Abstract
The nasal cavities are complex anatomical structures with high inter-individual variability that relates to different functions. Different anatomic variants may manifest at this site, mainly belonging to the nasal septum and turbinates. Precise knowledge of the anatomy and variants is fundamental for both radiologists and ENT surgeons. This article provides an overview of the main anatomic variants and their frequency, according to the existing literature, as well as ongoing research on nasal cavity segmentation in order to obtain personal 3D models and to predict post-surgical results.
Keywords: Computed tomography, nasal septum, nasal cavity, anatomic variants, nasal turbinate
Introduction
The nasal cavities are complex anatomical structures that relate to different functions and are characterised by high inter-individual variability. The main functioning consists of humidification and warming of the inspired air, filtration and paranasal sinuses ventilation, but they are also involved in olfaction and speech.
Their variants in shape and morphology can alter the airflow and affect the function of the nose, but they can also determine significant sequelae in the lower respiratory tract. Moreover, nasal airway affections can alter other homeostatic systems, such as sleep and cardiovascular health.1
The assessment of anatomical variants of the nasal cavities with computed tomography (CT) and cone-beam computed tomography (CBCT) has grown in importance, as different forms of such alterations may change the drainage pathways from the nasal cavity and paranasal sinuses, resulting in obstruction and sinusitis; that is, anatomical variants of the middle turbinate have a role in the pathogenesis of phlogistic processes of the paranasal sinuses.2,3 Moreover, inadequate knowledge in recognising anatomical variants may result in surgical complications.4,5 Knowledge of these anatomical structures and their spatial relationships is critical for diagnosis and treatment planning.
Definition
The nasal cavity is a bilateral structure located in the midface, limited inferiorly by the hard palate, laterally by the maxillary sinuses medial walls and cranially by the nasal, ethmoid and sphenoid bones,6 and includes the nasal septum, the nasal mucosa and the nasal turbinates. A midline septum oriented in the sagittal plane divides the nasal cavity into two bilateral cavities.
The nasal cavities are essential for humidifying and warming the inspired air. Anatomically, they are limited superiorly by the nasal spine of the frontal bone and the nasal bone anteriorly, and by the cribriform plate of the ethmoid bone and the body of the sphenoid bone posteriorly.6 Inferiorly, the floor of the nasal cavities is constituted anteriorly by the palatine process of the maxilla and posteriorly by the horizontal plate of the palatine bone. The lateral walls of the nasal cavities are made by the ethmoid bone, the perpendicular plate of the palatine bone, the medial plate of the pterygoid process of the sphenoid bone, the medial surface of the lacrimal and maxillary bones and the inferior concha.6,7 Medially, the two nasal cavities are divided by the nasal septum.
The nasal turbinates (or conchae) are bony structures extending from the lateral and superior walls of each nasal cavity and projecting infero-medially.7 The turbinates are usually in three pairs, classified as maxilloturbinals (inferior turbinates) and ethmoturbinals (middle and superior turbinates). Rarely, a fourth turbinate – the supreme turbinate, also called Santorini’s concha – is observed. This is situated at the posterosuperior portion of the lateral nasal wall, close to the lateral border of the ostium of the sphenoid sinus. Each pair of turbinates develops through an endochondral ossification, with cartilaginous precursors observable as early as eight weeks in utero.7,8 The inferior concha typically is the largest, while the superior is the smallest.
The turbinates divide each nasal cavity into channel-like paths known as meatuses (Figure 1), located inferolateral to each turbinate.7 The inferior meatus is positioned below the inferior turbinate and is the point of drainage of the nasolacrimal duct; the middle meatus is the point of drainage for the frontal, anterior ethmoid and maxillary sinuses. The superior meatus communicates with the posterior ethmoid and sphenoid sinuses through the spheno-ethmoidal recess that is located behind the superior turbinate, lateral to the nasal septum.9 Maxillary sinuses communicate with the middle meatus through the ostium. The middle turbinate represents an important landmark for the identification of anatomic structures located in the lateral wall of the nasal cavity, and the knowledge of its anatomy and possible variations is pivotal in endoscopic sinus surgery.10
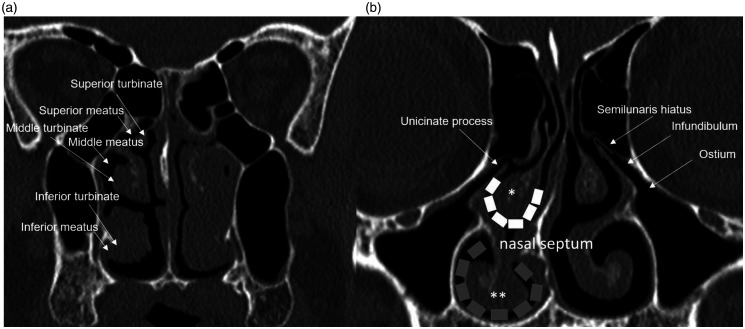
Figure 1.
