Abstract
Antiretroviral therapy (ART) adherence is vital for optimal HIV treatment. However, there is limited ART adherence research on the US Latinx population, who are at increased risk for HIV infection and worse HIV health outcomes. This study examined electronically measured ART adherence (Medication Event Monitoring System) and its association with demographic, clinical, neurocognitive, and sociocultural variables in Latinx and non-Latinx white (NLW) persons living with HIV [PLWH (N = 128)]. Latinx participants demonstrated worse adherence than NLW participants (p = 0.04). Linear regressions revealed different predictors of adherence. Among Latinx participants, recent cocaine use, stress, and, unexpectedly, higher US acculturation predicted worse adherence (ps < 0.05). Among NLW participants, recent cocaine use predicted worse adherence (p < 0.05). Intergroup comparisons within the Latinx group were not conducted due to subsample size. Thus, ethnicity, sociocultural variables, and cocaine use are important considerations for ART adherence, and poor ART adherence may be one pathway explaining worse outcomes in Latinx PLWH. Culturally tailored adherence interventions incorporating substance use treatment, acculturation, and stress management are warranted to improve health outcomes.
Keywords: HIV/AIDS, Hispanic/Latinx, health disparities, antiretroviral medication adherence, cognition
Introduction
Latinx adults in the United States are disproportionately affected by health disparities, particularly HIV/AIDS. Latinx adults comprise 18% of the US population,1 but account for ∼25% of new HIV diagnoses per year.2 Further, HIV prevalence in the US Latinx population is expected to grow, comprising up to 32% of HIV cases in the United States by 2045.3 Upon seroconversion, Latinx persons living with HIV (PLWH) also experience worse health outcomes compared with their non-Latinx white (NLW) PLWH counterparts, including earlier mortality and higher rates of comorbidities, such as HIV-induced cognitive and functional impairment also known as HIV-associated neurocognitive disorders.4–11 While the reasons for these worse health outcomes among Latinx PLWH remain poorly understood, an important factor to consider is antiretroviral therapy (ART) adherence.
Optimal ART adherence is necessary for HIV viral suppression and has been associated with higher CD4 count (i.e., immune reconstitution) and decreased rates of hospitalization, opportunistic infections, morbidity, and mortality.12–16 Most research suggests that PLWH should maintain a 90–100% adherence rate for ART to be effective.13,15,16 Suboptimal ART adherence is associated with worse health outcomes, including incidence of multidrug-resistant viral strains, increased morbidity, and higher rates of disease transmission.15,17–19
Among primarily NLW and African American PLWH, worse ART adherence is associated with neurocognitive dysfunction; psychiatric disorders/substance use; psychosocial difficulties (i.e., HIV-related stigma, poor social support, and poor patient/physician relationships); and sociocultural factors [i.e., quality of education, socioeconomic status (SES), acculturation20–25]. Research also suggests a bidirectional relationship between neurocognitive functioning and ART adherence, such that better ART adherence is associated with better neurocognitive functioning and vice versa.21,22,26–28 However, these relationships remain poorly understood in the Latinx PLWH population.
Of the limited research focused on US-based samples of Latinx PLWH, studies suggest that Latinx PLWH may be less adherent to ART, but important methodological and sociocultural considerations warrant attention. In one large-scale study of self-reported adherence,29 several Latinx PLHW subpopulations (i.e., Caribbean, Central American, South American origin) reported lower adherence rates in comparison with NLWs and other racial/ethnic minority groups, but the authors noted that a major limitation of this study was the omission of acculturation data to better understand these findings.
Another important consideration is how adherence is measured—few studies inclusive of Latinx PLWH, of which we are aware, have utilized electronic measures of adherence. The adherence research conducted with Latinx PLWH has primarily relied on self-report measures of ART adherence,30–32 yet research has shown that self-report may overestimate adherence.33 One study that utilized directly observed therapy (DOT) found that Latinx PLWH were significantly more likely to make errors when taking their ART medications than their NLW counterparts, but did not examine sociocultural factors to contextualize these findings.34
Only one study to date that used an electronic measure of ART adherence, Medication Event Monitoring System (MEMS caps),35 also examined the role of sociocultural factors in ART adherence among Latinx PLWH.36 Specifically, Robbins et al. found that better ART adherence was associated with higher acculturation to both majority culture (United States) and “culture of origin” (Latinx), which includes either physical (i.e., birthplace) or family cultural origin. Thus, there is also a need to (1) examine electronically measured ART adherence in this population (i.e., MEMS35) and (2) comprehensively characterize potential predictors of ART adherence.
Similarly, another important limitation in the current literature is the insufficient exploration between sociocultural factors, medication adherence, and neurocognitive functioning. While acculturation is linked to neurocognitive functioning in Latinx PLWH,37 this research does not investigate the relationship between sociocultural factors and ART adherence among Latinx PLWH. Prior research among Latinx clinical populations other than HIV (e.g., those living with diabetes, hypertension, cancer, liver disease) has found that sociocultural factors (e.g., acculturation, language, health literacy) are associated with treatment adherence.38–41 Despite these important findings, no research to date has taken a comprehensive approach to characterizing adherence in Latinx groups while simultaneously measuring other potential contributing factors (e.g., depressive symptomatology, substance use).
In sum, research suggests that Latinx adults experience worse HIV-associated health outcomes and are more likely to have suboptimal ART adherence. This suggests ART adherence may be an important pathway for understanding health disparities experienced by Latinx PLWH, but no study to date has examined these issues while electronically measuring ART adherence. Further, no study to date has utilized a comprehensive biopsychosociocultural theoretical framework42 to assess ART adherence in this population, including consideration of neurocognitive, psychiatric/substance use, psychosocial, and sociocultural factors.
Therefore, the aim of this study was to apply this framework to understand adherence among Latinx PLWH. To that end, we sought to compare rates of electronically measured ART adherence over the course of 30 days and to characterize if and how neurocognitive functioning, psychiatric/substance use, psychosocial, and sociocultural factors contribute to ART adherence in a well-characterized sample of NLW and Latinx PLWH participants. It was hypothesized that:
-
(1)
After accounting for relevant covariates the Latinx group would demonstrate significantly worse, electronically measured ART adherence compared with the NLW group.
-
(2)
Neurocognitive functioning, psychiatric/substance use (i.e., depressive symptomatology and recent substance use based on urine toxicology results), and sociocultural factors (i.e., quality of education, SES, health literacy, medication beliefs, perceived stress) would significantly predict ART adherence in both the Latinx and NLW groups.
-
(3)
Acculturation to US culture and Latinx culture of origin would be significantly positively associated with ART adherence in the Latinx group.
Methods
Participants
A total of 128 PLWH (95 Latinx and 33 NLW participants) participated in the NIMH-funded Medication Adherence Study (K23MH078718; Principal Investigator: M. Rivera Mindt) at the Icahn School of Medicine at Mount Sinai (ISMMS) in New York City. A majority of participants were recruited through community-based outreach and self-referral in Spanish Harlem and the Bronx. Participants were also referred to the study by clinics and related research studies at ISMMS.
Inclusion criteria
All participants were HIV-seropositive (confirmed by medical records), 18–80 years old, self-identified as Latinx (of any race) or NLW, and proficient in English. To ensure familiarity with their medication regimen, only participants who were independently taking their prescribed ART medications in pill form for at least 12 weeks were included in the study.
Exclusion criteria
Participants were excluded if they met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) diagnostic criteria for current or past schizophrenia spectrum and other psychotic or bipolar disorders based on a structured clinical interview (i.e., Composite International Diagnostic Interview43) administered by trained research staff.
Procedures
All participants provided written informed consent. This study was approved by both the ISMMS and Fordham University Institutional Review Boards (IRB). Participants completed two study visits ∼30 days apart.
