Sir,
We read with interest the recently published article by García et al. describing the epidemiological and clinical characteristics of coronavirus disease 2019 (COVID-19) among healthcare workers (HCWs) in a Spanish hospital, and their observations regarding HCW–HCW transmission [1]. However, we noted that ancillary workers contracted by outsourced service providers, including cleaning staff, security officers, and maintenance services, were excluded. Inclusion of ancillary workers is crucial in the implementation of infection prevention and control (IPC) guidelines during disease outbreaks [2]. Furthermore, compliance may be uneven across the hospital workforce; for instance, lower rates of hand hygiene have been reported among hospital cleaners [3]. Provision of adequate personal protective equipment (PPE) and surveillance among ancillary HCWs should form part of IPC strategies during the ongoing pandemic.
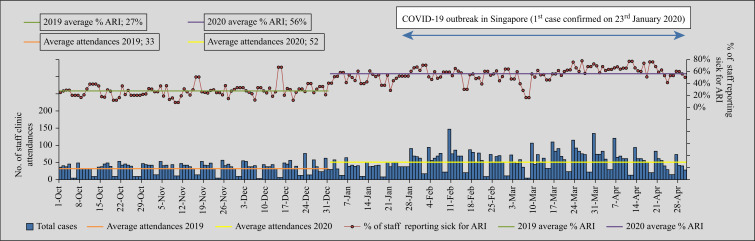
In Singapore, a globalized Asian city-state, the COVID-19 outbreak has been ongoing since end-January 2020. Comprehensive strategies were rolled out at our institution, the largest tertiary hospital in Singapore, to contain COVID-19 among HCWs [4]. All HCWs campus-wide were required to measure temperature twice-daily in an electronic surveillance system; HCWs with fever or symptoms of acute respiratory illness (ARI) were required to report to the staff clinic for COVID-19 testing (Figure 1 ). This surveillance was extended to outsourced ancillary HCWs. By April 2020, almost one-fifth of ancillary HCWs (21.2%, 518/2444) had presented at least once to staff clinic for ARI, with outsourced ancillary HCWs having higher odds of presentation compared to non-outsourced ancillary HCWs (27.8%, 495/1780 vs 12.8%, 85/664; odds ratio: 2.62; 95% confidence interval (CI): 2.04–3.37). From the start of the COVID-19 outbreak, ancillary HCWs working in ‘fever areas’ catering to suspected/confirmed cases of COVID-19 were mandated to use full PPE during significant exposure (Table I ) and given full access to adequate PPE by the hospital, with a universal masking policy initiated from February 2020. In April 2020, there was a significant COVID-19 outbreak among migrant workers living in dormitories [5]. Given that some of our outsourced ancillary HCWs were foreign workers, in end-April 2020 all outsourced ancillary HCWs in our institution were universally screened for COVID-19.
Figure 1.
Staff clinic attendances attributed to acute respiratory illness (ARI) at a tertiary hospital in Singapore during a COVID-19 outbreak, with a focus on ancillary healthcare workers.
Table I.
Personal protective equipment guidelines for healthcare workers during a COVID-19 outbreak, including ancillary workers
| Target personnel | Activity in ‘fever area’ | Type of personal protective equipment |
|---|---|---|
| Healthcare workers | Providing direct patient care to suspect patient within 2 m zone | N95 mask + eye protection + gown + gloves |
| Aerosol-generating procedures performed | N95 mask + eye protection + gown + gloves | |
| Healthcare workers | No patient contact; in corridors of ‘fever areas’ | N95 mask |
| Cleaners | Environmental cleaning including washing of toilet and bathroom | N95 mask + eye protection + gown + gloves |
| Security guard | Patrolling of ‘fever area’; crowd control | N95 mask |
| Porter | Escorting patient from ‘fever area’ to ward | N95 mask + eye protection + gown + gloves |
| All staff | Eating/drinking at rest areas | PPE not required but social distancing |
| All staff | Resting at rest areas | Surgical mask or personal reusable cloth mask |
The majority (86.9%, 1548/1780) of ancillary HCWs participated. In total, five cases of COVID-19 were detected among outsourced ancillary HCWs. In the corresponding period, only five cases of COVID-19 were reported in frontline medical staff (one doctor, four nurses) [4]. Rates of infection were higher in outsourced ancillary HCWs compared to medical and nursing staff (0.32%, 5/1548, vs 0.01%, 5/5101; incidence rate ratio: 3.29, 95% CI: 0.76–14.32, P = 0.04). Of the five ancillary worker cases, four stayed in dormitories with known COVID-19 clusters; as they were not deployed to designated hospital areas managing confirmed/suspect cases of COVID-19 and were not identified as staff close-contacts during contact tracing for cases of COVID-19 managed in our institution, acquisition of COVID-19 was likely from community transmission. One case of hitherto unsuspected COVID-19 infection was detected in a minimally symptomatic security guard stationed at our emergency department's ‘fever area’ [6]. Given the absence of epidemiological linkage and work in a high-risk area, outbreak investigations were commenced.
