Abstract
Background
Sexualized drug use (SDU; the use of any psychoactive substance before or during sexual intercourse) is prevalent among men who have sex with men (MSM) and may aggravate the worsening HIV epidemic in this key population.
Objective
This observational prospective cohort study investigated factors predicting the occurrence of SDU within a 6-month follow-up period among a sample of MSM in Hong Kong. We hypothesized that perceptions related to SDU would mediate the association between the influence of social media/gay social networking apps and SDU during the follow-up period.
Methods
Participants were Chinese-speaking men in Hong Kong, China who had anal intercourse with at least one man in the past year. Among 600 participants who completed the baseline telephone survey, 407 (67.8%) completed another telephone survey 6 months later. Logistic regression models and path analysis were fitted.
Results
At Month 6, 6.9% (28/407) and 4.4% (18/407) of participants reported SDU and chemsex during the follow-up period. After adjustment for significant baseline background variables (use of pre-exposure prophylaxis; history of HIV and other sexually transmitted infections; anal intercourse with nonregular male sex partners, condomless anal intercourse with men, multiple male sex partnerships, and SDU at baseline), three constructs of the Theory of Planned Behavior (TPB) were significantly associated with SDU during the follow-up period: (1) positive attitudes toward SDU (adjusted odds ratio [AOR] 1.19, 95% CI 1.05-1.36), (2) perceived support for SDU from significant others (AOR 1.15, 95% CI 1.01-1.30), and (3) perceived behavioral control of refraining from SDU (AOR 0.76, 95% CI 0.59-0.98). Exposure to information supporting SDU on social media and gay social networking apps was also significantly associated with SDU (AOR 1.11, 95% CI 1.01-1.22). Bootstrapping analyses indicated that social media influence was indirectly associated with SDU through TPB-related perceptions of SDU (β=.04; B=.002, 95% CI 0.001-0.01).
Conclusions
Social media and gay social networking apps may be a major source of influence on MSM’s perceptions and actual behaviors related to SDU.
Keywords: influence of social media, sexualized drug use, chemsex, men who have sex with men, prospective observational cohort study
Introduction
Psychoactive substance use and HIV are intertwined epidemics among MSM [1]. Sexualized drug use (SDU) refers to the use of any psychoactive substance before or during sexual intercourse [2]. Chemsex is considered a subset of SDU, which is commonly defined as the use of specific drugs (methamphetamine, mephedrone, γ-hydroxybutyrate [GHB/GBL], ketamine and cocaine) before or during sexual intercourse [3-5]. Two published systematic reviews addressed SDU and chemsex among MSM and found these practices prevalent across settings [3,6]. A recent study found that 54% of MSM visiting sexually transmitted infection (STI) clinics in the Netherlands reported SDU [4]. The prevalence of using alcohol or illicit psychoactive substances before or during sexual intercourse was 41% among an online sample of MSM in the United Kingdom [5]. In Hong Kong, China, 12.0% of MSM reported SDU in 2017 [7]. The prevalence of chemsex among MSM ranged from 3% to 35% across countries [3,8-10]. Psychoactive substances such as those used for SDU/chemsex adversely affect users’ capacity to perceive and respond to risks during sexual encounters, and may prompt them to engage in high-risk sexual practices [11]. Studies have consistently shown that SDU and chemsex were associated with a higher risk of condomless anal intercourse (CAI), group sex, and fisting, resulting in a higher risk of HIV and other STIs [3,8,12]. SDU/chemsex among MSM in Hong Kong may aggravate the worsening HIV epidemic in this group (6.54% of MSM were HIV-positive in 2017) [13]. However, there is a lack of effective behavioral interventions targeting SDU/chemsex [14-17].
Factors associated with SDU/chemsex among MSM included those related to sociodemographics (eg, age, ethnicity, income, education level, and employment status), sexual orientation, and utilization of HIV testing and other HIV/STI prevention services [3,5,9]. Studies also showed that MSM with SDU/chemsex experience were more likely to access pre-exposure prophylaxis (PrEP) [10,12]. These factors were considered in this study. Perceptions related to SDU also play important roles, and are important for theory-based interventions to address. Qualitative studies found that a key reason MSM engaged in SDU/chemsex was the belief that psychoactive substances could increase stamina and arousal levels, so that an individual could engage in sex for a sustained period [3]. Other reasons given included the following: overcoming underconfidence, enhancing the emotional connection with sex partners, and coping with stress [3]. Although a qualitative study suggested that MSM are under peer pressure to have SDU and chemsex [18], other social network–related factors (such as fear of loss of partners or friends) deterred MSM from using psychoactive substances before or during sexual intercourse [3]. Only one quantitative study showed that a perceived lower confidence of practicing safe sex consistently was associated with a higher likelihood of chemsex among MSM in the United Kingdom [5]. In this study, we chose the Theory of Planned Behavior (TPB) as the framework to guide our examination of perceptions related to SDU [19]. The TPB has commonly been applied to explain various types of risk behaviors [20] and design various health-related interventions [21]. The TPB specifies that attitudes, subjective norms (ie, whether others approve of certain behaviors), and perceived behavioral control (perceived availability of resources and opportunities that enable a person to perform behaviors) determine health behaviors [19]. This framework is potentially applicable for understanding the factors related to SDU/chemsex among MSM, given findings from previous studies that noted the importance of attitudes, norms, and perceived control on this behavior.
Constructs from the TPB and subsequent behaviors may be shaped by social network–related factors as well as the use of social media and gay social networking apps. In Hong Kong, 96% of residents have access to a smartphone [22]; 85% and 57% use Facebook and Instagram, respectively [23]; and about 70% of local MSM use gay social networking apps to seek sex partners [24]. Social media (eg, Facebook, Twitter, Instagram, Weibo) and location-aware gay social networking apps (eg, Grindr, Jack’d, Blued) have facilitated drug purchasing and seeking SDU and chemsex in one’s geographical location [18,25,26]. Across countries, MSM reported that it was common to encounter information related to SDU/chemsex when browsing these social media and apps [18,25,26]. Many MSM openly solicit chemsex in their online profiles [18,25,26], while others reported being asked to use psychoactive substances or engage in SDU/chemsex by other MSM through these apps [18,25-28]. In addition, posts on social media such as Facebook or Twitter usually portray psychoactive substance use as normative, which may increase intentions to practice SDU or chemsex [29,30]. Despite the potential for social media and apps to increase SDU and chemsex among MSM in Hong Kong, no quantitative studies have investigated the influence of these factors.
In addition to social media and gay social networking apps, peer behaviors may also influence SDU and chemsex practices among MSM. Compared to other HIV key populations, MSM tend to have large and dense social networks [31]. Most Chinese MSM are heavily involved in the MSM community, and have strong ties to each other [32]. As MSM are a highly marginalized community in Hong Kong, individuals within it may perceive a high level of similarity to their MSM peers and may consequently find their peers’ experiences particularly valuable and influential. Prior studies have found that peers within an individual’s social network are the most common source for obtaining psychoactive substances [33,34]. Qualitative studies have suggested that MSM often introduce SDU and chemsex to their peers. Previous studies suggested that a higher number of psychoactive substance users in one’s social network was positively associated with substance use in various populations [35-37], including MSM [36].
The Social Learning Theory posits that people learn by both direct experience and observation [38]. Observation of peers is a major source of influence on people’s health attitudes and behaviors [39]. Given the close relationships and high level of perceived similarity among MSM, observing peer behaviors plays an important role in influencing MSM’s attitudes and behaviors related to SDU/chemsex. Such interactions and observations may occur online and offline. In this study, we hypothesized that being exposed to information supporting SDU on social media/gay apps and observing SDU among peers would influence MSM’s perceptions related to SDU, which would influence the occurrence of SDU.
To address these gaps, this study investigated predictors of SDU within a 6-month follow-up period among a sample of MSM in Hong Kong. Potential predictors measured at baseline included sociodemographics and behavioral characteristics of the participants, perceptions related to SDU based on the TPB, and the influence of social media/gay social networking apps and peers. We further tested the hypothesis that perceptions of SDU would mediate the associations between the influence of social media/gay social networking apps and peers on SDU.