During the first visit, participants underwent brief neuromedical evaluations (i.e., neuromedical interview, blood draw, urine toxicology), comprehensive neurocognitive and psychiatric/substance use assessments, and demographic and psychosociocultural questionnaires. They were also trained to use the MEMS and were sent home with instructions and an MEMS bottle and cap to use for 30 days. During the second visit, participants returned the MEMS caps for data analysis and completed an MEMS follow-up survey. Participants were compensated for their time.
Neuromedical evaluation
Participants completed a brief neuromedical questionnaire assessing HIV-related medical history, including nadir CD4, viral load, date of HIV diagnosis, current and past medical history, and current medications (including ART). They also underwent a blood draw for CD4 cell count and plasma HIV viral load assays.
Psychiatric/substance use evaluation
Recent depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II total score44). Participants provided a urine sample for toxicology testing for the presence of cocaine and other illicit substances (e.g., heroin, nonprescribed marijuana).
Neurocognitive evaluation
Table 1 summarizes the comprehensive neurocognitive evaluation that participants completed, which assessed seven neurocognitive domains: verbal fluency, executive functioning, processing speed, attention/working memory, learning, memory, and psychomotor functioning. This battery has been well validated for use in HIV/AIDS research.45 Trained psychometrists administered the battery using standardized procedures. A board-certified clinical neuropsychologist (M.R.M.) oversaw all data collection and interpretation.
Table 1.
Neurocognitive Measures and Normative Data Sources
| Neurocognitive domains and tests | Normative data sources |
|---|---|
| Executive function | |
| Wisconsin Card Sorting Task-64 Item Version | Kongs et al. (2000)91 |
| Trail Making Test (Part B) | Heaton et al. (2004)92 |
| Attention/working memory | |
| WAIS-III Letter Number Sequencing | Heaton et al. (2003)93 |
| PASAT Total Correct | Heaton et al. (2004)92 |
| Learning, memory | |
| Hopkins Verbal Learning Test-Revised (Total Recall; Delayed Recall) | Benedict et al. (1998)94 |
| Brief Visuospatial Memory Test-Revised (Total Recall; Delayed Recall) | Benedict (1997)95 |
| Motor function | |
| Grooved Pegboard Time (dominant and nondominant hand) | Heaton et al. (2004)92 |
| Processing speed | |
| WAIS-III Digit Symbol | Heaton et al. (2003)93 |
| WAIS-III Symbol Search | Heaton et al. (2003)93 |
| Trail Making Test (Part A) | Heaton et al. (2003)93 |
| Verbal fluency | |
| Controlled Oral Word Association Test (F-A-S; Animals) | Heaton et al. (2004)92 |
Consistent with empirically supported methods, raw neurocognitive test scores were transformed into demographically corrected T-scores using the best available published normative data (see Table 1).6,46 The T-scores of the individual tests in each domain were averaged to create neurocognitive mean domain T-scores, and all individual test T-scores were averaged to create the Global Neurocognitive Average T-score, which reflects global neurocognitive functioning. Consistent with prior literature, Global Neurocognitive and Neurocognitive Domain Average T-scores less than 40 were considered impaired.47
Demographic, psychosocial, and sociocultural evaluation
Demographics
The demographic questionnaire assessed age, years of education, gender, race/ethnicity, employment status, SES, housing status, and language use.
Quality of education
Quality of education was measured using the Wechsler Test of Adult Reading (WTAR). The WTAR is a test of single-word reading that was developed as a measure of estimated premorbid functioning. Single-word reading tests, including the WTAR, have been validated as a measure of the quality of education.48–50 The WTAR has well-established reliability and validity.51 The WTAR Standard Score was used in all analyses.
Acculturation
The Abbreviated Multidimensional Acculturation Scale (AMAS52) is a self-report, bidirectional measure that assesses acculturation levels to both majority culture (United States) and culture of origin (Latinx). It includes six subscales (three for each culture) related to language competence, cultural competency, and cultural identity, producing two summary scores: (1) Total US Acculturation Score and (2) Total Latinx Acculturation Score (scores range from 1 to 4; higher scores indicate higher acculturation levels). The AMAS has excellent psychometric characteristics and has been validated with the urban populations of PLWH similar to the current sample.53 For this study, the AMAS Total US Acculturation and Total Latinx Acculturation Scores were used.
Socioeconomic status
Information about participants' educational and occupational history was obtained through a demographic questionnaire. SES was estimated using the Hollingshead Index of Social Prestige (ISP) score, which was calculated based on a weighted sum of the participant's educational level and occupational rank54 and is among the most commonly used SES measures in the literature.55 For a more detailed description of the Hollingshead ISP calculation in this sample, see Arentoft et al.56
Health literacy
The Test of Functional Health Literacy (TOFHLA) objectively measures comprehension of health-related materials, testing reading comprehension and arithmetic ability.57 There are three separate factors (literacy for prose passages, literacy for appointment slips, documents, and prescription bottle directions, and quantitative numeracy), from which a total score is computed. The TOFHLA has good psychometric properties and is frequently used to measure health literacy,58 particularly in HIV+ populations.58–62 The TOFHLA total score was used for this study.
Medication beliefs
The Beliefs Related to Medications Survey (BERMA) is a 53-item self-report measure that assesses efficacy-related beliefs regarding medications, which may play a vital role in medication adherence.63 Prior research supports the psychometric properties of the BERMA.64 The three BERMA subscale scores were used: Medication Management Efficacy, Dealing with Health Professionals, and Attitudes About Medications.
Perceived stress
The Perceived Stress Scale-10 (PSS) is a 10-item self-report questionnaire that measures an individual's appraisal of stressful situations.65,66 The measure has well-established psychometric properties with both NLW and Latinx populations.67 The PSS total score was used in this study.
Medication adherence evaluation
The Medication Event Monitoring System (MEMS68) was used to electronically measure adherence to HIV medications. At the first study visit, participants were given an MEMS medication bottle and cap containing a microchip to record the date and time of every bottle opening. MEMS is a well-validated measure of ART adherence in HIV.21,69–72
Participants used the MEMS to track one of their ART medications—either their protease inhibitor or their most frequently dosed nonprotease inhibitor. Participants were trained to use the MEMS as described by Bova et al.73 Specifically, they were informed about the microchip recorder, instructed to only remove the designated dose at each opening, and told not to remove more than one dose of medication at a time (“pocket dosing”). Finally, they were trained to open and close the pill bottle properly so that the recording device was activated. Study staff transferred the selected ART medication into the MEMS bottle and taught participants to do this on their own, in case a medication refill occurred during the monitoring period. After training, the MEMS caps monitored participants' ART adherence for at least 30 days.
At the second study visit, conducted at least 30 days later, participants returned their MEMS device and completed a brief MEMS follow-up interview to ensure that it was used correctly during the monitoring period. MEMS data were then downloaded and analyzed. Each participant's overall adherence rate was calculated as the number of monitored doses taken during the 30-day monitoring period (subtracting any “pocket doses” or extra container openings reported by the participant during the MEMS follow-up interview) divided by the number of doses prescribed during that period. The dependent variable for the study analyses was the Total Adherence Score. In addition, we utilized the visual analog scale as a self-report measure of ART adherence. While this was not our measure of adherence for hypothesis testing, it was included to examine the association between self-report and electronic measurement of ART adherence.68
Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics Version 24. Most variables met homogeneity of variance assumptions and were normally distributed; variables that did not meet assumptions were analyzed using nonparametric tests or transformed as recommended by Field.74 Plasma HIV viral loads were significantly positively skewed, and these variables were logarithmically transformed. In addition, as expected, medication adherence was significantly negatively skewed. When possible, nonparametric analyses (i.e., Spearman's correlations) were used to account for this. In all multivariable analyses utilizing parametric analyses [i.e., partial correlations, analysis of variance (ANCOVA), linear regressions], we transformed the Total Adherence Score variable by applying reverse (i.e., subtracting each score from 1+ the highest score obtained) and square root transformations.75,76
Categorical variables were examined using chi-square. Independent-samples t-tests, Mann–Whitney U-tests, and ANCOVA were used to analyze group differences on continuous variables. Spearman's correlations were used to examine linear relationships between adherence and other variables, and linear regressions were used to compute overall models. In addition, covariates (i.e., age, education) were added to relevant analyses if a demographic variable demonstrated between-group ethnic differences and/or was related to the dependent variable. For instance, the WTAR was used as a covariate in the between-group ethnic comparisons of neurocognitive functioning, as measures of quality of education and literacy, such as the WTAR, are known to be significantly associated with neurocognitive test performance.48–50
Results
Sample overview
Overall, 46.5% of the sample was monitored on a single-pill combination ART, and the remaining 53.5% were monitored on either a protease inhibitor or their most frequently dosed nonprotease inhibitor. The sample's total adherence ranged from 9% to 100% {M = 83% (SD = 21.70); Mdn = 90.6% [interquartile range (IQR) = 17%]}. Less than half of the sample was adherent at the 90%+ rate (47.4%). Table 2 illustrates the demographic (i.e., age, education, gender), clinical (i.e., HIV, psychiatric, substance use), neurocognitive (i.e., average neurocognitive T-scores), and sociocultural (i.e., quality of education, SES, health literacy, medication beliefs, perceived stress) characteristics of the study sample. Herein we highlight the characteristics of the overall sample, between-group differences for the Latinx and NLW groups, and key bivariate correlations between the HIV-specific clinical and adherence variables to assess the validity of our adherence measure.
