Abstract
Objectives
To evaluate associations of risk perception, self-efficacy and response-efficacy with HPV vaccination decisions among parents/guardians of adolescents.
Methods
A cross-sectional survey of parents/guardians of adolescents was conducted at the Minnesota State Fair. Risk perception was measured by participant rankings of HPV infection and vaccine risks against diseases/side-effects for which numerical risks were provided. Response efficacy was measured as perceived ability of the vaccine to prevent HPV infection, and self-efficacy was measured as the perceived ability to prevent infection without vaccination (scale 0–100). Chi-squared and Fisher's exact tests compared risk perception, self-efficacy and response-efficacy of vaccinators to non-vaccinators.
Results
Of 405 eligible participants, 355 completed vaccination questions; 304 (86%) were vaccinators and 51 (14%) were non-vaccinators. Non-vaccinators had lower risk-perception of HPV-related cancers (p < 0.05) and higher risk-perception of vaccine-related side-effects (p < 0.05). Self-efficacy was higher (64 ± 24 vs. 30 ± 29; p < 0.0001) and perceived HPV vaccine response efficacy was lower (52 ± 31 vs. 83 ± 19; p < 0.0001) among non-vaccinators compared to vaccinators.
Conclusions
Lower HPV-related cancer risk perception and higher self-efficacy were associated with the decision not to vaccinate. HPV vaccination decisions were similar to meningococcal vaccination decisions, suggesting reluctance to vaccinate in general rather than resistance to the HPV vaccine specifically drove the results.
Keywords: HPV vaccination, Self-efficacy, Risk-perception, Perceived vaccine efficacy, Parents/guardians, Adolescents
Highlights
-
•
Minnesota State Fair Cross-sectional survey of parents/guardians of adolescents.
-
•
Higher HPV-related cancer risk perception associated with HPV vaccination.
-
•
Genital wart perception not associated with HPV vaccination decision.
-
•
Non-vaccination associated with perceived ability to prevent HPV infection.
-
•
Lower vaccine risk perception associated with decision to vaccinate against HPV.
1. Introduction
A highly-effective vaccine against human papillomavirus (HPV) has been available since 2006, yet current vaccination coverage is only 68%, and completion rates (2 doses for individuals <15 years of age, 3 doses for individuals 15+ years of age) for eligible individuals is only 51% in the United States. In contrast, meningococcal vaccination coverage is 87% [1]. While a lag between a new vaccine recommendation and uptake is expected, the HPV vaccine is especially controversial. The vaccine against a primarily sexually-transmitted virus is recommended for adolescents 11–12 years of age, with a goal of completing the vaccine series prior to the initiation of sexual activity. Additionally, despite the fact that 79 million Americans are currently infected with HPV [2], many people believe they are not at risk for the virus. Lastly, supported by the larger anti-vaccination movement, there is significant press coverage regarding adverse effects of the HPV vaccine, despite the fact that severe adverse events such as chronic fatigue syndrome, premature ovarian failure and death have not been proven in clinical trials or post-marketing surveillance [3]. Multiple studies assessing the safety of the HPV vaccine have shown adverse effects are short-term and mild, with injection site reactions comprising pain, redness and swelling most commonly reported; serious adverse effects were rare and similar between those receiving the vaccine or placebo [4]. In an effort to counteract the negative sentiment about HPV vaccination, multiple health organizations, including the Centers for Disease Control and Prevention, encourage healthcare providers to strongly recommend the vaccine [5], and have also directly appealed to parents/guardians through traditional (e.g. television, radio, magazine ads) and online media [6,7].
The efficacy of healthcare promotions depends not only on the effectiveness of the advertising, but also an individual's personal perceptions and beliefs [8]. Risk perception is the subjective assessment of characteristics and severity of a risk. For example, some would perceive a potentially avoidable 5% risk of an HPV infection causing cervical cancer as high, whereas others perceive this risk level as low enough that intervention is not indicated. Self-efficacy is one's belief in their ability to succeed in a specific situation or accomplish a task, for example one's belief that s/he can do something to prevent HPV infection or its sequelae. The parallel to this is response-efficacy which is one's belief that a particular action will avoid the threat, or in this setting the belief that HPV vaccination will prevent HPV infection and subsequent cancer or genital warts.
