To the Editor: At this moment in the United States, we are battling 2 of the largest public health crises of our time: the coronavirus disease 2019 (COVID-19) pandemic and systemic racism, which has existed for centuries but recently came into sharper public focus. In tandem, these public health crises mean that the COVID-19 pandemic has placed a disproportionate burden of disease incidence, hospitalizations, and deaths on our most vulnerable communities.1 For medical professionals, there has never been a more important time to systematically address health equity in policy and practice.
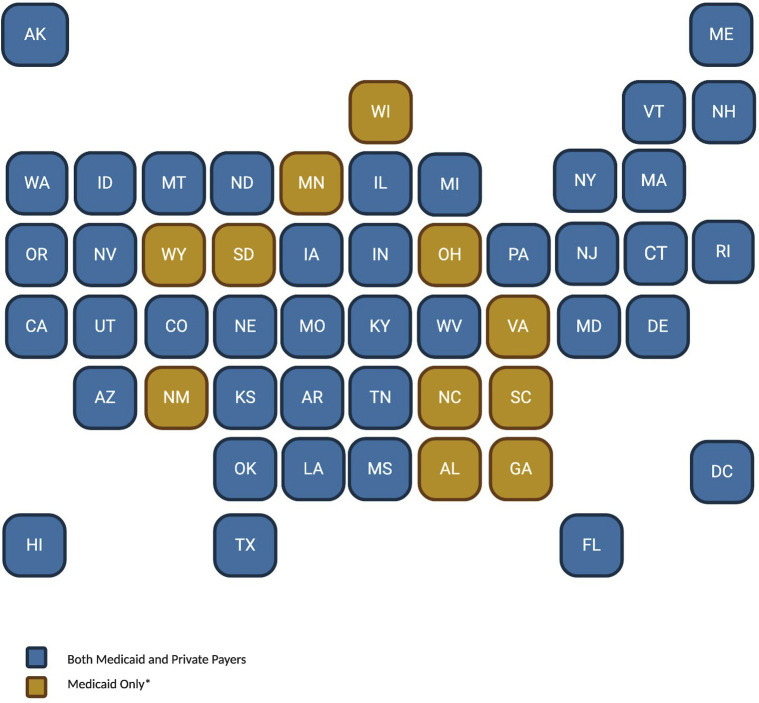
One of the most significant health policy changes during COVID-19 has been the rapid adoption of executive orders, emergency legislation, and regulations to expand access to telehealth services. At the federal level, the Centers for Medicare & Medicaid Services markedly expanded telehealth coverage, including outpatient office visits for new and established patients. All 50 states have broadened telehealth access and decreased regulatory burdens for patients covered by Medicaid plans.2 Most have also released guidelines expanding telehealth access for patients with private plans (Fig 1 ). In response to this and shelter-in-place guidelines, telehealth claims increased by 4347% from March 2019 to March 2020.3 Before the pandemic, ambiguity surrounding Medicaid telehealth policies and coverage was found to be a recurrent barrier to telehealth adoption by safety-net providers.4 Thus, sweeping telehealth coverage gains for patients with Medicaid in particular have been crucial to allow us to continue to care for all patients, especially our most vulnerable, throughout the pandemic.
Fig 1.
States that have enacted statewide legislative or regulatory policy changes to temporarily expand access or remove barriers to telehealth services during the coronavirus disease 2019 pandemic. AK, Alaska; AL, Alabama; AR, Arkansas; AZ, Arizona; CA, California; CO, Colorado; CT, Connecticut; DC, District of Columbia; DE, Delaware; FL, Florida; GA, Georgia; HI, Hawaii; IA, Iowa; ID, Idaho; IL, Illinois; IN, Indiana; KS, Kansas; KY, Kentucky; LA, Louisiana; MA, Massachusetts; MD, Maryland; ME, Maine; MI, Michigan; MN, Minnesota; MO, Missouri; MS, Mississippi; MT, Montana; NC, North Carolina; ND, North Dakota; NE, Nebraska; NH, New Hampshire; NJ, New Jersey; NM, New Mexico; NV, Nevada; NY, New York; OH, Ohio; OK, Oklahoma; OR, Oregon; PA, Pennsylvania; RI, Rhode Island; SC, South Carolina; SD, South Dakota; TN, Tennessee; TX, Texas; UT, Utah; VA, Virginia; VT, Vermont; WA, Washington; WI, Wisconsin; WV, West Virginia; WY, Wyoming. ∗Private payer coverage already in place or optional.
Nearly all of these policy changes, however, will expire at the end of this pandemic. Now is the time for health care providers to advocate for an end to the legislative, regulatory, and technologic barriers to remote care, allowing telehealth access to continue beyond the pandemic. Studies have shown that telehealth can result in significant indirect cost savings, decreased travel time and accompanying work absenteeism, and improved convenience for patients.5 These savings could especially benefit low-income minority patients, many of whom are disproportionately affected by the economic shocks and unemployment caused by the pandemic.
Dermatologists have long advocated for expanded telehealth access, but disparities in access to dermatologic care linger in the current reimbursement framework, particularly for the most vulnerable patients. Now more than ever, we should be at the forefront of promoting long-term policy changes that allow for ongoing telehealth coverage. This is particularly important for patients with Medicaid and Medicare, for whom physical disability, transportation limitations, and inflexible work schedules may limit attendance at in-person appointments. As we work to build a more equitable system, we must ensure that our policies do not present telehealth as a luxury service, but rather as a necessary link in the fabric of our health care system: bridging vulnerable populations to care. Additional research must examine how the “digital divide” and various levels of e-health literacy have affected telehealth adoption among marginalized patients during the COVID-19 pandemic. Beyond this research, telehealth equity and health justice will require ongoing advocacy at both state and federal levels to ensure continued access to essential remote care for those who need it most.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
Reprints not available from the authors.
References
- 1.Azar K.M.J., Shen Z., Romanelli R.J., et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff (Millwood) 2020;39(7):1253–1262. doi: 10.1377/hlthaff.2020.00598. [DOI] [PubMed] [Google Scholar]
- 2.Center for Connected Health Policy COVID-19 telehealth coverage policies. https://www.cchpca.org/resources/covid-19-telehealth-coverage-policies Available at: Accessed June 1, 2020.
- 3.FH NPIC® database of more than 31 billion privately billed medical and dental claim records from more than 60 contributors nationwide. Copyright 2020, FAIR Health, Inc. All rights reserved. CPT © 2019 American Medical Association (AMA), Available at: https://www.prnewswire.com/news-releases/telehealth-claim-lines-increase-4-347-percent-national-from-march-2019-to-march-2020-301069182.html. Accessed June 1, 2020.
- 4.Uscher-Pines L., Bouskill K., Sousa J., Shen M., Fischer S. RAND Corporation; Santa Monica, CA: 2019. Experiences of Medicaid programs and health centers in implementing telehealth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Powell R.E., Henstenburg J.M., Cooper G., Hollander J.E., Rising K.L. Patient perceptions of telehealth primary care video visits. Ann Fam Med. 2017;15(3):225–229. doi: 10.1370/afm.2095. [DOI] [PMC free article] [PubMed] [Google Scholar]