Anatomy of the nasal turbinates and meatuses. (a) Nasal polyposis obstructing the left nasal cavity. On the right side, inferior, middle and inferior turbinates are visible; inferior meatus is partially occupied by hypertrophic inferior meatus. (b) White dashed line: middle meatus; grey dashed line: inferior meatus; asterisk: middle turbinate; double asterisks: inferior turbinate.
While the superior turbinate (and supreme turbinate, if present) is usually covered by olfactory mucosa, the middle and the inferior ones show respiratory mucosa, with high-density vascular capillaries and venous sinusoid structures, which help warm, moisten and filter the inspired air, changing the airflow resistance. They constantly swell and shrink in response to external conditions and endogenous stimuli, under the control of the sympathetic nervous system. This process is called the ‘nasal cycle’ and is characterised by congestion and decongestion of the nasal cavities.11 Swelling of the turbinate tissue due to inflammation, allergy or a reaction to environmental pollution results in blockage of the nasal airway. Some hormonal changes such as pregnancy or the premenstrual stage can also determine prolonged or transitory congestion of turbinate tissues.
The right and left nasal cavities are divided by the nasal septum (Figure 2), which is a mixed osseous and cartilaginous structure made up of five components: the quadrangular cartilage, the perpendicular plate of the ethmoid bone, the vomer, the nasal crest of maxillary bones and palatine bones. The vomer and the ethmoid bone contribute to the osseous, posterior part of the septum.10 Vascular supply for the nasal cavities is provided by the internal maxillary artery that derives from the external carotid artery, and by the anterior and posterior ethmoidal arteries, branches of the internal carotid artery.11 The nasal cavity is innervated by the olfactory, ophthalmic and maxillary branches of the trigeminal and facial nerves.
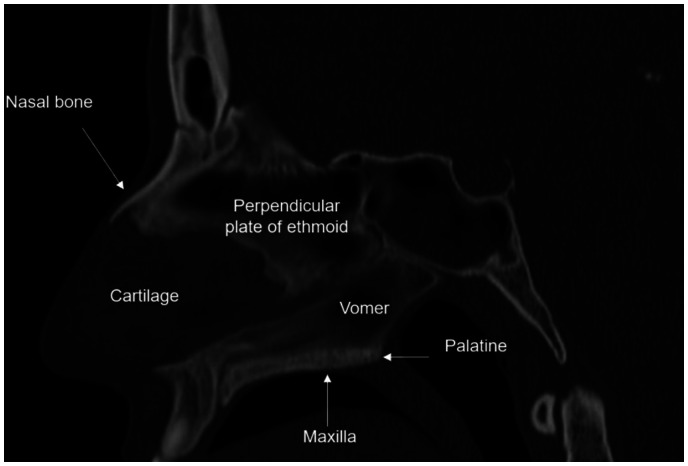
Figure 2.
Composition of the nasal septum: the anterior cartilage component, and the bony posterior component, constituted by the vomer, by the perpendicular plate of the ethmoid, the maxillary crest.
Anatomical variants
Nasal septum deviation
Nasal septum deviation (Figure 3) consists of any deviation of the septal contour towards one side of the nasal cavity12 and is recognisable in >50% of patients.13 It can be described as a right-sided, left-sided or S-shaped curvature. The incidence of septum deviation ranges from 14.1%14 to 90.4%.15 Septal deformities are far more common than a non-deviated septum.16
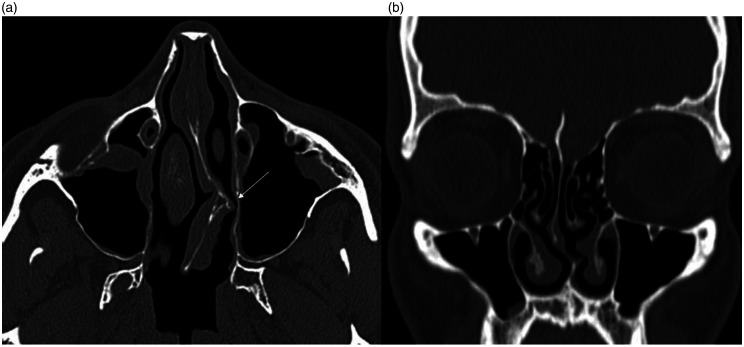
Figure 3.