The primary objective of this study was to evaluate the association between risk-perception, self-efficacy and response-efficacy with parental/guardian decision-making regarding adolescent HPV vaccination. We hypothesized that low HPV risk-perception and high perceived self-efficacy to prevent HPV infection or its sequelae would be associated with decision not to vaccinate. In contrast, we hypothesized that high vaccine response efficacy and low perceived risk of vaccine-related side-effects would be associated with the decision to vaccinate against HPV. The secondary objective of this study was to compare self-efficacy and response-efficacy for prevention of HPV infection with prevention of meningococcal infection.
2. Methods
2.1. Data
The study was approved by the University of Minnesota's Institutional Review Board (STUDY00003413). The study was a cross-sectional survey of parents and guardians of HPV vaccine age-eligible adolescents 9–17 years of age who attended the Minnesota State Fair. The Minnesota State Fair attracts over two-million people annually from Minnesota and the surrounding states, with attendee demographics generally representative of the state of Minnesota. Participants were recruited at the University of Minnesota Driven to Discover building, a site dedicated to research study recruitment for University of Minnesota faculty and associates. Participants were recruited over three 7-h shifts over 1 week in August 2018. State fair attendees were eligible to participate in the study if they self-identified as the parent or guardian of an adolescent 9–17 years of age, were able to read and write in English, and were able to provide consent. Parents/guardians of more than one adolescent within the target age range were asked to respond to vaccination questions as they pertained to the oldest adolescent within the target age range (e.g. participants with children 8, 11, 15 and 21 years of age answered vaccination questions as they pertained to the 15 year-old). The survey was administered online via electronic tablet, and the data were collected and managed using Research Electronic Data Capture (REDCap) [9]. All data were collected anonymously. Participants received a University of Minnesota drawstring backpack on completion of the survey.
2.2. Measures
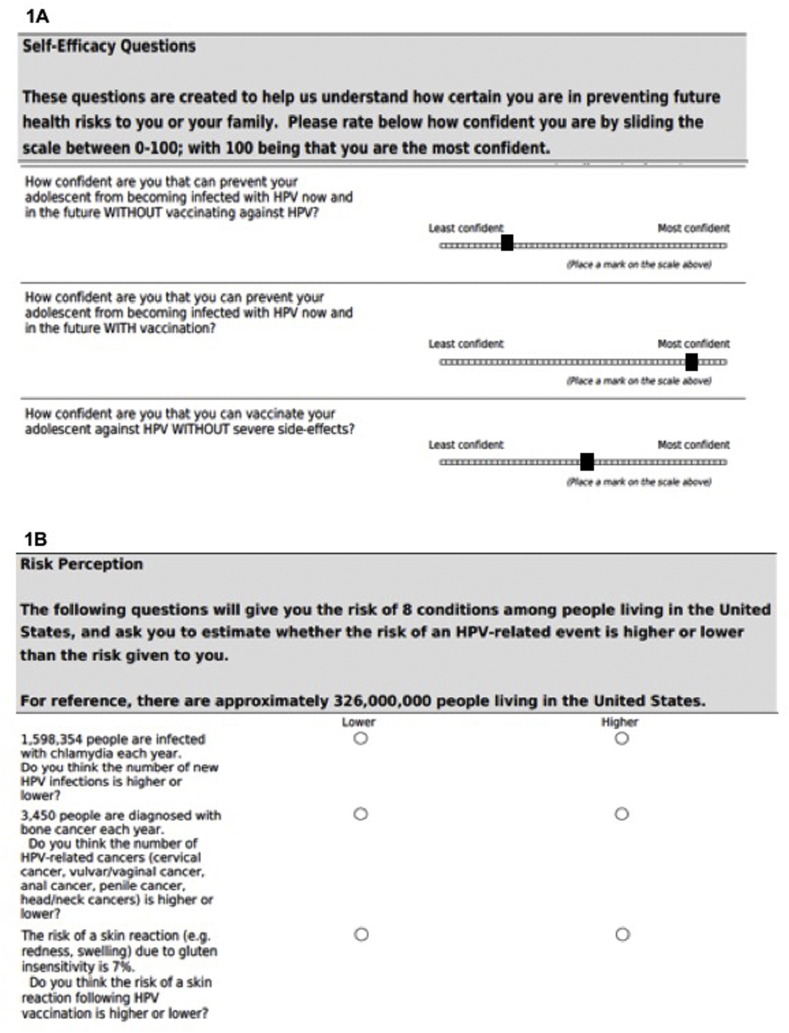
The survey included 68 questions covering the following topics: 1) self-efficacy: confidence in one's ability to prevent HPV or meningitis infection without vaccination; confidence in one's ability to research the risks/benefits of HPV vaccination; 2) response-efficacy: confidence in the vaccine's ability to prevent HPV or meningococcal infection; confidence in ability to vaccinate without severe side-effects; 3) risk-perception: perceived risks of HPV-related cancers, genital warts, and vaccine-related side-effects; 4) parent/guardian-reported