Abstract
Aim
The trauma-psychosis cycle proposes an interactive relationship between impaired developmental and cognitive trajectory, childhood trauma exposure, and increased risk for psychosis. This study explored how childhood trauma (CT) and atypical development (AD) impact clinical course in an early psychosis cohort.
Methods
A retrospective chart review of behavioural and clinical research data was conducted with individuals ages 12 to 40 (N = 508; 72.4% males) evaluated by an early psychosis program.
Results
CT exposure was associated with earlier onset of full threshold psychosis, more hospitalizations, higher ratings of negative symptoms, and increased likelihood of engaging in suicidal behaviour. AD alone was associated with earlier onset of psychosis symptoms, higher ratings of negative symptoms and greater likelihood of engaging in non-suicidal self-injury. The combination of CT and AD was associated with the earliest symptom onset and poorest psychosocial functioning.
Conclusions
The findings contribute to our understanding of heterogeneity in the early psychosis population and highlight the specific risk factors that could be targets in treatment.
Keywords: atypical development, childhood trauma, clinical course, early psychosis
INTRODUCTION
Two lines of evidence suggest atypical development (AD) and childhood trauma (CT) contribute to heterogeneity in risk, clinical course and outcome among individuals with psychosis. First, individuals with psychosis have high comorbidity rates of cognitive and developmental disorders (ie, attention-deficit/ hyperactivity disorder and autism spectrum disorders; Stahlberg, Soderstrom, Rastam, & Gillberg, 2004) and early childhood delays in language and motor development (Barch et al., 2017; Cannon et al., 2002; Laurens & Cullen, 2016; Macmanus et al., 2012; Parellada, Gomez-Vallejo, Burdeus, & Arango, 2017). Additionally, psychosis is associated with widespread neurocognitive impairments in global intellectual functioning, verbal and nonverbal memory, attention, executive functioning and motor performance (Flashman & Green, 2004). Consistent with the neurodevelopmental model of schizophrenia (Feinberg, 1982; Murray & Lewis, 1987; Walker & Diforio, 1997; Weinberger, 1987), psychotic disorders are proposed to arise from the interaction between early neurological insults or genetic risk factors and subsequent environmental stressors that contribute to the expression of psychosis, with varying degrees of cognitive deficit, clinical symptoms, and functional impairment (Rapoport, Giedd, & Gogtay, 2012).
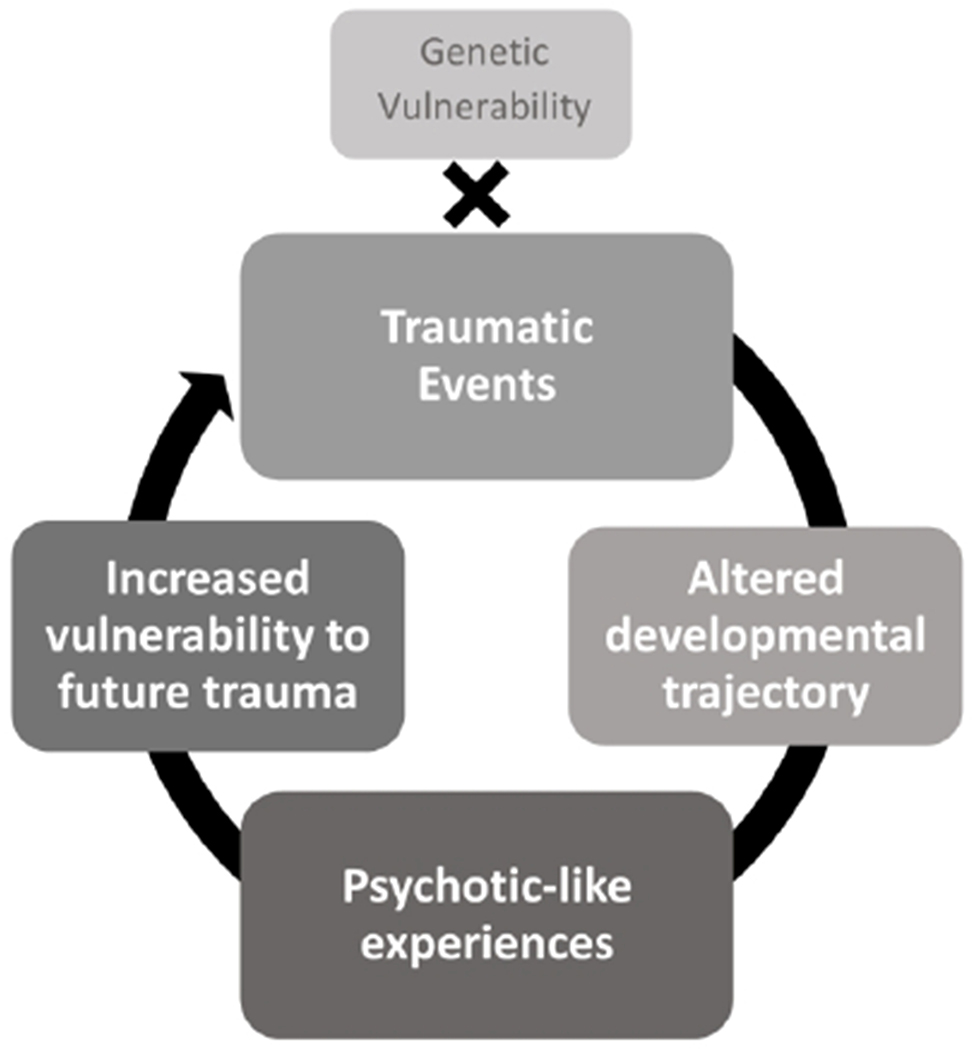
Second, consistent with this model, exposure to CT may represent a key environmental stressor associated with increased psychosis risk (Addington et al., 2013; Arseneault et al., 2011; Kelleher et al., 2013; Mayo et al., 2017), higher relapse rates (Cotter, Kaess, & Yung, 2015), and poorer long-term functioning (Petros et al., 2016). These findings suggest a cyclical pattern implicating CT, AD, and psychosis (Figure 1). The trauma-psychosis cycle (Mayo et al., 2017) proposes that, in conjunction with neurobiological and/or genetic risk, CT represents an environmental stressor that derails developmental course, contributing to impaired cognition and functioning, subsequently increasing vulnerability to future stressors (Lardinois, Lataster, Mengelers, Van Os, & Myin-Germeys, 2011; Schenkel, Spaulding, DiLillo, & Silverstein, 2005; Shannon et al., 2009). Alterations in development are associated with the consequences of CT exposure include changes in cognition, such as impaired executive functioning (Kavanaugh, Dupont-Frechette, Jerskey, & Holler, 2017), as well as poor social engagement and/or academic performance. Both of these subsequently increase vulnerability to future stressors and risk for psychosis onset (Kim et al., 2011). AD is associated with similar challenges in cognition and functioning, suggesting that individuals with AD may incur similar risk for psychosis. With the onset of psychosis symptoms, individuals are further impaired in their adaptive coping and thus more vulnerable to future adversity. Furthermore, as neurocognitive function, childhood trauma exposure, and psychosis are all implicated in risk for suicidal behaviours (Akyuz, Sar, Kugu, & Doğan, 2005; Grattan, Tully, Lesh, Carter, & Niendam, 2019; Lopez-Garcia et al., 2019; Pompili et al., 2011; Richard-Devantoy, Berlim, & Jollant, 2014), self-harm behaviours are a critical domain to examine in this complex and high-risk population. As such, the current study examined suicide attempts and non-suicidal self-injurious behaviours (NSSIB). Examination of the relationship between AD, CT, and psychosis could inform treatment and elucidate the contributing factors for heterogeneity in illness course, namely psychosis symptom trajectory and severity, and overall functioning.
