Abstract
A history of cardiovascular comorbidity or experiencing acute cardiac injury during the coronavirus disease 2019 is accompanied by a poor prognosis. Also, it seems myocardial ischemia (or infarction) accounts for a major part of the cardiac involvement observed in this disease. Therefore, particular consideration is needed to protect the cardiovascular system during this pandemic. The gaps highlighted in this review are an issue to be explored through future research.
Keywords: cardiovascular disease, myocardial infarction, coronavirus
Introduction
The novel emerged severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) responsible for the coronavirus disease 2019 (COVID-19) pandemic has affected more than 3 million people and taken thousands of lives so far, yet the statistics are exponentially increasing. The high capacity of spreading, the substantial fatality of SARS-CoV-2 (as indicated by the basic reproduction number of 2–2.5), and the case fatality rate of 1.4% indicate this virus is a devastating pathogen (1, 2). As studies are conducted worldwide, our information about this virus and the disease is promptly updated. At first, the condition was described as novel pneumonia seen in a cluster of patients at Wuhan, and to date, a typical case of COVID-19 is characterized by its respiratory manifestation. Soon after that, a growing body of literature reported that older patients with cardiovascular disease or hypertension are at a greater risk of death and critical illness. Also, reports demonstrated an association between cardiac injury and disease severity or mortality (3). Based on these findings, cardiovascular damage seems to be a major complication of COVID-19 associated with high morbidity and mortality. To the best of our knowledge, there are only a few studies on the cardiovascular aspects of COVID-19 and the field remains a challenging, unsettled issue. Therefore, the current review sought to address this issue with a focus on myocardial injury in COVID-19.
COVID-19 and the heart
Cardiac involvement in COVID-19 seems a life-threatening aspect of the disease. Underlying cardiovascular diseases and hypertension represent the most lethal comorbidities in patients with COVID-19. Also, Risk factors that contribute to the worsening outcomes in COVID-19 are similar to the ones we know within the context of cardiovascular diseases (including age). Acute cardiac injury was observed in 20%–30% of hospitalized patients and was responsible for 40% of the deaths (4). In another study, cardiac injury, defined by high-sensitivity troponin I (hs-TnI)>99th percentile upper reference limit, or a new abnormality in the electrocardiograph or echocardiography, was present in 17% of all patients and 22% of the critical cases who required admission into the intensive care unit. According to some studies, of the cardiac manifestations observed among hospitalized patients; arrhythmia, cardiac injury, and heart failure accounted for the majority (5, 6).
Moreover, multiple case reports of patients who experienced events of cardiac injury and later were diagnosed with pathological features of myocarditis have been published. Possible underlying mechanisms that explain the occurrence of myocarditis include indirect damage to the myocardium mediated by the immune response to systemic inflammation caused by cytokine storms and/or direct infection of myocytes by the virus, which has not been confirmed yet (7, 8). Recently, Tavazzi et al. (9) found virus particles within inflammatory macrophages that infiltrated the myocardium, but not in myocytes, which could either be due to the viraemic phase of infection or the migration of pulmonary macrophages to the myocardium. In contrast, the findings of a recent report support the notion of the capability of the virus to mediate direct cardiac damage. The study described a patient that experienced acute cardiac injury following the elevation of myocardial enzymes. Subsequently, post-mortem biopsies of endocardium and myocardium did not show any infiltration of inflammatory cells, while the test results of reverse transcription-polymerase chain reaction assay performed on cardiac tissue samples were positive for SARS-CoV-2 (10).
The question of whether and how cardiomyocytes remain intact can be an area of interest considering a wide expression of angiotensin-converting enzyme 2 (ACE2) receptors in the heart that can also serve as a portal of entry into the cell for SARS-CoV-2. Also, viral ribonucleic acid (RNA) was detected in 35% of the cardiac autopsies in the Toronto SARS epidemic. As such, efforts to find the SARS-CoV-2 viral RNA or particles in the heart must be continued (11).