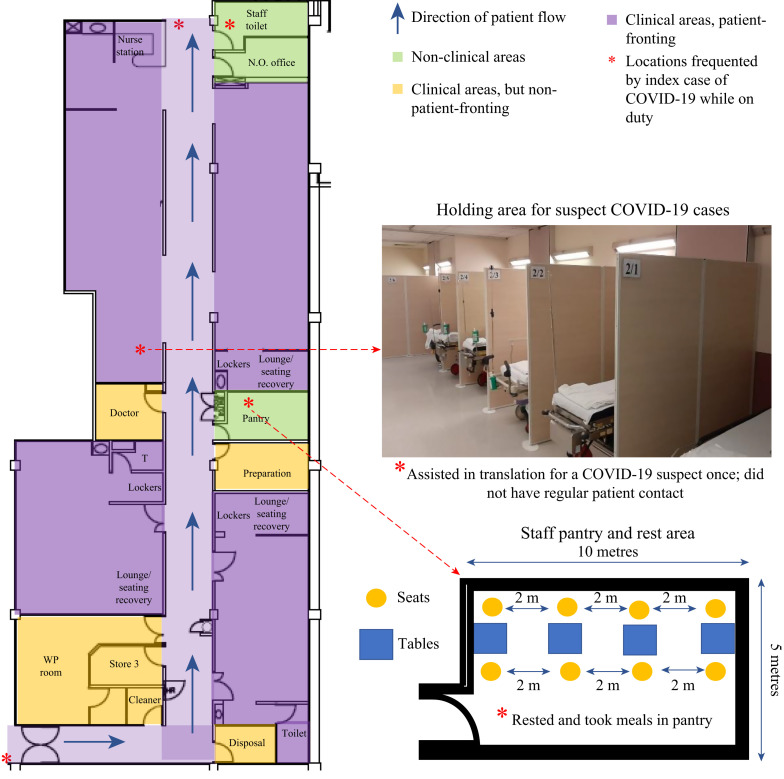
On activity mapping for the index case (Figure 2 ), the security guard assisted with crowd control and did not have direct patient contact. The HCW wore an N95 respirator while on duty, but reported gaps in adherence during long duty hours. Twelve days prior to diagnosis, the index case assisted in translation for a high-risk COVID-19 suspect case in the ‘fever area’ who subsequently tested positive. The HCW stood more than 1 m away from the suspect case for around 20 min and was wearing N95 respirator but no gown or gloves. During shifts, the HCW would use the shared pantry in the ‘fever area’ for rest breaks, as well as the shared staff toilet. Given that during mealtimes it was not possible to use masks and that social distancing was employed instead (Figure 3 ), investigations focused on HCWs who had used the shared pantry [7]. The index case, as well as all HCWs working in the ‘fever area’ over the preceding two weeks, were interviewed and closed-circuit camera footage of the pantry area was utilized to identify at-risk contacts. A total of 68 HCWs were identified as potential contacts, with the majority (72.1%, 49/68) having used the shared pantry. All HCW contacts were tested for COVID-19; none tested positive. No additional cases of COVID-19 were detected among HCWs working in the ‘fever area’ on 28-day follow-up. There was no evidence of a staff cluster and the HCWs had very limited patient contact, making healthcare-associated transmission less likely. To date, more than 1500 cases of COVID-19 have been managed in our institution, without patient–HCW transmission.
Figure 2.
‘Fever area’ in emergency department during COVID-19 outbreak: layout and activity mapping for minimally symptomatic ancillary worker (security guard).
Figure 3.
Safe distancing in staff rest areas during COVID-19 outbreak. Transparent partitions set up between seating areas to minimize risk of droplet spread; mandatory masking in clinical areas except when eating.
A solitary undetected case of COVID-19 in a minimally symptomatic ancillary worker resulted in the potential exposure of 68 other HCWs. Ancillary workers should not be overlooked in hospital-wide IPC efforts to mitigate COVID-19 spread. Surveillance, adequate PPE provision, and rigorous outbreak investigations successfully contained COVID-19 among ancillary HCWs.
Ethics approval
Waiver of informed consent for publication was approved by our hospital's Institutional Review Board (CIRB Ref 2020/2436). ORCID: 0001-6428-9999.
Acknowledgements
We thank our colleagues for their unstinting efforts against COVID-19.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.García I.S., López M.J., Vicente A.S., Abascal P.L. SARS-CoV-2 infection among healthcare workers in a hospital in Madrid, Spain. J Hosp Infect. 2020 Jul 20 doi: 10.1016/j.jhin.2020.07.020. S0195-6701(20)30351-0 [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Houghton C., Meskell P., Delaney H., Smalle M., Glenton C., Booth A. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4):CD013582. doi: 10.1002/14651858.CD013582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sendall M.C., McCosker L.K., Halton K. Cleaning staff’s attitudes about hand hygiene in a metropolitan hospital in Australia: a qualitative study. Int J Environ Res Public Health. 2019;16:1067. doi: 10.3390/ijerph16061067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wee L.E., Sim J.X.Y., Conceicao E.P., Aung M.K., Goh J.Q., Yeo D.W.T. Containment of COVID-19 cases amongst healthcare workers: the role of surveillance, early detection and outbreak management. Infect Control Hosp Epidemiol. 2020 May 11:1–21. doi: 10.1017/ice.2020.219. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koh D. Migrant workers and COVID-19. Occup Environ Med. 2020;77:634–636. doi: 10.1136/oemed-2020-106626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wee L.E., Fua T.P., Chua Y.Y., Ho A.F.W., Sim X.Y.J., Conceicao E.P. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27:379–387. doi: 10.1111/acem.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wee L.E., Conceicao E.P., Sim X.Y.J., Aung M.K., Tan K.Y., Wong H.M. Minimising intra-hospital transmission of COVID-19: the role of social distancing. J Hosp Infect. 2020;105:113–115. doi: 10.1016/j.jhin.2020.04.016. pii: S0195-6701(20)30191-30192. [DOI] [PMC free article] [PubMed] [Google Scholar]