Figure 1.
A proposed model for the link between trauma and psychosis, adapted from Mayo et al., 2017.
We conducted a retrospective chart review to examine the distinct and combined impact of CT and AD on the clinical presentation of individuals experiencing recent onset of psychosis.
Compared to individuals who have experienced neither CT nor AD, we predicted that distinct experiences of either CT or AD would be associated with an earlier age at onset of psychosis as well as a history of increased hospitalization, increased self-harm behaviours, and poorer psychosocial functioning prior to presentation for care. Furthermore, we predicted that individuals who report both CT and AD would be at the greatest disadvantage across these measures.
METHODS
Participants were recruited from the UC Davis Early Psychosis (UCD EP) programs and the Sacramento area as part of a larger study (PI: Carter, NIMH 5R01MH059883). Eligible individuals (ages 12-40) had a Wechsler Abbreviated Scale Intelligence score > 70 (Wechsler, 1999) and psychosis onset within 2 years prior to intake, according to the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1996). A standardized retrospective chart review of behavioural and clinical research data, conducted by research staff and supervised by T.A.N, provided data on demographics, developmental, trauma, and medical history. Date of psychosis onset, defined as point at which psychosis symptoms reached full threshold due to significant distress or impact on functioning (SIPS; McGlashan, 2001), was based on all available data. While participants were not systematically asked about CT or AD, researchers documented presence of these variables if they were mentioned anywhere in the chart materials. AD was noted when records mentioned an early developmental delay (eg, speech, motor) or any suspected or diagnosed neurodevelopmental disorders (ie, attention-deficit/hyperactivity disorder; ADHD, autism spectrum disorders; ASD, or pervasive developmental disorder: PDD, per DSM-IV). Presence of CT was noted for individuals whose charts included mention of physical or sexual abuse, neglect, emotional or verbal abuse, bullying, or indirect exposure to violence (e.g., witnessing domestic violence) in their youth (i.e., prior to age 25). “Suspected trauma” was coded if clinical or physical indications of trauma were noted, but exposure was not explicitly confirmed. Clinician-rated measures of symptoms at intake (Brief Psychiatric Rating Scale [BPRS; Lukoff, Nuechterlein, & Ventura, 1986], Scale for the Assessment of Positive Symptoms [SAPS; Andreasen, 1984], Scale for the Assessment of Negative Symptoms [SANS; Andreasen, 1984], global functioning (Global Assessment of Functioning [GAF; Hall, 1995]), social and role functioning at intake and the highest/lowest in the year prior to intake (Global Functioning: Role and Global Functioning: Social [Cornblatt et al., 2007]), and the Columbia-Suicide Severity Rating Scale (CSSRS; Posner et al., 2008) were also examined.
Data were checked for outliers and non-normal data were transformed or non-parametric tests were used. T-tests, ANOVAS, and χ2 tests were used to examine group differences between key variables related to clinical course using IBM SPSS Statistics (Version 25.0). Significance level was established at P < .05, with notable trends reported for P < .10.
RESULTS
See Table 1 for participant demographics. A total of 151 (30.0%) individuals endorsed a history of at least one type of AD, including a formal or suspected diagnosis of developmental delay (n = 55, 11.0%), specific learning disorder (n = 113, 23.1%), ADHD (n = 65, 13.1%), and PDD or ASD (n = 18, 3.7%; Table 2). Individuals with any kind of AD experienced an earlier age at onset of full-threshold psychotic symptoms (M = 18.08, SD = 4.26) compared to individuals who did not report AD (M = 20.02, SD = 4.21; t[460] = 4.53, P < .001). AD individuals were also more likely to report engaging in NSSIB (χ2[2] = 7.131; P = .008). AD individuals had higher SANS scores (M = 9.56, SD = 4.27) than individuals with no AD (M = 8.49, SD = 4.08; t[398] = −2.29, P = .02) but no other differences in clinical scores were found (Table 3).