Methods
Participants and Data Collection
We conducted an observational prospective cohort study among MSM in Hong Kong, China from April 2018 to July 2019. Inclusion criteria for participants of the cohort study were the following: (1) Chinese-speaking men in Hong Kong, (2) aged 18 years or above, and (3) had anal intercourse with at least one man in the last 12 months. Participants were recruited through multiple sources. A recent mapping exercise was conducted by the government, which identified 12 gay bars and 16 gay saunas in Hong Kong. Upon obtaining the approval of the owners, trained and experienced fieldworkers approached prospective MSM participants in these venues at different time slots during weekdays and weekends. They briefed prospective participants about the study details and gave them an information sheet. The research team also conducted online outreach by posting information about the study periodically as discussion topics on the two gay websites with the highest traffic in Hong Kong. If prospective participants were interested in this study, they could contact the interviewers through private messaging or other means (eg, WhatsApp, telephone, email). Recruitment was supplemented by peer referrals. Participants were guaranteed anonymity during the study, and had the right to end participation in the study at any time. Their refusal or withdrawal from the study would not affect their access to any future services. Verbal consent was obtained instead of written consent to allow participants to maintain anonymity, and the fieldworkers signed a form pledging that the participants had been fully informed about the study. Multiple forms of contact information were obtained to make an appointment to conduct a baseline telephone interview. Trained telephone interviewers confirmed participants’ eligibility and consent to participate in the study, and conducted telephone interviews that took approximately 30 minutes to complete. Another telephone survey was conducted 6 months later. At least 5 follow-up calls were made during different time slots during weekdays and weekends before considering the participant lost to follow-up. Upon completion of both surveys, a HK $50 (US $6.45) supermarket or café coupon was mailed to participants as compensation for their time. Telephone numbers and addresses were cross-checked to avoid repetition. Of the 1131 prospective participants approached through outreach in gay venues (n=211), online recruitment (n=607), and peer referral (n=313), 711 were eligible for participation after screening (venues: n=117; online: n=401; referral: n=193). Of these, 600 provided verbal informed consent and completed the baseline telephone interview (venues: n=85; online: n=345; referral: n=170). The response rate was 84.3%. At Month 6, 407 (67.8%) participants completed the follow-up survey. The Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong approved this study (reference number 160051).
Measures
Design of the Questionnaires
A panel consisting of a public health researcher, an epidemiologist, a psychologist, an MSM community member, and a community-based organization worker was formed to develop the questionnaires. The questionnaires were tested by 10 local MSM. Based on their feedback, the questionnaires were then finalized by the panel.
Baseline Background Characteristics
Information collected included sociodemographics (age, highest education level attained, current marital status, monthly personal income, and current employment status), sexual orientation; utilization of HIV prevention services and PrEP; history of HIV and other STIs; and sexual behaviors with regular and nonregular male sex partners in the last year. A regular male sex partner (RP) was defined as a stable boyfriend, while a nonregular male sex partner (NRP) was defined as a casual sex partner or a male sex worker.
Patterns of SDU/Chemsex
In this study, SDU is defined as the use of any of the following psychoactive substances before or during sexual intercourse: ketamine, methamphetamine, cocaine, cannabis, ecstasy, Dormicum/Halcion/Erimin 5/nonprescription hypnotic drugs, heroin, cough suppressant (not for curing cough), amyl nitrite (popper), GHB/GBL, 5-methoxy-N, N-diisopropyltryptamine (Foxy), and mephedrone. We defined chemsex as the use of ketamine, methamphetamine, cocaine, GHB/GBL, or mephedrone before or during sexual intercourse. Such definitions have been used in a number of studies [3-5]. Participants were asked whether they had used any of the aforementioned psychoactive substances at baseline and Month 6 during different reference periods (baseline: lifetime and past year; Month 6: in the past 6 months).
Participants with SDU experience were asked about behavioral details, including the following: (1) types of psychoactive substance used during sexual intercourse, (2) poly-use of psychoactive substances during sexual intercourse, (3) time since the first episode of SDU, (4) frequency of SDU, (5) CAI during SDU, and (6) sexual risk behaviors during their most recent episode of SDU (ie, the number of participants; the use of alcohol and erectile dysfunction drugs; and the occurrence of CAI or group sex).
Influence of Social Media/Gay Social Networking Apps and Peers Measured at Baseline
Participants were asked to report the frequency of their exposure to the following information related to SDU on social media (eg, Facebook, Twitter, Instagram, Weibo) or gay social networking apps (eg, Grindr, Jack’d, Blued) in the last 12 months (eg, “Frequency of exposure to others’ personal experiences supporting psychoactive substance use”) with the following response categories: 1=Never, 2=Seldom, 3=Sometimes, and 4=Always. The Influence of Social Media Scale was formed by summing up individual item scores, with higher scores indicating higher levels of exposure to information supporting SDU from social media and gay social networking apps. The Cronbach α for this scale was .70, and a single factor was identified by exploratory factor analysis, explaining 70.1% of total variance. Additionally, the questionnaire also measured the number of peers in one’s social network who had experience with SDU (response categories: None, 1-2, 3-5, 6-10, and >10).
Perceptions Related to SDU Based on the TPB
Five scales derived from the TPB were constructed [40]. Positive attitudes toward SDU were measured by four items (eg, “It is easier for you to find sex partners when using psychoactive substances before/during sexual intercourse”). The Positive Attitude Scale was formed by summing up individual item scores (from 1=Strongly disagree to 5=Strongly agree). Higher scores on the scale indicated more positive attitudes toward SDU. The Cronbach α of the Positive Attitude Scale was .82; one factor was identified by exploratory factor analysis, explaining 65.1% of total variance.
Four items (with response options ranging from 1=Strongly disagree to 5=Strongly agree) were used to measure negative attitudes toward SDU (eg, “Using psychoactive substances before/during sexual intercourse would increase your risk of having CAI”). The Negative Attitude Scale was formed by summing up individual item scores. Higher scores on the scale indicated more negative attitudes toward SDU. The Cronbach α of the Negative Attitude Scale was .62; one factor was identified by exploratory factor analysis, explaining 63.0% of total variance.
Four items were used to measure participants’ perceived support from their significant others (referring to regular and nonregular male sex partners and MSM friends) for SDU. Items were measured on a 5-point Likert Scale from 1=Strongly disagree to 5=Strongly agree. The Perceived Subjective Norms for SDU among MSM Scale was constructed by summing up individual item scores. Higher scores indicated perceived subjective norms that were more supportive of SDU. The Cronbach α of the Perceived Subjective Norm Scale was .90; one factor was identified by exploratory factor analysis, explaining 76.8% of total variance.
Perceived behavioral control in refusing SDU and perceived behavioral control in refraining from SDU were measured by two items each. The Perceived Behavioral Control of Refusing SDU Scale and the Perceived Behavioral Control of Refraining from SDU Scale were formed by summing up individual item scores (from 1=Strongly disagree to 5=Strongly agree). Higher scores of the Perceived Behavioral Control of Refusing SDU Scale indicated lower levels of control of refusing SDU, while higher scores in the Perceived Behavioral Control of Refraining from SDU indicated higher levels of control of refraining from SDU. The Cronbach α of the Perceived Behavioral Control of Refusing SDU Scale and the Perceived Behavioral Control of Refraining from SDU Scale were .93 and .95, respectively; single factors were identified by exploratory factor analysis, explaining 93.5% and 95.6% of total variance, respectively.
Data Analyses
Baseline background characteristics of participants who were followed up at Month 6 and those who were lost to follow-up were compared using chi-square tests (for categorical variables) or independent sample t tests (for continuous variables). The subsequent analysis was performed among those who had completed both surveys. Using SDU during the follow-up period as the dependent variable, and background characteristics measured at baseline as independent variables, univariate odds ratios (OR) predicting the dependent variable were obtained using logistic regression models. After adjusting for variables with P<.05 in the univariate analysis, associations between independent variables of interest (ie, perceptions, the influence of social media and gay social networking apps and peers) and the dependent variable were then assessed by adjusted OR (AOR). Each AOR was obtained by fitting a single logistic regression model, which involved one of the independent variables of interest and the significant background variables.
Path analysis was conducted to test the mediation model. The means for social media influence and peer influence were used as independent variables, while SDU during the follow-up period was used as the dependent variable. The means of the Positive Attitude Scale, the Negative Attitude Scale, the Perceived Subjective Norm Scale, the Perceived Behavioral Control for Refusing SDU Scale, and the Perceived Behavioral Control for Refraining from SDU Scale were used as indicators to represent the latent variable of perceptions related to SDU based on the TPB; confirmatory factor analysis was then conducted to test the goodness of fit of this construct. All significant background variables were controlled for in the model. Goodness of fit was tested by using the chi-square test, the Comparative Fit Index (CFI), the Non-Normed Fit Index (NNFI), and the root mean square error of approximation (RMSEA). A CFI and NNFI greater than .90 and RMSEA lower than .08 indicated acceptable goodness of fit [41]. Standardized path coefficients (β) and unstandardized path coefficients (B) were reported. We tested the mediation analyses using bootstrapping. The 95% CI of the indirect effects were obtained from 5000 bootstrap samples. A statistically significant mediation effect was observed when the CI did not include zero. The level of statistical significance was .05. SPSS (Version 18.0, IBM Corp) and AMOS were used.
