Abstract
Despite widespread use in schizophrenia-spectrum research, uncertainty remains around an empirically supported and theoretically meaningful factor structure of the Schizotypal Personality Questionnaire (SPQ). Current identified structures are limited by reliance on exclusively nonclinical samples. The current study compared factor structures of the SPQ in a sample of 335 nonpsychiatric individuals, 292 schizotypy-spectrum individuals (schizophrenia, schizoaffective disorder, or schizotypal personality disorder), and the combined group (N = 627). Unidimensional, correlated, and hierarchical models were assessed in addition to a bifactor model, wherein subscales load simultaneously onto a general factor and a specific factor. The best-fitting model across samples was a two-specific factor bifactor model, consistent with the nine symptom dimensions of schizotypy as primarily a direct manifestation of a unitary construct. Such findings, for the first time demonstrated in a clinical sample, have broad implications for transdiagnostic approaches, including reifying schizotypy as a construct underlying diverse manifestations of phenomenology across a wide range of severity.
Keywords: schizophrenia, schizotypy, psychosis, factor analysis, RDoC, constructs, self-report
Schizotypy is a broad, multidimensional construct that refers to a personality organization theorized to underlie schizophrenia-spectrum disorders (Grant, Green, & Mason, 2018). Accordingly, schizotypy is defined by a continuum of traits that can exist to a lesser extent in nonpsychiatric individuals and in greater magnitude and number in individuals with formal personality or psychotic disorders (Chapman, Chapman, & Raulin, 1978; Lenzenweger, 2018; Mason & Claridge, 2006; Torgersen et al., 2002). In fact, recent models of personality in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013) reflect this spectrum, suggesting that personality disorders reflect the extreme end of classic five-factor personality traits (Suzuki, Samuel, Pahlen, & Krueger, 2015). These findings have been borne out for schizotypy specifically: Models show invariance for samples of psychotic and nonpsychotic individuals, whereby schizophrenia symptom and schizotypy trait measures loaded together on respective factors (e.g., negative features on extraversion) (Cicero, Jonas, Li, Perlman, & Kotov, 2019).
Clinically severe manifestations of this personality trait have been conceptualized as schizotypal personality disorder (SPD). Originally, the DSM-III (APA, 1980) criteria for SPD were developed with consideration and observation of features common to schizophrenia-like patients and, to a lesser extent, to nonpsychotic family members (Kendler, 1985). Therefore, it seems reasonable that criteria for SPD overlap with the clinical presentation of individuals with schizophrenia or other psychotic disorders, because there is an inherent genetic relationship reflected by the selection criteria.
SPD can be assessed using the Schizotypal Personality Questionnaire (SPQ), a well-validated (Fonseca-Pedrero, Fumero, et al., 2014; Ortuño-Sierra et al., 2013; Raine, 1991) self-report measure modeled after the dichotomous diagnostic criteria outlined in DSM-III. Although specifically developed to assess SPD, the SPQ is suitable for the spectrum-based measure of select schizotypal traits. The nine characteristics assessed via Likert scale by the SPQ relate to core phenomena underlying the schizophrenia spectrum of disorders in DSM-5. For example, many items assess mild symptomatic features, such as “Some people find me a bit vague and elusive during a conversation.” Other items extend to more severe symptomatology, such as “I often hear a voice speaking my thoughts aloud.”
Research has pointed to schizotypy as an important transdiagnostic construct across a variety of psychotic disorders. Accordingly, individuals with schizophrenia and SPD and relatives of individuals with schizophrenia score higher on measures of schizotypy compared to nonpsychiatric controls (Camisa et al., 2005; Moreno-Izco et al., 2015), suggesting that the SPQ may reflect schizotypal features that manifest throughout the spectrum. Moreover, similarities across the schizophrenia spectrum exist on various measures of key biomarkers, neurological function and characteristics, and behavior/ability (Carpenter et al., 2009; Lui et al., 2018). Finally, common genetic risk factors exist for schizophrenia, SPD, and other psychotic disorders (Cadenhead & Braff, 2002; Vollema, Sitskoorn, Appels, & Kahn, 2002).
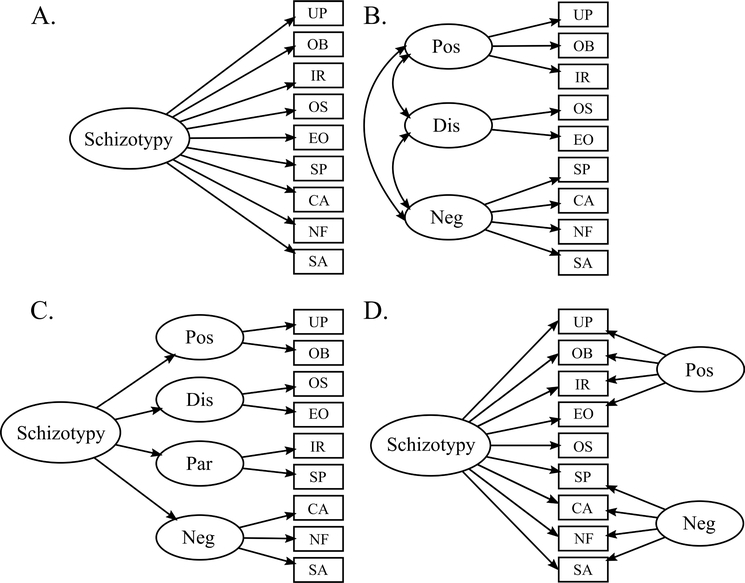
Spectrum-based approaches to understanding psychopathology have motivated efforts to identify general constructs (cf. Blonigen, Hicks, Krueger, Patrick, & Iacono, 2005; Caspi et al., 2014; Raine, 2006; Schürhoff, Laguerre, Szöke, Méary, & Leboyer, 2005; Sharp et al., 2015) that reflect a propensity to experience an array of phenomenological features (Kotov et al., 2017; Krueger, 1999). Identifying a conceptually sound factor structure of the SPQ with psychometrically flexible properties provides a valuable conceptual framework for critically understanding latent construct(s). Many studies have derived SPQ factor structures describing clustering of nine subscales of schizotypy into broader symptom categories. Four types of models have been implemented: unidimensional, correlated, hierarchical (second-order), and bifactor models. These models instantiate different conceptualizations of the structure likely embedded in these subscales (Figure 1).
FIGURE 1.
Model examples. A: Unidimensional, B: Correlated specific factors, C: Hierarchical, D: Bifactor; Schizotypy = general schizotypy factor, Pos = positive symptom, Neg = negative symptoms, Dis = disorganized symptoms, Par = paranoid symptoms, UP = Unusual Perceptual Experiences, OB = Odd Beliefs or Magical Thinking, IR = Ideas of Reference, SP = Suspiciousness and Paranoia, CA = Inappropriate or Constricted Affect, NF = No Close Friends, SA = Excessive Social Anxiety, OS = Odd Thinking and Speech, EO = Odd or Eccentric Behavior.
Unidimensional models are attractive due to their parsimony and relation to traditional item response theory approaches. However, psychological measures with conceptual breadth are rarely consistent with the assumptions of a unidimensional model (Reise, Morizot, & Hays, 2007). For example, unidimensionality may be established for a specific feature of a psychological disorder, such as positive symptoms in schizotypy. Rarely, though, can unidimensionality be established for the more general construct, which is often the primary focus of the measure. No study to date has found good model fit for a unidimensional model of the SPQ (Fonseca-Pedrero, Compton, et al., 2014; Fonseca-Pedrero, Debbane, et al., 2018; Reynolds, Raine, Mellingen, Venables, & Mednick, 2000; Stefanis et al., 2004).
Correlated models (Figure 1B) have been the most popular for analysis of the SPQ. Correlated factor models allow a measure to be parsed into meaningful correlated specific factors. Originally, two-factor correlated models were proposed for the SPQ and included a positive and a negative factor, identified in a sample of 29 White twin pairs (Kendler et al., 1991). The most well-studied are three or four specific factor-correlated models (Compton, Goulding, Bakeman, & McClure-Tone, 2009; Fonseca-Pedrero, Compton, et al., 2014; Stefanis et al., 2004). The correlated three-factor model initially proposed by Raine and colleagues (1994) was derived from 822 undergraduates and 102 community members. This model, consisting of cognitive-perceptual, interpersonal, and disorganized specific factors, replicated across demographic variables, including psychopathology, culture, and gender, in 1,201 individuals from Mauritius (Reynolds et al., 2000) and replicated across age in a sample of 352 Australians (Badcock & Dragović, 2006). Moreover, the model generalized to a schizophrenia sample (Rossi & Daneluzzo, 2002). Other three-factor models have been proposed, typically consisting of positive, interpersonal, and a disorganized or paranoid factor (Wuthrich & Bates, 2006). Correlated four-factor models, like that identified by Stefanis and colleagues (2004) in 2,243 Greek conscripts, include negative, positive, paranoid, and disorganized symptoms. In a sample of 1,445 undergraduates, Gross, Mellin, Silvia, Barrantes-Vidal, and Kwapil (2014) identified the Stefanis four-factor model in a confirmatory factor analysis (CFA), but in an exploratory factor analysis (EFA) a two-factor model was identified as the best-fitting model. In some models, when the disorganized factor is not present, subscales such as odd/eccentric beliefs and speech tend to group in the positive or interpersonal factor or not load on any factor (Stefanis et al., 2004). Despite substantial conceptual benefits and empirical support for correlated factor models, their psychometric properties are problematic because they do not preserve the readily interpretable conceptual relationship between subscales and the primary construct assessed by the measure. This creates practical concerns, including limited justification for use of total scores often used in the literature (cf. Badcock & Dragović, 2006; Bora & Baysan Arabaci, 2009; Daneluzzo, Bustini, Stratta, Casacchia, & Rossi, 1998; Park & McTigue, 1997; Raine, 1992; Yaralian et al., 2000), and theoretical concerns, elaborated below.
