Abstract
Objective
The performance of anti-NMDAR Encephalitis One-Year Functional Status (NEOS) in predicting the 1-year functional status in Chinese patients with anti-NMDAR encephalitis is unknown.
Methods
We recruited patients with anti-NMDAR encephalitis from the Multicenter and Prospective Clinical Registry Study of Anti-NMDAR Encephalitis in Beijing Area. Patients were followed up for 1 year. We defined the poor functional status as a modified Rankin Scale score of more than 2 and good functional status as a modified Rankin Scale score of no more than 2. We performed a receiver-operator characteristic analysis to assess the discriminatory power of the NEOS score in predicting the 1-year functional status by using the area under the curve (AUC). Calibration was assessed by Pearson correlation coefficient and Hosmer-Lemeshow tests.
Results
Among the 111 patients with anti-NMDAR encephalitis recruited from 364 potentially eligible participants, 87 (78.4%) had good functional status at 1 year, whereas the remaining 24 (21.6%) had poor functional status. The AUC of the NEOS score for 1-year poor functional status was 0.86 (95% CI 0.78–0.93, p < 0.001). The increased NEOS was associated with higher risk of 1-year poor functional status in patients with anti-NMDAR encephalitis.
Conclusions
The NEOS score is considered a reliable predictor of the risk of 1-year poor functional status in Chinese patients with anti-NMDAR encephalitis. This score could help to estimate the velocity of clinical improvement in advance.
Clinicaltrial.gov identifier
Classification of evidence
This study provides Class III evidence that in patients with anti-NMDAR encephalitis, the NEOS score predicts 1-year functional status.
Anti-NMDAR encephalitis is a rare, debilitating, and potentially treatable condition that is characterized by acute to subacute psychiatric and/or neurologic complaints.1 Early identification of patients with poor prognosis remains to be a major concern in clinical practice.2,3 Some predictive factors, such as delayed treatment,4–6 intensive care unit (ICU) admission,7–9 and abnormal CSF inflammation,3,10 might be considered useful in the early identification of patients with poor prognosis. The anti-NMDAR Encephalitis One-Year Functional Status (NEOS) score, including not only the aforementioned factors, has been developed and assisted in predicting the risk of 1-year poor functional status, which in turn is useful in deciding whether early second-line immunotherapy or other novel salvage therapies should be offered to those patients with anti-NMDAR encephalitis.11 However, it has not been validated in Chinese population to date. This study aimed to validate the performance of the NEOS score in Chinese patients with anti-NMDAR encephalitis for predicting poor functional status at 1 year.
Methods
Data sources
The Multicenter and Prospective Clinical Registry Study of Anti-NMDAR Encephalitis in Beijing Area (Clinicaltrials.gov number: NCT02443350) was a multicenter clinically registered study with consecutive suspected patients with encephalitis conducted at 5 clinical centers in China. The inclusion criteria were as follows: patients (1) older than 6 months; (2) with at least one or more clinical features of the following: fever, epilepsy, focal neurologic deficiency symptoms, changes in CSF, changes in EEG, and radiographic abnormalities; (3) with confirmed anti-NMDAR encephalitis whose CSF or serum showing a characteristic pattern of reactivity in rat brain tissues and specific immunolabeling of HEK293 cells expressing GluN1 subunits of NMDAR12,13; and (4) screened at least once for systemic tumors.
Study population
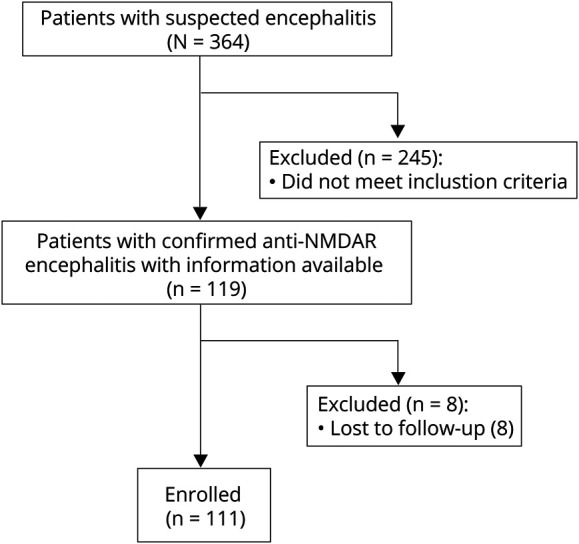
We enrolled patients with anti-NMDAR encephalitis with the available information between July 15, 2014, and February 20, 2019. All participants signed written informed consent before study initiation. This study was approved by the ethics committee of each study center. A total of 364 patients were included, and 245 (67%) among these were excluded because they were diagnosed with other diseases and 8 (7%) patients were lost to follow up (figure 1).
