Abstract
Fatigue and anhedonia are commonly reported, co-occurring clinical symptoms associated with chronic illnesses. Fatigue is a multidimensional construct that is defined as a distressing, persistent, subjective sense of physical, cognitive, or emotional tiredness that interferes with usual functioning. Anhedonia is a component of depressive disorders and other psychiatric conditions, such as schizophrenia, and is defined by the reduced ability to experience pleasure. Both symptoms greatly affect the health-related quality of life of patients with chronic illnesses. Although fatigue and anhedonia are commonly associated with each other, understanding the differences between the two constructs is necessary for diagnosis and clinical treatment. A scoping review was conducted based on published guidance, starting with a comprehensive search of existing literature to understand the similarities and differences between fatigue and anhedonia. An initial search of PubMed using fatigue and anhedonia as medical subject headings yielded a total of 5254 articles. A complete full-text review of the final 21 articles was conducted to find articles that treated both constructs similarly and articles that presented fatigue and anhedonia as distinct constructs. About 60% of the reviewed articles consider both constructs as distinct, but a considerable number of the reviewed articles found these constructs indistinguishable. Nomenclature and biology were two themes from the reviewed articles supporting the idea that anhedonia and fatigue are indistinguishable constructs. The information generated from this review is clinically relevant to optimize the management of fatigue related to anhedonia from other fatigue subtypes.
Subject terms: Diseases, Schizophrenia
Introduction
Fatigue is a commonly reported and disabling symptom in neurological1,2, rheumatologic3,4, and oncologic conditions5. It is generally defined as a feeling of malaise, lack of energy, and complaints of tiredness and exhaustion6. Fatigue is often associated with depression and is described as a core symptom of major depressive episode (MDE)7,8. However, one study reported that fatigue independently decreased the quality of life of patients when controlling for depression and other symptoms6. Despite its prevalence, the etiology of fatigue is still poorly understood due to the multidimensionality of this construct9. Fatigue is proposed to comprise of physical, affective, and cognitive dimensions10,11. Currently, fatigue is measured by validated self-report instruments12.
Anhedonia is also present in a myriad of diseases; however, it is most commonly known as a major symptom of depression13 and other psychiatric conditions, such as schizophrenia7,14. Anhedonia, which translates to “without pleasure” in Greek15, is defined as the inability or diminished ability to experience pleasure16. Like fatigue, anhedonia has been proposed to comprise of different categories of pleasure, such as physical, social, anticipatory, motivational, and consummatory pleasures. Individuals with anhedonia are still able to experience pain and negative emotions, but usually they no longer participate in previously pleasurable activities17. Like fatigue, measuring anhedonia is difficult as it relies on the subjective experience of pleasure and is generally measured by self-report.
Seminal articles have explored the relationships of fatigue and anhedonia in psychiatric conditions. For example, endogenomorphic depression equated low energy to fatigue and anhedonia without distinguishing one from the other18. In schizophrenia, although there was also no distinction of low energy as fatigue or anhedonia, the understanding of low energy was linked to a neurological dysfunction in this disorder19. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), anhedonia and fatigue are features of psychiatric disorders, most notably, major depressive disorder (MDD) and schizophrenia7. While the two symptoms are commonly understood as co-occurring within these psychiatric conditions, current research elucidates the individual complexities and unique attributes of each symptom20,21. The recommended management of fatigue and anhedonia involves pharmacological stimulants and treatment of the associated chronic illness22. Despite these advances, there is still limited literature that clarifies the relationship between fatigue and anhedonia. This scoping review was conducted based on established methodological frameworks23 in order to clarify the relationship between fatigue and anhedonia from the extant literature.
Methods and study selection
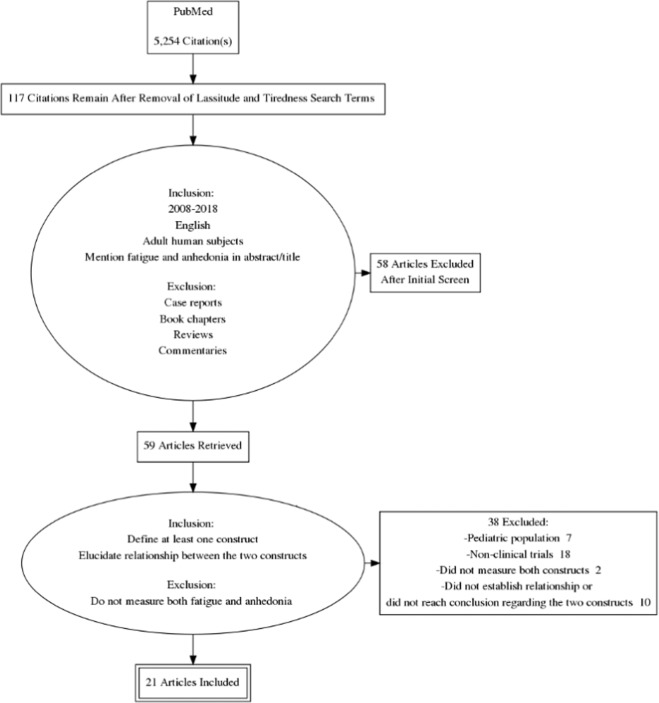
An initial literature query was conducted using the PubMed database with the assistance of a medical librarian at the National Institutes of Health. We used “fatigue” and “anhedonia” as MeSH terms and included the corresponding synonyms, such as “lassitude” and “tiredness.” This initial search yielded 5254 articles.
Fatigue and tiredness are used interchangeably. For example, in some measures like the Fibromyalgia Impact Questionnaire (FIQ), its main descriptor is fatigue, and then one of its subscale is morning tiredness65. In this case, fatigue and tiredness are loosely differentiated. This non-differentiation is also observed in the way fatigue is described in many medical conditions where it states, “the tiredness or lack of energy in fatigue is associated with exhaustion”66. For this review, the authors focused solely on fatigue as the construct of interest and its association with anhedonia. After removing “lassitude” and “tiredness” as search terms, 117 articles remained.
Our second filtering criteria aimed to remove articles that were not written in English, did not enroll human participants, or were published before 2008. Letters, commentaries, meeting abstracts, editorials, and dissertations were also excluded. This second screen narrowed our initial yield total to 61 articles for full-text review.