Hierarchical (second-order) models provide an extension of correlated models by characterizing the correlations between specific factors. However, much like correlated factor models, the relationships to the primary construct and subscales are obscured. Furthermore, in hierarchical models and correlated factor models, model associations may be biased by unspecified relationships between the general factor and indicators. This creates major theoretical concerns. Researchers may be more likely to identify minor “nuisance” factors as meaningful specific factors, possibly due to superficial features such as item presentation, because such factors contain substantial variance due to the general construct (Chen, West, & Sousa, 2006; Reise et al., 2007). Much like the unidimensional model, little to no support has been found for hierarchical models of the SPQ (Compton et al., 2009; Preti et al., 2015).
More recently, a study by Preti and colleagues (2015) identified a bifactor model (Figure 1D) as the best factor structure fit for the SPQ in a sample of 649 college students. Specifically, a two-factor bifactor model composed of negative (Excessive Social Anxiety, No Close Friends, Inappropriate or Constricted Affect) and positive (Ideas of Reference, Odd Beliefs or Magical Thinking, Unusual Perceptual Experiences, Odd or Eccentric Behavior, Odd Thinking and Speech, Suspiciousness and Paranoia) subfactors exhibited better fit than the best corresponding correlated and hierarchical models, although the Stefanis four-factor model (correlated and hierarchical) also exhibited acceptable fit (Preti et al., 2015). Bifactor models (Cai, Yang, & Hansen, 2011; Gibbons et al., 2007) allow subscales (e.g., Ideas of Reference) to load on both a primary dimension, in this case schizotypy, and one specific subfactor. For example, the subscale “unusual perceptions” has loadings on the latent schizotypy general factor and simultaneously the “positive symptoms” specific factor, but not the “negative symptoms” specific factor (Figure 1D and Figure 2). This provides valuable information about which subscales are most indicative of general schizotypy severity, while other subscales may be more indicative of severity within a specific factor of symptoms. Moreover, unlike correlated and hierarchical models, bifactor models allow investigators to parse out variance due to the general factor versus variance due to the specific factor of interest for each subscale. As identified by Gross and colleagues (2014), high correlation between factors on the SPQ brings into question whether these factors are distinct and, accordingly, poses difficulty in understanding which real-world constructs these factors may be tapping. The bifactor approach allows for better evaluation of the validity of subscales and increases the predictive specificity of factor scores related to specific factors (Chen et al., 2006; Reise, 2012). Thus, researchers can theoretically link constructs (specific factors, e.g., negative symptoms) with outside criteria of interest (e.g., neurobiological or psychosocial measures) while controlling for the effect of the general construct. Recently, some researchers have expressed concerns about the flexibility of bifactor models, stating that generalizability of identified specific factors may be limited (Bonifay, Lane, & Reise, 2017). Despite these criticisms, support for a similar bifactor structure of the SPQ has been shown across recent studies (Fonseca-Pedrero, Ortuño, et al., 2018; Fonseca-Pedrero et al., 2017; Preti et al., 2015).
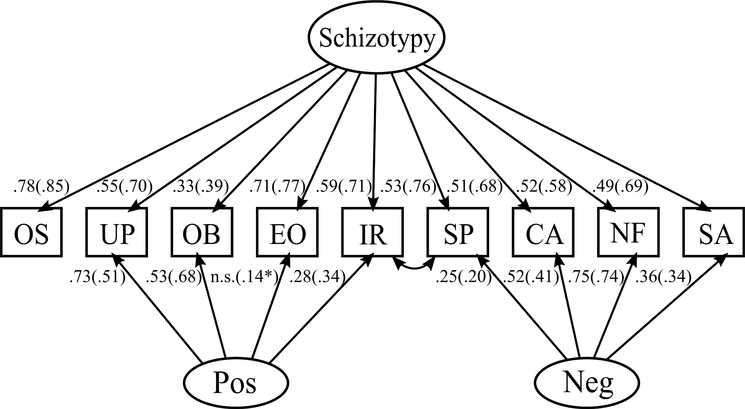
FIGURE 2.
Two specific-factor bifactor model path diagram. Standardized loadings of the control group (outside parentheses) and schizophrenia-spectrum group (inside parentheses). Loadings are directly to the left of their respective pathways. Schizotypy = general schizotypy factor, Pos = positive symptom specific factor; Neg = negative symptom specific factor, UP = Unusual Perceptual Experiences, OB = Odd Beliefs or Magical Thinking, IR = Ideas of Reference, SP = Suspiciousness and Paranoia, CA = Inappropriate or Constricted Affect, NF = No Close Friends, SA = Excessive Social Anxiety, OS = Odd Thinking and Speech, EO = Odd or Eccentric Behavior. *p < .01, n.s. = not significant path and therefore not included in the model for that group. All other paths not specified are significant at p < .001.
In addition to the study by Preti and colleagues (2015), only one other previous study has assessed a bifactor model of the SPQ. Fonseca-Pedrero and colleagues (Fonseca-Pedrero et al., 2017; Fonseca-Pedrero, Debbane, et al., 2018) found acceptable model fit for a three-specific factor (i.e., cognitive/perceptual, interpersonal, disorganized) bifactor model in a sample of 27,001 nonpsychiatric controls from colleges and the general population of 21 independent sites spanning 12 countries, although three-factor and four-factor hierarchical models were determined to have the best fit. Cultural measurement invariance suggested that schizotypy is not solely a cultural or environmental phenomenon.
In sum, correlated factor models partition variation of subscales into conceptually distinct factors, leaving only an implicit relationship to a general construct in the model. However, evidence and practice support schizotypy as an overarching construct. Accordingly, hierarchical and bifactor models include a general schizotypy factor to explain covariation reflective of a common construct underlying variation in all SPQ subscales. A major conceptual difference is that bifactor models do not presuppose that the general schizotypy factor manifests its influence onto subscales only indirectly by bifurcating into specific factors. Rather, the general factor in a bifactor model specifies that variation of subscales is directly reflective of the general construct in tandem with other orthogonal specific factors contributing to variation within subscales (Yung, Thissen, & McLeod, 1999).
The current study evaluated competing continuous unidimensional (Figure 1A), correlated (Figure 1B), hierarchical (Figure 1C), and bifactor (Figure 1D) models of the SPQ in a group consisting of only those diagnosed with SPD or a psychosis spectrum disorder (schizophrenia, schizoaffective disorder), from this point on referred to as the “schizophrenia-spectrum” group; a healthy, nonpsychiatric control group; and the full sample. Most previous studies have been constrained by fairly homogeneous subject samples, which can bias resulting factor structures. Stefanis and colleagues (2004) noted that most studies suffer from small sample sizes and include either healthy controls or a single diagnosis (e.g., only schizophrenia). Close examination of the merits of these models in the present study, as well as use of a sample spanning the schizotypy spectrum, provides a valuable framework into the utilization of the SPQ as a measure and the theoretical representation of the schizotypy construct.
METHODS
SAMPLE CHARACTERISTICS
Participants for this study were healthy controls or stable, local outpatients recruited within the Greater Bloomington and Indianapolis Areas by flyers and advertisements in local newspapers and buses. All procedures were approved by the Indiana University Institutional Review Board. Written, informed consent was obtained, and analyses were performed on a sample of 627 individuals. The current study included (a) 335 nonpsychiatric individuals and (b) 292 individuals with a psychiatric diagnosis on the schizophrenia spectrum, including a formal diagnosis of schizophrenia, schizoaffective disorder, or SPD (Table 1). The control group contained individuals with no formal Axis I or Axis II diagnoses. The schizophrenia-spectrum group was formed according to literature suggesting genetic and phenomenological links between schizophrenia, affective psychoses (Shevlin, McElroy, Bentall, Reininghaus, & Murphy, 2017) and SPD (Cadenhead & Braff, 2002).
TABLE 1.
Participant Demographics
| Control (n = 335) | Spectrum (n = 292) | Full Sample (N = 627) | Statistics (t or χ2) † | p value † | |
|
| |||||
| Sex (male/female) | 155/180 | 178/114 | 333/294 | 13.52 | < .01 |
| Ethnicity (C/A/H/O) | 214/97/5/19 | 118/150/7/17 | 332/247/12/36 | 40.66 | < .01 |
| Age (years; M [SD]) | 36.77 (11.46) | 38.20 (10.90) | 37.44 (11.21) | −1.60 | ns |
| Education (years; M [SD]) | 14.86 (2.88) | 13.05 (7.13) | 13.91 (5.59) | 3.604 | < .001 |
| Diagnoses (%) | SZ (58.6) | SZ (27.3) | |||
| SZAff (20.9) | SZAff (9.7) | ||||
| SPD (20.5) | SPD (9.6) | ||||
| Control (53.4) | |||||
| M (SD) | M (SD) | M (SD) | |||
|
| |||||
| SPQ Total Score | 12.09 (10.47) | 36.32 (17.84) | 23.38 (18.78) | −20.35 | < .01 |
| Ideas of Reference | 1.26 (1.88) | 4.54 (3.00) | 2.79 (2.96) | −16.10 | < .01 |
| Social Anxiety | 1.98 (2.10) | 4.39 (2.65) | 3.10 (2.66) | −12.50 | < .01 |
| Odd Beliefs | 0.81 (1.38) | 2.85 (2.32) | 1.76 (2.13) | −13.16 | < .01 |
| Unusual Perceptions | 0.98 (1.58) | 4.11 (2.73) | 2.44 (2.69) | −17.24 | < .01 |
| Odd Behavior | 1.01 (1.58) | 3.38 (2.35) | 2.12 (2.30) | −14.61 | < .01 |
| No Close Friends | 1.51 (1.94) | 4.72 (2.74) | 3.00 (2.84) | −16.67 | < .01 |
| Odd Speech | 1.89 (2.04) | 4.36 (2.87) | 3.04 (2.75) | −12.28 | < .01 |
| Constricted Affect | 1.52 (1.53) | 3.59 (2.09) | 2.49 (2.08) | −13.98 | < .01 |
| Suspiciousness/Paranoia | 1.13 (1.61) | 4.37 (2.76) | 2.64 (2.75) | −17.67 | < .01 |
Note.
Comparison between control and schizophrenia-spectrum groups.
Italic text indicates a significant difference between groups. C = Caucasian; A = African American; H = Hispanic; O = Other; ns = not significant; SZ = schizophrenia; SZAff = schizoaffective disorder; SPD = schizotypal personality disorder; Spectrum = schizophrenia-spectrum.
