Summary:
There are currently 2 approved residency training models in the United States conferring eligibility for the American Board of Plastic Surgery examination—the integrated pathway and the independent pathway. While both pathways allow for board certification, there has been much debate regarding the effectiveness of one training model over the other. In this article, we review the existing literature to compare these pathways with regard to quality of trainees, proficiency of graduates, and practice or career outcomes. Ongoing studies are strongly encouraged to continue to identify areas of improvement for both types of training programs.
INTRODUCTION
Plastic surgery training programs have changed tremendously since their inception. Currently, the Residency Review Committee of the Accreditation Council for Graduate Medical Education (ACGME) has approved of 2 avenues for admissibility to the American Board of Plastic Surgery (ABPS) examination: the independent pathway and the integrated pathway.1 The independent model requires completion of a formal residency in either general surgery, otolaryngology, neurosurgery, urology, orthopedics, or oral maxillofacial surgery before a requisite 3 years of training in plastic surgery.2,3 The integrated model, first recognized by the ABPS in 1995, is a 6-year training program under complete guidance of a plastic surgery department or division.2,3 While both pathways ultimately provide ABPS board admissibility, much debate exists regarding the effectiveness of one program over another in their ability to produce well-trained, capable plastic surgeons.4 Additional questions have emerged regarding the advantages and disadvantages of each pathway, as well as trainee selection criteria and the future career paths.
In this article, we review the history of and current literature regarding independent and integrated plastic surgery residency training and differentiate the (1) prerequisites and selection criteria for candidates, (2) trainee evaluations, and (3) postgraduation plans and practice patterns.
HISTORY
The independent model was the first educational model to gain broad acceptance as a viable, standardized training pathway for plastic surgeons in the United States.1–3 Before the 1930s, plastic surgeons were trained in relatively informal, haphazard apprenticeships.1 Major hospitals with well-known plastic surgery departments attracted aspiring plastic surgeons, who have observed established surgeons perform their craft. In 1938, the establishment of the ABPS as a subsidiary of the American Board of Surgery was the first step toward the formation of a standardized plastic surgery residency.1 Originally, only residents previously trained in general surgery were eligible for certification after 2 years of plastic surgery training; however, in 1972, the board widened eligibility to include those previously trained in Neurological Surgery, Orthopedic Surgery, Otolaryngology, Urology, Thoracic Surgery, Vascular Surgery, or Oral and Maxillofacial Surgery.1
The integrated model was first pioneered in 1960 by Dr. Robert Chase at Stanford University.1 Initially, the model was considered an anomaly and did not gain widespread acceptance until 1995, when the ABPS first formally recognized the integrated pathway. However, in recent years, the integrated model has grown significantly in popularity. From 2007 to 2019, the number of integrated plastic surgery residency positions increased from 92 to 172.5 Simultaneously, the number of independent plastic surgery residency positions available through the San Francisco Match reached historic lows, decreasing from 93 to 63.6
Historically, some plastic surgeons were trained in a third model, known as the combined pathway. In the combined model, physicians were required to complete 3 years of training in general surgery, followed by 3 years of training in plastic surgery at either the same institution or a different institution.3 In 2015, in coordination with the ABPS, the ACGME voted to eliminate this model, and it has been phased out with programs converting to either an independent or an integrated model.
A summary of all 3 training models is depicted in Figure 1.
Fig. 1.
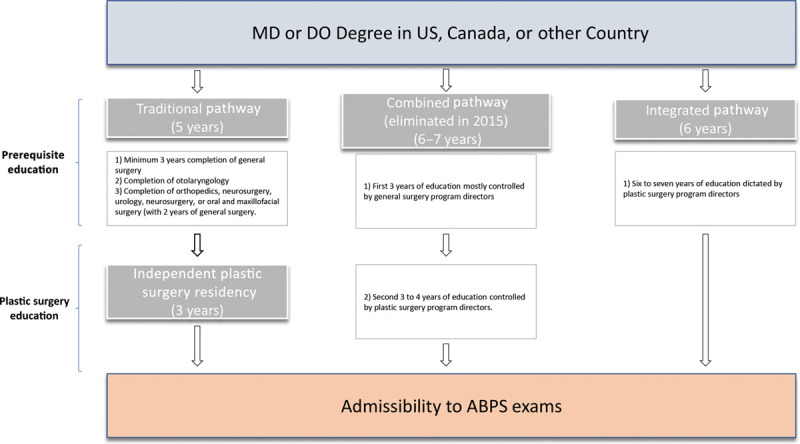
Summary chart showing the differences among independent, integrated, and combined pathways.