To establish the relationship between the two constructs, articles that did not measure both fatigue and anhedonia were excluded. Further, articles that did not define at least one of the constructs or help elucidate the relationship between the two constructs were also excluded. A final 21 articles were included in this scoping review (Fig. 1). These 21 articles are summarized in Tables 1 and 2.
Fig. 1. Screening flow process.
Figure describes the procedures and the eligibility criteria used to select articles to be included in the review, based on the methods required for scoping reviews67.
Table 1.
Fatigue and anhedonia as associated constructs.
| Author | Population | Definition of fatigue | Measurement of fatigue | Definition of anhedonia | Measurement of anhedonia | Relationship of the constructs |
|---|---|---|---|---|---|---|
| Capuron et al.24 | n = 35 hepatitis C virus (HCV) patients | Not specified; fatigue subscales tested: general, physical, mental, reduced activity, reduced motivation | MFI | Not specified | SHAPS | Cytokines may contribute to anhedonia and fatigue in depression due to effects on dopamine function. Reduced activation of the ventral striatum was significantly correlated with greater symptoms of anhedonia, depression, and fatigue |
| DellaGioia et al.25 | n = 10 healthy participants | Not specified | POMS-Fatigue | Social interest | MADRS-Anhedonia | Bupropion (norepinephrine and dopamine reuptake inhibitor) had NO effect on lipopolysaccharide-induced depressive symptoms (anhedonia and fatigue). This suggests that these symptoms can be reduced by serotonin reuptake inhibition (Hannestad et al.46) but not by norepinephrine or dopamine reuptake inhibition |
| Hannestad et al.46 | n = 11 (men = 6) healthy patients | Not specified | MADRS-Lassitude | Social anhedonia: visual analog scale of “I want to be alone” versus “I want to be with other people” | VAS | Citalopram, which has negligible effects on neurotransmitters other than serotonin, can reduce endotoxin-induced fatigue. Most of the preventative effect of citalopram was due to an inhibition of endotoxin-induced increases in the lassitude item of MADRS, which measures fatigue and motivation |
| Johansson et al.29 | n = 627 (age range: 65–82) | Loss of energy | SF-36 | Loss of interest in usual activities | HADS | Fatigue, anhedonia, and sleepiness were amalgamated into the same symptom cluster called “sickness behavior.” This symptom cluster is associated with inflammation |
| Pfeil et al.33 | N = 218 unemployed (at least 12 months) patients at least 50 y/o | Loss of energy | DSM-IV TR or DSM-V criteria; PHQ-9 | Loss of interest and pleasure | DSM-IV TR or DSM-V criteria; PHQ-9 | Depressed mood, anhedonia, and fatigue are the most frequently reported symptoms in patients with minor depression. These symptoms distinguish minor depression from major depression |
| Chaudhari et al.68 | n = 267 PD patients (n = 89 control/placebo) (men = 58) | “Fatigue (tiredness) or lack of energy”—as defined by the NMSS | NMSS | “Difficulty experiencing pleasure”—as defined by the NMSS | NMSS | Rotigotine transdermal system has a positive effect on fatigue and mood disturbances (symptoms of depression and anhedonia), and apathy in patients with PD |
| Solla et al.37 | n = 81 PD patients (men = 48) | Physical fatigue. Classified as a non-motor symptom | PFS; FSS | Classified as a non-motor, affective symptom | NMSS | Motor and non-motor symptoms of PD are related to fatigue severity, although non-motor symptoms and mostly affective conditions (anhedonia) and sleep disturbances were the main factors influencing fatigue. The affective sphere seems to be closely related to the appearance of fatigue |
| Tsai et al.39 | n = 986,647 veterans from 130 VA facilities (men = 897,849) | Generally accepted to be a somatic symptom | PHQ-9 | Not known to be somatic or non-somatic. Different models argue differently | PHQ-9 | DSM-5 MDD symptoms are best represented by two factors, as somatic and non-somatic (or affective) factors. Somatic factors include symptoms like fatigue and anhedonia |
Lists the articles that presented fatigue and anhedonia as indistinguishable constructs.
Table 2.
Fatigue and anhedonia as separate constructs.
| Author | Population | Definition of fatigue | Measurement of fatigue | Definition of anhedonia | Measurement of anhedonia | Relationship of the constructs |
|---|---|---|---|---|---|---|
| Ang et al.32 | n = 505 healthy (men = 211, 23 = gender undisclosed); online survey | The feeling of exhaustion caused by the exertion of effort, which is unrelated to actual exertion of energy by muscles | MFIS | Is a mood disorder characterized by an inability to derive pleasure | SHAPS | Different subtypes of apathy are predictive of different associations with depression, anhedonia, and fatigue in healthy people. Apathy and anhedonia have a close relationship; however, there are unique aspects of anhedonia not related to apathy |
| Bennett et al.40 | All women (n = 20 CFS, n = 20 post cancer fatigue, n = 16 major depression) | Physical fatigue in chronic fatigue: “difficulty achieving motor tasks,” mental fatigue in chronic fatigue: “difficulty achieving cognitive tasks” | SCIN; SPHERE | “Loss of motivation”, “mood disturbance” | SCIN, SPHERE | Fatigue in women with chronic fatigue syndrome, post-infective fatigue syndrome, post-cancer fatigue, and major depression is an indistinguishable symptom of depression. Anhedonia, however, is unique and a distinguishable symptom of depression. Fatigue–sadness was most associated with an increased risk of major cardiac events |
| Doyle et al.41 | n = 408 hospitalized with acute coronary syndrome (ACS) (men = 326.7) | Classified as vital exhaustion, “tired,” “without energy” | HADS-D; BDI-FS | Not specified | HADS-D; BDI-FS | Anhedonia may be potentially less cardiotoxic than fatigue and sadness, which are strong predictors of cardiovascular prognosis |
| Drijgers et al.45 | n = 25 with PD, 25 healthy controls (AGE matched) female = 2 in each group, 4 total | Not specified | POMS | A mood and motivational symptom | SHAPS | Acute stimulation of methylphenidate (dopamine reuptake inhibitor), but not pramipexole (dopamine 2 receptor agonist), improved anhedonia and vigor in PD patients, implies that dopamine plays a role in mood (anhedonia) but not cognition (fatigue) |