Figure 1. Trial profile.
Data collection and follow-up
We collected detailed information of baseline demographics, time of symptom onset, clinical features, therapeutic regimen, and the 5 variables involved in the NEOS score (see below). The follow-up duration was at least 1 year, and the information of functional status (quantified using the modified Rankin Scale [mRS]) was collected through face to face or telephone by neurologists who were not aware of this study. Poor functional status was defined as a mRS score of more than 2 (mRS score of 6 represents death), whereas good functional status was defined as a mRS score of no more than 2. We defined relapse of encephalitis as the new onset or worsening of symptoms occurring after at least 2 months of improvement or stabilization.4 Mortality occurs because of encephalitis or its associated complications. The outcomes discussed above were determined by at least 2 neurologists based on the clinical features. If there was any disagreement, we would resort to a third senior neurologist to reach a consensus decision. EEG was classified as abnormal when the presence of any of the following was recorded: electrographic seizures, rhythmic slowing, epileptic form discharges, extreme delta brush,14 focal or diffuse slowing, or abnormal state changes. Brain MRI scans were classified as abnormal if the images determined by both radiologists and neurologists were consistent or suggestive of encephalitis.7
NEOS score
The NEOS score11 was derived from the study conducted by Balu and his colleagues, in which 382 patients with confirmed anti-NMDAR encephalitis were recruited. A multivariable logistic regression model was constructed by entering variables of ICU admission, the absence of treatment for more than 4 weeks, improvement delay of more than 4 weeks after starting treatment, abnormal MRI, and CSF white blood cell (WBC) count of more than 20 cells/μL. Each variable was given 1 point, and the score ranges from 0 to 5 points. The NEOS score was strongly associated with the probability of poor functional status at 1 year.
Statistical analysis
The categorical variables were presented as frequencies (percentages). The baseline variables were analyzed by χ2 statistics or Fisher exact tests. OR with 95% CI was used to measure the effect of the NEOS score. We tested the performance of the NEOS score by estimating its discrimination and calibration. The discriminatory power of the NEOS score was assessed by the area under the receiver operating characteristic curves (AUCs) and 95% CI. An AUC of 1.0 indicated perfect prediction, and 0.5 indicated no better than random prediction. Calibration was assessed by using Pearson correlation coefficient and Hosmer-Lemeshow tests. The α level of significance was p < 0.05 on both sides. All analyses were performed using SPSS (version 25; IBM Corp., Armonk, NY) and SAS software version 9.3 (SAS Institute Inc., Cary, NC).
Classification of evidence
The primary aim was to explore whether the NEOS score was appropriate for Chinese patients with anti-NMDAR encephalitis to predict the poor functional status at 1 year. The classification of evidence assigned to these questions is Class III.
Data availability
All data are available to researchers on request for the purpose of reproducing the results or replicating the procedure by directly contacting the corresponding author.
Results
Patient characteristics
Of the 111 patients, 87 (78.4%) had good functional status at 1 year, whereas the remaining 24 (21.6%) had poor functional status. All the 24 patients with poor functional status at 1 year were followed up for 2 years after initial presentation. In this subset after follow-up for 2 years, 7 (29.2%) were recovered to good functional status.
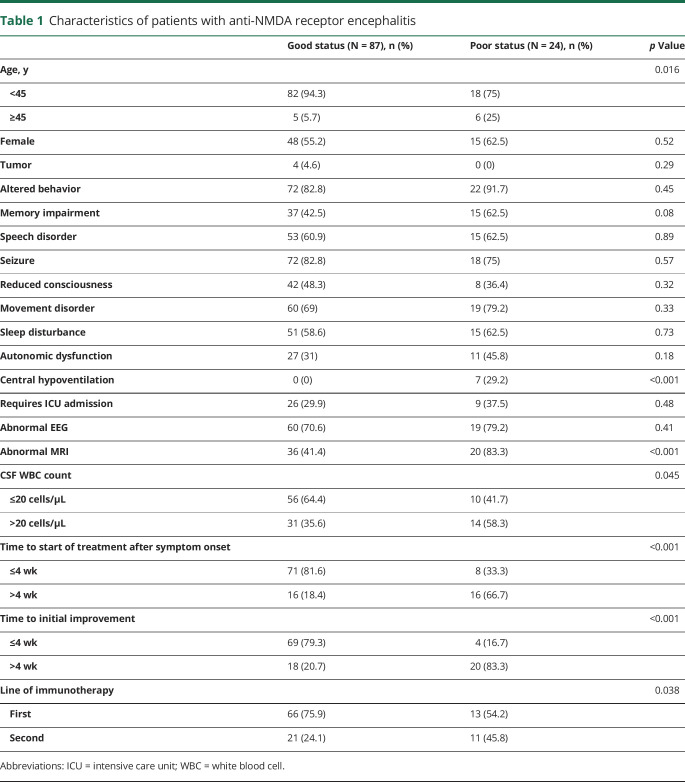
The baseline characteristics of patients are shown in table 1. The patients with poor functional status were more likely to be younger, had central hypoventilation, had abnormal MRI, had CSF WBC counts of more than 20 cells μL, had no treatment within 4 weeks of symptom onset, had treatment delay of >4 weeks, and had first-line immunotherapy (table 1).