Table 1.
Participant Demographics
| Demographics | Combined Sample (N=508) | AD Only (N=124) | CT Only (N=41) | CT+AD (N=29) | Neither (N=314) | Statistical Differences |
|---|---|---|---|---|---|---|
| Age at intake, M (SD) | 20.04 (4.26) | 18.71 (3.94) | 19.73 (4.16) | 17.87 (3.43) | 20.82 (4.28) | ***Neither > AD |
| Estimated WASI IQ, M (SD) | 98.82 (4.33) | 98.14 (16.88) | 98.11 (14.63) | 93.96 (11.78) | 99.67 (14.288) | -- |
| Caregiver 1/Mother years of education, M (SD) | 13.65 (3.39) | 13.45 (3.50) | 12.89 (3.10) | 12.11 (3.364) | 13.95 (3.36) | -- |
| Caregiver 2/Father years of education, M (SD) | 13.77 (3.90) | 13.82 (3.90) | 12.88 (3.60) | 12.41 (2.58) | 13.96 (3.93) | -- |
| Male gender, N (%) | 368 (58.4) | 96 (77.40) | 23 (56.1) | 18 (62.1) | 231 (73.6) | -- |
| Hispanic , N (%) | 77 (12.2) | 29 (23.4) | 4 (9.8) | 5 (17.2) | 39 (12.4) | -- |
| Asian or Pacific Islander, N (%) | 67 (10.7) | 1 (13.8) | 10 (24.4) | 4 (13.7) | 36 (11.4) | -- |
| Native American, N (%) | 8 (1.3) | 2 (1.6) | 2 (4.9) | 4 (13.8) | 0 | -- |
| African American, N (%) | 81 (12.9) | 24 (19.4) | 4 (9.8) | 9 (31.0) | 44 (14.0) | -- |
| Caucasian, N (%) | 292 (46.3) | 64 (51.6) | 21 (51.2) | 10 (34.5) | 197 (62.7) | -- |
| More than one race, N (%) | 51 (8.1) | 14 (11.3) | 4 (9.8) | 2 (6.9) | 31 (9.9) | -- |
| Primary DSM-IV Diagnosis at Intake, N (%) | ||||||
| Schizophrenia | 118 (18.7) | 30 (24.2) | 14 (34.1) | 3 (10.3) | 71 (22.6) | -- |
| Schizoaffective Disorder | 43 (6.8) | 8 (6.5) | 4 (9.8) | 2 (6.9) | 29 (9.2) | -- |
| Schizophreniform Disorder | 134 (21.3) | 31 (25.0) | 9 (22.0) | 5 (17.2) | 89 (28.3) | -- |
| Bipolar Disorder | 65 (10.3) | 12 (9.7) | 8 (19.5) | 3 (10.3) | 42 (13.4) | -- |
| Major Depressive Disorder w/psychotic features | 24 (3.8) | 6 (4.8) | 1 (2.4) | 4 (13.8) | 13 (4.1) | -- |
| Psychotic Disorder NOS | 53 (8.4) | 14 (11.3) | 3 (7.3) | 5 (17.2) | 31 (9.9) | -- |
| Unknown | 16 (2.5) | 4 (3.2) | 0 | 1 (3.4) | 4 (1.2) | -- |
p<.05,
p<.01,
p<.001
Table 2.
Frequencies of AD and CT in sample.
| Atypical Development, N (%) | All AD | AD only |
|---|---|---|
| Developmental Delay | 55 (11.0) | 42 (34.4) |
| Specific Learning Disorder | 113 (23.1) | 83 (68.0) |
| ADHD | 65 (13.1) | 50 (41.0) |
| PDD or ASD | 18 (3.7) | 14 (11.5) |
| Childhood Trauma, N (%) | All CT | CT only |
| Suspected trauma | 22 (4.4) | 4 (36.4) |
| Sexual abuse | 43 (30.9) | 5 (45.5) |
| Witness domestic or community violence | 31 (22.3) | 6 (54.5) |
| Physical abuse or attack | 19 (13.7) | 0 (0) |
| Bullying | 9 (1.8) | 4 (36.4) |
| Physical or emotional neglect | 4 (0.8) | 0 (0) |
| Emotional or verbal abuse | 11 (7.9) | 2 (18.2) |
Note: “AD only” refers to participants who had AD in the absence of CT, while “All AD” refers to participants who had AD with or without CT in addition. The same distinction applies for “All CT” versus “CT only.” Specific Learning Disorder encompasses disorders in reading, writing, and mathematics. PDD classification was based on DSM-IV criteria.
Table 3.