PREREQUISITES AND SELECTION CRITERIA
Matching into a plastic surgery residency program through either pathway is a highly competitive process. In the 2018 National Resident Matching Program Integrated Match, there were 222 applicants for only 168 positions, with an average United States Medical Licensing Exam (USMLE) Step 1 score of 249 for those who matched.7 This represents an applicant-to-position ratio of 1.32. In contrast, in the 2018 San Francisco Match, there were 83 applicants for 66 positions, with a 1.28 applicant-to-position ratio.6
The importance of different selection criteria varies in importance between the 2 program types. For integrated programs, a survey of 15 program directors found that the most important objective criterion was Alpha Omega Alpha Honor Society membership, followed by publications in peer-reviewed journals and quality letters of recommendation from a plastic surgeon known to the evaluator.8 For independent programs, program directors stated that letters of recommendation played the most important factor, followed by residency program reputation.9 Both integrated and independent program directors listed USMLE Step 1 score as an important factor in a successful application.8,9 While applying to either pathway requires high levels of achievement, some data suggest that matching into an integrated program is more challenging. A 2008 study showed that integrated residents graduate from more highly ranked medical schools than independent residents, have higher USMLE Step 1 scores, and have a higher number of pre-residency publications.4 As multiple studies have established higher USMLE Step 1 scores as a strong predictor of a trainee’s likelihood of passing professional licensing examinations,10–13 this discrepancy may be valuable to note. However, many program directors argue that these discrepancies in achievement exist because integrated programs are able to recruit students with higher levels of academic achievement, possibly due to the enticement of a shorter training period.14 Additionally, it is important to note the difficulty of comparing the qualifications of applicants to these 2 different program types. The criteria used to evaluate a medical student’s potential aptitude to be a plastic surgeon vary dramatically from the criteria used to evaluate a trained surgeon with 3 years of experience. Likely, achievements earned in medical school are not considered as important for independent programs, explaining this discrepancy in USMLE Step 1 scores and pre-residency publications.
TRAINEE EVALUATION
During training, plastic surgery residents are frequently evaluated using a variety of methods. Yet for many programs, the only objective measure of knowledge and performance is the Plastic Surgery In-Service Examination. Beyond this examination, tools used to determine progress vary. A 2009 survey of recent plastic surgery graduates found that the most common assessment tools used in residency were the Plastic Surgery In-Service Examination (99%), scheduled formal verbal feedback (77%), global assessment scores (65%), oral examinations (24%), and a 360-degree evaluation (24%).15 In regard to In-Service Examination scores, Silvestre et al16 found that on average, both independent and integrated residents perform better on the test with each additional year of training. However, at each level of training, integrated residents (years 4–6) performed better than their independent (years 1–3) counterparts.15 Girotto et al17 also found that from 2009 to 2015, independent residents failed the ABPS Written Examination at a significantly higher rate than integrated residents (8.8% versus 2.7%; P < 0.001).
Another commonly used measure to gauge resident performance is faculty feedback. Although subjective in nature, this feedback offers a window into the perception of trainee progress and competency. In a 2012 survey of interviewed faculty, 49% of faculty believed that integrated/combined residents were “superior in knowledge” to independent residents, compared with the 32% who believed the opposite.18 However, most faculty felt that independent residents were “superior in technical ability” (50% versus 19%) and research acumen (57% versus 19%).18
Residents can also be evaluated by case volume, a critical aspect of surgical education and a useful barometer for experience. Using ACGME’s Case Log System, residents are required to submit a record of their operative experiences. The ACGME sets case minimums for types of operations specific to the field of plastic surgery. Although these minimums must be met by all residents to graduate, significant variation in case quantity may exist between graduates of independent and integrated programs. A 2014 survey found no difference in the number of esthetic surgery procedures performed by integrated and independent residency programs.19 In contrast, a 2019 study found that independent/combined residents reported significantly more esthetic breast surgery cases than integrated residents (86.5 ± 53.4 versus 70.9 ± 34.4).20 Within the category of esthetic surgery, independent/combined residents reported performing more breast augmentations, mastopexies, cosmetic breast fat grafting, and “other” esthetic breast surgeries. A similar study from the same author found that approximately 10% of independent/combined residents did not meet case minimums for hand arterial repair and congenital deformity.21 Although these studies highlight possible discrepancies in specific content areas, it is difficult to draw conclusions since each training program (whether integrated or independent) has variable case type and volume.