ASSESSMENT
Participants were evaluated with a battery of diagnostic assessments to determine eligibility and characterize symptomatology. The SCID-I and SCID-II interviews were administered (First, Benjamin, Gibbon, Spitzer, & Williams, 1997; First, Spitzer, Gibbon, & Williams, 2002). Participants reporting a history of psychotic symptoms were administered the SCID-I/P (Patient Version), whereas healthy controls were administered the SCID-I/NP (Non-Patient Version) and SCID-II Cluster A Personality Disorders section to confirm absence of current psychiatric diagnoses and the Family Interview for Genetic Studies (FIGS; Maxwell, 1992) to confirm no familial history of a psychotic disorder. SCID-I sections for mood disorders, psychotic disorders, and substance use disorders were administered to persons within the psychotic spectrum. For the SCID-II, only the sections for paranoid personality disorder, SPD, schizoid personality disorder, and antisocial personality disorder were administered. In addition, subjects were administered the anxiety sections from the Mini International Neuropsychiatric Interview (MINI; Lecrubier et al., 1997). Although anxiety disorders were not the focus of this study, the MINI allowed for efficient assessment of anxiety disorders and symptomatology for the purpose of participant exclusion for such comorbidities without the time-intensive detail like that gathered though the SCID.
Participants also completed the 74-item SPQ (Raine, 1991), which captures the nine subcategories of the disorder outlined in the DSM: Odd Beliefs or Magical Thinking, Unusual Perceptual Experiences, Ideas of Reference, Suspiciousness and Paranoia, Inappropriate or Constricted Affect, Odd or Eccentric Behavior, No Close Friends, Excessive Social Anxiety, Odd Thinking and Speech (see Appendix Table A1 for subscale content). Valid responses were “yes” or “no,” with “yes” indicating endorsement of experiences or symptomatology. Of an originally recruited sample of 717 individuals, 90 individuals (12.6% of the original sample) were excluded for incomplete questionnaires due to invalid responding (i.e., written in responses, missing response) leaving a total sample of 627 individuals included in analyses. No significant differences in sex or years of education were present between those included and excluded in the analyses.
STATISTICAL ANALYSES AND INTERNAL CONSISTENCY RELIABILITY
R version 3.4.0 was used for all analyses (R Core Team, 2014), with the exception of bifactor-specific indices, including utilization of the “psych” package for computation of Ordinal alpha (Zumbo, Gadermann, & Zeisser, 2007) and Cronbach’s alpha (Revelle, 2017), and the “lavaan” package CFA confirmatory factor analysis and factor score calculation using the regression method (Rosseel, 2011). Bifactor-specific indices were calculated using a Microsoft Excel–based tool (Dueber, 2017).
Scale reliability was measured using Ordinal alpha. For group comparisons, alpha values greater than 0.70 are considered satisfactory when assessing subscales derived from a single measure (Nunnally, 1967).
ITEM-LEVEL CONFIRMATORY FACTOR ANALYSIS
The item-level nine-subscale structure of the SPQ was confirmed separately in the full sample (i.e., nonpsychiatric control and schizophrenia-spectrum) and subsamples. This step justifies using summed subscales for subsequent analyses. Item-level CFA was modeled with the “lavaan” package utilizing the diagonally weighted least squares estimator (WLSMV). This estimator is commonly used for ordered categorical data (Brown, 2014), such as dichotomous items. Adequate model fit is reflected by a root mean square error of approximation (RMSEA) < 0.08 and comparative fit index (CFI) and Tucker-Lewis fit index (TFI) > 0.94 (Bentler & Bonett, 1980; Browne & Cudeck, 1992; Hu & Bentler, 1999).
SUBSCALE-LEVEL CONFIRMATORY FACTOR ANALYSIS
Given their wide support in the literature, the Stefanis four-factor correlated model and the Raine three-factor correlated model were used as templates to fit the models of highest dimensionality. Although both models allow subscales to cross-load onto multiple latent factors, the current study did not allow cross-loading in an effort to increase interpretability and comparison across tested models. Accordingly, the four-factor model in the current study (see Figure 1C, hierarchical form) was identical to that of Stefanis and colleagues (2004), except Excessive Social Anxiety was solely an indicator of the Negative factor and Suspiciousness and Paranoia was solely an indicator of the Paranoid factor. The three-factor model tested was nearly identical to the Raine (Raine et al., 1994) model, except Suspiciousness and Paranoia was solely an indicator of the Negative factor (Figure 1B). Due to the inconclusiveness in the current literature regarding the loading of Suspiciousness and Paranoia and the difficulty of interpretation of cross-loading within a bifactor model, Suspiciousness and Paranoia was placed in the negative factor due to the relationship of these items to interpersonal pathology, which more closely relates to the content of this factor.
The full sample, control group, and schizophrenia-spectrum group were all fitted, using the “lavaan” package utilizing maximum likelihood estimation, with seven models: unidimensional; two-, three-, and four-factor correlated; three- and four-factor hierarchical; and two-specific factor bifactor models. Models including latent factors with only two indicators and no association to another factor (e.g., two-factor hierarchical, three- and four-specific factor bifactor models) are not identified. Therefore, all combinations of specific factors and model-type could not be estimated.
Adequate model fit was assessed using the RMSEA, CFI, TFI, and chi-square test statistic. Ideally, a nonsignificant chi-square indicates excellent fit, but it is important to note that this is difficult to achieve in studies with larger sample sizes (N > 200), even when a model has exceptional fit based on other indices (Brown, 2014). Bayesian Information Criteria (BIC) were utilized for model comparisons, which is a useful measure of model fit that stresses parsimony by penalizing models that are more complex. Models with lower BIC values should be preferred, with BIC differences of 0–2 showing weak evidence, 2–6 showing positive evidence, 6–10 showing strong evidence, and difference of >10 indicating very strong evidence in favor of the model with lower value (Raftery, 1995).
Recent studies have shown that traditional CFA fit statistics can be biased toward bifactor models (Greene et al., 2019; Morgan, Hodge, Wells, & Watkins, 2015), making additional information to compare tested models necessary. Accordingly, EFA was used to examine the loading patterns between correlated factor models and number of extracted factors based on CFA results, using both a “promax” rotation (i.e., correlated factors) and a bifactor rotation (Jennrich & Bentler, 2011). In this approach, the bifactor model is simply a rotation of the correlated model allowing for a useful comparison.
BIFACTOR INDICES
Three fit indices were selected to further assess the contribution of factors within the fitted bifactor model: (a) explained common variance (ECV), the proportion of all common variance explained by the general factor (Andreasen et al., 1994); (b) percent of uncontaminated correlations (PUC), representing the percentage of covariance terms that only reflect variance from the general dimension; and (c) individual explained common variance (IECV; Cohen & Davis, 2009), representing the extent to which a subscale’s responses are accounted for by variation in the latent general dimension alone (Rodriguez, Reise, & Haviland, 2016; Stucky, Thissen, & Orlando Edelen, 2013).
RESULTS
Demographic characteristics of the samples are shown in Table 1.
INTERNAL CONSISTENCY RELIABILITY
The nine subscales of the SPQ showed excellent reliability with Ordinal alpha values for the total measures of 0.99, 0.93, and 0.97 in the full sample, the control group, and the schizophrenia-spectrum group, respectively (see Appendix Table A2 for subscale Ordinal and Cronbach’s alpha).
ITEM-LEVEL CFA OF NINE-SUBSCALE STRUCTURE
Item-level CFA, which was consistent with the nine-subscale structure of the SPQ, fit the data well, χ2(with corrected robust estimation) = 4298.39 (df = 2591), p < .001, CFI = 0.96, TFI = 0.96, RMSEA = 0.032, supporting the use of the nine summed subscales in subsequent analyses. The nine-subscale structure also fit adequately in the control group, χ2 = 2966.405 (df = 2591), p < .001, CFI = 0.94, TFI = 0.94, RMSEA = 0.021, and the schizophrenia-spectrum group, χ2 = 3495.203 (df = 2591), p < .001, CFI = 0.94, TFI = 0.93, RMSEA = 0.035.
SUBSCALE-LEVEL CFA MODEL COMPARISONS
The two-specific factor bifactor model achieved acceptable model fit in the full sample, the control group, and the schizophrenia-spectrum group (Table 2, Figure 2). It is important to note that in the control group the Odd or Eccentric Behavior and Odd Thinking and Speech subscales did not load onto a specific factor, and loaded only onto the general schizotypy factor (Table 3, Figure 2); accordingly, those factors were dropped from the model. Conversely, in the full sample and the schizophrenia-spectrum group, there was a significant path from the Odd or Eccentric Behavior subscale to the positive symptom factor in the two-specific factor bifactor model, and thus it was included in the model (Figure 2). The two-specific factor bifactor model had very strong support as assessed by the BIC statistic with a BIC difference > 10 between the two-specific bifactor model and all other models fitted in each sample (Table 2). Modification indices indicated that the greatest source of misfit was covariation of residual variance of the Ideas of Reference and Suspiciousness and Paranoia subscales. Consequently, to achieve acceptable model fit, the residuals of the Ideas of Reference and Suspiciousness and Paranoia subscales were allowed to covary in all models that did not include a specific paranoid factor consisting of these subscales.
TABLE 2.
