Abstract
BACKGROUND:
Sleep is often challenging for medical students because of the considerable amount of learning they have to do. The aim of this study was to identify the patterns of sleep quality and daytime sleepiness among medical students in Saudi Arabia and to identify the possible factors associated with poor quality of sleep and daytime sleepiness.
MATERIALS AND METHODS:
This cross-sectional questionnaire-based study was conducted at College of Medicine, Imam Abdulrahman Bin Faisal University, Saudi Arabia. The questionnaire included the prevalidated Pittsburgh Sleep Quality Index (PSQI) to measure sleep quality and the Epworth Sleepiness Scale (ESS) to measure daytime sleepiness. Covariates included sociodemographic characteristics and academic performance. Bivariate and multivariate logistic regression analyses were used to obtain adjusted and unadjusted odds ratios (ORs).
RESULTS:
The sampled population comprised 36.7% males and 63.30% females. The mean global PSQI score was (standard deviation (SD)=4.66), while the mean global ESS score was 8.03 (SD=4.66). Further analysis showed that 80.60% had poor sleep quality and 37.80% of the students suffered from excessive daytime sleepiness. Multivariate regression showed that poor sleep quality was significantly associated with poor academic achievement (adjusted OR = 3.33, 95% confidence interval [CI] = 1.28–8.63). Furthermore, excessive sleepiness significantly increased the odds of poor academic performance (adjusted OR = 4.58, 95% CI = 1.09–20.81).
CONCLUSIONS:
The results on daytime sleepiness were found to be within the ranges reported worldwide; poor sleep quality was found to be among the highest ever reported. Both sleep quality and daytime sleepiness significantly affect academic achievement.
Keywords: Daytime sleepiness, medical students, sleep quality
Introduction
Sleep for students in medical schools is often challenging because of the considerable amount of learning they have to do. Many factors could affect the patterns of sleep, thus marring the quality and reducing the duration of sleep. These include stress, depression, and increased workload as well as environmental and behavioral factors, particularly the consumption of such stimulants as caffeine, nicotine, and alcohol. Other factors may also include media use, especially before bedtime, and exercise, which is likely to have a positive impact on the quality and duration of sleep.[1,2,3,4,5]
A poor pattern of sleep is a problem of wide distribution that affects almost all students, both medical and nonmedical.[6,7] In a study done in the UK, poor sleep was reported by 24% of graduate students who had difficulty in sleeping or slept for <7 h or were unable to wake up properly on time.[8] Poor sleep quality affects the academic performance of students as their attention span, and overall energy in class to participate and learn diminishes.[9] Insufficient sleep impacts on alertness and leads to attention decline, and therefore, slows down cognitive processing. In addition, insufficient sleep interferes with the prefrontal cortex and hippocampus function, and this affects memory, language, creativity, and logical and critical reasoning. Therefore, students' academic performance may be compromised, thereby increasing the risk of medical malpractice and maltreatment in the future.[2,6]
On the other hand, optimal sleep impacts on mental performance and improves health, the quality of life, and productivity and thus affects the performance of students on examinations and eventually their overall academic achievement.[10] Simply put, sleep affects every aspect of our daily lives, mental, physical, and emotional. Evidence has shown that mental performance such as reaction time, memory, concentration, and reasoning all decline with chronic poor sleep.[11]
The epidemiological data of poor sleep patterns in different countries were found to vary between studies according to the tools used and the characteristics of the population including marital status, gender, age, and culture.[12] In the locally relevant study at King Saud University in Riyadh, Saudi Arabia, the prevalence of poor sleep patterns was found to be especially high among female medical students.[13] Although there have been previous attempts to study sleep in Saudi students, the results of its effect on academic performance were inconsistent.[14,15]
This study aims to identify the patterns of poor sleep quality and daytime sleepiness in the medical students at one of the largest medical colleges in Saudi Arabia and their association with academic performance. It was also to identify possible factors associated with poor sleep quality and daytime sleepiness.