Results
Baseline Background Characteristics
Most of the 600 participants were 18 to 30 years old (n=342, 57.0%), currently single (n=504, 84.0%), employed full-time (n=498, 83.0%), with a monthly personal income of HK $20,000 (US $2580) or higher (n=336, 56.0%), and had attained at least a college education (n=505, 84.2%). Over half had received HIV antibody testing (n=430, 71.7%) and utilized other HIV prevention services (n=335, 55.8%) in the last year; 3.8% (n=23) were using PrEP at the time of the baseline survey. Among the participants, 3.3% (n=20) self-reported as living with HIV and 20.5% (n=123) had a history of other STIs. In the last year, 85.0% (n=510) and 60.5% (n=363) had had anal intercourse with RP and NRP, respectively. Furthermore, 40.2% (n=241) and 69.0% (n=414) reported CAI with men and multiple sex partnerships, respectively. The lifetime prevalence of SDU and chemsex were 19.3% (n=116) and 8.7% (n=52), respectively. Means and standard deviation of items/scales related to the influence of social media/gay apps, the influence of peers, and perceptions related to SDU based on the TPB were described in Table 1. No significant difference was found in baseline characteristics between those with follow-up data available (n=407) and those who were lost to follow-up at Month 6 (n=193), with the exception of self-reported HIV status (P=.04), the frequency of exposure to commentary/discussion about psychoactive substance use on social media/gay apps (P=.001), and the score on the Perceived Behavioral Control of Refraining from SDU Scale (P=.04).
Table 1.
Baseline characteristics of the participants.
| Characteristics | All participants (n=600) | Follow-up at Month 6 (n=407) | Loss to follow-up (n=193) | P value | ||
| Sociodemographics | ||||||
|
|
Age group (years), n (%) | .29 | ||||
|
|
|
18-24 | 124 (20.7) | 80 (19.7) | 44 (22.8) | |
|
|
|
25-30 | 218 (36.3) | 146 (35.9) | 72 (37.3) | |
|
|
|
31-40 | 187 (31.2) | 126 (31.0) | 61 (31.6) | |
|
|
|
>40 | 71 (11.8) | 55 (13.5) | 16 (8.3) | |
|
|
Highest educational level attained, n (%) | .73 | ||||
|
|
|
Senior high school or below | 95 (15.8) | 63 (15.5) | 32 (16.6) | |
|
|
|
College or above | 505 (84.2) | 344 (84.5) | 161 (83.4) | |
|
|
Current marital status, n (%) | .38 | ||||
|
|
|
Currently single | 504 (84.0) | 344 (84.5) | 160 (82.9) | |
|
|
|
Married/cohabiting with a man | 93 (15.5) | 60 (14.7) | 33 (17.1) | |
|
|
|
Married/cohabiting with a woman | 3 (0.5) | 3 (0.7) | 0 (0.0) | |
|
|
Monthly personal income (HK $), n (%) | >.99 | ||||
|
|
|
<10,000 (<US $1290) | 84 (14.0) | 57 (14.0) | 27 (14.0) | |
|
|
|
10,000-19,999 (US $1290-2580) | 174 (29.0) | 120 (29.5) | 54 (28.0) | |
|
|
|
20,000-39,999 (US $2580-3870) | 220 (36.7) | 148 (36.4) | 72 (37.3) | |
|
|
|
>40,000 (>US $5161) | 116 (19.3) | 78 (19.2) | 38 (19.7) | |
|
|
|
Refuse to disclose | 6 (1.0) | 4 (1.0) | 2 (1.0) | |
|
|
Current employment status, n (%) | .61 | ||||
|
|
|
Full-time | 498 (83.0) | 340 (83.5) | 158 (81.9) | |
|
|
|
Part-time/unemployed/retired/students | 102 (17.0) | 67 (16.5) | 35 (18.1) | |
|
|
Sexual orientation, n (%) | .35 | ||||
|
|
|
Homosexual | 546 (91.0) | 375 (92.1) | 171 (88.6) | |
|
|
|
Bisexual | 52 (8.7) | 31 (7.6) | 21 (10.9) | |
|
|
|
Heterosexual | 2 (0.3) | 1 (0.3) | 1 (0.5) | |
| Service utilization, n (%) | ||||||
|
|
HIV testing in the last 12 months | .15 | ||||
|
|
|
No | 170 (28.3) | 108 (26.5) | 62 (32.1) | |
|
|
|
Yes | 430 (71.7) | 299 (73.5) | 131 (67.9) | |
|
|
Other HIV prevention services in the last 12 months (eg, condom distribution, peer education, pamphlet and lectures) | .46 | ||||
|
|
|
No | 265 (44.2) | 184 (45.2) | 81 (42.0) | |
|
|
|
Yes | 335 (55.8) | 223 (54.8) | 112 (58.0) | |
|
|
Currently on PrEP (pre-exposure prophylaxis) | .78 | ||||
|
|
|
No | 577 (96.2) | 392 (96.3) | 185 (95.9) | |
|
|
|
Yes | 23 (3.8) | 15 (3.7) | 8 (4.1) | |
| History of HIV/sexually transmitted infections, n (%) | ||||||
|
|
Self-reported HIV status | .04 | ||||
|
|
|
Never tested for HIV | 26 (4.3) | 11 (2.7) | 15 (7.8) | |
|
|
|
Negative | 549 (91.5) | 380 (93.4) | 169 (87.6) | |
|
|
|
Positive | 20 (3.3) | 13 (3.2) | 7 (3.6) | |
|
|
|
Refuse to disclose | 5 (0.8) | 3 (0.7) | 2 (1.0) | |
|
|
History of other sexually transmitted infections | .76 | ||||
|
|
|
No | 477 (79.5) | 325 (79.9) | 152 (78.8) | |
|
|
|
Yes | 123 (20.5) | 82 (20.1) | 41 (21.2) | |
| Sexual behaviors in the last 12 months, n (%) | ||||||
|
|
Has had anal intercourse with regular male sex partners | .14 | ||||
|
|
|
No | 90 (15.0) | 55 (13.5) | 35 (18.1) | |
|
|
|
Yes | 510 (85.0) | 352 (86.5) | 158 (81.9) | |
|
|
Has had anal intercourse with nonregular male sex partners | .69 | ||||
|
|
|
No | 237 (39.5) | 163 (40.0) | 74 (38.3) | |
|
|
|
Yes | 363 (60.5) | 244 (60.0) | 119 (61.7) | |
|
|
Condomless anal intercourse with men | .33 | ||||
|
|
|
No | 359 (59.8) | 249 (61.2) | 110 (57.0) | |
|
|
|
Yes | 241 (40.2) | 158 (38.8) | 83 (43.0) | |
|
|
Multiple male sex partnerships | .88 | ||||
|
|
|
No | 186 (31.0) | 127 (31.2) | 59 (30.6) | |
|
|
|
Yes | 414 (69.0) | 280 (68.8) | 134 (69.4) | |
| Experience of sexualized drug use (SDU)a, n (%) | ||||||
|
|
SDU in lifetime | .61 | ||||
|
|
|
No | 484 (80.7) | 326 (80.1) | 158 (81.9) | |
|
|
|
Yes | 116 (19.3) | 81 (19.9) | 35 (18.1) | |
|
|
SDU in the past year | .68 | ||||
|
|
|
No | 512 (85.3) | 349 (85.7) | 163 (84.5) | |
|
|
|
Yes | 88 (14.7) | 58 (14.3) | 30 (15.5) | |
| Influence of social media related to SDU | ||||||
|
|
Frequency of exposure to information supporting SDU on social media/gay social networking apps in the past year, % Sometimes/Always | |||||
|
|
|
Sharing of personal experiences to support MSM using psychoactive substances | 253 (42.2) | 168 (41.3) | 85 (44.0) | .52 |
|
