Abstract
Background
In February 2020, a coronavirus disease 2019 (COVID-19) outbreak was reported in fitness centers in Cheonan, Korea.
Methods
From February 24 to March 13, an epidemiological investigation was conducted on the fitness center outbreak. All those who were screened were tested for severe acute respiratory syndrome coronavirus-2 (SARS CoV-2) using real-time reverse transcriptase polymerase chain reaction. Contacts were traced and self-isolated for 14 days. We determined the epidemiological characteristics of confirmed cases of SARS-CoV-2 infection, and estimated the time-dependent reproduction number to assess the transmission dynamics of the infection.
Results
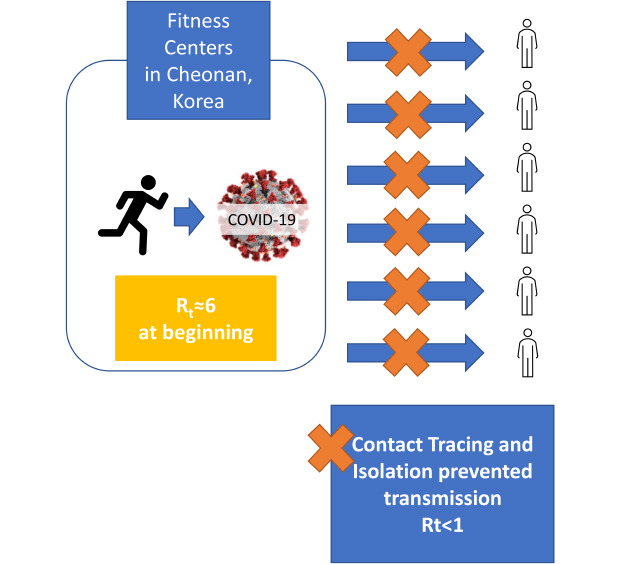
A total of 116 cases were confirmed, and 1,687 contacts were traced. The source cases were 8 Zumba instructors who led aerobics classes in 10 fitness centers, and had the largest average number of contacts. A total of 57 Zumba class participants, 37 of their family members, and 14 other contacts were confirmed as cases. The attack rate was 7.3%. The contacts at Zumba classes and homes had a higher attack rate than other contacts. The mean serial interval (± standard deviation) were estimated to be 5.2 (± 3.8) days. The time-dependent reproduction number was estimated to be 6.1 at the beginning of the outbreak, but it dropped to less than 1, 2 days after the epidemiological investigation was launched.
Conclusion
The results suggest that the COVID-19 outbreak was effectively contained with rigorous contact tracing, isolating, and testing in combination with social distancing without a lock-down.
Keywords: Coronavirus, Disease Outbreak, Epidemiology, Basic Reproduction Number, Fitness Centers
Graphical Abstract
INTRODUCTION
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and often presents with cough, fever, and shortness of breath. The severity varies from mild discomfort to fatal, and according to the Korea Centers for Disease Control and Prevention (KCDC), the crude case fatality rate in Korea is reported to be 3.02% among males and 1.91% among females as of May 2020.1 The first case in Korea, identified on January 19, 2020, was a Chinese woman traveling from Wuhan, China. She had fever of 38.3°C when she arrived at Incheon Airport, Korea.2 The 29th case reported in Korea was the first person who had not traveled to China, and the confirmation of this case was taken as a sign of imminent community spread. Soon, an outbreak at a church in Daegu which involved the 31st reported case, and another outbreak at a local hospital in Cheongdo dramatically increased the number of cases diagnosed in Korea. On February 23, within a week of the first outbreak, the Korean government raised its infectious disease alert level from Alert (Orange) to Serious (Red), and more people with respiratory symptoms were tested for SARS-CoV-2.3
On February 24, the first cases were confirmed in Cheonan, Chunchungnam-do (province), a city with population of 650,000. An official epidemiological investigation was launched jointly by the Chungnam Center for Infectious Disease Control & Prevention and the KCDC, in cooperation with local governments. The number of cases in Cheonan increased rapidly, and on February 27, 35 new cases were confirmed as having COVID-19. Among the newly confirmed cases, three with similar date of onset had reported attending the same fitness center. This was the first clue, and an outbreak associated with Zumba classes in fitness centers was identified in subsequent epidemiological investigations. As of March 11, a total of 116 cases of among instructors, students, their family members, and co-workers had been confirmed.4
Zumba is an exercise fitness program which combines aerobic exercise with music, and Oriental and Latin dance moves.5 In the fitness centers where the Zumba classes were held, a large number of students had taken classes in a relatively crowded space, although ventilation systems were working properly. Zumba is one of the most popular high-impact physical activities,6 and it provides benefits regarding cardiovascular, respiratory and proprioceptive functions.7,8,9 However, considering that COVID-19 is transmitted by droplet and fomites,10 high-impact group exercise in a confined indoor space, such as a Zumba class, could provide an environment prone to easy transmission of SARS-CoV-2 infection, as the droplets produced by exhalation or cough of a patient during the exercise have higher chance of reaching the nose, mouth or eye of other class participants directly, as well as remaining on the surface of the exercise equipment and later transmitted by contact.
