Abstract
Background:
Telemedicine is defined as “the use of medical information exchanged from one site to another via electronic communications to improve a patient’s health status”. This relatively new concept of healthcare is based on the fusion between medical assistance and Information and Communication Technology (ICT) to provide support to people located in remote and underserved areas. It can be found not only in hospitals, but also in other healthcare facilities such as pharmacies. Starting from 2010, telemedicine or telehealth was formally introduced in the Italian pharmaceutical context with the “Pharmacy of Services Decree”. In spite of this regulatory framework, the implementation of this technology was very slow and there are no data about the spreading and use of these services in Italian pharmacies.
Objective:
The present study has therefore developed a survey to collect information on the diffusion of telemedicine/telehealth services within Italian pharmacies.
Methods:
A two-part questionnaire in Italian was developed using SurveyMonkey, setting a mechanism aimed to have different outcomes according to the answers given. Six hundred eighty-three respondents returned the questionnaire. The results were then analysed statistically.
Results:
The questionnaire results have shown a limited diffusion of telemedicine/telehealth services among Italian pharmacies and an apparently limited interest of health authorities in supporting the integration of this technology.
Conclusions:
More efforts should be spent by national public health stakeholders to better analyse the contribution of telemedicine services available in public pharmacies and to find the best solutions to implement this innovative technology as an established service.
Keywords: Telemedicine, Delivery of Health Care, Medically Underserved Area, Public Health, Primary Health Care, Pharmacies, Pharmaceutical Services, Pharmacists, Surveys and Questionnaires, Italy
INTRODUCTION
Telemedicine, according to the American Telemedicine Association, is “the use of medical information exchanged from one site to another via electronic communications to improve a patient’s health status”.1 Telemedicine is found in hospitals, clinics, and pharmacies and also in non-health environments, where it allows various types of diagnostic and therapeutic applications.2-4 In fact, it has also been described as the use of the most modern and up-to-date medical and information technology (IT), in order to provide “remote” healthcare.1,5
In 2016, the US Agency for Healthcare Research & Quality (AHRQ), part of the Department of Health and Human Services, published a report on telemedicine interventions and their impact on patient outcomes. In particular, their data showed positive results in remote monitoring of patients suffering from chronic diseases.6 A 2017 study on the use of telemedicine to enhance pharmacy services in the nursing facility reported that patients appreciate the benefits of telemedicine, and noted that important economic savings had been achieved.7 This study estimated that a hospital that uses telemedicine technologies can save around USD 261,109 a year compared to a hospital that does not use teleservice technologies.7 Furthermore, health professionals, doctors, pharmacists and nurses clearly expressed their comfort in using these technologies and their satisfaction with them.7
While telemedicine/telehealth applications can vary, it has proven particularly useful in pharmacies as part of the their healthcare offer.6-11 For example, pharmacists who offer blood pressure, blood oxygenation or spirometry measurements, blood clotting or blood glucose tests, dermatological tests or electrocardiograms can quickly monitor the patient’s health status and report the results directly to patient’s physician. Pharmacists can query patients about their compliance with treatment 24 hours a day, report irregularities or adverse drug reactions (ADEs), and collaborate with the general practitioner when problems arise.12,13
Pharmaceutical service in Italy is regulated by various sets of legislation that, over time, have ended up overlapping each other.14 Pharmaceutical service to the population is provided mainly through local pharmacies, classified as urban if located in cities with more than 5,000 inhabitants, and rural if located in towns with fewer than 5,000 inhabitants. The density of pharmacies is one pharmacy per an average of 3,000 inhabitants, a value in line with the European standards. Pharmacies in Italy can be owned by private pharmacists or can be government-owned, in which case they are called “municipal pharmacies”. In Italy, as of March 2019 there were 19,331 pharmacies, 17,656 of which were privately owned and 1,675 of which were government-owned municipal pharmacies.15
In the last 10 years, Italian pharmacies have evolved significantly. Previously they were limited to sales of medicines and health products and to advising customers about medicines or healthcare. Then, with the ministerial decree of 16 December 2010, commonly called the “Pharmacy of Services Decree”, pharmacies were given permission to provide services such as “self-diagnostic” tests, that is, those that patients could also perform at home independently, if equipped with suitable equipment and self-sufficiency, or tests that require the participation and help of a healthcare professional, such as electrocardiograms and spirometry measurements.16 Using appropriate telemedicine devices such as smart phones, tablets or computers through certified connections, it is possible to share the patient’s health information with a doctor, who in turn can return to the patient prescriptions and instructions.17 Moreover, patients can now book specialist examinations directly in the pharmacy, as well as collect medical reports.
European Union institutions have implemented measures to regulate aspects and applications of telemedicine, but laws still differ among the various member states, which have sometimes maintained their own regulations.18 According to the Italian Ministry of Health guidelines and regulations for telemedicine in Italy, telemonitoring is defined as the performance of clinical examinations and sharing of the results with an off-site physician, so the latter can send prescriptions and instructions for the patient.19
Although telemedicine and telepharmacy are gaining in popularity among professionals and patients, the literature provides little information on how telemedicine is actually implemented in pharmacies, or systematic analysis of the actual impact on patient health.7
To the best of our knowledge, no governmental or private entity has studied the effects of the 2010 Pharmacy of Services Decree in the area of telemedicine, and there is no information about the impact of this decree in the Italian pharmaceutical context, or the extent to which telemedicine approaches have been adopted.20
The present study has therefore investigated how telemedicine/telehealth service are used in Italian pharmacies, by administering a questionnaire to members of the National Federation of Associations of Italian Young Pharmacists (FENAGIFAR). This federation is made up of pharmacists aged under 38.
The results obtained may provide interesting insights into how the telemedicine is being used in Italian pharmacies.
METHODS
The questionnaire
The two-part questionnaire in Italian was designed using SurveyMonkey.21 The 3 questions in Part 1 asked about the type of pharmacy where the respondent works, its location, and whether or not the pharmacy provides telemedicine service. Respondents who indicated that their pharmacy offers this service were asked to continue to Part II and answer 25 questions about their experience.
The type of questions included were as follow: 27 close-ended questions (that about the type of services provided envisaged more than one answer possible, while the remaining 26 envisaged only one answer); 1 open-ended question about the geographic location of the pharmacy. The English version of the questionnaire is included in the Appendix at the bottom of the article. The mechanism of the survey is depicted in the flowchart in Figure 1.
Figure 1. The questionnaire mechanism shows the different outcomes possible, according to the third answer in section 1, the checkpoint of the survey.
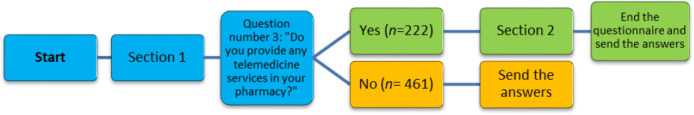
An affirmative answer to this question allows the respondent to continue to the second section. Otherwise, the respondent stops working on the questionnaire and send the answers given up to that point. The questionnaire was submitted to 3,400 pharmacists with a response rate of 20%.
The questionnaire was developed and the investigation carried out by researchers of the “Telemedicine and Telepharmacy Center” of the University of Camerino. A local community pharmacist whose pharmacy is equipped with telemedicine devices was asked to critique the questionnaire in terms of construction, wording, and content, and once those suggestions were incorporated, the text was sent to the FENAGIFAR president for further assessment. The most glaring problem was the length of the survey. The researchers cooperated to find a suitable solution, and in the end, decided to merge sixteen of the remaining queries into 2 questions about the average number and mean age of patients who took advantage of each telemedicine service cited. Then, each researcher assessed the items using the CVI scale to analyse the appropriateness of the instrument. Once the questionnaire was approved unanimously by the research team and the FENAGIFAR president, it was transcribed into the SurveyMonkey tool.22 After that, the researchers tested the survey to ascertain that the mechanism worked properly, but did not allow the answers to be registered in the system.
