Abstract
Although numerous longitudinal studies have examined heterogeneity in posttraumatic stress disorder (PTSD) symptom course, the long-term course of the disorder remains poorly understood. This study sought to understand and predict long-term PTSD symptom course among a nationwide sample of Operations Enduring Freedom and Iraqi Freedom veterans enrolled in Veterans Health Administration services. We assessed PTSD symptoms at four time points over approximately 4.5 years (M = 55.11 months, SD = 6.89). Participants (N = 1,353) with and without probable PTSD were sampled at a 3:1 ratio, and male and female veterans were sampled at a 1:1 ratio to fully explore the heterogeneity of PTSD symptom course and the effect of sex on symptom course. By coding time as years since index trauma, we estimated the course of PTSD symptoms over 20 years. Results indicate symptom course is most appropriately characterized by substantial heterogeneity. On average, veterans experienced initial PTSD symptom severity above the diagnostic threshold following trauma exposure, which was initially stable over time, then later began to gradually improve. Although results indicate symptoms eventually began to decline, this effect was gradual; most participants continued to meet or exceed the PTSD long after trauma exposure. We identified several predictors and correlates of symptom course, including Hispanic ethnicity, post-deployment social support, and co-occurring psychopathology. Results highlight the heterogeneous nature of PTSD symptom course following trauma exposure and the urgency of the need to ensure access to evidence-based care and to improve available treatments.
Keywords: PTSD, trauma, veterans, OEF/OIF, growth curve modeling
General Scientific Summary
This study examined the course of posttraumatic stress disorder (PTSD) symptoms among a nationwide sample of Operations Enduring Freedom (OEF) and Iraqi Freedom (OIF) veterans enrolled in Veterans Health Administration (VHA) services (N = 1,353). On average, veterans experienced initial PTSD symptom severity above the diagnostic threshold following trauma exposure, which was initially stable over time, then later began to gradually improve. Results highlight the heterogeneous nature of PTSD symptom course following trauma exposure and the urgency of the need to ensure access to evidence-based care and to improve available treatments.
Introduction
Numerous longitudinal studies examined posttraumatic stress disorder (PTSD) symptom course following trauma exposure among combat veterans (see Galatzer-Levy, Huang, & Bonanno, 2018; Able & Benedek, in press, for reviews). This work provided important insights into PTSD symptom course among veterans, many of whom struggle with severe PTSD and associated impairment (e.g., Hoge, Auchterlonie, & Milliken, 2006; Schnurr et al, 2009). Most research on symptom course to date focused on either short-term (i.e., the first few years) or medium-term (i.e., 5–10 years) course following trauma exposure (e.g., Bonanno et al., 2012; Eekhout, Geuze, & Vermetten, 2016; Karstoft, Armour, Elklit, & Solomon, 2013; Mota et al., 2019; Orcutt, Erickson, & Wolfe, 2004; Vasterling et al., 2016). These studies typically measure symptoms relatively frequently (e.g., every year) in order to understand symptom change over time, but are unable to provide insight into long-term symptom course.
A smaller group of studies examined the longer-term PTSD symptom course. One such study was the National Vietnam Veterans Longitudinal Study (NVVLS), which assessed PTSD symptoms among Vietnam veterans on two occasions approximately 10 and 40 years after the conclusion of the war and found that many veterans struggled with significant mental health problems decades after combat exposure (Marmar et al., 2015). Likewise, Koenen and colleagues (2003) examined PTSD symptoms at two points approximately 9 and 23 years after the conclusion of the war. These long-term studies provide critical insights into diagnostic status or symptom severity long after trauma exposure. However, due to infrequent measurement, these studies are unable to describe more closely the dynamics of symptom change in the gap between two occasions that were decades apart.
The absence of a design that both assesses longer-term outcomes and includes more frequent measurement occasions leaves much about the long-term PTSD symptom course poorly understood. Most long-term studies identified predictors of diagnostic status or severity at a single follow-up occasion (e.g., Koenen et al., 2003; Steenkamp et al., 2017). Due to limited assessment occasions, these studies are unable to provide insights into the association between predictors and symptom change over time. Conversely, shorter-term studies of predictors of PTSD diagnosis or symptom severity with more frequent observations can provide insight into predictors of early symptom course, but are unable to determine if these factors predict long-term symptom course.
Shorter-term studies have identified numerous predictors of adverse symptom course, including cumulative trauma exposure, exposure to specific traumatic events (e.g., combat, childhood abuse), comorbid psychopathology, lower social support, and racial minority status (Bonanno et al., 2012; Eekhout et al., 2016; Karstoft et al., 2013; Mota et al., 2019; Orcutt et al., 2004; Vasterling et al., 2016). Some of these predictors are related to PTSD at follow-up in the existing long-term studies, including trauma exposure, lower social support, and racial minority status (e.g., Koenen et al., 2003; Steenkamp et al., 2017). However, how well these factors predict early symptom course, later symptom course, or both, remains unknown. Further, most research on predictors has only examined how well these predictors measured at one time point predict later PTSD symptoms, prohibiting more complex examinations of how variation in predictors over time relates to variation in PTSD symptoms over time. Finally, despite an abundance of research on PTSD symptom course among veterans, perhaps one of the least understood areas of this work is differences in symptom course between male and female veterans, on account of insufficient numbers of female veterans included in prior study samples. This omission represents a major limitation of prior work, particularly considering the recently increased role of women in combat (Hoge, Clark, & Castro, 2007).
Accelerated longitudinal designs offer one solution to address the challenge of observing participants over a longer time period since trauma exposure using more frequent measurement occasions. Whereas longitudinal investigations typically have followed participants across time uniformly since trauma exposure, an alternative method is to examine PTSD symptom course among participants who vary in time since trauma exposure. For example, within an accelerated longitudinal design with a 5-year follow-up, at baseline, participants would vary in their time since trauma exposure. Participants who experienced an index trauma within the past year at baseline will be observed from Years 1 to 5 following trauma exposure; their data would contribute to estimation of PTSD symptom course shortly following trauma exposure. Other participants who identified an index event 10 years ago will be observed in Years 11 to 15 following trauma exposure, thus contributing to our estimation of longer-term PTSD symptom course. Together, these individual trajectories allow us to extrapolate what PTSD symptoms would look like over a lengthier span of time than the observational period of the study. Adjusting for baseline age (i.e., age at index trauma) allows us to estimate within-person change in PTSD trajectory independently from between-person differences in age at trauma exposure (Sliwinski, Hoffman, & Hofer, 2010). This approach is commonly used in developmental studies to capture developmental phenomena occurring over decades (e.g., cognitive change from age 50 to 85 without collecting data for 35 years; Schaie, 1965, 2005). Growth curve models are appropriate to examine to what degree individual trajectories converge onto the average curve, as well as predictors of trajectory parameters (e.g., intercepts and slope; McArdle & Bell, 2000). Such an approach has the potential to generate unique understanding of long-term PTSD symptom course, and predictors thereof.
The Veterans After-discharge Longitudinal Registry (Project VALOR; Rosen et al., 2012), one of the largest longitudinal studies of mental health symptoms among OEF/OIF veterans to date, was designed as a longitudinal nationwide registry of Army and Marine Corps veterans who deployed in support of OEF/OIF and now receive Veterans Healthcare Administration (VHA) services. In contrast to studies of population-based representative samples, Project VALOR over-sampled for PTSD and female veterans so that heterogeneity of PTSD symptom course and the effect of sex on PTSD symptom course could be adequately explored. Project VALOR is, therefore, the ideal sample to investigate the long-term symptom course of PTSD among veterans receiving VHA services. Importantly, participants in this study varied in time since trauma exposure. We used the aforementioned time-coding approach with Project VALOR data to estimate long-term PTSD symptom course, and predictors thereof, among veterans enrolled in VHA care.