|
|
Sharing of personal experiences against MSM using psychoactive substances (reverse coded) | 180 (30.0) | 131 (32.2) | 49 (25.4) | .09 |
|
|
|
Receiving personal invitations to use psychoactive substances from MSM friends | 93 (15.5) | 58 (14.3) | 35 (18.1) | .22 |
|
|
|
Receiving personal invitations to have SDU/chemsex from MSM friends | 90 (15.0) | 55 (13.5) | 35 (18.1) | .14 |
|
|
|
Receiving personal invitations to use psychoactive substances from strangers | 212 (35.3) | 145 (35.6) | 67 (34.7) | .83 |
|
|
|
Receiving personal invitations to have SDU/chemsex from strangers | 218 (36.3) | 150 (36.9) | 68 (35.2) | .70 |
|
|
|
Commentary/discussion about psychoactive substance use | 168 (28.0) | 97 (23.8) | 71 (36.8) | .001 |
|
|
The Influence of Social Media Scale, mean (SD) | 7.7 (4.4) | 7.5 (4.3) | 8.1 (4.4) | .13 | |
| Influence of peers related to SDU | ||||||
|
|
Regular male sex partners had experience of SDU/chemsex, % Yes | 48 (8.0) | 39 (9.6) | 9 (4.7) | .04 | |
|
|
Nonregular male sex partners had experience of SDU/chemsex, % Yes | 109 (18.2) | 72 (17.7) | 37 (19.2) | .66 | |
|
|
Close friends had experience of SDU/chemsex, % Yes | 129 (21.5) | 94 (23.1) | 35 (18.1) | .17 | |
|
|
Other friends had experience of SDU/chemsex, % Yes | 229 (38.2) | 151 (37.1) | 78 (40.4) | .44 | |
|
|
Number of peers in one’s social network who had ever engaged in SDU/chemsex, n (%) | .62 | ||||
|
|
|
0 | 178 (29.7) | 121 (29.7) | 57 (29.5) | |
|
|
|
1-2 | 148 (24.7) | 104 (25.6) | 44 (22.8) | |
|
|
|
3-5 | 143 (23.8) | 92 (22.6) | 51 (26.4) | |
|
|
|
6-10 | 48 (8.0) | 36 (8.8) | 16 (8.2) | |
|
|
|
>10 | 83 (13.8) | 54 (13.3) | 29 (15.0) | |
| Perceptions related to SDU based on the Theory of Planned Behavior | ||||||
|
|
Positive attitudes toward SDU, % Agree/Strongly agree | |||||
|
|
|
SDU allows you temporary escape from reality | 106 (17.7) | 70 (17.2) | 36 (18.7) | .66 |
|
|
|
SDU increases your sexual pleasure | 139 (23.2) | 99 (24.3) | 40 (20.7) | .33 |
|
|
|
It is easier to find sex partners during SDU | 74 (12.3) | 47 (11.5) | 27 (14.0) | .40 |
|
|
|
SDU would heighten euphoria | 131 (21.8) | 93 (22.9) | 38 (19.7) | .38 |
|
|
Positive Attitude Scale, mean (SD) | 8.0 (4.2) | 8.8 (4.1) | 8.8 (4.3) | .93 | |
|
|
Negative attitudes toward SDU, % Agree/Strongly agree | |||||
|
|
|
SDU would harm your cognitive function | 558 (94.0) | 379 (93.1) | 185 (95.9) | .19 |
|
|
|
SDU would have negative impact on your relationship with sex partners | 384 (64.0) | 265 (65.1) | 119 (61.7) | .41 |
|
|
|
SDU would increase your risk of having condomless anal intercourse | 381 (63.5) | 258 (63.4) | 123 (63.7) | .94 |
|
|
|
SDU would increase your risk of HIV infection | 511 (85.2) | 341 (83.8) | 170 (88.1) | .17 |
|
|
Negative Attitude Scale, mean (SD) | 16.8 (2.9) | 16.7 (2.9) | 16.8 (2.8) | .72 | |
|
|
Perceived subjective norms related to SDU, % Agree/Strongly agree | |||||
|
|
|
Your male sex partners support you using psychoactive substances | 29 (4.8) | 19 (4.7) | 10 (5.2) | .78 |
|
|
|
Your other MSM friends support you using psychoactive substances | 17 (2.8) | 12 (2.9) | 5 (2.6) | .81 |
|
|
|
Your male sex partners support you having SDU | 21 (3.5) | 14 (3.4) | 7 (3.6) | .91 |
|
|
|
Your other MSM friends support you having SDU | 11 (1.8) | 8 (2.0) | 3 (1.6) | .73 |
|
|
Perceived Subjective Norms Scale, mean (SD) | 5.9 (3.1) | 5.8 (3.1) | 6.0 (3.0) | .40 | |
|
|
Perceived behavioral control of refusing SDU, % Agree/Strongly agree | |||||
|
|
|
If your sex partner asks you to use psychoactive substances, it is difficult for you to refuse | 60 (10.0) | 36 (8.8) | 24 (12.4) | .17 |
|
|
|
If your sex partner asks you to have SDU, it is difficult for you to refuse | 55 (9.2) | 31 (7.6) | 24 (12.4) | .06 |
|
|
Perceived Behavioral Control of Refusing SDU Scale, mean (SD) | 3.5 (2.2) | 3.4 (2.1) | 3.7 (2.3) | .10 | |
|
|
Perceived behavioral control of refraining from SDU, % Agree/Strongly agree | |||||
|
|
|
You can exercise self-control to stop using psychoactive substance | 541 (90.2) | 371 (91.2) | 170 (88.1) | .24 |
|
|
|
You can exercise self-control to stop having SDU | 550 (91.7) | 378 (92.9) | 172 (89.1) | .12 |
|
|
Perceived Behavioral Control of Refraining from SDU Scale, mean (SD) | 9.2 (1.7) | 9.3 (1.5) | 9.0 (2.0) | .04 | |
aSDU: sexualized drug use. Sexualized drug use is defined as the use of any of the following psychoactive substances before/during anal intercourse: ketamine, methamphetamine, cocaine, cannabis, ecstasy, Dormicum/Halcion/Erimin 5/nonprescription hypnotic drugs, heroin, cough suppressant (not for curing cough), amyl nitrite (popper), GHB/GBL (γ-hydroxybutyrate), 5-methoxy-N, N-diisopropyltryptamine (Foxy), and mephedrone.
Patterns of SDU and Chemsex at Baseline and Month 6
At baseline, 14.7% (88/600) and 6.7% (40/600) of the participants reported SDU and chemsex in the past year, respectively. During the 6-month follow-up period, their prevalence was 6.9% (28/407) and 4.4% (18/407), respectively. Among 58 participants with experience of SDU who completed the Month 6 follow-up survey, 36% (n=21) reported SDU during the follow-up period. Among 26 MSM who had chemsex at baseline and completed the Month 6 follow-up survey, 14 (54%) reported chemsex during the follow-up period.
Patterns of SDU one year prior to the baseline and during the 6-month follow-up period were similar. Amyl nitrite, methamphetamine, and GHB/GBL were the most commonly used psychoactive substances during sexual intercourse. About half of MSM who reported SDU reported poly-use of psychoactive substances and CAI. SDU commonly involved more than two people, the use of erectile dysfunction drugs, and group sex (Table 2).
Table 2.
Patterns of sexualized drug use in different reference periods.