The criteria for eligibility to participate in the survey were a degree in pharmacy, board certification, and work in one of the three types of pharmacies (privately owned urban pharmacy, privately owned rural pharmacy, or government-owned municipal pharmacy). The researchers invited 10 eligible pharmacists to complete and critique the questionnaire. Their answers to the questions were not recorded in the system at this point. They reported no problems, and so the questionnaire was emailed to all FENAGIFAR members with a cover letter from the two survey creators explaining the purpose of the study and specifying that data collected would be treated confidentially. No informed consent was requested, as the decision to click on the link to participate in the survey was considered permission. In any case, no personal data were collected and anonymity was maintained, in respect of the European privacy law (GDPR EU 2016/679).23 No reminders were sent. Data collection was carried out between May and June 2019.
Statistics
Once the questionnaires were completed, the researchers used a SurveyMonkey Excel worksheet as the basis for calculating the frequencies of the answers and producing bar graphs. Frequencies were calculated based on the whole sample of 683 respondents for the first three questions. Question three, which asked whether their pharmacy provided telemedicine services, was the cut-off point. From the fourth question onward, frequencies were calculated for 222 respondents, that is, the number of pharmacists whose workplaces offered telemedicine services.
Data stratification
Further data analysis consisted of data stratification using two variables, namely, the type of pharmacy and its geographic location, to investigate whether these parameters affected the use of telemedicine services.
The types of pharmacy considered were government-owned municipal pharmacies, privately-owned urban pharmacies, and privately-owned rural ones. Geographical partition adopted sectors identified by the Italian National Institute of Statistics, namely North-West (NW), North-East (NE), Centre, South, and main Islands (Sicily and Sardinia).24 The frequencies for each question were calculated according to these variables. Again, from the fourth question onwards, percentages for each subgroup were calculated in terms of the number of respondents whose workplaces use telemedicine.
Next, these data were transferred into the Origin 9.1 (Origin Lab) software to perform the chi-square test to find any differences, using the total sample data as reference.
RESULTS
In this section, the most outstanding data are presented to give an insight of the phenomenon studied. Information is organized into three subsections, namely general analysis and the two stratifications. This to give first a comprehensive overview of the entity of the diffusion of the telemedicine/telehealth in the Italian pharmaceutical context and implications that lay behind it. Then, our second purpose is to shed the light on possible variables that could affect its distribution within the Italian soil. The results of analysis of the questionnaire input are organized into two sections. The first section provides an overview of the extent to which telemedicine in used in Italian pharmacies, while the second section reports information analysed in terms of the type of pharmacy and its geographic location.
General analysis
The survey had a response rate of 20%: it was sent to 3,400 pharmacists, of whom 683 chose to participate.
It was not possible to ascertain the number of those who did not respond to the questionnaire for the reason that they do not work in pharmacies and thus were ineligible.
Telemedicine in Italy. According to the data collected, telemedicine is not a well-established practice in Italian pharmacies. In fact, only one third of our interviewees (32.5%) offer telemedicine services, and of these, 82.4% have done so for over a year. As noted above, this question was the checkpoint of the questionnaire.
Among all the available services, ECG, BP and BG were the most commonly offered examinations (respectively 86.9%, 67.1%, 56.8%)
Compliance with regulations. In general, good practice regulations were respected, as over 90% of the respondents indicated that they perform the examinations in a separate room, and most require patients to provide informed consent. The patient’s right to information, in the context of health treatment, is of crucial importance, the violation of which by healthcare personnel constitutes a hypothesis of medical liability (so-called medical malpractice). The acquisition of consent is in fact different from the health service, and its purpose is to protect the fundamental right to health.
Failure to comply with the obligation to acquire informed consent violates the patient’s right to self-determination regarding his / her psycho-physical state, protected by law.
The patient who has not been adequately informed by the doctor before being subjected to a therapy or a diagnostic examination, may institute a judgment against the health care professional to ascertain the latter’s responsibility and therefore to obtain compensation for the damage suffered.
Trend of use. Respondents were asked to indicate the average number of clients per month who use the services, their mean age, and whether these clients used the services more than once. Unfortunately, respondents usually indicated “I don’t know” for the first two questions. The most detailed data were provided for ECG and BP. For ECG, “fewer than 20 patients a month” was answer the most commonly indicated, whilst for BP, a slightly higher tendency for the answer “between 20 and 60 patients per month” was registered. Some interesting trends were observed for BP and BG (Table 1).
Table 1. Patients using telemedicine services per month.
| < 20 patients | 20 - 60 patients | > 60 patients | I don’t know | |
|---|---|---|---|---|
| Electrocardiogram | 169 (76.1) | 25 (11.3) | 1 (0.5) | 27 (12.2) |
| Blood oxygenation | 44 (19.8) | 8 (3.6) | 0 (0.0) | 170 (76.6) |
| Spirometry | 30 (13.5) | 2 (0.9) | 0 (0.0) | 190 (85.6) |
| Blood clotting | 41 (18.5) | 7 (3.2) | 4 (1.8) | 170 (76.6) |
| Dermatological test | 33 (14.9) | 6 (2.7) | 2 (0.9) | 181 (81.5) |
| Blood pressure | 62 (27.9) | 67 (0.2) | 48 (21.6) | 45 (20.3) |
| Blood glucose | 70 (31.5) | 67 (7.9) | 17 (7.7) | 73 (32.9) |
| Other | 104 (46.8) | 27 (12.2) | 4 (1.8) | 87 (39.2) |
Data are expressed as the absolute frequencies (percentage).
Respondents were asked to indicate for each service the mean age of clients who use it, choosing from a list of 5 age groups (AG): under 30 years (AG1), 30-40 (AG2), 41-50 (AG3), 51-60 (AG4), over 60 years (AG5). The most significant results concerned the ages of clients who use ECG, BP, and BG services (Table 2).
Table 2. Patients using telemedicine services per month and use of telemedicine services according to the different age groups.
| <30 years | 30-40 years | 41-50 years | 51-60 years | 60 years | I don’t know | |
|---|---|---|---|---|---|---|
| Electrocardiogram | 32 (14.4) | 42 (18.9) | 48 (21.6) | 43 (19.4) | 14 (6.3) | 43 (19.4) |
| Blood oxygenation | 3 (1.4) | 4 (1.8) | 8 (3.6) | 13 (5.9) | 13 (5.9) | 181 (81.5) |
| Spirometry | 4 (1.8) | 3 (1.4) | 8 (3.6) | 6 (2.7) | 2 (0.9) | 199 (89.6) |
| Blood clotting | 3 (1.4) | 4 (1.8) | 4 (1.8) | 17 (7.7) | 19 (8.6) | 175 (78.8) |
| Dermatological test | 5 (2.3) | 11 (5.0) | 16 (7.2) | 5 (2.3) | 2 (0.9) | 183 (82.4) |
| Blood pressure | 1 (0.5) | 3 (1.4) | 32 (14.4) | 77 (34.7) | 48 (21.6) | 61 (27.5) |
| Blood glucose | 1 (0.5) | 2 (0.9) | 42 (18.9) | 63 (28.4) | 33 (14.9) | 81 (36.5) |
| Other | 1 (0.5) | 13 (5.9) | 34 (15.3) | 38 (17.1) | 14 (6.3) | 122 (55.0) |
Data are expressed as the absolute frequencies (percentage).