| Emmert-Aronson and Brown27 | N = 2907 anxiety/mood disorder patients | As defined by DSM-IV | ADIS-IV-L-semi-structured interview and dimensionally rated | Correlated with low mood, as defined by DSM-IV | ADIS-IV-L-semi-structured interview and dimensionally rated | “Depressed mood” and “anhedonia” showed higher discrimination of higher depression (alpha = 3.25) than the other symptoms. Fatigue also discriminates better than most symptoms (alpha = 1.97). Anhedonia and depressed mood are required for diagnosis of MDD but could also create a very inclusive and encompassing symptom set for all severities of depression that includes depressed mood, anhedonia, fatigue, and concentration difficulties |
| Hawkins et al.28 | n = 326 HF patients (women = 132) | Physical, somatic symptom of depression | PHQ-9 | Behavioral, non-somatic symptom of depression | PHQ-9 | Interventions that target a patient’s somatic symptoms (fatigue) may not yield maximum cognitive benefit compared to comprehensive treatment that targets depressed mood, anhedonia, and other non-somatic symptoms |
| Lapidus et al.30 | n = 11 with major depressive disorder (MDD), n = 10 age-/sex-matched controls | Not specified. Noted to have an effect on motivation to participate in enjoyable activities | MFI | Reduced capacity to experience pleasure | QIDS-SR | There is no association between fatigue and glutathione levels (antioxidant) in the MDD group. Anhedonia is negatively correlated with brain occipital glutathione levels, supporting the role of glutathione in oxidative stress and inflammation, specifically in anhedonia in MDD |
| Leventhal et al.44 | n = 187 regular smokers | Fatigue domain in POMS: “Fatigue (e.g., “worn out,” “fatigued”)” | POMS-Fatigue | Anhedonia, a specific factor for depression indicative of reduced interest/motivation, pleasure, and positive affect, and is putatively distinct from anxiety | MASQ-AD; (e.g., “felt like there wasn’t anything interesting or fun to do,” “felt like nothing was very enjoyable”) | Anhedonia, but not fatigue, was associated with only abstinence-induced reductions in positive affect. Used the tripartite model to elucidate the relation of anxiety and depressive symptoms to tobacco withdrawal and found that anhedonia predicts greater smoking relapse risk |
| McGuire et al.31 | n = 323 (women = 73) patients who were admitted because of a cardiac event | Physical or mental weariness, part of somatic symptom cluster of depression | BDI; HRSD | Loss of interest or pleasure in activities, part of cognitive/affective symptom cluster of depression | BDI, HRSD | Cognitive/affective symptom clusters (anhedonia) is important for initial screening and are unique correlates of depression in patients with CHD. However, cognitive/affective symptoms must accompany somatic symptoms (fatigue) before depression can be diagnosed |
| Olivan-Blazquez et al.42 | n = 741 primary care patients | Loss of energy within the context of depression | DSM-V criteria; CIDI v2 | Decreased/lack of interest within the context of depression | DSM-V criteria | Out of the nine proposed diagnostic symptoms of depression, anhedonia and depressed mood are essential for the diagnosis. Anhedonia was significant in the first 6–12 months of onset of depression. Fatigue was only significant within the first 12 months of onset of depression |
| Ritchie et al.35 | n = 1000 community-dwelling older adults (age >65 years) | Feeling tired, classified as a physical symptom | BSS | Classified as an affective symptom | BSS | Fatigue was found to be most related to other symptoms and most commonly endorsed when evaluating symptoms in older adults. No conclusion on anhedonia |
| Sibitz et al.36 | n = 290 physically ill general hospital patients | Decreased energy or increased fatigability | PQm (adapted) | Loss of interest of pleasure | PQm (adapted) | Inclusion of “fatigue” does not yield an advantage to just using “depressed mood” and/or “anhedonia” to screen depression. Special attention to be paid to “anhedonia” as a screening symptom of depression |
| Trincas et al.38 | n = 456 participants (women = 328), with dysphoric reactions (low mood to depression) | Physical symptom of depression | CES-D; DSM-V criteria | Predicted by Failure schema in the Young Schema Questionnaire, which is the belief that one is inadequate compared with others | CES-D; DSM-V criteria | Depression is not a unitary phenomenon. Fatigue and other physical symptoms were not predicted by any of the early maladaptive schemas (EMSs). The occurrence of anhedonia was predicted by the EMS Failure, that is, the belief that one is inadequate compared with others |
Lists the articles that presented fatigue and anhedonia as distinct constructs.
Results
Characteristics of the selected articles
Sixteen of the 21 articles were published in the past 5 years. More than half (60%) were cross-sectional studies24–40, while two were longitudinal prospective cohort studies41,42. Two articles used both cross-sectional and longitudinal study designs1,24,40,43. There was one within-subject experimental study design44 and three randomized placebo-controlled trials25,45–47.
Across the 21 studies, 9 were conducted in Europe26,29,32,33,36–38,41,42,45, and 10 were conducted in the United States24,25,27,28,30,31,35,39,44,46. One study took place in Australia40, and another study was a multi-continental venture involving 12 different countries47. Out of the 9175 participants enrolled across these studies (excluding the veteran population study), 45.7% of the participants enrolled were male. One study analyzed medical records from a veteran database that enlisted close to a million veterans in the United States, 91% of whom were male39. Three studies enrolled in-patient participants31,36,41, and seven studies enrolled outpatient populations24,26,30,36,37,42,45. The rest enrolled healthy or primary care patients.
A common patient population studied was those with heart conditions (19%), including depression in acute coronary syndrome patients41, heart failure28, coronary heart disease31, and impaired cardiac function in community-dwelling elders29. About 14% of the studies enrolled patients with Parkinson’s disease (PD)37,45,47. Other patient populations included patients with chronic hepatitis C virus (HCV)24, cancer40, anxiety and mood disorders27, MDD or depression30,33, dysphoric episodes38, and non-psychiatric conditions who were hospitalized36. Healthy volunteers25,32,46 and primary care patients42 were also assessed, as were community-dwelling elder adults35 and tobacco smokers44.
Two studies collected data via online assessments32,38, and four studies either retrospectively analyzed data or utilized previously collected datasets29,31,39,47. Two studies utilized healthy controls30,45, and six studies used the control groups or placebo groups for comparison24–26,33,46,47.
