Abstract
Introduction:
The number and outcomes of pregnancies experienced by a woman are consequential determinants of her health status. However, there is no published research comparing the patterns of subsequent pregnancy outcomes following a live birth, natural fetal loss, or induced abortion.
Objectives:
The objective of this study was to describe the characteristic patterns of subsequent pregnancy outcomes evolving from each of three initiating outcome events (birth, induced abortion, natural fetal loss) occurring in a Medicaid population fully insured for all reproductive health services.
Methods:
We identified 7,388,842 pregnancy outcomes occurring to Medicaid-eligible women in the 17 states which paid for abortion services between 1999-2014. The first known pregnancy outcome for each woman was marked as the index outcome which assigned each woman to one of three cohorts. All subsequent outcomes occurring up to the fifth known pregnancy were identified. Analyses of the three index outcome cohorts were conducted separately for all pregnancy outcomes, three age bands (<17, 17-35, 36+), and three race/ethnicity groups (Hispanic, Black, White).
Results:
Women with index abortions experienced more lifetime pregnancies than women with index births or natural fetal losses and were increasingly more likely to experience another pregnancy with each subsequent pregnancy. Women whose index pregnancy ended in abortion were also increasingly more likely to experience another abortion at each subsequent pregnancy. Both births and natural fetal losses were likely to result in a subsequent birth, rather than abortion. Women with natural losses were increasingly more likely to have a subsequent birth than women with an index birth. All age and racial/ethnic groups exhibited the characteristic pattern we have described for all pregnancy outcomes: abortion is associated with more subsequent pregnancies and abortions; births and fetal losses are associated with subsequent births. Other differences between groups are, however, apparent. Age is positively associated with the likelihood of a birth following an index birth, but negatively associated with the likelihood of a birth following an index abortion. Hispanic women are always more likely to have a birth and less likely to have an abortion than Black or White women, for all combinations of index outcome and the number of subsequent pregnancies. Similarly, Black women are always more likely to have an abortion and less likely to experience a birth than Hispanic or White women.
Conclusion:
Women experiencing repeated pregnancies and subsequent abortions following an index abortion are subjected to an increased exposure to hemorrhage and infection, the major causes of maternal mortality, and other adverse consequences resulting from multiple separation events.
Keywords: pregnancy outcomes, induced abortion, natural fetal loss, Medicaid
Introduction
A woman’s reproductive history is a consequential determinant of her health status. The number of pregnancies experienced, and the outcomes of each pregnancy, may impact the women’s own physical and mental health, longevity, and the outcomes of future subsequent pregnancies.1-7 Low income women may be particularly susceptible to the possibility of any adverse effects and, therefore, the costs of state Medicaid programs may also be impacted by the differences in the number and sequence of pregnancy outcomes, as well as any resultant health services utilization.
In our search of the existing literature, we found no published research on the patterns of subsequent pregnancy outcomes following a live birth, induced abortion, or natural fetal loss. While the reproductive history of each woman is influenced by multiple interacting medical and personal circumstances, an aggregated view of the different longitudinal trajectories of subsequent pregnancy outcomes can inform both the clinical research regarding the effect of pregnancy outcomes and the policy discussion regarding public funding of reproductive health services.
The Hyde Amendment bans the use of federal funds for abortion coverage except in cases of rape, incest, or life endangerment of the mother, which represent only a tiny fraction of induced abortions. However, 17 states have had a policy to use their own Medicaid funds to provide payment for essentially all abortions. In states that fund abortion, Medicaid beneficiaries represent more than half of all abortions.8 This circumstance provides an opportunity to investigate the sequencing of pregnancy outcomes over an extended period of time. Therefore, the objective of this study was to describe the characteristic patterns of subsequent pregnancy outcomes evolving from each of 3 initiating outcome events (birth, induced abortion, natural fetal loss) occurring in a Medicaid population fully insured for all reproductive health services.
Methods
Data were obtained from the enrollee-level Medicaid Analytic eXtract (MAX) licensed through the Centers for Medicare and Medicaid Services (CMS) Chronic Condition Data Warehouse’s (CCW) Medicaid data. At the time of this study data were available for years 1999 through 2014. The study population consisted of enrollees from the 17 states where Medicaid includes coverage of all reproductive health care services, including induced abortion. Due to lags in reporting timeframes not all states had submitted claims data through 2014. The last year of data relative to each of the states was 2012 for Alaska, Illinois, Maryland, Montana, and New Mexico; through 2013 for Arizona, Connecticut, Hawaii, Massachusetts, New York, Oregon, and Washington; and through 2014 for California, Minnesota, New Jersey, Vermont, and West Virginia.
The study population was limited to women over 13 years of age with at least one identifiable pregnancy outcome from 1999 through the latest year of data available for each state. During the study period all unique pregnancy outcomes were identified for each beneficiary using International Classification of Diseases, Ninth Revision (ICD9) codes. In addition, Current Procedural Terminology, 4th Edition (CPT4) and Healthcare Common Procedure Coding System (HCPCS) codes were utilized to verify pregnancy outcomes.