An approximatively homogeneous distribution, from AG1 to AG4, was seen for ECGs, while the rate of use dramatically dropped off for the most elderly patients (AG5). BP and BG were more attractive for the last three groups, with a peak in AG4 (34.7% for BP; 28.4% for BG). Overall, the youngest patients were more interested in ECGs, the oldest ones in BP measurements. Respondents indicated that 59% of their clients use a service more than once.
Physician involvement. These examinations are meant to monitor health parameters, and sometimes can reveal the need for follow-up care, or even a medical emergency. The availability of such services in the pharmacy saves the long waiting list for such services from the public healthcare system, usually conducted in a hospital. Thus we investigated the degree to which medical professionals are involved in follow-up care, asking how many patients (I) turn to a specialist, (II) get a new prescription from their general practitioner (GP), or (III) from a specialist, (IV) have their therapy modified by the GP, or (V) by a specialist. The possible options were “fewer than 10%”, “10-20%”, “21-40%”, “over 40%”, and “I don’t know” (Table 3). Quite a high percentage answered “I don’t know,” but even so, the results offered some interesting information.
Table 3. Physician’s involvement after performing a test in the pharmacy.
| To how many patients, following a Telemonitoring, … | < 10% | 10%-20% | 20%-40% | > 40% | I don’t know |
|---|---|---|---|---|---|
| call on to the medical specialist? | 35 (15.8) | 37 (16.7) | 37 (16.7) | 58 (26.1) | 55 (24.8) |
| a drug therapy is prescribed by the general practitioner? | 37 (16.7) | 40 (18.0) | 37 (16.7) | 20 (9.0) | 88 (39.6) |
| a drug therapy is prescribed by the medical specialist? | 32 (14.4) | 32 (14.4) | 35 (15.8) | 24 (10.8) | 99 (44.6) |
| a previous drug therapy is modified by the general practitioner? | 39 (17.6) | 41 (18.5) | 24 (10.8) | 9 (4.1) | 109 (49.1) |
| a previous drug therapy is modified by the medical specialist? | 42 (18.9) | 36 (16.2) | 20 (9.0) | 10 (4.5) | 114 (51.4) |
Data are expressed as the absolute frequencies (percentage).
Relationship between the pharmacy and local health authorities. Fully 97% of the respondents indicated the lack of an agreement with local governmental health authorities to oversee the fruition of services. Similarly, 70.3% responded that authorities do not assess the quality of service or determine whether regulations are being respected. Moreover, the majority of those who answered that there is a periodic inspection stated that they are carried out less than once a year (62.1%). Pharmacies are periodically inspected by competent authorities and police forces (such as the “Nuclei Anti Sofisticazioni”, acronym NAS). The purpose of this question is to investigate whether the presence of telemedicine entailed greater involvement of local health authorities. These inspections are intended to verify that the telehealth procedures carried out inside the pharmacies comply with current legislation in terms of health, hygiene and privacy.
Device and computer network quality check. Most of the respondents indicated that quality checks are carried out for devices (82.9%) and computer networks (69.4%), but considering the previous results, one may surmise that they are carried out by the companies that sell the equipment.
Patient’s medical report. A considerable percentage of respondents (62.2%) indicated that their pharmacy has an agreement with one or more specialists to analyse the results of the health parameter measurements conducted in their pharmacy. These specialists usually work for a private healthcare company (66.7%) rather than the governmental healthcare service (33.3%).
The efficiency of telemedicine/telehealth services was attested to by the fact that the waiting time to receive the medical report from the specialists is less than 24 hours in slightly more than half of the cases (50.9% of respondents). In addition, 77.9% of respondents said the medical report could be sent directly to the patient.
However, it is crucial that pharmacies establish agreements with companies recognized by the national health system, and operating through certified health care professionals. On the contrary, it may represent an illegal activity that can endanger the patient’s health and privacy.
Pharmacist’s training and provision of services. Generally, pharmacists received training in how to use the equipment (for example, blood pressure cuffs, blood glucose kits, or ECG sets) from the seller (82.4%). Some respondents indicated they “obtained training independently” (14.4%), “from local health authorities” (2.3%), or “from a university or a hospital” (0.9%).
In terms of provision of services, we asked how many pharmacists are responsible for carrying out the clinical tests, and what hours of the workday the services are provided. The percentage obtained for the different options are as follow: In 31.1% of the cases, “only one pharmacist” handled the tests, while 46.8% answered “more than one”, and 22.1% answered “all the pharmacists”. Moreover, the vast majority of respondents (87.8%) indicated that services were provided throughout the opening hours of the pharmacy.
Stratification
We looked at the data provided by the questionnaires from the points of view of the type of pharmacy and its geographic location, to assess whether implementation of telemedicine is positively or negatively conditioned by these two variables. This in the hope of identifying issues that Italian health authorities should address in their efforts to foster more widespread use of telemedicine in Italy. The most interesting differences are presented below.
Type of pharmacy
Most respondents (69.5%) work in an urban private pharmacy, 24.6% in a rural private pharmacy and just 5.9% in a municipal one (Table 4). In general, 30% of all the pharmacy types use telemedicine solutions, though urban privately-owned ones have the highest percentage of implementation 33.3% and municipal ones the lowest 27.5%; telemedicine is implemented in the 31.5% of the rural private pharmacies.
Table 4. Pharmacy type and geographic location stratification.
| Categories | n (%) |
|---|---|
| Stratification by type of pharmacy | |
| Municipal pharmacies | 40 (5.9) |
| Urban private pharmacies | 475 (69.5) |
| Rural private pharmacies | 168 (24.6) |
| Stratification by geographic location (according to ISTAT regional classification) | |
| North-West (NW) | 224 (33.3) |
| North-East (NE) | 141 (21.0) |
| Centre | 111 (16.5) |
| South | 121 (18.0) |
| Islands | 75 (11.2) |
No remarkable deviations from the total sample were observed for the average number of patients per month, while the mean age question provided some differences from the general trend. Municipal pharmacies showed the highest number of variations. As a matter of fact, ECGs were more likely to be requested by patients 30-40 years old, while no patients under 30 requested this service. BO and DM were requested only by patients 41-50 years old, while SP and BC only by those 51-60 years old (Table 5). However, given that a very high percentage of respondents indicated “I don’t know” for these questions, these results may not be fully representative of the reality.