Assessments of fatigue and anhedonia
Questionnaires used in the reviewed articles that assessed both fatigue and anhedonia included the Clinical Interview Neurasthenia, the Somatic Psychological Health Report, Hospital Anxiety and Depression Scale, Beck Depression Inventory, Hamilton Rating Scale for Depression, Diagnostic and Statistical Manual of Mental Disorders (DSM-IV and DSM-V), Brief Symptom Screen, modified Patient Questionnaire, the Center for Epidemiologic Studies Depression Scale, the Montgomery–Asberg Depression Rating Scale (MADRS), Non-Motor Symptoms Questionnaire, and the Patient Health Questionnaire (PHQ-9).
The DSM-IV and DSM-V criteria were used the most by the reviewed articles to define fatigue27,33,38,42. A total of seven different questionnaires were used to specifically assess fatigue, which included the Modified Fatigue Impact Scale, Multidimensional Fatigue Inventory, Profile Mood of States-Fatigue (POMS-F), Vitality Scale of the Short Form Health Survey (SF-36), Fatigue Severity Scale, Parkinson’s Disease Fatigue Scale, and the sleep/fatigue domain of the Non-Motor Symptoms Scale (NMSS).
The Snaith–Hamilton Pleasure Scale was the commonly used questionnaire to assess anhedonia24,32,45 and has been validated to measure anhedonia48. Other questionnaires that were used to assess anhedonia included the Visual Analog Scale for anhedonia, the Quick Inventory of Depressive Symptomology-Self Report, Mood and Anxiety Symptom Questionnaire—Anhedonic Depression Symptom, item 8 of the MADRS-Anhedonia, and the mood/apathy domain of the NMSS.
Definition of fatigue
There was no consensus on the definition of fatigue. By far, the most common definition of fatigue described it as a loss of energy or a lack of energy29,33,36,42. Similarly, fatigue was also described as a physical feeling of lassitude46, feeling tired35, the feeling of exhaustion or vital exhaustion32,41, worn out as described by POMS44, and decreased energy or increased fatigability36. Some articles classified fatigue as a non-motor symptom of PD26,37, while other articles classified it as a somatic or physical symptom of depression28,31,35,38,39. Capuron et al.24 tested different subscales of fatigue, including general fatigue, physical fatigue, and mental fatigue. Bennett et al.40 described both physical and mental fatigue, where physical fatigue in chronic fatigue syndrome was defined as “difficulty achieving motor tasks” and mental fatigue was defined as “difficulty achieving cognitive tasks.”
Definition of anhedonia
There was not a clear consensus on the definition of anhedonia. By far, the most common definition of anhedonia was a loss of interest or pleasure in activities29,31,33,36. Similarly, anhedonia was also defined as a decreased/lack of interest42, dysphoria or a markedly diminished interest/pleasure in most daily activities34, and reduced interest/motivation, pleasure, and positive affect and is putatively distinct from anxiety44. Anhedonia was also defined as an impaired ability to experience pleasure or difficulty experiencing pleasure24,30,47. The construct of anhedonia was categorized as a behavioral, non-somatic symptom of depression28 or classified as a non-motor, affective symptom in PD37 or an affective symptom in community-dwelling older adults35. Anhedonia was also commonly classified as a mood disturbance or motivational symptom32,40,45. Anhedonia was also defined by its dimensions, such as social anhedonia, which was assessed by a one-item VAS, “I want to be alone” on one end and “I want to be with others” on the other end46. Trincas et al.38 noted that anhedonia was predicted by the Failure schema in the Young Schema Questionnaire, which is the belief that one is inadequate compared with others in the context of depressive symptoms following dysphoric episodes.
Relationship of fatigue and anhedonia
Eight studies presented fatigue and anhedonia as associated or overlapping constructs. For example, four articles presented fatigue and anhedonia both as symptoms of depression24,33,39,46. These articles showed the two constructs as related within the context of depression. Three articles presented potentially common mechanisms or pathways to explain how the symptoms of fatigue and anhedonia are associated24,46,47. Capuron et al.24 presented a potential mechanism by which inflammatory cytokines affect fatigue and anhedonia, thereby implicating dopamine function as a common mechanism shared by the two constructs in the HCV patient population. Hannestad et al.46 implicated citalopram, a serotonin reuptake inhibitor, as having a preventative effect on endotoxin-induced increases in fatigue and motivation (anhedonia). Chaudhari et al.68 found that the rotigotine transdermal system (a non-ergoline dopamine receptor agonist) may have a positive effect on fatigue and mood disturbances (anhedonia) in patients with PD. Fatigue and anhedonia when amalgamated into a symptom cluster called “sickness behavior,” were also shown to be associated with inflammation and directly affected by impaired cardiac function in patients with cardiac failure29. Finally, two articles presented fatigue and anhedonia as one of the prodromal symptoms of a condition, such as early-stage PD26,37.
However, 12 articles presented fatigue and anhedonia as separate constructs, each with its own unique implications. Four articles presented anhedonia as a unique and distinguishable symptom of depression in that fatigue alone is not enough to diagnose major depression31,36,40,42. These four articles described the importance of anhedonia, more so than fatigue, as a diagnostic screening tool for depression, because it was found that anhedonia is an essential and distinguishing feature of a depression diagnosis. Two articles implicated separate pathophysiological mechanisms for fatigue and anhedonia30,45. Drijgers et al.45 found that acute stimulation of methylphenidate (norepinephrine–dopamine reuptake inhibitor) improved anhedonia and vigor in PD patients, implying that dopamine plays a role in anhedonia (mood) but not fatigue (cognition). Lapidus et al.30 found that anhedonia, but not fatigue, is negatively correlated with brain glutathione levels in patients with MDD. Three other articles found that either fatigue or anhedonia had unique implications on specific patient populations28,41,44. Doyle et al.41 found that anhedonia could potentially be less cardiotoxic than fatigue and sadness in hospitalized patients with acute coronary syndrome. Hawkins et al.28 found that interventions targeting patients’ somatic symptoms, such as fatigue, may not yield maximum cognitive benefit in comparison to comprehensive treatment targeting non-somatic symptoms, such as anhedonia in patients with heart failure. Leventhal et al.44 implicated anhedonia, but not fatigue, as being predictive of greater smoking relapse risk in the tobacco-smoking population.
Anhedonia was found to be predicted by an early maladaptive schema of failure when analyzing symptoms of depression that emerged after dysphoric episodes and its potential to be predicted by stable personality characteristics like early maladaptive schemas38. In aging populations (age >65 years), fatigue but not anhedonia was found to be most related to other symptoms and most commonly reported by the elderly population35. Finally, fatigue and anhedonia were also shown to be associated with different subtypes of apathy in healthy people32.