Table 2.
Demographic, Clinical, Neurocognitive, and Sociocultural Variables for the Study Sample and by Ethnicity
| |
All participants (N = 128) |
Latinx (n = 95) |
Non-Hispanic white (n = 33) |
|
|
|||
|---|---|---|---|---|---|---|---|---|
| Demographic and clinical variables | M or % | SD | M or % | SD | M or % | SD | t or X2 | p |
| Age (years) | 47.01 | 8.17 | 45.93 | 7.35 | 50.12 | 9.62 | 2.60 | 0.01* |
| Education (years) | 12.68 | 2.72 | 12.08 | 2.39 | 14.39 | 2.92 | 2.39 | <0.01** |
| Gender (% female) | 31% | 35% | 18% | 3.17 | 0.08 | |||
| Toxicology (positive for cocaine) | 15% | 14% | 19% | 0.52 | 0.47 | |||
| Mdn | IQR | Mdn | IQR | Mdn | IQR | U | p | |
| HIV duration (years) | 17.00 | 7.25 | 16.00 | 6.75 | 20.00 | 5.25 | 224.00 | 0.05 |
| Nadir CD4 count | 167.0 | 208.0 | 176.5 | 254.8 | 164.0 | 131.0 | 1065.50 | 0.93 |
| CD4 count | 466.5 | 432.0 | 444.0 | 437.0 | 625.0 | 558.5 | 1122.00 | 0.04* |
| Plasma HIV viral loada | 1.41 | 0.90 | 1.67 | 1.29 | 1.38 | 0.29 | 1885.00 | <0.01** |
| BDI-II total score | 9.00 | 14.00 | 9.00 | 13.00 | 10.00 | 15.00 | 1244.0 | 0.11 |
| Neurocognitive T-scores | M | SD | M | SD | M | SD | T | p |
| Global | 41.62 | 7.35 | 40.98 | 7.35 | 43.44 | 7.14 | 1.64 | 0.10 |
| Executive functioning | 43.80 | 9.81 | 43.09 | 8.60 | 44.44 | 12.72 | 0.62 | 0.54 |
| Attention/working memory | 42.58 | 8.84 | 42.84 | 8.23 | 41.90 | 10.38 | 0.52 | 0.60 |
| Learningb | 36.49 | 12.10 | 34.56 | 11.11 | 41.86 | 13.26 | 0.69 | 0.49 |
| Memoryb | 37.26 | 12.67 | 35.48 | 11.74 | 42.22 | 14.01 | 0.43 | 0.66 |
| Motor function | 41.70 | 10.22 | 42.48 | 10.60 | 39.50 | 8.84 | 0.98 | 0.17 |
| Processing speed | 45.80 | 9.06 | 45.31 | 9.37 | 47.20 | 8.08 | 1.01 | 0.31 |
| Verbal fluencyb | 44.61 | 11.34 | 43.24 | 11.51 | 48.50 | 10.05 | 0.12 | 0.90 |
| Sociocultural variables | M | SD | M | SD | M | SD | T | p |
| Hollingshead ISP | 37.37 | 13.36 | 33.90 | 11.59 | 47.12 | 13.34 | 0.45 | <0.01** |
| WTAR Standard Score | 90.50 | 17.54 | 85.97 | 15.31 | 103.81 | 17.11 | 0.98 | <0.01** |
| AMAS | ||||||||
| Total US Acculturation | n/a | n/a | 3.38 | 0.48 | n/a | n/a | n/a | n/a |
| Total Latinx Acculturation | n/a | n/a | 3.14 | 0.55 | n/a | n/a | n/a | n/a |
| TOFHLA totalc | 86.41 | 10.61 | 84.44 | 11.45 | 91.93 | 4.53 | 711.50 | <0.01** |
| BERMA | ||||||||
| Health Professional | 81.98 | 15.84 | 81.11 | 16.51 | 84.39 | 13.75 | 3.24 | 0.31 |
| Memory for Medications | 93.49 | 15.42 | 93.71 | 15.86 | 92.84 | 14.32 | 2.41 | 0.79 |
| Attitudes About Medications | 37.58 | 6.20 | 37.67 | 6.30 | 37.31 | 5.98 | 0.41 | 0.78 |
| PSS total | 15.70 | 6.38 | 15.14 | 6.38 | 17.35 | 6.24 | 0.12 | 0.15 |
log10 transformed.
t-ratios for ethnicity based on comparisons for neurocognitive scores utilizing analysis of variance with Wechsler Test of Adult Reading as covariate.
Mann–Whitney U due to skewness of variable.
p < 0.05.
p < 0.01.
AMAS, Abbreviated Multidimensional Acculturation Scale; BDI-II, Beck Depression Inventory-II; BERMA, Beliefs Related To Medications; IQR, interquartile range; ISP, Index of Social Prestige; PSS, Perceived Stress Scale; TOFHLA, Test of Functional Health Literacy; WTAR, Wechsler Test of Adult Reading.
Demographic characteristics
On average, the sample was middle-aged and had approximately a high school level of education. The sample was primarily male and Latinx. Compared with the NLW group, the Latinx group was significantly younger and completed significantly fewer years of education (all ps < 0.01), and these variables were included as covariates in the between-group comparison of adherence. In addition, within the Latinx group, 81% identified as Caribbean (75% Puerto Rican, 5% Dominican, and 1% Cuban), 7% as Mexican, 7% as Central American, 4% as South American, and 1% as “Other Latinx subpopulation.”
Clinical characteristics
Participants had been diagnosed with HIV for a median of 17 years (IQR = 7.00) and 11% of the sample was immunosuppressed (based on current CD4 count <200). The Latinx group had significantly lower current CD4 count and higher current plasma HIV viral load compared with the NLW group (all ps < 0.05). However, the two groups did not significantly differ on nadir CD4 count (p > 0.10). In terms of psychiatric characteristics, average depressive symptomology (based on the BDI-II) fell within normal limits, and there were no ethnic group differences. Regarding recent substance use, the most prevalent recently used substances were tetrahydrocannabinol (THC) (30.5%), cocaine (14.1%), benzodiazepines (7.8%), and opiates (6.3%), as measured by urine toxicology. There were no ethnic group differences, with the exception of recent opiate use, in which NLW participants demonstrated greater recent use of opiates (p < 0.05).
Neurocognitive characteristics
Within the entire sample, average neurocognitive functioning fell within normal limits for global functioning and all domains, with the exception of learning and memory. Impairments in these areas appeared to be driven by learning and memory impairments in the Latinx group. There were no significant differences between the Latinx and NLW participants in the global or other neurocognitive domains after accounting for effects of quality of education (WTAR; all ps > 0.05).
