Abstract
Objectives
The provision of high-quality family planning (FP) counseling can both enhance clients' experience of care and improve their ability to make and act on their contraceptive decisions. The Interpersonal Quality of Family Planning (IQFP) scale measures FP counseling quality and has been validated in the United States. We aimed to explore whether it remains appropriate for use in a low-/middle-income country (LMIC).
Study design
We surveyed 1201 nonsterilized married women ages 18–29 in Maharashtra, India, between September 2018 and June 2019. Respondents rated their FP provider from “poor” (1) to “excellent” (5) across 11 IQFP items. We assessed scale reliability via Cronbach's α test and used exploratory factor analysis to evaluate unidimensionality and regression models of plausibly related outcomes to assess construct validity.
Results
Five hundred four women (42%) had seen an FP provider within the past year, 491 (97%) of whom answered all items. Mean IQFP score was 2.62 out of 5 (SD 0.94, range 1–5). Scale reliability was high (α = 0.97). Exploratory factor analyses support unidimensionality (all factor loadings > 0.4). A 1-point increase in average IQFP score was associated with nearly double the odds of current modern contraceptive use (adjusted odds ratio = 1.73, 95% confidence interval = 1.36–2.19).
Conclusions
The IQFP scale shows good reliability and construct validity in this context, and its use in LMIC settings should be broadly considered. A higher IQFP score was associated with greater odds of contraceptive use. The reported FP counseling quality was low, so future public health efforts should aim to increase counseling quality to better meet the needs of women in low-resource settings like rural India. Measurement tools like IQFP can support success evaluation of the quality of care provided by family planning programs.
Implications
The Interpersonal Quality of Family Planning scale is a useful tool in rural India, a different context than the one in which it was developed. Use of the IQFP scale should be considered in other low-/middle-income countries to better measure the quality of family planning care provided.
Keywords: Contraceptive counseling, Family planning, Person-centered care, Validation, Quality of care
1. Introduction
Public health efforts often strive to increase utilization of effective contraceptive methods, particularly long-acting reversible contraceptives. Expanding access to contraceptives broadly has been shown to prevent maternal and infant morbidity and mortality [1]. However, programmatic global targets for family planning (FP) use can increase provider encouragement or even pressure for clients to use specific FP methods, which can compromise reproductive autonomy [2,3]. The Family Planning Program in India has a history of utilizing a contraceptive-specific target approach, incentivizing clinicians to provide specific methods, and providing contraception through sometimes unsafe FP camps and other potentially coercive practices [4,5].
In the international FP field, there has been recognition of the importance of interpersonal communication with FP providers since the 1990s, when the influential Bruce–Jain framework was first published [6]. Since then, there has been a continued emphasis on providing care that is respectful and focuses on meeting the reproductive needs of a person or couple rather than fertility regulation as the primary focus [[7], [8], [9]]. However, studies that have assessed the quality of counseling using recordings of visits have suggested that there remains significant room for improvement in the extent to which counseling is truly person-centered [10,11].
Measuring client-reported quality of FP counseling has the potential to allow for efficient assessment of the quality of FP programs and tracking of changes in response to quality improvement activities. However, tools that attempt to systematically measure the quality of FP care based on client report rarely focus on the dimensions of individuals' experiences with counseling [2]. Only a few existing tools designed to measure the quality of contraceptive counseling have assessed for reliability and validity in low- and middle-income countries (LMICs) [8,[12], [13], [14]]. Sudhinaraset et al., developed and validated the Person-Centered Family Planning scale in India and Kenya as a 20- or 22-item measure capturing two primary domains: autonomy, respectful care and communication; and health facility environment [14]. Jain et al. developed and validated a contraceptive care measure in India, both a longer 22-item and shorter 10-item form, capturing information exchange and interpersonal relations between provider and client on four domains: respectful care, method selection, effective use of method selected and continuity of contraceptive care [12]. Holt et al., developed and validated the Quality of Contraceptive Counseling scale in Mexico as a 22-item measure of FP client experiences with providers, focusing on three domains: information exchange, interpersonal relationship and disrespect/abuse [13]. All three measures capture slightly different dimensions of the FP experience. We sought to assess reliability and validity of a of measure of person-centered communication about FP in an LMIC. Focusing on person-centered communication is a valuable approach to ensure the protection of FP clients' rights and is essential to FP-related research and program quality improvement efforts.