Table 1.
Characteristics of patients with anti-NMDA receptor encephalitis
NEOS score and risk of poor functional status
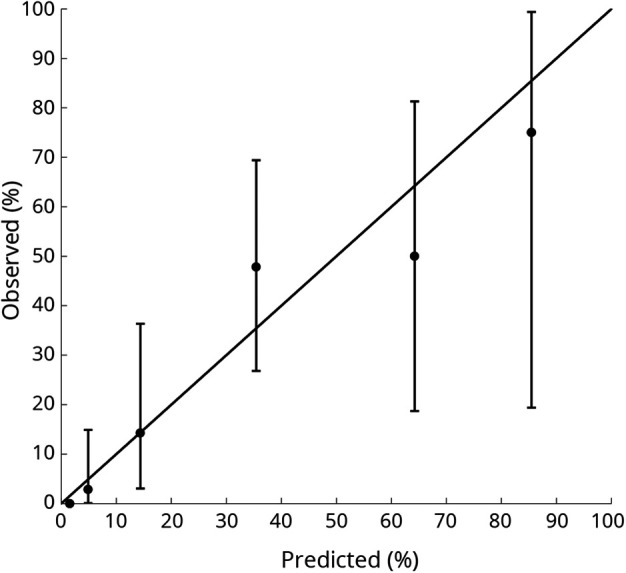
As shown in table 2, patients with higher NEOS scores have significantly higher rate of 1-year poor functional status. The AUC of the NEOS score was presented in figure 2. The NEOS score was shown to be a significant predictor of poor functional status (AUC 0.86, 95% CI 0.78–0.93, p < 0.001).
Table 2.
NEOS score and risk of poor functional status
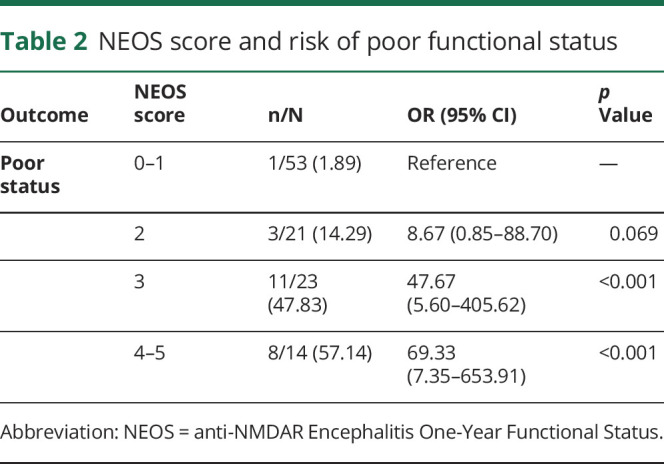
Figure 2. Receiver operator characteristic curve for prediction of 1-year prognosis of the NEOS score.
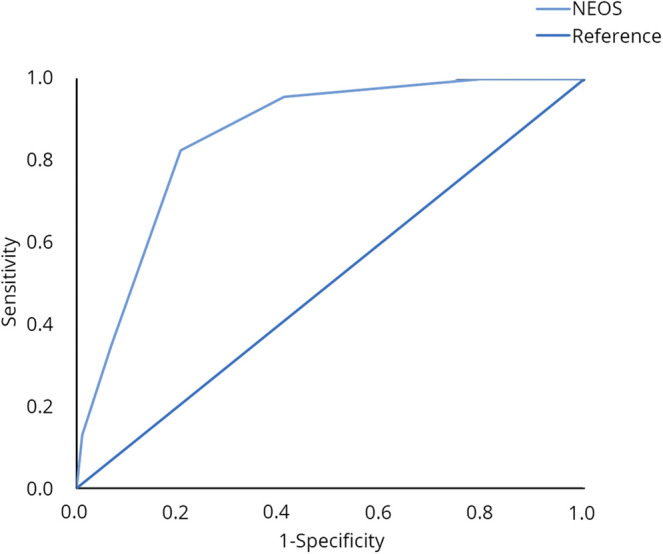
NEOS = anti-NMDAR Encephalitis One-Year Functional Status.