Methods
Participants and Procedure
We recruited veterans throughout the United States who had undergone a mental health evaluation at a VHA facility and sampled veterans with and without probable PTSD (defined as a medical record PTSD diagnosis by a mental health professional during two separate visits) on a 3:1 ratio, and male and female veterans on a 1:1 ratio. We administered self-report questionnaires online or by mail when requested. Participants completed the second (T2), third (T3), and fourth (T4) assessments a mean of 2.47 years (SD = 0.52), 3.47 years (SD = 0.54), and 4.64 years (SD = 0.50) following the initial assessment (T1). All study procedures were approved by the VA Boston Healthcare System Institutional Review Board and the Human Research Protection Office of the US Army Medical Research and Materiel Command (IRB protocol #2739: “Project VALOR: Trajectories of Change in PTSD in Combat-Exposed Veterans”).
Of the 4,331 potential participants identified by the Department of Veterans Affairs (VA) Environmental Epidemiology Service and contacted by phone, 2,712 (62.62%) consented to participate, 2,169 (50.08%) completed the questionnaires, and 1,649 (38.07%) completed both the questionnaires and the diagnostic interview. The only potential exclusion criterion was elevated suicide risk at the first assessment, operationalized as a score of ≥ 17 on the Mini-International Neuropsychiatric Interview (Sheehan et al., 1997) suicide module. Of the 1,649 participants who completed the initial assessment, 151 (9.16%) met this criterion; we determined participation was contraindicated for 42 of these participants based on contact with participants’ treatment providers and they were excluded from follow-up assessment. We treated follow-up data for these participants as missing.
Of the 1,649 participants who completed the initial assessment, valid time since index trauma was available for 1,483 (88.33%). An additional 81 participants were missing PTSD symptom scores at all assessment points and were excluded. Of the remaining 1,402 participants, 36 participants identified index traumatic events that occurred more than 20 years prior to the first assessment and 13 would have all follow-up assessment points beyond 20 years. Given the limited number of observations available to estimate symptom course beyond 20 years, we excluded these 49 participants. We conducted analyses using the remaining 1,353 participants. An additional 49 participants identified an index trauma that occurred prior to deployment; we excluded these participants from analyses involving deployment-related predictors of symptom course (e.g., combat exposure). We describe this subsample as the deployment-related sample (n = 1,304).
Time since index trauma ranged from within the past year (coded as 0.5) to 18 years ago (M = 5.95, SD = 2.24). We provide additional sample demographic information in Supplemental Table 1 and details regarding sample trauma exposure in Supplemental Table 2. Most participants identified an index event that occurred during deployment. Some participants served in conflicts prior to OEF/OIF and identified index events that occurred during these earlier deployments (e.g., Gulf War, Haiti, Panama).
Measures
We assessed age, sex, race, ethnicity, education level, marital status, military service branch, and number of deployments with a demographic questionnaire at T1. We collected electronic medical record information regarding VA service-connected PTSD disability status (receiving benefits, compensation, or both vs. not) at T1 for all participants. Additionally, the questionnaire included the question “Did you request medical treatment or counseling during your time of active duty or after your discharge for any emotional problems, including sleep difficulties, “flashbacks,” or other emotional problems?” at T1 and “Are you currently receiving mental health treatment either through VA or in the community?” at T2–T4.
We assessed PTSD symptom severity using the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV; American Psychiatric Association, [APA] 2000) correspondent PTSD Checklist, Civilian version (PCL-C; Weathers, Litz, Herman, Huska, & Keane, 1993) at T1 and again at T4 to compare with the DSM-5 edition (PCL-5; Weathers et al., 2013), which was administered at T2–T4, reflecting the publication of the DSM-5 (APA, 2013). The PCL-C and PCL-5 are 17-item and 20-item, respectively, self-report measures of PTSD symptom severity reported during the past month time window. Psychometric evidence for both measures is strong, including test-retest reliability, internal consistency, construct validity, and diagnostic utility relative to structured diagnostic interviews (Bovin et al., 2016; Weathers et al., 1993; Wilkins, Lang, & Norman, 2011). The PCL-C (α = .95) at T1 and PCL-5 (α = .96 at T2, T3, and T4) both demonstrated excellent internal consistency. To examine PTSD symptoms across occasions on a common metric, T1 PCL-C scores (range = 17–85) were rescaled to estimated PCL-5 scores (range = 0–80). To evaluate the degree to which this score reflected actual PCL-5 scores, this estimated score was calculated using the PCL-C at T4 and correlated with PCL-5 scores at that time point. Estimated PCL-5 scores were highly correlated with actual PCL-5 scores (r = .924, p < .001). PCL-5 scores ≥ 33 are indicative of a provisional diagnosis (Bovin et al., 2016). Responses to the PCL were not specifically linked to the index trauma. Instructions at all four time points read “Below is a list of problems and complaints that people sometimes have in response to stressful life experiences. Please read each one carefully, then circle one of the numbers to the right to indicate how much you have been bothered by that problem in the past month.”
We measured trauma exposure using several approaches. First, we identified the index trauma using the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1995) PTSD module. Specifically, we asked participants to identify the event that affected them most. Second, we assessed lifetime trauma exposure using the Life Events Checklist (LEC; Gray, Litz, Hsu, & Lombardo, 2004) at T1. Additionally, we summed the number of categories of traumatic events participants reported direct exposure to as a proxy variable for cumulative trauma exposure. The LEC has been validated relative to other validated self-report measures of trauma history and exhibited adequate test-retest reliability (Gray et al., 2004).
Third, we measured combat exposure and battle aftermath experiences at T1 using the respective scales of the Deployment Risk and Resilience Inventory (DRRI; King, King, Vogt, Knight, & Samper, 2006). The combat exposure scale is a measure of exposure to a variety of combat-related experiences. The battle aftermath scale measures exposure to consequences of combat (e.g., handling human remains). The DRRI scales were validated relative to other measures of psychiatric symptoms by comparing scores between key groups (e.g., combat and battle aftermath experience score differences between combat-arms versus service-support military personnel; King et al., 2006; Vogt, Proctor, King, King, & Vasterling, 2008). The combat exposure (α = .91) and aftermath of battle experiences (α = .92) scales both demonstrated excellent internal consistency.
Fourth, we extracted results of the VA military sexual trauma (MST) screen at T1 from participants’ electronic medical records to determine MST status. We coded veterans as screening positive for MST if they endorsed “uninvited and unwanted sexual attention, such as touching, cornering, pressure for sexual favors, or verbal remarks,” “force or threat of force to have sexual contact,” or both. This screening measure has been subjected to limited psychometric evaluation. However, Kimerling and colleagues (2007) found that veterans who screened positive for MST on this measure were at significantly higher risk for psychiatric diagnoses (e.g., PTSD, alcohol use disorder) and numerous physical health conditions (e.g., chronic pulmonary disease).
Finally, we measured childhood trauma using the Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998) administered at T3. This 28-item self-report questionnaire assesses exposure to several categories of adverse childhood experiences; we only included the childhood physical and sexual abuse scales in analyses. Respondents rate degree of exposure to each of these forms of abuse on a 5-item scale ranging from never to very often. The CTQ was validated against structured interview measures of childhood abuse in multiple samples (Bernstein et al., 1994; Bernstein, Ahluvalia, Pogge, & Handelsman, 1997). The physical (α = .83) and sexual abuse (α = .95) subscales both demonstrated adequate internal consistency.
We assessed peritraumatic emotional responding using the Measure of Emotional Responses to Trauma (MERT; Bovin et al., 2012; Engel-Rebitzer, Bovin, Black, Rosen, Keane, & Marx, 2017) administered at T1. Participants reported all the emotions they experienced “during or immediately after (within 1 week) the trauma.” Responses were coded as binary (yes or no). For this study, peritraumatic fear, helplessness, horror, surprise, and numbness were included in analyses. There are currently no published reliability or validity data for the MERT.
We assessed traumatic brain injury (TBI) history using a structured interview based on recognized classification standards (Kay et al., 1993; see Wisco et al., 2014 for a detailed description) administered at T1. Probable TBI and moderate to severe TBI classification details are described in Wisco et al. (2014). Interrater agreement for TBI classification was high (κ = .97; see Wisco et al., 2014). This brief screening measure was developed for this study; there are currently no published validity data for this measure.
We assessed post-deployment social support using the respective DRRI scale at T1. The 15-item post-deployment social support scale measures perceived emotional and instrumental assistance from numerous sources (e.g., family, friends, community members). This scale demonstrated adequate internal consistency (α = .86).
