Highlights
-
•
COVID-related restrictions on public life in the commonwealth of virginia resulted in a temporary 43% reduction in trauma volume.
-
•
There were no drastic changes in trauma patterns and injury mechanisms in the short term.
-
•
Trauma patients admitted during the COVID pandemic had higher injury severity and were discharged after shorter hospital length of stays.
-
•
Some changes in trauma patterns may not manifest until after easing of COVID-related restrictions.
Keywords: Covid pandemic, United states, Trauma center, State of emergency, Lockdown, Trauma volume
Abstract
The COVID pandemic of 2020 resulted in unprecedented restrictions of public life in most countries around the world, and many hospital systems experienced dramatic decreases in non-COVID related patient admissions. We aimed to compare trauma volumes, patient characteristics, and trauma mechanisms at a large, urban Level 1 trauma center in the United States during a state-wide “State of Emergency” and “stay-at-home” order to corresponding historic dates.
All adult trauma activations from March 1 through April 30, 2020 and a historic control from March 1 through April 30, 2018 and 2019 were reviewed in the institution's trauma registry. Trauma volumes, patient characteristics, and trauma mechanisms were compared over time as increasingly stricter COVID-related restrictions were enacted in the Commonwealth of Virginia.
After declaration of a state-wide “Public Health Emergency” on March 17, 2020, the daily number of trauma activations significantly declined to a mean of 4.7 (standard deviation, SD = 2.6), a decrease by 43% from a mean of 8.2 (SD = 0.3) for the same dates in 2018 and 2019. Trauma activations during COVID restrictions vs. historic control were characterized by significantly higher prevalence of chronic alcohol use (15.5% vs. 6.8%, p < 0.01), higher median (25th – 75th percentile) Injury Severity Score of 9 (5 – 16) vs. 6 (4 – 14), p = 0.01, and shorter median (25th – 75th percentile) length of hospital stay of 2 (1 – 6) days vs. 3 (1 – 7) days, p = 0.03.
The COVID-related Public Health Emergency and “stay-at-home” order in the Commonwealth of Virginia dramatically reduced overall trauma volumes with minor but interesting changes in trauma patterns.
Introduction
In an effort to mitigate the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during the coronavirus disease (COVID) pandemic of 2020, unprecedented social distancing measures and limitations of public life were implemented in many countries throughout the world. In the United States, these measures often progressed from the cancellation of large events to travel restrictions and ultimately “stay-at-home” or lockdown orders [11]. Hospitals and surgery centers were required to postpone non-emergent operative interventions to preserve resources and many hospitals imposed visiting restrictions for the families of patients [17]. These actions resulted in a dramatic slowdown of public life in an attempt to “flatten the curve” of COVID spread and a desirable reduction in patient visits to hospitals, thus allowing health systems to prepare for an anticipated surge in COVID patients. However, patient visits for medical emergencies such as strokes and cardiac events declined as well, raising concerns that patients were not seeking medical attention even when this was potentially life-threatening [4, 6, 9, 16].
While most trauma patients cannot choose whether to seek medical care in a trauma center or not, our American College of Surgeons (ACS)-verified and state-designated Level 1 trauma center expected to see a decline in trauma volume [3, 5] due to the limitations imposed on public life in the Commonwealth of Virginia [12], [13], [14], [15]. We hypothesized that increasingly stricter measures would result in a decreased number of total trauma activations, decline in traffic-related and outdoor incidents, while simultaneously fearing a rise in violent behaviors due to social isolation, desperation, and economic hardship [7, 10].
Methods
All adult trauma activations in the months of March and April 2018, 2019, and 2020 in our institution's trauma registry were reviewed. These months spanned the time from initial awareness of COVID in the Commonwealth of Virginia to the State of Emergency Declaration, closure of non-essential businesses, and a full month under a stay-at-home order in the city of Richmond, VA and the entire state. Trauma activations and patterns in the months of March and April 2018 and 2019 acted as historic control. Our Institutional Review Board approved this study for exemption from full review.
Patient demographics, trauma mechanisms, locations, and injury severity were obtained from the registry and using International Classification of Diseases (ICD)−10 codes to define major trauma categories. Average daily number of trauma activations and their characteristics during COVID-related restrictions on public life in 2020 were compared to corresponding dates in 2018 and 2019. Three pertinent dates marked increasingly stricter COVID-related limitations in the Commonwealth of Virginia [9], [10], [11], [12] on March 17, 2020, the Governor and State Health Commissioner of Virginia released “Order of Public Health Emergency One”, limiting gatherings to fewer than ten people and making Virginians acutely aware of the gravity and severe impact of the COVID pandemic in the Commonwealth; on March 25, 2020, educational institutions and all non-essential businesses including bars and restaurants were closed; on March 30, 2020, Executive Order 55 followed, mandating that “All individuals in Virginia shall remain at their place of residence”, with exceptions.