| Variables | One year prior to baseline survey (among MSMa who reported sexualized drug use in the past year at baseline, n=88), n (%) | During the 6-month follow-up period (among MSM who reported sexualized drug use during the follow-up, n=28), n (%) | ||
| Types of psychoactive substance used during chemsex | ||||
|
|
Ketamine | 2 (2.3) | 2 (7.1) | |
|
|
Methamphetamine | 32 (36.4) | 11 (39.3) | |
|
|
Cocaine | 0 (0.0) | 0 (0.0) | |
|
|
Cannabis | 7 (8.0) | 1 (3.6) | |
|
|
Ecstasy | 2 (2.3) | 2 (7.1) | |
|
|
Dormicum/Halcion/Erimin 5/Hypnotic drugs (nonprescription) | 0 (0.0) | 1 (3.6) | |
|
|
Heroin | 0 (0.0) | 0 (0.0) | |
|
|
Cough suppressant (not for curing cough) | 1 (1.1) | 2 (7.1) | |
|
|
Amyl nitrite | 69 (78.4) | 20 (71.4) | |
|
|
γ-hydroxybutyrate (GHB/GBL) | 29 (33.0) | 10 (35.7) | |
|
|
5-methoxy-N, N-diisopropyltryptamine | 5 (5.7) | 1 (3.6) | |
|
|
Mephedrone | 0 (0.0) | 1 (3.6) | |
| Poly-use of psychoactive substances | ||||
|
|
No | 57 (64.8) | 14 (50.0) | |
|
|
Yes | 31 (35.2) | 14 (50.0) | |
| Frequency of sexualized drug use | ||||
|
|
<1 episode/month | 0 (0.0) | 13 (46.4) | |
|
|
1 episode/month | 35 (39.8) | 11 (39.3) | |
|
|
1-2 episodes/month | 24 (27.3) | 2 (7.1) | |
|
|
≥3 episodes/month | 29 (33.0) | 2 (7.1) | |
| Condomless anal intercourse during sexualized drug use | ||||
|
|
No | 41 (46.6) | 10 (35.7) | |
|
|
Yes | 47 (53.4) | 18 (64.3) | |
| Characteristics of most recent episode of sexualized drug use | ||||
|
|
Number of participants | |||
|
|
|
2 | 67 (76.1) | 19 (67.9) |
|
|
|
≥3 | 21 (23.9) | 9 (32.1) |
|
|
Alcohol consumption | |||
|
|
|
No | 77 (87.5) | 28 (100.0) |
|
|
|
Yes | 11 (12.5) | 0 (0.0) |
|
|
Use of erectile dysfunction drugs | |||
|
|
|
No | 62 (70.5) | 16 (57.9) |
|
|
|
Yes | 26 (29.5) | 12 (42.1) |
|
|
Group sex | |||
|
|
|
No | 18 (20.5) | 11 (39.3) |
|
|
|
Yes | 70 (79.5) | 17 (60.7) |
|
|
Condomless anal intercourse | |||
|
|
|
No | 45 (51.1) | 15 (53.6) |
|
|
|
Yes | 43 (48.9) | 13 (46.4) |
aMSM: men who have sex with men.
Baseline Factors Predicting SDU During the Follow-Up Period
Baseline background variables that were significantly associated with SDU during the follow-up period included the following: (1) currently on PrEP, (2) self-reported living with HIV, (3) history of other STI, (4) any anal intercourse with NRP, (5) CAI with any male sexual partners, (6) multiple male sex partnerships, and (7) SDU in the past year (Table 3).
Table 3.
Baseline background variables associated with sexualized drug use during the follow-up period for MSM in Hong Kong (among those being followed up at Month 6, n=407).
| Variables | Participants, n (%) | ORa (95% CI) | ||
| Sociodemographics measured at baseline | ||||
|
|
Age group (years) | |||
|
|
|
18-24 | 4 (5.0) | 1.0 |
|
|
|
25-30 | 10 (6.8) | 1.40 (0.42-4.61) |
|
|
|
31-40 | 11 (8.7) | 1.82 (0.56-5.92) |
|
|
|
>40 | 3 (5.5) | 1.10 (0.24-5.10) |
|
|
Highest educational level attained | |||
|
|
|
Senior high school or below | 7 (11.1) | 1.0 |
|
|
|
College or above | 21 (6.1) | 0.52 (0.21-1.28) |
|
|
Current marital status | |||
|
|
|
Currently single | 24 (7.0) | 1.0 |
|
|
|
Married/cohabiting with a man | 3 (5.0) | 0.70 (0.21-2.41) |
|
|
|
Married/cohabiting with a woman | 1 (33.3) | 6.67 (0.58-76.18) |
|
|
Monthly personal income (HK $) | |||
|
|
|
<10,000 (<US $1290) | 5 (8.8) | 1.0 |
|
|
|
10,000-19,999 (US $1290-2580) | 6 (5.0) | 0.55 (0.16-1.88) |
|
|
|
20,000-39,999 (US $2580-3870) | 12 (8.1) | 0.92 (0.31-2.73) |
|
|
|
>40,000 (>US $5161) | 5 (6.4) | 0.71 (0.20-2.59) |
|
|
|
Refuse to disclose | 0 (0.0) | N/Ab |
|
|
Current employment status | |||
|
|
|
Full-time | 21 (6.2) | 1.0 |
|
|
|
Part-time/unemployed/retired/student | 7 (10.4) | 1.77 (0.72-4.35) |
|
|
Sexual orientation | |||
|
|
|
Homosexual | 27 (7.2) | 1.0 |
|
|
|
Bisexual | 1 (3.2) | 0.43 (0.05-3.27) |
|
|
|
Heterosexual | 0 (0.0) | N/A |
| Service utilization measured at baseline | ||||
|
|
HIV testing in the last 12 months | |||
|
|
|
No | 4 (3.7) | 1.0 |
|
|
|
Yes | 24 (8.0) | 2.27 (0.77-6.70) |
|
|
Other HIV prevention services in the last 12 months (eg, condom distribution, peer education, pamphlets, lectures) | |||
|
|
|
No | 12 (6.5) | 1.0 |
|
|
|
Yes | 16 (7.2) | 1.11 (0.51-2.41) |
|
|
Currently on PrEP (pre-exposure prophylaxis) | |||
|
|
|
No | 23 (5.9) | 1.0 |
|
|
|
Yes | 5 (33.3) | 8.02 (2.53-25.42)c |
| History of HIV/sexual transmitted infections | ||||
|
|
Self-reported HIV status | |||
|
|
|
Negative/never tested for HIV/refuse to disclose | 24 (6.1) | 1.0 |
|
|
|
Positive | 4 (30.8) | 6.85 (1.97-23.87)d |
|
|
History of other sexually transmitted infections | |||
|
|
|
No | 16 (4.9) | 1.0 |
|
|
|
Yes | 12 (14.6) | 3.31 (1.50-7.31)d |
| Sexual behaviors in the last 12 months as measured at baseline | ||||
|
|
Anal intercourse with regular male sex partners | |||
|
|
|
No | 2 (3.6) | 1.0 |
|
|
|
Yes | 26 (7.4) | 2.11 (.49-9.17) |
|
|
Anal intercourse with nonregular male sex partners | |||
|
|
|
No | 1 (.6) | 1.0 |
|
|
|
Yes | 27 (11.1) | 20.16 (2.71-149.88)d |
|
|
Condomless anal intercourse with men | |||
|
|
|
No | 8 (3.2) | 1.0 |
|
|
|
Yes | 20 (12.7) | 4.37 (1.87-10.18)d |
|
|
Multiple male sex partnerships | |||
|
|
|
No | 0 (0) | N/A |
|
|
|
Yes | 28 (10.0) | N/Ae |
| Experience of sexualized drug use as measured at baseline | ||||
|
|
Sexualized drug use in the past year | |||
|
|
|
No | 7 (2.0) | 1.0 |
|
|
|
Yes | 21 (36.2) | 27.73 (11.05-69.60)c |
aOR: univariate odds ratio.
bN/A: not applicable.
cP<.001.
dP<.01.
eP<.05.
After adjusting for significant variables, three constructs of the TPB measured at baseline were significantly associated with SDU during the follow-up period. These constructs included: (1) positive attitudes toward SDU (AOR 1.19, 95% CI 1.05-1.36), (2) perceived support for SDU from significant others (AOR 1.15, 95% CI 1.01-1.30), and (3) perceived behavioral control of refraining from SDU (AOR 0.76, 95% CI 0.59-0.98). A higher level of exposure to information supporting SDU on social media/gay apps as measured at baseline was associated with a higher likelihood of SDU during the follow-up period (AOR 1.11, 95% CI 1.01-1.22). The association between the number of peers in one’s social network who had ever engaged in SDU and the dependent variable was of marginal statistical significance (AOR 1.43, 95% CI 0.95-2.16, P=.06; Table 4.
Table 4.
Factors associated with sexualized drug use during the follow-up period (among those being followed up at Month 6, n=407)a.
| Factors | ORb (95% CI) | AORc (95% CI) | |
| Influence of social media/gay apps related to sexualized drug use | |||
|
|
Influence of Social Media Scale | 1.23 (1.13, 1.34)d | 1.11 (1.01, 1.22)e |
| Influence of peers related to sexualized drug use | |||
|
|
Number of peers in one’s social network who had ever engaged in SDU/chemsex | 2.29 (1.67, 3.14)d | 1.43 (0.95, 2.16)f |
| Perceptions related to sexualized drug use based on the Theory of Planned Behavior | |||
|
|
Positive Attitude Scale | 1.33 (1.19, 1.47)d | 1.19 (1.05, 1.36)g |
|
|
Negative Attitude Scale | 0.86 (0.76, 0.97)e | 0.99 (0.84, 1.16) |
|
|
Perceived Subjective Norm Scale | 1.29 (1.18, 1.42)d | 1.15 (1.01, 1.30)e |
|
|
Perceived Behavioral Control of Refusing Sexualized Drug Use Scale | 1.33 (1.15, 1.55)d | 1.08 (0.89, 1.33) |
|
|
Perceived Behavioral Control of Refraining from Sexualized Drug Use Scale | 0.76 (0.64, 0.91)g | 0.76 (0.59, 0.98)e |
a6.9% of participants reported sexualized drug use during the follow-up period.
bOR: univariate odds ratio. The OR represents the increase in the odds of sexualized drug use caused by a one-unit increase in the item/scale score.
cAOR: adjusted odds ratio. The AOR is adjusted for the significant background variables listed in Table 3 and multiple sex partnerships in the past year.
dP<.001.
eP<.05.
f.05<P<.10.
gP<.01.