We measured unipolar depressive symptoms using the 9-item Prime-MD Patient Health Questionnaire (PHQ-9; Spitzer et al., 1999) at each time point. The PHQ-9 has relatively strong psychometric support, including internal consistency, responsiveness to intervention, diagnostic utility relative to structured diagnostic interviews, and construct validity (e.g., Beard, Hsu, Rifkin, Busch, & Björgvinsson, 2016; Cannon et al., 2007; Kroenke, Spitzer, & Williams, 2001; Löwe, Kroenke, Herzog, & Gräfe, 2004; Titov, Dear, McMillan, Anderson, Zou, & Sunderland, 2011). The PHQ-9 demonstrated excellent internal consistency at all time points (α ranged from .88–.92). We measured suicidal ideation (SI) using item nine of this measure, which asks respondents to report how often they experienced “thoughts that you would be better off dead, or of hurting yourself.” At each time point, over 20% of the sample reported experiencing SI during the past two weeks.
We measured alcohol use disorder symptoms using the Alcohol Use Disorder Identification Test (AUDIT; Saunders, Aasland, Babor, Fuente, & Grant, 1993) at each time point. The psychometric properties of the AUDIT support its diagnostic utility relative to structured diagnostic interviews, internal consistency, predictive validity, and construct validity (see Allen, Litten, Fertig, & Babor, 1997 for a review). The AUDIT demonstrated adequate internal consistency at all time points (α ranged from .86 – .89).
Data Analytic Strategy
We first inspected raw data of individual PTSD symptom trajectories plotted over time since index trauma. We used growth curve modeling to estimate PTSD symptom course with time coded as years since index trauma and allowed to vary across participants. To identify the model that most appropriately fit the data, we compared intercept only, intercept plus linear slope, and intercept plus linear and quadratic slopes models with and without random effects. Based on visual inspection of raw data, we did not further consider spline or higher-order polynomial models of change. We examined model fit using Akaike’s information criterion (AIC; Akaike, 1974) and Bayes information criterion (BIC; Schwarz, 1978); nested models were compared using likelihood ratio test. We examined growth curve models separately for the full sample, deployment trauma subsample, and for participants with symptoms 0–10 and 10–20 years following trauma exposure. Due to a small number of participants reporting symptoms ≥ 10 years post-trauma at T1, we only used time points T2–T4 for analyses examining symptom course 10–20 years post-trauma. Accordingly, we did not examine a quadratic slope for this model.
Once we identified a best fitting model of PTSD symptom trajectories over time since trauma, we evaluated time invariant and time varying covariates. Supplemental Table 3 provides descriptive data for covariates. We examined covariates in separate models initially due to concerns regarding multicollinearity among predictors, then in multivariable models. We examined age at the time of index trauma occurrence, sex, race, and ethnicity as demographic predictors of symptom course for all participants. We only examined deployment experiences (e.g., combat exposure, aftermath of battle experiences) as predictors for participants who identified an index trauma that occurred during deployment. We tested depression, SI, alcohol abuse, and treatment engagement as time varying covariates of PTSD symptom course. We adjusted all analyses for age at index trauma occurrence.
We handled all missing data using multiple imputation. Consistent with established guidelines (Bodner, 2008), we used 114 imputed datasets. With the exception of the PCL at T1, data were missing for no more than 29% of participants. Due to an oversight, the first 698 participants (42.33%) did not receive the PCL at T1. We conducted all analyses using Mplus version 7 (Muthén & Muthén, 2017).
Results
Sample Trauma Characteristics
Participants reported experiencing a wide range of traumatic experiences and identified index traumatic events that occurred before, during, and after deployment (see Supplemental Table 2). Combat represented the index trauma for most participants (86.10%). Over 18% of the total sample reported MST. Strikingly, among participants who identified sexual assault as their index trauma, the majority (57.69%) reported an assault that occurred during deployment.
Unconditional Models
An intercept plus linear and quadratic slopes model with random effects provided the best fit for the full sample and deployment trauma subsample (see Supplemental Table 4). As shown in Table 1, in both the full sample and the deployment trauma subsample, estimates of the intercept and slope variance components indicated substantial individual differences in both initial levels of PTSD at the time of index trauma and in how PTSD symptoms change over time (see Figure 1). On average, at the time of trauma exposure, veterans experienced PTSD symptoms corresponding to a PCL-5 score of 46.70 (SE = 1.92). The positive linear slope was not significant, indicating mean symptom severity did not initially change. The significant quadratic term indicated that symptoms eventually decreased (quadratic slope = −0.08; SE = 0.02). Results for the deployment-related trauma subsample were similar. Age at index trauma was not significantly associated with initial symptom severity nor symptom change over time in either model, suggesting no mean difference in PTSD trajectory between veterans who were older vs. younger at the time of their index traumas.
Table 1.
Unstandardized Parameter Estimates (and Standard Errors) for Growth Curve Models.
| Parameter | Full Sample (N = 1,353) | Deployment Trauma Subsample (n = 1,304) | Years 1–10 Dep. Trauma (n = 1,290) | Years 10–20 Dep. Trauma (n = 672) |
|---|---|---|---|---|
| Means/Intercepts | ||||
| Intercept | 46.70 (1.92)* | 45.93 (2.26)* | 43.77 (2.43)* | 55.44 (3.81)* |
| Linear Slope | 0.16 (0.40) | 0.41 (0.49) | 1.10 (0.61) | −1.43 (0.39)* |
| Quadratic Slope | −0.08 (0.02)* | −0.09 (0.03)* | −0.15 (0.04)* | - |
| Covariances | ||||
| Intercept - Linear Slope | −29.00 (7.42)* | −21.47 (8.32)* | −11.52 (9.93) | −61.92 (29.57)* |
| Intercept - Quadratic Slope | −0.51 (0.25)* | −0.84 (0.33)* | −0.92 (0.52) | - |
| Linear Slope - Quadratic Slope | −0.38 (0.06)* | −0.40 (0.09)* | −0.24 (0.14) | - |
| Residual Variances | ||||
| Intercept | 372.58 (46.82)* | 323.66 (47.58)* | 297.94 (52.62)* | 925.27 (307.50)* |
| Linear Slope | 12.10 (1.57)* | 11.58 (2.05)* | 7.41 (2.70)* | 6.12 (2.89)* |
| Quadratic Slope | 0.02 (<0.01)* | 0.03 (0.01)* | 0.02 (0.01) | - |
| PCL (equated) | 82.80 (3.24)* | 83.18 (3.31)* | 94.44 (4.32)* | 85.27 (5.58)* |
| Age at Index Trauma | ||||
| Intercept | −0.28 (0.15) | −0.30 (0.16) | −0.45 (0.17)* | −0.54 (0.23)* |
| Linear Slope | 0.02 (0.03) | 0.02 (0.04) | 0.10 (0.04)* | 0.05 (0.02)* |
| Quadratic Slope | <0.01 (<0.01) | <0.01 (<0.01) | −0.01 (<0.01)* | - |
Note.
p < .05; PCL = PTSD Checklist.
Figure 1.