Calibration ability of the NEOS score
Calibration analysis of the NEOS score showed a moderate correlation between the predicted and observed probabilities of 1-year poor functional status, and the coefficient of r was 0.53 (p < 0.001). The significance level of the Hosmer-Lemeshow test for prediction of poor functional status was 0.35 (figure 3).
Figure 3. Calibration plot of the NEOS score for poor functional status.
The vertical lines indicate 95% CIs of predicted rates of clinical status. NEOS = anti-NMDAR Encephalitis One-Year Functional Status.
Discussion
Our study showed that the NEOS score well predicted the probability of 1-year poor functional status after initial symptom presentation in Chinese patients with anti-NMDAR encephalitis.
For patients with poor status, the slow and variable trajectory of recovery and step-by-step treatment meant delay in more effective treatment, imparting significant stress onto the family members of patients.15 Understanding the possible prognosis is essential in providing information to clinicians, patients, and families, as well as potentially influencing the future treatment strategies. The NEOS score can be easily calculated at bedside within 4 weeks of treatment initiation and capable of discriminating the differences in the probability of poor functional status at 1 year over a wide range of score value. To some extent, this might help clinicians to counsel patients and their families. Furthermore, to our knowledge, our study is the first prospective study to externally validate the NEOS score, except the original study.
This study showed several features that are not consistent with the original NEOS study. Patients with anti-NMDAR encephalitis in our study demonstrated a lower incidence in women, with tumors, central hypoventilation, and a better prognosis, and this is consistent with the results of previous studies in China.16–18 There was no sex difference, but a tendency to women was found. The prevalence of tumors was also lower in the Korean population than in the Western study populations.19 Experts have suggested that a race-specific factor, the human leucocyte antigen, or other genetic factors might play a significant role.20 It is unclear as to whether the discrepancy of central hypoventilation incidence occurs because of earlier diagnosis or if they showed location differences in the brainstem control of breathing or expression of NMDAR between different populations. The specific mechanism requires further exploration on brain imaging and animal model. In addition, more than half of the patients (57%) were juveniles in our sample. An anti-NMDAR encephalitis study on children and adolescents has reported that the incidence of central hypoventilation in juveniles is lower, and the symptoms seemed to be less severe than that in adults.21 As a matter of fact, the main reasons for ICU admission in our cohort were coma, seizures, agitation/confusion, and acute respiratory failure in turn. Multiple studies reported better prognosis in the Chinese population, suggesting that the prognosis of anti-NMDAR encephalitis might be predominantly related to race and natural history of the disorder.
However, our study has some limitations. First, our study included only 5 major hospitals with more medical resources and experts than other hospitals in rural areas and included small sample size. Thus, selection bias can arise in the study. Studies with larger sample size are warranted to validate external validity of the NEOS score and to better identify the subgroup of patients with poor functional status. Second, the study included variations in treatment approaches. For pediatric patients, second-line immunotherapy might be limited because of security reasons when first-line therapies fail. Third, Western populations were not included, and so inter-racial differences cannot be excluded. Finally, our study lacked biomarkers that are connected with response to treatment, which might decrease the scores' ability to predict the ultimate clinical outcome.
In conclusion, our study showed that the NEOS score was a reliable and accurate tool for physicians to predict the risk of poor functional status in Chinese patients with anti-NMDAR encephalitis at 1 year. This score could be helpful to estimate the velocity of clinical improvement and might allow clinicians to stratify patients who could benefit from novel therapies in the future clinical trials.
Acknowledgment
The authors thank Yuesong Pan from Beijing Tiantan Hospital, Capital Medical University, Beijing, China, for providing statistics assistance, and Jiejie Li from Beijing Tiantan Hospital, Capital Medical University, Beijing, China, for revising the manuscript. In addition, they appreciated all the investigators and patients who participated in the registry.
Glossary
- AUC
area under the receiver operating characteristic curve
- ICU
intensive care unit
- mRS
modified Rankin Scale
- NEOS
anti-NMDAR Encephalitis One-Year Functional Status
- WBC
white blood cell
Appendix. Authors

Footnotes
Class of Evidence: NPub.org/coe
Study funding
Supported by grants from the following: National Natural Science Foundation of China (81771313, 81870950); Youth Program of National Natural Science Foundation of China (81301029); Beijing Municipal Natural Science Foundation (19G11041, 7182077); Beijing Hospitals Authority Youth Program (QML20150206); Key Research and Development Plan of the Ministry of Science and Technology of the People's Republic of China (2016YFC0904502); Beijing Science and Technology Project “Capital Characteristics” (Z171100001017039); Key Projects of Medical Development in Capital (2014-1-1101); Beijing Tongren Hospital, Capital Medical University, Key Medical Development Plan (TRYY-KYJJ-2017-054).
