Abstract
Objective:
As rates of childhood obesity and pediatric type 2 diabetes (T2D) increase, a better understanding is needed of how these two conditions relate, and which subgroups of children are more likely to develop diabetes with and without obesity.
Methods:
To compare hotspots of childhood obesity and pediatric T2D in New York City, we performed geospatial clustering analyses on obesity estimates obtained from surveys of school-aged children and diabetes estimates obtained from healthcare claims data, from 2009–2013. Analyses were performed at the Census tract level. We then used multivariable regression analysis to identify sociodemographic and environmental factors associated with these hotspots.
Results:
We identified obesity hotspots in Census tracts with a higher proportion of Black or Hispanic residents, with low median household income, or located in a food swamp. 51.1% of pediatric T2D hotspots overlapped with obesity hotspots. For pediatric T2D, hotspots were identified in Census tracts with a higher proportion of Black residents and a lower proportion of Hispanic residents.
Conclusions:
Non-Hispanic Black neighborhoods had a higher probability of being hotspots of both childhood obesity and pediatric type 2 diabetes. However, we identified a discordance between hotspots of childhood obesity and pediatric diabetes in Hispanic neighborhoods, suggesting either under-detection or under-diagnosis of diabetes, or that obesity may influence diabetes risk differently in these two populations. These findings warrant further investigation of the relationship between childhood obesity and pediatric diabetes among different racial and ethnic groups, and may help guide pediatric public health interventions to specific neighborhoods.
Keywords: childhood obesity, pediatric diabetes, hotspots, geographic analysis, sociodemographic factors
INTRODUCTION
The relationship between childhood obesity and pediatric diabetes in the United States has been well established.1–3 However, as the rates of both childhood obesity and pediatric diabetes continue to increase, more study of which subgroups of children are more likely to develop diabetes with and without obesity is necessary in order to implement effective preventive intervention. According to surveillance sources, the estimated prevalence of pediatric type 2 diabetes (T2D) in New York City (NYC) is 0.11%, more than twice that of the national estimate which is 0.05%.4, 5 Additionally, almost half of NYC public school children are overweight or obese; nationwide, about 1 in 5 children are estimated to be obese and another 15% are overweight.6, 7 In both NYC and nationwide, children from racial/ethnic minority groups and children from low-income households are disproportionately affected by both obesity and diabetes.8, 9 In addition, geographic disparities have been observed nationally beyond those attributable to race and socioeconomic factors.10
Geographic disparities have also been observed in obesity and diabetes prevalence among NYC children.5, 10 Our study compared hotspots of childhood obesity and hotspots of pediatric diabetes in NYC, using emergency claims data from a New York State claims database to estimate type 2 diabetes, and data from K-12 school screening to evaluate for obesity. Approximately 30% of NYC children visit an emergency department (ED) in a given year; thus, emergency claims data offers a larger sample than other potential data sources.11 Emergency claims data has been shown to correlate accurately with other methods for chronic disease prevalence estimation, such as survey data or registry data.5, 12 Geospatial analysis was used to identify areas of concordance and discordance between childhood obesity and pediatric diabetes in NYC. The goal of this ecologic study was to understand where these hotspots overlap and do not overlap by analyzing demographics, socioeconomic status, and food environment, all of which we hypothesized would play a role in determining rates of childhood obesity and pediatric diabetes.
METHODS
Study Design and Setting
To compare hotspots of childhood obesity and pediatric diabetes in NYC, we performed geospatial clustering analyses on prevalence estimates obtained from surveys of school-aged children and healthcare claims data. The healthcare claims data was geocoded using each patient’s home address. The target population included school-aged children from ages 5 to 19 years old, and the study period was 2009 to 2013. All analyses were performed at the Census tract level. We then used multivariable regression to identify demographic, socioeconomic, and environmental factors associated with these hotspots of childhood obesity and diabetes.
Data Sources
The data on children with obesity comes from the NYC Fitnessgram, which is an annual assessment of public school and charter school students in grades K-12 that is conducted by the NYC Department of Health and Mental Hygiene Office of School Health (OSH).13 The percentage of students who are overweight or obese is calculated based on the Centers for Disease Control and Prevention (CDC) BMI percentiles for age and gender. Diabetes prevalence was estimated as previously described in the literature using emergency claims data from the Statewide Planning and Research Cooperative System (SPARCS), an all-payer New York State claims database.14 Sociodemographic factors were obtained from Census data from the American Community Survey.15 Data on restaurants and retail food stores were obtained from inspection data from the NYC Department of Health and Mental Hygiene and the New York State Department of Agriculture and Markets.16
Main Outcomes
The main outcome was the identification of childhood obesity and pediatric diabetes hotspots. As determined by the CDC, childhood obesity was defined as a body-mass-index at or above the 95th percentile for children and teens of the same age and sex.17 Pediatric T2D were analyzed separately using emergency claims data. We estimated the prevalence of T2D among unique children who had visited the ED one or more times during the study period. Pediatric ED visitors were identified as diabetic if they had a primary or secondary International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code with the prefix 250. Using unique identifiers, we accounted for repeated emergency visits by the same child across multiple hospitals. Prevalence estimates, defined as the number of unique ED patients with a diagnosis of T2D respectively divided by the total number of unique ED patients, were made at the Census tract level and then analyzed for hot and cold spots.