Discussion
This review explored the association between fatigue and anhedonia. About 60% of the reviewed articles considered both constructs as distinct, but still, a considerable number of the reviewed articles found these constructs indistinguishable. This finding has several clinical and research implications: (1) the lack of agreement in the association of both constructs poses more questions on current diagnostic criteria that clumps both constructs together, (2) the initial evidence of distinct biologic underpinnings for each construct provides opportunities to develop targeted therapies, and (3) the lack of consensus in a standard approach to measuring these constructs provides challenges to appropriately apply the diagnostic criteria and evaluate distinct etiologies for these constructs.
Anhedonia and fatigue as indistinguishable constructs
In the reviewed articles, nomenclature and biology were two themes supporting the idea that anhedonia and fatigue are indistinguishable constructs. Some conditions, such as depression, historically consider fatigue and anhedonia as inter-related and interchangeable constructs, except when motor systems are affected. Depressive symptoms are often categorized into somatic and non-somatic symptoms39. Anhedonia is clustered together with concentration difficulties and psychomotor agitation/retardation; while fatigue, together with sleep difficulties, and appetite changes are often classified under the somatic category of depressive symptoms.
Anhedonia was first featured in the DSM and the International Classification of Diseases in 1992, while fatigue was featured in DSM-III in 198049. In the early versions of the DSM, fatigue was suggested to mean physical energy50 and described as “flu-like symptoms” in depressive disorders of DSM-III51. There were no diagnostic criteria for fatigue as a stand-alone somatoform disorder in DSM-III51. Hence, fatigue, like insomnia, was less frequently diagnosed as a separate condition because the established criteria prohibited the classification of either of these symptoms as a stand-alone somatoform disorder52.
As the historical usage of fatigue suggests a loss of physical energy, fatigue has been considered as synonymous with a loss in pleasure experience16. Researchers argue that loss of energy or loss of pleasure can be traced to neural systems that block reward reinforcement from the source of pleasurable stimuli18. When the DSM was revised, the term anhedonia expanded from the “loss of pleasure” to also include the loss of interest and/or capacity for pleasure with the inclusion of melancholia features, which is the inability to respond to all pleasurable stimuli53. It was from this distinction in DSM-IV that fatigue meshed with the melancholia construct53.
Another concept that clumps these two constructs together is sickness behavior. Sickness behavior refers to the coordinated set of behavioral changes that develop in individuals during the course of an infection. These changes are due to the effects of pro-inflammatory cytokines that influence the nervous system and behavior54. In depression, a network of cytokines are believed to regulate mood and influence motivation54. It is believed that, during acute infection, pro-inflammatory cytokines like interleukin (IL)-1, IL-6, and tumor necrosis factor-alpha are released peripherally via a fast transmission pathway, which influences the activities of the primary afferent nerves. The interactions between the pro-inflammatory cytokines and the primary afferent nerves activate the hypothalamic–pituitary–adrenal axis producing a constellation of behavioral symptoms referred to as sickness behavior, which include fatigue and anhedonia54,55. What is lacking in this hypothesis is that these specific symptoms exist under a wider cluster of comorbid conditions so that these sickness behaviors may not exclusively include fatigue and anhedonia behaviors. Long-term administration of inflammatory cytokines was also observed to decrease activation in the ventral striatum, which significantly correlated with greater symptoms of anhedonia, depression, and fatigue24. Administration of these inflammatory cytokines was associated with decreased presynaptic striatal dopamine, and these changes correlated with behavioral alterations in fatigue and anhedonia47. Application of a non-ergoline dopamine receptor agonist (rotigotine transdermal patches) improved both fatigue and anhedonia in patients with PD. These findings support the idea that the interplay of peripheral and central mechanisms triggered by inflammation blur distinct pathways that can distinguish fatigue from anhedonia.
Anhedonia and fatigue as distinct constructs
Clinical reports of persistent fatigue after remission of depression helped pave the notion that perhaps anhedonia and fatigue are distinct constructs32. The reviewed articles proposed that distinct biology distinguishes these constructs. The roles of dopamine47, serotonin25, and oxidative stress/inflammation30 were specifically mentioned as pathways that can distinguish fatigue and anhedonia.
Methylphenidate (dopamine reuptake inhibitor) was used to improve anhedonia but not fatigue in patients with PD in comparison to controls45. Pramipexole (a dopamine D2 receptor agonist), on the other hand, had negative effects on mood and fatigue but had an insignificant effect on anhedonia46. Pretreatment of bupropion (a dopamine and norepinephrine reuptake inhibitor) had no significant effect on lipopolysaccharide-induced anhedonia and fatigue, while pretreatment with citalopram (a serotonin reuptake inhibitor) significantly improved endotoxin-induced fatigue but had no effect in anhedonia46). These findings serve to implicate the distinct roles of dopamine and serotonin receptors in distinguishing anhedonia from fatigue.
Fatigue and anhedonia in the context of psychiatric conditions
Fatigue and anhedonia have been explored not only in depression but also in other psychiatric conditions such as schizophrenia, where one in every three patients has anhedonia14,56–58. In depression, the seminal work of Klein18 pointed out the construct of low energy in depression, specifically in individuals with the depressive-neurotic type of personality. This personality type has low self-esteem and depends on external environmental cues to experience pleasure18. In schizophrenia, anhedonia is a core negative symptom and is associated with functional impairment59. It is captured as the “diminished ability to experience pleasure”19.
Instruments used to assess depression used similar and distinguishing terms to capture fatigue and anhedonia. For example, MDD, as described in DSM-V, treats fatigue as “low energy” and anhedonia as a “lack of pleasurable interests.” In the 17-item Hamilton Depression Scale, the construct of fatigue is captured in items that used the following terms: “somatic symptoms,” “loss of energy,” and “fatigability,” while anhedonia is captured using the following terms: “loss of interest in hobbies, decreased social activities, decreased in productivity, and inability to work”60.