Based on these codes, all pregnancy outcomes were subdivided into 4 categories: live birth (ICD9 V27.0, V27.2, and V27.5), natural fetal loss (ICD9 V27.1, V27.4, V27.7, 630, 631, 633, 634), induced abortion (ICD9 635.xx, CPT4: 59840, 59841, 59850, 59851, 59852, 59855, 59856, 59857, and HCPCS: S0199, S2260, S2265, S2266, S2267, X7724, X7726, S0190, S0191), and undetermined (ICD9 636.xx, 637.xx, 638.xx). In order to uniquely define each pregnancy event, multiple diagnostic or treatment codes within 30 days of a pregnancy loss (natural, induced, or undetermined) were collapsed into a single pregnancy outcome using the first date associated with that cluster of Medicaid claims. Similarly, multiple diagnostic or treatment codes within 180 days of a delivery were collapsed into a single pregnancy outcome. Twins and multiple pregnancies resulting in a combination of both live birth and fetal loss were excluded from the analysis.
The first known pregnancy outcome for each beneficiary was marked as that woman’s index pregnancy. The index outcome is the first known pregnancy outcome for each beneficiary in this data set. At the index outcome, the beneficiary is assigned to 1 of 3 index outcome cohorts, and all subsequent outcomes occurring within the study period for pregnancies 2 to 5 are identified. The composite index cohort represents the actual summed totals of specific pregnancy outcomes in order of occurrence. Our analytical objective was to determine whether there were significant differences in the patterns of pregnancies subsequent to each of 3 index pregnancy outcomes. Since these patterns involved multiple outcomes with sequential and incremental effects, no multivariate model with a single dependent outcome could represent all dimensions of these patterns. We concluded that a comprehensive descriptive approach would enable detection of significant differences in the overall pattern and also enable comparison for each index outcome/subsequent pregnancy combination.
Tables were constructed to identify subsequent pregnancy outcomes for each index outcome cohort. A comprehensive analysis was conducted separately for all pregnancy outcomes, 3 age bands (<17, 17-35, 36+), and 3 race/ethnicity groups (Hispanic, black, white). Women were placed in age bands based upon their age at the time of the index pregnancy outcome without consideration of age at each subsequent pregnancy outcome. For all group comparisons, we calculated odds ratios (OR) and confidence intervals (CI) for P < .05. Summary analytic tables were created using (SAS/STAT) software, version (10) of the SAS System for (Unix). Copyright (2019) SAS Institute Inc. All comparative analyses were completed using Microsoft Excel (Version 16).
Findings
The Study Population
During the study period, 7 388 842 pregnancy outcomes were identified as either a live birth, natural loss, or induced abortion which occurred as the index through the fifth pregnancy (Table 1). Another 540 393 pregnancy outcomes were undetermined. With each successive pregnancy, a decreasing percent of births and an increasing percent of abortions were apparent. Births were 81.4% of the known outcomes of index pregnancies but only 51.6% of the known fifth pregnancy outcomes. Abortions, by contrast increased from 9.0% of the index pregnancies to 33.1% of fifth pregnancies. Natural losses also increased from 9.6% of the index pregnancies to 15.3% of known fifth pregnancies.
Table 1.
Total Pregnancy Outcomes, Index and Subsequent 2 to 5 Number and Percent of Known Outcomes.
| Cohort pregnancy number | Live birth | % Known | Natural loss | % Known | Induced abortion | % Known | Undetermined | Grand total |
|---|---|---|---|---|---|---|---|---|
| Index | 3 807 694 | 81.40% | 449 182 | 9.60% | 421 011 | 9.00% | 288 662 | 4 966 549 |
| 2 | 1 178 787 | 72.10% | 208 712 | 12.80% | 247 432 | 15.10% | 140 527 | 1 775 458 |
| 3 | 427 171 | 64.80% | 94 926 | 14.40% | 136 847 | 20.80% | 66 078 | 725 022 |
| 4 | 165 370 | 58.00% | 42 782 | 15.00% | 76 967 | 27.00% | 30 388 | 315 507 |
| 5 | 68 047 | 51.60% | 20 171 | 15.30% | 43 743 | 33.10% | 14 738 | 146 699 |
| Grand total | 5 647 069 | 76.40% | 815 773 | 11.00% | 926 000 | 12.50% | 540 393 | 7 929 235 |
Subsequent Pregnancies
Table 2 and Figure 1 show the pattern of pregnancy outcomes for each index pregnancy cohort. Women whose index pregnancy was an induced abortion experienced more subsequent pregnancies than women with other index pregnancy outcomes. The 421 011 women who had index pregnancy abortions experienced 425 814 known outcomes of subsequent pregnancies 2 to 5, or 101% of the number of index pregnancies. Women with index pregnancy births and natural losses had significantly fewer subsequent total pregnancies 2 to 5 (2 167 955; 56.9% and 368 917; 82.1%, respectively). Women with index pregnancy abortions were also increasingly more likely to experience a pregnancy following each subsequent pregnancy than were women with index pregnancy births: second pregnancy OR: 1.84, CI (1.83-1.85); third pregnancy OR: 2.36, CI (2.35-2.38); fourth pregnancy OR: 3.04, CI (3.01-3.07); fifth pregnancy OR: 3.86, CI (3.81-3.91).
Table 2.