Categorical data was described as number (percentage) and compared using Chi-squared and Fisher's Exact test, as appropriate. Continuous data was expressed as mean (standard deviation, SD) or median (interquartile range, 25th to 75th percentile) for normal or non-normal distributed measurements, respectively, and compared using t-test or Wilcoxon-Mann-Whitney test, as appropriate. A sample size calculation was not performed as all patients fulfilling inclusion criteria for the time were analyzed. Two-tailed p values of 0.05 or less were considered statistically significant. Statistical analyses were performed with JMP® Pro 15.0.0, © 2019 SAS Institute Inc.
Results
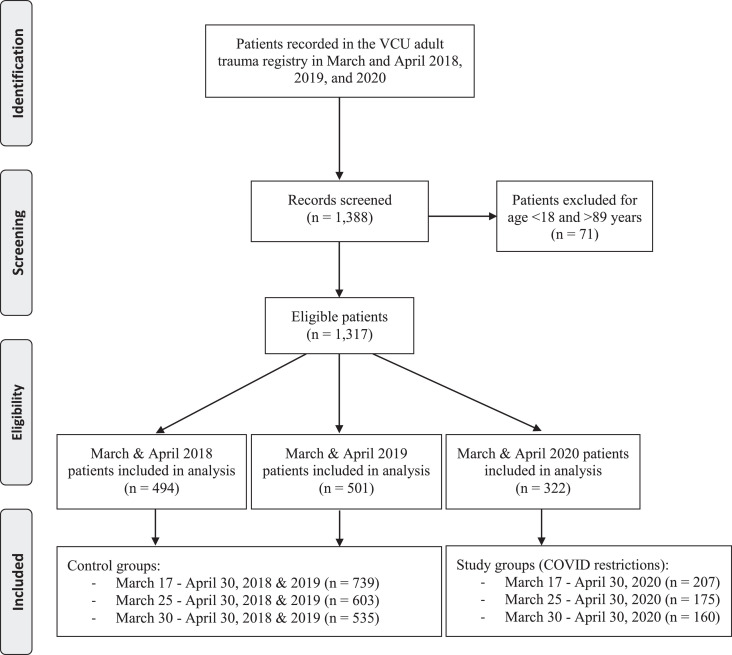
A total of 1317 trauma activations from March 1 through April 30, 2018, 2019, and 2020 fulfilled inclusion criteria (Fig. 1 ). In the 61 days of March and April 2020, 322 trauma activations represented a mean rate of 5.3 (SD = 0.4) trauma activations per day, or mean of 158.2 (SD = 13) averaged over 30 days. This was a significant decrease compared to March and April 2018 and 2019, in which 995 patients were seen in 122 days, translating into a mean of 8.2 (SD = 0.3) trauma activations per day, or mean of 244.7 (SD = 7.9) averaged over 30 days.
Fig. 1.
PRISMA-style flow diagram of patient selection and inclusion.
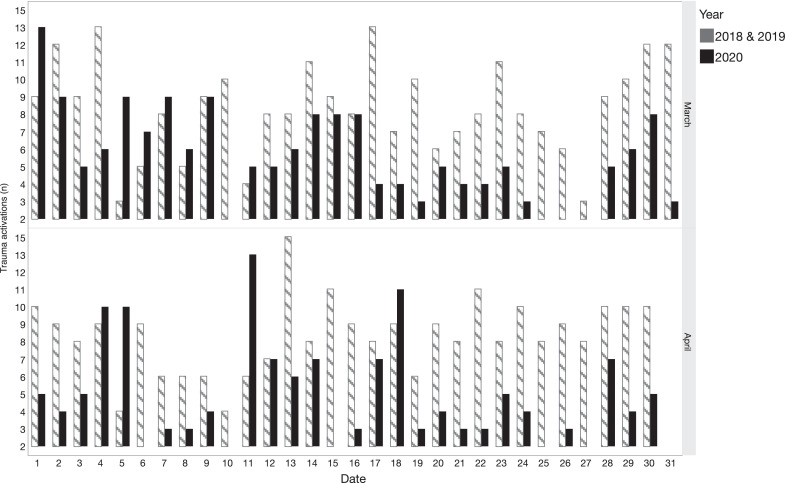
In March 2020 alone, the average number of trauma activations per day significantly declined from a mean of 7.2 (SD = 2.5) from March 1 through March 16 to a mean of 4 (SD = 0.8) from March 17 through March 24; to a mean of 3 (SD = 2.4) from March 25 through March 29; and to a mean of 5 (SD = 2.9) from March 30 through April 30, 2020 (Fig. 2 ).