Materials and Methods
This cross-sectional study required a minimum sample of 172 students from Imam Abdulrahman Bin Faisal University (IAU) in Dammam, Saudi Arabia, to obtain an acceptable power of 90%. Targeted students were those in their clinical years, i.e., the 4th, 5th, and 6th years in the College of Medicine during the 2018–2019 academic year. Ethical approval was obtained from the Ethical Committee of IAU and informed written consent was obtained from all the participants. The total number of 4th year students was 128, 5th year students was 148, and 6th year students was 136. A stratified proportional random sampling technique using the aforementioned student list was used and every second student was selected. Every effort was made to obtain equal number of the three respective clinical years. The questionnaires, in English, were administered by trained research assistants, and a total of 180 students submitted their responses. It was explained to the students that participation was voluntary.
The questionnaire included sociodemographic and specific lifestyle information related to the consumption of caffeinated drinks and the use of mobile phones. It also included two formerly validated questionnaires: the first was the Pittsburgh Sleep Quality Index (PSQI) which is used to evaluate sleep disturbance and the second was the Epworth Sleepiness Scale (ESS) which is used to evaluate the presence of daytime sleepiness.[16,17]
The PSQI is a prevalidated questionnaire consisting of 19 self-rated questions incorporating information on seven components: perceived sleep quality (accepting one of four responses ranging from very good to very poor), sleep latency, sleep duration (calculated to the nearest hour), habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime sleepiness and disturbances during the day. Scores are added to give a maximum score of 21, which indicates overall very good sleep quality. An overall PSQI score of <5 indicates that the individual may have difficulties in a minimum of two components.[16]
The ESS questionnaire is also one that allows participants to self-evaluate their tendency to doze off in eight different situations, each with a possible score of 0 to 3. Scores are then summed up to give a global ESS score between 0 and 24.[17]
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 20.0 (IBM Corp., Armonk, NY).[18] There were two main outcomes: the first was the overall sleep quality as measured by the PSQI and the second was excessive daytime sleepiness as measured by the ESS. Bivariate logistic regression was used to obtain unadjusted odds ratios (ORs) and their relative 95% confidence intervals (CIs). Adjusted ORs were estimated through a multivariate logistic regression.
Results
The study included a total of 180 students who were randomly recruited from the College of Medicine at IAU. Every effort was made to obtain an equal number of students from the three clinical years.
The sampled population consisted of 36.7% males and 63.3% females; 13.3% of this population were married. The majority lived with families (85%), while 12.8% were in student accommodation. The average hours of sleep were 6 h and the average time of waking up was 8:00 am. The calculated global PSQI had a mean of 8.0 ± 4.6 SD, and the mean ESS score was 8.03 ± 3.5. The distribution of both the scores by academic achievement is shown in Figure 1. These scores were then categorized according to the preset thresholds where it was found that only 19.4% had good quality of sleep, while 80.6% had poor sleep. Furthermore, the calculated global ESS had shown that 37.8% suffered from excessive daytime sleepiness [Table 1].
Figure 1.
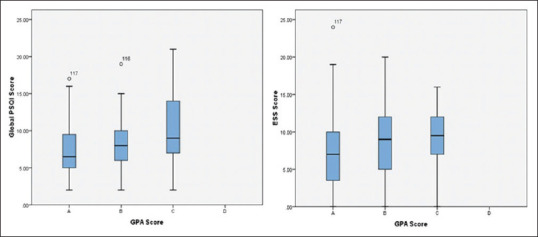
Global Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale scores by academic achievement of medical students in their clinical years at Imam Abdulrahman Bin Faisal University, Saudi Arabia, in the academic year 2018–2019
Table 1.