Total Pregnancy Outcomes for Index and Subsequent Pregnancies, Number and Percent of Pregnancies 2 to 5, and the Index Outcome Cohort.
| Index pregnancy live birth | Live birth | % of Known | Natural loss | % of Known | Induced abortion | % of known | Undetermined | Total | % of Cohort (Table 1) |
| 2nd Pregnancy | 986 834 | 79.1% | 131 302 | 10.5% | 129 168 | 10.4% | 99 587 | 1 346 891 | 35.4% |
| 3rd Pregnancy | 339 676 | 72.0% | 62 704 | 13.3% | 69 423 | 14.7% | 45 936 | 517 739 | 13.6% |
| 4th Pregnancy | 126 645 | 66.2% | 27 470 | 14.4% | 37 086 | 19.4% | 20 241 | 211 442 | 5.6% |
| 5th Pregnancy | 50 294 | 60.9% | 12 279 | 14.9% | 20 069 | 24.3% | 9241 | 91 883 | 2.4% |
| Total | 1 503 449 | 75.4% | 233 755 | 11.7% | 255 746 | 12.8% | 175 005 | 2 167 955 | 56.9% |
| Index pregnancy natural loss | Live birth | % of Known | Natural loss | % of Known | Induced abortion | % of Known | Undetermined | Total | % of cohort (Table 1) |
| 2nd Pregnancy | 120 189 | 62.7% | 60 305 | 31.5% | 11 220 | 5.9% | 25 670 | 217 384 | 48.4% |
| 3rd Pregnancy | 51 326 | 62.4% | 22 020 | 26.8% | 8921 | 10.8% | 10 881 | 93 148 | 20.7% |
| 4th Pregnancy | 20 710 | 58.3% | 9570 | 27.0% | 5219 | 14.7% | 4731 | 40 230 | 9.0% |
| 5th Pregnancy | 8515 | 53.1% | 4540 | 28.3% | 2978 | 18.6% | 2122 | 18 155 | 4.0% |
| Total | 200 740 | 61.7% | 96 435 | 29.6% | 28 338 | 8.7% | 43 404 | 368 917 | 82.1% |
| Index pregnancy induced abortion | Live birth | % of Known | Natural loss | % Known | Induced abortion | % of Known | Undetermined | Total | % of Cohort (Table 1) |
| 2nd Pregnancy | 71 764 | 36.6% | 17 105 | 8.7% | 107 044 | 54.6% | 15 270 | 211 183 | 50.2% |
| 3rd Pregnancy | 36 169 | 34.5% | 10 202 | 9.7% | 58 503 | 55.8% | 9 261 | 114 135 | 27.1% |
| 4th Pregnancy | 18 015 | 30.8% | 5742 | 9.8% | 34 662 | 59.3% | 5416 | 63 835 | 15.2% |
| 5th Pregnancy | 9238 | 27.8% | 3352 | 10.1% | 20 696 | 62.2% | 3375 | 36 661 | 8.7% |
| Total | 135 186 | 34.4% | 36 401 | 9.3% | 220 905 | 56.3% | 33 322 | 425 814 | 100.1% |
| Subsequent pregnancy totals | 1 839 375 | 67.8% | 366 591 | 13.5% | 504 989 | 18.6% | 251 731 | 2 962 686 | 59.7% |
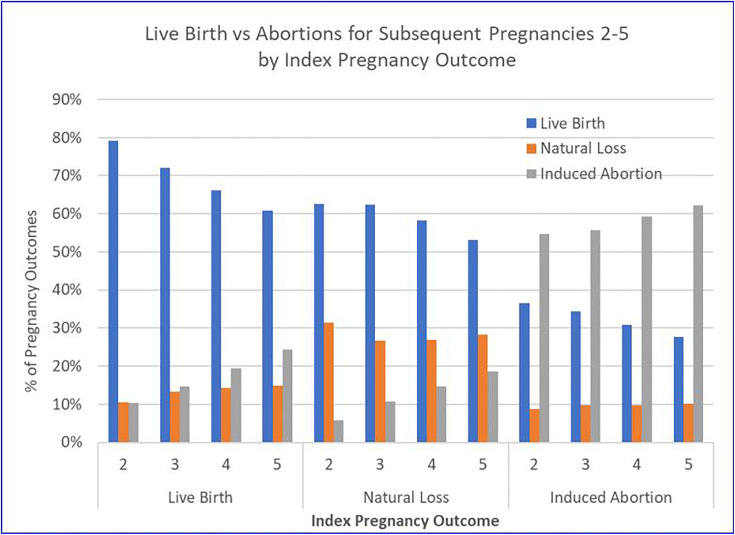
Figure 1.
Live Birth vs. Abortions for Subsequent Pregnancies 2-5 by Index Pregnancy Outcome.
Subsequent Pregnancy Outcomes
Women whose index pregnancy ended in abortion had more abortions than any other pregnancy outcome for subsequent pregnancies 2 to 5; and they increasingly selected abortion over birth with each subsequent pregnancy, as shown in Table 2 and Figure 1: second pregnancy OR: 1.49, CI (1.48-1.51); third pregnancy OR: 1.62, CI (1.60-1.64); fourth pregnancy OR: 1.92, CI (1.89-1.96); fifth pregnancy OR: 2.24, CI (2.19-2.30).
Women who had index pregnancy births had more births than any other known pregnancy outcome for subsequent pregnancies 2 to 5, but abortion did become more likely with each subsequent pregnancy.
The 3 807 694 women who had index pregnancy births consistently but decreasingly selected birth rather than abortion for subsequent outcomes: second pregnancy OR: 7.64, CI (7.59-7.69); third pregnancy OR: 4.89, CI (4.85-4.93); fourth pregnancy OR: 3.41, CI (3.38-3.45); fifth pregnancy OR: 2.51, CI (2.47-2.55).