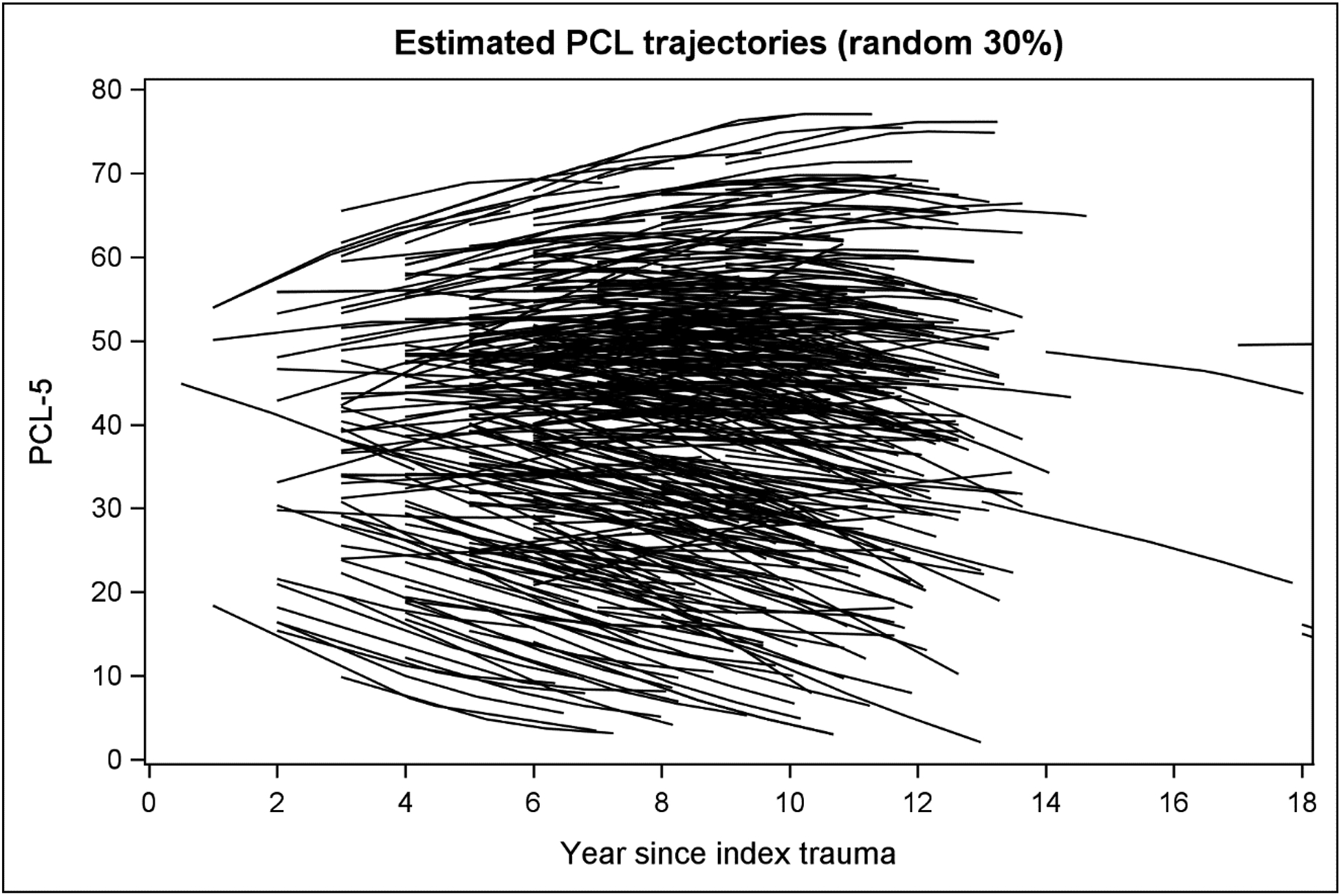
Estimated trajectories from the 20-year course of posttraumatic stress disorder symptoms among veterans.
Time Invariant Covariates
We examined a series of univariate models to examine the association of each covariate to age-adjusted PCL intercepts and slopes in separate models. As shown in Supplemental Table 5, among the full sample, Hispanic ethnicity and greater education were associated with lower initial levels of PTSD symptom severity (i.e., at the time of trauma exposure); TBI, greater cumulative trauma exposure, childhood sexual abuse, and peritraumatic helplessness, horror, and numbing were each associated with worse initial levels of PTSD symptom severity. Only ethnicity was significantly associated with symptom change; Hispanic ethnicity was associated with greater initial symptom increase over time. Among the deployment-trauma subsample, Hispanic ethnicity and greater post-deployment social support were associated with lower initial levels of PTSD symptom severity; greater combat exposure, battle aftermath experiences, greater cumulative trauma, childhood physical and sexual abuse, and peritraumatic helplessness, horror, and numbing were each associated with worse initial levels of PTSD symptom severity. As with the full sample, Hispanic ethnicity was associated with greater initial symptom increase over time.
Next, we carried forward significant covariates from the univariate models into multivariable models, which we examined in three steps (Supplemental Table 6). Model 1 included demographic factors only. Age was not associated with initial symptom severity or symptom change over time; Hispanic ethnicity was associated with lower initial levels of PTSD symptom severity and greater initial symptom increase over time. Model 2 retained these demographic features and added significant trauma characteristics. In this model, Hispanic ethnicity and greater post-deployment social support were associated with lower initial levels of PTSD symptom severity; peritraumatic horror was associated with worse initial symptom severity; Hispanic ethnicity was associated with greater initial symptom increase over time. In Model 3, we retained only the significant covariates in Model 2. In this trimmed model, we observed the same pattern of associations between the covariates and the growth parameters as Model 2. Of note, compared with the age-adjusted model, this model further accounted for 48.12% of the individual differences in initial levels of PTSD (i.e., intercept variance changed from 372.58 to 193.31) and 4.05% of the individual differences in linear PTSD change (i.e., linear slope variance was reduced from 12.10 to 11.61).
Figure 2 displays the effects of these predictors on PTSD symptom course. Relative to non-Hispanic veterans, Hispanic veterans appear to experience a curvilinear pattern of symptom course characterized by lower initial PTSD symptom severity, a greater initial increase in symptom severity, and greater plateau and decrease long after trauma exposure. As displayed in Figure 2, the protective effect of social support on initial symptom severity does not deteriorate for decades following trauma exposure. Lastly, veterans who reported experiencing peritraumatic horror experienced worse initial symptom severity but eventually experienced symptoms comparable with those who did not experience peritraumatic horror.
Figure 2.
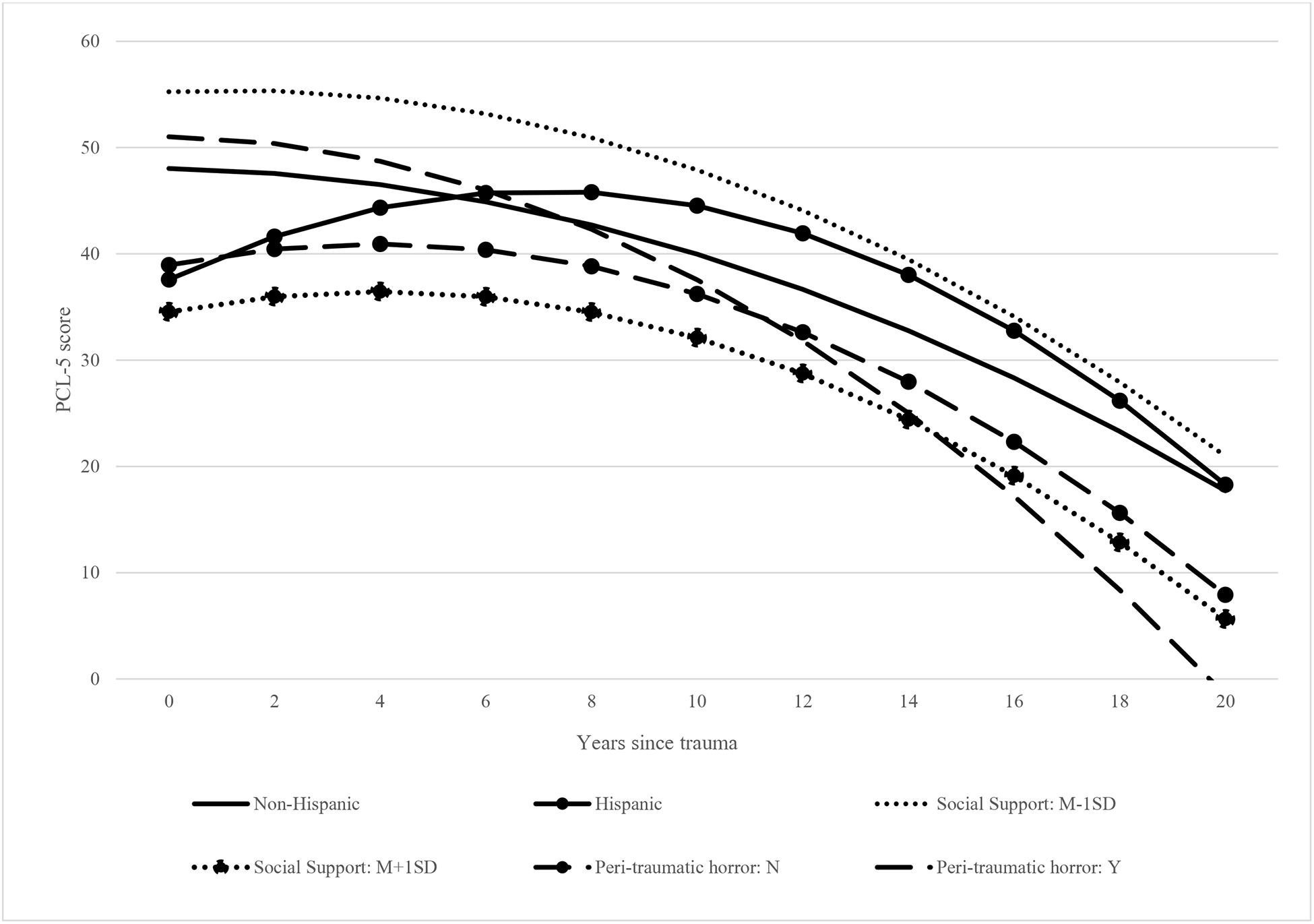
The 20-year course of posttraumatic stress disorder symptoms among veterans by social support and Hispanic ethnicity.