State versus trait anhedonia
In differentiating fatigue from anhedonia, the understanding of state versus trait anhedonia may be helpful. Anhedonia is a complex and nuanced symptom related to a number of health conditions. It occurs independently of one’s ability to experience general stimulation and negative emotions61. In addition, it can occur with or without feelings of sadness62. The pathological symptom of anhedonia presents itself in various psychological and physical conditions and likely involves dysregulation of a number of neurochemical pathways in the brain63. When other mental or physical symptoms are present, anhedonia can be conceptualized as a pathologic symptom (state) of the primary condition, such as in depression or schizophrenia. Nevertheless, the literature is silent on whether state or trait anhedonia is associated with fatigue. However, hedonic inability, whether as a symptom or a trait, is frequently correlated with the presence of psychomotor delay even if confused with affective flattening in schizophrenia or even if it represents as a psychopathologic characteristic that is specific for depression64.
Gaps in the study
Three gaps were observed in this review: (1) lack in consensus in the definitions of fatigue and anhedonia, (2) lack of agreement in standard measures to assess fatigue and anhedonia, and (3) no validated shared and/or distinct pathways that can explain the association of both constructs. The lack of consensus stems from how the fatigue construct was understood within depression in DSM-III and the way fatigue has evolved to its current stand-alone construct in DSM-V to include its dimensions, such as physical, cognitive, and behavioral components7.
Anhedonia continues to be a diagnostic criterion in MDE diagnosis in DSM-V separate from fatigue. Its description overlapped and became more pronounced in the diagnostic criteria of unspecified depressive disorder with melancholic features7. However, since the anhedonia construct has evolved to include dimensions of perception (cognitive), action/sensorial/motor (physical), and pleasure (affective), it began to overlap with the construct of apathy (lack of emotion). These fatigue and anhedonia usages were first treated as co-existing constructs in depression. The comorbid status of depression with other medical conditions impacts the understanding of the fatigue–anhedonia relationship. One example of this is reflected in PD with comorbid depression. The lack of condition-specific definitions of constructs are observed in the current measures that assess anhedonia and fatigue. Further, the lack of clarity in the relationship of fatigue and anhedonia has slowed our understanding of the neural pathways that influence these behaviors, including the role of presynaptic striatal dopamine, the serotonergic regulation, oxidative stress pathways, and the role of inflammation.
Recommendations
There is a need to establish condition-specific definitions to understand further the dynamic relationships of fatigue and anhedonia. In the future revision of the DSM criteria, the dimensional construct of fatigue should be considered to classify its severity, duration, and frequency. Similarly, the melancholic features of depressive disorders require a dimensional understanding of anhedonia as a construct. Future research designs must capture the dimensional understanding of fatigue and anhedonia in relation to specific medical conditions of interest.
Conclusion
The purpose of this review was to clarify the relationship of fatigue and anhedonia. Historically, diagnostic nomenclature of fatigue and anhedonia had overlaps in its usage (DSM-III, DSM-IV). Through time, anhedonia had its own descriptive criteria in the melancholia features of MDDs. In DSM-V, fatigue severity is recognized as a unique entity. The future of discriminating the relationships between the two constructs must take into account the health condition being studied and its comorbidities.
Acknowledgements
The authors thank Alicia A. Livinski, MPH, MLS, NIH Library Writing Center for manuscript editing. The authors also thank Diane Cooper, NIH Library for her assistance with literature search. The present study is fully supported by the Division of Intramural Research of the National Institute of Nursing Research, National Institutes of Health, Bethesda, MD, USA under Grant number: ZIA NR000020-06.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Friedman JH, et al. Fatigue in Parkinson’s disease: a review. Mov. Disord. 2007;22:297–308. doi: 10.1002/mds.21240. [DOI] [PubMed] [Google Scholar]
- 2.Krupp L. Fatigue is intrinsic to multiple sclerosis (MS) and is the most commonly reported symptom of the disease. Mult. Scler. 2006;12:367–368. doi: 10.1191/135248506ms1373ed. [DOI] [PubMed] [Google Scholar]
- 3.Murphy SL, Smith DM, Clauw DJ, Alexander NB. The impact of momentary pain and fatigue on physical activity in women with osteoarthritis. Arthritis Rheum. 2008;59:849–856. doi: 10.1002/art.23710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramsey-Goldman R, Rothrock N. Fatigue in systemic lupus erythematosus and rheumatoid arthritis. PM R. 2010;2:384–392. doi: 10.1016/j.pmrj.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 5.Liu L, et al. The longitudinal relationship between fatigue and sleep in breast cancer patients undergoing chemotherapy. Sleep. 2012;35:237–245. doi: 10.5665/sleep.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Visser MR, Smets EM. Fatigue, depression and quality of life in cancer patients: how are they related? Support Care Cancer. 1998;6:101–108. doi: 10.1007/s005200050142. [DOI] [PubMed] [Google Scholar]
- 7.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (APA, Washington, DC, 2013).
- 8.Ray C. Chronic fatigue syndrome and depression: conceptual and methodological ambiguities. Psychol. Med. 1991;21:1–9. doi: 10.1017/s0033291700014586. [DOI] [PubMed] [Google Scholar]
- 9.Sharpe M, Wilks D. Fatigue. BMJ. 2002;325:480–483. doi: 10.1136/bmj.325.7362.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glaus A, Muller S. [Measuring fatigue of cancer patients in the German-speaking region: development of the Fatigue Assessment Questionnaire] Pflege. 2001;14:161–170. doi: 10.1024/1012-5302.14.3.161. [DOI] [PubMed] [Google Scholar]
- 11.Haghighat S, Akbari ME, Holakouei K, Rahimi A, Montazeri A. Factors predicting fatigue in breast cancer patients. Support Care Cancer. 2003;11:533–538. doi: 10.1007/s00520-003-0473-5. [DOI] [PubMed] [Google Scholar]
- 12.Whitehead L. The measurement of fatigue in chronic illness: a systematic review of unidimensional and multidimensional fatigue measures. J. Pain Symptom Manag. 2009;37:107–128. doi: 10.1016/j.jpainsymman.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 13.Higa-McMillan CK, Smith RL, Chorpita BF, Hayashi K. Common and unique factors associated with DSM-IV-TR internalizing disorders in children. J. Abnorm. Child Psychol. 2008;36:1279–1288. doi: 10.1007/s10802-008-9250-8. [DOI] [PubMed] [Google Scholar]
- 14.Horan WP, Kring AM, Blanchard JJ. Anhedonia in schizophrenia: a review of assessment strategies. Schizophr. Bull. 2006;32:259–273. doi: 10.1093/schbul/sbj009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fuhrer R, Wessely S. The epidemiology of fatigue and depression: a French primary-care study. Psychol. Med. 1995;25:895–905. doi: 10.1017/s0033291700037387. [DOI] [PubMed] [Google Scholar]
- 16.Berrios GE, Olivares JM. The anhedonias: a conceptual history. Hist. Psychiatry. 1995;6:453–470. doi: 10.1177/0957154X9500602403. [DOI] [PubMed] [Google Scholar]
- 17.Ho N, Sommers M. Anhedonia: a concept analysis. Arch. Psychiatr. Nurs. 2013;27:121–129. doi: 10.1016/j.apnu.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Klein DF. Endogenomorphic depression. A conceptual and terminological revision. Arch. Gen. Psychiatry. 1974;31:447–454. doi: 10.1001/archpsyc.1974.01760160005001. [DOI] [PubMed] [Google Scholar]
- 19.Meehl PE. Some methodological reflections on the difficulties of psychoanalytic research. Psychol. Issues. 1973;8:104–117. [PubMed] [Google Scholar]
- 20.Dantzer R, Heijnen CJ, Kavelaars A, Laye S, Capuron L. The neuroimmune basis of fatigue. Trends Neurosci. 2014;37:39–46. doi: 10.1016/j.tins.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gorwood P. Neurobiological mechanisms of anhedonia. Dialogues Clin. Neurosci. 2008;10:291–299. doi: 10.31887/DCNS.2008.10.3/pgorwood. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Comprehensive Cancer Network. Fatigue. https://www.nccn.org/patients/resources/life_with_cancer/managing_symptoms/fatigue.aspx (2018).