Table 5. Use of pharmacy telehealth services in the different type of pharmacies according to patient age groups.
| Total | Municipal | Rural | Urban | Total | Municipal | Rural | Urban | ||
|---|---|---|---|---|---|---|---|---|---|
| Electrocardiogram | Blood oxygenation | ||||||||
| < 30 years | 32 (14.4) | 0 (0.0) | 8 (15.1) | 24 (15.2) | < 30 years | 3 (1.4) | 0 (0.0) | 1 (1.9) | 2 (1.3) |
| 30-40 years | 42 (18.9) | 5 (45.5) | 9 (17.0) | 28 (17.7) | 30-40 years | 4 (1.8) | 0 (0.0) | 1 (1.9) | 3 (1.9) |
| 41-50 years | 48 (21.6) | 2 (18.2) | 11 (20.8) | 35 (22.2) | 41-50 years | 8 (3.6) | 1 (9.1) | 1 (1.9) | 6 (3.8) |
| 51-60 years | 43 (19.4) | 1 (9.1) | 12 (22.6) | 30 (19.0) | 51-60 years | 13 (5.9) | 0 (0.0) | 3 (5.7) | 10 (6.3) |
| >60 years | 14 (6.3) | 1 (9.1) | 2 (3.8) | 11 (7.0) | >60 years | 13 (5.9) | 0 (0.0) | 5 (9.4) | 8 (5.1) |
| I don’t know | 43 (19.4) | 2 (18.2) | 11 (20.8) | 30 (19.0) | I don’t know | 181 (81.5) | 10 (90.9) | 42 (79.2) | 129 (81.6) |
| Spirometry | Blood clotting | ||||||||
| < 30 years | 4 (1.8) | 0 (0.0) | 1 (1.9) | 3 (1.9) | < 30 years | 3 (1.4) | 0 (0.0) | 1 (1.9) | 2 (1.3) |
| 30-40 years | 3 (1.4) | 0 (0.0) | 1 (1.9) | 2 (1.3) | 30-40 years | 4 (1.8) | 0 (0.0) | 1 (1.9) | 3 (1.9) |
| 41-50 years | 8 (3.6) | 0 (0.0) | 3 (5.7) | 5 (3.2) | 41-50 years | 4 (1.8) | 0 (0.0) | 0 (0.0) | 4 (2.5) |
| 51-60 years | 6 (2.7) | 1 (9.1) | 1 (1.9) | 4 (2.5) | 51-60 years | 17 (7.7) | 1 (9.1) | 5 (9.4) | 11 (7.0) |
| >60 years | 2 (0.9) | 0 (0.0) | 1 (1.9) | 1 (0.6) | >60 years | 19 (8.6) | 0 (0.0) | 3 (5.7) | 16 (10.1) |
| I don’t know | 199 (89.6) | 10 (90.9) | 46 (86.8) | 143 (90.5) | I don’t know | 175 (78.8) | 10 (90.9) | 43 (81.1) | 122 (77.2) |
| Dermatological test | Blood pressure | ||||||||
| < 30 years | 5 (2.3) | 0 (0.0) | 1 (1.9) | 4 (2.5) | < 30 years | 1 (0.5) | 0 (0.0) | 0 (0.0) | 1 (0.6) |
| 30-40 years | 11 (5.0) | 0 (0.0) | 5 (9.4) | 6 (3.8) | 30-40 years | 3 (1.4) | 0 (0.0) | 1 (1.9) | 2 (1.3) |
| 41-50 years | 16 (7.2) | 1 (9.1) | 5 (9.4) | 10 (6.3) | 41-50 years | 32 (14.4) | 3 (27.3) | 8 (15.1) | 21 (13.3) |
| 51-60 years | 5 (2.3) | 0 (0.0) | 0 (0.0) | 5 (3.2) | 51-60 years | 77 (34.7) | 6 (54.5) | 17 (32.1) | 54 (34.2) |
| >60 years | 2 (0.9) | 0 (0.0) | 0 (0.0) | 2 (1.3) | >60 years | 48 (21.6) | 0 (0.0) | 15 (28.3) | 33 (20.9) |
| I don’t know | 183 (82.4) | 10 (90.9) | 42 (79.2) | 131 (82.9) | I don’t know | 61 (27.5) | 2 (18.2) | 12 (22.6) | 47 (29.7) |
| Blood glucose | Other | ||||||||
| < 30 years | 1 (0.5) | 0 (0.0) | 0 (0.0) | 1 (0.6) | < 30 years | 1 (0.5) | 0 (0.0) | 0 (0.0) | 1 (0.6) |
| 30-40 years | 2 (0.9) | 0 (0.0) | 1 (1.9) | 1 (0.6) | 30-40 years | 13 (5.9) | 1 (9.1) | 2 (3.8) | 10 (6.3) |
| 41-50 years | 42 (18.9) | 4 (36.4) | 14 (26.4) | 24 (15.2) | 41-50 years | 34 (15.3) | 1 (9.1) | 11 (20.8) | 22 (13.9) |
| 51-60 years | 63 (28.4) | 2 (18.2) | 14 (26.4) | 47 (29.2) | 51-60 years | 38 (17.1) | 0 (0.0) | 9 (17.0) | 29 (18.4) |
| >60 years | 33 (14.9) | 1 (9.1) | 9 (17.0) | 23 (14.6) | >60 years | 14 (6.3) | 1 (9.1) | 5 (9.4) | 8 (5.1) |
| I don’t know | 81 (36.5) | 4 (36.4) | 15 (28.3) | 62 (39.2) | I don’t know | 122 (55.0) | 8 (72.7) | 26 (49.1) | 88 (55.7) |
Data are expressed as the absolute frequencies (percentage).
Follow up to pharmacy telemedicine/telehealth services
(I) Turning to a specialist. Clients of urban private pharmacies were more likely to see a specialist after a telemedicine service. In fact, 25.3% of respondents working in urban private pharmacies indicated that “more than 40%” of clients followed up the in-pharmacy tests by getting an appointment with a specialist. (II) New prescription from a GP. Clients of rural pharmacies were more likely to follow-up their tests or measurements done in the pharmacy by obtaining a new prescription from a GP. (III) New prescription from specialist. For all three types of pharmacies, for under 50% of clients, in-pharmacy results were followed up with a change in prescription from a specialist. (IV) Modification of treatment by a GP. Similarly, for under 50% of clients of all three types of pharmacies, in-pharmacy services were followed up with modification of treatment ordered by a GP. (V) Modification of treatment by a specialist. In contrast, “more than 40%” of clients of urban pharmacies usually got a treatment modification from a specialist.
Relationship between the pharmacy and local health authorities. The quality inspections for the telemedicine services are carried out by the local health authorities in the 54.5% of the municipal pharmacies, in the 25.9% of the urban private pharmacies and in the 35.8% of the rural private pharmacies; these quality checks are significantly higher (p<0.05) in the municipal pharmacies, as stands to reason, given that they are pharmacies belonging to public institutions.
In fact, even though 62.1% of respondents working in municipal pharmacies indicated that officials inspected their pharmacy “less than once a year,” the answer “every two or three months” was definitely higher among respondents working in municipal pharmacies than among those working in private ones (16.7% municipal pharmacies vs. 5.3% rural and 4.9% urban).
Specialists. Agreements with one or more specialists to analyse the results of the health parameter measurements conducted in the pharmacy and to provide a medical report were most common in municipal pharmacies (81.8%), followed by private rural pharmacies (71.7%) and private urban ones (57.6%).
Device and computer network quality check. All the municipal pharmacists reported that devices were periodically checked, while a small percentage of private rural (11.3%) and private urban (20.3%) ones indicated that no checks were carried out. Hence, considering the scarce commitment of local health authorities, it could be possible that this quality check is carried out by the device supplier.
Provision of services. Some fluctuations were also observed in how service was organized. While respondents working in municipal pharmacies and private urban pharmacies presented a peak in the option “more than one pharmacist is in charge of carrying out the clinical examinations”, private rural ones had a homogenous distribution among the answer options of “only one pharmacist” “more than one” and “all the pharmacists”. Respondents among all three types of pharmacies indicated that they provide telemedicine services throughout the workday, though limitation to only some time slots was definitely more likely in municipal pharmacies (36.4%) than the other two (urban 9.4%; rural 11.4%).
Geographical location. For this kind of stratification, the sample was reduced to 672 respondents, as 11 were excluded due to incorrect information about geographical location. It should be considered that the percentages were calculated over the number of pharmacies in each area, so as to take into account the relative proportion in each group. Moreover, the importance of data has to be evaluated by comparing them with the overall values, namely those shown in general analysis section.