Fig. 2.
Trauma activations per day in March and April 2018 and 2019 vs. 2020.
A = Declaration of public health emergency; B = Closure of non-essential businesses; C = “Stay-at-home” order.
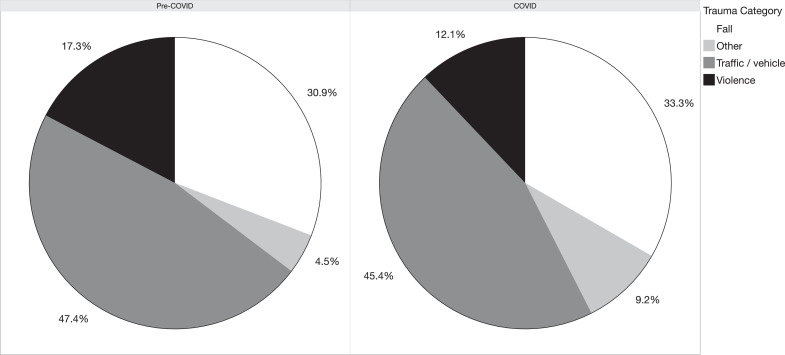
Trauma activations after implementation of COVID restrictions on March 17, 2020 were characterized by a significantly larger proportion of patients with chronic alcohol abuse, higher injury severity score (ISS), and shorter hospital length of stay (LOS). There was a trend towards fewer patients presenting to the Emergency Department (ED) in a private vehicle as well as a trend towards decreased incidence of violent trauma (Table 1 ). Similar findings were observed when evaluating trauma activations after implementation of more restrictive measures on March 25 and March 30, 2020. After March 25, 2020, the decreased use of private vehicles to present to the ED reached statistical significance (8.3% vs. 3.4%, p = 0.03), and after March 30, 2020, we experienced a significant decline in violent incidents as cause of trauma (10.6% vs. 17%, p = 0.05). Trauma categories and mechanisms before and after March 17, 2020 are shown in Fig. 3 .
Table 1.
Patient demographics and trauma details before (“pre-COVID”) and after (“COVID”) initiation of COVID-related restrictions on March 17, 2020.
| Pre-COVID n (%) | COVID n (%) | P value | |
|---|---|---|---|
| Age (years)1 | 47 (29 – 63) | 46 (30 – 64) | 0.88 |
| Gender (female) | 260 (35.2%) | 66 (31.9%) | 0.38 |
| Race (African American) | 310 (42%) | 83 (40.1%) | 0.69 |
| Transport (private vehicle) | 61 (8.3%) | 9 (4.4%) | 0.07 |
| Trauma location (home) | 242 (40.9%) | 75 (44.4%) | 0.42 |
| Blunt mechanism | 655 (88.6%) | 189 (91.3%) | 0.27 |
| Traffic-related injury2 | 350 (47.4%) | 94 (45.4%) | 0.62 |
| Violent trauma3 | 130 (17.6%) | 26 (12.6%) | 0.09 |
| Self-harm | 9 (1.2%) | 3 (1.5%) | 0.73 |
| Alcohol intoxication4 | 144 (19.5%) | 43 (20.8%) | 0.69 |
| Intoxication with other substance | 77 (10.4%) | 18 (8.7%) | 0.51 |
| Chronic alcohol abuse | 50 (6.8%) | 32 (15.5%) | < 0.01* |
| Chronic substance abuse | 54 (7.3%) | 20 (9.7%) | 0.31 |
| Injury Severity Score1 | 6 (4 – 14) | 9 (5 – 16) | 0.01* |
| Length of hospital stay1 | 3 (1 – 7) | 2 (1 – 6) | 0.03* |
| Mortality | 27 (3.7%) | 10 (5%) | 0.41 |
= median (25th – 75th percentile)
= motor-vehicle or -cycle crash, auto-vs-pedestrian
= blunt assault, gunshot wound, or stabbing.
= blood alcohol level > 50 mg/dL; * = statistical significance.
Fig. 3.
Major trauma categories before and after implementation of COVID-related restrictions in the Commonwealth of Virginia on March 17, 2020.