COVID-19 and renin-angiotensin system
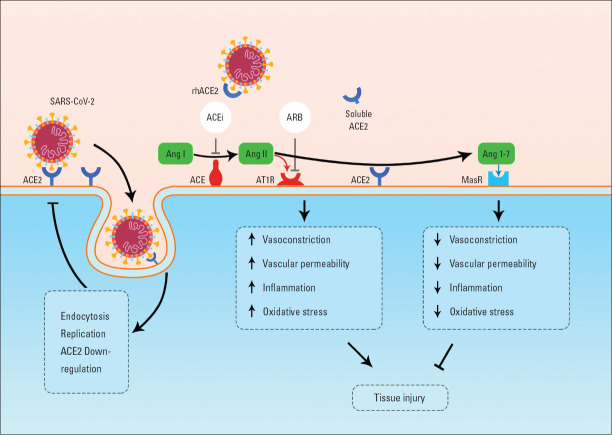
The catalytic enzyme ACE2 is a key regulator of the renin-angiotensin system (RAS) and cardiovascular function. It has also been shown that ACE2 receptors, which are present mostly on the cell membranes of organs such as heart, lung, kidney, and intestines; and to a lesser extent in the soluble form, bind to the spike protein of SARS-CoV-2 and acts as a receptor for the virus’s entry into the cell (12). The enzyme degrades angiotensin II (Ang II) to angiotensin 1–7 and therefore, inhibits Ang II-related deleterious effects mediated by angiotensin II type 1 receptor (AT1R) which include vasoconstriction, increased pulmonary endothelial permeability, enhanced inflammation, increased oxidative stress, and thrombosis (13).
On the other hand, angiotensin 1–7 acts on the Mas receptor and results in contrary effects to Ang II including Vasodilation, attenuated inflammation, and oxidative stress (14). The 2 signaling pathways ACE-Ang II and ACE2-Ang 1–7 are in equilibrium under normal body circumstances, while over-activation of one compared to the other may lead to tissue damage in response to infection (Fig. 1). Consistent with this notion, reports revealed significantly greater Ang II levels in the serum of patients with COVID-19 which was associated with a higher viral load and lung damage (15). Another study evaluated the plasma levels of Ang I in patients with acute respiratory distress syndrome and presented significantly higher Ang 1 levels among non-survivors (16).
Figure 1.
Interactions between SARS-CoV-2 and the renin-angiotensin system. Angiotensin-converting enzyme (ACE) converts angiotensin I (Ang I) to angiotensin II (Ang II), which activates Ang II type 1 receptor (AT1R) and leads to increased vasoconstriction, increased vascular permeability, inflammation, and oxidative stress. ACE2 degrades Ang II to angiotensin 1–7 which activates the Mas receptor to mediate protective effects. Spike proteins of SARS-CoV-2 bind to its ACE2 receptors and cause internalization of the virus into the cell which results in ACE2 downregulation. ACE inhibitors (ACEi) and angiotensin receptor blockers (ARBs) inhibit the generation of Ang II and activation of AT1R respectively. rhACE2 - recombinant human ACE2
Studies confirmed the entry of the virus into cells through membrane fusion is associated with a significant downregulation of external site ACE2 receptors, which supposedly diminish ACE2 related protective effects (17). ACE2 receptors is also abundant in great levels on the membrane of myocardial pericytes, which plays a crucial role in maintaining the endothelial function. Thus, presumably, dysfunctions of these cells can lead to disruptions in downstream myocardial circulation and subsequent ischemia (13).
Furthermore, an in vivo study showed knockdown mice for ACE2 gen developed severe left ventricular dysfunction (18). In agreement with the belief that conditions leading to adverse outcomes of COVID-19 express a lower amount of ACE2 receptors in tissues, including cardiovascular disease, hypertension, and diabetes. Two studies have provided evidence of the successful treatment of SARS coronavirus lung injury by new recombinant ACE2 and losartan (19, 20). Also, a new in vitro study used recombinant ACE2 as a decoy receptor for SARS-CoV-2 and demonstrated its capability to reduce viral infection and growth in cell culture (21). Trials on the safety and tolerability aspects of recombinant human ACE2 in patients with acute lung injury are currently being conducted (NCT00886353, NCT01597635).