The geographical distribution of the pharmacies of the respondents is summarized in Table 4. No municipal pharmacies are present in the Islands, while the highest concentration of rural ones is in the NE. The NW had the highest number of pharmacies adopting telemedicine solutions (37.5%) (84/224), followed closely by 37.2% for the South (45/121), 34.2% for the Centre (38/111), 27.7% for the NE (39/141), and 17.3% for the Islands (13/75) (Table 6).
Table 6. Data about the implementation of telemedicine and relationship with local health authorities distinguished from a geographical point of view.
| North-West | North-East | Centre | South | Islands | |
|---|---|---|---|---|---|
| Degree of telemedicine adoption | 84 (37.5) | 39 (27.7) | 38 (34.2) | 45 (37.2) | 13 (17.3) * |
| How long has your pharmacy been using telemedicine solutions? (less than 1 year) | 8 (9.5) | 1 (2.6) | 4 (10.5) | 5 (11.1) | 3 (23.1) * |
| Agreement with local health authorities (yes) | 4 (4.8) | 0 (0.0) * | 2 (5.3) | 4 (8.9) | 3 (23.1) * |
| Quality check carried out by local health authorities (yes) | 26 (30.9) | 9 (23.1) | 10 (26.3) | 15 (33.3) | 5 (38.5) |
Data are expressed as the absolute frequencies (percentage). The values marked by an asterisk (*) are statistically significant data.
An interesting trend is that the Islands had the lowest number of pharmacies offering telemedicine services, but the highest proportion of pharmacies that have recently adopted these services. The highest value for all the geographic areas was registered for the answer “more than 1 year”. Pharmacies in Southern Italy had the highest percentage of clients who use telemedicine services more than once (80% of Southern Italian pharmacies vs a general trend of 59%). On the contrary, the NW showed an inverse trend, as the percentage of clients who are repeat users of telemedicine (43.6%) is lower than those who used it only once (56.4%).
Results on the age distribution of patients highlighted some differences. Patients under 30 demonstrated higher interest in ECG in the NE (28.2%) compared with the results of the whole sample. In the Islands, results for ECG varied from the general trend, as it appeared to be more attractive for older patients (38.5% for those 51-60 years old). Patients 30-40 years old in the Islands (7.7%) had more BP examinations than the overall value (1.4%), while those 51-60 years old had the lowest percentage (15.4% vs the general value of 34.7%) (Table 7). Surprisingly, while telemedicine technology is less present in Island pharmacies, as noted previously, this area had the highest number of pharmacies that have established an agreement with local health authorities and receive periodic inspections.
Table 7. Use of pharmacy telehealth services in the different geographic areas according to patient age groups.
| Total | North-west | North-east | Centre | South | Islands | |
|---|---|---|---|---|---|---|
| Electrocardiogram | ||||||
| < 30 years | 32 (14.4) | 10 (11.9) | 11 (28.2) | 2 (5.3) | 9 (20.0) | 0 (0.0) |
| 30-40 years | 42 (18.9) | 17 (20.2) | 8 (20.5) | 4 (10.5) | 11 (24.4) | 1 (7.7) |
| 41-50 years | 48 (21.6) | 19 (22.6) | 9 (23.1) | 5 (13.2) | 12 (26.7) | 3 (23.1) |
| 51-60 years | 43 (19.4) | 18 (21.4) | 4 (10.3) | 10 (26.3) | 6 (13.3) | 5 (38.5) |
| >60 years | 14 (6.3) | 9 (10.7) | 0 (0.0) | 4 (10.5) | 1 (2.2) | 0 (0.0) |
| Age not Known | 43 (19.4) | 11 (13.1) | 7 (17.9) | 13 (34.2) | 6 (13.3) | 4 (30.8) |
| Blood oxygenation | ||||||
| < 30 years | 3 (1.4) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 2 (4.4) | 0 (0.0) |
| 30-40 years | 4 (1.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (4.4) | 1 (7.7) |
| 41-50 years | 8 (3.6) | 1 (1.2) | 1 (2.6) | 0 (0.0) | 4 (8.9) | 2 (15.4) |
| 51-60 years | 13 (5.9) | 8 (9.5) | 0 (0.0) | 3 (7.9) | 2 (4.4) | 0 (0.0) |
| >60 years | 13 (5.9) | 8 (9.5) | 0 (0.0) | 4 (10.5) | 1 (2.2) | 0 (0.0) |
| Age not Known | 181 (81.5) | 66 (78.6) | 38 (97.4) | 31 (81.6) | 34 (75.6) | 10 (76.9) |
| Spirometry | ||||||
| < 30 years | 4 (1.8) | 1 (1.2) | 0 (0.0) | 1 (2.6) | 2 (4.4) | 0 (0.0) |
| 30-40 years | 3 (1.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (4.4) | 0 (0.0) |
| 41-50 years | 8 (3.6) | 2 (2.4) | 1 (2.6) | 0 (0.0) | 3 (6.7) | 2 (15.4) |
| 51-60 years | 6 (2.7) | 3 (3.6) | 1 (2.6) | 1 (2.6) | 1 (2.2) | 0 (0.0) |
| >60 years | 2 (0.9) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 1 (2.2) | 0 (0.0) |
| Age not Known | 199 (89.6) | 77 (91.7) | 37 (94.9) | 36 (94.7) | 36 (80.0) | 11 (84.6) |
| Blood clotting | ||||||
| < 30 years | 3 (1.4) | 1 (1.2) | 0 80.0) | 0 (0.0) | 2 (4.4) | 0 (0.0) |
| 30-40 years | 4 (1.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (4.4) | 1 (7.7) |
| 41-50 years | 4 (1.8) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 1 (2.2) | 2 (15.4) |
| 51-60 years | 17 (7.7) | 8 (9.5) | 3 (7.7) | 2 (5.3) | 4 (8.9) | 0 (0.0) |
| >60 years | 19 (8.6) | 5 (6.0) | 2 (5.1) | 8 (21.1) | 3 (6.7) | 1 (7.7) |
| Age not Known | 175 (78.8) | 69 (82.1) | 34 (87.2) | 28 (73.7) | 33 (73.3) | 9 (69.2) |
| Dermatological test | ||||||
| < 30 years | 5 82.3) | 0 (0.0) | 1 (2.6) | 0 (0.0) | 3 (6.7) | 1 (7.7) |
| 30-40 years | 11 (5.0) | 5 (6.0) | 1 (2.6) | 1 (2.6) | 3 (6.7) | 0 (0.0) |
| 41-50 years | 16 (7.2) | 5 (6.0) | 4 (10.3) | 3 (7.9) | 3 (6.7) | 1 (7.7) |
| 51-60 years | 5 (2.3) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 3 (6.7) | 1 (7.7) |
| >60 years | 2 (0.9) | 1 (1.2) | 0 (0.0) | 1 (2.6) | 0 (0.0) | 0 (0.0) |
| Age not Known | 183 (82.4) | 72 (85.7) | 33 (84.6) | 33 (86.8) | 33 (73.3) | 10 (76.9) |
| Blood Pressure | ||||||
| < 30 years | 1 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.2) | 0 (0.0) |
| 30-40 years | 3 (1.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.2) | 1 (7.7) |
| 41-50 years | 32 (14.4) | 9 (10.7) | 6 (15.4) | 5 (13.2) | 10 (22.2) | 1 (7.7) |
| 51-60 years | 77 (34.7) | 31 (36.9) | 15 (38.5) | 12 (31.6) | 17 (37.8) | 2 (15.4) |
| >60 years | 48 (21.6) | 23 (27.4) | 6 (15.4) | 11 (28.9) | 6 (13.3) | 2 (15.4) |
| Age not Known | 61 (27.5) | 21 (25.0) | 12 (30.8) | 10 (26.3) | 10 (22.2) | 7 (53.8) |
| Blood glucose | ||||||
| < 30 years | 1 (0.5) | 0 80.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (7.7) |
| 30-40 years | 2 (0.9) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 41-50 years | 42 (18.9) | 13 (15.5) | 7 (17.9) | 9 (23.7) | 12 (26.7) | 1 (7.7) |
| 51-60 years | 63 (28.4) | 25 (29.8) | 13 (33.3) | 8 (21.1) | 15 (33.3) | 2 (15.4) |
| >60 years | 33 (14.9) | 18 (21.4) | 3 (7.7) | 5 (13.2) | 6 (13.3) | 1 (7.7) |
| Age not Known | 81 (36.5) | 27 (32.1) | 16 (41.0) | 16 (42.1) | 12 (26.7) | 8 (61.5) |
| Other | ||||||
| < 30 years | 1 (0.5) | 0 (0.0) | 1 (2.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 30-40 years | 13 (5.9) | 2 (2.4) | 3 (7.7) | 0 (0.0) | 6 (13.3) | 1 (7.7) |
| 41-50 years | 34 (15.3) | 16 (19.0) | 4 (10.3) | 8 (21.1) | 5 (11.1) | 1 (7.7) |
| 51-60 years | 38 (17.1) | 14 (16.7) | 6 (15.4) | 5 (13.2) | 10 (22.2) | 3 (23.1) |
| >60 years | 14 (6.3) | 6 (7.1) | 1 (2.6) | 2 (5.3) | 2 (4.4) | 3 (23.1) |
| Age not Known | 122 (55.0) | 46 (54.8) | 24 (61.5) | 23 (60.5) | 22 (48.9) | 5 (38.5) |
Data are expressed as the absolute frequencies (percentage).