Discussion
The Governor of Virginia issued Executive Order 51 on March 12, 2020, declaring a “state of emergency due to novel coronavirus (COVID-19)” for the Commonwealth of Virginia [13]. Over the subsequent two weeks as COVID cases continued to rise in Virginia, further restrictions were enacted resulting in unprecedented limitations of public and commercial life. These changes resulted in a decrease in trauma volume at our urban level 1 trauma center by half. Similar dramatic decreases in trauma cases were reported from California [5] as well as world-wide for trauma [3] non-trauma emergencies [6, 9]. However, in some parts of the United States, an unbridled volume of trauma and particularly violent incidents was observed [1, 8]. Throughout April 2020, we begun to experience a slight increase in trauma volume, with trauma volume in May 2020 approaching that of prior years (preliminary institutional data). Though non-essential businesses remained closed in the city of Richmond, VA throughout the month of May 2020, the increase in trauma may be related to “lockdown fatigue”, i.e. gradual easing and liberal interpretation of restrictions by the public.
We did not see major changes in trauma patterns and injury mechanisms. Our clinical impression of decreased vehicle- and traffic-related trauma was not confirmed by our data, though traffic volume in the region had clearly declined. Preliminary estimates of road fatalities from the U.S. National Safety Council suggest a similar picture nationwide. Despite less road traffic due to COVID restrictions in March 2020, there was an increase in road fatalities, with substantial regional differences [2]. Fewer cars on the road do not translate into safer driving habits and while minor “fender-benders” may have declined, major motor vehicle and -cycle crashes were not affected and would still present to a level 1 trauma center.
An anticipated rise in violent trauma, domestic abuse, and self-harm was of major concern due to the expected economic hardship and stress caused by the COVID pandemic, exacerbated by a reluctance of patients to seek medical attention and inability of domestic abuse victims to escape their home environment [4, 7, 16]. We did not see such changes in our trauma activations, and the volume of violent trauma actually declined after the stay-at-home order in Virginia had been issued. Consistent with the universally observed increase in violent trauma in summer months, many of these incidents occur in the public space, and gatherings leading to such violence were not possible after March 30, 2020. However, it is possible that we will only begin to learn of heightened rates of domestic abuse and self-harm due to stress and economic hardship in the weeks and months to come. Indeed, our institution's Injury and Violence Program (IVPP) continued to offer telehealth services throughout the COVID pandemic and reported an increased number of phone calls and video consultations of patients affected by violence.
A larger proportion of trauma patients suffered from chronic alcohol abuse and continued to present with disease-related injuries, perhaps exacerbated by an inability to “stay at home” due to homelessness, worsening economic hardship, and an inability to suspend daily alcohol use. Trauma patients seen during COVID restrictions also had more severe injuries, likely reflecting a reluctance of those with minor trauma such as ground level falls or minor traffic incidents to present to the hospital. Patients who were admitted to our trauma service had a decreased hospital length of stay, likely reflecting efforts of our institution to facilitate rapid discharge home, if safe, to prepare for an expected surge in COVID cases. Indeed, discharges home with home health follow-up nearly doubled, suggesting that some lessons learned during this pandemic may be helpful in improving the efficiency of discharge planning in the future. Some patients and families had also expressed their desire to be discharged as soon as possible and safe due to concerns of contracting COVID during the hospital stay. Similarly, patients opted for home care rather than care at a facility after their discharge, if at all safe medically, due to the reported high incidence of COVID infection in nursing and long-term care facilities.
Our analysis is primarily limited by the focus on a single institution, which may not be representative of other health systems and trauma centers in the U.S. and world-wide. The consequences of the COVID pandemic on public life as well as health systems were highly variable across countries as well as states in the U.S., and are often influenced by disparities in race, socioeconomic status, and geography. While missing data was rare, we were not able to clearly classify all trauma mechanisms and locations as home vs. public or violent vs. non-violent, which may have led to over- or underreporting in certain categories.
Conclusions
The unprecedented limitations of public life in the Commonwealth of Virginia throughout the COVID pandemic of 2020 resulted in a dramatic decline in trauma activations at one of Virginia's largest trauma centers. Despite decreased volume, anticipated changes in trauma patterns such a rise in (domestic) violence or fewer traffic-related injuries were not identified. Reported experiences from other trauma centers world-wide are still limited in number but suggest that changes in trauma volume and patterns may be highly individualized and influenced by geography, patient population, and other factors.