adolescent information: age, biologic sex, gender, sexual history, health insurance status, HPV vaccination status; 5) participant demographics: age, sex, race. Self-efficacy and response-efficacy were rated on a scale of 0 (not confident) to 100 (very confident) using a slide-rule (Fig. 1A). Risk-perception was measured by ranking the HPV or vaccine-related risk as “higher” or “lower” than the given risk for which a numerical measure (incidence or prevalence) was provided (Fig. 1B). A measure of relative risk perception was used as it reduced the ambiguity inherent to interpersonal variability in interpretation of terms such as “high-risk” or “low-risk,” and allowed comparison of over-estimation or under-estimation of risk by HPV vaccination status.
Fig. 1.
Examples of question format for self-efficacy and vaccine response efficacy (Fig. 1A) and risk-perception questions (Fig. 1B).
2.3. Survey development
The survey was developed by the study investigators. The phrasing and structure of the self-efficacy questions were developed based on Albert Bandura's “Guide for constructing self-efficacy scales” [10]. An initial survey was tested among a panel of undergraduate and medical students for content and clarity. The revised survey was then piloted tested using a convenience sample of adolescent parents/guardians, and the survey was revised a second time prior to conducting the study. No formal validation testing was performed.
2.4. Analyses
Survey responses were summarized using descriptive statistics. Parents/guardians who had vaccinated or planned to vaccinate their adolescent (“vaccinators”) were compared to those who did not plan to vaccinate their adolescent (“non-vaccinators”) by demographic characteristics, self-efficacy, response-efficacy and risk-perception using Chi-squared tests and Fisher's exact tests as appropriate for categorical variables, and using two-sided two-sample t-tests assuming unequal variance for continuous variables. Means ± standard deviations (SD) and frequencies and percentages are reported unless otherwise noted. Statistical analyses were performed using SAS 9.4 (Cary, NC), and p-values less than 0.05 were considered statistically significant.
3. Results
3.1. Participants
A total of 424 state fair attendees initiated the survey, and 405 (96%) eligible participants completed the survey. Demographics of the parents/guardians and their adolescents are detailed in Table 1. A majority of parents/guardians were 41–50 years (55%), female (71%), and identified as White race (83%). Just over half of participants (58%) answered questions in regard to a female child. Most parents/guardians thought their adolescent was heterosexual (89%) and only 6% thought their adolescent was sexually active. Most adolescents (86%) were covered by private insurance.
Table 1.
Participant & adolescent demographics (N=405)a.