Analysis of in-pharmacy measurements and tests revealed that e NE was the only area where the number of pharmacies with no agreement with specialists to analyse the results of the health parameter measurements conducted in their pharmacy (53.8%) exceeded those that had one (46.2%). The number of pharmacists per pharmacy responsible for conducting tests and measurements, and the hours of the day such services were available fluctuated among the geographic areas. A higher percentage of Island pharmacies assigned all the pharmacy staff responsibility for carrying out examinations (30.8% vs 22.1% general trend). In contrast, availability of such services throughout the opening hours was not ensured by 38.5% of Island pharmacies. This is the highest percentage registered, especially compared to the value calculated in the general analysis (12.2%). The question on the providers of training in the use of measurement devices and tests pointed out a deviation from the overall trend for Island pharmacies. In fact, in this area there was a markedly higher percentage of pharmacists trained by a local health authority (15.4% vs 2.3% general trend) or by a university/hospital (7.7% vs 0.9% general trend).
DISCUSSION
As a broad trend, telemedicine offers a new model of medical care to support patients in remote areas or those unable to travel to healthcare service providers, for example, the homebound.25,26 In addition, even patients able to travel can benefit, as they would be spared the expenditure of time and money for travel to medical appointments.27 If this technology is used to enable physicians to interact with a greater number of patients, for example, through videoconferencing, it can help in facing the upcoming shortage of physicians and improve the sustainability of health systems worldwide.28 In Italy, it has been estimated that 56,000 doctors will retire in the next fifteen years, and it is foreseen that the health system will not be able to cope properly with this haemorrhage.29 In fact, it has been predicted that 1.4 million Italians will remain without a GP.30 As a consequence of this trend, there will be inequalities in accessing the care provided by doctors and understaffed hospitals. Pharmacies able to offer basic medical tests and measurements and to communicate results to the client’s physician could provide a partial solution to this problem. In fact, considering that pharmacies are located throughout the nation, even in small towns or rural areas lacking a physician, their adoption of telemedicine services can help bridge the gap for clients.
A few scientific papers deal with telemedicine/telehealth pharmacy services, but those available indicate promising developments.31 One US study described a program of telemedicine pharmacy services to support organ transplant patients through such services as medication reconciliation, monitoring of patient compliance in taking medications, and provision of patient education.31 In Italy, the Templar Project has demonstrated the efficacy of having pharmacies coordinate the distance monitoring of patient blood pressure to manage hypertension.20 People living in remote and rural areas may not have easy access to pharmacy services and may resort to unnecessary GP consultations, or travel long distances to access a municipal pharmacy.32
Telemedicine/telehealth services in Italian pharmacies may have great potential, but the current reality is not exciting. Only one third of our respondents indicated that their pharmacies have implemented telehealth services. Moreover, even though telemonitoring can encompass a variety of clinical examinations, respondents reported that clients relied mostly on ECG, BP, and BG services.
There is a significant increase in the incidence of chronic diseases worldwide, and telemedicine examinations could play an important role in early detection in order to reduce mortality rates and disabilities.33
Telepharmacy may offer unique opportunity to improve access to screening and healthcare for cardiovascular patients.20,34,35
Studies have highlighted potential applications of telepharmacy in the prevention and treatment of other pathological conditions, such as diabetes, depression, asthma, etc.7
As shown by our data, the limited extent of telemedicine/telehealth use in Italian pharmacies probably depends by political reasons. A low commitment of health authorities in supporting the integration of this technology in pharmacies has belied expectations created after the promulgation of the decree introducing telehealth services in pharmacies. Health authorities were expected to act as a guide in helping pharmacists implement telemedicine. Instead, our respondents indicated that local health authorities focused on quality control inspections of state-owned pharmacies devices, and much less so of privately owned ones, even though, according to our results, the municipal pharmacies had the lowest degree of adoption of telemedicine services.
The Italian Local Health Authorities (commonly called in Italian as “Aziende Sanitarie Locali”, acronym ASL) are institutions of the Italian public health administration, responsible for the provision of health services. The ASL is part of the National Health Service and is the competence of the Regions. Through the National Accord between the National Health System and the pharmacies, the latter becomes part of the National Health System, as a real healthcare point.36,37
Relations between pharmacies and the National Health System are regulated by this National Agreement stipulated between Federfarma and the Regions with renewal every three years.37
At the local level, the ASL carries out a Pharmaceutical Service whose activity includes: health education activities about drugs and implementation of scientific information plans prepared by the Ministry of Health; technical and administrative activities in the areas of their competence; control over medicines and the rest of the medical instruments used by hospitals, facilities, and others; control on the proper application of the aforementioned National Agreement, with a technical-pharmacological evaluation of medical prescription and also statistical surveys on the prescriptions of medicines; drafting of the annual report on the trend of pharmaceutical expenditure and the consumption of medicines and the remaining health material at hospitals, facilities, and services of the ASL.36,37
Recently, the national and regional governments have increased their involvement in implementing telehealth in the pharmacy setting as witnessed by the recent opening of an experimental project to test the efficacy of some services provided by pharmacies, among them telemedicine services for ECG, spirometry, and Holter measurements for cardiac and blood pressure parameters.38 It is to be augured that 30% rate of adoption of telehealth in pharmacies identified in our study may improve over the next months or years, though we cannot predict its evolution.