Participant Clinical Characteristics
| Entire Sample (n=504) | Neither AD nor CT | AD | No AD | Statistical Differences | CT | No CT | Statistical Differences | |
|---|---|---|---|---|---|---|---|---|
| SAPS Total Score, M (SD) | 5.41 (0.18) | 4.77 (0.47 | 5.13 (0.32) | 5.53 (0.22) | 4.92 (3.55) | 5.61 (3.90) | -- | |
| SANS Total Score, M (SD) | 8.77 (0.21) | 8.13 (0.54) | 9.56 (0.42) | 8.48 (0.24) | *AD > No AD | 7.97 (4.06) | 8.56 (4.09) | -- |
| BPRS Total Score, M (SD) | 42.76 (0.56) | 41.27 (1.74) | 43.80 (1.14) | 42.35 (0.66) | -- | 43.31 (12.06) | 42.22 (10.10) | -- |
| Age at psychosis onset, M (SD) | 19.44 (0.20) | 19.07 (0.51) | 18.08 (0.36) | 20.02 (0.23) | ***No AD > AD | 19.39 (3.97) | 20.10 (4.24) | *CT<No CT |
| Number of psych hospital/ED Visits, M (SD) | 1.06 (0.05) | 1.42 (0.14) | 1.11 (0.10) | 1.05 (0.05) | -- | 1.39 (1.24) | 1.00 (0.93) | *CT > No CT |
| Engaged in NSSIB, N (%) | 285 (56.5) | 38 (56.7) | 99 (65.6) | 186 (52.7) | **AD > No AD | 40 (57.1) | 245 (56.5) | -- |
| Engaged in Suicide attempts, N (%) | 41 (8.1) | 7 (10.4) | 16 (10.6) | 25 (7.1) | -- | 12 (17.1) | 29 (6.7) | **No CT > CT |
p<.05,
p<.01,
p<.001
Seventy (13.9%) individuals indicated a history of CT exposure, including 22 (4.3%) with “suspected trauma.” Trauma types in order of frequency were: sexual abuse (n = 43, 30.9%), witnessed domestic or community violence (n = 31, 22.3%), physical abuse or a physical attack (n = 19, 13.7%), bullying (n = 9, 1.8%), emotional or verbal abuse (n = 11, 7.9%) and physical or emotional neglect (n = 4, 0.8%; Table 2). Over half of individuals were below age 12 at the time of their first traumatic experience (n = 40, 74.1%). CT individuals had an earlier age at psychosis onset compared to those without CT (Mann-Whitney U = 10 428.50, P = .04). CT individuals also endorsed more psychiatric hospital or emergency department visits (Mann- Whitney U = 12 225.00, P = .005), but were less likely to have made a suicide attempt than individuals without CT (χ2[2] = 8.83; P = .003). No significant differences in clinical symptoms at intake (SAPS, SANS, BPRS) were found between individuals with and without CT (Table 3).
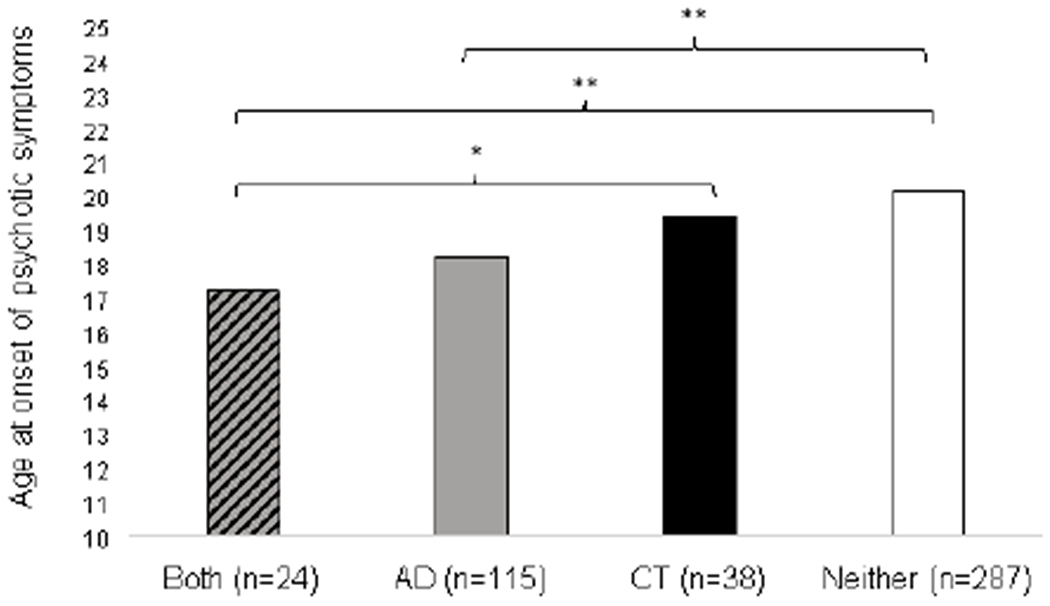
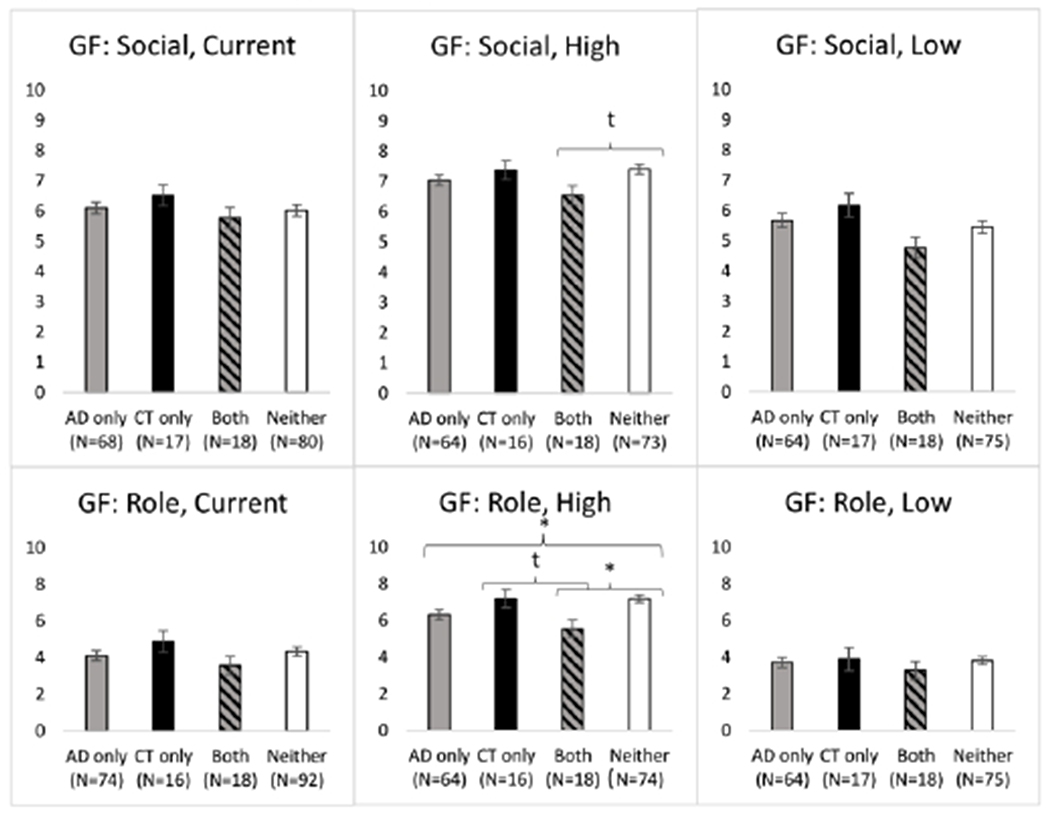
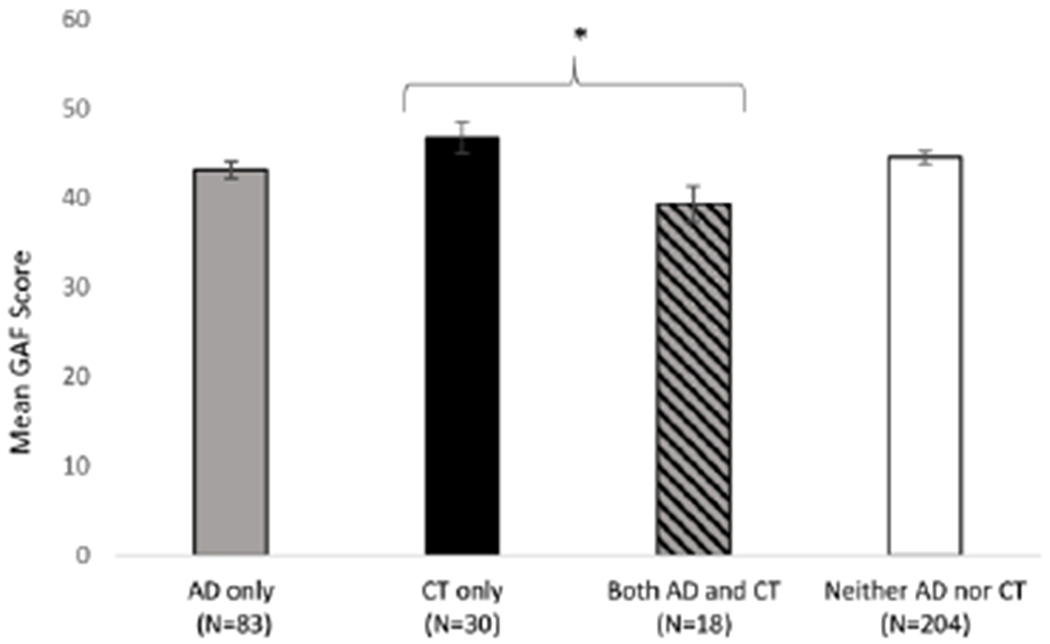