Sociocultural characteristics
As illustrated in Table 2, compared with NLW participants, Latinx participants had significantly lower SES (i.e., Hollingshead ISP; p < 0.05), quality of education (i.e., WTAR; p < 0.01), and health literacy (i.e., TOFHLA total score, p < 0.01). There were no significant group differences in beliefs about medications (i.e., BERMA subscale scores) or perceived stress (i.e., PSS total score; all ps > 0.05). Within the Latinx sample, average US and Latinx acculturation scores fell in the high range suggesting that the Latinx sample was highly acculturated to both cultures and essentially bicultural.
Demographic, clinical, and sociocultural variables
Entire study sample analyses
As noted in Table 3, across the entire sample, we examined the relationship between urine toxicology test results and total adherence rates, and participants who tested positive for recent cocaine use had significantly lower adherence rates than those who tested negative for recent cocaine use (U = 539.00, p < 0.01). No significant differences were observed between those who tested positive or negative for recent use of any other illicit substances (all ps > 0.10).
Table 3.
Nonparametric Correlations and Mann–Whitney U-Tests Examining Total Adherence and Demographic, Clinical, and Sociocultural Variables for the Entire Study Sample and by Ethnic Group
| |
All participants (N = 128) |
Latinx (n = 95) |
Non-Hispanic white (n = 33) |
|||
|---|---|---|---|---|---|---|
| Demographic and clinical variables | rs | p | rs | P | rs | p |
| Age (years) | 0.10 | 0.24 | 0.06 | 0.59 | 0.17 | 0.34 |
| Education total (years) | −0.06 | 0.54 | −0.11 | 0.28 | −0.16 | 0.38 |
| BDI-II total score | −0.04 | 0.69 | −0.02 | 0.89 | −0.19 | 0.29 |
| U | p | U | p | U | p | |
| Gender | 1977.50 | 0.21 | 186.00 | 0.20 | 97.00 | 0.48 |
| Recent cocaine use | 539.00 | <0.01* | 284.00 | 0.03* | 32.50 | 0.03* |
| Sociocultural variables | rs | p | rs | p | rs | p |
| Hollingshead ISP | −0.04 | 0.67 | −0.16 | 0.14 | 0.01 | 0.94 |
| WTAR Standard Score | −0.05 | 0.59 | −0.14 | 0.19 | 0.07 | 0.69 |
| AMAS | ||||||
| Total US Acculturation | n/a | n/a | −0.32 | <0.01** | n/a | n/a |
| Total Latinx Acculturation | n/a | n/a | −0.17 | 0.11 | n/a | n/a |
| TOFHLA total score | <−0.01 | 0.98 | −0.10 | 0.38 | 0.26 | 0.17 |
| BERMA | ||||||
| Health Professional | 0.18 | 0.04* | 0.11 | 0.31 | 0.39 | 0.03* |
| Memory for Medications | 0.03 | 0.76 | 0.10 | 0.36 | −0.21 | 0.25 |
| Attitudes About Medications | 0.05 | 0.55 | −0.01 | 0.92 | 0.30 | 0.10 |
| PSS total score | −0.11 | 0.32 | −0.25 | 0.04* | 0.39 | 0.07 |
p < 0.05.
p < 0.01.
AMAS, Abbreviated Multidimensional Acculturation Scale; BDI-II, Beck Depression Inventory-II; BERMA, Beliefs Related To Medications; ISP, Index of Social Prestige; PSS, Perceived Stress Scale; TOFHLA, Test of Functional Health Literacy; WTAR, Wechsler Test of Adult Reading.
We then examined associations between adherence and other study variables. These results revealed that higher adherence was also significantly positively correlated with greater perceived capacity for dealing with health professionals (BERMA-Health Professional subscale; rs = 0.18, p = 0.04). No other significant associations were observed between adherence and demographic, clinical, or any other sociocultural variables (all ps > 0.05). Thus, cocaine use and the BERMA-Health Professional subscale were added as covariates for the between-group comparison of adherence.
To examine the validity of our adherence measurement, we examined the correlations between our adherence measure (Total Adherence Score) and HIV clinical indices. The results revealed that higher adherence was positively correlated with current CD4 count (rs = 0.27, p < 0.01) and negatively correlated with current HIV viral load level (rs = −0.20, p = 0.03). Of note, our electronically measured adherence variable was also positively correlated with self-reported adherence (rs = 0.61, p < 0.01). The correlation between CD4 count and adherence was not significantly different between the Latinx group and the NLW group (Fisher's Z = 0.41, p > 0.05). However, the correlation between HIV viral load and adherence was significantly greater in the NLW group (rs = −0.67, p < 0.01) than in the Latinx group (rs = −0.23, p < 0.05; Fisher's Z = 2.67, p < 0.01).
Between-group ethnic comparisons
For descriptive purposes, Fig. 1 provides an overview of the mean adherence rates for the two groups, which indicated a small-to-medium effect size. To test the first hypothesis regarding ethnic differences in ART adherence, ANCOVA was computed to assess whether there was a significant difference between ethnic groups on total adherence after accounting for relevant covariates (i.e., age, education, recent cocaine use, and BERMA Health Professional subscale).
FIG. 1.
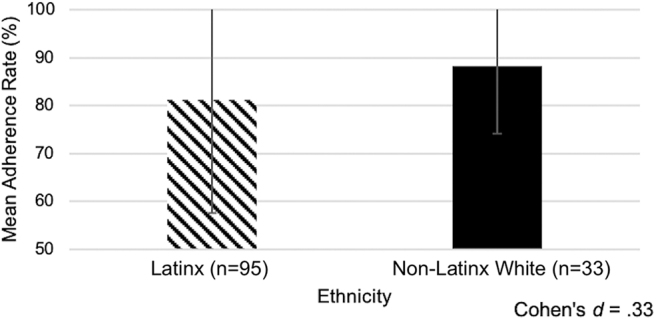
There was a significant effect of ethnicity on adherence rate. The Latinx group had significantly lower total adherence compared with the non-Latinx white group.
The results revealed that the model was significant (F(5,112) = 4.63, p < 0.001) and there was significant effect for ethnicity such that the Latinx group had significantly lower total adherence compared with the NLW group (F(1,112) = 4.21, p = 0.04). Next, the relationships between adherence with demographic and clinical characteristics within each of the ethnic groups were examined using separate bivariate correlations to test the second and third hypotheses.
Within-group Latinx analyses
As Table 3 illustrates, Latinx participants who tested positive for recent cocaine use had significantly lower adherence rates (Mdn = 80.55) than Latinx participants who tested negative (Mdn = 90.32; p < 0.05). Within the Latinx group, total adherence was significantly negatively correlated with US acculturation (i.e., AMAS Total US Acculturation) and self-reported stress (i.e., PSS total), such that better adherence was associated with lower US acculturation and self-reported stress (all ps < 0.05). Adherence was not significantly related to any other demographic, clinical, or sociocultural characteristic in this group (all ps > 0.05). In addition, within-group comparisons of adherence based on the country of origin were not computed due to the small sample sizes in all of the Latinx subgroups with the exception of the Puerto Rican group.
Within-group NLW analyses
As noted in Table 3, NLW participants who tested positive for recent cocaine use also had significantly lower adherence rates (Mdn = 82.06) than NLW participants who tested negative (Mdn = 93.74; p < 0.05). Within the NLW group, total adherence was significantly positively correlated with the BERMA “Dealing with Health Professionals” subscale (p = 0.03). Total adherence was not significantly related to any other demographic, clinical, or sociocultural characteristics in this group (all ps > 0.05).
Neurocognitive variables
A series of partial correlations were computed to examine the association between neurocognitive function and total adherence. Given the potential impact on neurocognitive test performance and its association with adherence, cocaine use was included as an additional covariate in the following analyses. In the Latinx group, the results revealed that total adherence was not significantly associated with any Neurocognitive Domain or the Global Neurocognitive Average T-scores (rs = 0.04–0.17; all ps > 0.10). In the NLW group, the results revealed that total adherence was significantly associated with the neurocognitive domains of Attention/Working Memory, Learning, and Memory (rs = 0.38–0.45; all ps < 0.05), such that better neurocognitive functioning was associated with better adherence. However, no other significant associations were observed with the Global or other neurocognitive domains (all ps > 0.10).