| Variable | n | (%) |
| Parent/Guardian Demographics | ||
| Age (in years) | ||
| 18-40 | 105 | (25.9) |
| 41-50 | 218 | (54.6) |
| ≥51 | 76 | (18.8) |
| Biological Sex | ||
| Male | 112 | (28.1) |
| Female | 284 | (71.2) |
| Transgender/gender-queer/gender-fluid/unsure | ||
| Yes | 3 | (0.8) |
| Race | ||
| American Indian or Alaska Native | 3 | (0.8) |
| Asian | 25 | (6.3) |
| Black/African/African American | 11 | (2.8) |
| White | 331 | (83.0) |
| Mixed (>1 race) | 11 | (2.8) |
| Other | 8 | (2.0) |
| Adolescent Demographics (per parent/guardian perception) | ||
| Biological sex | ||
| Male | 168 | (42.1) |
| Female | 231 | (57.9) |
| Adolescent's sexual identity | ||
| Straight/heterosexual | 353 | (88.5) |
| Gay/lesbian/bisexual | 8 | (2.0) |
| Other sexual identity | 2 | (0.5) |
| Not sure | 24 | (6.0) |
| Sexually active | ||
| Yes | 24 | (6.0) |
| No | 343 | (86.0) |
| I don't know | 25 | (6.3) |
| Adolescent's health insurance status | ||
| No insurance | 3 | (0.8) |
| Private insurance | 341 | (85.5) |
| Government insurance | 29 | (7.3) |
| Combination private and government | 13 | (3.3) |
| Adolescent HPV Vaccination History/Plans | ||
| Received 1+ dose of HPV vaccine | ||
| Yes | 245 | (61.3) |
| No, but I do plan to vaccinate | 59 | (14.8) |
| No, I do not plan to vaccinate | 51 | (12.8) |
| I don't know | 45 | (11.3) |
| Number of HPV vaccine doses received (among vaccinated; N=245) | ||
| 1 | 74 | (30.2) |
| 2 | 88 | (35.9) |
| 3 | 54 | (22.0) |
| Currently getting vaccinated (plan for 1+ more doses) | 12 | (4.9) |
| Unsure | 17 | (6.9) |
| Age at HPV vaccination initiation (among vaccinated or planned; N=304) | ||
| 9–10 years | 48 | (15.8) |
| 11–12 years | 134 | (44.1) |
| 13–14 years | 86 | (28.3) |
| 15–17 years | 31 | (10.2) |
| 18–26 years | 5 | (1.6) |
| Healthcare provider recommendation for HPV vaccine (N=405) | ||
| Yes | 295 | (73.8) |
| No | 59 | (14.8) |
“Prefer not to answer” and missing data omitted from table.
3.2. HPV vaccination history
A majority of participants (61%) reported their adolescent had at least initiated the HPV vaccine series, and an additional 15% planned to vaccinate their adolescent (Table 1). Almost half (44%) vaccinated or planned to vaccinate their adolescent at the Advisory Committee on Immunization Practices-recommended age of 11–12 years of age, with 16% vaccinating at the early but acceptable age of 9–10 years, and an additional 28% vaccinating or planning to vaccinate at age 13–14 years. There was no difference in vaccination rates by adolescent sex (57% of vaccinated individuals were female vs. 63% of unvaccinated were female; p = 0.43) or parental/guardian perception of their adolescent's sexual activity (p = 0.46; Table 2). While most participants reported a healthcare provider had recommended the HPV vaccine, vaccinators were more likely to report a healthcare provider recommendation (83% vs. 69%, p = 0.01).
Table 2.
Adolescent variables potentially associated with HPV vaccination.
| Variable | Vaccinators (N = 304)a |
Non-vaccinators (N = 51) |
p-value | ||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Biological sex | 0.43 | ||||
| Male | 131 | (43.1) | 19 | (37.3) | |
| Female | 173 | (56.9) | 32 | (62.8) | |
| Sexually active | 0.46 | ||||
| Yes | 17 | (5.6) | 4 | (7.8) | |
| No | 268 | (88.2) | 42 | (82.4) | |
| I don't know | 15 | (4.9) | 4 | (7.8) | |
| Prefer not to answer | 4 | (1.3) | 1 | (2.0) | |
| Healthcare provider recommendation for HPV vaccine | 0.01 | ||||
| Yes | 253 | (83.2) | 35 | (68.6) | |
| No | 32 | (10.5) | 13 | (25.5) | |
HPV, human papillomavirus.
Vaccinators include HPV vaccine series initiated and those who plan to vaccinate.
3.3. Self-efficacy, response efficacy
Among the entire study population, participants were moderately confident they could prevent HPV infection with vaccination (78 ± 23) and without severe side-effects (67 ± 30); this was similar to meningococcal prevention (78 ± 22). Self-efficacy was low and similar for HPV (37 ± 31) and meningococcal infection (36 ± 31) prevention.