Axial images of (a) left-sided septal deviation associated with bony spur (white arrow), with contact with the medial wall of the left maxillary sinus and (b) coronal reformations showing S-shaped septal deviation.
In a study of 594 maxillary sinus CT scans, left-sided deviations were observed more frequently than right-sided ones (43.9% vs. 36.4%). S-curved septal deviations were found in 18.5% of patients, with the highest prevalence in males. Dorso-ventral deviations were seen in 10.9%, and caudal-rostral deviations in 7.6% of cases.12
A group of 150 patients with nasal septal deviation was studied by Yazici, who observed that conchal abnormalities were present in 63.3% of cases, with concha bullosa being the most prevalent variation (45.3%), followed by paradox middle concha (8.7%) and pneumatised upper concha (9.3%). According to his results, the incidence of concha bullosa was higher in patients with nasal septal deviation when compared to the current literature.17
A deviated nasal septum may be congenital or due to trauma, including minor trauma in early life or birth trauma. The deviation may be mild and asymptomatic. When a deviation is severe, it can determine obstructive symptomatology, with redirection of the inspired air through the nasal cavity. Moreover, a septal deviation determines compensatory hypertrophy of the contralateral inferior turbinate and concha bullosa of the middle turbinate, thus worsening the obstruction, or results in hypoplasia of the ipsilateral turbinates.
Nasal septum pneumatisation
Pneumatisation of the nasal septum (Figure 4) is rarely observed. The reported incidence ranges from 0%17 to 4%.18 In some cases, this pneumatisation may narrow the spheno-ethmoidal recess thereby limiting access to the sphenoid ostium.19 Pneumatisation of the perpendicular plate of the ethmoid bone has also been reported in cases of nasal septal mucocele.20
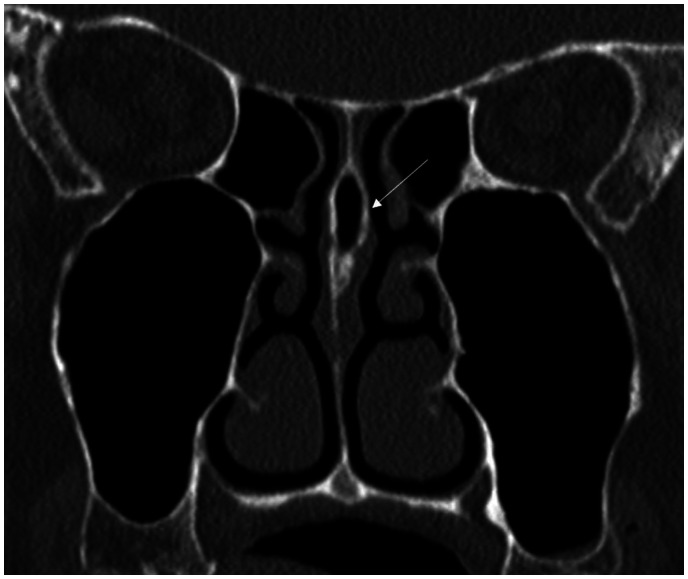
Figure 4.
Nasal septum pneumatisation (white arrow).
Septal spur
A septal spur may be associated with septal deviation (Figure 4),19 with a reported incidence of 34.0% without significant differences according to the side, or it can also manifest with a normally aligned septum, with an incidence of 5.8%, more frequently reported on the left side. Bridging spurs, between the septum and the adjacent nasal wall, are frequently associated with hypoplasia of the middle turbinate and accessory ostium of the sinuses.21 In a study of patients affected by rhinogenic contact point headache, patients with septal spurs presented with the most intense pain sensation and the highest duration and frequency of headaches. It was therefore suggested that pressure between mucosal surfaces in the small area of septal spur determines a more intense sense of pain than in cases of septal deviation and concha bullosa, which is related to the production and local mucosal liberation of substance P and other neuropeptides.22
Concha bullosa
Concha bullosa consists of the pneumatisation of a turbinate or the presence of an air cell in the turbinate. Its frequency ranges from 14% to 53.6% of the population.23,24 The precise mechanism of concha bullosa formation is not clear and may be related to compensatory changes in airflow linked to a deviated septum or individual anatomical factors.12
The expression ‘concha bullosa of the middle turbinate’ refers to the pneumatisation of the inferior bulbous portion, whereas when the pneumatisation is limited to the vertical lamella above the level of the osteomeatal unit, it is called ‘Grunwald’s cells’ or ‘lamellar bulla’ (Figure 5).25 It is most frequent in the middle turbinate, although pneumatised inferior and superior turbinate (Figure 6) have also been described, and it may be unilateral or bilateral. The pneumatised cavity presents with a connection to the corresponding nasal meatus. In a study of South Korean patients, inferior concha bullosa was found only in males, with an incidence of 1%.12 Unilateral concha bullosa is frequently associated with a deviation of the nasal septum, away from the side of the concha.