Multivariable models predicting adherence
Lastly, linear regressions were computed to examine the relationship between clinical, neurocognitive, and sociocultural variables with total adherence. Because significant predictors of adherence differed across ethnic groups, separate regression models were computed for the Latinx and NLW groups. Variables that were significantly associated with adherence, in the analyses above, were entered into each respective model.
For the Latinx group, recent cocaine use, AMAS Total US Acculturation score, and perceived stress (i.e., PSS score) were entered into the model. The results revealed that this model significantly accounted for 25.7% of the variance in adherence scores (F(3, 61) = 7.04, p < 0.001), and the results showed that all three variables significantly contributed to the model: recent cocaine use (B = 1.75, SE = 0.079, p = 0.03), AMAS Total US Acculturation (B = 0.25, SE = 0.08, p < 0.01), and perceived stress (B = 0.10, SE = 0.04, p = 0.03) were significant predictors of adherence. Overall, lack of recent cocaine use, lower US acculturation, and lower perceived stress predicted better adherence in the Latinx group.
For the NLW group, recent cocaine use, Attention/Working Memory, Learning, and Memory Domain T-scores, and BERMA-Health Professional subscale were entered into the model. The results revealed that this model significantly accounted for 49% of the variance in adherence (F(5, 31) = 5.09, p < 0.001), and the results showed that only recent cocaine use (B = 2.68, SE = 0.64, p < 0.001) was a significant predictor of adherence. Thus, lack of recent cocaine use predicted better adherence in the NLW group.
Discussion
This study sought to identify potential ethnic disparities in electronically measured ART adherence over a 1-month period and apply a biopsychosociocultural framework to understand how neurocognitive (e.g., learning, memory), sociocultural (i.e., acculturation, medication and health beliefs, perceived stress, SES, health literacy), and other factors (i.e., depressive symptomatology, cocaine use) relate to adherence in Latinx and NLW PLWH. The results revealed important ethnic differences in ART adherence, such that the Latinx PLWH demonstrated significantly worse adherence than the NLW PLWH. In general, predictors of adherence differed between the two ethnic groups, with one exception. In the Latinx group, sociocultural factors (i.e., lower US acculturation, lower perceived stress) predicted better adherence. In the NLW group, better neurocognitive functioning (i.e., learning, memory, attention/working memory) and only one sociocultural factor (better ability to deal with health professionals) predicted better adherence. However, recent cocaine use was a robust predictor of adherence for both groups, such that recent cocaine use at the baseline visit (as measured with urine toxicology) predicted worse adherence in the subsequent 30-day period.
Our finding that the Latinx group had significantly worse ART adherence compared with the NLW group extends the prior literature in important ways. First, this study supports the validity of prior studies that used self-report measures.29–32,53 Second, the current findings extend the Arnsten et al.34 DOT findings on the increased risk for medication errors in Latinx PLWH by providing sociocultural data to better contextualize adherence behaviors in this population. Together, these converging findings suggest that ethnic disparities in adherence exist and Latinx PLWH are at increased risk for worse HIV health outcomes compared with NLW PLWH.
In fact, the current study results revealed that the Latinx group demonstrated significantly worse HIV-related clinical outcomes. Specifically, the Latinx group had significantly lower CD4 count and higher HIV viral load compared with the NLW group, suggesting greater disease progression and worse control of HIV viremia. While causal inferences cannot be made, worse ART adherence may be linked to the HIV-related health disparities (e.g., opportunistic infections, neuropathy, mortality, morbidity) observed in the Latinx PLWH population.
Further, the relationship between HIV viral load and total adherence was significantly stronger in the NLW group than the Latinx group, suggesting that ethnicity may modify the association between medication adherence and HIV viral load. Subsequently, understanding the underpinnings of adherence in this population at a granular level is imperative to effectively improve adherence and reduce HIV health disparities revealed in this and prior studies.4–11,29–32,34 To that end, a series of within-group analyses were conducted to better understand adherence in each ethnic group. Based on these results, a somewhat differential pattern of predictors of adherence emerged for the two groups.
In the Latinx group, two sociocultural factors (acculturation and perceived stress) and cocaine toxicology (discussed below) predicted adherence within our multivariate model. Contrary to our hypothesis and prior research, the current results showed that lower US acculturation was associated with better adherence. This was unexpected given that Robbins et al.36 found that higher US acculturation was related to better adherence in a similar sample of PLWH. However, different measures of acculturation were used in the two studies, the AMAS53 in the current study and the Bicultural Scale for Puerto Ricans in the Robbins et al.36 study. The current results may be consistent with “negative acculturation” theory, which suggests that acculturation to the majority-dominant US culture involves greater adoption of American values, which can include behaviors that adversely affect health.77,78 Research has shown that among Latinx individuals, higher levels of US acculturation are associated with poorer nutrition and dietary habits, worse perinatal outcomes (including low birth weight and prematurity), and increased substance use (particularly alcohol and nicotine use).79 Therefore, the relationship between acculturation and adherence in this sample may suggest adoption of attitudes or behaviors from the majority culture that directly or indirectly reduce ART adherence.
In addition, lower perceived stress was also associated with better adherence in the Latinx group. This is consistent with prior studies reporting that stressors are associated with lower medication adherence, among other health outcomes.80,81 The current findings provide support for a culturally tailored approach to adherence interventions that emphasizes the importance of medication adherence and highlight stress management as a potentially modifiable factor to improve adherence in this population.
It is also notable that within the Latinx group, neurocognitive functioning was not significantly associated with ART adherence. This finding was unexpected given the literature suggesting otherwise in NLW and African American populations.21,22,27,28 However, given the fact that psychometrically sound normative data are generally available for neurocognitive tests for NLW and African American populations compared with the US-dwelling Latinx population, it is possible that normative data could have impacted the current results.
In the NLW group, bivariate analyses revealed that better neurocognitive functioning in learning, memory, attention/working memory, better ability to deal with health professionals, and lack of recent cocaine use predicted better adherence. However, the results of a multivariable analysis with all three of these variables included in the model revealed that only recent cocaine use significantly contributed to the model.
For both ethnic groups, cocaine use was significantly related to adherence such that recent cocaine use at the baseline visit predicted worse adherence in the subsequent 30 days. This is consistent with prior research showing that active substance use, particularly recent stimulant use, is associated with lower ART adherence in PLWH.82 Studies have also shown that cocaine users had the lowest adherence rates,83 and that the relationship between poor neurocognitive performance and lower medication adherence rates was partially mediated by cocaine use.84 Thus, the current findings and prior literature suggest that assessment and treatment of substance use, and particularly cocaine use, should be an integral part of interventions to improve adherence in both Latinx and NLW PLWH.
Study strengths and limitations
The current study has several strengths that warrant consideration. This is the first large-scale study to focus on ART adherence in Latinx PLWH using MEMS, an electronic measure of adherence. Second, this is the first study to apply a comprehensive biopsychosociocultural theoretical framework to adherence in Latinx and NLW PLWH and utilized well-validated measures for all aspects of assessment. Further, by evaluating the relative importance of several predictors, such as acculturation and perceived stress, this work suggests that sociocultural factors, which are infrequently assessed in the literature, may play a more important role in adherence among Latinx individuals than the factors that are traditionally measured. Third, the sociocultural characteristics of the Latinx group were well characterized; the US Latinx population is highly heterogeneous, and including this information makes it clear for whom these findings are most generalizable (i.e., Latinx from Caribbean backgrounds). Fourth and finally, this study is of high clinical significance given that (1) the majority of Latinx participants were recruited from Spanish Harlem and the Bronx, areas with some of the highest rates of HIV infection and Latinx health disparities in the United States,85,86 and (2) compared with other US-dwelling Latinx subpopulations (e.g., Mexican, Cuban), Puerto Ricans are at the greatest risk for HIV and experience worse HIV-related health outcomes.7,87
Despite these study strengths, a number of study limitations also merit discussion. The NLW subsample was relatively small (n = 33), and this may have limited power for related within-group analyses. However, despite this limitation, the within-group linear regression analysis in this subsample still accounted for almost half of the variance in ART adherence.