Testing the Mediation Effects of TPB Constructs in the Association Between Social Media/Peers Influences and SDU
Model Testing
The results of the confirmatory factor analysis found that perceptions related to SDU based on the TPB did not show adequate model fit to the data (χ25=19.01, P<.01; CFI=.94; NNFI=.89; RMSEA=.08). Modification indices suggested adding a covariance between the Perceived Behavioral Control of Refusing SDU Scale’s error and the Perceived Behavioral Control of Refraining from SDU Scale’s error (B=–0.58, P<.001). Since the two scales are related constructs [19], we added the covariance accordingly. The modified model showed excellent fit (χ24=3.81, P=.43; CFI=.99; NNFI=.99; RMSEA=.01). The chi-square test showed that the model fit change was significant (χ2 change=15.20, degrees of freedom change=1, P<.05). All factor loadings were significant at P<.001, with absolute values of standardized coefficients greater than .25. The mediation model fit the data well (χ2147=188.71, P<.05; CFI=.92; NNFI=.91; RMSEA=.06; Figure 1).
Figure 1.
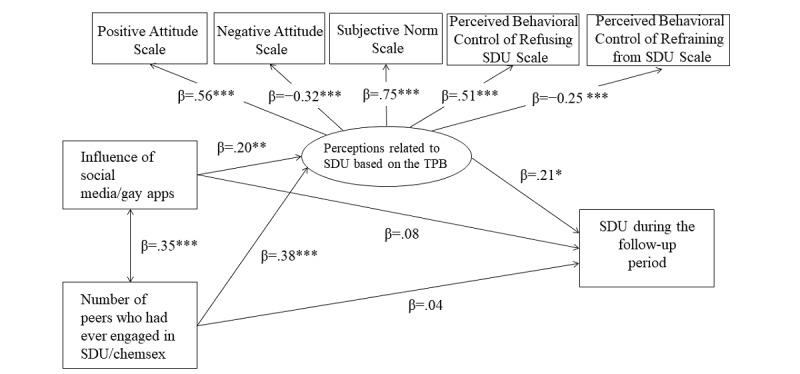
The proposed mediation models with standardized path coefficients. *P<.05; **P<.01; ***P<.001. SDU: sexualized drug use; TPB: Theory of Planned Behavior.
Path Coefficients
The influence of social media/gay apps was positively associated with perceptions related to SDU based on the TPB (β=.20, B=.11, P=.001), while it was not significantly associated with SDU (β=.08, B=.004, P=.11). Peer influence was positively associated with perceptions related to SDU based on the TPB (β=.38, B=.68, P<.001), while it was not significantly associated with SDU (β=.04, B=.01, P=.50). Perceptions related to SDU based on the TPB was positively associated with SDU (β=.21, B=.02, P=.02).
Mediation Effects
Bootstrapping analyses indicated that social media influence had a significant indirect effect on SDU through perceptions of SDU in the hypothesized direction (β=.04, B=.002, 95% CI 0.001-0.01). However, peer influence was not significantly associated with SDU through perceptions of SDU (β=.08, B=.01, 95% CI –0.002 to 0.04).
Discussion
We found that 6.9% and 4.4% of MSM in Hong Kong practiced SDU and chemsex at the end of the 6-month follow-up period. Such prevalence was lower than that reported among MSM in Western Europe. At Month 6, about half of participants having SDU or chemsex at baseline refrained from these behaviors, while very few initiated these behaviors. Studies with longer follow-up periods are needed in the future to understand trends in SDU and chemsex among MSM in Hong Kong. Such studies are useful to understand the effectiveness of SDU/chemsex interventions conducted by local community-based organizations.
Similar to studies conducted in Western countries, amyl nitrite, methamphetamine, and GHB/GBL were the most commonly used psychoactive substances during SDU at both baseline and Month 6 [7]. The prevalence of risky practices during SDU (ie, poly-use of psychoactive substance, CAI, and group sex) was high at both time points. Effective risk reduction strategies should be explored to address these risky practices.
According to social marketing approaches, careful segmentation improves the effectiveness of health promotion programs [42]. First, heath care workers and interventions should tailor SDU and chemsex reduction measures to MSM living with HIV. Similar to findings conducted in mainland China [43] and other countries [3], MSM living with HIV were more likely to practice SDU compared to HIV-negative or status unknown MSM. They have a high risk of HIV transmission through SDU. For MSM living with HIV, SDU may be a potential maladaptive coping method for stressful situations caused by perceived stigma and experiences of violence and prejudice [44]. Reducing substance use during sex should be an essential part of care for MSM living with HIV. Second, health care workers and interventionists should focus on MSM with multiple risk behaviors (eg, anal intercourse with NRP, CAI, and multiple male sex partnerships), as these participants were more likely to practice SDU. Those with experience of SDU at baseline also had a much higher risk of practicing SDU during the 6-month follow-up period compared to those who had never practiced SDU. Moreover, MSM who were on PrEP reported higher likelihood of SDU than those not on PrEP. Studies conducted both locally and internationally consistently demonstrated the significant association between SDU and PrEP use [3,24]. This association may be due to the fact that some MSM may continue or initiate SDU as PrEP has minimized their risk of HIV infection. Health care providers supervising MSM on PrEP should continue to provide education about other sexual risks of SDU, such as acquiring STIs, or reduced adherence to PrEP.
Our results showed that MSM in Hong Kong are frequently exposed to information about psychoactive substances and received invitations to use such substances or engage in SDU/chemsex on social media and gay social networking apps. This exposure was associated with a higher prevalence of SDU during the follow-up period. Previous studies consistently showed that social media and gay social networking apps have facilitated access to psychoactive substances, SDU, and chemsex for MSM [18,25,26]. One of the important contributions of this study is that it examined the potential mechanism of the associations between social media and peer influences and SDU. Our results suggest that social media exposure may enhance positive perceptions of SDU, which in turn increase the risk of SDU. The significant mediation effect supports mechanisms proposed by the Social Learning Theory [38] to understand how social media may influence one’s behavior related to SDU. Most social media sites allow users to leave comments, and express approval or disapproval of the contents. Therefore, users can see how many others (and sometimes exactly who) expressed approval when they view social media. This may explain why MSM find social media content to be a believable and influential source of information. Gay social networking apps provide a quick and convenient way to locate and connect with other MSM nearby, and MSM commonly use these apps to seek SDU or chemsex [18,25-28]. Gay social networking app users may perceive SDU as normative as many users may openly solicit SDU or chemsex in their online profiles [18,25,26]. Additionally, receiving a personal invitation of SDU through these apps may make MSM less likely to refuse. Interventions should consider disseminating messages on reducing harm associated with SDU and chemsex on gay apps platforms to reduce perceptions of SDU as normative.
The association between the number of peers in their social network who had experience with SDU/chemsex and SDU was of marginal statistical significance. Previous studies suggested that peers are common sources of obtaining psychoactive substances among MSM [33,34]. It is also common for MSM to introduce and invite peers to have SDU or chemsex [33,34]. However, the TPB perceptions of SDU were not a significant mediator between peer influence and SDU. Other potential theory-based mediators should be explored in future work. We found significant correlations between peer influence and social media influence, and between peer influence and TPB constructs. MSM in Hong Kong contact each other mainly through social media and gay apps. Some of these peers may be online friends that they have never physically met. Since MSM have very close connections to each other, they may find their peers’ experiences particularly valuable [32]. Furthermore, knowing more peers who practice SDU may make MSM perceive such behavior as normative.