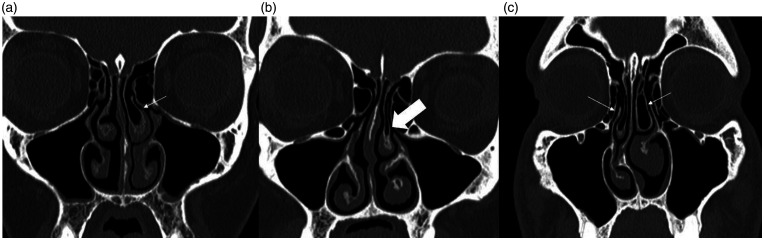
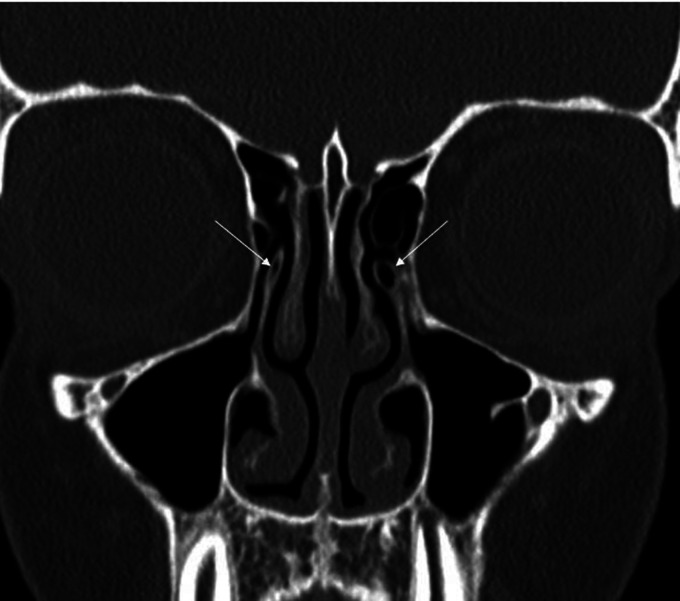
Figure 5.
Anatomical variants of the left middle turbinate, with evidence of (a) concha bullosa (white arrow), with pneumatisation of the inferior bulbous portion, and (b) Grunwald’s cell (thick white arrow), with pneumatisation of the vertical lamella above the level of the osteomeatal unit. (c) Bilateral concha bullosa is visible (white arrows).
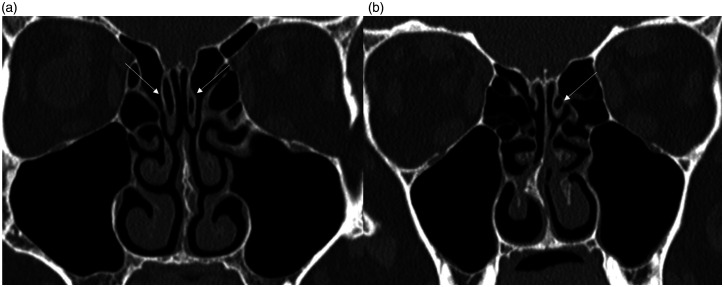
Figure 6.
Pneumatisation of both (a) the superior turbinates and (b) the left superior turbinate (white arrows).