To make pharmacists more familiar with telehealth/telemedicine, teaching programs in universities and training activities within the panel of the Continuing Medical Education Program are necessary.39,40 As noted in section one, over 80% of respondents received training in how to use telemedicine-related equipment such as blood pressure cuffs, blood glucose kits or ECG sets from the seller, about 14% from independent sources, only about 2% “from local health authorities” and a negligible percentage (0.9%) “from a university or a hospital”. It would appear that the national or local healthcare authorities are not interested in keeping pace with the innovations of the health domain, at least as far as telemedicine in pharmacies is concerned. This lack of attention is also borne out by respondents who seemed to indicate that quality inspections on devices and computer networks are carried out not by healthcare authorities but by the companies that sell the equipment, and in general, that inspections of pharmacies are generally conducted for government-owned community ones, not privately owned ones. This concern should be addressed by incorporating telehealth/telemedicine training into the obligatory continuing medical education credits that pharmacists are required by law to earn, and by organizing teaching programs on these skills in universities.39,40
To sum up, our study has revealed some encouraging results about the use of telemedicine in the pharmacy, the number of pharmacists in each pharmacy who are responsible for providing these services and the number of hours in a workday that they are offered. The opportunity for patients to receive their medical report at home is another positive factor. These services can expand the patient’s options for such tests and measurements and thus reduce the workload for hospitals.
Limitations
The study has some limitations. First of all, only 20% of the pharmacists contacted by email chose to participate by filling out the questionnaire; even so, the number was sufficient for a national survey with a confidence level of 95% and a confidence interval of 5%. One reason for the low level of participation could be that few of those contacted were interested in the topic. Another possible but not probable explanation is that few uses the internet and email, and thus did not receive the questionnaires. Probably the most tenable reason is that even though our team made every effort to design the questionnaire for simple and quick response, pharmacists were unwilling or unable to take time out of their very busy days to fill it out and return it. The research team did not collect any personal data in compliance with the Privacy Regulations in force. As a result, there is no way to know which of our respondents are pharmacy owners or employees. In addition, while submitting the questionnaire, we asked to participants to respect a ratio 1:1 between pharmacists and pharmacies. Since this kind of surveys is not carried out in person, it is hard for the investigators to verify whether the respondents stick to the instructions. As a result, the authors cannot ascertain if the ratio required was respected.
CONCLUSIONS
Our study results indicate that, despite its great potential, telemedicine/telehealth has yet to gain a strong foothold in Italian pharmacies. There is a disproportion in the offer of telemedicine services, as 33.3% of respondents in urban pharmacies use it, compared to 27.5% of respondents who work in municipal ones. The main reason could be that local healthcare authorities have failed to support the realization of the telemedicine provisions of the 2010 Pharmacy of Services legislation. This investigation has highlighted some of the most pressing problems limiting the satisfactory incorporation of digitalized patient care services in pharmacies. Future studies should analyse the economic sustainability of such services and evaluate the feasibility of government assistance to pharmacies for the purchase of equipment and to patients for expenditures on these in-pharmacy tests and measurements. In view of this, national health authorities, pharmacy regulatory bodies and academia should cooperate to identify the best possible solutions, starting from the awareness of how this technology could benefit patients and reduce healthcare inequalities. A recent agreement (October 2019) between the National and Regional Governments to which belong the responsibility of delivery locally health services make resources available for the development of large-scale tests on the “pharmacy of services”.36 We hope that this initiative could bring to a relaunch of such a project for the benefit of citizens that are the recipients of health services.
ACKNOWLEDGEMENTS
The support of the Italian Federazione Nazionale Associazioni Giovani Farmacisti (FENAGIFAR) and of their President Dr. Davide Petrosillo in discussing the different versions of the questionnaire and in spreading it among their associates is gratefully acknowledged. The present work was supported by institutional resources of the Camerino University. Stylistic revision of the manuscript by Ms. Sheilla Beatty is gratefully acknowledged.
Footnotes
CONFLICT OF INTEREST
Authors declare that there is no conflict of interests.
FUNDING
S. Baldoni was recipient of an EUREKA project bursary co-financed by Marches Regional Government, University of Camerino and Namirial SpA, Senigallia (Italy). G. Pallotta and G. G. Sagaro were recipients of University of Camerino PhD boursaries. G. Nittari was recipient of a position of Research Assistant (Assegno di Ricerca) of the School of Medicinal and Health Products Sciences of the University of Camerino.
Contributor Information
Simone Baldoni, Telemedicine and Telepharmacy Center, School of Medicinal and Health Products Sciences, University of Camerino. Camerino (Italy). simone.baldoni@unicam.it.
Graziano Pallotta, Telemedicine and Telepharmacy Center, School of Medicinal and Health Products Sciences, University of Camerino. Camerino (Italy). graziano.pallotta@gmail.com.
Enea Traini, Telemedicine and Telepharmacy Center, School of Medicinal and Health Products Sciences, University of Camerino. Camerino (Italy). enea.traini@unicam.it.
Getu G. Sagaro, Telemedicine and Telepharmacy Center, School of Medicinal and Health Products Sciences, University of Camerino. Camerino (Italy). getugamo.sagaro@unicam.it
Giulio Nittari, Telemedicine and Telepharmacy Center, School of Medicinal and Health Products Sciences, University of Camerino. Camerino (Italy). giulio.nittari@unicam.it.
Francesco Amenta, Telemedicine and Telepharmacy Center, School of Medicinal and Health Products Sciences, University of Camerino. Camerino (Italy). francesco.amenta@unicam.it.
References
- 1.American Telemedicine Association. [(accessed Jul 5 2020)];Core operational guidelines for telehealth services involving provider-patient interactions. Available at: https://www.uwyo.edu/wind/_files/docs/wytn-doc/toolkit-docs/ata_core_provider.pdf .
- 2.Stern A, Mitsakakis N, Paulden M, Alibhai S, Wong J, Tomlinson G, Brooker AS, Krahn M, Zwarenstein M. Pressure ulcer multidisciplinary teams via telemedicine:a pragmatic cluster randomized stepped wedge trial in long term care. BMC Health Serv Res. 2014;14:83. doi: 10.1186/1472-6963-14-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grabowski DC, O'Malley AJ. Use of telemedicine can reduce hospitalizations of nursing home residents and generate savings for medicare. Health Aff (Millwood) 2014;33(2):244–250. doi: 10.1377/hlthaff.2013.0922. [DOI] [PubMed] [Google Scholar]
- 4.Edirippulige S, Martin-Khan M, Beattie E, Smith AC, Gray LC. A systematic review of telemedicine services for residents in long term care facilities. J Telemed Telecare. 2013;19(3):127–132. doi: 10.1177/1357633x13483256. [DOI] [PubMed] [Google Scholar]
- 5.Dorsey ER, Topol EJ. State of Telehealth. N Engl J Med. 2016;375(2):154–161. doi: 10.1056/nejmra1601705. [DOI] [PubMed] [Google Scholar]
- 6.Totten AM, Womack DM, Eden KB, McDonagh MS, Griffin JC, Grusing S, Hersh WR. Mapping the Evidence for Patient Outcomes From Systematic Reviews. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016. AHRQ Comparative Effectiveness Technical Briefs Telehealth. [PubMed] [Google Scholar]
- 7.Kane-Gill SL, Niznik JD, Kellum JA, Culley CM, Boyce RD, Marcum ZA, He H, Perera S, Handler SM. Use of Telemedicine to Enhance Pharmacist Services in the Nursing Facility. Consult Pharm. 2017;32(2):93–98. doi: 10.4140/tcp.n.2017.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Di Cerbo A, Morales-Medina JC, Palmieri B, Iannitti T. Narrative review of telemedicine consultation in medical practice. Patient Prefer Adherence. 2015;9:65–75. doi: 10.2147/ppa.s61617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore MA, Coffman M, Jetty A, Klink K, Petterson S, Bazemore A. Family Physicians Report Considerable Interest in, but Limited Use of, Telehealth Services. J Am Board Fam Med. 2017;30(3):320–330. doi: 10.3122/jabfm.2017.03.160201. [DOI] [PubMed] [Google Scholar]
- 10.Uscher-Pines L, Mehrotra A. Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Aff (Millwood) 2014;33(2):258–264. doi: 10.1377/hlthaff.2013.0989. [DOI] [PubMed] [Google Scholar]
- 11.Sankaranarayanan J, Murante LJ, Moffett LM. A retrospective evaluation of remote pharmacist interventions in a telepharmacy service model using a conceptual framework. Telemed J E Health. 2014;20(10):893–901. doi: 10.1089/tmj.2013.0362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin CM, McSpadden CS. Changes in the state operations manual:implications for consultant pharmacy practice. Consult Pharm. 2006;21(12):948–961. doi: 10.4140/tcp.n.2006.948. [DOI] [PubMed] [Google Scholar]
- 13.Clark TR. Gap analysis:assessing the value perception of consultant pharmacist services and the performance of consultant pharmacists. Consult Pharm. 2008;23(Suppl C):3–15. [PubMed] [Google Scholar]
- 14.Garattini L, Van De Vooren K, Curto A. Will the reform of community pharmacies in Italy be of benefit to patients or the Italian National Health Service? Drugs Ther Perspect. 2012;28:23–26. doi: 10.1007/BF03262138. [DOI] [Google Scholar]
- 15.Federfarma. [(accessed Jul 5 2020)];[Italian Pharmacy] https://www.federfarma.it/Documenti/farmacia_italiana2018_19.aspx .