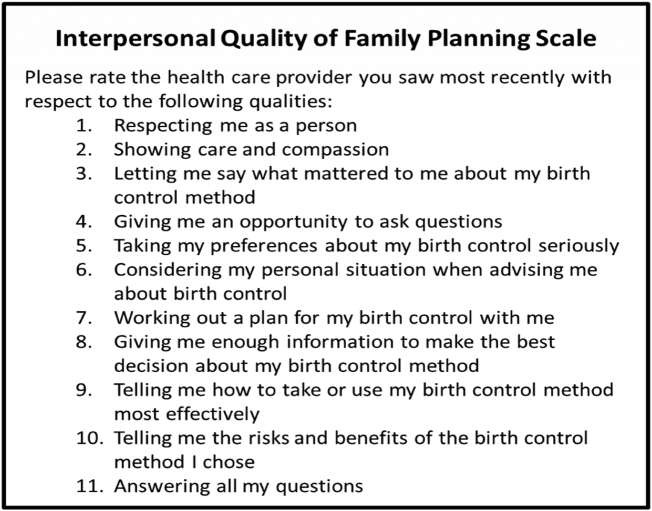
The Interpersonal Quality of Family Planning (IQFP) scale is a validated client-reported evaluation of their recent FP provider's communication during contraceptive counseling [15] (Fig. 1). It consists of 11 items assessing general client–provider communication and FP-specific communication and was initially developed to capture three domains: interpersonal connection, receiving adequate information and decision support. Each item is a 5-point Likert scale ranging from poor [1] to excellent [5]. Prior research has established that high quality of contraceptive counseling is associated with increased uptake and continuation of contraception, as measured by the IQFP scale [16] and other measures of counseling quality [17]. However, the IQFP scale has not yet been studied or used in the Indian or other LMIC context.
Fig. 1.
IQFP items.
Efforts aimed at improving the quality of contraceptive counseling in India have the potential to better meet the reproductive needs of people and couples while ensuring their reproductive autonomy. The IQFP scale may be a valuable tool to both measure and track progress in improving counseling quality, but it has not been validated outside of the United States. In this study, we tested the IQFP scale's reliability and validity in India and assessed whether the experience of person-centered and high-quality FP counseling was associated with contraceptive use and related outcomes.
2. Material and methods
2.1. Data source
The Counseling Husbands & wives to Achieve Reproductive health and Marital equity (CHARM2) study is a gender-synchronized, gender-transformative counseling intervention that aims to support use of modern contraceptive methods when desired and to decrease interpersonal violence. It is an ongoing cluster randomized controlled trial of young married couples in the rural Pune district of Maharashtra, India, further described in detail elsewhere [18]. Modern contraceptive method use in this area is 32% among nonsterilized women age 15–49 years [19]. We examined IQFP scale response at baseline among the 1201 women who completed surveys between September 2018 and June 2019. Inclusion criteria for the CHARM2 study included married couples with women age 18–29 years, both partners nonsterilized, living together for at least 6 months and no plan to migrate in the subsequent 2 years. We recruited participants via random selection from household rosters and approached and interviewed them in their homes. The baseline survey assessed demographics; FP history, behaviors and preferences; and FP and gender norms and attitudes, and included the IQFP scale. Institutional Review Boards of The University of California San Diego, the Indian Council of Medical Research–National Institute for Research in Reproductive Health in India and the Population Council approved all procedures for the CHARM2 study.
2.2. Adaptation of the IQFP scale
A clinic-based sample in urban California was utilized for initial development and validation of the IQFP scale. [15]. Briefly, to develop the scale, initial item selection was based on qualitative work regarding patient preferences for contraceptive counseling. Content and construct validity were then assessed among a cohort of 346 women immediately following a visit at a participating FP, primary care or gynecology clinic between 2009 and 2012. Modern contraceptive method use in this context is upwards of 65% among nonsterilized women age 18–49 years [20].
In contrast to the setting in which the scale was developed, we administered cross-sectional surveys in CHARM2 in homes rather than in clinic settings. As such, we modified the scale prompt to refer to the most recent FP provider a respondent had seen, limited to a provider seen within the past year to minimize recall bias. Local experts and study field staff reviewed the survey items and did not identify any other changes to content necessary for appropriateness or understanding in the local context. We therefore used the 11 IQFP items and their response options verbatim translated to the local language, Marathi, by bilingual study staff. We then pretested the IQFP items via cognitive interviews with 20 female participants before final implementation and did not identify any additional changes necessary for understanding from these interviews.
2.3. Measures
2.3.1. IQFP scale
Each of the 11 items in the IQFP scale had answer options as follows: poor (1), fair (2), good (3), very good (4) and excellent (5). We evaluated the scale outcome as a mean score and as a categorical average response.