Bolger et al. proposed a classification, according to the location, of three types: lamellar, if the pneumatisation occurs in the vertical lamella, also described as Grunwald’s cells; bulbous, when the pneumatisation is located in the bulbous segment of the concha; or extensive, when the pneumatisation affects both the lamella and the bulbous portion.26
The vast majority of concha bullosa are asymptomatic, but it may be associated with complications such as ventilation and drainage alteration related to its size.27 There is no consensus about a possible aetiological role of middle turbinate concha bullosa in recurrent chronic sinusitis. This can be hypothesised when this variant impinges or hinders the osteomeatal complex.12
Comparative studies between asymptomatic subjects and patients affected by sinusitis have produced discordant results. Some studies observed a higher incidence of concha bullosa,28,29 this was not confirmed in the study by Azila et al., showing a similar frequency of these variants in patients and asymptomatic individuals,30 and by studies involving only symptomatic patients.24 In a study based on CT analysis of 36 with recurrent acute rhinosinusitis compared to a control group of 42, the patient group showed a higher frequency of concha bullosa (41.7% vs. 28.6%), but this difference was not statistically significant.31 No statistically significant correlation has been observed between different types of concha bullosa (lamellar, bulbous and extensive) and sinus disease.23 The reported incidence of superior turbinate pneumatisation reaches 57%.32 Extensive pneumatisation can cause nasal obstruction and headache.33
Inferior turbinate concha bullosa has rarely been reported,24 with an incidence <1%,20 related to an altered epithelial invagination during inferior turbinate ossification, resulting in a double lamella,20 or to an extension of the maxillary sinus pneumatisation to the inferior turbinate during foetal development.34 It can be asymptomatic or related to complications due to its large size, when overly pneumatised, and leads to nasal obstruction.
Paradoxical turbinate
Paradoxical curvature (Figure 7) is a peculiar morphology of the middle turbinate with a scroll convexity in the lateral rather than medial aspect, facing the nasal septum, and is seen in 4–27% of the population, usually bilaterally.10,30 This anatomic variant alone is not pathological, but it can lead to significant narrowing and blockage of the middle meatus or the osteomeatal complex, with consequent hindering of the normal drainage, resulting in rhinosinusitis. When combined with a bulbous middle turbinate, it can potentially cause nasal obstruction.32 Paradoxical turbinate usually occurs bilaterally.9
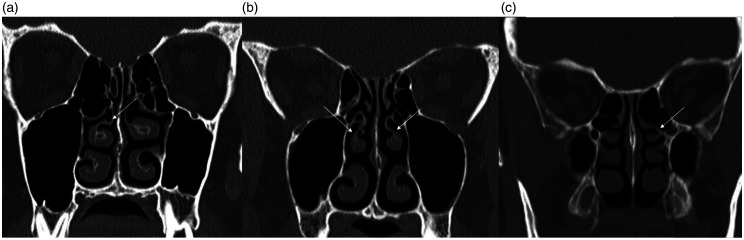
Figure 7.
Right paradoxical middle turbinate showing (a) inferomedially curved turbinate edge with the concave surface facing the nasal septum, (b) bilateral paradoxical middle turbinates and (c) paradoxical left superior turbinate.
Rare anatomic variants of the middle turbinate
The inferior portion of the middle turbinate can curve on itself, creating a deep invagination called a ‘turbinate sinus’ (Figure 8(a)).20 Another rare variant is the development of a secondary middle turbinate (Figure 8(b)), visible as a bony projection covered with mucosa, originating from the lateral nasal wall.35 The reported incidence is 0.8–6.8% of cases.36 These variations may result in osteomeatal complex narrowing and favour paranasal inflammations. The bifid turbinate (Figure 8(c)) is a rare variant, recognisable when two bony lamellae share the same root. This variant has also been observed in the inferior turbinate35 and is more frequently observed among patients affected by rhinosinusitis.18
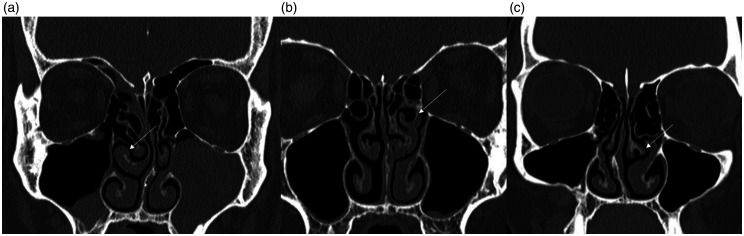
Figure 8.
(a) Turbinate sinus (white arrow): evidence of deep invagination of the inferior portion of the turbinate. (b) Secondary left middle turbinate (white arrow). Presence of accessory curved bony lamella covered by soft tissue protruding into the nasal cavity. (c) Left middle bifid turbinate (white arrow).
Uncinate process pneumatisation
The uncinate process is a sickle-shaped bone lamella with an inferior attachment to the inferior concha and palatine bone and an anterosuperior attachment to the lacrimal bone. The posterosuperior attachment is variable. Also known as ‘uncinate bulla’ (Figure 9), it is a rare variant, being observed in 0.4–5% of cases.26,36 It is believed to be related to an extension of the agger nasi cell in the anterosuperior part of the uncinate process, and may determine a significant narrowing of the infundibulum, with a consequent hindering to sinus ventilation.37,38
Figure 9.