Model Fit Indices
| Specific Factors | Model | CFI | TFI | RMSEA | BIC | χ2 (df) |
|---|---|---|---|---|---|---|
| Control | (n = 335) | |||||
|
| ||||||
| U | .713 | .617 | .193 | 11 082.73 | 362.78 (27) | |
| Pos/Neg | C | .880 | .827 | .130 | 10 897.08 | 165.51 (25) |
| Pos/Neg/Dis | C | .937 | .902 | .098 | 10 839.49 | 96.28 (23) |
| Pos/Neg/Dis/Par | C | .949 | .913 | .092 | 10 834.85 | 80.01 (21) |
| Pos/Neg/Dis | H | .937 | .902 | .098 | 10 839.50 | 96.28 (23) |
| Pos/Neg/Dis/Par | H | .930 | .891 | .103 | 10 847.57 | 104.37 (23) |
| Pos/Neg | B | .976 | .954 | .067 | 10 813.76 | 47.30 (19) |
|
| ||||||
| Schizophrenia-Spectrum | (n = 292) | |||||
|
| ||||||
| U | .802 | .736 | .203 | 11 237.07 | 352.45 (27) | |
| Pos/Neg | C | .903 | .860 | .148 | 11 080.47 | 184.50 (25) |
| Pos/Neg/Dis | C | .937 | .902 | .124 | 11 033.06 | 125.74 (23) |
| Pos/Neg/Dis/Par | C | .936 | .890 | .131 | 11 045.40 | 126.72 (21) |
| Pos/Neg/Dis | H | .937 | .902 | .124 | 11 033.07 | 125.74 (23) |
| Pos/Neg/Dis/Par | H | .925 | .883 | .135 | 11 053.14 | 145.81 (23) |
| Pos/Neg | B | .989 | .977 | .060 | 10 972.42 | 36.71 (18)* |
|
| ||||||
| Full sample | (N = 627) | |||||
|
| ||||||
| U | .850 | .800 | .198 | 22 926.63 | 691.05 (27) | |
| Pos/Neg | C | .929 | .897 | .142 | 22 590.38 | 341.92 (25) |
| Pos/Neg/Dis | C | .952 | .925 | .121 | 22 497.17 | 235.82 (23) |
| Pos/Neg/Dis/Par | C | .963 | .937 | .111 | 22 458.53 | 184.31 (21) |
| Pos/Neg/Dis | H | .952 | .925 | .121 | 22 497.17 | 235.82 (23) |
| Pos/Neg/Dis/Par | H | .955 | .929 | .118 | 22 485.82 | 224.47 (23) |
| Pos/Neg | B | .988 | .975 | .069 | 22 365.26 | 71.72 (18) |
Note. CFI = comparative fit index; TFI = Tucker-Lewis index; RMSEA = root mean square error approximation; BIC = Bayesian information criteria; U = unidimensional; C = correlated; H = hierarchical; B = bifactor; Pos = positive symptom; Neg = negative symptoms; Dis = disorganized symptoms; Par = paranoid symptoms; χ2 = p < .001.
p < .01.
TABLE 3.
Factor Loadings for Unidimensional, Correlated Factor Models, and Hierarchical Models
| Model | UP | OB | IR | SP | CA | NF | SA | OS | EO | 2nd order | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Uni | .58 (.73) | .38 (.46) | .73 (.81) | .71 (84) | .64(.72) | .67(.67) | .56(.72) | .63(.78) | .59(.73) | - | |
|
| |||||||||||
| Corr. 2 | Pos | .71 (80) | .51 (.56) | .64 (.77) | .67(.79) | .64(.78) | - | ||||
| Neg | .58 (.79) | .76(.81) | .84(.79) | .61(.78) | - | ||||||
|
| |||||||||||
| Corr. 3 | Pos | .86 (.87) | .62 (.64) | .58 (.77) | - | ||||||
| Neg | .49 (.77) | .76(.80) | .84(.79) | .62(.77) | - | ||||||
| Dis | .78(.86) | .73(.80) | - | ||||||||
|
| |||||||||||
| Corr. 4 | Pos | .91 (.95) | .62 (.65) | - | |||||||
| Neg | .76(.82) | .84(.81) | .63(.79) | - | |||||||
| Dis | .78(.86) | .73(.80) | - | ||||||||
| Par | .88 (.86) | .77 (.88) | - | ||||||||
|
| |||||||||||
| Hier. 3 | Pos | .86 (.87) | .62 (.64) | .58 (.77) | .68(.84) | ||||||
| Neg | .49 (.77) | .76(.80) | .84(.79) | .62(.77) | .67(.85) | ||||||
| Dis | .78(.86) | .73(.80) | .96(.98) | ||||||||
|
| |||||||||||
| Hier. 4 | Pos | .97 (1.01) | .59 (.61) | .65(.73) | |||||||
| Neg | .76(.82) | .84(.81) | .63(.79) | .70(.83) | |||||||
| Dis | .78(.85) | .73(.80) | .80(.91) | ||||||||
| Par | .87 (.86) | .77 (.89) | .84(.92) | ||||||||
Note. Standardized factor loadings of control group (outside parentheses) and schizophrenia-spectrum group (inside parentheses). UP = Unusual Perceptual Experiences; OB = Odd Beliefs or Magical Thinking; IR = Ideas of Reference; SP = Suspiciousness and Paranoia; CA = Inappropriate or Constricted Affect; NF = No Close Friends; SA = Excessive Social Anxiety; OS = Odd Thinking and Speech; EO = Odd or Eccentric Behavior; Uni = unidimensional; Corr. = correlated factor model; Hier = hierarchical factor model; Pos = positive symptom; Neg = negative symptoms; Dis = disorganized symptoms; Par = paranoid symptoms; 2nd order = specific factors loading on the second order general schizotypy factor. All loadings significant at p < .001.
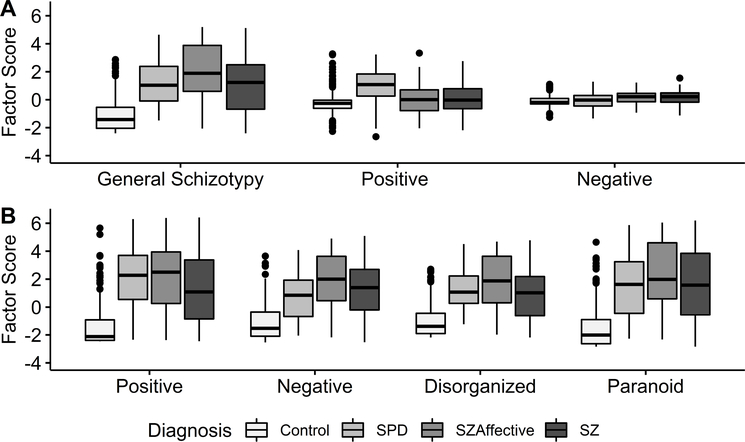
To better understand the utility of the models of interest, a post hoc qualitative (Figure 3, Table 4) comparison of factor scores generated from the two-specific factor bifactor and four-factor correlated models was performed.
FIGURE 3.
Box plot of factor scores across diagnostic groups. Distribution of factors scores from (A) the two-specific factor bifactor model and (B) the four-factor correlated model. SPD = Schizotypal Personality Disorder, SZAffective = Schizoaffective, SZ = Schizophrenia.
TABLE 4.
Factor Score Descriptive Statistics by Group
| Control | SPD | SZAffective | SZ | |
|---|---|---|---|---|
| Factor Scores from Correlated Model | ||||
| Pos | −1.41 (1.41) | 2.02 (2.21) | 2.21 (2.63) | 1.27 (2.49) |
| Neg | −1.12 (1.27) | .81 (1.64) | 1.96 (1.94) | 1.22 (1.93) |
| Dis | −1.04 (1.11) | 1.28 (1.46) | 1.82 (1.88) | .93 (1.85) |
| Par | −1.52 (1.42) | 1.51 (2.25) | 2.39 (2.50) | 1.60 (2.55) |
| Factor Scores from Bifactor Model | ||||
| Schiz | −1.13 (1.16) | 1.22 (1.61) | 2.02 (2.00) | 1.07 (2.00) |
| Pos | −0.22 (0.75) | 0.88 (1.28) | −0.01 (1.09) | 0.13 (1.01) |
| Neg | −0.10 (0.37) | −0.08 (0.58) | 0.14 (0.47) | 0.17 (0.45) |
Note. Means (and standard deviations) of factor scores. Pos = Positive; Neg = Negative; Dis = Disorganized; Par = Paranoid; Schiz = general schizotypy factor; SPD = Schizotypal Personality Disorder; SZAffective = Schizoaffective Disorder; SZ = Schizophrenia.
EXPLORATORY FACTOR ANALYSIS
Given that the best-fitting correlated factor model was the four-factor model, a four-factor EFA was conducted with both a promax and a bifactor rotation using the full sample (Appendix Table A3). This model fit the data very well, χ2(6) = 5.46, p = .48. The promax rotation recovered essentially the same model as the CFA four-factor correlated model with Positive, Negative, Disorganized, and Paranoid factor Eigen values of 1.32, 2.48, 1.61, and 1.40, respectively. The bifactor rotation included a general factor and negative, disorganized, and paranoid specific factors with Eigen values of 5.78, 0.75, 0.43, and 0.38, respectively. Importantly, the general factor in the bifactor rotation accounted for 61% of the variance, resembling the cumulative variance from the first three factors in the promax rotation. Furthermore, the loadings on the general factor in the bifactor model were all quite robust (0.68–0.84).
BIFACTOR INDICES
ECV and PUC > 0.70 suggest that the model is clearly saturated by a strong general factor and could be modeled as unidimensional with only slight bias (Rodriguez et al., 2016). Bifactor indices indicated the presence of a strong general factor as shown by ECV = 0.80 and PUC = 0.67.
A subscale(s) with IECV > 0.85 may be interpreted to assess the latent general construct almost exclusively. IECV estimations indicated substantial differences between subscales in the amount of variation attributed to the general schizotypy factor alone. IECV estimation for each subscale was Odd Beliefs or Magical Thinking = 0.47, Unusual Perceptual Experiences = 0.74, Ideas of Reference = 0.90, Suspiciousness and Paranoia = 0.95, Inappropriate or Constricted Affect = 0.78, Odd or Eccentric Behavior = 0.99, No Close Friends = 0.57, Excessive Social Anxiety = 0.85, and Odd Thinking and Speech = 0.99. This signifies that the general schizotypy factor accounts for the vast majority of variation within some subscales (e.g., Odd or Eccentric Behavior and Odd Thinking and Speech) while accounting for only about half the variation within others (e.g., Odd Beliefs or Magical Thinking).
DISCUSSION
The current study examined the factor structure of the SPQ in a large, diagnostically heterogeneous sample to uncover the best model fit and evaluate the conceptual advantages of the models assessed. Only two studies have previously assessed the bifactor model structure of the SPQ, which has conceptual, theoretical, and psychometric advantages to previously studied unidimensional, correlated, and hierarchical models. The current study is unique because participants spanned the schizophrenia spectrum, ranging from attenuated symptom severity and functional impairment in SPD to more significant symptoms and functional impairment in schizophrenia, and also included a nonpsychiatric control group.