The staff of a hospital where some of the cases were treated have reported on the clinical characteristics of 54 cases who were treated in their hospital.11 We included these cases in our investigation. However, the previous report was not based on the results of the official epidemiological investigation conducted by the KCDC, and it did not cover the all aspects of the outbreak, but described only a portion of the cases and contacts. In this report, we describe the epidemiological characteristics of the COVID-19 outbreak at fitness centers in Cheonan, Korea, based on the official epidemiological investigation, and document the effectiveness of contact tracing and isolation at containing the outbreaks.
METHODS
Diagnostic sampling and testing
From February 24 to March 13, 2020, all specimens of contacts were collected at designated screening centers/stations, based on the residential address of the contact. A total of 16 screening centers in 5 metropolitan cities/provinces, Cheonan and Asan in Chunchungnam-do, Sejong, Seoul, Daegu, and Gyeonggi-do, were visited by the contacts. In Sejong, Cheonan, and Asan, where most of the cases related to Zumba classes occurred, drive-through screening sites were opened on February 26 and 28, and March 3, respectively, and most contacts used this method.
Nasopharyngeal and oropharyngeal swab samples were collected from the contacts and sent to testing facilities selected by the KCDC which had been certified for quality control. Samples were tested for SARS-CoV-2 using real-time reverse transcriptase polymerase chain reaction (RT-PCR).
Contact tracing and isolation
During the outbreak, approximately 298 public health workers were involved in contact tracing and isolation: 13 epidemiological investigators, approximately 140 at screening centers/stations, and 145 in quick response teams.
When a person was confirmed with COVID-19, he or she was interviewed and asked the onset date of their symptoms. Then they were asked about their movements during the 14-days before the onset of symptoms. Closed-circuit television camera footage, tracking credit card usage, and retrieving GPS signal records of their mobile phone were used to identify possible transmission paths. Contact was defined as any person who had been within 2 m from a confirmed case from 1 day before symptom onset of the case, without appropriate personal protection. However, in practice, the technical definition may vary due to type of mask, symptom of confirmed case, duration of contact, exposure status and timing, and the designation of contact was made based on the final assessment by epidemiological investigators. The contacts were instructed within 24 hours of being identified as a contact to self-quarantine for 14 days, and their activities were monitored telephonically twice a day by a public health official. The contacts were tested for SARS-CoV-2 when they developed related symptoms. The screening policy for asymptomatic contacts differed from one local government to another, and not all asymptomatic contacts were tested. In order to identify undetected contacts, public announcements on the movement of the cases were made and those who had been to the same places as the cases were encouraged to seek testing if they developed any COVID-19-related symptoms. We recorded the daily number of contacts tested.
Demographic characteristics including age and sex, symptom onset date, the earliest and latest contact date with case were gathered by interviewing the patients at the time of epidemiological investigation. The symptom onset date of four cases who were identified by contact tracing could not be determined, and their dates of onset had not been recorded.