Women who had experienced index natural losses (n = 449 182) were increasingly more likely than index birth women to have a live birth in subsequent pregnancies: second pregnancy OR: 2.39, CI (2.36-2.41); third pregnancy OR: 2.68, CI (2.65-2.72); fourth pregnancy OR: 3.57, CI (3.50-3.64); fifth pregnancy OR: 4.52, CI (4.40-4.65).
Age and Subsequent Pregnancy Outcomes
All 3 age bands (<17, 17-35, 36+) exhibited the characteristic patterns of post index pregnancy outcomes we have previously described for the entire study population of pregnancy outcomes (see Table 3 and Figure 2). That is, the abortion of an index pregnancy was associated with an increased likelihood of a subsequent abortion, which increased with each pregnancy, and the decreasing likelihood of a birth. Index births and fetal losses were associated with a greater likelihood that subsequent pregnancies would end in a birth, though the likelihood of abortion increased and the likelihood of a birth decreased with each subsequent pregnancy.
Table 3.
Total Pregnancy Outcomes for Index and Subsequent Outcomes 2 to 5, by 3 Age Bands.
| Pregnancy outcomes—index and subsequent | Age | |||||
|---|---|---|---|---|---|---|
| <17 | 17-35 | 36+ | ||||
| Number | % Known | Number | % Known | Number | % Known | |
| Live birth | 130 267 | 1 605 946 | 22 982 | |||
| Live birth | 106 552 | 1 376 584 | 20 313 | |||
| 2 | 59 097 | 76.2% | 911 226 | 79.5% | 16 511 | 71.5% |
| 3 | 28 618 | 71.0% | 308 247 | 72.2% | 2811 | 59.0% |
| 4 | 13 139 | 65.5% | 112 773 | 66.4% | 733 | 53.5% |
| 5 | 5698 | 59.3% | 44 338 | 61.1% | 258 | 53.8% |
| Abortion | 23 715 | 78.4% | 229 362 | 68.0% | 2669 | 37.7% |
| 2 | 10 052 | 13.0% | 117 138 | 10.2% | 1978 | 8.6% |
| 3 | 6742 | 16.7% | 62 167 | 14.6% | 514 | 10.8% |
| 4 | 4299 | 21.4% | 32 650 | 19.2% | 137 | 10.0% |
| 5 | 2622 | 27.3% | 17 407 | 24.0% | 40 | 8.3% |
| Induced abortion | 40 866 | 307 903 | 7322 | |||
| Live birth | 17 719 | 115 676 | 1791 | |||
| 2 | 8757 | 43.5% | 61 718 | 36.4% | 1289 | 21.2% |
| 3 | 4951 | 39.6% | 30 864 | 34.1% | 354 | 19.8% |
| 4 | 2636 | 34.7% | 15 269 | 30.4% | 110 | 18.2% |
| 5 | 1375 | 30.0% | 7825 | 27.5% | 38 | 18.3% |
| Abortion | 23 147 | 215.8% | 192 227 | 233.6% | 5531 | 257.3% |
| 2 | 9764 | 48.5% | 93 393 | 55.0% | 3887 | 63.9% |
| 3 | 6352 | 50.9% | 51 038 | 56.3% | 1113 | 62.2% |
| 4 | 4267 | 56.1% | 30 002 | 59.8% | 393 | 64.9% |
| 5 | 2764 | 60.3% | 17 794 | 62.4% | 138 | 66.3% |
| Natural loss | 17 906 | 203 064 | 8108 | |||
| Live birth | 15 194 | 178 367 | 7179 | |||
| 2 | 7882 | 67.5% | 106 897 | 64.2% | 5410 | 40.2% |
| 3 | 4262 | 65.4% | 45 738 | 63.3% | 1326 | 38.4% |
| 4 | 2057 | 60.6% | 18 315 | 59.2% | 338 | 29.4% |
| 5 | 993 | 55.9% | 7417 | 53.8% | 105 | 22.0% |
| Abortion | 2712 | 60.4% | 24 697 | 50.0% | 929 | 22.3% |
| 2 | 847 | 7.3% | 9755 | 5.9% | 618 | 4.6% |
| 3 | 862 | 13.2% | 7841 | 10.8% | 218 | 6.3% |
| 4 | 619 | 18.2% | 4534 | 14.6% | 66 | 5.7% |
| 5 | 384 | 21.6% | 2567 | 18.6% | 27 | 5.7% |
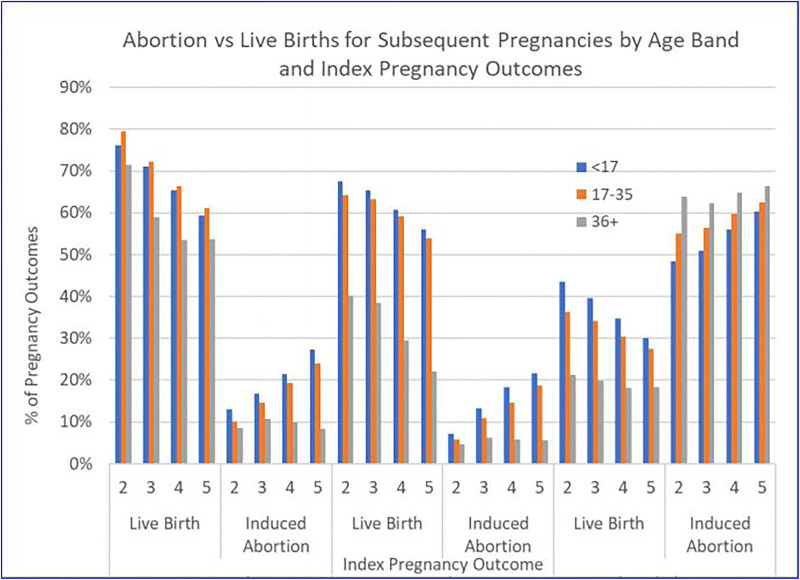
Figure 2.