- 16.Paolillo C. [The pharmacy of services] Minist Heal Ital Repub. 2019:1–2. [Google Scholar]
- 17.Ministero della salute. [(accessed Jul 5 2020)];[Telemedicine National guidelines] Available at: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2129_allegato.pdf .
- 18.Baldoni S, Amenta F, Ricci G. Telepharmacy Services:Present Status and Future Perspectives:A Review. Medicina (Kaunas) 2019;55(7):327. doi: 10.3390/medicina55070327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ministero della salute. [(accessed Jul 5 2020)];[Decree about The pharmacy of services] Available at: http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?aggiornamenti=&attoCompleto=si&id=37427 .
- 20.Omboni S, Mancinelli A, Rizzi F, Parati G TEMPLAR (TEleMonitoring of blood Pressure in Local phARmacies) Project Group. Telemonitoring of 24-Hour Blood Pressure in Local Pharmacies and Blood Pressure Control in the Community:The Templar Project. Am J Hypertens. 2019;32(7):629–639. doi: 10.1093/ajh/hpz049. [DOI] [PubMed] [Google Scholar]
- 21. [(accessed Jul 5 2020)];SurveyMonkey. Available at: https://www.surveymonkey.com .
- 22.Trakman GL, Forsyth A, Hoye R, Belski R. Developing and validating a nutrition knowledge questionnaire:key methods and considerations. Public Health Nutr. 2017;20(15):2670–2679. doi: 10.1017/s1368980017001471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. [(accessed Jul 5 2020)];European Parliament Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC. Available at: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32016R0679&from=EN .
- 24.ISTAT. [(accessed Jul 5 2020)];Geographical distribution of Italian regions. Available at: http://dwcis.istat.it/cis/docs/4-8.htm .
- 25.Nayak KS, Ronco C, Karopadi AN, Rosner MH. Telemedicine and Remote Monitoring:Supporting the Patient on Peritoneal Dialysis. Perit Dial Int. 2016;36(4):362–366. doi: 10.3747/pdi.2015.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nittari G, Khuman R, Baldoni S, Pallotta G, Battineni G, Sirignano A, Amenta F, Ricci G. Telemedicine Practice:Review of the Current Ethical and Legal Challenges . Telemed J E Health. 2020 doi: 10.1089/tmj.2019.0158. [Ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Russo JE, McCool RR, Davies L. VA Telemedicine:An Analysis of Cost and Time Savings. Telemed J E Health. 2016;22(3):209–215. doi: 10.1089/tmj.2015.0055. [DOI] [PubMed] [Google Scholar]
- 28.Bashshur RL, Howell JD, Krupinski EA, Harms KM, Bashshur N, Doarn CR. The Empirical Foundations of Telemedicine Interventions in Primary Care. Telemed J E Health. 2016;22(5):342–375. doi: 10.1089/tmj.2016.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pini V. [In 15 years Italy will lose 14.000 physicians] [(accessed Jul 5 2020)];La Repubblica. 2019 Available at: https://www.repubblica.it/salute/medicina-e-ricerca/2019/04/18/news/se_in_italia_mancano_i_medici-224339652/
- 30.[Alert about the lack of physicians, 45.000 will retire in 5 years] [(accessed Jul 5 2020)];Ansa. Available from: http://www.ansa.it/canale_saluteebenessere/notizie/sanita/2018/02/09/-allarme-carenza-medici-45.000-in-pensione-in-5-anni-_aaa943db-7592-4649-8c1e-f80f4952e196.html .
- 31.Jandovitz N, Li H, Watts B, Monteiro J, Kohlberg D, Tsapepas D. Telemedicine pharmacy services implementation in organ transplantation at a metropolitan academic medical center. Digit Health. 2018;4:2055207618789322. doi: 10.1177/2055207618789322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Todd A, Copeland A, Husband A, Kasim A, Bambra C. Access all areas?An area-level analysis of accessibility to general practice and community pharmacy services in England by urbanity and social deprivation. BMJ Open. 2015;5(5):e007328. doi: 10.1136/bmjopen-2014-007328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. [(accessed Jul 5 2020)];Integrated Chronic Disease Prevention. Available at: https://www.who.int/chp/about/integrated_cd/en/
- 34.Omboni S, Tenti M. Telepharmacy for the management of cardiovascular patients in the community. Trends Cardiovasc Med. 2019;29(2):109–117. doi: 10.1016/j.tcm.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 35.Omboni S, Tenti M, Coronetti C. Physician-pharmacist collaborative practice and telehealth may transform hypertension management. J Hum Hypertens. 2019;33(3):177–187. doi: 10.1038/s41371-018-0147-x. [DOI] [PubMed] [Google Scholar]
- 36.Federfarma. [(accessed Jul 5 2020)];[The Pharmaceutical Convention] Available at: https://www.federfarma.it/Farmaci-e-farmacie/Farmacie-e-farmacisti-in-Italia/La-convenzione-farmaceutica.aspx .
- 37.Farmacie Comunali Riunite. [National Collective Agreement for the Relations with Pharmacies] Available at: http://www.fcr.re.it/accordo-collettivo-nazionale-per-la-disciplina-dei-rapporti-con-le-farmacie .
- 38. [(accessed Jul 5 2020)];[Starting of experimentation of pharmacy of services] Available at: https://www.ordinefarmacistimilano.it/553-la-conferenza-stato-regioni-da'-il-via-alla-farmacia-dei-servizi .
- 39.Merrell RC, Doarn CR. Students in Telemedicine:A Lasting Impact. Telemed J E Health. 2016;22(8):623. doi: 10.1089/tmj.2016.29010.rcm. [DOI] [PubMed] [Google Scholar]
- 40.[Continuous medical education] Radiol Med. 2003;106:16–17. [Google Scholar]