Sociodemographic characteristics of medical students (in their clinical years) at Imam Abdulrahman Bin Faisal University, Saudi Arabia, in the academic year 2018–2019
| Characteristics | N (%) |
|---|---|
| Sex | |
| Males | 66 (36.7) |
| Females | 114 (63.3) |
| Marital status | |
| Single | 156 (86.7) |
| Married | 24 (13.3) |
| Divorced | - |
| Widowed | - |
| Medical year | |
| Fourth year | 60 (33.3) |
| Fifth year | 60 (33.3) |
| Sixth year | 60 (33.3) |
| Living situation | |
| With family | 153 (85.0) |
| Student accommodation | 23 (12.8) |
| With relatives/friends | 04 (02.2) |
| Sleep quality | |
| Good | 35 (19.4) |
| Poor | 145 (80.6) |
| Daytime sleepiness | |
| Normal daytime sleepiness | 112 (62.2) |
| Excessive daytime sleepiness | 68 (37.8) |
| GPA | |
| A | 72 (40.0) |
| B | 98 (54.4) |
| C | 10 (05.6) |
GPA=Grade point average
Examining the quality of sleep in the bivariate analyses revealed its association with academic achievement, in which poor sleep quality was associated with poor academic achievement (unadjusted OR = 2.30, 95% CI = 1.07–4.96). This association remained significant after adjustment in the multivariate model (adjusted OR = 3.33, 95% CI = 1.28–8.63). The adjusted model has shown that the odds of achieving a grade of C were higher with poor sleep quality although not being statistically significant (OR = 4.07). Furthermore, not consuming coffee or tea was found to be negatively associated with poor sleep quality indicating a protective effect, which was significant in both the adjusted and unadjusted estimates (adjusted OR = 0.32, 95% CI = 0.10–0.98) [Table 2]. After adjusting for gender as a possible confounder in the association between excessive sleepiness and academic performance, it was found that excessive sleepiness increased the odds of poor academic achievement in our student sample. This was statistically significant after adjustment (OR = 4.58, 95% CI = 1.09–20.81) [Table 3].
Table 2.
Associations between sleep quality and academic performance adjusting for sex, caffeinated drink consumption, and mobile use among medical students (in their clinical years) at Imam Abdulrahman Bin Faisal University, Saudi Arabia, in the academic year 2018–2019
| Predictors | Good sleep quality N (%) | Poor sleep quality N (%) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Sex | ||||
| Males | 17 (9.4) | 49 (27.2) | 0.54 (0.25–1.14) | 0.19 (0.07–0.55) |
| Females | 18 (10.0) | 96 (53.3) | ||
| GPA | ||||
| A | 20 (11.1) | 52 (28.9) | ||
| B | 14 (7.8) | 84 (46.7) | 2.30 (1.07–4.96) | 3.33 (1.28–8.63) |
| C | 1 (0.6) | 9 (5.0) | 3.46 (0.41–29.11) | 4.07 (0.38–42.85) |
| Coffee and tea consumption | ||||
| One | 12 (6.7) | 70 (38.9) | ||
| Two to five cups | 12 (6.7) | 59 (32.8) | 0.84 (0.35–2.01) | 1.16 (0.44–3.04) |
| None | 11 (6.1) | 16 (8.9) | 0.24 (0.09–0.66) | 0.32 (0.10–0.98) |
| Soda consumption | ||||
| One | 2 (1.1) | 35 (19.4) | 5.11 (1.16–22.48) | 13.97 (2.52–77.40) |
| Two to five cups | 2 (1.1) | 4 (2.2) | 0.58 (0.10–3.34) | 1.68 (0.22–12.64) |
| None | 31 (17.2) | 106 (58.9) | ||
| Use of mobile device for e-books | ||||
| Yes | 7 (3.9) | 57 (31.7) | 2.59 (1.06–6.32) | 3.60 (1.29–10.05) |
| No | 28 (15.6) | 88 (48.9) |
CI=Confidence interval, OR=Odds ratio, GPA=Grade point average
Table 3.