Abortion vs. Live Births for Subsequent Pregnancies by Age Band and Index Pregnancy Outcomes.
Women under the age of 17 who experience an index birth are always more likely to experience another birth rather than an abortion for subsequent pregnancies 2 to 5: second OR: 6.56, CI (6.32-6.79); third pregnancy OR: 5.45, CI (5.20-5.70); fourth pregnancy OR: 4.95, CI (4.66-5.25); fifth pregnancy OR: 4.37, CI (4.03-4.73). At the second pregnancy, they are 5.8 times more likely to have a birth than an abortion. By the fifth pregnancy, they are 2.2 times as likely.
Women ages 17 to 35 who experience an index birth are similarly more likely to experience another birth rather than an abortion at any subsequent pregnancy: second pregnancy OR: 11.77, CI (11.63-11.91); third pregnancy OR: 8.20, CI (8.07-8.33); fourth pregnancy OR: 6.79, CI (6.65-6.03); fifth pregnancy OR: 5.79, CI (5.64-5.95). At the second pregnancy, they are 7.9 times more likely to have a birth than an abortion. By the fifth pregnancy, they are 2.5 times as likely.
Women 36+ who experience an index birth are also more likely to experience another birth rather than an abortion at any subsequent pregnancy: second pregnancy OR: 25.17, CI (23.27-27.22); third pregnancy OR: 17.19, CI (15.12-19.55); fourth pregnancy OR: 19.12, CI (15.39-23.74); fifth pregnancy OR: 23.42, CI (16.31-33.64). At second pregnancy, they are 8.3 times more likely to have a birth than an abortion. By the fifth pregnancy, they are still 6.6 times as likely.
Therefore, following an index birth, age is positively associated with the likelihood of a birth. That is, women 36+ are the most likely to select birth rather than abortion for subsequent pregnancies. However, following an index abortion, age is negatively associated with the likelihood of a subsequent birth. Women 36+ are increasingly less likely to experience a birth after an index abortion, and more likely to abort any subsequent pregnancy.
Following an index natural loss, women <17 were increasingly more likely to have a birth at each subsequent pregnancy than women 36+: second pregnancy OR: 3.10, CI (2.94-3.26); third pregnancy OR: 3.04, CI (2.79-3.31); fourth pregnancy OR: 3.70, CI (3.20-4.28); fifth pregnancy OR: 4.50, CI (3.55-5.70). Note for all age groups and for all subsequent pregnancies the strong preference for a live birth rather than an abortion following a natural fetal loss. For the second pregnancy, women <17 were 9.2 times (OR: 26.59, CI: 24.55-28.81) more likely to have a birth than an abortion. Women 17 to 35 were 10.9 times as likely (OR: 28.79, CI: 28.14-29.46), and women 36+ were 8.7 times as likely (OR: 13.96, CI: 12.79-15.25).
Race and Subsequent Pregnancy Outcomes
All racial and ethnic groups exhibited the same trend in pregnancy outcome patterns described above. Specifically, an index birth predicted more birth outcomes in subsequent pregnancies whereas an index abortion predicted more subsequent abortions. However, some racial and ethnic differences were observed.
As shown in Table 4 and Figure 3, the distribution of outcomes relative to the index pregnancy had significant racial differences. Hispanic women had the highest percent of index births (86.8%) and the lowest percent of index abortions (3.4%). Black women had the index lowest percent of births (72.3%) and the highest percent of index abortions (16.8%).
Table 4.
Total Pregnancy Outcomes for Index and Subsequent Outcomes 2 to 5, by Race.