Bilateral pneumatisation of the uncinate processes (white arrows).
Segmentation analysis
As corrective surgery for nasal obstruction has a high frequency but up to 37% of patients report poor or no improvement in the symptomatology after the intervention,1,39 new techniques such as computational fluid dynamics (CFD) to predict surgical outcome have been developed. These are mainly based on segmentation procedures to produce an anatomically precise model derived from CT and magnetic resonance imaging (Figure 10).40–42 One critical step is the segmentation of the nasal cavities from imaging data sets. The anatomical complexity of these structures and the extensive connection to other airway components, such as the ethmoid sinuses and the pharynx, makes the segmentation of the only nasal cavity difficult without the manual intervention of an experienced operator. Nasal airway segmentation can also be applied in surgical planning and the assessment of postoperative results.43
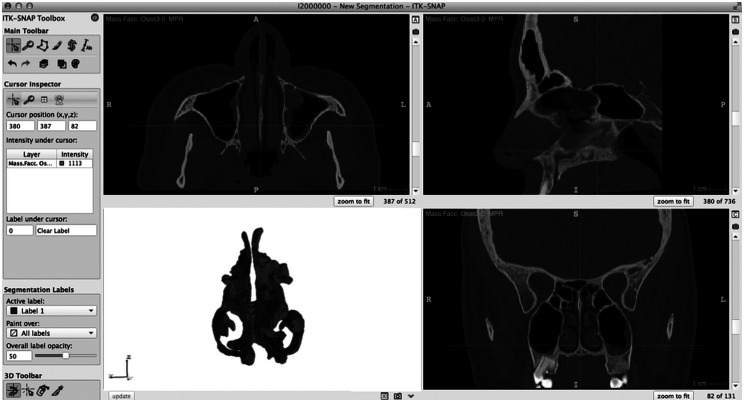
Figure 10.
Segmentation procedures of the nasal cavities with ITK SNAP.
Different techniques have been developed for the segmentation of nasal cavities. In a study on CBCT, Bui et al.41 proposed an automatic multi-step level-set segmentation procedure for the nasal cavity and the paranasal sinuses. Semi-automatic segmentation can be executed with a preset threshold in Hounsfield Units43 and region-growing methods.44 This second method has also been proposed for the calculation of nasal air space volumes, and the measurements of sinonasal polyps and mucosal thickening. Keustermans et al. used an active shape model to obtain a semi-automatic segmentation of the nasal cavities. This is a landmark-based statistical shape model technique that applies anatomical knowledge to form a set of training data in order to obtain a segmentation of determined structures, such as the nasal cavities, decreasing the manual intervention time required for the operation.45 Huang et al. elaborated on an automatic segmentation in order to obtain nasal models from CT for the analysis of CFD, showing high segmentation accuracy and an average distance error of 0.3 mm.40
Conclusions
There are a multitude of anatomic variants of the nasal cavities, some of which are very common in the population. CT is the gold standard to image patients with suspected nasal and paranasal inflammatory diseases. Knowledge of these anatomical variants and the correct identification of CT data sets aid in the understanding of factors favouring sinusitis and help in planning the right ENT treatment.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
ORCID iDs
Michaela Cellina https://orcid.org/0000-0002-7401-1971
Daniele Gibelli https://orcid.org/0000-0002-9591-1047
References
- 1.Bhattacharyya N. Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngoscope 2010; 120: 635–638. [DOI] [PubMed] [Google Scholar]
- 2.Basić N, Basić V, Jelić M, et al. [Pneumatization of the middle nasal turbinate: a CT study]. Lijec Vjesn 1998; 120: 200–201. [PubMed] [Google Scholar]
- 3.Hasso AN, Kim-Miller MJ. Imaging of craniofacial and sinonasal anomalies. Neuroradiol J 2006; 19: 413–426. [DOI] [PubMed] [Google Scholar]
- 4.Marsot-Dupuch K. Anatomic variations of paranasal sinuses: application to functional endoscopic surgery. Rivist Neuroradiol 2000; 13; 221–229. [Google Scholar]
- 5.Gibelli D, Cellina M, Gibelli S, et al. Anatomical variants of sphenoid sinuses pneumatisation: a CT scan study on a Northern Italian population. Radiol Med 2017; 122: 575–580. [DOI] [PubMed] [Google Scholar]
- 6.Parks ET. Cone beam computed tomography for the nasal cavity and paranasal sinuses. Dent Clin North Am 2014; 58: 627–651. [DOI] [PubMed] [Google Scholar]