RAS inhibitors have been widely prescribed worldwide and since some studies reported that the use of these medications might cause an increase in ACE2 levels (22, 23), concerns were raised regarding theoretically higher susceptibility to SARS-CoV-2 infection or COVID-19 severity. Although the serum ACE2 level is directly proportional to the number of viral receptors, does it also imply that this causes more infection susceptibility and severity?
Advanced age, male gender, and cardiovascular comorbidities are the main risk factors for poor prognosis. However, it is proven that ACE2 expression is reduced in such conditions (20, 24). Additionally, Sama et al. (25) in two independent cohorts demonstrated that the use of ACE inhibitors (ACEis) or angiotensin receptor blockers (ARBs) are not associated with plasma levels of ACE2. The use of ACEis or ARBs in the setting of COVID-19 is a controversial topic, while some found it bifacial to patients, others concluded an impartial or detrimental effect. In a retrospective study conducted by Zhang et al. (26), it was expressed that patients with COVID-19 and preexisting hypertension who used in-hospital ACEis or ARBs had significantly fewer all-cause mortality than non-ACEi-ARB users. Another study found that neither ACEis nor ARBs users with COVID-19 were at increased risk of admission to the hospital including fatal cases and those admitted to the ICU. However, this study showed diabetic patients who were on RAS inhibitors users required less hospitalization (27).
Also, two other observational studies reported no association between the severity of illness and RAS inhibitors in hospitalized patients (28, 29). Nevertheless, contrary to previous reports, a clinical retrospective study showed a higher mortality rate among those patients who received angiotensin 2 receptor blockers or ACE inhibitors (36% vs. 25%), however, the higher mortality rate might be a tribute to an underlying cardiovascular disease (CVD), and the confounding effect must be adjusted for (30).
The relationship between underlying comorbidities, RAS inhibitors, and the RAS seems to be more complex in COVID-19. Furthermore, there were numerous limitations in previous studies; the designs were retrospective, dose, and duration of medication use were not assessed, and the studies were only on in-patient subjects. As ACEis and ARBs are indicated for chronic conditions such as hypertension, chronic kidney disease, and heart failure and the patients have been using these medications for a long time, abrupt cessation may lead to complications. Based on the evidence to date and newly published guidelines in this area, we recommend continuing the usage of drugs as before.
COVID-19 and cardiac injury
Cardiac injury as indicated by elevated cardiac enzymes before or during the hospitalization of patients with COVID-19 is an independent risk factor for adverse outcomes including death and intensive care unit admission (13, 31, 32).
In a retrospective study, more than half of those who died had an increase in TnI. Another study on 416 in-patient cases showed that those with cardiac injury had a significantly higher mortality rate than those without cardiac injury (51% vs. 4.5%) (33). The difference was more pronounced in the study by Guo et al. (30) when comparing mortality associated with elevated troponin T (TnT) or underlying CVD; Patients with neither raised TnI nor history of CVD had a 7.62% in-hospital mortality rate whereas this number for those with either only underlying CVD, only raised TnI, and the combination was increased to 13.33%, 37.5%, and 69.44% respectively.
Elevation of TnI/T levels is associated with an increase in other inflammatory mediators such as D-dimer, Ferritin, IL6, and Lactate Dehydrogenase; suggesting the key role of systemic inflammation in the cardiac damage process (8). Additionally, elevated troponin levels in survivors did not change significantly during the hospitalization whereas it increased significantly in non-survivors suggesting an association of dynamic changes in troponin with the increased risk of death (8, 30). The rise in the troponin enzyme in the course of COVID-19 may have several origins including myocardial infarction (MI), myocarditis, pulmonary embolism, and renal injury. However, this effect might be seen in the setting of positive pressure ventilation and must be adjusted for when assessing the hazard risk.