Time Varying Covariates
We examined depression, SI, and alcohol abuse as time varying covariates of PTSD symptoms. In the age-adjusted latent growth curve model of PTSD symptoms, we further regressed PTSD symptoms at each occasion on a covariate assessed concurrently and at the prior occasion. The within-time regression coefficient represents the coupling of the covariate with PTSD symptom, after accounting for one’s expected PTSD trajectory over time and prior status on the covariate. For example, the lagged regression coefficient represents the influence of prior depression on current PTSD symptoms, after accounting for current status on depression and one’s expected PTSD trajectory over time. Depression, SI, and alcohol abuse were each significantly associated with PTSD symptoms over time (see Supplemental Table 7), indicating changes in PTSD symptoms over time were associated with changes in these constructs. Additionally, significant lagged effects were observed for depression and SI at all time points, and for alcohol abuse at T2, indicating veterans with greater depression, SI, and alcohol abuse had worse subsequent PTSD symptoms, even after accounting for one’s current status on these factors. Additionally, psychological treatment at each time point and VA service-connected disability for PTSD at T1 were each significantly associated with greater PTSD symptom severity at each time point.
Early vs. Later Symptom Course
Finally, we partitioned the data such that participants whose symptoms were measured during the first 10 years after trauma exposure (n = 1,290) and those whose symptoms were measured 10–20 years after trauma exposure (n = 709) were examined separately. An intercept plus linear and quadratic slopes model with random effects provided the best fit for the 0–10 year symptom course analyses (see Supplemental Table 4). As a quadratic slope was not considered for the 10–20 year analyses, an intercept plus linear slope model with random effects provided the best fit. As with the full sample, results indicate, on average, veterans experienced initial PTSD symptom severity well above the diagnostic threshold which did not initially change but eventually decreased in years 0–10 following trauma exposure. Among the 10–20 year subsample, veterans experienced PTSD symptom severity well above the diagnostic threshold 10 years following trauma exposure which decreased 10–20 years after trauma occurrence.
We examined the same multivariable models from the full and deployment-trauma sample in each group (see Table 2). In years 0–10 following trauma exposure, the first model examining demographic predictors revealed that older age at the time of trauma exposure was associated with a greater initial symptom increase but also greater plateau and eventual decrease. In the second model, older age at the time of trauma occurrence and greater post-deployment social support were associated with lower initial symptom severity; childhood sexual abuse was associated with worse initial symptom severity. Finally, in the third model older age at the time of the index trauma and greater post-deployment social support were associated with lower initial symptom severity; peritraumatic horror was associated with worse initial symptom severity. Additionally, older age at the time of the index trauma was associated with a greater initial symptom increase and greater plateau in symptom increase over time.
Table 2.
Unstandardized Parameter Estimates (and Standard Errors) of Predictors in Multivariable Growth Curve Models among Deployment-Trauma Subsample during the First- and Second-Decades Following Trauma Exposure.
| 0–10 Years Following Trauma (n = 1,290) | 10–20 Years Following Trauma (n = 709) | ||||
|---|---|---|---|---|---|
| Model and Predictors | Intercept | Linear Slope | Quadratic Slope | Intercept | Linear Slope |
| Model 1: Demographics | |||||
| Age at Index Trauma | −0.43 (0.17) | 0.09 (0.04)* | −0.01 (<0.01)* | −0.55 (0.23)* | 0.06 (0.02)* |
| Hispanic Ethnicity | −2.80 (4.72) | 0.13 (1.16) | 0.08 (0.07) | −11.85 (7.06) | 1.40 (0.72) |
| Model 2: Demographics and Trauma Characteristics | |||||
| Age at Index Trauma | −0.36 (0.16)* | 0.08 (0.04) | −0.01 (<0.01) | −0.49 (0.22)* | 0.05 (0.02)* |
| Hispanic Ethnicity | −3.19 (4.37) | 0.21 (1.14) | 0.07 (0.08) | −11.46 (6.80) | 1.30 (0.69) |
| Combat | 0.33 (0.22) | −0.03 (0.06) | <0.01 (<0.01) | 0.14 (0.38) | <0.01 (0.04) |
| Battle Aftermath | 0.24 (0.20) | −0.01 (0.05) | <0.01 (<0.01) | 0.39 (0.30) | −0.03 (0.03) |
| Post-Deployment Social Support | −0.67 (0.14)* | 0.01 (0.04) | <0.01 (<0.01) | −0.36 (0.22) | −0.02 (0.02) |
| Trauma Categories | 0.55 (0.62) | −0.03 (0.16) | <0.01 (0.01) | 0.65 (1.11) | −0.03 (0.11) |
| Childhood Physical Abuse | −0.06 (0.41) | 0.10 (0.10) | −0.01 (0.01) | 0.48 (0.66) | −0.03 (0.07) |
| Childhood Sexual Abuse | 0.74 (0.32)* | −0.07 (0.08) | <0.01 (0.01) | 1.08 (0.58) | −0.08 (0.06) |
| Peritraumatic Helplessness | 6.41 (3.76) | −1.59 (0.98) | 0.14 (0.06)* | 3.36 (6.04) | −0.08 (0.61) |
| Peritraumatic Horror | 5.30 (3.45) | 0.42 (0.91) | −0.07 (0.06) | −3.59 (4.23) | 0.72 (0.43) |
| Peritraumatic Numbing | 6.75 (3.55) | −0.81 (0.87) | 0.05 (0.06) | 4.57 (5.46) | −0.15 (0.52) |
| Model 3: Trimmed Model | |||||
| Age at Index Trauma | −0.36 (0.16)* | 0.08 (0.04)* | −0.01 (<0.01)* | −0.51 (0.23)* | 0.05 (0.02)* |
| Hispanic Ethnicity | −3.54 (4.38) | 0.29 (1.10) | 0.07 (0.07) | −11.77 (6.82) | 1.35 (0.69) |
| Post-Deployment Social Support | −0.84 (0.13)* | 0.02 (0.03) | <0.01 (<0.01) | −0.56 (0.20)* | −0.01 (0.02) |
| Peritraumatic Horror | 9.87 (3.19)* | −0.29 (0.80) | −0.02 (0.05) | −0.19 (4.23) | 0.57 (0.43) |
Note.
= p < .05.
We repeated these analyses for the 10–20 year subsample. Older age at the time of index trauma occurrence was associated with lower symptom severity 10 years after the index trauma but was also associated with less symptom reduction during the 10–20 year period. In the model examining demographic and trauma characteristics, only the significant effects of age at the time of index trauma occurrence from the previous model emerged as significant. In the final trimmed model, older age at the time of index trauma occurrence and greater post-deployment social support were associated with lower symptom severity 10 years after the index trauma; only age at the time of index trauma occurrence was associated with slope 10–20 years post-trauma.