Statistical analysis
The contacts were divided into 3 groups: students, family, and others including co-workers according to the setting of contact. We calculated attack rate for each contact type, and the attack rates were averaged. We subtracted the earliest and the latest contact dates from onset date to estimate incubation period. We used the two dates at the beginning and end of the contact window to estimate the minimum and maximum possible incubation periods, and calculated the medians of the estimated minimum and maximum individual incubation periods.
We estimated serial interval and time-dependent reproduction number (Rt) as an indicator to measure the transmission of SARS-CoV-2. We estimated Rt based on the date of symptom onset, using package “R0”12 of R version 3.6.3.13 The serial interval was estimated based on the assumption of a gamma distribution. We also estimated the reproduction number of the present outbreak using the exponential growth method.
Ethics statement
The data were collected as part of an epidemiological investigation of KCDC, and ethical approval and individual consent were not applicable. The use of the data was approved by KCDC.
RESULTS
The epidemiological investigation revealed that the 8 Zumba instructors among the cases had attended a national Zumba instructors workshop in Cheonan, and contacted a unknown source case.4 These instructors led Zumba classes in 10 fitness centers. Zumba class students were contacted. Among the cases, 8 were Zumba instructors and 57 were their students, and additional 37 of their family members and 14 other contacts were diagnosed with COVID-19 during the outbreak. The instructors had highest average number of contacts (Table 1).
Table 1. Demographics of the confirmed cases in coronavirus disease 2019 outbreak in fitness centers in Cheonan, Korea.
| Variables | Type of case | ||||
|---|---|---|---|---|---|
| All | Instructors | Students | Family | Other | |
| No. of subjects | 116 | 8 | 57 | 37 | 14 |
| Age, yr | 39.1 ± 15.2 | 38.5 ± 7.4 | 43.6 ± 8.8 | 33.9 ± 21.6 | 35.1 ± 13.9 |
| Sex, female | 87 (75.0) | 8 (100.0) | 57 (100.0) | 11 (29.7) | 11 (78.6) |
| No. of contacts, persons | 14.5 ± 26.3 | 41.6 ± 45.0 | 13.5 ± 16.0 | 11.0 ± 32.5 | 12.6 ± 22.3 |
Data are presented as mean ± standard deviation or number (%).
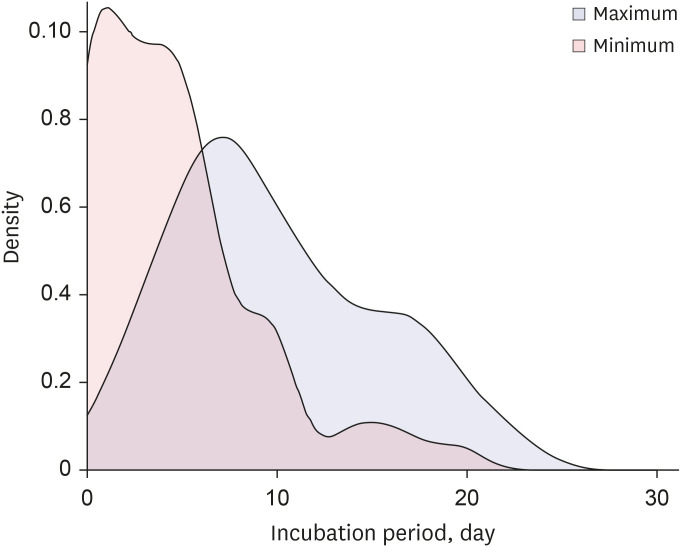
There were 1,687 contacts identified, and 108 were diagnosed (except the first cases from the national workshop, who were not contacts). The attack rate was 7.3%, but it was higher among the Zumba students (23.2% in fitness centers) and family members (21.6% in homes) (Table 2). Among family members, spouses of the cases had the highest attack rate (28%). The median incubation period is estimated between 4 and 9 days, and the maximum of the estimates of shortest and longest were 20 and 22 days, respectively (Fig. 1).