The mean vaccine response-efficacy was higher among vaccinators (83 ± 19 vs. 52 ± 31; p < 0.0001; Table 3), and was similar for both the HPV and meningococcal vaccines. Similarly, the mean confidence score for ability to vaccinate against HPV without severe side-effects was significantly higher among vaccinators (75 ± 26 vs. 29 ± 30; p < 0.0001). In contrast, the mean self-efficacy was higher for non-vaccinators compared to vaccinators (64 ± 24 vs. 30 ± 29; p < 0.0001), and again was similar for both HPV and meningococcal infection prevention.
Table 3.
| Confidence in ability to: | Vaccinatorsc (N = 304) |
Non-vaccinators (N = 51) |
p-value |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Prevent HPV without vaccine | 30.0 (29.2) | 64.1 (23.9) | <0.0001 |
| Prevent HPV with vaccine | 82.8 (18.5) | 51.7 (30.5) | <0.0001 |
| Vaccinate against HPV without severe side effects | 74.8 (25.5) | 29.3 (29.9) | <0.0001 |
| Research risks and benefits of HPV vaccination | 81.4 (19.1) | 67.4 (29.6) | 0.002 |
| Prevent meningitis without vaccine | 31.8 (29.6) | 49.2 (32.4) | 0.0006 |
| Prevent meningitis with vaccine | 81.1 (19.1) | 62.4 (30.0) | <0.0001 |
HPV, human papillomavirus.
Self-efficacy: Confidence in one's ability to prevent disease.
Response-efficacy: Confidence in the vaccine's ability to prevent disease.
Vaccinated includes HPV vaccine series initiated and those who plan to vaccinate.
3.4. Risk perception
Among all participants, relative risk perception of HPV-related diseases was over-estimated, and relative risk-perception of HPV vaccine-related side-effects was under-estimated. Vaccinators were more likely to perceive a higher risk of HPV-related cancers, with 87% accurately ranking HPV-related cancers as higher than bone cancer (compared to 75% of non-vaccinators, p = 0.02), and 75% over-estimating the risk of HPV-related cancers compared to colon cancer (compared to 57% of non-vaccinators, p = 0.009) [Table 4]. However, there was no difference in perceived sexually transmitted infection risk between vaccinators and non-vaccinators. Non-vaccinators had a higher perceived risk of HPV vaccine-related side-effects. Notably, vaccinators were more likely to under-estimate the risk of common HPV vaccine side-effects such as skin reactions (defined as injection site pain and swelling; p = 0.0002) and headaches (p = 0.002) and accurately estimate the risk of fainting (p = 0.01). Perceived risk of vaccine-induced infertility, which data do not support as an adverse effect of the HPV vaccine, was similarly over-estimated to be greater than 14% in both groups (p = 0.67).
Table 4.
Risk perception of HPV- or vaccine related events.a.
| Variable | Vaccinators (N = 304) |
Non-vaccinators (N = 51) |
p-value | ||
|---|---|---|---|---|---|
| N | (%) | N | (%) | ||
| HPV-related cancersbvs. bone cancer | 0.02 | ||||
| Lower | 39 | (12.8) | 13 | (25.5) | |
| Higher* | 265 | (87.2) | 38 | (74.5) | |
| HPV-related cancersbvs. colon cancer | 0.009 | ||||
| Lower* | 77 | (25.3) | 22 | (43.1) | |
| Higher | 227 | (74.7) | 29 | (56.9) | |
| Genital warts vs. genital herpes | 0.46 | ||||
| Lower* | 69 | (22.7) | 14 | (27.5) | |
| Higher | 235 | (77.3) | 37 | (72.6) | |
| HPV infection vs. chlamydia infection | 0.47 | ||||
| Lower | 92 | (30.3) | 18 | (35.3) | |
| Higher* | 212 | (69.7) | 33 | (64.7) | |
| Infertility due to HPV vaccination vs. smoking | 0.67 | ||||
| Lower* | 129 | (42.4) | 20 | (39.2) | |
| Higher | 175 | (57.6) | 31 | (60.8) | |
| Skin reaction due to HPV vaccination vs. gluten hypersensitivity | 0.0002 | ||||
| Lower | 185 | (60.9) | 17 | (33.3) | |
| Higher* | 119 | (39.1) | 34 | (66.7) | |
| Fainting following HPV vaccination vs. during pregnancy | 0.01 | ||||
| Lower* | 211 | (69.4) | 26 | (51.0) | |
| Higher | 93 | (30.6) | 25 | (49.0) | |
| Headache following HPV vaccination vs. migraines | 0.002 | ||||
| Lower | 206 | (67.8) | 23 | (45.1) | |
| Higher* | 98 | (32.2) | 28 | (54.9) | |
Participants ranked the risk of HPV- or vaccine-related events as higher or lower than the events listed which included a risk in terms of percent or absolute number affected in the United States each year. Correct response indicated by (*).