In a continuous effort to improve graduate medical education, the ACGME has stressed the implementation of external, quantifiable metrics in the assessment of resident performance. In an attempt to move toward competency-based education, the ACGME and ABPS designed the Plastic Surgery Milestone Project in 2015.22 The objective of this project was to provide programs with a standardized framework for gauging resident performance, with specific milestone achievements appropriate for each level of residency training. Data from the Milestone Project are compiled annually by the ACGME Milestones research team, and results are published in the annual Milestones National Report.23 In this report, box plots displaying average evaluation scores in each competency domain allow for easy visualization of overall resident progression throughout graduate medical education. Future use of these large datasets may prove valuable, as these scores allow for direct comparisons of average performance between residents in integrated programs and those in independent ones. However, given this project’s recent implementation, it remains to be seen if this can be a viable assessment tool. So far, program directors have responded favorably to the transition, with 55% of program directors believing that Milestones are an improvement over the previous evaluation system.24
POSTGRADUATION CAREER PLANS
Another point of interest when comparing independent versus integrated programs is the future practices of graduates. Newly graduating plastic surgeons are faced with difficult choices that will shape the future of their careers, including fellowship training and practice type. For those who choose to forgo additional training, the decision then involves academic versus private or group practice. Often, this choice is a reflection of a multitude of personal priorities such as career goals, surgical interests, geographical location, and family needs.
An increasing percentage of graduates are choosing to practice privately, with a current estimate of 90% of plastic surgeons eventually choosing nonacademic jobs.25 Herrera et al26 found that graduates of independent plastic surgery programs were much more likely to pursue private practice immediately after graduation, compared with those graduating from integrated/combined programs (56% versus 36%; odds ratio, 2.24; 95% confidence interval, 1.50–3.32). Additionally, while 56% of plastic surgeons from integrated/combined programs chose to immediately pursue a fellowship, only 36% of surgeons from independent programs did the same. Finally, when accounting for the completion of fellowship training, integrated graduates were still significantly more likely to pursue an academic position compared with independent graduates (odds ratio, 1.63).26 There are a few possible explanations for these findings. Graduates from independent programs are generally older, with a mean age of 36 years compared with the integrated/combined graduates’ mean age of 33.8 years.26 Additionally, independent program graduates have been training for longer (mean, 7.5 versus 6 years), which represents a significant opportunity cost. An increased age, along with an overall longer length of training, may play a role in their increased likelihood to enter private practice without further subspecialty training. Integrated graduates, on the other hand, may be younger and more willing to pursue further education. Integrated residents also tend to have a higher number of pre-residency publications than independent residents, fostering an interest in research that possibly translates to a higher likelihood to pursue an academic career.4
Unfortunately, some residents choose to leave plastic surgery training before completion. Physician burnout has become an important topic of discussion in recent years, with recent surveys estimating the prevalence to be as high as 67%.27 And while plastic surgery has been associated with higher levels of career satisfaction relative to other surgical subspecialties,28 high levels of resident attrition can still be seen in programs across the nation. A 2018 study by Yang et al29 estimated average attrition rates of 2.15% for independent plastic surgery programs and 0.85% for integrated programs. One possible explanation for these higher rates in independent programs is that trainees from independent programs tend to start their plastic surgery training at an older age, with priorities that differ from those of their younger, integrated counterparts. Another theory is that because enrollment into independent programs implies successful completion of previous surgical residency, independent residents have an alternative career to which they can return.