Table 2. Attack rates and incubation period of coronavirus disease 2019 outbreak in fitness centers in Cheonan, Korea.
| Variables | Place of contact | |||
|---|---|---|---|---|
| All | Fitness centers | Homes | Others | |
| No. of subjects | 1,687 | 233 | 200 | 1,254 |
| Diagnosed | 108 | 57 | 37 | 14 |
| Attack rates, % | 7.3 ± 16.8 | 23.2 ± 25.7 | 21.6 ± 35.3 | 1.7 ± 8.4 |
| Incubation periods, day, median rangea | 4–9 | 5–7 | 2–11 | 2.5–13 |
Data are presented as number or mean ± standard deviation.
aMedian range: The range between the medians of the shortest estimation and that of the longest estimation.
Fig. 1. Distributions of estimated incubation periods of coronavirus disease 2019 in fitness center outbreak in Cheonan. Maximum period was calculated by substracting earliest contact date from incidence date. Minimum period was calculated by substracting latest contact date from incidence date.
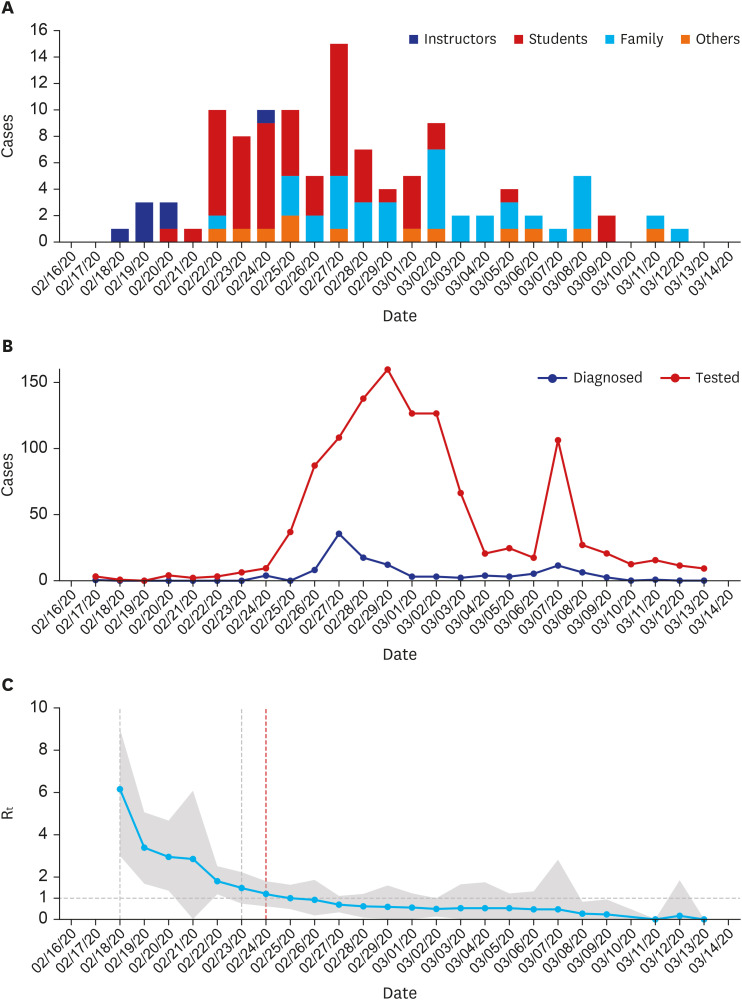
The mean serial interval (± standard deviation) was estimated to be 5.2 (± 3.8) days. The epidemic curve (Fig. 2A) shows the waves of transmission of SARS-CoV-2. The first wave was the students who were infected by the instructors, and the second wave included the exposed family members. The trend of the number of testing shows two peaks which are roughly coincide with the number of the diagnosed (Fig. 2B).