Declaration of Competing Interest
This research did not receive any specific grant from funding agencies. Declarations of interest: none.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.injury.2020.08.014.
Appendix. Supplementary materials
References
- 1.Bates J. “We're Catching It Double.” Amid Coronavirus Lockdowns, Gun Violence Continues to Plague Chicago [Internet]. TIME Mag. 2020 [cited 2020 May 25]; Available from: https://time.com/5818553/gun-violence-chicago-coronavirus/.
- 2.Bates J.National Safety Council. Motor Vehicle Fatality Rates Jump 14% in March Despite Quarantines [Internet]. 2020[cited 2020 May 25]. Available from: https://www.nsc.org/in-the-newsroom/motor-vehicle-fatality-rates-jump-14-in-march-despite-quarantines.
- 3.Christey G., Amey J., Campbell A., Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133(1513):81–88. [PubMed] [Google Scholar]
- 4.Fatke B., Hölzle P., Frank A., Förstl H. [COVID-19 Crisis: psychische Probleme in der Pandemie – Beobachtungen während der COVID-19-Krise [COVID-19 Crisis: early Observations on a Pandemic's Psychiatric Problems] Dtsch Med Wochenschr. 2020;145(10):675–681. doi: 10.1055/a-1147-2889. [DOI] [PubMed] [Google Scholar]
- 5.Forrester J.D., Liou R., Knowlton L.M., Jou R.M., Spain D.A. Vol. 5. Published 2020 May 7; California: March 2020. Impact of shelter-in-place order for COVID-19 on trauma activations: santa Clara County. (Trauma surg acute care open). 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Graham-Harrison E., Giuffrida A., Smith H. Lockdowns around the world bring rise in domestic violence [Internet]. The Guardian. 2020[cited 2020 May 1]; Available from: https://www.theguardian.com/society/2020/mar/28/lockdowns-world-rise-domestic-violence.
- 8.Hatchimonji J.S., Swendiman R.A., Seamon M.J., Nance M.L. Trauma does not Quarantine: violence during the COVID-19 Pandemic. Ann Surg. 2020 Apr 29 doi: 10.1097/SLA.0000000000003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020 May 14;41(19):1852–1853. doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Coalition Against Domestic Violence. COVID-19 and Domestic Violence [Internet]. [cited2020 May 1]; Available from: http://www.ncadv.org/covid-19-and-domestic-violence.
- 11.National Governors Association. Coronavirus: what You Need to Know [Internet]. 2020[cited 2020 May 1]; Available from: https://www.nga.org/coronavirus/#glance.
- 12.Northam R.S., Oliver M.N.Amended order of the Governor and State Health Commissioner declaration of public health emergency [Internet]. 2020[cited 2020 May 1]; Available from: https://www.governor.virginia.gov/media/governorvirginiagov/executive-actions/Amended-Order-of-the-Governor-and-State-Health-Commissioner-Declaration-of-Public-Health-Emergency.pdf.
- 13.Northam RS. Executive Order 51: Declaration of a state of emergency due to novel coronavirus (COVID-19) [Internet]. 2020[cited 2020 May 1]; Available from: https://www.governor.virginia.gov/media/governorvirginiagov/governor-of-virginia/pdf/eo/EO-51-Declaration-of-a-State-of-Emergency-Due-to-Novel-Coronavirus-(COVID-19).pdf.
- 14.Northam R.S. Executive Order 53 (amended): extension of temporary restrictions on restaurants, recreational, entertainment, gastherings, non-essential retail businesses, and closure of K-12 schools due to novel coronavirus (COVID-19) [Internet]. 2020[cited 2020 May 1]; Available from: https://www.governor.virginia.gov/media/governorvirginiagov/executive-actions/EO-53-AMENDED-Temporary-Restrictions-Due-To-Novel-Coronavirus-(COVID-19).pdf.
- 15.Northam RS.Executive Order 55: Temporary stay at home order due to novel coronavirus (COVID-19) [Internet]. 2020[cited 2020 May 1]; Available from: https://www.governor.virginia.gov/media/governorvirginiagov/executive-actions/EO-55-Temporary-Stay-at-Home-Order-Due-to-Novel-Coronavirus-(COVID-19).pdf.
- 16.Rosenbaum L. The Untold Toll - The Pandemic's Effects on Patients without Covid-19. N Engl J Med. 2020;382(24):2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 17.VCU Health. VCU Health implements temporary no-visitor policy, changes to valet parking [Internet]. 2020[cited 2020 May 1]; Available from: https://www.vcuhealth.org/news-center/news-story?&news=1587.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.