Associations between daytime sleepiness and academic performance adjusting for sex, caffeinated drink consumption, and mobile use amongst medical students (in their clinical years) at Imam Abdulrahman Bin Faisal University, Saudi Arabia, in the academic year 2018–2019
| Predictors | Normal daytime sleepiness N (%) | Excessive daytime sleepiness N (%) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Sex | ||||
| Males | 47 (26.1) | 19 (10.6) | 0.53 (0.28–1.02) | 0.39 (0.17–0.88) |
| Females | 65 (36.1) | 49 (27.2) | ||
| GPA | ||||
| A | 52 (28.9) | 20 (11.1) | ||
| B | 55 (30.6) | 43 (23.9) | 2.03 (1.05–3.90) | 3.20 (1.40–07.27) |
| C | 5 (2.8) | 5 (2.8) | 2.60 (0.67–9.95) | 4.58 (1.09–20.81) |
| Coffee and tea consumption | ||||
| One or less | 52 (28.9) | 30 (16.7) | ||
| Two to five cups | 38 (21.1) | 33 (18.3) | 1.50 (0.78–2.87) | 1.51 (0.70–3.23) |
| None | 22 (12.2) | 5 (2.8) | 0.39 (0.13–1.14) | 0.37 (0.10–1.26) |
| Soda consumption | ||||
| One or less | 38 (21.1) | 36 (20.0) | ||
| Two to five cups | 7 (3.9) | 4 (2.2) | 1.97 (1.20–4.27) | 1.97 (0.93–4.13) |
| None | 67 (37.2) | 28 (15.6) | 1.36 (0.37–5.04) | 0.96 (0.22–4.20) |
| Use of mobile device for social networking | ||||
| Yes | 87 (48.3) | 43 (23.9) | ||
| No | 25 (13.9) | 25 (13.9) | 2.02 (1.04–3.93) | 1.70 (0.76–3.83) |
CI=Confidence interval, OR=Odds ratio, GPA=Grade point average
Discussion
More than two-third of our students in clinical years reported poor sleep. This is higher than the prevalence reported both in Saudi Arabia and worldwide.[19,20,21,22] The prevalence in our study population was found to be very similar to that of Colombian medical students, which was reported to be 79.3%.[22] Poor sleep quality of medical students was found to be lowest in Estonia, with a prevalence of 7%.[20] It was found to be 41.8% in Malaysian students and 64.2% in Pakistani students.[23] There was no significant difference between the poor sleep quality of the male and female students of our study as both reported troubled sleep. This is also true for medical students of other nationalities. This was unlike medical students in Taif where statistical differences were observed between genders.[24] A Moroccan study revealed no gender differences between male and female medical students with regard to their poor quality of sleep.[22]
Excessive daytime sleepiness, assessed by ESS, is a commonly reported phenomenon in medical students, the prevalence of which was reported to range from 24% to 39%.[12,13] These ranges do not differ significantly from what was found in our population, 37.8% of whom reported suffering from excessive daytime sleepiness.
A lot of medical students and junior clinicians think that sleep is overrated and not as important as study time, presentations, work submission, and examination preparations.[25] This is reflected by the big number reported in the literature of the poor sleep quality of workers in the medical profession although an increasingly large body of evidence has confirmed the fact that good sleep is essential for mental and physical health, cognition, and motor performance.[26] The demanding and overwhelming load of work encountered by medical students and young doctors early in their career not only affects the duration and quality of their sleep directly but also affects sleep by the buildup of stress indirectly. This creates a continuous vicious cycle of poor sleep, more stress, and less academic achievement.[14] It has been frequently reported that poor quality of sleep can negatively affect academic achievement as a direct result of poorer concentration and cognitive function owing to neuronal loss affected by shorter sleeping hours, poor sleep quality, and sleep–wake habits.[1] The results of our study also support the previously published data on the negative association between suboptimal sleep quality, excessive daytime sleepiness, and poor academic achievement, represented by the GPA of the students,[15,27] and the direct positive association between good sleep quality and longer duration of sleep with better academic performance.[28]
The results showing the association between excessive daytime sleepiness and poor academic achievement have not always been consistent in the literature. Al-Zahrani et al.[14] and El Hangouche et al.[22] found no significant effect of daytime sleepiness on the academic achievement of medical students. One reason that might explain such differences in the results is the presence of other factors that might have influenced daytime sleepiness such as the consumption of caffeinated drinks and energy drinks, technology, and the use of social media and characteristics of the sleeping environment, i.e., noise, light, and temperature.[4] Another reason could be the lower number of enrolled students in our population compared to the others.