Using algorithms in the published literature, we identified children as having T2D if they were at least 10 years old and more than 50% of their diabetes diagnosis codes were listed as type 2. We excluded children with type 1 diabetes, identified as having 50% or more diabetes diagnosis codes listed as type 1 (last digit of ICD-9 code of 1 or 3) or being <10 years old. This algorithm has been reported to be 88.4% sensitive and 88.5% specific.18 Prior research suggests that more complex algorithms that include data not available in claims data (e.g., laboratory values or prescription records) only provided a modest improvement over using diagnosis codes alone.19
Multivariable Predictors
We examined whether the following sociodemographic factors were associated with childhood obesity and diabetes hotspots: the proportion of residents that were children, female, non-Hispanic Black (here on referenced as Black), and Hispanic, to account for age, sex, race and ethnicity. We also included median household income to account for socioeconomic differences. To characterize the food environment, we identified fast food swamps and retail food swamps. Fast food “swamps” were identified by the proportion of nearby restaurants categorized as fast food. After excluding non-restaurants and collapsing observations to unique restaurants by name and location, we identified fast food restaurants by a venue marked as fast food or service marked as take-out or counter service only. For the retail food environment, we used inspection data from the New York State Department of Agriculture and Markets.16 Retail food “swamps” were identified as the proportion of retail food stores categorized as bodegas or small convenience stores, which often have poorer food choices than larger grocery stores.20 For both food environment measures, we included the restaurants and food stores within a one-mile radius of each Census tract’s centroid based on prior studies.21
Statistical Analysis
To identify statistically significant hotspots of childhood obesity and diabetes, we used the Getis-Ord Gi-star statistic to identify hotspots where our prevalence estimates for childhood obesity and diabetes demonstrated statistically significant clustering.22 A distance band of one mile was used to identify clustered values. We used a confidence level of 95% to identify hotspots and used a false discovery rate correction to account for multiple comparisons. We then performed a logistic regression with robust standard errors to identify predictors of childhood obesity and diabetes hotspots. We used an adjusted p-value of less than 0.025 using Bonferroni correction to account for the two separate regression analyses.23 In addition to reporting statistical significance, we used a margins analysis to compare the effect size of the included variables.5 We calculated the probability of being located in a childhood obesity or diabetes hotspot by changing a given predictor variable to its maximum value (except for income which was assessed at its lowest value) as compared to the average citywide probability.
We excluded a few tracts where the estimated population error from Census data was greater than half of the total number of residents estimated in each tract. This exclusion was to eliminate the influence of tracts where Census estimates were not stable enough for analysis. Of 2,167 Census tracts in NYC, this exclusion affected 40 tracts with zero population (mostly parks and airports) and 27 tracts with substantial sampling error. Of the remaining 2,089 tracts, 11 Census tracts had less than 30 children with height and weight measurements and 25 Census tracts had less than 100 unique children identified in emergency claims data. These Census tracts were also excluded to ensure stability of prevalence estimates for obesity and diabetes. Our final sample included 2,064 census tracts (95% of total).
Statistical analyses were performed in Stata 14.2 (StataCorp: College Station, TX, 2015). Geographic analysis was performed using ArcGIS Desktop 10.3.1 (ESRI: Redlands, CA, 2015) and GeoDa 1.8 (Center for Spatial Data Science: University of Chicago, 2016). Our study protocol was approved by the Institutional Review Board at the NYU School of Medicine.
RESULTS
Among NYC Census tracts, the proportion of children ranged from 1.3% to 49.8%. The proportion of female residents ranged from 34.0% to 66.3%. The proportion of Black residents ranged from 0.0% to 99.3%. The proportion of Hispanic residents ranged from 0.0% to 97.3%. Median household income ranged from $9,959 to $250,001. The proportion of restaurants within one mile categorized as fast food ranged from 34.2% to 100%, and the proportion of retail food stores within one mile categorized as convenience stores ranged from 54.2% to 100%. Among the Census tracts studied, the prevalence of childhood obesity and pediatric T2D ranged from 2.5% to 31.9% and 0.0% to 1.2%, respectively.