- 23.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2007;8:19–32. [Google Scholar]
- 24.Capuron L, et al. Dopaminergic mechanisms of reduced basal ganglia responses to hedonic reward during interferon alfa administration. Arch. Gen. Psychiatry. 2012;69:1044–1053. doi: 10.1001/archgenpsychiatry.2011.2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.DellaGioia N, Devine L, Pittman B, Hannestad J. Bupropion pre-treatment of endotoxin-induced depressive symptoms. Brain Behav. Immun. 2013;31:197–204. doi: 10.1016/j.bbi.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 26.Dujardin K, et al. Apathy in untreated early-stage Parkinson disease: relationship with other non-motor symptoms. Mov. Disord. 2014;29:1796–1801. doi: 10.1002/mds.26058. [DOI] [PubMed] [Google Scholar]
- 27.Emmert-Aronson BO, Brown TA. An IRT analysis of the symptoms of major depressive disorder. Assessment. 2015;22:332–340. doi: 10.1177/1073191114544470. [DOI] [PubMed] [Google Scholar]
- 28.Hawkins MA, et al. Cognitive function in heart failure is associated with nonsomatic symptoms of depression but not somatic symptoms. J. Cardiovasc. Nurs. 2015;30:E9–E17. doi: 10.1097/JCN.0000000000000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johansson P, et al. Sickness behavior in community-dwelling elderly: associations with impaired cardiac function and inflammation. Biol. Res. Nurs. 2014;16:105–113. doi: 10.1177/1099800412466170. [DOI] [PubMed] [Google Scholar]
- 30.Lapidus KA, et al. In vivo (1)H MRS study of potential associations between glutathione, oxidative stress and anhedonia in major depressive disorder. Neurosci. Lett. 2014;569:74–79. doi: 10.1016/j.neulet.2014.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGuire AW, Eastwood JA, Hays RD, Macabasco-O’Connell A, Doering LV. Depressed or not depressed: untangling symptoms of depression in patients hospitalized with coronary heart disease. Am. J. Crit. Care. 2014;23:106–116. doi: 10.4037/ajcc2014146. [DOI] [PubMed] [Google Scholar]
- 32.Ang YS, Lockwood P, Apps MA, Muhammed K, Husain M. Distinct subtypes of apathy revealed by the Apathy Motivation Index. PLoS ONE. 2017;12:e0169938. doi: 10.1371/journal.pone.0169938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pfeil S, Holtz K, Kopf KA, Hegerl U, Rummel-Kluge C. Minor depression in older, long-term unemployed people seeking vocational support. BMC Psychiatry. 2017;17:243. doi: 10.1186/s12888-017-1404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Potvin O, Hudon C, Grenier S, Preville M. Non-essential symptoms of depression and cognitive impairment no dementia (CIND) in community-dwelling elders without dysphoria or anhedonia. Int. Psychogeriatr. 2010;22:1344–1352. doi: 10.1017/S1041610210001419. [DOI] [PubMed] [Google Scholar]
- 35.Ritchie CS, et al. Measuring symptoms in community-dwelling older adults: the psychometric properties of a brief symptom screen. Med. Care. 2013;51:949–955. doi: 10.1097/MLR.0b013e3182a53d1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sibitz I, et al. ICD-10 or DSM-IV? Anhedonia, fatigue and depressed mood as screening symptoms for diagnosing a current depressive episode in physically ill patients in general hospital. J. Affect. Disord. 2010;126:245–251. doi: 10.1016/j.jad.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 37.Solla P, et al. Association between fatigue and other motor and non-motor symptoms in Parkinson’s disease patients. J. Neurol. 2014;261:382–391. doi: 10.1007/s00415-013-7207-5. [DOI] [PubMed] [Google Scholar]
- 38.Trincas R, et al. Specific dysphoric symptoms are predicted by early maladaptive schemas. ScientificWorldJournal. 2014;2014:231965. doi: 10.1155/2014/231965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsai, J., Elhai, J. D., Pietrzak, R. H., Hoff, R. A. & Harpaz-Rotem, I. Comparing four competing models of depressive symptomatology: a confirmatory factor analytic study of 986,647 U.S. veterans. J. Affect. Disord. 165, 166–169, (2014) 10.1016/j.jad.2014.04.075. [DOI] [PubMed]
- 40.Bennett BK, et al. Characterization of fatigue states in medicine and psychiatry by structured interview. Psychosom. Med. 2014;76:379–388. doi: 10.1097/psy.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 41.Doyle F, Conroy R, McGee H, Delaney M. Depressive symptoms in persons with acute coronary syndrome: specific symptom scales and prognosis. J. Psychosom. Res. 2010;68:121–130. doi: 10.1016/j.jpsychores.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 42.Olivan-Blazquez B, Rubio-Aranda E, Garcia-Sanz O, Magallon-Botaya R. Correlation between diagnosis of depression and symptoms present in primary care patients. Actas Esp. Psiquiatr. 2016;44:55–63. [PubMed] [Google Scholar]