Broadly, the current findings support the use of a bifactor model to describe the factor structure of the SPQ, similar to Preti and colleagues (2015), supporting a general construct linking traits across the psychosis spectrum. As in the current study, the nine subscales of the SPQ (Figure 2) were moderate to strong indicators of the general schizotypy factor. The superior fit of the bifactor model in comparison to the hierarchical model indicates that variation in SPQ subscales is saturated by a coherent general construct (schizotypy). Similarly, specific subscales within the measure are also saturated by specific factors (i.e., positive, negative) that are not correlated with the general factor (Krueger, Markon, Patrick, Benning, & Kramer, 2007). Finally, bifactor indices support the conceptualization of a strong general factor underlying variation within the SPQ and responding across diagnostic groups; however, this strong general factor may indicate that the generalizability of specific factors in such models should continue to be evaluated.
Evaluating broader clinical correlates in future studies may provide insight into the meaning of this general schizotypy factor. In the current study, general factor scores were elevated across all diagnostic groups (Figure 3A, Table 4) compared to other bifactor subfactors. This qualitative finding lends support to a shared underlying feature of psychosis spectrum disorders that is distinct from other features (i.e., positive and negative, which exhibited different diagnostic factor score patterns). In contrast, the four-factor correlated model (Figure 3B) reflected a consistent diagnostic pattern across all factors, indicating that the correlated model does a poor job specifically accounting for this general feature compared to the bifactor. Moreover, the discrepancy in variance accounted for by these two models (Appendix Table A3) garners support for the importance of a general factor within the SPQ.
Taken together, this provides support for a general unifying construct. However, it remains unclear in the current study, due to limited clinical dimensionality and measures of phenomenology, if the general factor is, in fact, general or related to schizotypy broadly. However, some evidence in the current study suggests that the general schizotypy factor identified from the bifactor model may reflect general severity. For example, evaluation of factor loadings between groups and across fitted models suggests that the general schizotypy factor has greater influence on SPQ variation in individuals of higher illness severity than nonpsychiatric controls (Table 3), which is further supported by higher general factor scores in the schizophrenia and schizoaffective groups. This is consistent with findings in the literature of general psychopathology risk or severity factors (Caspi & Moffitt, 2018; Lahey, Krueger, Rathouz, Waldman, & Zald, 2017).
The current findings are also consistent with existing models, suggesting the stability of these factor structures across samples. Within the current study, the three-factor correlated model, similar to the Raine model, had the best fit of correlated models in the schizophrenia-spectrum group (Table 2). The four-factor correlated model, similar to the Stefanis model, was the best-fitting correlated factor model in the control group and full sample (Table 2).
Consistent with Preti and colleagues (2015), the current study obtained adequate model fit and a readily interpretable model with two specific factors. This finding suggests that additional specific factors (e.g., disorganized symptoms) identified in other models may not be independent symptom clusters like positive and negative, but instead reflect common features imbedded within and better accounted for by the general schizotypy factor. For example, consistent with the findings from Preti and colleagues (2015), the subscales of Odd Thinking and Speech and Odd or Eccentric Behavior appear to be primarily measures of the broader schizotypy construct in both samples, with little residual variance accounted for by any specific subfactor. As assessed by the SPQ, disorganized symptomatology is seemingly a manifestation of increased general schizotypy symptomatology rather than any specific subfactor (e.g., positive or negative symptoms). Results from hierarchical models further support this conclusion. The disorganized latent variable was almost entirely explained by the general factor, because second-order factor loadings of the disorganized factor onto the schizotypy general factor were 0.96 and 0.98 for the control and schizophrenia-spectrum groups, respectively, in the three-factor hierarchical model. This provides valuable insight into the conceptualization of disorganized pathology. It seems more likely that disorganization as assessed by the SPQ is an indication of general schizotypy severity rather than a conceptually distinct cluster of specific symptoms/experiences.
Interestingly, in the current study and the study by Preti and colleagues (2015), the Odd Beliefs or Magical Thinking subscale was primarily a measure of the positive symptoms specific factor, while also having the lowest loading on the general schizotypy factor of any subscale (Figure 2). This observation is not readily interpretable from correlated and hierarchical models (Table 3), but it provides valuable insight into a more disparate process accounting for variation within the Odd Beliefs subscale separate from general schizotypy. Similarly, the No Close Friends subscale was a very strong indicator of the negative specific factor, as well as a strong indicator of the general schizotypy factor. These results provide guidance for utilizing individual subscales of the SPQ to link specific factors of schizotypy to other criteria of interest while controlling for the effect of the general schizotypy construct. Notably, in the current model, the Suspiciousness and Paranoia subscale loaded on the negative specific factor instead of the positive specific factor, as identified by Preti and colleagues (2015). Noteworthy is the factor structure of the SPQ determined in the current study in relation to identified structures of schizophrenia, including negative, positive, and disorganized symptomatology (Lenzenweger & Dworkin, 1996; Liddle, 1987). This striking similarity supports early conceptualizations of schizotypy and its relation to the schizophrenia spectrum (Cicero et al., 2019; Grant et al., 2018; Kendler, 1985) and may further explain the similarities in external indicators such as biomarkers, neural correlates, and behavioral performance across diagnoses (Carpenter et al., 2009; Lenzenweger & Loranger, 1989; Meehl, 1962). Going forward, the bifactor structure identified in the current study will be useful, particularly for a Research Domain Criteria (RDoC) framework, to link these constructs that seem to span symptomatology with external criteria and measures.
Limitations of the present study must be noted. First, the schizophrenia-spectrum group contains an overrepresentation of individuals with schizophrenia compared to other psychotic disorders and, further, does not extend to other clinical dimension of psychopathology. This study suffers from selection bias because the schizophrenia participants were stable outpatients, thus narrowing the upper range of symptom severity. Second, although this study assessed a noteworthy range of the schizotypy spectrum, the use of the SPQ as a reflection of this construct narrowed the extent of “schizotypy” that could be assessed because SPD, for which the SPQ was developed, only describes a subset of schizotypal phenomenology. Third, in all models without a paranoid-specific factor, the residual variances of the Ideas of Reference and Suspiciousness and Paranoia subscales were allowed to covary. This suggests that there is residual similarity in these subscales that is not accounted for by the general factor. It is possible this observed covariation is a result of superficial similarities of items across scales, which appear to exist within items across the Ideas of Reference and Suspiciousness and Paranoia subscales of the SPQ (e.g., Item 9 in the Suspiciousness and Paranoia subscale, “I am sure I am being talked about behind my back,” and Item 63 in the Ideas of Reference subscale, “Do you sometimes feel that people are talking about you?”). The current study was unable to fit a bifactor model with the inclusion of this latent factor because it comprised only two subscales.
Future work may benefit from a larger sample size for multigroup modeling and comparison of continuous and discontinuous latent structures of schizotypy (Andreasen et al., 1994). Although the current study suggests a similar latent structure, higher scale variances (4–20×) in the schizophrenia-spectrum group compared to the control group (Table 1) and differences in CFA parameter estimates (Figure 2) suggest that the prospect of meaningful measurement invariance across groups may be low. Measurement invariance has not yet been evaluated for the SPQ across clinically distinct samples, but it may provide a promising future direction. Similarly, the current study evaluated only continuous models of schizotypy, although direct comparison of discontinuous model alternatives would provide important insights into the construct of schizotypy. Finally, a promising extension of this work would be to explicitly examine the utility of a bifactor model in predicting external criteria of interest compared to more traditional models.
CONCLUDING REMARKS
The current findings support a bifactor structure to describe the SPQ, which lends itself to the RDoC model for the study of schizotypy as a continuum through mild to severe schizophrenia-related experiences and traits. This study further demonstrates the ability of the SPQ to simultaneously capture variation of primary and specific (positive and negative) dimensions of schizotypy, permitting future, rigorous validation against external constructs.
Acknowledgments
We wish to thank the patients and their families for participation in this study as well as the support of the staff and administration of Larue D. Carter Memorial Hospital (Indianapolis, IN). This work was supported by the National Institutes of Health (grant number T32 MH103213 to W.P.H. and A.B.M.; R01 MH074983 to W.PH.; T32 DA024628 to A.J.B.; Indiana Clinical and Translational Sciences Institute award TL1 TR001107 and UL1 TR001108 to A.B.M.; and R21 MH091774 to B.F.O.); and the Brain and Behavior Research Foundation (NARSAD Young Investigator Award to A.R.B.).
APPENDIX
TABLE A1.