On an interesting note, we found in the present study that the less caffeinated drinks consumed, the better the sleep quality, which in turn showed that not consuming caffeinated beverages and tea could have a protective effect on the quality of sleep, hence indirectly positively affecting academic achievement. This is routinely mentioned by physicians to patients suffering from poor sleep quality as part of their sleep hygiene counseling. Consuming fewer caffeinated drinks earlier in the day better improves the quality sleep and decreases the symptoms of insomnia.[29] It is important to note that the confidence intervals reported here reflect the low sample size acquired.
One must bear in mind that this study was done in a single educational institution, which may, therefore, negatively affect the ability to generalize the results to cover all other medical students. It is only by extensively exploring all aspects of sleep and sleeping patterns, that we can get to the root of the problem. The authors would also like to acknowledge that the cross-sectional study design and the survey method for data collection may have resulted in recall bias which contributes to the limitations of this work.
Conclusion
This research has examined poor sleep quality and daytime sleepiness of medical students in Saudi Arabia. The results on daytime sleepiness were found to be within ranges reported worldwide, while poor sleep quality was found to be among the highest ever reported. Both sleep quality and daytime sleepiness significantly affect academic achievement.
Programs to relieve stress and mindfulness and wellness programs to decrease levels of perceived stress in medical students are essential to break the cycle of poor sleep, more stress, and less academic achievement. Medical cultures that promote healthy diversity, responsibility, and accountability rather than competition and shaming are core to the solution of this issue encountered by students worldwide.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Genzel L, Ahrberg K, Roselli C, Niedermaier S, Steiger A, Dresler M, et al. Sleep timing is more important than sleep length or quality for medical school performance. Chronobiol Int. 2013;30:766–71. doi: 10.3109/07420528.2012.763132. [DOI] [PubMed] [Google Scholar]
- 2.Zeek ML, Savoie MJ, Song M, Kennemur LM, Qian J, Jungnickel PW, et al. sleep duration and academic performance among student pharmacists. Am J Pharm Educ. 2015;79:63. doi: 10.5688/ajpe79563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gomes AA, Tavares J, de Azevedo MH. Sleep and academic performance in undergraduates: A multi-measure, multi-predictor approach. Chronobiol Int. 2011;28:786–801. doi: 10.3109/07420528.2011.606518. [DOI] [PubMed] [Google Scholar]
- 4.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124–32. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 5.Xu X. The influence of social media on sleep quality: A study of undergraduate students in Chongqing, China. J Nurs Care. 2015;4 [Google Scholar]
- 6.Adeosun SO, Asa SO, Babalola OO, Akanmu MA. Effects of night-reading on daytime sleepiness, sleep quality and academic performance of undergraduate pharmacy students in Nigeria. Sleep Biol Rhythms. 2008;6:91–4. [Google Scholar]
- 7.James B, Omoaregba J, Igberase O. Prevalence and correlates of poor sleep quality among medical students at a Nigerian university. Ann Niger Med. 2011;5:1–5. [Google Scholar]
- 8.Webb E, Ashton CH, Kelly P, Kamali F. Alcohol and drug use in UK university students. Lancet. 1996;348:922–5. doi: 10.1016/s0140-6736(96)03410-1. [DOI] [PubMed] [Google Scholar]