2.3.2. Associated outcomes
We defined current modern contraceptive use as use of a reversible modern method available locally [condoms, pills, intrauterine devices (IUDs), injectable contraception or emergency contraceptive pills] within the past 3 months among nonpregnant women [21]. Two items assessed contraceptive self-efficacy: “How sure are you that you could use FP?” and “How sure are you that you could use FP even if your husband did not want you to?” [22]. For each, we dichotomized responses “completely sure” or “somewhat sure” to “yes,” and “neither sure nor unsure,” “somewhat unsure” or “completely unsure” to “no.” Only current users were asked about receipt of desired method, as indicated by answering “yes” to the question “Is the method you used in the last 3 months the one you wanted?”
2.4. Analyses
We first summarized the mean and categorical average IQFP score. We assessed internal scale reliability via Cronbach's α test. We assessed individual item performance via item–total correlations (e.g., correlation in response between each individual item and the total scale score; if an item is poorly correlated with the total score, it suggests that item is less reliable) and Chronbach's α if item deleted (e.g., calculated Cronbach's α with each item removed from the scale; if α increases substantially when an item is removed, it suggests that item is less reliable). We used exploratory factor analysis to evaluate scale unidimensionality or whether all scale items capture one construct rather than multiple separate constructs. If factor analysis suggests that the scale is multidimensional (multiple factors), the scale would potentially be separated into those component parts rather than considered as a single scale. Finally, we conducted multivariate logistic regression analyses of several plausibly related outcomes — modern contraceptive method use, contraceptive self-efficacy and receipt of desired method (or no method if none was desired) — to assess construct validity. We constructed both unadjusted models and models accounting for baseline demographics known to be associated with contraceptive use including age, parity, highest level of education, poverty [household has Below Poverty Line (BPL) card], religion (Hindu or other) and caste. Significance was set at p <.05 for all comparisons, and 95% confidence intervals (CIs) are reported throughout. All analyses were conducted using STATA 15.1.
3. Results
3.1. Description of the sample
Forty-two percent (504) of women reported seeing a healthcare provider for FP within the past year; 97% (491/504) of those answered all IQFP items (Table 1). Characteristics of women who had seen a provider and answered the IQFP scale were similar to those of the overall study population (Table 1), though women who had seen a provider and answered the scale items were less likely to be nulliparous (16% nulliparous among CHARM2 study sample, 11% nulliparous among IQFP respondents). IQFP scale respondents were 24 years old on average (SD 3 years), most had higher secondary or postsecondary education (55%), the majority were Hindu (89%), and a quarter were low income. Of these 491 women, 49% reported currently using a modern contraceptive method, 97% reported they were certain that they would be able to use contraception, 37% reported that they were certain they would be able to use contraception even if their husband did not want them to, and 95% reported they were using the method that they wanted to use. Of the modern contraceptive methods in use, male condoms were the most popular (28% use) followed by IUDs (15%) and pills (5%).
Table 1.
Characteristics of CHARM2 study participants (n = 1201) and IQFP scale respondents (n = 491)
| CHARM2 | IQFP respondents | |
|---|---|---|
| N = 1201 | N = 491 | |
| N (%) | N (%) | |
| Visited an FP provider in past year | ||
| Yes | 504 (42%) | 491 (100%) |
| No | 696 (58%) | – |
| Declined | 1 (< 1%) | – |
| Demographics | ||
| Age | ||
| Mean (SD) | 23.9 (3.0) | 23.9 (3.0) |
| Education | ||
| None or primary | 169 (14.1) | 86 (17.5) |
| Secondary | 345 (28.7) | 135 (27.5) |
| Higher secondary or postsecondary | 687 (57.2) | 270 (55.0) |
| Religion | ||
| Hindu | 1110 (92.4) | 437 (89.0) |
| Muslim, Buddhist, Jain, Christian, none, other | 91 (7.6) | 54 (11.0) |
| Scheduled tribe/scheduled caste | ||
| No | 818 (68.1) | 337 (68.6) |
| Yes | 383 (31.9) | 154 (31.4) |
| BPL card ownership | ||
| No | 902 (75.2) | 368 (75.0) |
| Yes | 297 (24.8) | 123 (25.0) |
| Parity | ||
| None | 197 (16.4) | 53 (10.8) |
| One | 644 (53.6) | 260 (53.0) |
| Two or more | 360 (30.0) | 178 (36.2) |
| Outcomes | ||
| Current modern contraceptive method usea | 379 (37.9) | 201 (49.3) |
| Pilla | 34 (3.4) | 22 (5.4) |
| IUDa | 89 (8.9) | 63 (15.4) |
| Male condoma | 257 (25.7) | 116 (28.4) |
| Injectablea | 4 (0.4) | 4 (1.0) |
| Self-efficacy to use contraception, general | 1142 (95.1) | 477 (97.1) |
| Self-efficacy to use contraception, husband opposition | 529 (44.0) | 180 (36.7) |
| Using desired contraceptive methodb | 596 (96.1) | 276 (95.5) |
Nonpregnant women only.