Discussion
By accounting for between-person differences in time since trauma exposure in a sample ranging widely in time since their index trauma, we were able to estimate the 20-year course of PTSD symptoms using frequent measurement occasions. Results indicate PTSD symptoms are most appropriately characterized by substantial heterogeneity in both initial severity and change over time. This result highlights the considerable variability in symptom course among the veteran population.
On average, veterans experienced initial PTSD symptom severity above the diagnostic threshold following trauma exposure, which was initially stable over time, then later began to gradually improve. We observed a similar pattern among the subsample of veterans who identified an index trauma that occurred during deployment. Although results from this study indicate symptoms eventually begin to improve, this effect was gradual; most participants continued to meet or exceed the PTSD symptom severity diagnostic threshold long after trauma exposure. This result is consistent with longitudinal research of symptom course among Vietnam veterans (e.g., Marmar et al., 2015) in characterizing PTSD as a relatively chronic disorder among veterans. This result is particularly concerning given that all participants were enrolled in VHA care and the majority reported some engagement in mental health treatment during study participation. Given the adverse interpersonal, occupational, health, and safety outcomes associated with chronic PTSD (e.g., cardiovascular diseases, respiratory diseases, accelerated aging, early mortality, suicide; Boscarino, 2008; Bullman & Kang, 1994), these results highlight the urgent need to improve the mental healthcare provided to veterans diagnosed with the disorder. In particular, greater efforts are needed to provide effective evidence-based interventions to those in need, determine what treatments are most appropriate for specific types of patients with PTSD, develop additional effective interventions, improve access to and delivery of treatment across public and private settings, promote earlier detection, and focus on prevention among those at greatest risk for developing PTSD.
The observed quadratic shape of average symptom course indicates symptoms began to improve for veterans long after trauma exposure. These results suggest that the years following trauma exposure appear to be a period of symptom stability over time, but that this chronicity begins to fade further after trauma exposure. This effect was only observable due to the analytic approach used in this study to build an estimate of long-term symptom course from individually varying time since trauma estimates; these results highlight the potential value of this approach for longitudinal symptom course research.
The strongest observed predictors of symptom course were the included time varying covariates depression, SI, and alcohol abuse. These results highlight the value of these constructs as intervention targets, particularly among veterans unwilling to engage in evidence-based trauma-focused therapy. The observed lagged effects suggest unresolved comorbid symptoms have a deleterious effect on subsequent PTSD symptom course. This is consistent with recent findings supporting antidepressant medications for PTSD treatment (Rauch et al., 2019). Given that SI is often conceptualized as secondary to PTSD symptoms, and that effective PTSD treatments reduce SI (e.g., Gradus, Suvak, Wisco, Marx, & Resick, 2013), the observed lagged effects of SI on subsequent PTSD symptoms were somewhat surprising. However, these results suggest that, beyond establishing patient safety, reducing SI could have beneficial impact on PTSD symptom severity. The deleterious effect of alcohol abuse on symptom course is consistent with replicated findings among veterans of previous conflicts (e.g., Keane & Wolfe, 1990). This result is particularly disconcerting given the observed high prevalence of alcohol abuse among OEF/OIF veterans (Thomas et al., 2010). Our results support the concurrent treatment of alcohol abuse and PTSD (e.g., Back et al., 2019; Brief et al., 2013).
Although several time invariant covariates predicted initial symptom severity, few predicted symptom course. Much effort has been undertaken to understand previous findings regarding differences in symptom course for Hispanic veterans (e.g., Kulka et al., 1988). Our results suggest the long-term symptom course is curvilinear in nature among Hispanic veterans. We plan to examine differences between Hispanic and non-Hispanic veterans in deployment- and trauma-experiences, as well as service utilization within VA using these data in future projects.
The adverse impact of trauma exposure at a younger age is well-established (Brewin, Andrews, & Valentine, 2000). The result that veterans who were younger at the time of trauma exposure experienced worse PTSD symptom severity 10 years following trauma exposure is particularly noteworthy given these analyses were conducted among participants who identified a trauma that occurred during deployment (i.e., these exclude childhood trauma). Accordingly, these results indicate younger service members who experience trauma during deployment appear at greater risk for PTSD symptoms long after trauma exposure.
The protective effect of post-deployment social support on symptom course is consistent with replicated findings among veterans of previous conflicts (e.g., Keane, Scott, Chavoya, Lamparski, & Fairbank, 1985). Interventions for PTSD that target improvement in social connectedness as a component of recovery, including cognitive-behavioral conjoint therapy for PTSD (Monson, Fredman, & Adair, 2008) and interpersonal psychotherapy for PTSD (Bleiberg & Markowitz, 2005), support the potential of social connectedness as an intervention target. Results from this study suggest this remains an intervention target worthy of further effort.
Although MST, as defined by the VA screener (i.e., “uninvited and unwanted sexual attention,” “force or threat of force to have sexual contact,” or both) did not predict symptom course, one related finding warrants discussion. The result that, among participants who identified sexual assault as their index trauma, the majority (57.69%) reported an assault that occurred during deployment is troubling. This remarkable statistic indicates deployment is a particularly vulnerable period for MST and highlights the critical need for greater efforts to reduce MST within the military, particularly during deployment.
Perhaps the most notable null finding is the effect of sex on symptom course. Our results indicate male and female veterans did not differ in initial symptom severity or symptom change over time. These results are noteworthy given the over-sampling for female veterans. This finding contrasts with a well-established literature on the increased risk for PTSD among women (Tolin & Foa, 2006) and suggests that, despite well-documented sex differences in pre-military trauma exposure, deployment experiences, and homecoming readjustment experiences (Street, Gradus, Giasson, Vogt, & Resick, 2013), symptom course did not differ between male and female veterans. It is worth noting that this finding is consistent with other work, including among nationally representative samples, indicating that female OEF/OIF veterans evidence similar rates of resilience to male veterans (Vogt et al., 2011). Some have speculated this difference may be attributable to increased levels of direct combat exposure among female OEF/OIF veterans relative to previous conflicts as well as improved training of female service members (Hoge et al., 2007).
Regarding the observed association between service-connected PTSD disability status and symptom course, the most parsimonious explanation is that those with the more severe symptoms are more likely to have greater associated impairment and thus more likely to be receiving compensation and other benefits for their PTSD-related disability. Because we do not have detailed information about the extent and type of PTSD treatment received by participants or response bias, we were unable to examine long-standing concerns that receiving PTSD-related disability compensation and other benefits may disincentivize treatment seeking or acknowledgement of symptom improvement (McNally & Frueh, 2013). Nonetheless, the observed symptom chronicity in this study highlights the urgent need for improved methods for alleviating symptoms in this population.
The finding that veterans with significantly more severe PTSD symptoms were more likely to be engaged in mental health treatment is encouraging in that these individuals are utilizing available care. Although this result could be cause for concern, as those in treatment do not appear to exhibit greater decreases in symptoms over time, this should be interpreted in the context of the very broad measurement of treatment utilization (e.g., individual and group psychotherapy, psychiatry, peer groups). We plan to conduct a more granular examination of what forms of treatment were associated with meaningful gains among study participants.
Although many features of this study are ideal for examining the longitudinal course of PTSD symptoms, others require consideration when interpreting these findings. Project VALOR was designed to oversample for PTSD to examine the heterogeneous nature of symptom course. Accordingly, findings are likely more generalizable to clinical than non-clinical populations. Likewise, the equal recruitment of male and female veterans was designed to provide sufficient power to study sex differences in PTSD symptom course. Therefore, this sample provides ideal conditions for examining PTSD heterogeneity among male and female veterans enrolled in VHA care but is not representative of the general veteran population. Exclusive reliance on a retrospective self-report questionnaire, albeit a measure extensively validated relative to structured diagnostic interviews, represents a limitation. Future work using this data set will incorporate multiple sources of data, including electronic medical record and genetic data.