Given the geographic location of the study and sample composition, the current findings may not be generalizable to suburban or rural populations, or other Latinx subpopulations. The study sample comes from an urban area (New York City) and the rate of optimal ART adherence was low, with only one-third of the sample demonstrating optimal adherence (90% ± adherence rate). Consistent with New York City demographics (particularly in Spanish Harlem and the Bronx, where the majority of study recruitment occurred), 81% of the Latinx group was Caribbean with the majority being Puerto Rican (75%), fluent in English, and highly acculturated to both US and Latinx cultures (or bicultural).88 The Latinx group was also younger, had fewer years of education, and had lower literacy, health literacy, and SES compared with the NLW group. However, none of these factors was related to adherence in this study. Finally, HIV-1 RNA was drawn at only the first study visit. The absence of a follow-up HIV-1 RNA assessment precluded objective measurement of adherence through laboratory indicators.
Future research is needed to replicate the current findings with larger sample sizes and within different geographic regions (suburban, rural) and Latinx subpopulations. Future investigations should also include sociocultural measures, such as acculturation. Closer examination of potential barriers to adherence in Latinx PLWH is needed. Given that recent cocaine use was the only variable to significantly predict adherence in both Latinx and NLW participants, further research is needed to better understand how substance use and treatment can impact adherence interventions. Moreover, given the potential explanation of the “negative acculturation” theory, determining how stress may be related to acculturation, and how substance use may be related to acculturative stress (or adapting to US majority culture) is also an essential next step. Last, future research should investigate culturally tailored interventions to improve adherence in Latinx PLWH.
It is also important to note that the US Latinx population is heterogeneous and includes a variety of subpopulations (e.g., Caribbean, Mexican, Central American groups). These subpopulations have origins in countries with unique cultural characteristics that may be important to studies of adherence. In our study, the largest Latinx groups originated from Caribbean countries and included those who identify as Puerto Rican, Dominican, or Cuban. However, given that 75% of our Latinx sample identified as Puerto Rican, with much smaller percentages of other Latinx groups, we were not able to make within-group comparisons.
Future research should examine how these factors may differ across Latinx subgroups, particularly the relationship between acculturation and adherence. Prior research has found that compared with HIV+ Latinx adults in the United States, HIV+ Latinx adults born in Cuba and Puerto Rico were less likely to be connected to care within 3 months of diagnosis. Moreover, HIV+ Latinx adults who resided in neighborhoods with less than 25% Latinx were less likely to be connected to HIV care.89 Thus, country of birth and neighborhood characteristics should also be considered when examining medication adherence and medical care engagement among HIV+ Latinx adults.89
Finally, it is important to acknowledge the role of structural marginalization in perpetuating health disparities, such as those observed in HIV outcomes. Structural marginalization stems from the uneven institutional distribution of benefits and burdens to different groups of people. This marginalization extends to a wide range of social identities, such as race, ethnicity, gender, class, sexual orientation, HIV status, and SES.90 Importantly, many of our participants have multiple marginalized social identities, which impacts not only their access to care but also treatment in health care systems at large. The consequences of systemic marginalization extend to health care behaviors, including medication adherence, and can go on to further perpetuate health disparities. This merits further investigation.
The present study results revealed important disparities in ART adherence and HIV-health outcomes such that Latinx PLWH demonstrated significantly worse adherence, immune function, and HIV viral suppression compared with their NLW counterparts. These disparities have immense social, economic, and public health implications in terms of risk for HIV transmission, opportunistic infections, mortality, and morbidity.
This study provides an initial step toward a better understanding of how cocaine use and sociocultural factors impact health behaviors, such as ART adherence, in a particularly vulnerable population through a comprehensive biopsychosociocultural framework. These findings suggest that poor ART adherence may be one pathway to worse HIV-health outcomes in Latinx PLWH. Culturally tailored adherence interventions that consider acculturation, substance use assessment/treatment, and stress management are warranted to improve outcomes and health equity.
Acknowledgments
The authors thank Drs. Susan Morgello (MHBB PI), Ana Abraído-Lanza, Julia Arnsten, Charles Hinkin, and Jane Simoni for their support of this project, and the participants. They would also like to thank the following research team members and community-based organizations for ensuring the success of this project: Erica D'Aquila, Ana Rosario, and Maria Pizzirusso, and Drs. Armando Fuentes, Caitlin Miranda, Jennifer Monzones, Kaori Kubo Germano, Kelly Coulehan, and Diane Scheiner as well as the Harlem Community Academic Partnership and the Manhatten HIV Care Network.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The authors would like to thank the Manhattan HIV Brain Bank (MHBB; Grant no.: U24MH100931). This research was supported by K23MH07971801 from the National Institutes of Health. MJS was supported by NSF award GRFP-G30328. AA was supported by NIH award SC2 MH118473. RNR was supported by NIH award P30 MH043520 (PI: Remien).
References
- 1. United States Census Bureau. QuickFacts. 2018. Available at: https://www.census.gov/quickfacts/fact/table/US/PST045218 (Last accessed December27, 2018).
- 2. Centers for Disease Control and Prevention (CDC). CDC Fact Sheet: HIV among Latinos. 2017. Available at: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/cdc-hiv-latinos-508.pdf (Last accessed October10, 2017).