Women reporting contraception use within 3 months only.
3.2. IQFP score descriptive statistics
The mean IQFP score was 2.62 out of 5 (SD 0.94, range 1–5), and 2% of the study sample provided a perfect score. About one in six women (16.3%) rated their most recent provider seen as poor (average score 1–1.5), 31.0% fair (average score 1.51–2.5), 35.6% good (average score 2.51–3.5), 14.1% very good (average score 3.51–4.5) and 3.1% excellent (average score 4.51–5) (Fig. 2).
Fig. 2.
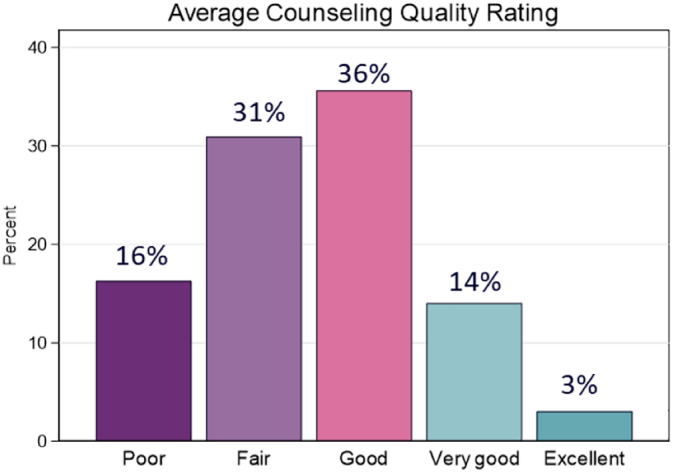
IQFP scale response in the study population (n = 491).
3.3. IQFP scale performance metrics
Scale reliability was very high (α = 0.97). Cronbach's α remained nearly unchanged when any one item was removed (α if item deleted ranging from 0.96 to 0.97) (Table 2). The mean item–total correlation coefficient was high (0.86), with individual item correlations to total ranging from 0.51 to 0.94.
Table 2.
Mean response, factor loads, item–total correlations and α if removed for items in the IQFP scale (n = 491)
| Item | Mean (SD) | Factor loading | Item–total correlation | α if item removed | |
|---|---|---|---|---|---|
| 1 | Respecting me as a person | 3.26 (0.80) | 0.46 | 0.51 | 0.97 |
| 2 | Showing care and compassion | 3.00 (0.87) | 0.67 | 0.71 | 0.97 |
| 3 | Letting me say what mattered to me about my birth control method | 2.62 (1.13) | 0.88 | 0.89 | 0.96 |
| 4 | Giving me the opportunity to ask questions | 2.72 (1.06) | 0.84 | 0.86 | 0.96 |
| 5 | Taking my preferences about my birth control seriously | 2.51 (1.14) | 0.91 | 0.91 | 0.96 |
| 6 | Considering my personal situation when advising me about birth control | 2.43 (1.13) | 0.91 | 0.91 | 0.96 |
| 7 | Working out a plan for my birth control with me | 2.40 (1.15) | 0.92 | 0.92 | 0.96 |
| 8 | Giving me enough information to make the best decision about my birth control method | 2.49 (1.17) | 0.94 | 0.94 | 0.96 |
| 9 | Telling me how to take or use my birth control method most effectively | 2.41 (1.14) | 0.93 | 0.93 | 0.96 |
| 10 | Telling me the risks and benefits of the birth control method I chose | 2.40 (1.11) | 0.89 | 0.90 | 0.96 |
| 11 | Answering all my questions | 2.59 (1.18) | 0.93 | 0.93 | 0.96 |
Exploratory factor analyses supported the scale's unidimensionality, with only one component with eigenvalue greater than 1 (single item eigenvalue 8.03), a very high percentage of variance explained by the single factor (97%) and factor loadings on the single factor ranging from 0.46 to 0.93 (Table 2). This suggests that the 11 items capture a single underlying construct and that all 11 items are related to that underlying construct.