| Pregnancy outcomes—index and subsequent | Race | |||||
|---|---|---|---|---|---|---|
| Hispanic number | % Known | White Number | % Known | Black number | % known | |
| Live birth | 1 073 021 | 81.9% | 1 397 065 | 76.7% | 637 464 | 68.0% |
| Live birth | ||||||
| 2 | 304 817 | 85.5% | 381 585 | 80.7% | 155 708 | 65.0% |
| 3 | 99 824 | 80.4% | 135 117 | 75.0% | 63 163 | 57.6% |
| 4 | 33 379 | 75.3% | 51 910 | 71.3% | 27 310 | 51.7% |
| 5 | 11 869 | 71.3% | 21 223 | 67.8% | 12 219 | 46.7% |
| Abortion | ||||||
| 2 | 15 279 | 4.3% | 39 463 | 8.3% | 54 392 | 22.7% |
| 3 | 8301 | 6.7% | 20 220 | 11.2% | 31 224 | 28.5% |
| 4 | 4448 | 10.0% | 10 301 | 14.1% | 17 954 | 34.0% |
| 5 | 2470 | 14.8% | 5224 | 16.7% | 10 331 | 39.5% |
| Induced abortion | 154 871 | 8.5% | 154 871 | 8.5% | 148 375 | 15.8% |
| Live birth | ||||||
| 2 | 9117 | 42.5% | 25 391 | 37.2% | 27 208 | 33.8% |
| 3 | 4909 | 41.4% | 12 549 | 36.5% | 14 412 | 30.3% |
| 4 | 2529 | 37.8% | 5841 | 32.8% | 7776 | 27.0% |
| 5 | 1295 | 34.6% | 2746 | 29.1% | 4392 | 25.0% |
| Abortion | ||||||
| 2 | 10 353 | 48.2% | 37 024 | 54.2% | 46 071 | 57.3% |
| 3 | 5751 | 48.5% | 18 555 | 53.9% | 28 515 | 59.9% |
| 4 | 3451 | 51.6% | 10 230 | 57.4% | 18 190 | 63.1% |
| 5 | 2075 | 55.4% | 5751 | 60.9% | 11 417 | 64.9% |
| Natural loss | 165 214 | 9.1% | 165 214 | 9.1% | 95 832 | 10.2% |
| Live birth | ||||||
| 2 | 32 686 | 65.6% | 46 706 | 63.8% | 24 740 | 57.6% |
| 3 | 13 893 | 67.3% | 20 813 | 65.3% | 10 703 | 53.0% |
| 4 | 5315 | 63.7% | 8510 | 62.1% | 4741 | 49.1% |
| 5 | 2039 | 57.6% | 3534 | 58.5% | 2164 | 44.3% |
| Abortion | ||||||
| 2 | 1301 | 2.6% | 3873 | 5.3% | 4640 | 10.8% |
| 3 | 1026 | 5.0% | 2814 | 8.8% | 4053 | 20.1% |
| 4 | 574 | 6.9% | 1583 | 11.5% | 2537 | 26.3% |
| 5 | 315 | 8.9% | 871 | 14.4% | 1550 | 31.7% |
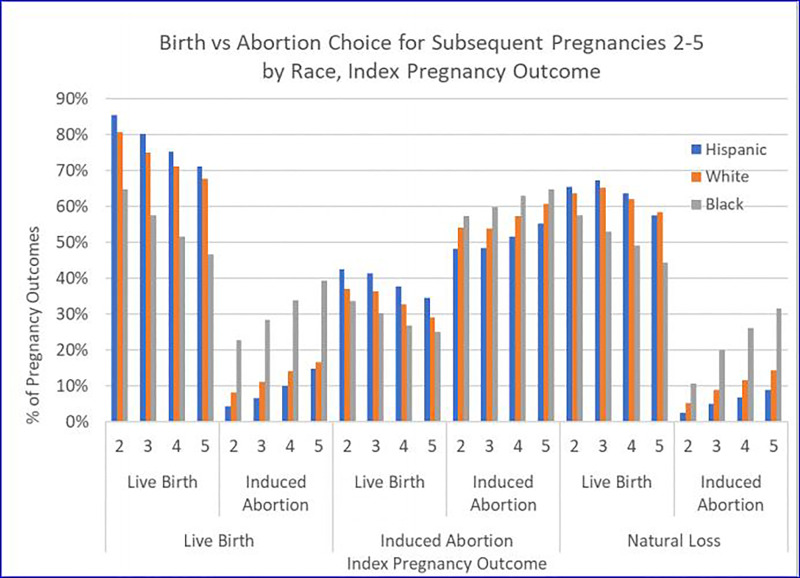
Figure 3.
Births vs. Abortion Choice for Subsequent Pregnancies 2-5 by Race, Index Pregnancy Outcome.
Following a live birth index outcome, Hispanic women were always more likely to experience a subsequent birth and less likely to experience a subsequent abortion than white or black women. Hispanic women were 21.2 times (OR: 132.03, CI: 129.58-134.52) more likely to have a birth rather than an abortion for a second subsequent pregnancy following an index birth. Black women who had an index birth were 2.9 times (OR: 6.32, CI: 6.24-6.40) more likely to experience a birth rather than abortion.
Following an index abortion, black women were more likely than white and Hispanic women to have an induced abortion and less likely to have a live birth for subsequent pregnancies 2 to 5. As always, the likelihood of an abortion increased with every subsequent pregnancy.
Following an index natural loss, similar to the pattern following an index live birth, live birth was preferred overwhelmingly to abortion for subsequent pregnancies. Even here, however, the high prevalence of abortion for black women was noteworthy. For subsequent pregnancies 2 to 5, and following an index natural loss, black women were 4.1 times (OR: 4.52, CI: 4.24-4.81), 4.1 times (OR: 4.80, CI: 4.48-5.15), 3.8 times (OR: 4.82, CI: 4.40-5.28), and 3.6 times (OR: 4.76, CI: 4.23-5.27) more likely to experience an abortion than Hispanic women.
Discussion
Abortion is associated with a starkly different pattern of subsequent pregnancy outcomes as compared to the pattern that is more common following live birth or natural fetal loss. Moreover, abortion is associated with an increase in the total number of pregnancies a woman will experience, and those pregnancies are more likely to result in subsequent abortions. Births and natural fetal losses, by contrast, are more likely to be followed by subsequent births.