To examine the combined impact of CT and AD, participants were divided into four groups: 1) those with recorded AD only (n = 122), 2) those with CT only (n = 41), 3) those with both CT + AD (n = 29), and 4) those with neither CT nor AD (n = 312). Individuals in the CT + AD group had the earliest age at onset of psychosis (H[3] = 20.01, P < .001; Figure 2). They also had the poorest global functioning at intake (F[3, 331] = 2.62, P = .05). When the highest level of role functioning in the year prior to intake was examined across the four groups, the CT + AD individuals’ role functioning was significantly lower than the other three groups (F[3167] = 3.99, P = .003; (Figure 3). There was a trend for CT + AD to have poorest social functioning at intake (H[3166] = 2.31, P = .08); however, this did not reach statistical significance Figure 4). CT + AD individuals also had the higher rates of psychiatrist hospital/ED visits (H[3] = 8.03, P = .05) compared to the other three groups. No significant differences in clinical symptoms at intake (SAPS, SANS, BPRS) were found between groups (Table 3).
Figure 2.
The age of psychosis onset by group
*p < .05
**p < .01
Figure 3.
Global social and role functioning by group
Note. “Current” refers to ratings of participant’s current social and role functioning. “High” refers to ratings of participant’s highest functioning in the past year, and “Low” refers to ratings of the participant’s lowest functioning in the past year.
t = trend (p<0.1)
*p < .05
**p < .01
Figure 4.
Global assessment of functioning (GAF Score) by group
*p < .05
** p < .01
DISCUSSION
Both CT and AD are independently associated with poorer clinical symptoms and functioning in early psychosis at initial presentation for early psychosis care. AD alone was associated with an earlier age at psychosis onset, greater likelihood of NSSIB, and higher ratings of negative symptoms. CT alone was associated with earlier age at psychosis onset and more hospitalizations. Combined experiences of CT and AD, although not associated with psychosis symptom ratings, are associated with the earliest age at symptom onset and poorest psychosocial functioning prior to presenting for care. This finding supports the notion that CT may alter one’s developmental trajectory, both in terms of neurocognitive development and functioning, which in turn have implications for the development of psychopathology (Mayo et al., 2017). Research also suggests that AD increases vulnerability to trauma exposure: children enrolled in special education are at higher risk for abuse than their peers (Algood, Hong, Gourdine, & Williams, 2011).