HPV-related cancer risk was based on a composite of the number of anal, cervical, oropharyngeal, penile, vulvar and vaginal cancers diagnosed annually.
4. Discussion
4.1. Discussion and review of the literature
The results from this cross-sectional study supported our hypotheses and previously published literature showing that parents/guardians who do not vaccinate their adolescents against HPV perceived lower HPV-related cancer risk and higher HPV vaccine side-effects risks than those who vaccinated or planned to vaccinate their adolescent [11]. What is less often studied is the role of self-efficacy in HPV vaccination decision-making. The results of our study show that non-vaccinators have a higher perceived ability to prevent HPV infection without vaccination. Prior to introduction of the HPV vaccine, cervical cancer mortality decreased by 70% with the implementation of routine cervical cancer screening and detection and treatment of precancerous lesions or early-stage cancers which are amenable to cure [12,13]. While secondary prevention for cervical cancer is effective and does improve one's ability to prevent cervical cancer in the absence of HPV vaccination, the procedures required to excise or treat the precancerous lesions are associated with a higher risk of morbidity than HPV vaccination. Furthermore, there are currently no secondary prevention methods for the other HPV-associated malignancies. Anti-HPV vaccine social media campaigns have exploited the fact that most HPV infections do not result in cancer, and inflate the unproven dangers of the vaccine [14,15].
Multiple studies have demonstrated a reverse disparity in uptake of HPV vaccination, with privately insured, more highly educated and/or White individuals less likely to initiate the vaccine series than minorities or those with public insurance [[16], [17], [18]]. Social inequity may result in differences in disease risk perception and self-efficacy among different populations. A study comparing risk perception in regard to the flu vaccine showed White individuals were more likely to refuse vaccination due to the perception that influenza is “no big deal,” whereas African American non-vaccinators were more likely to cite vaccine side-effects and low perceived vaccine efficacy as primary motivators not to vaccinate [19]. This may be especially relevant in regard to the HPV vaccine since cervical cancer disproportionately affects individuals of lower socioeconomic class due to inadequate access to secondary prevention measures—approximately 60% of cervical cancer diagnoses in the United States occur amongst underserved populations, and mortality is higher in Black women compared to White women [20,21]. Our study did not show a difference in HPV vaccination decisions by race, but was limited by the predominantly White race (83%) of our participants, reflective of the demographics of the state of Minnesota.
Strong beliefs in sexual abstinence also play a role in HPV vaccination decisions. Survey studies have shown an inverse correlation between level of religious commitment and HPV vaccination coverage [22,23]. Furthermore, mediation analyses evaluating the relationship between religious beliefs, sexual activity and HPV vaccination among young adult women showed that sexual activity fully mediated the association between religious beliefs and HPV vaccination status [23]. These findings suggest that parents/guardians with strong religious or cultural beliefs that abstinence will overcome their adolescent's lifetime risk of HPV infection will require a different approach to increase HPV vaccination coverage. While religious beliefs were not measured in this study, it is notable that only 6% of participants thought their adolescent was sexually active; in contrast, results from the National Survey of Sexual Health and Human Behavior showed at least 30% of adolescents younger than 18 years of age have had heterosexual intercourse, and an additional proportion have engaged in other forms of sexual activity [24]. The large discrepancy in parental/guardian perceptions of adolescent sexual behavior and the published sexual health data is just one example of the discordance between perceived and true ability to prevent HPV infection.