FUTURE OF PROGRAMS
The integrated model of plastic surgery training has gained rapid popularity in the last 10 years. From 2007 to 2019, the number of integrated positions offered in the National Resident Matching Program Match has increased from 92 to 172.30 In the same time period, the number of independent positions available in the San Francisco Match has decreased from 93 to 63 (Fig. 2).6 It seems likely that this trend will continue in the near future, with more programs converting their independent programs into integrated ones. Additionally, the number of applicants participating in the San Francisco Match has been steadily decreasing, with 103 participants in 2010 and 83 in 2018.31
Fig. 2.
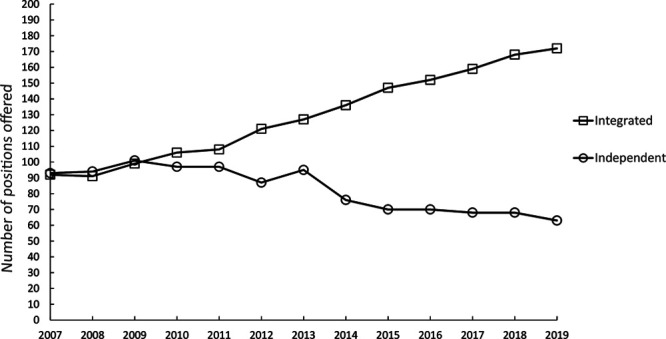
Number of positions offered for integrated and independent plastic surgery programs from years 2007 to 2019.
Many program directors believe that the field of plastic surgery, which was once thought of as an offshoot of general surgery, has specialized to the point of needing complete separation.14 Precedent can be seen in other surgical specialties such as otolaryngology, neurosurgery, and urology, which were originally pioneered in general surgery but have since separated to form distinct specialty training programs. In a survey of plastic surgery program directors, 54.76% of respondents either agreed or strongly agreed that the integrated residency training program is superior to the independent program.14 When asked why programs were transitioning to an integrated model, 69.2% cited the higher academic performance of entering residents as a potential factor. Additionally, 61.5% of responders believed that an increased ability to gain independence from the general surgery departments/faculty was a potential factor. Other reasons included the potential to have a greater number of residents, as well as the ease of training less-experienced residents. In the same study, program directors reported that reasons for not transitioning to an integrated training program included lack of funding and support from their institution and a higher level of comfort with previously trained surgeons.
However, the independent pathway does offer several advantages that may maintain its viability in the future. The independent pathway offers a route to plastic surgery for those who do not get exposure to plastic surgery during medical school or for those who are hesitant or not fully committed to the field. Additionally, many medical students attend medical schools that do not have an affiliated Plastic Surgery Divisions or Departments. In 2016, of the 141 accredited allopathic medical schools, only 59 had affiliated integrated plastic surgery residencies.32 Having a home institution conveys a massive advantage for medical students applying to plastic surgery, in terms of exposure to the specialty, networking, and research opportunities. A study by Hashmi et al33 in 2017 found that 19.6% of current integrated plastic surgery residents attended the same institution for medical school. For medical students without home plastic surgery departments or divisions, independent plastic surgery programs are highly valuable, offering a pipeline for talented surgeons to still pursue a career in plastics and make meaningful contributions to the field.
Also, the independent pathway could be a better option for students interested in pursuing a career in academic leadership. Fishman et al34 found that 81% of plastic surgery leadership (chiefs or chairs) were trained in the independent pathway, as well as a majority of plastic surgery program directors (58%). However, this observation may be due to the relative lack of integrated residencies when these leaders were in training. Another study found that independent residents had fewer probations and significantly fewer dismissals than integrated residents, although the reason for this is unclear.9 These studies, along with the persistence of independent programs at several highly competitive institutions,31 support the potential preservation of the independent pathway.