Trauma exposure subsequent to the index trauma was not collected in this study. Although we made efforts to examine numerous aspects of collective trauma exposure (e.g., childhood physical and sexual abuse, cumulative trauma categories endorsed, military sexual trauma), we were unable to examine the impact of trauma exposure between assessment occasions on subsequent symptom course. An important future direction for this line of research will be to quantify the deleterious effects of subsequent trauma exposure on long-term symptom course. Finally, the observed symptom chronicity should be considered in the context of the oversampling for VHA users who exhibit PTSD symptoms. It is possible that participants recruited for the study, by definition, experience more chronic symptoms than trauma-exposed veterans not enrolled in VHA care. This possibility is supported by evidence that veterans enrolled in VHA care tend to have lower income, less education, and are less likely to be employed than those veterans not enrolled in VA care (e.g., Agha, Lofgren, VanRuiswyk, & Layde, 2000). Accordingly, an important future avenue of research is to examine differences in PTSD symptom course between veterans who do an do not utilize VHA care.
An important caveat to our conclusions worth discussing is that responses to the PCL were not specifically linked to the index trauma identified in the SCID. Participants could have completed the SCID in reference to one traumatic event and the PCL in reference to another, or PCLs at different time points in reference to different events. Another approach to measuring PTSD symptom severity over time is to measure trauma exposure between each interval and link symptoms to the most distressing at each time point; the index trauma would vary for some participants but not others. That approach potentially provides conceptual clarity of the link between symptoms and specific events. However, the relation between trauma exposure and symptom onset and course, both in research and clinical practice, is rarely straightforward for two reasons. First, selection of the index trauma is a challenging and often nebulous process for both respondents and assessors. This is particularly true for many veterans and servicemembers who often experience a series of traumatic events in close temporal proximity (e.g., multiple combat experiences during a deployment) or in multiple phases of life (e.g., during childhood, military service, and after discharge). Sometimes these multiple traumatic stressors are categorically similar (e.g., multiple combat-related traumas) but sometimes they are categorically dissimilar (e.g., combat-related, motor vehicle accident, sexual assault by an acquaintance) during one military deployment. Teasing the sequelae to one trauma from another when someone has numerous traumatic exposures either in a brief period of time or even over a lifetime can be difficult. Second, and related to the first point, most current assessment approaches rely on the assumption that participants can accurately attribute symptoms to a specific event. However, this remains a relatively untested assumption. The limited work examining this assumption suggests that individuals have difficulty distinguishing symptoms related to different events, even when some events do not meet the definition of Criterion A (Long et al., 2008), and assessment of symptoms in relation to multiple events produces highly similar results to assessment of symptoms in relation to a single index trauma (Kilpatrick et al., 2013). Collectively, these issues represent serious, ongoing challenges to the study of trauma exposure and PTSD, in general. None of these points offsets the limitation that responses to the PCL were not specifically linked to the index trauma identified in the SCID. However, results should be interpreted within the context of study methodology choices and within the challenges that have faced trauma researchers for decades.
This study presents one of the largest prospective studies of mental health symptoms among OEF/OIF veterans receiving VHA services and is one of only a handful to examine the long-term course of PTSD symptoms. Results highlight the broad array of traumatic events veterans experience before, during, and after deployment, characterize PTSD symptoms as generally stable for many years following trauma exposure, and point toward several important predictors of symptom course. These results shed light on the long-term toll of combat deployments on mental health among veterans and highlight the urgent need for improved methods for alleviating symptoms in this population.
Supplementary Material
Acknowledgments
This work was funded by the US Department of Defense Awards W81XWH-08-2-0102 and W81XWH-08-2-0100. DJL and SJD were supported by National Institute of Mental Health award #5T32MH019836-16; LOL was supported by National Institute on Aging awards K08-AG048221 and RF1-AG064006. We thank the large number of assessors, research assistants, and support staff who assisted with data collection.
References
- Able ML, & Benedek DM (in press) Severity and symptom trajectory in combat-related PTSD: A review of the literature. Current Psychiatry Reports. [DOI] [PubMed] [Google Scholar]
- Agha Z, Lofgren RP, VanRuiswyk JV, & Layde PM (2000). Are patients at Veterans Affairs medical centers sicker?: A comparative analysis of health status and medical resource use. Archives of Internal Medicine, 160, 3252–3257. [DOI] [PubMed] [Google Scholar]
- Akaike H (1974). A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19, 716–723. [Google Scholar]
- Allen JP, Litten RZ, Fertig JB, & Babor T (1997). A review of research on the Alcohol Use Disorders Identification Test (AUDIT). Alcoholism: Clinical and Experimental Research, 21, 613–619. [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Back SE, Killeen T, Badour CL, Flanagan JC, Allan NP, Santa Ana EJ, & Brady KT (2019). Concurrent treatment of PTSD and substance use disorders using prolonged exposure: A randomized clinical trial in military veterans. Addictive Behaviors, 90, 369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C, Hsu KJ, Rifkin LS, Busch AB, & Björgvinsson T (2016). Validation of the PHQ-9 in a psychiatric sample. Journal of Affective Disorders, 193, 267–273. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, & Handelsman L (1997). Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 340–348. [DOI] [PubMed] [Google Scholar]
- Bernstein D, & Fink L (1998). Manual for the childhood trauma questionnaire. New York, NY: The Psychological Corporation. [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, … & Ruggiero J (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American Journal of Psychiatry, 151, 1132–1136. [DOI] [PubMed] [Google Scholar]
- Bleiberg KL, & Markowitz JC (2005). A pilot study of interpersonal psychotherapy for posttraumatic stress disorder. American Journal of Psychiatry, 162, 181–183. [DOI] [PubMed] [Google Scholar]
- Bodner Todd E. (2008) What improves with increased missing data imputations? Structural Equation Modeling: A Multidisciplinary Journal, 15, 651–675. [Google Scholar]
- Bonanno GA, Mancini AD, Horton JL, Powell TM, LeardMann CA, Boyko EJ, … & Millennium Cohort Study Team. (2012). Trajectories of trauma symptoms and resilience in deployed US military service members: Prospective cohort study. The British Journal of Psychiatry, 200, 317–323. [DOI] [PubMed] [Google Scholar]
- Boscarino JA (2008). A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: Implications for surveillance and prevention. Psychosomatic Medicine, 70, 668–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Wisco BE, Holowka DW, Marx BP, Gates MA, Guey LT, … Keane TM (2012). Peritraumatic response, PTSD and functional impairment among OEF/OIF veterans In Fetzner(Chair.) MG, On trauma: A theoretical and clinical perspective on how traumatic experiences shape subsequent PTSD. Arlington, Virginia: Symposium conducted at the annual meeting of the Anxiety Disorders Association of America. [Google Scholar]
- Brewin CR, Andrews B, & Valentine JD (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68, 748–766. [DOI] [PubMed] [Google Scholar]
- Brief DJ, Rubin A, Keane TM, Enggasser JL, Roy M, Helmuth E, … & Rosenbloom D (2013). Web intervention for OEF/OIF veterans with problem drinking and PTSD symptoms: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 81, 890–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bullman TA, & Kang HK (1994). Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. Journal of Nervous and Mental Disease, 182], 604–610. [DOI] [PubMed] [Google Scholar]
- Cannon DS, Tiffany ST, Coon H, Scholand MB, McMahon WM, & Leppert MF (2007). The PHQ-9 as a brief assessment of lifetime major depression. Psychological Assessment, 19, 247–251. [DOI] [PubMed] [Google Scholar]
- Eekhout I, Reijnen A, Vermetten E, & Geuze E (2016). Post-traumatic stress symptoms 5 years after military deployment to Afghanistan: An observational cohort study. The Lancet Psychiatry, 3, 58–64. [DOI] [PubMed] [Google Scholar]