The strengths of our study include the large number of participants outside of a vaccine-related clinical encounter. However, this may increase recall bias. While there was a striking difference in reported healthcare provider recommendation for the vaccine by vaccination status, it is unclear if this statistic truly reinforces the effect of a strong provider recommendation, or if vaccinators are just more likely to recall a recommendation than non-vaccinators. The study population was representative of Minnesota demographics, but generalizability of our study is limited by the fact that this was primarily a White, privately-insured and highly vaccinated population. Despite the lack of formal survey validation, the validity of our results is strengthened by the uniformity in responses regarding efficacy for both HPV vaccination and meningococcal vaccination, as well as uniformity in responses regarding risk perception, with striking differences between HPV infection-related risks compared to vaccine-related side-effects.
5. Conclusions
The results of our study show that parental/guardian HPV vaccination decisions for adolescents often parallel decisions regarding other adolescent vaccines, and that a strong recommendation by a healthcare provider is a key motivator for vaccination. Beyond the healthcare provider recommendation, the decision to vaccinate is influenced by disease and vaccine risk perception, but also self-efficacy to prevent HPV infection without vaccination. In addition to combating misinformation about vaccine risks, education efforts need to emphasize the difficulty in preventing HPV infection and its associated malignancies without vaccination, especially malignancies for which secondary prevention options do not exist.
Funding
This work was supported by the Driven to Discover State Fair Grant issued by the Masonic Cancer Center, University of Minnesota; National Institutes of Health (grant numbers K12HD055887, P30 CA77598 & UL1TR002494); The Masonic Cancer Center Women's Health Scholarship, University of Minnesota.
CRediT authorship contribution statement
Alicia Myhre: Conceptualization, Methodology, Investigation, Data curation, Writing - original draft, Writing - review & editing, Visualization. Tiaj Xiong: Conceptualization, Methodology, Software, Investigation, Writing - review & editing. Rachel I. Vogel: Conceptualization, Methodology, Validation, Formal analysis, Data curation, Writing - review & editing. Deanna Teoh: Conceptualization, Methodology, Investigation, Data curation, Writing - original draft, Writing - review & editing, Visualization, Supervision, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Macey McClay, Ayesha Sohail, Surbhi Sarup, Taylor Zoellner, who contributed significantly to development and testing of the survey.
Huda Adam, Melat Ashagre, Elif Ersahin, Tenley Klc, Jessica Lawrence, Madeline Lawrence, Jill Miller, Sena Muledhu, Laruen Reagan, Sharon Ogata, Megan Olson, Mariam Ramoni, Alena Tofte, Locke Uppendahl, Nujasaubnusi Vue who helped administer the survey at the Minnesota State Fair.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pvr.2020.100204.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Walker T.Y., Elam-Evans L.D., Yankey D., Markowitz L.E., Williams C.L., Fredua B. MMWR Morbidity and mortality weekly report. Vol. 68. 2019. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 Years - United States, 2018; pp. 718–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Genital HPV infection--fact sheet. 2017. https://www.cdc.gov/std/hpv/stdfact-hpv.htm accessed 1/28/19.
- 3.Udesky L. Push to mandate HPV vaccine triggers backlash in USA. Lancet. 2007;369:979–980. doi: 10.1016/S0140-6736(07)60475-9. [DOI] [PubMed] [Google Scholar]
- 4.Arbyn M., Xu L., Simoens C., Martin-Hirsch P.P. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018;5:CD009069. doi: 10.1002/14651858.CD009069.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Human papillomavirus: for healthcare professionals. https://www.cdc.gov/hpv/hcp/ accessed 6/1/20.
- 6.Centers for Disease Control and Prevention For immunization partners: video and audio resources. https://www.cdc.gov/vaccines/partners/teens/video-audio.html accessed 6/1/20.
- 7.Centers for Disease Control and Prevention For immunizaton partners: flyers/posters for teens/preteens. https://www.cdc.gov/vaccines/partners/teens/posters.html accessed 6/1/20.