CONCLUSIONS
When Dr. Robert A. Chase implemented the first integrated plastic surgery residency at Stanford University in the early 1960s, many criticized the format.35 Critics believed this “fast track” method of training would produce “less than adequate” plastic surgeons, ultimately inferior to those trained in the longer independent model.2 In this review, we have summarized the current literature on differences between plastic surgeons trained under the integrated model versus the independent model with regards to selection criteria, trainee performance, and patterns of practice. While integrated plastic surgery programs will likely be the ideal route for students who demonstrate early interest in plastic surgery, the integrated model provides an important inroad for surgeons who otherwise would not have an opportunity to enter the field. Additionally, while the integrated model is gaining popularity, both independent and integrated plastic surgery programs have been proven to reliably produce high-quality surgeons. Future research, ideally using objective, validated measures of resident performance, may help elucidate disparities between integrated and independent programs and facilitate positive changes to optimize the training of plastic surgeons.
Footnotes
Published online 17 July 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Mackay DR, Johnson S. The origins and current state of plastic surgery residency in the United States. J Craniofac Surg. 2015;26:2251–2253. [DOI] [PubMed] [Google Scholar]
- 2.Noland SS, Lee GK. Plastic surgery residency graduate outcomes: a 43-year experience at a single institution and the first “integrated” training program in the United States. Ann Plast Surg. 2012;68:404–409. [DOI] [PubMed] [Google Scholar]
- 3.Rifkin WJ, Cammarata MJ, Kantar RS, et al. From “Coordinated” to “Integrated” residency training: evaluating changes and the current state of plastic surgery programs. Plast Reconstr Surg. 2019;143:644e–654e. [DOI] [PubMed] [Google Scholar]
- 4.Guo L, Friend J, Kim E, et al. Comparison of quantitative educational metrics between integrated and independent plastic surgery residents. Plast Reconstr Surg. 2008;122:972–978; discussion 979. [DOI] [PubMed] [Google Scholar]
- 5.Borsting EA, Chim JH, Thaller SR. An updated view of the integrated plastic surgery match. Ann Plast Surg. 2015;75:556–559. [DOI] [PubMed] [Google Scholar]
- 6.Sfmatch. Plastic Surgery Residency Match Report. Available at https://sfmatch.org/SpecialtyInsideAll.aspx?id=19&typ=2&name=Plastic Surgery#. Accessed October 17, 2019.
- 7.MATCH. Charting Outcomes in the Match: US Allopathic Seniors 2018. 2018. Available at https://www.nrmp.org. Accessed October 17, 2019.
- 8.LaGrasso JR, Kennedy DA, Hoehn JG, et al. Selection criteria for the integrated model of plastic surgery residency. Plast Reconstr Surg. 2008;121:121e–125e. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen AT, Janis JE. Resident selection protocols in plastic surgery: a national survey of plastic surgery independent program directors. Plast Reconstr Surg. 2012;130:459–469. [DOI] [PubMed] [Google Scholar]
- 10.Nagasawa DT, Beckett JS, Lagman C, et al. United States Medical Licensing Examination Step 1 scores directly correlate with American Board of Neurological Surgery scores: a single-institution experience. World Neurosurg. 2017;98:427–431. [DOI] [PubMed] [Google Scholar]
- 11.Horn GL, Jr, Herrmann S, Masood I, et al. Predictors for failing the American Board of Radiology core examination. AJR Am J Roentgenol. 2019;213:485–489. [DOI] [PubMed] [Google Scholar]
- 12.Dyrstad BW, Pope D, Milbrandt JC, et al. Predictive measures of a resident’s performance on written Orthopaedic Board scores. Iowa Orthop J. 2011;31:238–243. [PMC free article] [PubMed] [Google Scholar]
- 13.McCaskill QE, Kirk JJ, Barata DM, et al. USMLE step 1 scores as a significant predictor of future board passage in pediatrics. Ambul Pediatr. 2007;7:192–195. [DOI] [PubMed] [Google Scholar]
- 14.Pace E, Mast B, Pierson JM, et al. Evolving perceptions of the plastic surgery integrated residency training program. J Surg Educ. 2016;73:799–806. [DOI] [PubMed] [Google Scholar]
