Sir:
Emerging evidence suggests that coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), induces a hypercoagulable state with micro- and macroangiopathy.1–3 As plastic surgeons are called on to evaluate the visible manifestations of this hypercoagulability, we must understand the pathophysiology behind these cutaneous lesions. Here, we report 2 critically ill patients with COVID-19-related retiform purpura progressing to digital gangrene in an attempt to elucidate the etiology of thrombotic microangiopathy secondary to SARS-CoV-2 infection.
A 40-year-old, previously healthy man presented with respiratory distress, cough, and fever due to COVID-19. He immediately developed hypoxemic respiratory failure, requiring intubation, prone positioning, veno-venous extracorporeal membrane oxygenation, and vasopressors. On hospital day (HD) 3, he developed retiform purpura of the right foot with loss of dorsalis pedis pulse, which persisted despite argatroban infusion. On HD 13, digital gangrene ensued, despite resurgence of his dorsalis pedis pulse. Of note, the retiform nature of the purpura and sporadic digital ischemia (Fig. 1A) were distinct from the typically homogenous pattern seen in pressor-induced necrosis. On HD 21, the patient died due to septic shock.
Fig. 1.

Acral gangrene in late-stage COVID-19 patients. A, Gangrene of the right foot involving the hallux and fourth toe with retiform purpura on the dorsal midfoot. B, Gangrene of the right hand involving the thumb, index, and small fingers, with prominent retiform purpura on the ring finger (arrow).
A 68-year-old man with a similar clinical course required intubation and vasopressors on HD 5. Twenty-four hours later, he developed retiform purpura of the right hand with triphasic Doppler signals of his palmar arch and proximal digital arteries. Despite consistent therapeutic anticoagulation, digital gangrene ensued (Fig. 1B). On HD 26, further care was withdrawn in the setting of persistent encephalopathy, and the patient expired.
Both patients’ serologies revealed elevated D-dimer (10.3 and 6.2), antithrombin III deficiency, and positive anticardiolipin IgG/IgM antibodies. Hematoxylin and eosin preparations of their skin biopsies showed extensive vascular microthrombi and eccrine gland necrosis.
Our patients developed nonsequential digital gangrene with a retiform morphology in the setting of severe SARS-CoV-2 infection. Although acral gangrene in the setting of COVID-related hypercoagulability has been described,4,5 sparse data exist on the pathophysiology of this phenomenon. Retiform purpura reflects the cutaneous manifestation of an occlusive microthrombotic process, as evidenced by the pervasive small vessel thrombi on biopsy (Fig. 2). Progression despite preserved major peripheral pulses also suggests a microvascular etiology to the digital necrosis. Acral distribution and delayed progression of ischemia after the acute respiratory insult imply that the thrombotic microangiopathy is secondary to cold-sensitive antibody/immunoglobulin activation in response to the virus, rather than a direct viral effect.
Fig. 2.
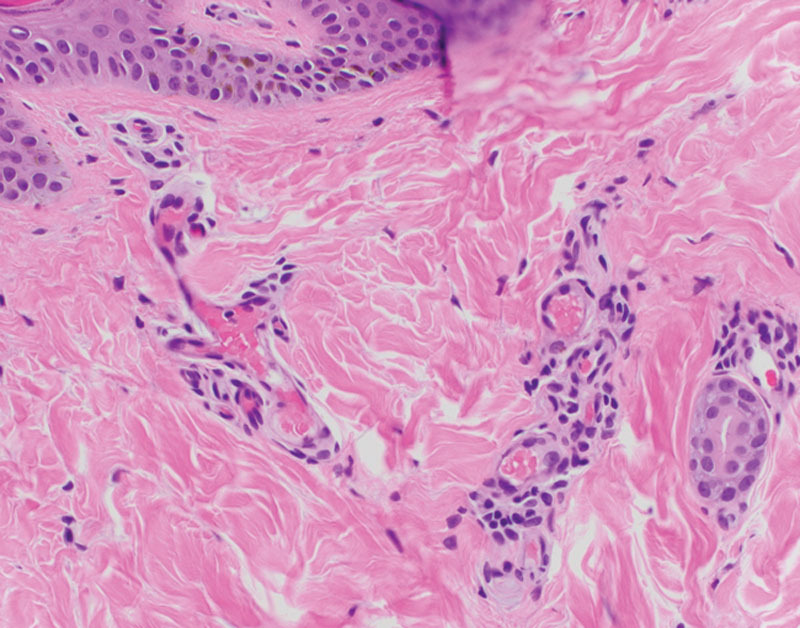
Immunofluorescence image of skin biopsy from purpuric region in COVID-19 patients. Hematoxylin and eosin stain demonstrates microthrombi.
Recent data suggest the presence of a complement-mediated microvascular injury in multiple organ systems,3 and we are pursuing direct immunofluorescence of the skin biopsies with this in mind. Currently, there is no accepted treatment protocol for COVID-19, and digital gangrene appears to portend end-stage disease. Although we advocate expectant management with no surgical intervention, we believe defining the etiology behind these dermatologic changes can contribute to the understanding and treatment of COVID-19. As demonstrated by our cases, progression of cutaneous ischemia despite early and aggressive anticoagulation underscores the need for a targeted immunotherapy that would effectively manage the catastrophic microangiopathic response induced by SARS-CoV-2.
Footnotes
Published online 8 July 2020.
REFERENCES
- 1.Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with COVID-19. N Engl J Med. 2020;382:e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klok FA, Kruip MJHA, van der Meer NJM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020;191:148–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magro C, Justin Mulvey J, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qian S-Z, Pan J-Y. COVID-19 with limb ischemic necrosis. J Cardiothorac Vasc Anesth. 2020;April 10:S1053–0770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schultz K, Wolf JM. Digital ischemia in COVID-19 patients: case report. J Hand Surg Am. 2020;45:518–522. [DOI] [PMC free article] [PubMed] [Google Scholar]