- 8.Paek H.J., Hove T. Oxford Research Encyclopedias; 2017. Risk Perceptions and Risk Characteristics. [DOI] [Google Scholar]
- 9.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bandura A. Guide for constructing self-efficacy scales. In: Pajares F., Urdan T.C., editors. Self-efficacy Beliefs of Adolescents. Greenwich, Conn. IAP - Information Age Pub., Inc.; 2006. p. 367. xii. [Google Scholar]
- 11.Newman P.A., Logie C.H., Lacombe-Duncan A., Baiden P., Tepjan S., Rubincam C. Parents' uptake of human papillomavirus vaccines for their children: a systematic review and meta-analysis of observational studies. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-019206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Christopherson W.M., Lundin F.E., Jr., Mendez W.M., Parker J.E. Cervical cancer control: a study of morbidity and mortality trends over a twenty-one-year period. Cancer. 1976;38:1357–1366. doi: 10.1002/1097-0142(197609)38:3<1357::aid-cncr2820380340>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 13.Siegel R., Naishadham D., Jemal A. Cancer statistics. CA Canc. J. Clin. 2012;62:10–29. doi: 10.3322/caac.20138. 2012. [DOI] [PubMed] [Google Scholar]
- 14.Massey P.M., Leader A., Yom-Tov E., Budenz A., Fisher K., Klassen A.C. Applying multiple data collection tools to quantify human papillomavirus vaccine communication on twitter. J. Med. Internet Res. 2016;18:e318. doi: 10.2196/jmir.6670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ekram S., Debiec K.E., Pumper M.A., Moreno M.A. Content and commentary: HPV vaccine and YouTube. J. Pediatr. Adolesc. Gynecol. 2019;32(2):153–157. doi: 10.1016/j.jpag.2018.11.001. [DOI] [PubMed] [Google Scholar]
- 16.O'Leary S.T., Lockhart S., Barnard J., Furniss A., Dickinson M., Dempsey A.F. Exploring facilitators and barriers to initiation and completion of the human papillomavirus (HPV) vaccine series among parents of girls in a safety net system. Int. J. Environ. Res. Publ. Health. 2018;15 doi: 10.3390/ijerph15020185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spencer J.C., Calo W.A., Brewer N.T. Disparities and reverse disparities in HPV vaccination: a systematic review and meta-analysis. Prev. Med. 2019;123:197–203. doi: 10.1016/j.ypmed.2019.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vickers M., Green C.L., Lee H.Y., Pierce J.Y., Daniel C.L. Factors associated with HPV vaccination uptake and HPV-associated cancers: a county-level analysis in the state of Alabama. J. Community Health. 2019;44:1214–1223. doi: 10.1007/s10900-019-00690-1. [DOI] [PubMed] [Google Scholar]
- 19.Freimuth V.S., Jamison A., Hancock G., Musa D., Hilyard K., Quinn S.C. The role of risk perception in flu vaccine behavior among african-American and white adults in the United States. Risk Anal. 2017;37:2150–2163. doi: 10.1111/risa.12790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scarinci I.C., Garcia F.A., Kobetz E., Partridge E.E., Brandt H.M., Bell M.C. Cervical cancer prevention: new tools and old barriers. Cancer. 2010;116:2531–2542. doi: 10.1002/cncr.25065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Cancer Institute Surveillance, epidemiology and end results Program cancer stat facts: cervical cancer. https://seer.cancer.gov/statfacts/html/cervix.html accessed 7/23/19.
- 22.Birmingham W.C., Macintosh J.L.B., Vaughn A.A., Graff T.C. Strength of belief: religious commitment, knowledge, and HPV vaccination adherence. Psycho Oncol. 2019;28:1227–1233. doi: 10.1002/pon.5071. [DOI] [PubMed] [Google Scholar]
- 23.Best A.L., Thompson E.L., Adamu A.M., Logan R., Delva J., Thomas M. Examining the influence of religious and spiritual beliefs on HPV vaccine uptake among College women. J. Relig. Health. 2019;58:2196–2207. doi: 10.1007/s10943-019-00890-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herbenick D., Reece M., Schick V., Sanders S.A., Dodge B., Fortenberry J.D. Sexual behavior in the United States: results from a national probability sample of men and women ages 14-94. J. Sex. Med. 2010;7(Suppl 5):255–265. doi: 10.1111/j.1743-6109.2010.02012.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.