dme.12531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riiser K, Ommundsen Y, Smastuen MC, Londal K, Misvaer N, & Helseth S (2014). The relationship between fitness and health-related quality of life and the mediating role of self-determined motivation in overweight adolescents. Scand J Public Health, 42(8), 766–772. doi: 10.1177/1403494814550517 [DOI] [PubMed] [Google Scholar]
- Schoemaker MJ, Swerdlow AJ, Higgins CD, Wright AF, Jacobs PA, & United Kingdom Clinical Cytogenetics G (2008). Mortality in women with turner syndrome in Great Britain: a national cohort study. J Clin Endocrinol Metab, 93(12), 4735–4742. doi: 10.1210/jc.2008-1049 [DOI] [PubMed] [Google Scholar]
- Sienkiewicz-Dianzenza E, Milde K, & Frac M (2006). [Declared attitudes of girls with Turner’s syndrome towards physical education classes]. Endokrynol Diabetol Chor Przemiany Materii Wieku Rozw, 12(2), 124–126. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16813717 [PubMed] [Google Scholar]
- Sienkiewicz-Dianzenza E, Milde K, Tomaszewski P, & Frac M (2011). [Physical activity of girls with Turner’s syndrome]. Pediatr Endocrinol Diabetes Metab, 17(3), 134–137. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22027066 [PubMed] [Google Scholar]
- Sirico F, Bianco A, D’Alicandro G, Castaldo C, Montagnani S, Spera R, … Nurzynska D (2018). Effects of Physical Exercise on Adiponectin, Leptin, and Inflammatory Markers in Childhood Obesity: Systematic Review and Meta-Analysis. Child Obes, 14(4), 207–217. doi: 10.1089/chi.2017.0269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sogut M, Clemente FM, Clark CCT, Nikolaidis PT, Rosemann T, & Knechtle B (2019). Variations in Central Adiposity, Cardiovascular Fitness, and Objectively Measured Physical Activity According to Weight Status in Children (9–11 Years). Front Physiol, 10, 936. doi: 10.3389/fphys.2019.00936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stochholm K, Juul S, Juel K, Naeraa RW, & Gravholt CH (2006). Prevalence, incidence, diagnostic delay, and mortality in Turner syndrome. J Clin Endocrinol Metab, 91(10), 3897–3902. doi: 10.1210/jc.2006-0558 [DOI] [PubMed] [Google Scholar]
- Thijssen CGE, Bons LR, Gokalp AL, Van Kimmenade RRJ, Mokhles MM, Pelliccia A, … Roos-Hesselink JW (2019). Exercise and sports participation in patients with thoracic aortic disease: a review. Expert Rev Cardiovasc Ther, 17(4), 251–266. doi: 10.1080/14779072.2019.1585807 [DOI] [PubMed] [Google Scholar]
- Tracy SJ (2010). Qualitative quality: Eight “big-tent” criteria for excellent qualitative research. Qualitative inquiry, 16(10), 837–851. [Google Scholar]
- Tucker CA, Bevans KB, Teneralli RE, Smith AW, Bowles HR, & Forrest CB (2014). Self-reported pediatric measures of physical activity, sedentary behavior, and strength impact for PROMIS: item development. Pediatr Phys Ther, 26(4), 385–392. doi: 10.1097/pep.0000000000000074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Mortel TF (2008). Faking it: social desirability response bias in self-report research. Australian Journal of Advanced Nursing, The, 25(4), 40. [Google Scholar]
- WHO Guidelines Approved by the Guidelines Review Committee. (2010). In Global Recommendations on Physical Activity for Health. Geneva: World Health Organization; [PubMed] [Google Scholar]
- Copyright (c) World Health Organization 2010.
- Wu XY, Han LH, Zhang JH, Luo S, Hu JW, & Sun K (2017). The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS One, 12(11), e0187668. doi: 10.1371/journal.pone.0187668 [DOI] [PMC free article] [PubMed] [Google Scholar]