A 1-point increase in average IQFP score was associated with nearly double the odds of current modern method use [odds ratio (OR)= 1.84, 95% CI = 1.47–2.31]; this finding remained significant when adjusting for age, parity, education, poverty, religion and caste [adjusted odds ratio (AOR)= 1.73, 95% CI = 1.36–2.19] (Table 3). Higher IQFP score was also associated with a trend towards greater self-efficacy to use contraception generally (AOR = 1.97, 95% CI = 0.93–4.17) and with significantly greater odds of self-efficacy to use contraception even when their husband opposed (AOR = 2.20, 95% CI = 1.74–2.78). There was no association between IQFP score and whether a woman was using her desired contraceptive method (AOR = 0.98, 95% CI = 0.53–1.82). As a post hoc analysis to further examine desired contraceptive method use, we tabulated reasons for not using a preferred method. The most frequently reported reason for use of a nonpreferred method was husband or in-law disapproval (38% of women who would have preferred an alternate method); only two women reported that they used a nonpreferred method because a provider recommended the current method instead.
Table 3.
Associations of mean IQFP score with related outcomes, unadjusted and adjusted logistic regression findings (n = 491)
| OR (95% CI) | AORc (95% CI) | |
|---|---|---|
| Current modern contraceptive method usea | 1.84 (1.47–2.31) | 1.73 (1.36–2.19) |
| Self-efficacy to use contraception, general | 2.07 (1.05–4.09) | 1.97 (0.93–4.17) |
| Self-efficacy to use contraception, husband opposition | 2.31 (1.84–2.89) | 2.20 (1.74–2.78) |
| Using desired contraceptive methodb | 1.09 (0.60–2.01) | 0.98 (0.53–1.82) |
Nonpregnant women only.
Women reporting contraception use within 3 months only.
Adjusted models include age, parity, education, poverty, religion and caste.
4. Discussion
The IQFP scale performed well in tests of reliability, unidimensionality and construct validity in this rural Indian setting, suggesting that the continuous IQFP scale is valid, relevant and useful both when administered in a nonclinical setting, and in an LMIC context.
We found that the quality of interpersonal communication in FP counseling was significantly associated with modern contraceptive use in this population. In addition to improving quality of counseling as a standalone goal, this finding supports existing literature that suggests measuring and improving the quality of counseling are important elements of understanding and improving FP utilization [16,23]. IQFP was also associated with self-efficacy to use FP in this population. The Social Cognitive Theory posits that self-efficacy is a key predictor of contraceptive use [24], and an association between self-efficacy and contraceptive use has been shown [25], especially for condoms [[26], [27], [28]].
IQFP score was not associated with receipt of desired method in our sample. This is likely because preferred method use was high (95%) and because the most frequently reported reasons for not using a preferred method were not directly related to counseling. Previous research also suggests that women may report having received their preferred method but not have actually been involved in the decision making for method type [29]. Women who indicated that they would have preferred an alternate method most frequently reported that their husband or in-laws disapproved, and husband and in-law influence over reproductive decision making has been shown to be common in rural India [30,31]. Therefore, while provision of high-quality counseling is an important element of contraceptive use, there remain a number of barriers beyond the healthcare encounter which affect clients' contraceptive use. While the IQFP captures an important domain of contraceptive care, researchers and clinicians seeking to understand the broader contraceptive context should consider items and scales that capture these domains in addition to the IQFP. Counseling which directly addresses male involvement in contraceptive decision making and reproductive coercion may offer a mechanism by which providers can reduce these barriers [32].
Despite the focus on person-centered care in the international FP field, the quality of counseling has remained poor. In this population, reported quality of FP counseling was low, with 47% of respondents rating their recent FP provider as “poor” or “fair” overall, and no single item had an average score above “good,” suggesting low quality of counseling overall. The low quality of counseling reported may still be overestimated in this context, as our study sample was limited to married women, and unmarried women may receive inferior care due to the stigma of premarital sex [33]. The IQFP in its initial development was also dichotomized to perfect vs. nonperfect score; given low overall quality and very low use of perfect scores (2%), it would not be appropriate to operationalize the scale as such in this population.
While all individual items had low scores, items with the lowest ratings were related to shared decision making and sharing of information. This likely reflects an authoritative healthcare provider–patient relationship in the Indian context generally [34,35]. Previous research has demonstrated that FP providers in India often impose barriers to FP beyond what is medically necessary based on judgments of patient characteristics such as age, parity and partner consent [36]. Person-centered FP care will require a shift in this approach to increase the agency of patients. Current theory and empirical evidence emphasize the importance of exchanging information and eliciting patients' preferences to support their choices and meet their needs [8,12,14,15,37].