- 7.Dalgorf DM, Harvey RJ. Chapter 1: sinonasal anatomy and function. Am J Rhinol Allergy 2013; 27: S3–6. [DOI] [PubMed] [Google Scholar]
- 8.Maier W, Ruf I. Morphology of the nasal capsule of primates – with special reference to Daubentonia and Homo. Anat Rec (Hoboken) 2014; 297: 1985–2006. [DOI] [PubMed] [Google Scholar]
- 9.Neskey D, Eloy JA, Casiano RR. Nasal, septal, and turbinate anatomy and embryology. Otolaryngol Clin North Am 2009; 42: 193–205, vii. [DOI] [PubMed] [Google Scholar]
- 10.Pérez-Piñas, Sabaté J, Carmona A, et al. Anatomical variations in the human paranasal sinus region studied by CT. J Anat 2000; 197: 221–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MacArthur FJ, McGarry GW. The arterial supply of the nasal cavity. Eur Arch Otorhinolaryngol 2017; 274: 809–815 [DOI] [PubMed] [Google Scholar]
- 12.Koo SK, Kim JD, Moon JS, et al. The incidence of concha bullosa, unusual anatomic variation and its relationship to nasal septal deviation: a retrospective radiologic study. Auris Nasus Larynx 2017; 44: 561–570. [DOI] [PubMed] [Google Scholar]
- 13.Beale TJ, Madani G, Morley SJ. Imaging of the paranasal sinuses and nasal cavity: normal anatomy and clinically relevant anatomical variants. Semin Ultrasound CT MR 2009; 30: 2–16. [DOI] [PubMed] [Google Scholar]
- 14.Arslan G, Karaali K. Concha bullosa and nasal septal deviation. AJNR Am J Neuroradiol 2005; 26: 1882. [PMC free article] [PubMed] [Google Scholar]
- 15.Shokri A, Faradmal MJ, Hekmat B. Correlations between anatomical variations of the nasal cavity and ethmoidal sinuses on cone-beam computed tomography scans. Imaging Sci Dent 2019; 49: 103–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gray LP. Deviated nasal septum. Incidence and etiology. Ann Otol Rhinol Laryngol Suppl 1978; 87: 3–20. [DOI] [PubMed] [Google Scholar]
- 17.Yazici D. The analysis of computed tomography of paranasal sinuses in nasal septal deviation. J Craniofac Surg 2019; 30: e143–e147. [DOI] [PubMed] [Google Scholar]
- 18.Gibelli D, Cellina M, Gibelli S, et al. Anatomical variants of ethmoid bone on multidetector CT. Surg Radiol Anat 2018; 40: 1301–1311. [DOI] [PubMed] [Google Scholar]
- 19.Vaid S, Vaid N. Normal anatomy and anatomic variants of the paranasal sinuses on computed tomography. Neuroimag Clin N Am 2015; 25: 527–548. [DOI] [PubMed] [Google Scholar]
- 20.Lei L, Wang R, Han D. Pneumatization of perpendicular plate of the ethmoid bone and nasal septal mucocele. Acta Otolaryngol 2004; 124: 221–222. [DOI] [PubMed] [Google Scholar]
- 21.Earwaker J. Anatomic variants in sinonasal CT. Radiographics 1993; 13: 381–415. [DOI] [PubMed] [Google Scholar]
- 22.Peric A, Rasic D, Grgurevic U. Surgical treatment of rhinogenic contact point headache: an experience from a tertiary care hospital. Int Arch Otorhinolaryngol 2016; 20: 166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hatipoğlu HG, Cetin MA, Yüksel E. Concha bullosa types: their relationship with sinusitis, ostiomeatal and frontal recess disease. Diagn Interv Radiol 2005; 11: 145–149. [PubMed] [Google Scholar]
- 24.Unlü HH, Akyar S, Caylan R, et al. Concha bullosa. J Otolaryngol 1994; 23: 23–27. [PubMed] [Google Scholar]
- 25.Tiwari R, Goyal R. Study of anatomical variations on CT in chronic sinusitis. Indian J Otolaryngol Head Neck Surg 2015; 67: 18–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope 1991; 101: 56–64. [DOI] [PubMed] [Google Scholar]
- 27.Uygur K, Tüz M, Doğru H. The correlation between septal deviation and concha bullosa. Otolaryngol Head Neck Surg 2003; 129: 33–36. [DOI] [PubMed] [Google Scholar]
- 28.Lloyd GA, Lund VJ, Scadding GK. CT of the paranasal sinuses and functional endoscopic surgery: a critical analysis of 100 symptomatic patients. J Laryngol Otol 1991; 105: 181–185. [DOI] [PubMed] [Google Scholar]