These results highlight the importance of modifying perceptions related to SDU based on the TPB. About 20% of the participants held positive attitudes toward SDU. They perceived that SDU would allow them escape from reality, increase their sexual pleasure, and facilitate finding sex partners. Given our findings about the indirect effect of social media influence on SDU behavior, interventions should use social media to shape these attitudes. Health communication messages about reducing substance use during sex and increasing MSM’s awareness of the harms associated with SDU and chemsex can be disseminated using the same keywords used to promote SDU and chemsex, allowing the messages to reach MSM at high risk of SDU and chemsex. Gay social networking apps are also useful for delivering such health communication messages. Some apps widely used in Hong Kong (eg, Blued) have incorporated HIV prevention information and referral to HIV testing services [45]. Although less than 5% of the participants perceived support for SDU from significant others, such perceptions were positively associated with SDU during the follow-up period. Health promotion efforts led by influential peers may be useful to cultivate subjective norms against SDU. Health promotion campaigns may also consider sponsoring support groups led by peers living healthy lifestyles to reduce the influence of substance-using peers. Perceived behavioral control of refraining from SDU needs to be further strengthened as it was a protective factor. Enhancement in self-control skills is warranted and rehearsals may be a useful component of future health promotion programs.
This study had some limitations. First, the results were self-reported and subject to social desirability bias, although anonymity likely reduced the bias compared to nonanonymously collected data. Second, participants were recruited by nonprobabilistic sampling in the absence of a sampling frame. As compared to a representative MSM survey in Hong Kong, our participants had a lower prevalence of HIV and sexual risk behaviors, but higher levels of HIV testing. Third, we were not able to obtain the characteristics of participants who refused to join the study; selection bias might exist. However, the response rate for our study was higher than in other published studies involving MSM in China. Fourth, we did not ask behavioral intention to have SDU or chemsex at baseline. Behavioral intention is an important construct of the TPB that predicts actual behaviors [46]. Furthermore, attrition bias might exist. Those who had lower perceived behavioral control in refraining from SDU were more likely to drop out. Perceived behavioral control in refraining from SDU was a protective factor of SDU. Therefore, the prevalence of SDU during the follow-up period is expected to be higher. Finally, the Negative Attitude Scale had a relatively low Cronbach α (.62) in our sample. Although previous studies suggested that Cronbach α≥.60 was acceptable for exploratory research [47,48], caution is still needed when interpreting the results. Future studies are needed to validate this scale.
In sum, MSM in Hong Kong reported a lower prevalence of SDU and chemsex than that of their counterparts in Western countries. Social media and gay social networking apps may be a major source of influence on MSM’s perceptions and actual behaviors related to SDU, and interventions delivered on these platforms may be especially effective.
Acknowledgments
The authors would like to thank Ms Willa Dong at the Department of Health Behavior, Gillings School of Global Public Health, the University of North Carolina at Chapel Hill for proofreading and correcting the manuscript.
This study was supported by the Beat Drugs Fund, Narcotics Division, Security Bureau of Hong Kong SAR, China (reference number 160051). The funder had no role in study design; collection, analysis, or interpretation of the data; writing the manuscript, or the decision to submit the paper for publication.
Abbreviations
- AOR
adjusted odds ratio
- CAI
condomless anal intercourse
- CFI
Comparative Fit Index
- GHB/GBL
γ-hydroxybutyrate
- MSM
men who have sex with men
- NNFI
Non-Normed Fit Index
- NRP
nonregular partner
- PrEP
pre-exposure prophylaxis
- RMSEA
root mean square error of approximation
- RP
regular partner
- SDU
sexualized drug use
- STI
sexually transmitted infection
- TPB
Theory of Planned Behavior
Footnotes
Conflicts of Interest: None declared.
References
- 1.Halkitis PN, Parsons JT, Stirratt MJ. A Double Epidemic. Journal of Homosexuality. 2001 Jul 10;41(2):17–35. doi: 10.1300/j082v41n02_02. [DOI] [PubMed] [Google Scholar]
- 2.Edmundson C, Heinsbroek E, Glass R, Hope V, Mohammed H, White M, Desai M. Sexualised drug use in the United Kingdom (UK): A review of the literature. International Journal of Drug Policy. 2018 May;55:131–148. doi: 10.1016/j.drugpo.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Maxwell S, Shahmanesh M, Gafos M. Chemsex behaviours among men who have sex with men: A systematic review of the literature. International Journal of Drug Policy. 2019 Jan;63:74–89. doi: 10.1016/j.drugpo.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 4.Evers YJ, Van Liere GAFS, Hoebe CJPA, Dukers-Muijrers NHTM. Chemsex among men who have sex with men living outside major cities and associations with sexually transmitted infections: A cross-sectional study in the Netherlands. PLoS ONE. 2019 May 14;14(5):e0216732. doi: 10.1371/journal.pone.0216732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hibbert MP, Brett CE, Porcellato LA, Hope VD. Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sex Transm Infect. 2019 Apr 12;95(5):342–350. doi: 10.1136/sextrans-2018-053933. [DOI] [PubMed] [Google Scholar]
- 6.Tomkins A, George R, Kliner M. Sexualised drug taking among men who have sex with men: a systematic review. Perspect Public Health. 2018 May 30;139(1):23–33. doi: 10.1177/1757913918778872. [DOI] [PubMed] [Google Scholar]
- 7.Wong NS, Kwan TH, Lee KCK, Lau JYC, Lee SS. Delineation of chemsex patterns of men who have sex with men in association with their sexual networks and linkage to HIV prevention. International Journal of Drug Policy. 2020 Jan;75:102591. doi: 10.1016/j.drugpo.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 8.Kohli M, Hickson F, Free C, Reid D, Weatherburn P. Cross-sectional analysis of chemsex drug use and gonorrhoea diagnosis among men who have sex with men in the UK. Sex Health. 2019;16(5):464. doi: 10.1071/sh18159. [DOI] [PubMed] [Google Scholar]
- 9.Sewell J, Cambiano V, Speakman A, Lampe FC, Phillips A, Stuart D, Gilson R, Asboe D, Nwokolo N, Clarke A, Rodger AJ. Changes in chemsex and sexual behaviour over time, among a cohort of MSM in London and Brighton: Findings from the AURAH2 study. International Journal of Drug Policy. 2019 Jun;68:54–61. doi: 10.1016/j.drugpo.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 10.Logan L, Fakoya I, Howarth A, Murphy Gary, Johnson Anne M, Rodger Alison J, Burns Fiona, Nardone Anthony. Combination prevention and HIV: a cross-sectional community survey of gay and bisexual men in London, October to December 2016. Euro Surveill. 2019 Jun;24(25):1800312. doi: 10.2807/1560-7917.ES.2019.24.25.1800312. http://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2019.24.25.1800312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurtz SP. Post-Circuit Blues: Motivations and Consequences of Crystal Meth Use Among Gay Men in Miami. AIDS Behav. 2005 Mar;9(1):63–72. doi: 10.1007/s10461-005-1682-3. [DOI] [PubMed] [Google Scholar]
- 12.Stevens O, Moncrieff M, Gafos M. Chemsex-related drug use and its association with health outcomes in men who have sex with men: a cross-sectional analysis of Antidote clinic service data. Sex Transm Infect. 2019 Jun 06;96(2):124–130. doi: 10.1136/sextrans-2019-054040. [DOI] [PubMed] [Google Scholar]
- 13.Centre for Health Protection Factsheet: PRiSM --- HIV prevalence and risk behavioural survey of men who have sex with men in Hong Kong 2017. 2018. [2020-06-30]. https://www.aids.gov.hk/english/surveillance/sur_report/prism2017e.pdf.