Despite promising findings, this study did have several limitations. First, while question understanding was reviewed by study staff, we saw evidence of possible enumerator bias in score reporting (average score ranging from 2.2 to 3.5 across different study enumerators); subsequent discussion suggested that this may have been due in part to misunderstanding on how to respond when a question did not apply, though this reportedly occurred infrequently. Use of “declined to answer” or “not applicable” should be explicitly defined and discussed in future scale use; contexts which use retrospective reporting such as described here should consider “don't remember” as an additional option. Second, a range of providers, including public and private clinics, hospitals and pharmacies, can deliver FP services in this context. We hypothesized that different providers may be more or less effective at providing quality FP care, and deficiencies in quality of care would have different implications and remedies by provider type. However, we did not collect information on who the FP providers were that were evaluated in the IQFP scale. Future use of the scale in similar contexts where FP can be provided by a range of practitioners would be well served to collect this information. Third, limitations on the generalizability of these findings are present, most importantly the exclusion of sterilized women from the cohort from which this study population was taken. We would hypothesize that patient–provider interactions that lead to female sterilization may be different from interactions regarding other forms of contraception, particularly in the Indian context where there is a history of coercive practices around sterilization [5]. Additionally, female sterilization is broadly used in this context, and exclusion of sterilized women excludes a meaningful proportion of the population using contraception, though not a meaningful proportion of the population seeking contraceptive counseling. However, while this may limit the generalizability of the IQFP scores seen here, we believe that the sample affirms the scale validity and utility more broadly in this context. Finally, formal formative work with the study population to elicit their preferences and priorities for quality in FP counseling was not conducted. While a subset of study participants and local study staff reviewed the items and confirmed their understanding and relevance, there may be additional domains of FP counseling quality which are important or relevant to this population which are not captured by this tool.
Though other measures exist that capture similar domains of care, the tool examined here has several potential advantages [[12], [13], [14]]. The IQFP utilizes Likert-style response options, which allow for greater nuance in reported care. In content, the IQFP focuses distinctly and specifically on the patient-centeredness of communication and counseling rather than the FP clinical encounter more generally, and it relies on patients' own experiences rather than on providers' performance of a prespecified set of actions. Finally, the IQFP is a relatively brief measure at only 11 items. The tools cited above also share some of these strengths, but the IQFP is unique in having all three. However, the purpose of this study was not to compare this measure to other available measures, and this study is not intended to establish the IQFP as the gold standard for measuring the quality of contraceptive care.
While the IQFP scores may have utility within a population, we have not established that IQFP scores can be directly compared across populations. This is due to a range of factors, including context-specific survey response patterns such as different levels of social desirability bias, differential use of scale scoring such as tendency to use or avoid extreme scores, and different expectations of clinical encounters and health-related communication more generally. Thus, while this validation study has demonstrated that the IQFP is appropriate to use in this LMIC context, it does not establish that the IQFP score has the equivalent meaning as it does in the context in which it was developed. Finally, while the IQFP appears valid in this context, this study was not originally designed specifically to be a validation study of this measure, and we did not test or compare alternate similar measures of the quality of contraceptive care. Future research should validate this measure across more diverse populations and contexts in India and across LMICs, inclusive of validation with other standard measures of quality of care, to verify current findings. Such research should include clinical and nonclinical settings, a range of potential FP providers and contexts with differing patterns of FP use. Further qualitative research examining the most relevant and important domains of FP care to patients in novel settings would also inform the value or shortcomings of the IQFP in this setting.
Ultimately, these findings reinforce the value of interpersonal quality of counseling to support women's contraceptive decision making, and demonstrate that measuring quality is useful and necessary for ensuring person-centered FP care. The IQFP should be considered for use more broadly by researchers interested in understanding how to support clients' decision making about contraception. Quality of care reported in this context was low, and future public health efforts should focus on increasing both the quality of counseling provided and contraceptive access to better meet the needs of women in low-resource settings like rural India.
Acknowledgments
Acknowledgments
We thank the CHARM2 participants, field research staff and the public and private healthcare providers who delivered the intervention to couples. We also thank Jennifer Yore for her work in study oversight, as well as Natalie Wyss and Alyssa Brodsky for their efforts in study coordination.
Funding
This work was supported by the National Institutes of Health (grant numbers R01-HD084453-01A1, NICHD 5K12HD001259) and the Bill & Melinda Gates Foundation, Seattle, WA (grant numbers OPP1163682, INV-002967). The funders had no role in study design; in collection, analysis or interpretation of data; in writing of the report; or in decision to submit for publication.