Disclosure
The authors have no conflicts interest to declare as regards this study. Go to Neurology.org/NN for full disclosures.
References
- 1.Dalmau J, Graus F. Antibody-mediated encephalitis. N Eng J Med 2018;378:840–851. [DOI] [PubMed] [Google Scholar]
- 2.Dalmau J, Gleichman AJ, Hughes EG, et al. . Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008;7:1091–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Broadley J, Seneviratne U, Beech P, et al. . Prognosticating autoimmune encephalitis: a systematic review. J Autoimmun 2019;96:24–34. [DOI] [PubMed] [Google Scholar]
- 4.Titulaer MJ, McCracken L, Gabilondo I, et al. . Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 2013;12:157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Titulaer MJ, McCracken L, Gabilondo I, et al. . Late-onset anti-NMDA receptor encephalitis. Neurology 2013;81:1058–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irani SR, Stagg CJ, Schott JM, et al. . Faciobrachial dystonic seizures: the influence of immunotherapy on seizure control and prevention of cognitive impairment in a broadening phenotype. Brain 2013;136:3151–3162. [DOI] [PubMed] [Google Scholar]
- 7.Graus F, Titulaer MJ, Balu R, et al. . A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 2016;15:391–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaquet P, de Montmollin E, Dupuis C, et al. . Functional outcomes in adult patients with herpes simplex encephalitis admitted to the ICU: a multicenter cohort study. Intensive Care Med 2019;45:1103–1111. [DOI] [PubMed] [Google Scholar]
- 9.de Montmollin E, Demeret S, Brulé N, et al. . Anti-N-methyl-d-aspartate receptor encephalitis in adult patients requiring intensive care. Am J Respir Crit Care Med 2017;195:491–499. [DOI] [PubMed] [Google Scholar]
- 10.Pillai SC, Hacohen Y, Tantsis E, et al. . Infectious and autoantibody-associated encephalitis: clinical features and long-term outcome. Pediatrics 2015;135:e974–e984. [DOI] [PubMed] [Google Scholar]
- 11.Balu R, McCracken L, Lancaster E, Graus F, Dalmau J, Titulaer MJ. A score that predicts 1-year functional status in patients with anti-NMDA receptor encephalitis. Neurology 2019;92:e244–e252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol 2011;10:63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li L, Sun L, Du R, et al. . Application of the 2016 diagnostic approach for autoimmune encephalitis from Lancet Neurology to Chinese patients. BMC Neurol 2017;17:195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schmitt SE, Pargeon K, Frechette ES, Hirsch LJ, Dalmau J, Friedman D. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology 2012;79:1094–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vora NM, Holman RC, Mehal JM, Steiner CA, Blanton J, Sejvar J. Burden of encephalitis-associated hospitalizations in the United States, 1998–2010. Neurology 2014;82:443–451. [DOI] [PubMed] [Google Scholar]
- 16.Wang W, Li JM, Hu FY, et al. . Anti-NMDA receptor encephalitis: clinical characteristics, predictors of outcome and the knowledge gap in southwest China. Eur J Neurol 2016;23:621–629. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Zhang W, Yin J, et al. . Anti-N-methyl-d-aspartate receptor encephalitis in children of Central South China: clinical features, treatment, influencing factors, and outcomes. J Neuroimmunol 2017;312:59–65. [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Liu G, Jiang M, Chen W, He Y, Su Y. Clinical characteristics and prognosis of severe anti-N-methyl-D-aspartate receptor encephalitis patients. Neurocrit Care 2018;29:264–272. [DOI] [PubMed] [Google Scholar]
- 19.Lim JA, Lee ST, Jung KH, et al. . Anti-N-methyl-d-aspartate receptor encephalitis in Korea: clinical features, treatment, and outcome. J Clin Neurol 2014;10:157–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Irani SR, Bera K, Waters P, et al. . N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 2010;133:1655–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Florance NR, Davis RL, Lam C, et al. . Anti-N-methyl-D-aspartate receptor (NMDAR) encephalitis in children and adolescents. Ann Neurol 2009;66:11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available to researchers on request for the purpose of reproducing the results or replicating the procedure by directly contacting the corresponding author.