Alternatively, individuals with AD may have less sophisticated coping mechanisms due to cognitive and developmental deficits, making them more vulnerable after CT exposure. Research has shown that strong cognitive abilities may boost resiliency among maltreated youth (Herrenkohl, Herrenkohl, & Egolf, 1994), putting AD youth at higher risk for psychopathology following CT than their typically developing peers. As the current study had an IQ cutoff of 70, it is possible that the impact of global cognitive functioning on these clinical outcomes are underreported here. Aligned with the proposed trauma-psychosis cycle, derailed developmental course may be even more pronounced in individuals with lower intellectual functioning, placing those individuals at even higher risk than what is captured in the current study. Future research should explore other impairments associated with AD (eg, low global IQ, social skills, emotional intelligence, social cognition, maturity) to understand their role in coping and increased risk for youth with both AD and CT history.
Furthermore, specific aspects of trauma are associated with varying degrees of risk. For example, prior research suggests that the age at which trauma exposure occurred may increase risk; early childhood exposure (ages 0-5) poses greater threat to development (Keiley, Howe, Dodge, Bates, & Pettit, 2001) compared to exposure at an older age. Additionally, trauma that is interpersonal in nature (ie, physical abuse perpetrated by a caregiver versus a natural disaster) is associated with higher rates of PTSD (Alisic et al., 2014). Due to small sample sizes within each trauma category and a lack of information on age at exposure, the current study was limited in its ability to examine how specific types of CT contribute to this interplay differently. Such details should be examined in future studies.
While this study had a substantial sample size, rates of CT reported here are lower than expected given previously reported prevalence rates ranging from 28% to 73% in an early psychosis population (Bendall, Jackson, Hulbert, & McGorry, 2007). This is likely due to the nature of retrospective data collection and that CT was not directly assessed. Although research is limited, rates of AD reported here were consistent with prior reported prevalence of learning disorders around 30% in a sample of individuals with schizophrenia (Hollis, 2003). Future research should use standardized evaluations to examine the impact of specific CT and AD categories on clinical course in early psychosis and individuals at clinical high risk, as well as the role of developmental and contextual protective factors, such as engagement with services, cognitive, social and emotional intelligence and family dynamics. Furthermore, the current study only examined clinical symptoms at initial presentation for early psychosis care. Future studies should examine longer-term trajectories of clinical course for those with combined risk factors.
Thorough assessment of clients’ developmental history and adverse childhood events may help clinicians identify important factors to consider for treatment, thereby improving clinical outcomes. Targeted developmental interventions, such as social skills development and school remediation, are key for AD individuals. Developmental approaches to early psychosis treatment are not typically discussed in the coordinated specialty care model; these results suggest the importance of doing so. Given the risk associated with CT (Springer, Sheridan, Kuo, & Carnes, 2007), trauma-focused interventions should also be included when appropriate (Cragin, Straus, Blacker, Tully, & Niendam, 2017). Among CT youth, family support predicts resilience and emotional well-being (Masten et al., 1999) and acts as a moderating factor between trauma exposure and the onset of PTSD (Day, 2013). Similarly, for AD youth, targeting family functioning and support is believed to yield the most successful outcomes via reductions in parent stress and increases in positive parenting (Dempsey, Keen, Pennell, O’Reilly, & Neilands, 2009). This suggests that CT + AD groups would benefit greatly from the incorporation of family support and involvement into early psychosis care.
This study reinforces the notion that early psychosis populations have a diverse set of risk factors impacting clinical presentation at initial presentation to care. To understand aetiology and for improving clinical interventions, the relationship between AD, CT and psychosis should continue to be explored.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the support of the research participants and families, who helped to make this work possible. This research was supported by the NIMH with 1K23MH087708 to T.A.N., 5R01MH059883 to C.S.C., and the Building Interdisciplinary Research Careers in Women’s Health award (K12 HD051958) awarded to L.M.T funded by the National Institute of Child Health and Human Development (NICHD), Office of Research on Women’s Health, Office of Dietary Supplements, and the National Institute of Aging.