- 3. Hood JE, Golden MR, Hughes JP, et al. . Projected demographic composition of the United States population of people living with diagnosed HIV. AIDS Care 2017;29:1543–1550 [DOI] [PubMed] [Google Scholar]
- 4. Cargill VA, Stone VE. HIV/AIDS: A minority health issue. Med Clin North Am 2005;89:895–912 [DOI] [PubMed] [Google Scholar]
- 5. Gonzalez JS, Hendriksen ES, Collins EM, et al. . Latinos and HIV/AIDS: Examining factors related to disparity and identifying opportunities for psychosocial intervention research. AIDS Behav 2009;13:582–602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heaton RK, Franklin DR Jr., Deutsch R, et al. . Neurocognitive change in the era of HIV combination antiretroviral therapy: The longitudinal CHARTER study. Clin Infect Dis 2015;60:473–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marquine MJ, Heaton A, Johnson N, et al. . Differences in neurocognitive impairment among HIV-infected latinos in the United States. J Int Neuropsychol Soc 2018;24:163–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McGinnis KA, Fine MJ, Sharma RK, et al. . Understanding racial disparities in HIV using data from the veterans aging cohort 3-site study and VA administrative data. Am J Public Health 2003;93:1728–1733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morgello S, Mahboob R, Yakoushina T, et al. . Autopsy findings in a human immunodeficiency virus-infected population over 2 decades: Influences of gender, ethnicity, risk factors, and time. Arch Pathol Lab Med 2002;126:182–190 [DOI] [PubMed] [Google Scholar]
- 10. Robinson-Papp J, Gelman BB, Grant I, et al. . Substance abuse increases the risk of neuropathy in an HIV-infected cohort. Muscle Nerve 2012;45:471–476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wojna V, Skolasky RL, Hechavarria R, et al. . Prevalence of human immunodeficiency virus-associated cognitive impairment in a group of Hispanic women at risk for neurological impairment. J Neurovirol 2006;12:356–364 [DOI] [PubMed] [Google Scholar]
- 12. Genberg BL, Wilson IB, Bangsberg DR, et al. . Patterns of antiretroviral therapy adherence and impact on HIV RNA among patients in North America. AIDS 2012;26:1415–1423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ortego C, Huedo-Medina TB, Llorca J, et al. . Adherence to highly active antiretroviral therapy (HAART): A meta-analysis. AIDS Behav 2011;15:1381–1396 [DOI] [PubMed] [Google Scholar]
- 14. Parker RA, Rabideau DJ, Sax PE, et al. . Impact of medication adherence on virologic failure in A5202: A randomized, partially blinded, phase 3B study. Clin Infect Dis 2017;64:1612–1614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Paterson DL, Swindells S, Mohr J, et al. . Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000;133:21–30 [DOI] [PubMed] [Google Scholar]
- 16. Valenti WM. Treatment adherence improves outcomes and manages costs. AIDS Read 2001;11:77–80 [PubMed] [Google Scholar]
- 17. Bangsberg DR, Hecht FM, Charlebois ED, et al. . Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS 2000;14:357–366 [DOI] [PubMed] [Google Scholar]
- 18. Cohen MS, Chen YQ, McCauley M, et al. . Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011;365:493–505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV. Department of Health and Human Services, 2015. Available at: http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf
- 20. Cofrancesco J Jr., Scherzer R, Tien PC, et al. . Illicit drug use and HIV treatment outcomes in a US cohort. AIDS 2008;22:357–365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hinkin CH, Castellon SA, Durvasula RS, et al. . Medication adherence among HIV+ adults: Effects of cognitive dysfunction and regimen complexity. Neurology 2002;59:1944–1950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hinkin CH, Hardy DJ, Mason KI, et al. . Medication adherence in HIV-infected adults: Effect of patient age, cognitive status, and substance abuse. AIDS 2004;18 Suppl 1:S19–S25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lima VD, Geller J, Bangsberg DR, et al. . The effect of adherence on the association between depressive symptoms and mortality among HIV-infected individuals first initiating HAART. AIDS 2007;21:1175–1183 [DOI] [PubMed] [Google Scholar]
- 24. Lovejoy TI, Suhr JA. The relationship between neuropsychological functioning and HAART adherence in HIV-positive adults: A systematic review. J Behav Med 2009;32:389–405 [DOI] [PubMed] [Google Scholar]
- 25. Schneider J, Kaplan SH, Greenfield S, et al. . Better physician-patient relationships are associated with higher reported adherence to antiretroviral therapy in patients with HIV infection. J Gen Intern Med 2004;19:1096–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Becker BW, Thames AD, Woo E, et al. . Longitudinal change in cognitive function and medication adherence in HIV-infected adults. AIDS Behav 2011;15:1888–1894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cysique LA, Brew BJ. Neuropsychological functioning and antiretroviral treatment in HIV/AIDS: A review. Neuropsychol Rev 2009;19:169–185 [DOI] [PubMed] [Google Scholar]
- 28. Ettenhofer ML, Foley J, Castellon SA, et al. . Reciprocal prediction of medication adherence and neurocognition in HIV/AIDS. Neurology 2010;74:1217–1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Oh DL, Sarafian F, Silvestre A, et al. . Evaluation of adherence and factors affecting adherence to combination antiretroviral therapy among White, Hispanic, and Black men in the MACS Cohort. J Acquir Immune Defic Syndr 2009;52:290–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Galvan FH, Bogart LM, Wagner GJ, et al. . Conceptualisations of masculinity and self-reported medication adherence among HIV-positive Latino men in Los Angeles, California, USA. Cult Health Sex 2014;16:697–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jernewall N, Zea MC, Reisen CA, et al. . Complementary and alternative medicine and adherence to care among HIV-positive Latino gay and bisexual men. AIDS Care 2005;17:601–609 [DOI] [PubMed] [Google Scholar]
- 32. van Servellen G, Lombardi E. Supportive relationships and medication adherence in HIV-infected, low-income Latinos. West J Nurs Res 2005;27:1023–1039 [DOI] [PubMed] [Google Scholar]
- 33. Simoni JM, Frick PA, Huang B. A longitudinal evaluation of a social support model of medication adherence among HIV-positive men and women on antiretroviral therapy. Health Psychol 2006;25:74–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Arnsten JH, Li X, Mizuno Y, et al. . Factors associated with antiretroviral therapy adherence and medication errors among HIV-infected injection drug users. J Acquir Immune Defic Syndr 2007;46 Suppl 2:S64–S71 [DOI] [PubMed] [Google Scholar]
- 35. Aardex Group. Advanced analytic research on drug exposure. Available at: http://www.aardex.ch/
- 36. Robbins RN, D'Aquila E, Morgello S, et al. . Cultural influences on antiretroviral therapy adherence among HIV-infected Puerto Ricans. J Assoc Nurses AIDS Care 2012;23:531–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Arentoft A, Byrd D, Robbins RN, et al. . Multidimensional effects of acculturation on English-language neuropsychological test performance among HIV+ Caribbean Latinas/os. J Clin Exp Neuropsychol 2012;34:814–825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Barron F, Hunter A, Mayo R, et al. . Acculturation and adherence: Issues for health care providers working with clients of Mexican origin. J Transcult Nurs 2004;15:331–337 [DOI] [PubMed] [Google Scholar]
- 39. Schwab T, Meyer J, Merrell R. Measuring attitudes and health beliefs among Mexican Americans with diabetes. Diabetes Educ 1994;20:221–227 [DOI] [PubMed] [Google Scholar]
- 40. Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev 2009;31:99–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wawrzyniak AJ, Ownby RL, McCoy K, et al. . Health literacy: Impact on the health of HIV-infected individuals. Curr HIV/AIDS Rep 2013;10:295–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rivera Mindt M, Byrd D, Ryan EL, et al. . Characterization and sociocultural predictors of neuropsychological test performance in HIV+ Hispanic individuals. Cultur Divers Ethnic Minor Psychol 2008;14:315–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. World Health Organization. Composite International Diagnostic Interview. Geneva: Switzerland; 1997 [Google Scholar]
- 44. Beck AT, Steer RA, Brown GK Beck Depression Inventory-Second Edition. San Antonio, TX: The Psychological Corporation; 1996
- 45. Heaton RK, Marcotte TD, Mindt MR, et al. . The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc 2004;10:317–331 [DOI] [PubMed] [Google Scholar]
- 46. Heaton RK, Clifford DB, Franklin DR Jr, et al. . HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology 2010;75:2087–2096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Heaton RK, Kirson D, Velin RA, et al. The utility of clinical ratings for detecting cognitive change in HIV infection. In: Psychology of HIV Infection. Grant I, Markin A, eds. New York, NY: Oxford University Press; 1994, pp. 188–206