SPQ Items
| Odd Beliefs or Magical Thinking | |
|
| |
| 3 | Have you had experiences with the supernatural? |
| 12 | Do you believe in telepathy (mind-reading)? |
| 21 | Are you sometimes sure that other people can tell what you are thinking? |
| 30 | Do you believe in clairvoyancy (psychic forces, fortune telling)? |
| 39 | Can other people feel your feelings when they are not there? |
| 47 | Have you had experiences with astrology, seeing the future, UFOs, ESP, or a sixth sense? |
| 55 | Have you ever felt that you are communicating with another person telepathically (by mind-reading)? |
|
| |
| Unusual Perceptual Experiences | |
|
| |
| 4 | Have you often mistaken objects or shadows for people, or noises for voices? |
| 13 | Have you ever had the sense that some person or force is around you, even though you cannot see anyone? |
| 22 | When you look at a person or yourself in a mirror, have you ever seen the face change right before your eyes? |
| 31 | I often hear a voice speaking my thoughts aloud. |
| 40 | Have you ever seen things invisible to other people? |
| 48 | Do everyday things seem unusually large or small? |
| 56 | Does your sense of smell sometimes become unusually strong? |
| 61 | Do you ever suddenly feel distracted by distant sounds that you are not normally aware of? |
| 64 | Are your thoughts sometimes so strong that you can almost hear them? |
|
| |
| Ideas of Reference | |
|
| |
| 1 | Do you sometimes feel that things you see on the TV or read in the newspaper have a special meaning for you? |
| 10 | I am aware that people notice me when I go out for a meal or to see a film. |
| 19 | Do some people drop hints about you or say things with a double meaning? |
| 28 | Have you ever noticed a common event or object that seemed to be a special sign for you? |
| 37 | Do you sometimes see special meanings in advertisements, shop windows, or in the way things are arranged around you? |
| 45 | When shopping do you get the feeling that other people are taking notice of you? |
| 53 | When you see people talking to each other, do you often wonder if they are talking about you? |
| 60 | Do you sometimes feel that other people are watching you? |
| 63 | Do you sometimes feel that people are talking about you? |
|
| |
| Suspiciousness and Paranoia | |
|
| |
| 9 | I am sure I am being talked about behind my back. |
| 18 | Do you often feel that other people have got it in for you? |
| 27 | Do you sometimes get concerned that friends or coworkers are not really loyal or trustworthy? |
| 36 | I feel I have to be on my guard even with friends. |
| 44 | Do you often pick up hidden threats or put-downs from what people say or do? |
| 52 | Have you found that it is best not to let other people know too much about you? |
| 59 | I often feel that others have it in for me. |
| 65 | Do you often have to keep an eye out to stop people from taking advantage of you? |
|
| |
| Inappropriate or Constricted Affect | |
|
| |
| 8 | People sometimes find me aloof and distant. |
| 17 | I am poor at expressing my true feelings by the way I talk and look. |
| 26 | I rarely laugh and smile. |
| 35 | My “nonverbal” communication (smiling and nodding during a conversation) is poor. |
| 43 | I am poor at returning social courtesies and gestures. |
| 51 | I tend to avoid eye contact when conversing with others. |
| 68 | I do not have an expressive and lively way of speaking. |
| 73 | I tend to keep my feelings to myself. |
|
| |
| No Close Friends | |
|
| |
| 6 | I have little interest in getting to know other people. |
| 15 | I prefer to keep to myself. |
| 24 | I am mostly quiet when with other people. |
| 33 | I find it hard to be emotionally close to other people. |
| 41 | Do you feel that there is no one you are really close to outside of your immediate family, or people you can confide in or talk to about personal problems? |
| 49 | Writing letters to friends is more trouble than it is worth. |
| 57 | I tend to keep in the background on social occasions. |
| 62 | I attach little importance to having close friends. |
| 66 | Do you feel that you are unable to get “close” to people? |
|
| |
| Excessive Social Anxiety | |
|
| |
| 2 | I sometimes avoid going to places where there will be many people because I will get anxious. |
| 11 | I get very nervous when I have to make polite conversation. |
| 20 | Do you ever get nervous when someone is walking behind you? |
| 29 | I get anxious when meeting people for the first time. |
| 38 | Do you often feel nervous when you are in a group of unfamiliar people? |
| 46 | I feel very uncomfortable in social situations involving unfamiliar people. |
| 54 | I would feel very anxious if I had to give a speech in front of a large group of people. |
| 71 | I feel very uneasy talking to people I do not know well. |
|
| |
| Odd Thinking and Speech | |
|
| |
| 7 | People sometimes find it hard to understand what I am saying. |
| 16 | I sometimes jump quickly from one topic to another when speaking. |
| 25 | I sometimes forget what I am trying to say. |
| 34 | I often ramble on too much when speaking. |
| 42 | Some people find me a bit vague and elusive during a conversation. |
| 50 | I sometimes use words in unusual ways. |
| 58 | Do you tend to wander off the topic when having a conversation? |
| 69 | I find it hard to communicate clearly what I want to say to people. |
| 72 | People occasionally comment that my conversation is confusing. |
|
| |
| Odd or Eccentric Behavior | |
|
| |
| 5 | Other people see me as slightly eccentric (odd). |
| 14 | People sometimes comment on my unusual mannerisms and habits. |
| 23 | Sometimes other people think that I am a little strange. |
| 32 | Some people think that I am a very bizarre person. |
| 67 | I am an odd, unusual person. |
| 70 | I have some eccentric (odd) habits. |
| 74 | People sometimes stare at me because of my odd appearance. |
TABLE A 2.
Subscale Ordinal and Cronbach’s Alpha
| Subscale Ordinal alpha Cronbach’s alpha |
Item | Frequency, % | Ordinal alpha* | Loading |
|---|---|---|---|---|
| Ideas of Reference | ||||
| .91 (.92) | 1. | 23(51) | .965(.976) | .81(.61) |
| .79 (.85) | 10. | 19(50) | .965(.976) | .67(.63) |
| 19. | 13(48) | .965(.975) | .79(.86) | |
| 28. | 16(48) | .965(.976) | .77(.67) | |
| 37. | 11(38) | .965(.976) | .68(.52) | |
| 45. | 12(52) | .965(.976) | .75(.81) | |
| 53. | 6(46) | .965(.975) | .74(.90) | |
| 60. | 14(61) | .965(.975) | .82(.91) | |
| 63. | 14(61) | .965(.975) | .87(.94) | |
| Excessive Social Anxiety | ||||
| .92 (.92) | 2. | 13(52) | .965(.976) | .81(.80) |
| .79 (.84) | 11. | 7(31) | .965(.976) | .85(.84) |
| 20. | 35(68) | .965(.976) | .66(.85) | |
| 29. | 28(52) | .965(.976) | .85(.74) | |
| 38. | 32(67) | .965(.976) | .93(.78) | |
| 46. | 18(54) | .965(.976) | .84(.83) | |
| 54. | 51(63) | .966(.976) | .46(.60) | |
| 71. | 13(51) | .965(.976) | .88(.81) | |
| Odd Beliefs or Magical Thinking | ||||
| .89 (.90) | 3. | 18(54) | .965(.976) | .85(.79) |
| .74 (.81) | 12. | 13(46) | .965(.976) | .87(.82) |
| 21. | 11(31) | .965(.976) | .70(.80) | |
| 30. | 19(45) | .966(.976) | .81(.80) | |
| 39. | 3(26) | .965(.976) | .79(.79) | |
| 47. | 13(47) | .965(.976) | .85(.82) | |
| 55. | 5(36) | .965(.976) | .78(.79) | |
| Unusual Perceptual Experiences | ||||
| .92 (.89) | 4. | 7(51) | .965(.976) | .66(.68) |
| .75 (.80) | 13. | 25(62) | .965(.976) | .75(.77) |
| 22. | 4(29) | .965(.976) | .65(.54) | |
| 31. | 2(37) | .965(.976) | .93(.71) | |
| 40. | 6(46) | .965(.976) | .72(.68) | |
| 48. | 3(29) | .965(.976) | .84(.66) | |
| 56. | 20(48) | .965(.976) | .75(.69) | |
| 61. | 17(54) | .965(.976) | .83(.81) | |
| 64. | 14(54) | .965(.976) | .91(.78) | |
| Odd or Eccentric Behavior | ||||
| .91 (.91) | 5. | 20(59) | .965(.976) | .93(.72) |
| .78 (.82) | 14. | 17(46) | .965(.976) | .81(.70) |
| 23. | 25(69) | .965(.975) | .90(.94) | |
| 32. | 6(41) | .965(.976) | .76(.78) | |
| 67. | 10(44) | .965(.976) | .79(.81) | |
| 70. | 20(52) | .965(.976) | .72(.78) | |
| 74. | 4(28) | .965(.976) | .68(.76) | |
| No Close Friends | ||||
| .90 (.90) | 6. | 8(40) | .965(.976) | .65(.67) |
| .77 (.81) | 15. | 26(68) | .965(.976) | .83(.64) |
| 24. | 29(35) | .965(.976) | .76(.64) | |
| 33. | 16(42) | .965(.976) | .82(.80) | |
| 41. | 14(54) | .965(.976) | .74(.67) | |
| 49. | 13(61) | .965(.976) | .52(.63) | |
| 57. | 30(33) | .965(.976) | .74(.81) | |
| 62. | 7(36) | .965(.976) | .69(.63) | |
| 66. | 9(51) | .965(.976) | .89(.90) | |
| Odd Thinking and Speech | ||||
| .90 (.91) | 7. | 15(48) | .965(.976) | .82(.66) |
| .76 (.83) | 16. | 36(61) | .965(.976) | .67(.76) |
| 25. | 44(68) | .965(.976) | .56(.81) | |
| 34. | 25(46) | .965(.976) | .64(.72) | |
| 42. | 11(44) | .965(.975) | .81(.90) | |
| 50. | 23(46) | .965(.976) | .73(.58) | |
| 58. | 20(51) | .965(.976) | .72(.80) | |
| 69. | 9(39) | .965(.976) | .84(.83) | |
| 72. | 6(33) | .965(.976) | .73(.68) | |
| Inappropriate or Constricted Affect | ||||
| .84 (.80) | 8. | 21(55) | .965(.976) | .78(.68) |
| .62 (.67) | 17. | 15(45) | .965(.976) | .76(.70) |
| 26. | 4(32) | .965(.976) | .69(.62) | |
| 35. | 7(33) | .965(.976) | .59(.71) | |
| 43. | 48(60) | .966(.977) | .27(.15) | |
| 51. | 5(28) | .966(.976) | .50(.66) | |
| 68. | 14(34) | .965(.976) | .69(.59) | |
| 73. | 37(72) | .965(.976) | .78(.68) | |
| Suspiciousness and Paranoia | ||||
| .93 (.94) | 9. | 12(51) | .965(.976) | .81(.87) |
| .75 (.86) | 18. | 2(44) | .965(.976) | .99(.87) |
| 27. | 23(63) | .965(.976) | .61(.80) | |
| 36. | 13(58) | .965(.976) | .88(.84) | |
| 44. | 9(44) | .965(.976) | .79(.80) | |
| 52. | 32(77) | .965(.976) | .87(.67) | |
| 59. | 2(40) | .965(.975) | .94(.93) | |
| 65. | 19(60) | .965(.976) | .77(.78) |
Note. Control group (outside of parentheses) and schizophrenia-spectrum group (inside parentheses). Frequency is the percentage of individuals who positively endorsed the given item.
Ordinal alpha of the measure with the corresponding item removed.
Loading = the first order factor loading of the item in the nine-subscale factor structure. Subscale = the specific subscale with the Ordinal alpha and Cronbach’s alpha reported below for the items within each respective subscale.
TABLE A3.