Fig. 2. Epidemiological characteristics of COVID-19 outbreak in fitness center in Cheonan, Korea. (A) Epidemic curve. (B) Trend of the number of the people tested for COVID-19 and diagnosed. (C) Time dependent reproduction number (Rt) and 95% confidence interval (grey area).
On Feb. 18th, the patient 31 was diagnosed, and on Feb. 23rd, the National Alert level was elevated to Serious (Red). On Feb. 24 (red vertical line), the fitness centers outbreak was identified, and the contact tracing and isolation began.
COVID-19 = coronavirus disease 2019.
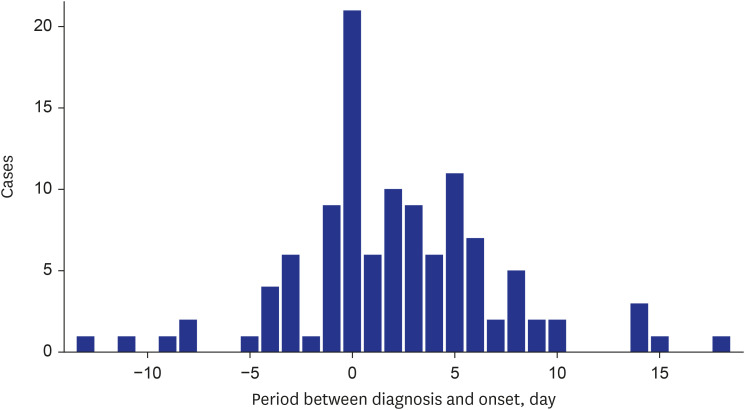
The highest number of testing were recorded on February 29, and 160 were tested. A total of 1,132 (66.4%) tests were conducted during the outbreak among the contacts. There was a mean of 2.2 (± 5.0) days between the date of symptom onset and diagnosis. Due to the pre-emptive diagnostic testing strategy, 30 cases of confirmed SARS-CoV-2 infection were asymptomatic at the time of diagnosis. They developed symptoms while under quarantine, and the longest interval between diagnosis and subsequent symptom onset was 13 days (Fig. 3). Among the initial asymptomatic patients, 4 transmitted SARS-CoV-2 infection to others.
Fig. 3. Distribution of period between diagnosis and symptom onset of coronavirus disease 2019 outbreak in fitness centers in Cheonan, Korea.
At the beginning of the outbreak, the Rt was estimated to be as high as 6.1, but it fell below 1 on February 26, 2 days after the initiation of the epidemiological investigation (Fig. 2C). The reproduction number of the present outbreak was 0.79 (95% CI, 0.66–0.93).
DISCUSSION
In the present study, we described epidemiological characteristics of a COVID-19 outbreak in fitness centers in Cheonan, Korea from February 24 to March 13, 2020. A total of 116 cases were diagnosed, and 1,687 contacts were isolated and traced.
As the epidemiological curve (Fig. 2A) shows, the SARS-CoV-2 infection was transmitted in waves, affecting the students and their family members. The attack rates were higher among contacts in the fitness centers and homes compared to other places. SARS-CoV-2 is transmitted by droplets and fomites,10 and the results of this investigation show that contacts in a confined indoor space, such as high intensity group exercises and homes, are more likely to become infected. Also, fitness centers and homes are places where social distancing and mask-wearing are hard to maintain, and contacts in these places are probably more vulnerable to infection. The attack rate among home contacts was higher than that reported at an outbreak at a call center in Seoul, Korea (16.2%).14 This may due to the different characteristics of the cases in the two outbreaks; the initial cases at homes in the present outbreak were mostly housewives (Zumba class enrollees), who spend a large amount of time at home and the chance of contacting other family members was probably higher than that among workers at a call center.
The mean period between diagnosis and symptom onset was 2.2 days, and this was achieved by contact tracing and isolating. Many took pre-emptive tests, and those who did not were closely monitored and tested as soon as they reported symptoms. This active contact tracing probably reduced the spread of SARS-CoV-2 in Korea, and the contact tracing eventually exceeded the transmission of the virus, ending the outbreak. For example, there were hospital staff and Cheonan City Hall officials among the cases whose routine daily activities bring them into contact with a large number of people and who thus probably have higher chance of transmitting the virus to the wider population, but this was successfully averted by early detection.