- 14.Coffin PO, Santos G, Colfax G, Das M, Matheson T, DeMicco E, Dilley J, Vittinghoff E, Raiford JL, Carry M, Herbst JH. Adapted Personalized Cognitive Counseling for Episodic Substance-Using Men Who Have Sex with Men: A Randomized Controlled Trial. AIDS Behav. 2014 Feb 9;18(7):1390–1400. doi: 10.1007/s10461-014-0712-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santos G, Coffin PO, Vittinghoff E, DeMicco E, Das M, Matheson T, Raiford JL, Carry M, Colfax G, Herbst JH, Dilley JW. Substance use and drinking outcomes in Personalized Cognitive Counseling randomized trial for episodic substance-using men who have sex with men. Drug and Alcohol Dependence. 2014 May;138:234–239. doi: 10.1016/j.drugalcdep.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kurtz SP, Stall RD, Buttram ME, Surratt HL, Chen M. A Randomized Trial of a Behavioral Intervention for High Risk Substance-Using MSM. AIDS Behav. 2013 Jun 4;17(9):2914–2926. doi: 10.1007/s10461-013-0531-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mansergh G, Koblin BA, McKirnan DJ, Hudson SM, Flores SA, Wiegand RE, Purcell DW, Colfax GN. An Intervention to Reduce HIV Risk Behavior of Substance-Using Men Who Have Sex with Men: A Two-Group Randomized Trial with a Nonrandomized Third Group. PLoS Med. 2010 Aug 24;7(8):e1000329. doi: 10.1371/journal.pmed.1000329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan RKJ, Wong CM, Chen MI, Chan YY, Bin Ibrahim MA, Lim OZ, Chio MT, Wong CS, Chan RKW, Chua LJ, Choong BCH. Chemsex among gay, bisexual, and other men who have sex with men in Singapore and the challenges ahead: A qualitative study. International Journal of Drug Policy. 2018 Nov;61:31–37. doi: 10.1016/j.drugpo.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991 Dec;50(2):179–211. doi: 10.1016/0749-5978(91)90020-t. [DOI] [Google Scholar]
- 20.Roberto AJ, Shafer MS, Marmo J. Predicting substance-abuse treatment providers' communication with clients about medication assisted treatment: A test of the theories of reasoned action and planned behavior. Journal of Substance Abuse Treatment. 2014 Nov;47(5):307–313. doi: 10.1016/j.jsat.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Vederhus J, Zemore SE, Rise J, Clausen T, Høie M. Predicting patient post-detoxification engagement in 12-step groups with an extended version of the theory of planned behavior. Addict Sci Clin Pract. 2015 Jun 20;10(1):15. doi: 10.1186/s13722-015-0036-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kao E. 96% of Hongkongers use their smartphone to go online everyday. [2020-06-30]. http://www.scmp.com/news/hong-kong/article/1298330/hong-kong-smartphone-use-doubles-two-years.
- 23.Statista Research Department Hong Kong social network penetration Q2-Q3 2018. [2020-06-30]. https://www.statista.com/statistics/412500/hk-social-network-penetration/
- 24.Kwan TH, Lee SS. Bridging Awareness and Acceptance of Pre-Exposure Prophylaxis Among Men Who Have Sex With Men and the Need for Targeting Chemsex and HIV Testing: Cross-Sectional Survey. JMIR Public Health Surveill. 2019 Jul 03;5(3):e13083. doi: 10.2196/13083. https://publichealth.jmir.org/2019/3/e13083/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bourne A, Reid D, Hickson F, Torres RS, Weatherburn P. The Chemsex Study: drug use in sexual settings among gay and bisexual men in Lambeth, Southwark & Lewisham. Technical Report. Sigma Research, London School of Hygiene & Tropical Medicine, London. [2020-06-30]. https://www.lambeth.gov.uk/sites/default/files/ssh-chemsex-study-final-main-report.pdf.
- 26.Van Hout MC, Crowley D, O’Dea S, Clarke S. Chasing the rainbow: pleasure, sex-based sociality and consumerism in navigating and exiting the Irish Chemsex scene. Culture, Health & Sexuality. 2019 Jan 02;21(9):1074–1086. doi: 10.1080/13691058.2018.1529336. [DOI] [PubMed] [Google Scholar]
- 27.Yeo TED, Ng YL. Sexual risk behaviors among apps-using young men who have sex with men in Hong Kong. AIDS Care. 2015 Oct 07;28(3):314–318. doi: 10.1080/09540121.2015.1093597. [DOI] [PubMed] [Google Scholar]
- 28.Young SD, Nianogo RA, Chiu CJ, Menacho L, Galea J. Substance use and sexual risk behaviors among Peruvian MSM social media users. AIDS Care. 2015 Sep 14;28(1):112–118. doi: 10.1080/09540121.2015.1069789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cavazos-Rehg P, Krauss M, Grucza R, Bierut L. Characterizing the followers and tweets of a marijuana-focused Twitter handle. J Med Internet Res. 2014 Jun 27;16(6):e157. doi: 10.2196/jmir.3247. https://www.jmir.org/2014/6/e157/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cavazos-Rehg PA, Krauss M, Fisher SL, Salyer P, Grucza RA, Bierut LJ. Twitter Chatter About Marijuana. Journal of Adolescent Health. 2015 Feb;56(2):139–145. doi: 10.1016/j.jadohealth.2014.10.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kelly JA, Amirkhanian YA, Seal DW, Galletly CM, DiFranceisco W, Glasman LR, Stevenson LY, Rosado N. Levels and Predictors of Sexual HIV Risk in Social Networks of Men who Have Sex with Men in the Midwest. AIDS Education and Prevention. 2010 Dec;22(6):483–495. doi: 10.1521/aeap.2010.22.6.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yun Gao M, Wang S. Participatory communication and HIV/AIDS prevention in a Chinese marginalized (MSM) population. AIDS Care. 2007 Jun 14;19(6):799–810. doi: 10.1080/09540120601114832. [DOI] [PubMed] [Google Scholar]
- 33.Harrison PA, Fulkerson JA, Park E. The Relative Importance of Social Versus Commercial Sources in Youth Access to Tobacco, Alcohol, and Other Drugs. Preventive Medicine. 2000 Jul;31(1):39–48. doi: 10.1006/pmed.2000.0691. [DOI] [PubMed] [Google Scholar]
- 34.McCabe SE, Boyd CJ. Sources of prescription drugs for illicit use. Addictive Behaviors. 2005 Aug;30(7):1342–1350. doi: 10.1016/j.addbeh.2005.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tyler KA, Handema R, Schmitz RM, Phiri F, Kuyper KS, Wood C. Multi-Level Risk and Protective Factors for Substance Use Among Zambian Street Youth. Substance Use & Misuse. 2016 May 04;51(7):922–931. doi: 10.3109/10826084.2016.1156702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janulis P, Birkett M, Phillips G, Mustanski B. Substance use network characteristics and drug and alcohol use behaviors among young men who have sex with men (YMSM) Drug and Alcohol Dependence. 2015 Dec;157:188–191. doi: 10.1016/j.drugalcdep.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scalco MD, Meisel SN, Colder CR. Misperception and accurate perception of close friend substance use in early adolescence: Developmental and intervention implications. Psychology of Addictive Behaviors. 2016 May;30(3):300–311. doi: 10.1037/adb0000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moreno MA, Whitehill JM. Influence of Social Media on Alcohol Use in Adolescents and Young Adults. Alcohol Res. 2014;36(1):91–100. http://europepmc.org/abstract/MED/26259003. [PMC free article] [PubMed] [Google Scholar]
- 39.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ, USA: Prentice-Hall; 1986. [Google Scholar]
- 40.Ajzen I. Constructing a TPB questionnaire: conceptual and methodological considerations. Constructing a TPB questionnaire: conceptual and methodological considerations storrs, CT: 2002. [2020-06-30]. https://pdfs.semanticscholar.org/0574/b20bd58130dd5a961f1a2db10fd1fcbae95d.pdf. [Google Scholar]
- 41.McDonald RP, Ho MR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7(1):64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- 42.Valente TW, Fosados R. Diffusion of Innovations and Network Segmentation: The Part Played by People in Promoting Health. Sexually Transmitted Diseases. 2006;33(Supplement):S23–S31. doi: 10.1097/01.olq.0000221018.32533.6d. [DOI] [PubMed] [Google Scholar]
- 43.Chen X, Mo PKH, Li J, Lau JTF. Factors Associated with Drug Use Among HIV-Infected Men Who Have Sex with Men in China. AIDS Behav. 2019 Sep 4;24(6):1612–1620. doi: 10.1007/s10461-019-02660-z. [DOI] [PubMed] [Google Scholar]
- 44.Li J, Mo PKH, Wu AMS, Lau JTF. Roles of Self-Stigma, Social Support, and Positive and Negative Affects as Determinants of Depressive Symptoms Among HIV Infected Men who have Sex with Men in China. AIDS Behav. 2016 Feb 20;21(1):261–273. doi: 10.1007/s10461-016-1321-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Muessig KE, Bien CH, Wei C, Lo EJ, Yang M, Tucker JD, Yang L, Meng G, Hightow-Weidman LB. A mixed-methods study on the acceptability of using eHealth for HIV prevention and sexual health care among men who have sex with men in China. J Med Internet Res. 2015 Apr 21;17(4):e100. doi: 10.2196/jmir.3370. https://www.jmir.org/2015/4/e100/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991 Dec;50(2):179–211. doi: 10.1016/0749-5978(91)90020-t. [DOI] [Google Scholar]
- 47.Fornell C, Larcker DF. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. Journal of Marketing Research. 2018 Nov 28;18(1):39–50. doi: 10.1177/002224378101800104. [DOI] [Google Scholar]
- 48.Hair J. Multivariate data analysis with readings (5th ed) Englewood Cliffs, NJ, USA: Prentice-Hall; 1998. [Google Scholar]