- 9.Asarnow LD, McGlinchey E, Harvey AG. The effects of bedtime and sleep duration on academic and emotional outcomes in a nationally representative sample of adolescents. J Adolesc Health. 2014;54:350–6. doi: 10.1016/j.jadohealth.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahrberg K, Dresler M, Niedermaier S, Steiger A, Genzel L. The interaction between sleep quality and academic performance. J Psychiatr Res. 2012;46:1618–22. doi: 10.1016/j.jpsychires.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 11.Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: Relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997;42:583–96. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- 12.Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: A global perspective. J Clin Sleep Med. 2015;11:69–74. doi: 10.5664/jcsm.4370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AM, Alhaqwi AI. Sleep disorder among medical students: Relationship to their academic performance. Med Teach. 2012;34(Suppl 1):S37–41. doi: 10.3109/0142159X.2012.656749. [DOI] [PubMed] [Google Scholar]
- 14.Al-Zahrani JM, Aldossari KK, Abdulmajeed I, Al-Ghamdi SH, Al-Shamrani AM, Al-Qahtani NS. Daytime sleepiness and academic performance among Arab medical students. J Thorac Dis. 2016;8:AB006. [Google Scholar]
- 15.Bahammam AS, Alaseem AM, Alzakri AA, Almeneessier AS, Sharif MM. The relationship between sleep and wake habits and academic performance in medical students: A cross-sectional study. BMC Med Educ. 2012;12:61. doi: 10.1186/1472-6920-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 17.Johns MW. Sleepiness in different situations measured by the epworth sleepiness scale. Sleep. 1994;17:703–10. doi: 10.1093/sleep/17.8.703. [DOI] [PubMed] [Google Scholar]
- 18.Corp I. IBM SPSS Statistics for Windows. Ver. 20.0. Armonk, NY: IBM Corp; 2011. [Google Scholar]
- 19.Alsaggaf MA, Wali SO, Merdad RA, Merdad LA. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years. Relationship with stress and academic performance. Saudi Med J. 2016;37:173–82. doi: 10.15537/smj.2016.2.14288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Veldi M, Aluoja A, Vasar V. Sleep quality and more common sleep-related problems in medical students. Sleep Med. 2005;6:269–75. doi: 10.1016/j.sleep.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, Jagmohni KS. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia. 2009;64:108–10. [PubMed] [Google Scholar]
- 22.El Hangouche AJ, Jniene A, Aboudrar S, Errguig L, Rkain H, Cherti M, et al. Relationship between poor quality sleep, excessive daytime sleepiness and low academic performance in medical students. Adv Med Educ Pract. 2018;9:631–8. doi: 10.2147/AMEP.S162350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maheshwari G, Shaukat F. Impact of poor sleep quality on the academic performance of medical students. Cureus. 2019;11:e4357. doi: 10.7759/cureus.4357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alqarni AB, Alzahrani NJ, Alsofyani MA, Almalki AA. The interaction between Sleep quality and academic performance among the medical students in Taif University. Egypt J Hosp Med. 2018;70:2202–8. [Google Scholar]
- 25.Rodrigues RN, Viegas CA, Abreu E Silva AA, Tavares P. Daytime sleepiness and academic performance in medical students. Arq Neuropsiquiatr. 2002;60:6–11. doi: 10.1590/s0004-282x2002000100002. [DOI] [PubMed] [Google Scholar]
- 26.Owens JA. Sleep loss and fatigue in medical training. Curr Opin Pulm Med. 2001;7:411–8. doi: 10.1097/00063198-200111000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Gaultney JF. The prevalence of sleep disorders in college students: Impact on academic performance. J Am Coll Health. 2010;59:91–7. doi: 10.1080/07448481.2010.483708. [DOI] [PubMed] [Google Scholar]
- 28.Okano K, Kaczmarzyk JR, Dave N, Gabrieli JDE, Grossman JC. Sleep quality, duration, and consistency are associated with better academic performance in college students. NPJ Sci Learn. 2019;4:16. doi: 10.1038/s41539-019-0055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brick CA, Seely DL, Palermo TM. Association between sleep hygiene and sleep quality in medical students. Behav Sleep Med. 2010;8:113–21. doi: 10.1080/15402001003622925. [DOI] [PMC free article] [PubMed] [Google Scholar]