The mean serial interval reported in early stage of outbreak was 7.5 days in Wuhan,15 and 6.6 days in Korea.16 These estimates are longer than our estimate of 5.2 days. Other study analyzed pooled data extracted from published reports and estimated that the serial interval was 4.7 days,17 which is comparable to our estimate. The estimates in the previous reports were based relatively small numbers of cases: 6, 7, and 28 pairs in Wuhan, Korea, and pooled data, respectively, compared to our 116 cases. Another study from China of 291 cases showed that estimated median incubation period was 4 days.18 The authors estimated the incubation period by calculating the interval between the earliest contact date and the date of symptom onset, which is comparable to our method of shortest estimation, which was 4 days.
The Rt declined gradually from the beginning of the outbreak. When the outbreak was first identified in Cheonan on February 24, the Rt was already as low as 1.19, and the decrease cannot be entirely explained by the measures taken after the identification of the outbreak. The decline before the initiation of the epidemiological investigation may be explained by two factors. First, transmission in the earlier stage occurred in the confined indoor spaces where vigorous physical activities were taking place, and this might have provided more suitable environment for the virus to spread than in the later stage of the outbreak. The other factor is increased public awareness for COVID-19. February 18, the date of onset of the first case in our study, was the same day that the 31st patient in Korea was notified, which had heightened public awareness. The Korean government initiated official social distancing on February 22 and raised its infectious disease alert level to the highest on February 23, one day before the identification of the outbreak. It is possible that the increased awareness and national intervention had led public to adopt effective measures against the transmission of the virus before the present outbreak was identified. In Wuhan, China, Rt was used to demonstrate the effect of public health interventions, such as city lockdown and home quarantine.19 In 13 days, the Rt decreased from 3.80 to 1.02 after the initiation of city lock-down. Cheonan had not been locked down, but the effectiveness of the measures appears to have been similar. As of May 8, no cases have been reported in Cheonan since the last case was reported March 17, except for imported cases from other cities in Korea or from outside the country.
The were no case fatalities reported in the present outbreak. Among the 54 hospitalized cases that described previously and only 1 patient (1.9%) required treatment with supplementary oxygen.11 An ecological study showed that case fatality rate was positively associated with the cumulative number of cases and negatively associated with the intensity of testing.20 The favorable clinical outcome of the present outbreak is probably the result of early detection of contacts and rigorous testing forSARS-CoV-2.
A previous epidemiological investigation of an outbreak in a single call center in Seoul, Korea reported that 99.8% of traced contacts had been tested.14 The contacts in the present study were not as rigorously tested, since the national capacity for testing was still being mobilized as the time of the outbreak. However, the same principle of early tracing, isolating, and testing of the contacts was effectively applied to control the outbreak at multiple fitness centers in a city with population of 650,000.
ACKNOWLEDGMENTS
We would like to express appreciation to Hyunok Baek, Younglim Jeong, Hyeongi Lee, Youngmi Kim, Jeongdong Shin, Wontae Cho, Kwanyong Jeong (Chungnam Epidemiology and Case Management Team), Yeongju Na, Sohee Lee, Jinseon Choi (Cheonan Seo-buk-gu Public Health Center), Asan Public Health Center, and Sejong Special Self-Governing City Public Health Center for their efforts to investigate and respond to this outbreak of COVID-19.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclosure.
- Conceptualization: Bae S, Kwon HJ.
- Data curation: Kim H, Jung TY, Lim JA, Jo DH, Kang GS, Jeong SH, Choi DK, Kim HJ, Cheon YH, Chun MK, Kim M, Choi S, Chun C, Shin SH, Kim HK, Park YJ, Park O.
- Formal analysis: Bae S.