Natriuretic peptides are known as biomarkers of myocardial stress. New reports on the role of B-type natriuretic peptide among patients with COVID-19 has revealed significantly greater levels in ICU-admitted patients, implying a prognostic role for it. However, TPI was a more specific index in this study (33). Also, patients with cardiac injury had higher levels of NT-proBNP (33). The study by Gao et al. (34) nexplored the prognostic value of NT-proBNP in patients with severe COVID-19 and identified it as an independent risk factor for in-hospital death. In the authors’ opinion, although elevated natriuretic peptide may indicate a poor prognosis, diagnostic work-up, and treatment for heart failure should take place when there are clear clinical grounds for it.
To recapitulate, the TnI level or the surrogate marker natriuretic peptide has a significant implication on prognosis estimation and risk stratification in hospitalized patients, which needs to be interpreted precisely.
COVID-19 and myocardial infarction
Although the literature on the prevalence and incidence of MI in patients with COVID-19 is lacking, the lessons from past experiences on the increased risk of MI in the clinical course of respiratory infections such as SARS and Influenza warn the health care system and acute care facilities to stay vigilant (35-37). Besides, the SARS epidemic heightened hospital mortality associated with acute MI (38).
An overview of the main possible contributory mechanisms that lead to MI is shown in the form of a concept map (Fig. 2). Following local infection, alveolar macrophages and pneumocytes release inflammatory cytokines such as interleukin IL-1, IL-6, and tumor necrosis factor which in turn initiates a systemic inflammatory response through the circulatory system, sometimes resulting in a cytokine storm or what is called severe inflammatory response syndrome (39). An imbalance in T cell subtype populations, especially a reduction in regulatory T cells, mediated by COVID-19 infection results in decreased anti-inflammatory cytokines and further amplified inflammation (40). These inflammatory mediators induce cardiac coronary endothelial and smooth muscle cells, which per se, activate preexisting macrophages in atheromatous plaques (39).
Figure 2.
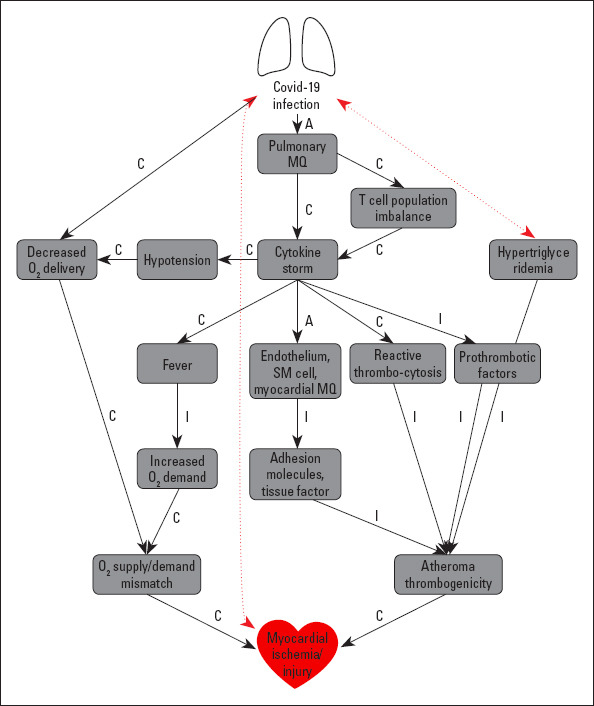
Concept map of mechanistic pathways linking COVID-19 infection to myocardial ischemia/injury. The black arrows indicate proved concepts and red arrows indicate possible connections
MQ- macrophage, SM- smooth muscle, A- activates, C- causes, I- increases, E- exacerbates
Besides, hypothetically, activated alveolar macrophages carrying SARS-CoV-2 particles may migrate to cardiac tissue and cause direct damage (9). Cardiac macrophages expedite the local inflammatory pathway and induce the expression of adhesion molecules which lead to the recruitment of more leukocytes, forming a positive feedback loop at the site of atheromatous plaque. Eventually, the situation increases the chance of rupture of the atheromatous plaque and provokes an acute coronary syndrome. Furthermore, fever and tachycardia increase myocardial oxygen (O2) demand and O2 delivery is reduced due to pneumonia, which results in cardiac stress. Patients with COVID-19 suffer from a coagulopathic state confirmed by elevated levels of D-dimer and fibrinogen degraded particles (41).