Footnotes
Clinical Trials Registry: NCT03514914.
References
- 1.Black R.E., Levin C., Walker N. Reproductive, maternal, newborn, and child health: key messages from disease control priorities 3rd edition. The Lancet. 2016;388:2811–2824. doi: 10.1016/S0140-6736(16)00738-8. [DOI] [PubMed] [Google Scholar]
- 2.Holt K., Dehlendorf C., Langer A. Defining quality in contraceptive counseling to improve measurement of individuals’ experiences and enable service delivery improvement. Contraception. 2017;96:133–137. doi: 10.1016/j.contraception.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Senderowicz L. “I was obligated to accept”: a qualitative exploration of contraceptive coercion. Soc Sci Med. 2019;239:112531. doi: 10.1016/j.socscimed.2019.112531. [DOI] [PubMed] [Google Scholar]
- 4.Pachauri S. Priority strategies for India’s family planning programme. Indian J Med Res. 2014;140(Suppl):S137–S146. [PMC free article] [PubMed] [Google Scholar]
- 5.Hardee K., Harris S., Rodriguez M. Achieving the goal of the London Summit on Family Planning by adhering to voluntary, rights-based family planning: what can we learn from past experiences with coercion? Int Perspect Sex Reprod Health. 2014;40:206–214. doi: 10.1363/4020614. [DOI] [PubMed] [Google Scholar]
- 6.Bruce J. Fundamental elements of the quality of care: a simple framework. Stud Fam Plann. 1990;21:61–91. [PubMed] [Google Scholar]
- 7.Diamond-Smith N., Warnock R., Sudhinaraset M. Interventions to improve the person-centered quality of family planning services: a narrative review. Reproductive health. 2018;15:144. doi: 10.1186/s12978-018-0592-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jain A.K., Hardee K. Revising the FP quality of care framework in the context of rights-based family planning. Stud Fam Plann. 2018;49:171–179. doi: 10.1111/sifp.12052. [DOI] [PubMed] [Google Scholar]
- 9.Holt K., Caglia J.M., Peca E., Sherry J.M., Langer A. A call for collaboration on respectful, person-centered health care in family planning and maternal health. Reproductive health. 2017;14:20. doi: 10.1186/s12978-017-0280-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim Y.M., Kols A., Mucheke S. Informed choice and decision-making in family planning counseling in Kenya. Int Fam Plan Perspect. 1998:4–42. [PubMed] [Google Scholar]
- 11.Kim Y.M., Kols A., Martin A. Promoting informed choice: evaluating a decision-making tool for family planning clients and providers in Mexico. Int Fam Plan Perspect. 2005:162–171. doi: 10.1363/3116205. [DOI] [PubMed] [Google Scholar]
- 12.Jain A., Aruldas K., Mozumdar A., Tobey E., Acharya R. Validation of two quality of care measures: results from a longitudinal study of reversible contraceptive users in India. Stud Fam Plann. 2019;50(2):179–193. doi: 10.1111/sifp.12093. [DOI] [PubMed] [Google Scholar]
- 13.Holt K., Zavala I., Quintero X., Hessler D., Langer A. Development and validation of the client-reported quality of contraceptive counseling scale to measure quality and fulfillment of rights in family planning programs. Stud Fam Plann. 2019;50:137–158. doi: 10.1111/sifp.12092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sudhinaraset M., Afulani P.A., Diamond-Smith N., Golub G., Srivastava A. Development of a person-centered family planning scale in India and Kenya. Stud Fam Plann. 2018;49:237–258. doi: 10.1111/sifp.12069. [DOI] [PubMed] [Google Scholar]
- 15.Dehlendorf C., Henderson J.T., Vittinghoff E., Steinauer J., Hessler D. Development of a patient-reported measure of the interpersonal quality of family planning care. Contraception. 2018;97:34–40. doi: 10.1016/j.contraception.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Dehlendorf C., Henderson J.T., Vittinghoff E. Association of the quality of interpersonal care during family planning counseling with contraceptive use. American journal of obstetrics and gynecology. 2016;215(78):e1–e9. doi: 10.1016/j.ajog.2016.01.173. [DOI] [PubMed] [Google Scholar]
- 17.RamaRao S., Lacuesta M., Costello M., Pangolibay B., Jones H. The link between quality of care and contraceptive use. Int Fam Plan Perspect. 2003:76–83. doi: 10.1363/ifpp.29.076.03. [DOI] [PubMed] [Google Scholar]
- 18.Dixit A., Averbach S., Yore J. A gender synchronized family planning intervention for married couples in rural India: study protocol for the CHARM2 cluster randomized controlled trial evaluation. Reproductive health. 2019;16:88. doi: 10.1186/s12978-019-0744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.IIPS. National Family Health Survey-4 2015–16. District fact sheet: Pune, Maharashtra.