- 29.Calhoun KH, Waggenspack GA, Simpson CB, et al. CT evaluation of the paranasal sinuses in symptomatic and asymptomatic populations. Otolaryngol Head Neck Surg 1991; 104: 480–483. [DOI] [PubMed] [Google Scholar]
- 30.Azila A, Irfan M, Rohaizan Y, et al. The prevalence of anatomical variations in osteomeatal unit in patients with chronic rhinosinusitis. Med J Malaysia 2011; 66: 191–194. [PubMed] [Google Scholar]
- 31.Alkire BC, Bhattacharyya N. An assessment of sinonasal anatomic variants potentially associated with recurrent acute rhinosinusitis. Laryngoscope 2010; 120: 631–634. [DOI] [PubMed] [Google Scholar]
- 32.Shpilberg KA, Daniel SC, Doshi AH, et al. CT of anatomic variants of the paranasal sinuses and nasal cavity: poor correlation with radiologically significant rhinosinusitis but importance in surgical planning. AJR Am J Roentgenol 2015; 204: 1255–1260. [DOI] [PubMed] [Google Scholar]
- 33.Herzallah IR, Hamed MA, Salem SM, et al. Mucosal contact points and paranasal sinus pneumatization: Does radiology predict headache causality? Laryngoscope 2015; 125: 2021–2026. [DOI] [PubMed] [Google Scholar]
- 34.Yang BT, Chong VF, Wang ZC, et al. CT appearance of pneumatized inferior turbinate. Clin Radiol 2008; 63: 901–905. [DOI] [PubMed] [Google Scholar]
- 35.Aksungur EH, Biçakçi K, Inal M, et al. CT demonstration of accessory nasal turbinates: secondary middle turbinate and bifid inferior turbinate. Eur J Radiol 1999; 31: 174–176. [DOI] [PubMed] [Google Scholar]
- 36.Vaid S, Vaid N, Rawat S, et al. An imaging checklist for pre-FESS CT: framing a surgically relevant report. Clin Radiol 2011; 66: 459–470. [DOI] [PubMed] [Google Scholar]
- 37.Kantarci M, Karasen RM, Alper F, et al. Remarkable anatomic variations in paranasal sinus region and their clinical importance. Eur J Radiol 2004; 50: 296–302. [DOI] [PubMed] [Google Scholar]
- 38.Parks ET. Cone beam computed tomography for the nasal cavity and paranasal sinuses. Dent Clin North Am 2014; 58: 627–651. [DOI] [PubMed] [Google Scholar]
- 39.Nouraei SA, Elisay AR, Dimarco A, et al. Variations in paranasal sinus anatomy: implications for the pathophysiology of chronic rhinosinusitis and safety of endoscopic sinus surgery. J Otolaryngol Head Neck Surg 2009; 38: 32–37. [PubMed] [Google Scholar]
- 40.Huang R, Nedanoski A, Fletcher DF, et al. An automated segmentation framework for nasal computational fluid dynamics analysis in computed tomography. Comput Biol Med 2019; 115: 103505. [DOI] [PubMed] [Google Scholar]
- 41.Bui NL, Ong SH, Foong KW. Automatic segmentation of the nasal cavity and paranasal sinuses from cone-beam CT images. Int J Comput Assist Radiol Surg 2015; 10: 1269–1277. [DOI] [PubMed] [Google Scholar]
- 42.Cellina M, Fetoni V, Baron P, et al. Unusual primary central nervous system lymphoma location involving the fourth ventricle and hypothalamus. Neuroradiol J 2015; 28: 120–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dastidar P, Heinonen T, Numminen J, et al. Semi-automatic segmentation of computed tomographic images in volumetric estimation of nasal airway. Eur Arch Otorhinolaryngol 1999; 256: 192–8198. [DOI] [PubMed] [Google Scholar]
- 44.Tingelhoff K, Moral AI, Kunkel ME, et al. Comparison between manual and semi-automatic segmentation of nasal cavity and paranasal sinuses from CT images. Conf Proc IEEE Eng Med Biol Soc 2007; 2007: 5505–5508. [DOI] [PubMed] [Google Scholar]
- 45.Keustermans W, Huysmans T, Schmelzer B, et al. Matlab® toolbox for semi-automatic segmentation of the human nasal cavity based on active shape modeling. Comput Biol Med 2019; 105: 27–38. [DOI] [PubMed] [Google Scholar]