Footnotes
CONFLICT OF INTEREST
Tara Niendam and Laura Tully are co-founders and shareholders in Safari Health, Inc.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- Addington J, Stowkowy J, Cadenhead KS, Cornblatt BA, McGlashan TH, Perkins DO, & Cannon TD (2013). Early traumatic experiences in those at clinical high risk for psychosis. Early intervention in psychiatry, 7(3), 300–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akyuz G, Sar V, Kugu N, & Doğan O (2005). Reported childhood trauma, attempted suicide and self-mutilative behavior among women in the general population. European Psychiatry, 20(3), 268–273. [DOI] [PubMed] [Google Scholar]
- Akyuz G, Sar V, Kugu N, & Doğan O (2005). Reported childhood trauma, attempted suicide and self-mutilative behavior among women in the general population. European Psychiatry, 20(3), 268–273. [DOI] [PubMed] [Google Scholar]
- Algood CL, Hong JS, Gourdine RM, & Williams AB (2011). Maltreatment of children with developmental disabilities: An ecological systems analysis. Children and Youth Services Review, 33(7), 1142–1148. [Google Scholar]
- Alisic E, Zalta AK, Van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, & Smid GE (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. The British Journal of Psychiatry, 204(5), 335–340. [DOI] [PubMed] [Google Scholar]
- Andreasen NC (1984a). Scale for the assessment of negative symptoms (SANS): University of Iowa; Iowa City. [Google Scholar]
- Andreasen NC (1984b). Scale for the assessment of positive symptoms (SAPS): University of Iowa; Iowa City. [Google Scholar]
- Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, & Caspi A (2011). Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. American Journal of Psychiatry, 168(1), 65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, … Yurgelun-Todd D (2017). Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Developmental cognitive neuroscience. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendall S, Jackson HJ, Hulbert CA, & McGorry PD (2007). Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophrenia bulletin, 34(3), 568–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandes D, Ben-Schachar G, Gilboa A, Bonne O, Freedman S, & Shalev AY (2002). PTSD symptoms and cognitive performance in recent trauma survivors. Psychiatry research, 110(3), 231–238. [DOI] [PubMed] [Google Scholar]
- Cannon M, Caspi A, Moffitt TE, Harrington H, Taylor A, Murray RM, & Poulton R (2002). Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder: results from a longitudinal birth cohort. Archives of general psychiatry, 59(5), 449–456. [DOI] [PubMed] [Google Scholar]
- Cornblatt BA, Auther AM, Niendam T, Smith CW, Zinberg J, Bearden CE, & Cannon TD (2007). Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophrenia Bulletin, 33(3), 688–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotter J, Kaess M, & Yung AR (2015). Childhood trauma and functional disability in psychosis, bipolar disorder and borderline personality disorder: a review of the literature. Irish Journal of Psychological Medicine, 32(1), 21–30. [DOI] [PubMed] [Google Scholar]
- Cragin CA, Straus MB, Blacker D, Tully LM, & Niendam TA (2017). Early Psychosis and Trauma-Related Disorders: Clinical Practice Guidelines and Future Directions. Frontiers in Psychiatry, 8(33). doi: 10.3389/fpsyt.2017.00033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Andrea W, Ford J, Stolbach B, Spinazzola J, & van der Kolk BA (2012). Understanding interpersonal trauma in children: Why we need a developmentally appropriate trauma diagnosis. American Journal of Orthopsychiatry, 82(2), 187. [DOI] [PubMed] [Google Scholar]
- Day T (2013). Resilience and Trauma in Maltreated Youth.
- Dempsey I, Keen D, Pennell D, O’Reilly J, & Neilands J (2009). Parent stress, parenting competence and family-centered support to young children with an intellectual or developmental disability. Research in developmental disabilities, 30(3), 558–566. [DOI] [PubMed] [Google Scholar]
- Feinberg I (1982). Schizophrenia: caused by a fault in programmed synaptic elimination during adolescence?. Journal of psychiatric research, 17(4), 319–334. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1996). Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV). Washington, DC: American Psychiatric Press. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1996). Structured clinical interview for DSM-IV axis I disorders, clinician version (SCID-CV). Washington, DC: American Psychiatric Press. [Google Scholar]
- Flashman LA, & Green MF (2004). Review of cognition and brain structure in schizophrenia: profiles, longitudinal course, and effects of treatment. Psychiatric Clinics of North America, 27(1), 1–18. doi: 10.1016/s0193-953x(03)00105-9 [DOI] [PubMed] [Google Scholar]
- Gothelf D, Feinstein C, Thompson T, Gu E, Penniman L, Van Stone E, Reiss AL (2007). Risk factors for the emergence of psychotic disorders in adolescents with 22q11. 2 deletion syndrome. American Journal of Psychiatry, 164(4), 663–669. [DOI] [PubMed] [Google Scholar]
- Grattan R, Tully L, Lesh T, Carter C, & Niendam T (2019). F64. Exploring the role of emotion dysregulation and impulsivity on suicidal ideation and behavior within an early psychosis population. Schizophrenia Bulletin, 45(Supplement_2), S279–S279. [Google Scholar]
- Hall RC (1995). Global assessment of functioning: a modified scale. Psychosomatics, 36(3), 267–275. [DOI] [PubMed] [Google Scholar]
- Herrenkohl EC, Herrenkohl RC, & Egolf B (1994). Resilient early school-age children from maltreating homes: Outcomes in late adolescence. American Journal of Orthopsychiatry, 64(2), 301. [DOI] [PubMed] [Google Scholar]
- Hollis C (2003). Developmental precursors of child-and adolescent-onset schizophrenia and affective psychoses: diagnostic specificity and continuity with symptom dimensions. The British Journal of Psychiatry, 182(1), 37–44. [DOI] [PubMed] [Google Scholar]
- Jonson-Reid M, Drake B, Kim J, Porterfield S, & Han L (2004). A prospective analysis of the relationship between reported child maltreatment and special education eligibility among poor children. Child maltreatment, 9(4), 382–394. [DOI] [PubMed] [Google Scholar]