Experiencing an index abortion is associated with an increase in the total number of pregnancies experienced by a woman in her lifetime. Each pregnancy involves the separation of the mother and the embryo/fetus. Maternal mortality encompasses live birth mortality but also mortality from all other pregnancy outcomes including induced abortion.9 Maternal deaths from hemorrhage and infection, the major causes of maternal mortality worldwide, occur at the time of the separation event. The more frequent the separation events, the more often a woman is exposed to risk. The hope that easier access to abortion would decrease maternal mortality has been rebutted by evidence to the contrary.10-12 These findings demonstrating that low-income women who have abortions are more likely to have more overall pregnancies, including more subsequent abortions, would tend to support the body of evidence indicating that abortion is associated with greater subsequent reproductive health risks.13,14
Abortion decreases the likelihood of a birth in any subsequent pregnancy. More than 60% of surveyed women seeking an abortion indicate that they had not completed their childbearing.15 Yet our findings show that abortion decreases the likelihood of a birth in the immediate subsequent pregnancy. This finding is inconsistent with the idea that abortion is primarily used to optimize child spacing. Instead, our finding supports the view that women who have experienced abortions may be more likely to seek replacement pregnancies, consciously or unconsciously, which may then result in more subsequent abortions because the pressures leading to the initial abortion remain unresolved.16 Repeat abortions may also be evidence that some women undergo multiple abortions as a form of self-punishment.16 Conflicting feelings over becoming pregnant (on one hand, a desire for a replacement pregnancy; on the other, a desire to avoid another pregnancy) may lead to more risk-taking behavior in the form of irregular birth control practices and reliance on less reliable methods of contraception. This pattern is suggested by a study regarding the advance provision of emergency contraception (EC) which found that over 65% of young women reported inconsistent use of birth control and that those provided with EC took even more risks relative to their birth control options.17 While the correlates and determinants of these patterns are subject to alternative explanations, the pregnancy outcome trajectory described here is clear: abortion begets abortion.
Support for public funding of abortion is partly based upon the assumption that it will enable women to continue their education and careers and stabilize their personal relationships, thus enabling a happier and healthier life. A cascade of repetitive pregnancies and abortions, however, is likely to subject a woman to the various adverse effects associated with these outcomes.
There are limitations related to the use of Medicaid claims data. Medicaid-eligible beneficiaries are by definition financially disadvantaged and are not representative of all women experiencing abortion. Conversely, a data set composed entirely of low-income women may also be considered an advantage since results are unlikely to be explained by differences in income or other factors strongly associated with income. Services received by eligible women but paid by another source (eg, out of pocket) are not included in the claims data. Services received when the women were not eligible are similarly not included. Administrative data are also subject to limitations regarding coding errors, inconsistent coding, and the exclusion of codes considered nonessential for billing. 18,19 There are inconsistencies in coding which may vary by state. Our data extraction protocol required an ICD code to identify beneficiaries who had an induced abortion. To the extent that some states or individual providers do not code an abortion with an ICD code, our study population may undercount the number of abortions. This undercount would likely be due to a random variation in coding protocols and is unlikely to affect the trends related in our findings.
The findings described here are also a prelude to future explanatory analyses, utilizing multivariate methods, which enable a more granular understanding of these outcomes. For example, the interpregnancy time interval associated with the index events may be influenced by sociodemographic factors as well as pre-index outcome health services utilization. Similarly, comparison of subpopulations of interest defined by this analysis can be addressed with multivariate methods, such as the demographic and regional differences in populations of Medicaid women without births versus those without abortions.
The results of this study suggest that Medicaid funding of abortion may have a direct impact on the number and outcome of subsequent pregnancies. Additional research is necessary to examine the impact of pregnancy outcome differences on total health care utilization, including hospitalizations, emergency room visits, prescription drug history, and psychiatric and behavioral services. Further research into this domain is essential.
Author Biographies
James Studnicki is currently Vice President and Director of Data Analytics at the Charlotte Lozier Institute in Arlington, Virginia. Over a span of four decades, he held academic appointments at the Johns Hopkins University School of Hygiene and Public Health, the University of South Florida College of Public Health, and the University of North Carolina, Charlotte, where for ten years he served as the Irwin Belk Endowed Chair in Health Services Research. Dr. Studnicki holds Doctor of Science (ScD) and Master of Public Health (MPH) degrees from Johns Hopkins and a Master of Business Administration (MBA) from the George Washington University.
John W. Fisher is currently an Associate Scholar at the Charlotte Lozier Institute. Following a 22 year career as a nuclear submarine officer, he served as the Director of Life Support and engineering at the Florida Aquarium, Chief Financial Officer of Technology Transfer Services, and 10 years as an Assistant Professor at the University of North Carolina at Charlotte College of Health and Human Services. Dr. Fisher holds a PhD in Information Systems and Decision Sciences from the University of South Florida, a JD from Massachusetts School of Law, and Master's degrees from the Massachusetts Institute of Technology (Ocean Engineering), University of Notre Dame (Administration), Indiana University (Business Administration), and the United States Naval War College (National Security Policy). He is currently a member of the bar in New Hampshire and Massachusetts.
David C. Reardon is the director of Elliot Institute, a biomedical ethicist, and a lead author on numerous studies and books examining the risk factors and effects of pregnancy loss on women and families.
Christopher Craver is an independent health services researcher affiliated with the Charlotte Lozier Institute focused on the use of secondary healthcare data sources in population based scientific research. He is widely published in many healthcare topics including cancer treatment, rare disease populations, and the efficacy of surgical services.