- Engel-Rebitzer E, Bovin MJ, Black SK, Rosen RC, Keane TM, & Marx BP (2017). A longitudinal examination of peritraumatic emotional responses and their association with posttraumatic stress disorder and major depressive disorder among veterans. Journal of Trauma & Dissociation, 18, 679–692. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JB (1995). Structured clinical interview for DSM-IV axis I disorders. New York: New York State Psychiatric Institute. [Google Scholar]
- Galatzer-Levy IR, Huang SH, & Bonanno GA (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55. [DOI] [PubMed] [Google Scholar]
- Gradus JL, Suvak MK, Wisco BE, Marx BP, & Resick PA (2013). Treatment of posttraumatic stress disorder reduces suicidal ideation. Depression and Anxiety, 30, 1046–1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the life events checklist. Assessment, 11, 330–341. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, & Milliken CS (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA, 295, 1023–1032. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Clark JC, & Castro CA (2007). Commentary: Women in combat and the risk of post-traumatic stress disorder and depression. International Journal of Epidemiology, 36, 327–329. [DOI] [PubMed] [Google Scholar]
- Karstoft K-I, Armour C, Elklit A, & Solomon Z (2013). Long-term trajectories of posttraumatic stress disorder in veterans: The role of social resources. The Journal of Clinical Psychiatry, 74, 1163–1168. [DOI] [PubMed] [Google Scholar]
- Kay T, Harrington DE, Adams R, Anderson T, Berrol S, Cicerone K, … & Hilt J (1993). Definition of mild traumatic brain injury. Journal of Head Trauma Rehabilitation, 8, 86–87. [Google Scholar]
- Keane TM, Scott WO, Chavoya GA, Lamparski DM, & Fairbank JA (1985). Social support in Vietnam veterans with posttraumatic stress disorder: A comparative analysis. Journal of Consulting and Clinical Psychology, 53, 95–102. [DOI] [PubMed] [Google Scholar]
- Keane TM, & Wolfe J (1990). Comorbidity in Post-Traumatic Stress Disorder: An Analysis of Community and Clinical Studies. Journal of Applied Social Psychology, 20, 1776–1788. [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling R, Gima K, Smith MW, Street A, & Frayne S (2007). The Veterans Health Administration and military sexual trauma. American Journal of Public Health, 97, 2160–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, & Samper RE (2006). Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology, 18, 89–120. [Google Scholar]
- Koenen KC, Stellman JM, Stellman SD, & Sommer JF Jr (2003). Risk factors for course of posttraumatic stress disorder among Vietnam veterans: A 14-year follow-up of American Legionnaires. Journal of Consulting and Clinical Psychology, 71, 980–986. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulka R, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, & Weiss DS (1988). National Vietnam Veterans Readjustment Study (NVVRS): Description, current status, and initial PTSD prevalence estimates. Washington, DC: Veterans Administration. [Google Scholar]
- Long ME, Elhai JD, Schweinle A, Gray MJ, Grubaugh AL, & Frueh BC (2008). Differences in posttraumatic stress disorder diagnostic rates and symptom severity between Criterion A1 and non-Criterion A1 stressors. Journal of Anxiety Disorders, 22, 1255–1263. [DOI] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, Herzog W, & Gräfe K (2004). Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the Patient Health Questionnaire (PHQ-9). Journal of Affective Disorders, 81, 61–66. [DOI] [PubMed] [Google Scholar]
- Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, … Horesh D (2015). Course of posttraumatic stress disorder 40 years after the Vietnam War: Findings from the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry, 72, 875–881. [DOI] [PubMed] [Google Scholar]
- McArdle JJ & Bell RQ (2000). An introduction to latent growth curve models for developmental data analysis In Little TD, Schnabel KU, & Baumert J (Eds.), Modeling Longitudinal and Multiple-Group Data: Practical Issues, Applied Approaches, and Scientific Examples. Mahwah, NJ: Erlbaum [Google Scholar]
- McNally RJ, & Frueh BC (2013). Why are Iraq and Afghanistan War veterans seeking PTSD disability compensation at unprecedented rates?. Journal of Anxiety Disorders, 27, 520–526. [DOI] [PubMed] [Google Scholar]
- Mota NP, Cook JM, Smith NB, Tsai J, Harpaz-Rotem I, Krystal JH, … & Pietrzak RH (2019). Posttraumatic stress symptom courses in US military veterans: A seven-year, nationally representative, prospective cohort study. Journal of Psychiatric Research, 119, 23–31. [DOI] [PubMed] [Google Scholar]
- Monson CM, Fredman SJ, & Adair KC (2008). Cognitive–behavioral conjoint therapy for posttraumatic stress disorder: Application to Operation Enduring and Iraqi Freedom veterans. Journal of Clinical Psychology, 64, 958–971. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2017). Mplus Version 7 user’s guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Orcutt HK, Erickson DJ, & Wolfe J (2004). The course of PTSD symptoms among Gulf War veterans: A growth mixture modeling approach. Journal of Traumatic Stress, 17, 195–202. [DOI] [PubMed] [Google Scholar]
- Rauch SA, Kim HM, Powell C, Tuerk PW, Simon NM, Acierno R, … & Stein MB (2019). Efficacy of prolonged exposure therapy, sertraline hydrochloride, and their combination among combat veterans with posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry, 76, 117–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen RC, Marx BP, Maserejian NN, Holowka DW, Gates MA, Sleeper LA, … Keane TM (2012). Project VALOR: Design and methods of a longitudinal registry of post-traumatic stress disorder (PTSD) in combat-exposed veterans in the Afghanistan and Iraqi military theaters of operations. International Journal of Methods in Psychiatric Research, 21, 5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Schaie KW (1965). A general model for the study of developmental problems. Psychological Bulletin, 64, 92–107 [DOI] [PubMed] [Google Scholar]
- Schaie KW (2005). Developmental influences on adult intelligence: The Seattle longitudinal study. Oxford University Press. [Google Scholar]
- Schnurr PP, Lunney CA, Bovin MJ, & Marx BP (2009). Posttraumatic stress disorder and quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical Psychology Review, 29, 727–735. [DOI] [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. Annals of Statistics, 6, 461–464. [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, … & Dunbar GC (1997). The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry, 12, 232–241. [Google Scholar]
- Spitzer RL, Kroenke K, & Williams JB (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary Care Evaluation of Mental Disorders. Journal of the American Medical Association, 282, 1737–1744. [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Schlenger WE, Corry N, Henn-Haase C, Qian M, Li M, … & Shalev A (2017). Predictors of PTSD 40 years after combat: Findings from the National Vietnam Veterans longitudinal study. Depression and Anxiety, 34, 711–722. [DOI] [PubMed] [Google Scholar]
- Street AE, Gradus JL, Giasson HL, Vogt D, & Resick PA (2013). Gender differences among veterans deployed in support of the wars in Afghanistan and Iraq. Journal of General Internal Medicine, 28, 556–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliwinski M, Hoffman L, & Hofer SM (2010). Evaluating convergence of within-person change and between-person age differences in age-heterogeneous longitudinal studies. Research in Human Development, 7, 45–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, & Hoge CW (2010). Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry, 67, 614–623. [DOI] [PubMed] [Google Scholar]
- Titov N, Dear BF, McMillan D, Anderson T, Zou J, & Sunderland M (2011). Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cognitive Behaviour Therapy, 40, 126–136. [DOI] [PubMed] [Google Scholar]
- Tolin DF, & Foa EB (2006). Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychological Bulletin, 132, 959–992. [DOI] [PubMed] [Google Scholar]
- Vasterling JJ, Aslan M, Proctor SP, Ko J, Marx BP, Jakupcak M, … & Concato J (2016). Longitudinal examination of posttraumatic stress disorder as a long-term outcome of Iraq war deployment. American Journal of Epidemiology, 184, 796–805. [DOI] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, & Vasterling JJ (2008). Validation of scales from the deployment risk and resilience inventory in a sample of operation iraqi freedom veterans. Assessment, 15, 391–403. [DOI] [PubMed] [Google Scholar]
- Vogt D, Vaughn R, Glickman ME, Schultz M, Drainoni ML, Elwy R, & Eisen S (2011). Gender differences in combat-related stressors and their association with postdeployment mental health in a nationally representative sample of US OEF/OIF veterans. Journal of Abnormal Psychology, 120, 797–806. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility Paper presented at the annual convention of the international society for traumatic stress studies, San Antonio, TX. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Wilkins KC, Lang AJ, & Norman SB (2011). Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and Anxiety, 28, 596–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, Holowka DW, Vasterling JJ, Han SC, Chen MS, … Keane TM (2014). Traumatic brain injury, PTSD, and current suicidal ideation among Iraq and Afghanistan US veterans. Journal of Traumatic Stress, 27, 244–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