- Kavanaugh BC, Dupont-Frechette JA, Jerskey BA, & Holler KA (2017). Neurocognitive deficits in children and adolescents following maltreatment: Neurodevelopmental consequences and neuropsychological implications of traumatic stress. Applied Neuropsychology: Child, 6(1), 64–78. [DOI] [PubMed] [Google Scholar]
- Keiley MK, Howe TR, Dodge KA, Bates JE, & Pettit GS (2001). The timing of
- Kelleher I, Keeley H, Corcoran P, Ramsay H, Wasserman C, Carli V, … & Cannon M (2013). Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. American Journal of Psychiatry, 170(7), 734–741. [DOI] [PubMed] [Google Scholar]
- Kim HS, Shin NY, Jang JH, Kim E, Shim G, Park HY, Kwon JS (2011). Social cognition and neurocognition as predictors of conversion to psychosis in individuals at ultra-high risk. Schizophrenia Research, 130(1), 170–175. [DOI] [PubMed] [Google Scholar]
- Lardinois M, Lataster T, Mengelers R, Van Os J, & Myin-Germeys I (2011). Childhood trauma and increased stress sensitivity in psychosis. Acta Psychiatrica Scandinavica, 123(1), 28–35. [DOI] [PubMed] [Google Scholar]
- Laurens KR, & Cullen AE (2016). Toward earlier identification and preventative intervention in schizophrenia: evidence from the London Child Health and Development Study. Social psychiatry and psychiatric epidemiology, 51(4), 475–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Garcia P, Ashby S, Patel P, Pierce KM, Meyer M, Rosenthal A, … & Niendam T (2019). Clinical and neurodevelopmental correlates of aggression in early psychosis. Schizophrenia research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukoff D, Nuechterlein K, & Ventura J (1986). Manual for the expanded brief psychiatric rating scale. Schizophrenia Bulletin, 12(4), 594–602. [Google Scholar]
- Macmanus D, Laurens KR, Walker E, Brasfield J, Riaz M, & Hodgins S (2012). Movement abnormalities and psychotic-like experiences in childhood: markers of developing schizophrenia? Psychological Medicine, 42(1), 99–109. [DOI] [PubMed] [Google Scholar]
- Masten AS, Hubbard JJ, Gest SD, Tellegen A, Garmezy N, & Ramirez M (1999). Competence in the context of adversity: Pathways to resilience and maladaptation from childhood to late adolescence. Development and psychopathology, 11(1), 143–169. [DOI] [PubMed] [Google Scholar]
- Mayo D, Corey S, Kelly LH, Yohannes S, Youngquist AL, Stuart BK, Loewy RL (2017). The role of trauma and stressful life events among individuals at clinical high risk for psychosis: a review. Frontiers in Psychiatry, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlashan TH: Structured Interview for Prodromal Syndromes (SIPS). New Haven: Yale University, 2001 [Google Scholar]
- Murray RM, Lewis SW. Is schizophrenia a neurodevelopmental disorder? Br Med J (Clin Res Ed). 1987;295(6600):681–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parellada M, Gomez-Vallejo S, Burdeus M, & Arango C (2017). Developmental Differences Between Schizophrenia and Bipolar Disorder. Schizophrenia Bulletin, 43(6), 1176–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petros N, Foglia E, Klamerus E, Beards S, Murray RM, & Bhattacharyya S (2016). Impact of childhood trauma on risk of relapse requiring psychiatric hospital admission for psychosis. The British Journal of Psychiatry, 209(2), 169–170. [DOI] [PubMed] [Google Scholar]
- Pompili M, Serafini G, Innamorati M, Lester D, Shrivastava A, Girardi P, & Nordentoft M (2011). Suicide risk in first episode psychosis: a selective review of the current literature. Schizophrenia research, 129(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Pompili M, Serafini G, Innamorati M, Lester D, Shrivastava A, Girardi P, & Nordentoft M (2011). Suicide risk in first episode psychosis: a selective review of the current literature. Schizophrenia research, 129(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, … & Mann J (2008). Columbia-suicide severity rating scale (C-SSRS). New York, NY: Columbia University Medical Center. [Google Scholar]
- Posner K, Brent D, Lucas C, Gould M, Stanley B, Brown G, & Mann J (2008). Columbia-suicide severity rating scale (C-SSRS). New York, NY: Columbia University Medical Center. [Google Scholar]
- Rapoport J, Giedd J, & Gogtay N (2012). Neurodevelopmental model of schizophrenia: update 2012. Molecular psychiatry, 17(12), 1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard-Devantoy S, Berlim MT, & Jollant F (2014). A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychological medicine, 44(8), 1663–1673. [DOI] [PubMed] [Google Scholar]
- Richard-Devantoy S, Szanto K, Butters MA, Kalkus J, & Dombrovski AY (2014). Cognitive inhibition in oder high-lethality suicide attempters. International Journal of Geriatric Psychiatry, 30(3), 274–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenkel LS, Spaulding WD, DiLillo D, & Silverstein SM (2005). Histories of childhood maltreatment in schizophrenia: relationships with premorbid functioning, symptomatology, and cognitive deficits. Schizophrenia Research, 76(2), 273–286. [DOI] [PubMed] [Google Scholar]
- Shannon C, Douse K, McCusker C, Feeney L, Barrett S, & Mulholland C (2009). The association between childhood trauma and memory functioning in schizophrenia. Schizophrenia Bulletin, 37(3), 531–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer KW, Sheridan J, Kuo D, & Carnes M (2007). Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child abuse & neglect, 31(5), 517–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahlberg O, Soderstrom H, Rastam M, & Gillberg C (2004). Bipolar disorder, schizophrenia, and other psychotic disorders in adults with childhood onset AD/HD and/or autism spectrum disorders. Journal of Neural Transmission, 111(7), 891–902. doi: 10.1007/s00702-004-0115-1 [DOI] [PubMed] [Google Scholar]
- Stahlberg O, Soderstrom H, Rastam M, & Gillberg C (2004). Bipolar disorder, schizophrenia, and other psychotic disorders in adults with childhood onset AD/HD and/or autism spectrum disorders. Journal of neural transmission, 111(7), 891–902. [DOI] [PubMed] [Google Scholar]
- Walker EF, & Diforio D (1997). Schizophrenia: a neural diathesis-stress model. Psychological review, 104(4), 667. [DOI] [PubMed] [Google Scholar]
- Wechsler D (1999). Manual for the Wechsler abbreviated intelligence scale (WASI). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Archives of general psychiatry. 1987;44(7):660–669. [DOI] [PubMed] [Google Scholar]