Exploratory Factor Analysis Loadings
| Model | Factor (EV) | UP | OB | IR | SP | CA | NF | SA | OS | EO |
|---|---|---|---|---|---|---|---|---|---|---|
| Corr. 4 promax | Pos (1.32) | .58 | .96 | |||||||
| Neg (2.48) | .38 | .79 | 1.16 | .58 | ||||||
| Dis (1.61) | 1.09 | .55 | ||||||||
| Par (1.40) | 1.04 | .52 | ||||||||
| Bifactor 4 | Schiz (5.78) | .82 | .68 | .84 | .83 | .78 | .84 | .72 | .75 | .75 |
| Neg (0.75) | −.28 | −.55 | .31 | .40 | .28 | |||||
| Dis (0.43) | .56 | .29 | ||||||||
| Par (0.38) | .54 | .25 |
Note. Corr. 4 = Correlated four-factor model; Bifactor 4 = bifactor with four factors (i.e., one general factor and three subfactors); Pos = Positive; Neg = Negative; Dis = Disorganized; Par = Paranoid; Schiz = general schizotypy factor; EV = eigenvalue of that extracted factor; UP = Unusual Perceptual Experiences; OB = Odd Beliefs or Magical Thinking; IR = Ideas of Reference; SP = Suspiciousness and Paranoia; CA = Inappropriate or Constricted Affect; NF = No Close Friends; SA = Excessive Social Anxiety; OS = Odd Thinking and Speech; EO = Odd or Eccentric Behavior. Factor loadings less than 0.25 are not shown.
Contributor Information
Alexandra B. Moussa-Tooks, Psychological & Brain Sciences, Indiana University Bloomington, Bloomington, Indiana; Program in Neuroscience, Indiana University Bloomington.
Allen J. Bailey, Psychological & Brain Sciences, Indiana University Bloomington, Bloomington, Indiana.
Amanda R. Bolbecker, Psychological & Brain Sciences, Indiana University Bloomington, Bloomington, Indiana; Larue D. Carter Memorial Hospital, Indianapolis, Indiana; Department of Psychiatry, Indiana University School of Medicine, Indianapolis, Indiana.
Richard J. Viken, Psychological & Brain Sciences, Indiana University Bloomington, Bloomington, Indiana; Program in Neuroscience, Indiana University Bloomington.
Brian F. O’Donnell, Larue D. Carter Memorial Hospital, Indianapolis, Indiana; Department of Psychiatry, Indiana University School of Medicine, Indianapolis, Indiana; Psychological & Brain Sciences, Indiana University Bloomington, Bloomington, Indiana; Program in Neuroscience, Indiana University Bloomington.
William P. Hetrick, Psychological & Brain Sciences, Indiana University Bloomington, Bloomington, Indiana; Larue D. Carter Memorial Hospital, Indianapolis, Indiana; Department of Psychiatry, Indiana University School of Medicine, Indianapolis, Indiana; Program in Neuroscience, Indiana University Bloomington.
REFERENCES
- American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Andreasen NC, Arndt S, Swayze V II, Cizadlo T, Flaum M, O’Leary D, … Yuh WT (1994). Thalamic abnormalities in schizophrenia visualized through magnetic resonance image averaging. Science, 266(5183), 294–298. [DOI] [PubMed] [Google Scholar]
- Badcock JC, & Dragović M (2006). Schizotypal personality in mature adults. Personality and Individual Differences, 40(1), 77–85. 10.1016/j.paid.2005.06.015 [DOI] [Google Scholar]
- Bentler PM, & Bonett DG (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88, 588–606. [Google Scholar]
- Blonigen DM, Hicks BM, Krueger RF, Patrick CJ, & Iacono WG (2005). Psychopathic personality traits: Heritability and genetic overlap with internalizing and externalizing psychopathology. Psychological Medicine, 35, 637–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonifay W, Lane SP, & Reise SP (2017). Three concerns with applying a bifactor model as a structure of psychopathology. Clinical Psychological Science, 5(1), 184–186. [Google Scholar]
- Bora E, & Baysan Arabaci L (2009). Effect of age and gender on schizotypal personality traits in the normal population. Psychiatry and Clinical Neurosciences, 63, 663–669. 10.1111/j.1440-1819.2009.02011.x [DOI] [PubMed] [Google Scholar]
- Brown TA (2014). Confirmatory factor analysis for applied research. New York, NY: Guilford. [Google Scholar]
- Browne MW, & Cudeck R (1992). Alternative ways of assessing model fit. Sociological Methods & Research, 21, 230–258. [Google Scholar]
- Cadenhead KS, & Braff DL (2002). Endophenotyping schizotypy: A prelude to genetic studies within the schizophrenia spectrum. Schizophrenia Research, 54(1–2), 47–57. [DOI] [PubMed] [Google Scholar]
- Cai L, Yang JS, & Hansen M (2011). Generalized full-information item bifactor analysis. Psychological Methods, 16, 221–248. 10.1037/a0023350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camisa KM, Bockbrader MA, Lysaker P, Rae LL, Brenner CA, & O’Donnell BF (2005). Personality traits in schizophrenia and related personality disorders. Psychiatry Research, 133(1), 23–33. 10.1016/j.psychres.2004.09.002 [DOI] [PubMed] [Google Scholar]
- Carpenter WT, Bustillo JR, Thaker GK, van Os J, Krueger RF, & Green MJ (2009). The psychoses: Cluster 3 of the proposed meta-structure for DSM-V and ICD-11. Psychological Medicine, 39, 2025–2042. 10.1017/S0033291709990286 [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S … Moffitt TE (2014). The p Factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137. 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, & Moffitt TE (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175, 831–844. 10.1176/appi.ajp.2018.17121383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman LJ, Chapman JP, & Raulin ML (1978). Body-image aberration in schizophrenia. Journal of Abnormal Psychology, 87, 399–407. [DOI] [PubMed] [Google Scholar]
- Chen FF, West SG, & Sousa KH (2006). A comparison of bifactor and second-order models of quality of life. Multivariate Behavioral Research, 41, 189–225. 10.1207/s15327906mbr4102_5 [DOI] [PubMed] [Google Scholar]
- Cicero DC, Jonas KG, Li K, Perlman G, & Kotov R (2019). Common taxonomy of traits and symptoms: Linking schizophrenia symptoms, schizotypy, and normal personality. Schizophrenia Bulletin, 45(6), 1336–1348. 10.1093/schbul/sbz005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AS, & Davis TE III. (2009). Quality of life across the schizotypy spectrum: Findings from a large nonclinical adult sample. Comprehensive Psychiatry, 50, 408–414. 10.1016/j.comppsych.2008.11.002 [DOI] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Bakeman R, & McClure-Tone EB (2009). Confirmation of a four-factor structure of the Schizotypal Personality Questionnaire among undergraduate students. Schizophrenia Research, 111(1–3), 46–52. 10.1016/j.schres.2009.02.012 [DOI] [PubMed] [Google Scholar]
- Daneluzzo E, Bustini M, Stratta P, Casacchia M, & Rossi A (1998). Schizotypal Personality Questionnaire and Wisconsin Card Sorting Test in a population of DSM-III-R schizophrenic patients and control subjects. Comprehensive Psychiatry, 39, 143–148. [DOI] [PubMed] [Google Scholar]
- Dueber DM (2017). Bifactor Indices Calculator: A Microsoft Excel–based tool to calculate various indices relevant to bifactor CFA models. [Computer Software]. 10.13023/edp.tool.01 [DOI] [Google Scholar]
- First MB, Benjamin LS, Gibbon M, Spitzer RL, & Williams JBW (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders. Washington, DC: American Psychiatric Press. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, research version, patient edition (SCID-I/P). New York, NY: Biometrics Research. [Google Scholar]
- Fonseca-Pedrero E, Compton MT, Tone EB, Ortuño-Sierra J, Paino M, Fumero A, & Lemos-Giráldez S (2014). Cross-cultural invariance of the factor structure of the Schizotypal Personality Questionnaire across Spanish and American college students. Psychiatry Research, 220, 1071–1076. 10.1016/j.psychres.2014.06.050 [DOI] [PubMed] [Google Scholar]
- Fonseca-Pedrero E, Debbane M, Ortuño-Sierra J, Chan RCK, Cicero DC, Zhang LC, … Jablensky A (2018). The structure of schizotypal personality traits: A cross-national study. Psychological Medicine, 48, 451–462. 10.1017/S0033291717001829 [DOI] [PubMed] [Google Scholar]
- Fonseca-Pedrero E, Fumero A, Paino M, de Miguel A, Ortuño-Sierra J, Lemos-Giráldez S, & Muniz J (2014). Schizotypal Personality Questionnaire: New sources of validity evidence in college students. Psychiatry Research, 219, 214–220. 10.1016/j.psychres.2014.04.054 [DOI] [PubMed] [Google Scholar]
- Fonseca-Pedrero E, Ortuño J, Debbane M, Chan RCK, Cicero D, Zhang LC, … Fried EI (2018). The network structure of schizotypal personality traits. Schizophrenia Bulletin, 44(Suppl. 2), S468–S479. 10.1093/schbul/sby044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca-Pedrero E, Ortuño-Sierra J, LucasMolina B, Debbane M, Chan RCK, Cicero DC, … Voracek M (2017). Brief assessment of schizotypal traits: A multinational study. Schizophrenia Research, 197, 182–191. 10.1016/j.schres.2017.10.043 [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Bock RD, Hedeker D, Weiss DJ, Segawa E, Bhaumik DK, … Stover A (2007). Full-information item bifactor analysis of graded response data. Applied Psychological Measurement, 31(1), 4–19. [Google Scholar]
- Grant P, Green MJ, & Mason OJ (2018). Models of schizotypy: The importance of conceptual clarity. Schizophrenia Bulletin, 44(Suppl. 2), S556–S563. 10.1093/schbul/sby012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene AL, Eaton NR, Li K, Forbes MK, Krueger RF, Markon KE, … Kotov R (2019). Are fit indices used to test psychopathology structure biased? A simulation study. Journal of Abnormal Psychology, 128, 740–764. 10.1037/abn0000434 [DOI] [PubMed] [Google Scholar]
- Gross GM, Mellin J, Silvia PJ, Barrantes-Vidal N, & Kwapil TR (2014). Comparing the factor structure of the Wisconsin Schizotypy Scales and the Schizotypal Personality Questionnaire. Personality Disorders: Theory, Research, and Treatment, 5, 397–405. [DOI] [PubMed] [Google Scholar]
- Hu L-T, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. [Google Scholar]