Multiple factors contribute to hemostasis disturbance, including hepatic dysfunction which per se increases the production of fibrinogen and tissue plasminogen activator inhibitor, and the reactive thrombocytosis mediated by the inflammation and prolonged bed rest (42).
Although there are insufficient data on dyslipidemia as a complication of COVID-19, this was one of the SARS complications probably caused by hepatic dysfunction (43). The study by Tao Guo et al. showed significantly higher triglyceride levels among COVID-19 patients who experienced cardiac injury (30). In a study by Chen et al. (44) it was shown that triglyceride levels were significantly higher in deceased patients than in those who recover. It was also shown that those who die have higher cardiac troponin levels. However, it is not stated whether these concepts correlate with each other or not (44). This factor and its effect can also be attributed to higher body mass index and diabetes mellitus, which may act as confounding factors. Whether or not agents lowering triglyceride levels can limit the disease progression remains unknown.
In line with the hypercoagulability state in COVID-19 patients, the report by Zhang et al. (45) described three cases of COVID-19 that presented with multiple cerebral infarctions. Additionally, another study showed the case of a 59-year-old female who presented to the emergency room with weakness and a history of cough one week before. On physical examination, she had fever and tachycardia. She was later diagnosed with massive pulmonary embolism and right-sided heart failure (46). From this standpoint, it warrants the question of whether or not anticoagulants can be considered as a therapeutic option in hospitalized COVID-19 patients, which was the aim of a recently published study by Paranjpe et al. (47). The results of their work confirmed an improvement in the mortality rate and median survival time in the mechanically ventilated patients who received anticoagulants as compared to those who did not. This effect was observed even after adjustment for mechanical ventilation (47).
Furthermore, it was suggested by the International Society on Thrombosis and Haemostasis that all hospitalized patients with COVID-19, whether ICU-admitted or not, be put on a prophylactic-dose low molecular weight heparin as well as guidelines by the National Institute for Public Health of the Netherlands (48, 49). The protective role of antithrombotic agents is addressed by many other national and international scientific societies. However, there are no clear indications and optimal dose for antithrombotic therapies yet. Future risk stratification guidelines and studies are recommended to be based on the D-dimer level.
Conclusion
To conclude, we as health care communities must be cautious of any alterations in the clinical, laboratory, or electrocardiographic findings and subsequently, look for the background reasons. This study provided a brief review of current issues in cardiology and COVID-19, and also presented mechanisms contributing to cardiac damage or infarction. Future studies are encouraged to investigate the mechanistic roles of ACE2, triglycerides, and related agents in disease severity and progression. Also, it is suggested to consider the use of cardiac markers in clinical management guidelines, decision making, and prognosis estimation. Further studies should aim to explore the prevalence and characteristics of MI in patients with COVID-19.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – F.H., N.V., M.M.A.R.; Design – F.H.; Supervision – M.M.A.R.; Funding – F.H., N.V., M.M.A.R.; Materials – F.H., N.V., M.M.A.R.; Data collection and/or processing – F.H., N.V., M.M.A.R.; Analysis and/or interpretation – F.H., N.V., M.M.A.R.; Literature search – F.H., N.V., M.M.A.R.; Writing – F.H., N.V., M.M.A.R.; Critical review – F.H., N.V., M.M.A.R.