- Investigation: Kim H, Jung TY, Lim JA, Jo DH, Kang GS, Jeong SH, Choi DK, Kim HJ, Cheon YH, Chun MK, Kim M, Choi S, Chun C, Shin SH, Kim HK, Park YJ, Park O.
- Methodology: Bae S, Park O, Kwon HJ.
- Project administration: Park O, Kwon HJ.
- Supervision: Park O, Kwon HJ.
- Validation: Kim H, Park YJ, Park O, Kwon HJ.
- Visualization: Bae S.
- Writing - original draft: Bae S, Kim H, Chun MK.
- Writing - review & editing: Park YJ, Park O, Kwon HJ.
References
- 1.U.S. Food and Drug Administration. Accelerated emergency use authorization (EUA) summary. SARS-CoV-2 assay (Rutgers Clinical Genomics Laboratory) [Updated 2020]. [Accessed August 5, 2020]. https://www.fda.gov/media/136875/download.
- 2.Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020;35(5):e61. doi: 10.3346/jkms.2020.35.e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35(10):e112. doi: 10.3346/jkms.2020.35.e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chungnam Center for Infectious Disease Control and Prevention; Epidemiology & Case Management Team; Covid-19 National Emergency Response Center; Korea Centers for Disease Control and Prevention . Investigation of COVID-19 outbreaks through Zumba dance classes in Korea. Public Heal Wkly Rep. 2020;13(16):998–1005. [Google Scholar]
- 5.Micallef C. The effectiveness of an 8-week Zumba programme for weight reduction in a group of Maltese overweight and obese women. Sport Sci Health. 2014;10(3):211–217. [Google Scholar]
- 6.Ubago-Guisado E, Sánchez Sánchez J, Vila Maldonado S, Gallardo L. Effects of Zumba® and aquagym on bone mass in inactive middle-aged women. Medicina (Kaunas) 2019;55(1):1–10. doi: 10.3390/medicina55010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Domene PA, Moir HJ, Pummell E, Knox A, Easton C. The health-enhancing efficacy of Zumba® fitness: an 8-week randomised controlled study. J Sports Sci. 2016;34(15):1396–1404. doi: 10.1080/02640414.2015.1112022. [DOI] [PubMed] [Google Scholar]
- 8.Barranco-Ruiz Y, Ramírez-Vélez R, Martínez-Amat A, Villa-González E. Effect of two choreographed fitness group-workouts on the body composition, cardiovascular and metabolic health of sedentary female workers. Int J Environ Res Public Health. 2019;16(24):1–12. doi: 10.3390/ijerph16244986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luettgen M, Foster C, Doberstein S, Mikat R, Porcari J. Zumba(®): is the “fitness-party” a good workout? J Sports Sci Med. 2012;11(2):357–358. [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) Geneva: World Health Organization; 2020. [Google Scholar]
- 11.Jang S, Han SH, Rhee JY. Cluster of coronavirus disease associated with fitness dance classes, South Korea. Emerg Infect Dis. 2020;26(8):1917–1920. doi: 10.3201/eid2608.200633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boelle PY, Obadia T. R0: Estimation of R0 and Real-Time Reproduction Number from Epidemics. Vienna: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 13.R Core Team. R: a Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2020. [Google Scholar]
- 14.Park SY, Kim YM, Yi S, Lee S, Na BJ, Kim CB, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis. 2020;26(8):1666–1670. doi: 10.3201/eid2608.201274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ki M Task Force for 2019-nCoV. Epidemiologic characteristics of early cases with 2019 novel coronavirus (2019-nCoV) disease in Korea. Epidemiol Health. 2020;42:e2020007. doi: 10.4178/epih.e2020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishiura H, Linton NM, Akhmetzhanov AR. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis. 2020;93:284–286. doi: 10.1016/j.ijid.2020.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020;323(19):1–9. doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kenyon C. Flattening-the-curve associated with reduced COVID-19 case fatality rates- an ecological analysis of 65 countries. J Infect. 2020;81(1):e98–e99. doi: 10.1016/j.jinf.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]