- Jennrich RI, & Bentler PM (2011). Exploratory bi-factor analysis. Psychometrika, 76, 537–549. 10.1007/s11336-011-9218-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS (1985). Diagnostic approaches to schizotypal personality disorder: A historical perspective. Schizophrenia Bulletin, 11, 538–553. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Ochs AL, Gorman AM, Hewitt JK, Ross DE, & Mirsky AF (1991). The structure of schizotypy: A pilot multitrait twin study. Psychiatry Research, 36, 19–36. [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, … Zimmerman M (2017). The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Krueger RF (1999). The structure of common mental disorders. Archives of General Psychiatry, 56, 921–926. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, & Kramer MD (2007). Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology, 116, 645–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, & Zald DH (2017). A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin, 143, 142–186. 10.1037/bul0000069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, … Dunbar GC (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12, 224–231. [Google Scholar]
- Lenzenweger MF (2018). Schizotypy, schizotypic psychopathology and schizophrenia. World Psychiatry, 17(1), 25–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenzenweger MF, & Dworkin RH (1996). The dimensions of schizophrenia phenomenology. Not one or two, at least three, perhaps four. British Journal of Psychiatry, 168, 432–440. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, & Loranger AW (1989). Psychosis proneness and clinical psychopathology: Examination of the correlates of schizotypy. Journal of Abnormal Psychology, 98(1), 3–8. [DOI] [PubMed] [Google Scholar]
- Liddle PF (1987). The symptoms of chronic schizophrenia. A re-examination of the positive-negative dichotomy. British Journal of Psychiatry, 151, 145–151. [DOI] [PubMed] [Google Scholar]
- Lui SSY, Hung KSY, Wang Y, Ho KKY, Yeung HKH, Wang Y, … Chan RCK (2018). Clustering of schizotypal features in unaffected first-degree relatives of schizophrenia patients. Schizophrenia Bulletin, 44(Suppl. 2), S536–S546. 10.1093/schbul/sby035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason O, & Claridge G (2006). The Oxford-Liverpool Inventory of Feelings and Experiences (O-LIFE): Further description and extended norms. Schizophrenia Research, 82, 203–211. [DOI] [PubMed] [Google Scholar]
- Maxwell ME (1992). Family Interview for Genetic Studies (FIGS): A manual for FIGS. Bethesda, MD: Clinical Neurogenetics Branch, Intramural Research Program, National Institute of Mental Health. [Google Scholar]
- Meehl PE (1962). Schizotaxia, schizotypy, schizophrenia. American Psychologist, 17, 827–838. [Google Scholar]
- Moreno-Izco L, Sanchez-Torres AM, LorenteOmenaca R, Fananas L, Rosa A, Salvatore P, … Cuesta MJ (2015). Ten-year stability of self-reported schizotypal personality features in patients with psychosis and their healthy siblings. Psychiatry Research, 227(2–3), 283–289. 10.1016/j.psychres.2015.02.020 [DOI] [PubMed] [Google Scholar]
- Morgan G, Hodge K, Wells K, & Watkins M (2015). Are fit indices biased in favor of bifactor models in cognitive ability research?: A comparison of fit in correlated factors, higher-order, and bi-factor models via Monte Carlo simulations. Journal of Intelligence, 3(1), 2–20. 10.3390/jintelligence3010002 [DOI] [Google Scholar]
- Nunnally JC (1967). Psychometric theory. New York, NY: McGraw-Hill. [Google Scholar]
- Ortuño-Sierra J, Badoud D, Knecht F, Paino M, Eliez S, Fonseca-Pedrero E, & Debbane M (2013). Testing measurement invariance of the Schizotypal Personality Questionnaire—Brief scores across Spanish and Swiss adolescents. PLoS One, 8(12), e82041. 10.1371/journal.pone.0082041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park S, & McTigue K (1997). Working memory and the syndromes of schizotypal personality. Schizophrenia Research, 26(2–3), 213–220. [DOI] [PubMed] [Google Scholar]
- Preti A, Siddi S, Vellante M, Scanu R, Muratore T, Gabrielli M, … Petretto DR (2015). Bifactor structure of the schizotypal personality questionnaire (SPQ). Psychiatry Research, 230, 940–950. 10.1016/j.psychres.2015.11.010 [DOI] [PubMed] [Google Scholar]
- Raftery AE (1995). Bayesian model selection in social research. Sociological Methodology, 25, 111–163. [Google Scholar]
- Raine A (1991). The SPQ: A scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophrenia Bulletin, 17, 555–564. [DOI] [PubMed] [Google Scholar]
- Raine A (1992). Sex differences in schizotypal personality in a nonclinical population. Journal of Abnormal Psychology, 101, 361–364. [DOI] [PubMed] [Google Scholar]
- Raine A (2006). Schizotypal personality: Neurodevelopmental and psychosocial trajectories. Annual Review of Clinical Psychology, 2, 291–326. 10.1146/annurev.clinpsy.2.022305.095318 [DOI] [PubMed] [Google Scholar]
- Raine A, Reynolds C, Lencz T, Scerbo A, Triphon N, & Kim D (1994). Cognitive-perceptual, interpersonal, and disorganized features of schizotypal personality. Schizophrenia Bulletin, 20, 191–201. [DOI] [PubMed] [Google Scholar]
- R Core Team. (2014). R: A language and environment for statistical computing [Computer software]. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Reise SP (2012). Invited Paper: The rediscovery of bifactor measurement models. Multivariate Behavioral Research, 47, 667–696. 10.1080/00273171.2012.715555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise SP, Morizot J, & Hays RD (2007). The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Quality of Life Research, 16(Suppl. 1), 19–31. 10.1007/s11136-007-9183-7 [DOI] [PubMed] [Google Scholar]
- Revelle WR (2017). psych: Procedures for personality and psychological research. [Computer software]. [Google Scholar]
- Reynolds CA, Raine A, Mellingen K, Venables PH, & Mednick SA (2000). Three-factor model of schizotypal personality: Invariance across culture, gender, religious affiliation, family adversity, and psychopathology. Schizophrenia Bulletin, 26, 603–618. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Reise SP, & Haviland MG (2016). Applying bifactor statistical indices in the evaluation of psychological measures. Journal of Personality Assessment, 98, 223–237. 10.1080/00223891.2015.1089249 [DOI] [PubMed] [Google Scholar]
- Rosseel Y (2011). lavaan: An R package for structural equation modeling and more Version 0.4–9 (BETA) [Computer software]. Ghent, Belgium: Ghent University. [Google Scholar]
- Rossi A, & Daneluzzo E (2002). Schizotypal dimensions in normals and schizophrenic patients: A comparison with other clinical samples. Schizophrenia Research, 54(1–2), 67–75. [DOI] [PubMed] [Google Scholar]
- Schürhoff F, Laguerre A, Szöke A, Méary A, & Leboyer M (2005). Schizotypal dimensions: Continuity between schizophrenia and bipolar disorders. Schizophrenia Research, 80(2–3), 235–242. 10.1016/j.schres.2005.07.009 [DOI] [PubMed] [Google Scholar]
- Sharp C, Wright AG, Fowler JC, Frueh BC, Allen JG, Oldham J, & Clark LA (2015). The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? Journal of Abnormal Psychology, 124, 387–398. 10.1037/abn0000033 [DOI] [PubMed] [Google Scholar]
- Shevlin M, McElroy E, Bentall RP, Reininghaus U, & Murphy J (2017). The psychosis continuum: Testing a bifactor model of psychosis in a general population sample. Schizophrenia Bulletin, 43, 133–141. 10.1093/schbul/sbw067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanis NC, Smyrnis N, Avramopoulos D, Evdokimidis I, Ntzoufras I, & Stefanis CN (2004). Factorial composition of self-rated schizotypal traits among young males undergoing military training. Schizophrenia Bulletin, 30, 335–350. [DOI] [PubMed] [Google Scholar]
- Stucky BD, Thissen D, & Orlando Edelen M (2013). Using logistic approximations of marginal trace lines to develop short assessments. Applied Psychological Measurement, 37(1), 41–57. [Google Scholar]
- Suzuki T, Samuel DB, Pahlen S, & Krueger RF (2015). DSM-5 alternative personality disorder model traits as maladaptive extreme variants of the five-factor model: An item-response theory analysis. Journal of Abnormal Psychology, 124, 343–354. 10.1037/abn0000035 [DOI] [PubMed] [Google Scholar]
- Torgersen S, Edvardsen J, Oien PA, Onstad S, Skre I, Lygren S, & Kringlen E (2002). Schizotypal personality disorder inside and outside the schizophrenic spectrum. Schizophrenia Research, 54(1–2), 33–38. [DOI] [PubMed] [Google Scholar]
- Vollema MG, Sitskoorn MM, Appels MC, & Kahn RS (2002). Does the Schizotypal Personality Questionnaire reflect the biological-genetic vulnerability to schizophrenia? Schizophrenia Research, 54(1–2), 39–45. [DOI] [PubMed] [Google Scholar]
- Wuthrich VM, & Bates TC (2006). Confirmatory factor analysis of the three-factor structure of the Schizotypal Personality Questionnaire and Chapman schizotypy scales. Journal of Personality Assessment, 8, 292–304. 10.1207/s15327752jpa8703_10 [DOI] [PubMed] [Google Scholar]
- Yaralian PS, Raine A, Lencz T, Hooley JM, Bihrle SE, Mills S, & Ventura J (2000). Elevated levels of cognitive-perceptual deficits in individuals with a family history of schizophrenia spectrum disorders. Schizophrenia Research, 46, 57–63. [DOI] [PubMed] [Google Scholar]
- Yung Y-F, Thissen D, & McLeod LD (1999). On the relationship between the higher-order factor model and the hierarchical factor model. Psychometrika, 64, 113–128. [Google Scholar]
- Zumbo BD, Gadermann AM, & Zeisser C (2007). Ordinal versions of coefficients alpha and theta for Likert rating scales. Journal of Modern Applied Statistical Methods, 6(1), 21–29. 10.22237/jmasm/1177992180 [DOI] [Google Scholar]