Tessa Longbons is a research associate with the Charlotte Lozier Institute. Her research focuses on abortion statistics at the state and national levels and the changing landscape of abortion policy, provision, and access in the United States.
Donna J. Harrison, M.D. dip ABOG received her M.D. from the University of Michigan and completed ObGyn residency at a University of Michigan Affiliate hospital (St. Joseph Mercy Hospital). She is currently Executive Director of the American Association of Pro-Life Obstetricians and Gynecologists.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Charlotte Lozier Institute.
ORCID iD: James Studnicki  https://orcid.org/0000-0003-2958-7493
https://orcid.org/0000-0003-2958-7493
Tessa Longbons  https://orcid.org/0000-0003-0479-9166
https://orcid.org/0000-0003-0479-9166
References
- 1. Chan A, McCaul KA, Keane RJ, Haan EA. Effect of parity, gravidity, previous miscarriage, and age on risk of Down’s syndrome: population based study. BMJ. 1998;317(7163):923–924. doi:10.1136/bmj.317.7163.923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhou W, Nielsen GL, Larsen H, Olsen J. Induced abortion and placenta complications in the subsequent pregnancy. Acta Obstet Gynecol Scand. 2001;80(12):1115–1120. doi:10.1034/j.1600-0412.2001.801207.x [DOI] [PubMed] [Google Scholar]
- 3. Akter S, Jesmin S, Rahman MM, et al. Higher gravidity and parity are associated with increased prevalence of metabolic syndrome among rural Bangladeshi women. PLoS One. 2013;8(8):e68319 doi:10.1371/journal.pone.0068319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Heidam LZ. Spontaneous abortions among factory workers: the importance of gravidity control. Scand J Soc Med. 1983;11(3):81–85. [PubMed] [Google Scholar]
- 5. Ajinkya S, Jadhav PR, Srivastava NN. Depression during pregnancy: prevalence and obstetric risk factors among pregnant women attending a tertiary care hospital in Navi Mumbai. Ind Psychiatry J. 2013;22(1):37–40. doi:10.4103/0972-6748.123615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reardon DC, Cougle JR, Rue VM, Shuping MW, Coleman PK, Ney PG. Psychiatric admissions of low-income women following abortion and childbirth. CMAJ. 2003;168(10):1253–1256. [PMC free article] [PubMed] [Google Scholar]
- 7. Coleman PK, Reardon DC, Calhoun BC. Reproductive history patterns and long-term mortality rates: a Danish, population-based record linkage study. Eur J Public Health. 2013;23(4):569–574. doi:10.1093/eurpub/cks107 [DOI] [PubMed] [Google Scholar]
- 8. Guttmacher Institute. Evidence you can use: Medicaid funding of abortion. 2020. Accessed May 6, 2020 https://www.guttmacher.org/evidence-you-can-use/medicaid-funding-abortion
- 9. Centers for Disease Control and Prevention. Pregnancy mortality surveillance system. Last reviewed February 4, 2020. Accessed May 6, 2020 https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm.
- 10. Koch E, Thorp J, Bravo M, et al. Women’s education level, maternal health facilities, abortion legislation and maternal deaths: a natural experiment in Chile from 1957 to 2007. PLoS One. 2012;7(5):e36613 doi:10.1371/journal.pone.0036613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koch E, Bravo M, Gatica S, et al. Overestimation of induced abortion in Colombia and other Latin American countries. Ginecol Obstet Mex. 2012;80(5):360–372. [PubMed] [Google Scholar]
- 12. Koch E, Chireau M, Pliego F, et al. Abortion legislation, maternal healthcare, fertility, female literacy, sanitation, violence against women and maternal deaths: a natural experiment in 32 Mexican states. BMJ Open. 2015;5:e006013 doi:10.1136/bmjopen-2014-006013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Reardon DC. The abortion and mental health controversy: a comprehensive literature review of common ground agreements, disagreements, actionable recommendations, and research opportunities. SAGE Open Med. 2018:6 doi:10.1177/2050312118807624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Reardon DC, Thorp JM. Pregnancy associated death in record linkage studies relative to delivery, termination of pregnancy, and natural losses: a systematic review with a narrative synthesis and meta-analysis. SAGE Open Med. 2017;5:2050312117740490 doi:10.1177/2050312117740490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM. Reasons U.S. women have abortions: quantitative and qualitative perspectives. Perspect Sex Reprod Health. 2005;37(3):110–118. doi:10.1363/psrh.37.110.05. [DOI] [PubMed] [Google Scholar]
- 16. Burke T, Reardon DC. Forbidden Grief: The Unspoken Pain of Abortion. Acorn Books; 2007. [Google Scholar]
- 17. Raine T, Harper C, Leon K, Darney P. Emergency contraception: advance provision in a young, high-risk clinic population. Obstet Gynecol. 2000;96(1):1–7. doi:10.1016/s0029-7844(00)00830-9 [DOI] [PubMed] [Google Scholar]
- 18. Hicks J. The Potential of Claims Data to Support the Measurement of Health Care Quality [dissertation]. RAND; 2003. [Google Scholar]
- 19. Romano PS. Using administrative data to identify associations between implanted medical devices and chronic diseases. Ann Epidemiol. 2000;10(4):197–199. doi:10.1016/s1047-2797(00)00041-7 [DOI] [PubMed] [Google Scholar]