- 20.Douglas-Hall A., Kost K., Kavanaugh M.L. Guttmacher Institute; New York: 2018. State-level estimates of contraceptive use in the United States, 2017. [Google Scholar]
- 21.Hubacher D., Trussell J. A definition of modern contraceptive methods. Contraception. 2015;92:420–421. doi: 10.1016/j.contraception.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 22.CARE USA. Women's Empowerment–Multidimensional Evaluation of Agency, Social Capital & Relations (WE-MEASR): a tool to measure women's empowerment in sexual, reproductive and maternal health programs. CARE USA Atlanta, GA; 2014.
- 23.Abdel-Tawab N., RamaRao S. Do improvements in client–provider interaction increase contraceptive continuation? Unraveling the puzzle. Patient Educ Couns. 2010;81:381–387. doi: 10.1016/j.pec.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 24.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 25.Hamidi O.P., Deimling T., Lehman E., Weisman C., Chuang C. High self-efficacy is associated with prescription contraceptive use. Womens Health Issues. 2018;28:509–513. doi: 10.1016/j.whi.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Do M., Fu H. Is women’s self-efficacy in negotiating sexual decisionmaking associated with condom use in marital relationships in Vietnam? Stud Fam Plann. 2011;42:273–282. doi: 10.1111/j.1728-4465.2011.00290.x. [DOI] [PubMed] [Google Scholar]
- 27.Closson K., Dietrich J.J., Lachowsky N.J. Gender, sexual self-efficacy and consistent condom use among adolescents living in the HIV hyper-endemic setting of Soweto. South Africa AIDS and behavior. 2018;22:671–680. doi: 10.1007/s10461-017-1950-z. [DOI] [PubMed] [Google Scholar]
- 28.Brafford L.J., Beck K.H. Development and validation of a condom self-efficacy scale for college students. J Am Coll Health. 1991;39 doi: 10.1080/07448481.1991.9936238. [DOI] [PubMed] [Google Scholar]
- 29.Mozumdar A., Gautam V., Gautam A. Choice of contraceptive methods in public and private facilities in rural India. BMC Health Serv Res. 2019;19:421. doi: 10.1186/s12913-019-4249-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghule M., Raj A., Palaye P. Barriers to use contraceptive methods among rural young married couples in Maharashtra, India: qualitative findings. Asian journal of research in social sciences and humanities. 2015;5:18. doi: 10.5958/2249-7315.2015.00132.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Char A., Saavala M., Kulmala T. Influence of mothers-in-law on young couples’ family planning decisions in rural India. Reprod Health Matters. 2010;18:154–162. doi: 10.1016/S0968-8080(10)35497-8. [DOI] [PubMed] [Google Scholar]
- 32.Tancredi D.J., Silverman J.G., Decker M.R. Cluster randomized controlled trial protocol: addressing reproductive coercion in health settings (ARCHES) BMC Womens Health. 2015;15:57. doi: 10.1186/s12905-015-0216-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Majumdar C. Attitudes towards premarital sex in India: traditionalism and cultural change. Sexuality & Culture. 2018;22:614–631. [Google Scholar]
- 34.Fochsen G., Deshpande K., Thorson A. Power imbalance and consumerism in the doctor-patient relationship: health care providers’ experiences of patient encounters in a rural district in India. Qual Health Res. 2006;16:1236–1251. doi: 10.1177/1049732306293776. [DOI] [PubMed] [Google Scholar]
- 35.Mole T.B., Begum H., Cooper-Moss N. Limits of ‘patient-centredness’: valuing contextually specific communication patterns. Med Educ. 2016;50:359–369. doi: 10.1111/medu.12946. [DOI] [PubMed] [Google Scholar]
- 36.Calhoun L.M., Speizer I.S., Rimal R. Provider imposed restrictions to clients’ access to family planning in urban Uttar Pradesh. India: a mixed methods study BMC health services research. 2013;13:532. doi: 10.1186/1472-6963-13-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sudhinaraset M., Afulani P., Diamond-Smith N., Bhattacharyya S., Donnay F., Montagu D. Advancing a conceptual model to improve maternal health quality: the person-centered care framework for reproductive health equity. Gates Open Res. 2017;1:1. doi: 10.12688/gatesopenres.12756.1. [DOI] [PMC free article] [PubMed] [Google Scholar]