- 15.Kasten SJ, Levi B, Eng D, et al. Toward outcomes-based plastic surgery training: a needs assessment of recent graduates. Plast Reconstr Surg. 2009;124:1703–1710. [DOI] [PubMed] [Google Scholar]
- 16.Silvestre J, Levin LS, Serletti JM, et al. Performance on a surgical in-training examination varies by training year and pathway. Plast Reconstr Surg. 2016;138:358e–364e. [DOI] [PubMed] [Google Scholar]
- 17.Girotto JA, Adams NS, Janis JE, et al. Saw it coming : the correlation between poor performance on the plastic surgery in service exam and failure on the American Board written exam. Plast Reconstr Surg Glob Open. 2017;59 Suppl79. [Google Scholar]
- 18.Roostaeian J, Fan KL, Sorice S, et al. Evaluation of plastic surgery training programs: integrated/combined versus independent. Plast Reconstr Surg. 2012;130:157e–167e. [DOI] [PubMed] [Google Scholar]
- 19.Momeni A, Kim RY, Wan DC, et al. Aesthetic surgery training during residency in the United States: a comparison of the integrated, combined, and independent training models. Plast Surg Int. 2014;2014:281923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silvestre J, Caruso VA, Hernandez JM, et al. The impact of training pathway on breast surgery cases performed during plastic surgery residency. Aesthetic Plast Surg. 2019;43:1663–1668. [DOI] [PubMed] [Google Scholar]
- 21.Silvestre J, Lin IC, Levin LS, et al. Variable operative experience in hand surgery for plastic surgery residents. J Surg Educ. 2017;74:650–655. [DOI] [PubMed] [Google Scholar]
- 22.McGrath MH. The plastic surgery milestone project. J Grad Med Educ. 2014;61 Suppl 1222–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamstra SJ, Yamazaki K, Shah H, et al. Milestones National Report 2019 Executive Summary. Available at https://www.acgme.org/What-We-Do/Accreditation/Milestones/Overview. Accessed March 10, 2020.
- 24.Drolet BC, Marwaha JS, Wasey A, et al. Program director perceptions of the general surgery milestones project. J Surg Educ. 2017;74:769–772. [DOI] [PubMed] [Google Scholar]
- 25.Mandel BA, Weber SM, Gutowski KA, et al. What influences a plastic surgery resident to pursue an academic career? Plast Reconstr Surg Glob Open. 2018;6:e1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Herrera FA, Chang EI, Suliman A, et al. Recent trends in resident career choices after plastic surgery training. Ann Plast Surg. 2013;70:694–697. [DOI] [PubMed] [Google Scholar]
- 27.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shanafelt TD, Balch CM, Bechamps GJ, et al. Burnout and career satisfaction among American surgeons. Ann Surg. 2009;250:463–471. [DOI] [PubMed] [Google Scholar]
- 29.Yang MK, Meyerson JM, Pearson GD. Resident attrition in plastic surgery: a national survey of plastic surgery program directors. Ann Plast Surg. 2018;81:360–363. [DOI] [PubMed] [Google Scholar]
- 30.National Resident Matching Program. Charting Outcomes in the Match: U.S. Allopathic Seniors. 2018. 2nd edAvailable at http://www.nrmp.org/wp-content/uploads/2018/06/Charting-Outcomes-in-the-Match-2018-Seniors.pdf. Accessed November 25, 2019.
- 31.Azoury SC, Kozak GM, Stranix JT, et al. The independent plastic surgery match (2010-2018): applicant and program trends, predictors of a successful match, and future directions. J Surg Educ. 2019;77:1–10. [DOI] [PubMed] [Google Scholar]
- 32.Drolet BC, Brower JP, Lifchez SD, et al. Away rotations and matching in integrated plastic surgery residency: applicant and program director perspectives. Plast Reconstr Surg. 2016;137:1337–1343. [DOI] [PubMed] [Google Scholar]
- 33.Hashmi A, Khan FA, Policherla R, et al. No place like home: is there selection bias in plastic surgery residency match process? Plast Reconstr Surg Glob Open. 2017;5:e1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fishman JE, Pang JHY, Losee JE, et al. Pathways to academic leadership in plastic surgery: a nationwide survey of program directors, division chiefs, and department chairs of plastic surgery. Plast Reconstr Surg. 2018;141:950e–958e. [DOI] [PubMed] [Google Scholar]
- 35.Chase RA. The Stanford integrated plastic surgery program—history and philosophy. Ann Plast Surg. 1981;7:97–98. [DOI] [PubMed] [Google Scholar]