- 43.Barat P, et al. Inflammatory, endocrine and metabolic correlates of fatigue in obese children. Psychoneuroendocrinology. 2016;74:158–163. doi: 10.1016/j.psyneuen.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 44.Leventhal AM, Ameringer KJ, Osborn E, Zvolensky MJ, Langdon KJ. Anxiety and depressive symptoms and affective patterns of tobacco withdrawal. Drug Alcohol Depend. 2013;133:324–329. doi: 10.1016/j.drugalcdep.2013.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Drijgers RL, et al. The role of the dopaminergic system in mood, motivation and cognition in Parkinson’s disease: a double blind randomized placebo-controlled experimental challenge with pramipexole and methylphenidate. J. Neurol. Sci. 2012;320:121–126. doi: 10.1016/j.jns.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 46.Hannestad J, DellaGioia N, Ortiz N, Pittman B, Bhagwagar Z. Citalopram reduces endotoxin-induced fatigue. Brain Behav. Immun. 2011;25:256–259. doi: 10.1016/j.bbi.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ray Chaudhuri K, et al. Rotigotine and specific non-motor symptoms of Parkinson’s disease: post hoc analysis of RECOVER. Parkinsonism Relat. Disord. 2013;19:660–665. doi: 10.1016/j.parkreldis.2013.02.018. [DOI] [PubMed] [Google Scholar]
- 48.Nakonezny PA, Carmody TJ, Morris DW, Kurian BT, Trivedi MH. Psychometric evaluation of the Snaith-Hamilton pleasure scale in adult outpatients with major depressive disorder. Int. Clin. Psychopharmacol. 2010;25:328–333. doi: 10.1097/YIC.0b013e32833eb5ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 3rd edn (APA, Washington, DC, 1980).
- 50.Herz MI, Endicott J, Spitzer RL. Brief hospitalization: a two-year follow-up. Am. J. Psychiatry. 1977;134:502–507. doi: 10.1176/ajp.134.5.502. [DOI] [PubMed] [Google Scholar]
- 51.Gruber AJ, Hudson JI, Pope HG., Jr The management of treatment-resistant depression in disorders on the interface of psychiatry and medicine. Fibromyalgia, chronic fatigue syndrome, migraine, irritable bowel syndrome, atypical facial pain, and premenstrual dysphoric disorder. Psychiatr. Clin. North Am. 1996;19:351–369. doi: 10.1016/s0193-953x(05)70292-6. [DOI] [PubMed] [Google Scholar]
- 52.Kroenke K, et al. Physical symptoms in primary care. Predictors of psychiatric disorders and functional impairment. Arch. Fam. Med. 1994;3:774–779. doi: 10.1001/archfami.3.9.774. [DOI] [PubMed] [Google Scholar]
- 53.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th edn (APA, Washington, DC, 1994).
- 54.Dantzer R. Cytokine-induced sickness behavior: where do we stand? Brain Behav. Immun. 2001;15:7–24. doi: 10.1006/brbi.2000.0613. [DOI] [PubMed] [Google Scholar]
- 55.Moreau M, et al. Inoculation of Bacillus Calmette-Guerin to mice induces an acute episode of sickness behavior followed by chronic depressive-like behavior. Brain Behav. Immun. 2008;22:1087–1095. doi: 10.1016/j.bbi.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chapman LJ, Chapman JP, Raulin ML. Scales for physical and social anhedonia. J. Abnorm. Psychol. 1976;85:374–382. doi: 10.1037//0021-843x.85.4.374. [DOI] [PubMed] [Google Scholar]
- 57.Rado S. The contribution of psychoanalysis to the medical study of behavior; the Freud Centenary Address. J. Nerv. Ment. Dis. 1956;123:421–427. doi: 10.1097/00005053-195605000-00001. [DOI] [PubMed] [Google Scholar]
- 58.Rado S. On the retransformation of psychoanalysis into a medical science. Compr. Psychiatry. 1962;3:317–329. doi: 10.1016/s0010-440x(62)80001-7. [DOI] [PubMed] [Google Scholar]
- 59.Horan WP, Green MF, Kring AM, Nuechterlein KH. Does anhedonia in schizophrenia reflect faulty memory for subjectively experienced emotions? J. Abnorm Psychol. 2006;115:496–508. doi: 10.1037/0021-843X.115.3.496. [DOI] [PubMed] [Google Scholar]
- 60.Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aguera-Ortiz L, Failde I, Mico JA, Cervilla J, Lopez-Ibor JJ. Pain as a symptom of depression: prevalence and clinical correlates in patients attending psychiatric clinics. J. Affect Disord. 2011;130:106–112. doi: 10.1016/j.jad.2010.10.022. [DOI] [PubMed] [Google Scholar]
- 62.Compton MT, Frank E. Mental health concerns among Canadian physicians: results from the 2007-2008 Canadian Physician Health Study. Compr. Psychiatry. 2011;52:542–547. doi: 10.1016/j.comppsych.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 63.Der-Avakian A, Markou A. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci. 2012;35:68–77. doi: 10.1016/j.tins.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lemke MR, Puhl P, Koethe N, Winkler T. Psychomotor retardation and anhedonia in depression. Acta Psychiatr. Scand. 1999;99:252–256. doi: 10.1111/j.1600-0447.1999.tb07221.x. [DOI] [PubMed] [Google Scholar]
- 65.Aparcio V, Ortega F, Carbonell-Baeza A, Cuevas M, Delgado-Ferndandez M, Jonatan R. Anxiety, depression and fibromyalgia pain and severity. Behav. Psychol. Psicología Conductual. 2013;21:381–392. [Google Scholar]
- 66.Sharpe M, Wilks D. Fatigue. BMJ. 2002;325:480–483. doi: 10.1136/bmj.325.7362.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 68.Chaudhuri, R., Martinez-Martin, P. & Trenkwalder, C. Rotigotine and specific non-motor symptoms of Parkinson’s disease: Post hoc analysis of recover. Parkinsonism Relat. Disord. 19, 660–665, (2013) 10.1016/j.parkreldis.2013.02.018. [DOI] [PubMed]