A substantial reduction has been reported in the number of patients admitted to hospitals with acute cardiovascular events—including ST-elevation myocardial infarctions, cardiac arrests, and strokes—coinciding with the onset of the COVID-19 pandemic. For example, there has been a 40% decrease in STEMI volume among 81 centers in Spain,1 a 38% reduction in cardiac catheterization lab activations for STEMI among 9 high-volume centers across the United States,2 and a decrease in weekly hospitalization for acute myocardial infarction in Northern California of up to 48%.3 In Northern Italy, there has been an increase in out-of-hospital cardiac arrests4 but also a significant decrease in hospitalizations related to acute coronary syndrome.5 One proposed explanation is that patients are afraid and reluctant to visit hospitals and access healthcare systems during a pandemic. In the prehospital setting, EMS clinicians are often the first point of contact and caregivers to the victims of acute cardiovascular events, and understanding patterns seen by EMS might provide a better perspective of the occurrence of acute cardiovascular events during the pandemic.
We surveyed the National Emergency Medical Services Information System (NEMSIS) database, which contains millions of EMS activations throughout the United States. Inclusion criteria were calls when EMS clinicians documented the presence of rhythms suggestive of a STEMI; ventricular fibrillation or ventricular tachycardia (VF/VT); asystole; or a stroke pre-arrival alert. The frequency of these calls during January, February, March, and April of 2020 were compared amongst each other and with historic trends (Figure 1).
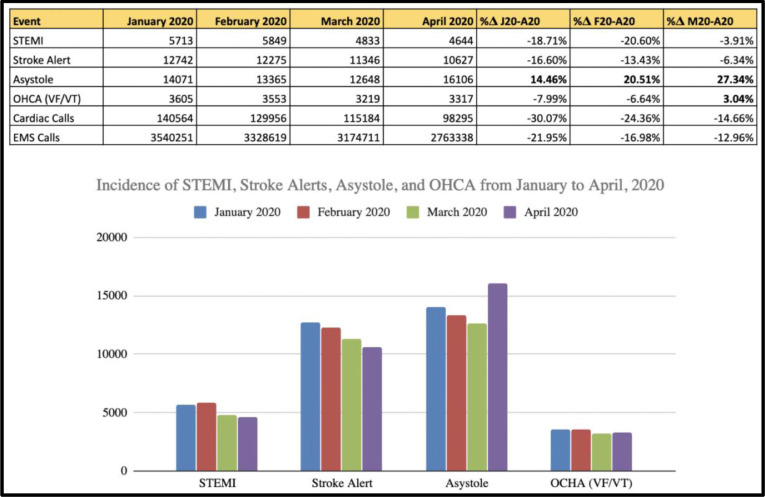
Figure 1.
(A) the incidence of various acute cardiac conditions and overall EMS activations seen in various months of 2020, including January (when the US was not significantly-affected), February (when awareness was growing and infections were emerging), March (after social distancing and stay-at-home orders began), and April (when projected mortality peaked in many communities). STEMI, stroke alerts, cardiac calls, and EMS calls all decreased across all months, while VF/VT and asystole decreased from January until March but spiked in April. (B): A graphical representation of EMS calls for various acute cardiovascular events. Along with overall EMS calls and general cardiac calls, STEMIs and strokes decreased from January to April, whereas OCHA and asystole decreased from January to March before increasing in April.
There was an overall 10.33% decrease in EMS calls between January and March 2020, a 4.62% decrease from February to March 2020, and a 12.96% decrease between March and April. Cardiac calls similarly decreased, with an even-greater magnitude. STEMIs and stroke alerts both decreased across all months. Interestingly, both the incidence of VF/VT and asystole decreased from January to March but increased from March to April: VF/VT increased 3.04%, while asystole increased 27.34% to a year-to-date high. These trends identified in 2020 are not seen in the databases’ previous years, eliminating the possibility of this variability being indicative of seasonal variation and suggesting unique patterns coinciding with the COVID-19 pandemic.
These data seem to confirm a decrease in the number of patients seeking care for acute cardiovascular events, a trend seen within many healthcare centers. It is unclear whether or not reductions in overall EMS calls, cardiac-specific calls, stroke alerts, and STEMIs are related to actual decrease in these events or an unwillingness of patients to seek medical care. The spike in asystole and VF/VT calls could be due to the pathophysiological effects of the virus. However, it is also possible that the increase in asystole and VF/VT following a decrease in STEMI, stroke, and general cardiac calls might indicate patients are avoiding seeking care in time-sensitive conditions, resulting in less-favorable outcomes. Although it would be rather difficult to investigate if patients have been reluctant to visit hospitals, a continued trend of VT/VF or asystole following decreases in STEMI, strokes, and cardiac calls might support such a notion. Further physiological studies should attempt to better understand the link between COVID-19 and acute cardiovascular events, and the public health community should examine patients’ willingness to self-triage and seek care during the pandemic.
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Rodríguez-Leor O, Cid-Álvarez B, Ojeda S, Martin-Moreiras J, Rumoroso JR, López-Palop R, Serrador A, Cequier Á, Romaguera R, Cruz I, de Prado AP. Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. REC Interv Cardiol. 2020;2(2):82–89. [Google Scholar]
- 2.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Solomon MD, McNulty EJ, Rana JS, Leong TK, Ambrosy AP, Sidney S, Go AS. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 4.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, Beretta G. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, Secco GG, Campo G, Gallone G, Verardi R, Gaido L. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]