- 48. Chin AL, Negash S, Xie S, et al. . Quality, and not just quantity, of education accounts for differences in psychometric performance between african americans and white non-hispanics with Alzheimer's disease. J Int Neuropsychol Soc 2012;18:277–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sayegh P, Arentoft A, Thaler NS, et al. . Quality of education predicts performance on the Wide Range Achievement Test-4th Edition Word Reading subtest. Arch Clin Neuropsychol 2014;29:731–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Silverberg ND, Hanks RA, Tompkins SC. Education quality, reading recognition, and racial differences in the neuropsychological outcome from traumatic brain injury. Arch Clin Neuropsychol 2013;28:485–491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Holdnack HA. Wechsler Test of Adult Reading: WTAR. San Antonio, TX: The Psychological Corporation; 2001
- 52. Zea MC, Asner-Self KK, Birman D, et al. . The abbreviated multidimensional acculturation scale: Empirical validation with two Latino/Latina samples. Cultur Divers Ethnic Minor Psychol 2003;9:107–126 [DOI] [PubMed] [Google Scholar]
- 53. Zea MC, Reisen CA, Poppen PJ, et al. . Disclosure of HIV-positive status to Latino gay men's social networks. Am J Community Psychol 2004;33:107–116 [DOI] [PubMed] [Google Scholar]
- 54. Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale University Press, 1975
- 55. Cirino PT, Chin CE, Sevcik RA, et al. . Measuring socioeconomic status: Reliability and preliminary validity for different approaches. Assessment 2002;9:145–155 [DOI] [PubMed] [Google Scholar]
- 56. Arentoft A, Byrd D, Monzones J, et al. . Socioeconomic status and neuropsychological functioning: Associations in an ethnically diverse HIV+ cohort. Clin Neuropsychol 2015;29:232–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Parker RM, Baker DW, Williams MV, et al. . The test of functional health literacy in adults: A new instrument for measuring patients' literacy skills. J Gen Intern Med 1995;10:537–541 [DOI] [PubMed] [Google Scholar]
- 58. Gakumo CA, Vance DE, Moneyham LD, et al. . Health numeracy and health literacy within the context of management of patients with human immunodeficiency virus. Nurs Res Rev 2013;3:23–31 [Google Scholar]
- 59. Drainoni ML, Rajabiun S, Rumptz M, et al. . Health literacy of HIV-positive individuals enrolled in an outreach intervention: Results of a cross-site analysis. J Health Commun 2008;13:287–302 [DOI] [PubMed] [Google Scholar]
- 60. Kalichman SC, Benotsch E, Suarez T, et al. . Health literacy and health-related knowledge among persons living with HIV/AIDS. Am J Prev Med 2000;18:325–331 [DOI] [PubMed] [Google Scholar]
- 61. Kalichman SC, Pope H, White D, et al. . Association between health literacy and HIV treatment adherence: Further evidence from objectively measured medication adherence. J Int Assoc Physicians AIDS Care (Chic) 2008;7:317–323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Waldrop-Valverde D, Jones DL, Gould F, et al. . Neurocognition, health-related reading literacy, and numeracy in medication management for HIV infection. AIDS Patient Care STDS 2010;24:477–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. McDonald-Miszczak L, Maris P, Fitzgibbon T, et al. . A pilot study examining older adults' beliefs related to medication adherence: The BERMA survey. J Aging Health 2004;16:591–614 [DOI] [PubMed] [Google Scholar]
- 64. Woods SP, Moran LM, Carey CL, et al. . Prospective memory in HIV infection: Is “remembering to remember” a unique predictor of self-reported medication management? Arch Clin Neuropsychol 2008;23:257–270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–396 [PubMed] [Google Scholar]
- 66. Cohen S. Perceived stress in a probability sample of the United States. In: The Claremont Symposium on Applied Social Psychology. The Social Psychology of Health. Oskamp SSS, ed. Thousand Oaks, CA: Sage Publications, Inc.; 1988, pp. 31–67
- 67. Perera MJ, Brintz CE, Birnbaum-Weitzman O, et al. . Factor structure of the Perceived Stress Scale-10 (PSS) across English and Spanish language responders in the HCHS/SOL Sociocultural Ancillary Study. Psychol Assess 2017;29:320–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Giordano TP, Guzman D, Clark R, et al. . Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clin Trials 2004;5:74–79 [DOI] [PubMed] [Google Scholar]
- 69. Arnsten JH, Demas PA, Farzadegan H, et al. . Antiretroviral therapy adherence and viral suppression in HIV-infected drug users: Comparison of self-report and electronic monitoring. Clin Infect Dis 2001;33:1417–1423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Lieu TA, Davis RL, Capra AM, et al. . Variation in clinician recommendations for multiple injections during adoption of inactivated polio vaccine. Pediatrics 2001;107:E49. [DOI] [PubMed] [Google Scholar]
- 71. McNabb JJ, Nicolau DP, Stoner JA, et al. . Patterns of adherence to antiretroviral medications: The value of electronic monitoring. AIDS 2003;17:1763–1767 [DOI] [PubMed] [Google Scholar]
- 72. Pearson CR, Simoni JM, Hoff P, et al. . Assessing antiretroviral adherence via electronic drug monitoring and self-report: An examination of key methodological issues. AIDS Behav 2007;11:161–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Bova CA, Fennie KP, Knafl GJ, et al. . Use of electronic monitoring devices to measure antiretroviral adherence: Practical considerations. AIDS Behav 2005;9:103–110 [DOI] [PubMed] [Google Scholar]
- 74. Field A. Discovering Statistics Using IBM SPSS Statistics. London, United Kingdom: Sage; 2013, p. 952
- 75. Howell DC. Statistical Methods for Psychology. 6th Edition. Belmont, CA: Thomson Wadsworth; 2007
- 76. Tabachnick BG, Fidell LS Using Multivariate Analysis. New York, NY: Allyn & Bacon/Pearson Education; 2007
- 77. Kaplan MS, Huguet N, Newsom JT, et al. . The association between length of residence and obesity among Hispanic immigrants. Am J Prev Med 2004;27:323–326 [DOI] [PubMed] [Google Scholar]
- 78. Ro A. The longer you stay, the worse your health? A critical review of the negative acculturation theory among Asian immigrants. Int J Environ Res Public Health 2014;11:8038–8057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Lara M, Gamboa C, Kahramanian MI, et al. . Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annu Rev Public Health 2005;26:367–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Chesney MA, Ickovics JR, Chambers DB, et al. . Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care 2000;12:255–266 [DOI] [PubMed] [Google Scholar]
- 81. Kalichman SC, Grebler T. Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosom Med 2010;72:810–816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Hinkin CH, Barclay TR, Castellon SA, et al. . Drug use and medication adherence among HIV-1 infected individuals. AIDS Behav 2007;11:185–194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Arnsten JH, Demas PA, Grant RW, et al. . Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. J Gen Intern Med 2002;17:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Meade CS, Conn NA, Skalski LM, et al. . Neurocognitive impairment and medication adherence in HIV patients with and without cocaine dependence. J Behav Med 2011;34:128–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. AIDSVu. Local Data: New York City. 2018. Available at: https://aidsvu.org/state/new-york/new-york-city/ (Last accessed December17, 2018).
- 86. HIV Epidemiology and Field Services Program. HIV Surveillance Annual Report, 2014. New York, NY: New York City Department of Health and Mental Hygiene, 2015
- 87. Centers for Disease Control and Prevention. Geographic differences in HIV infection among hispanics or latinos—46 states and Puerto Rico, 2010. MMWR 2012;61:805–810 [PubMed] [Google Scholar]
- 88. United States Census Bureau. 2010. Census Summary File 1. Washington, DC: United States Census Bureau; 2011. Available at: https://www.census.gov/prod/cen2010/doc/sf1.pdf
- 89. Sheehan DM, Cosner C, Fennie KP, et al. . Role of country of birth, testing site, and neighborhood characteristics on nonlinkage to HIV care among Latinos. AIDS Patient Care STDS 2018;32:165–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Arrington-Sanders R, Hailey-Fair K, Wirtz AL, et al. . Role of structural marginalization, HIV stigma, and mistrust on HIV prevention and treatment among young Black Latinx Men who have sex with men and transgender women: Perspectives from youth service providers. AIDS Patient Care STDS 2020;34:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kongs SK, Thompson LL, Iverson GL, Heaton RK WCST-64: Wisconsin Card Sorting Test-64 Card Version, Professional Manual. Odessa, FL: Psychological Assessment Resources, 2000
- 92. Heaton RK, Miller SW, Taylor MJ, Grant I. Revised Comprehensive Norms for an Expanded Halstead-Reitan Battery: Demographically Adjusted Neuropsychological Norms for African American and Caucasian Adults (HRB). Odessa, FL: Psychological Assessment Resources, Inc, 2004
- 93. Heaton RK, Taylor MJ, Manly J. Demographic effects and use of demographically corrected norms with the WAIS-III and WMS-III. In: Tulsky DS, Saklofske DH, Chelune GJ, et al., (eds.). Clinical Interpretation of the WAIS-III and WMS-III. Orlando, FL: Elsevier Science, 2003
- 94. Benedict RHB, Schretlen D, Groninger L, Brandt J. Hopkins Verbal Learning Test–Revised: normative data and analysis of inter-form and test–retest reliability. Clin Neuropsychol 1998;12:43–55 [Google Scholar]
- 95. Benedict R. Brief Visuospatial Memory Test–Revised Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc, 1997