References
- 1.Wu JT, Leung K, Bushman M, Kishore N, Niehus R, de Salazar PM, et al. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med. 2020;26:506–10. doi: 10.1038/s41591-020-0822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368:489–93. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li JW, Han TW, Woodward M, Anderson CS, Zhou H, Chen YD, et al. The impact of 2019 novel coronavirus on heart injury:A Systematic review and Meta-analysis. Prog Cardiovasc Dis. 2020 doi: 10.1016/j.pcad.2020.04.008. S0033-0620(20)30080-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akhmerov A, Marbán E. COVID-19 and the Heart. Circ Res. 2020;126:1443–55. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–60. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yao XH, Li TY, He ZC, Ping YF, Liu HW, Yu SC, et al. [A pathological report of three COVID-19 cases by minimal invasive autopsies] Zhonghua Bing Li Xue Za Zhi. 2020;49:411–7. doi: 10.3760/cma.j.cn112151-20200312-00193. [DOI] [PubMed] [Google Scholar]
- 8.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China:a retrospective cohort study. Lancet. 2020;395:1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–5. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M, et al. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod Pathol. 2020;33:1007–14. doi: 10.1038/s41379-020-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–9. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 12.Tikellis C, Thomas MC. Angiotensin-Converting Enzyme 2 (ACE2) Is a Key Modulator of the Renin Angiotensin System in Health and Disease. Int J Pept. 2012;2012:256294. doi: 10.1155/2012/256294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. 2020;116:1097–100. doi: 10.1093/cvr/cvaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.South AM, Shaltout HA, Washburn LK, Hendricks AS, Diz DI, Chappell MC. Fetal programming and the angiotensin-(1-7) axis:a review of the experimental and clinical data. Clin Sci (Lond) 2019;133:55–74. doi: 10.1042/CS20171550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Y, Yang Y, Zhang C, Huang F, Wang F, Yuan J, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–74. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reddy R, Asante I, Liu S, Parikh P, Liebler J, Borok Z, et al. Circulating angiotensin peptides levels in Acute Respiratory Distress Syndrome correlate with clinical outcomes:A pilot study. PLoS One. 2019;14:e0213096. doi: 10.1371/journal.pone.0213096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39:618–25. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, et al. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature. 2002;417:822–8. doi: 10.1038/nature00786. [DOI] [PubMed] [Google Scholar]
- 19.Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–6. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11:875–9. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Monteil V, Kwon H, Prado P, Hagelkrüys A, Wimmer RA, Stahl M, et al. Inhibition of SARS-CoV-2 Infections in Engineered Human Tissues Using Clinical-Grade Soluble Human ACE2. Cell. 2020;181:905–13.e7. doi: 10.1016/j.cell.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111:2605–10. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 23.Keidar S, Gamliel-Lazarovich A, Kaplan M, Pavlotzky E, Hamoud S, Hayek T, et al. Mineralocorticoid receptor blocker increases angiotensin-converting enzyme 2 activity in congestive heart failure patients. Circ Res. 2005;97:946–53. doi: 10.1161/01.RES.0000187500.24964.7A. [DOI] [PubMed] [Google Scholar]
- 24.Xie X, Chen J, Wang X, Zhang F, Liu Y. Age- and gender-related difference of ACE2 expression in rat lung. Life Sci. 2006;78:2166–71. doi: 10.1016/j.lfs.2005.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sama IE, Ravera A, Santema BT, van Goor H, Ter Maaten JM, Cleland JGF, et al. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin-angiotensin-aldosterone inhibitors. Eur Heart J. 2020;41:1810–7. doi: 10.1093/eurheartj/ehaa373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang P, Zhu L, Cai J, Lei F, Qin JJ, Xie J, et al. Association of Inpatient Use of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers With Mortality Among Patients With Hypertension Hospitalized With COVID-19. Circ Res. 2020;126:1671–81. doi: 10.1161/CIRCRESAHA.120.317134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Abajo FJ, Rodríguez-Martín S, Lerma V, Mejía-Abril G, Aguilar M, García-Luque A, et al. MED-ACE2-COVID19 study group. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital:a case-population study. Lancet. 2020;395:1705–14. doi: 10.1016/S0140-6736(20)31030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bean DM, Kraljevic Z, Searle T, Bendayan R, Kevin O G, Pickles A, et al. ACE-inhibitors and Angiotensin-2 Receptor Blockers are not associated with severe SARS-COVID19 infection in a multi-site UK acute Hospital Trust. Eur J Heart Fail. 2020 doi: 10.1002/ejhf.1924. 10.1002/ejhf.1924. doi:10.1002/ejhf.1924. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J, Wang X, Chen J, Zhang H, Deng A. Association of Renin-Angiotensin System Inhibitors With Severity or Risk of Death in Patients With Hypertension Hospitalized for Coronavirus Disease 2019 (COVID-19) Infection in Wuhan, China. JAMA Cardiol. 2020:e201624. doi: 10.1001/jamacardio.2020.1624. doi:10.1001/jamacardio.2020.1624. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020:e201017. doi: 10.1001/jamacardio.2020.1017. doi:10.1001/jamacardio.2020.1017. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–8. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020:e200950. doi: 10.1001/jamacardio.2020.0950. doi:10.1001/jamacardio.2020.0950. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gao L, Jiang D, Wen XS, Cheng XC, Sun M, He B, et al. Prognostic value of NT-proBNP in patients with severe COVID-19. Version 2. Respir Res. 2020;21:83. doi: 10.1186/s12931-020-01352-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet. 2013;381:496–505. doi: 10.1016/S0140-6736(12)61266-5. [DOI] [PubMed] [Google Scholar]
- 36.Blackburn R, Zhao H, Pebody R, Hayward A, Warren-Gash C. Laboratory-Confirmed Respiratory Infections as Predictors of Hospital Admission for Myocardial Infarction and Stroke:Time-Series Analysis of English Data for 2004-2015. Clin Infect Dis. 2018;67:8–17. doi: 10.1093/cid/cix1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kwong JC, Schwartz KL, Campitelli MA, Chung H, Crowcroft NS, Karnauchow T, et al. Acute Myocardial Infarction after Laboratory-Confirmed Influenza Infection. N Engl J Med. 2018;378:345–53. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 38.Arabi YM, Balkhy HH, Hayden FG, Bouchama A, Luke T, Baillie JK, et al. Middle East Respiratory Syndrome. N Engl J Med. 2017;376:584–94. doi: 10.1056/NEJMsr1408795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Libby P, Nahrendorf M, Swirski FK. Leukocytes Link Local and Systemic Inflammation in Ischemic Cardiovascular Disease:An Expanded “Cardiovascular Continuum. J Am Coll Cardiol. 2016;67:1091–103. doi: 10.1016/j.jacc.2015.12.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020:ciaa248. doi: 10.1093/cid/ciaa248. doi:10.1093/cid/ciaa248. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009;145:24–33. doi: 10.1111/j.1365-2141.2009.07600.x. [DOI] [PubMed] [Google Scholar]
- 42.Libby P, Loscalzo J, Ridker PM, Farkouh ME, Hsue PY, Fuster V, et al. Inflammation, Immunity, and Infection in Atherothrombosis:JACC Review Topic of the Week. J Am Coll Cardiol. 2018;72:2071–81. doi: 10.1016/j.jacc.2018.08.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu Q, Zhou L, Sun X, Yan Z, Hu C, Wu J, et al. Altered Lipid Metabolism in Recovered SARS Patients Twelve Years after Infection. Sci Rep. 2017;7:9110. doi: 10.1038/s41598-017-09536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019:retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W, et al. Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. N Engl J Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ullah W, Saeed R, Sarwar U, Patel R, Fischman DL. COVID-19 complicated by Acute Pulmonary Embolism and Right-Sided Heart Failure. JACC Case Rep. 2020 doi: 10.1016/j.jaccas.2020.04.008. doi:10.1016/j.jaccas.2020.04.008. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Paranjpe I, Fuster V, Lala A, Russak A, Glicksberg BS, Levin MA, et al. Association of Treatment Dose Anticoagulation with In-Hospital Survival Among Hospitalized Patients with COVID-19. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.05.001. S0735-1097(20)35218-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–6. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oudkerk M, Büller HR, Kuijpers D, van Es N, Oudkerk SF, McLoud TC, et al. Diagnosis, Prevention, and Treatment of Thromboembolic Complications in COVID-19:Report of the National Institute for Public Health of the Netherlands. Radiology. 2020:201629. doi: 10.1148/radiol.2020201629. doi:10.1148/radiol.2020201629. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]