Hotspots of Childhood Obesity and Diabetes
In NYC, we identified statistically significant hotspots of childhood obesity and T2D, respectively, in 34.1% and 20.5% of the Census tracts analyzed in our study. On average, the prevalence of childhood obesity and T2D were, respectively, 1.4 and 1.8 times higher in hotspots versus non-hotspots. 51.1% of T2D hotspots overlapped with obesity hotspots (Figures 1 and 2). The overlap between hotspots of T2D and obesity was primarily concentrated in Census tracts within Brooklyn.
Figure 1:
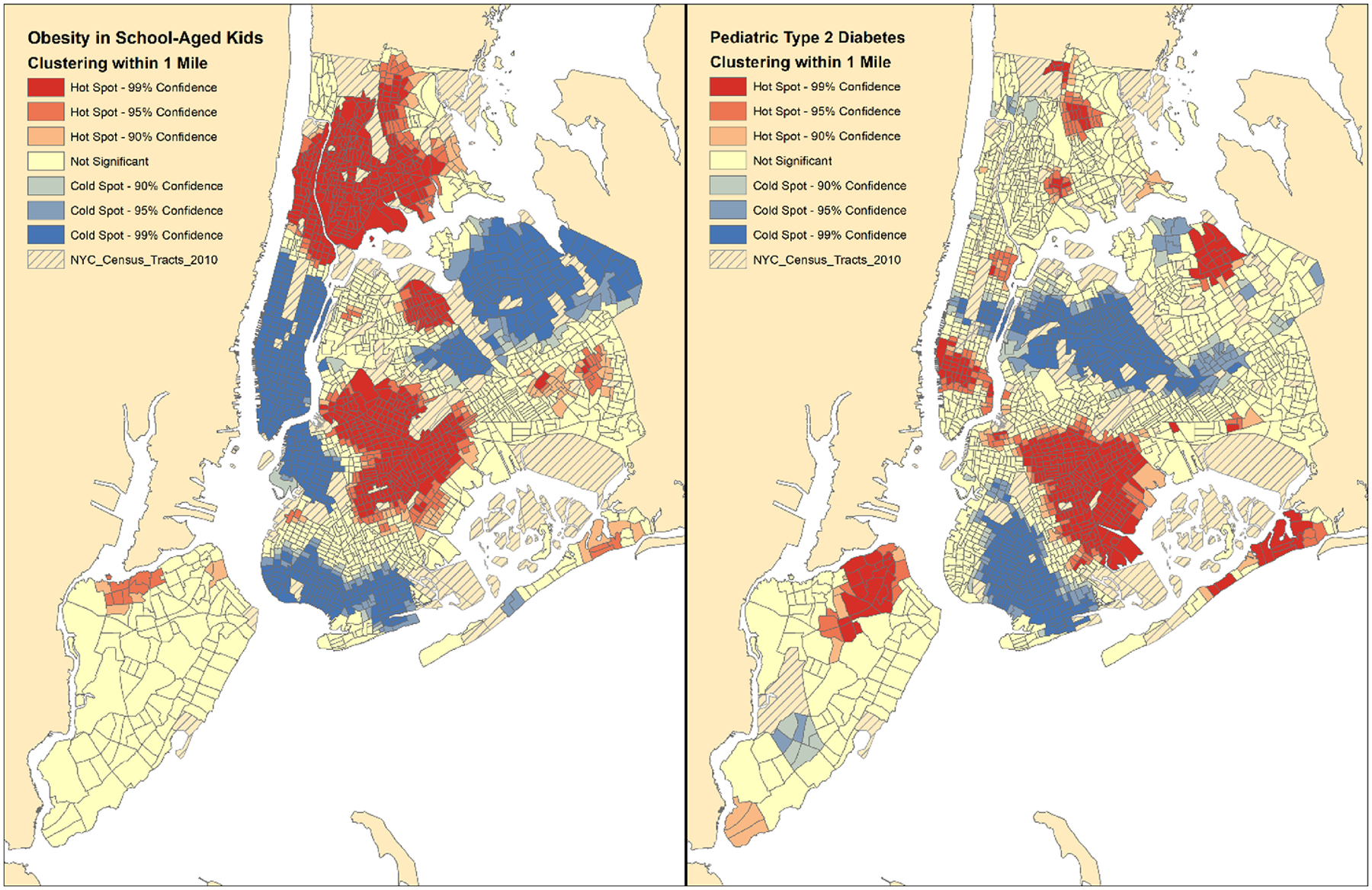
Geographic Clustering of Obesity versus Type 2 Diabetes Among School-Aged Children
Figure 2a:
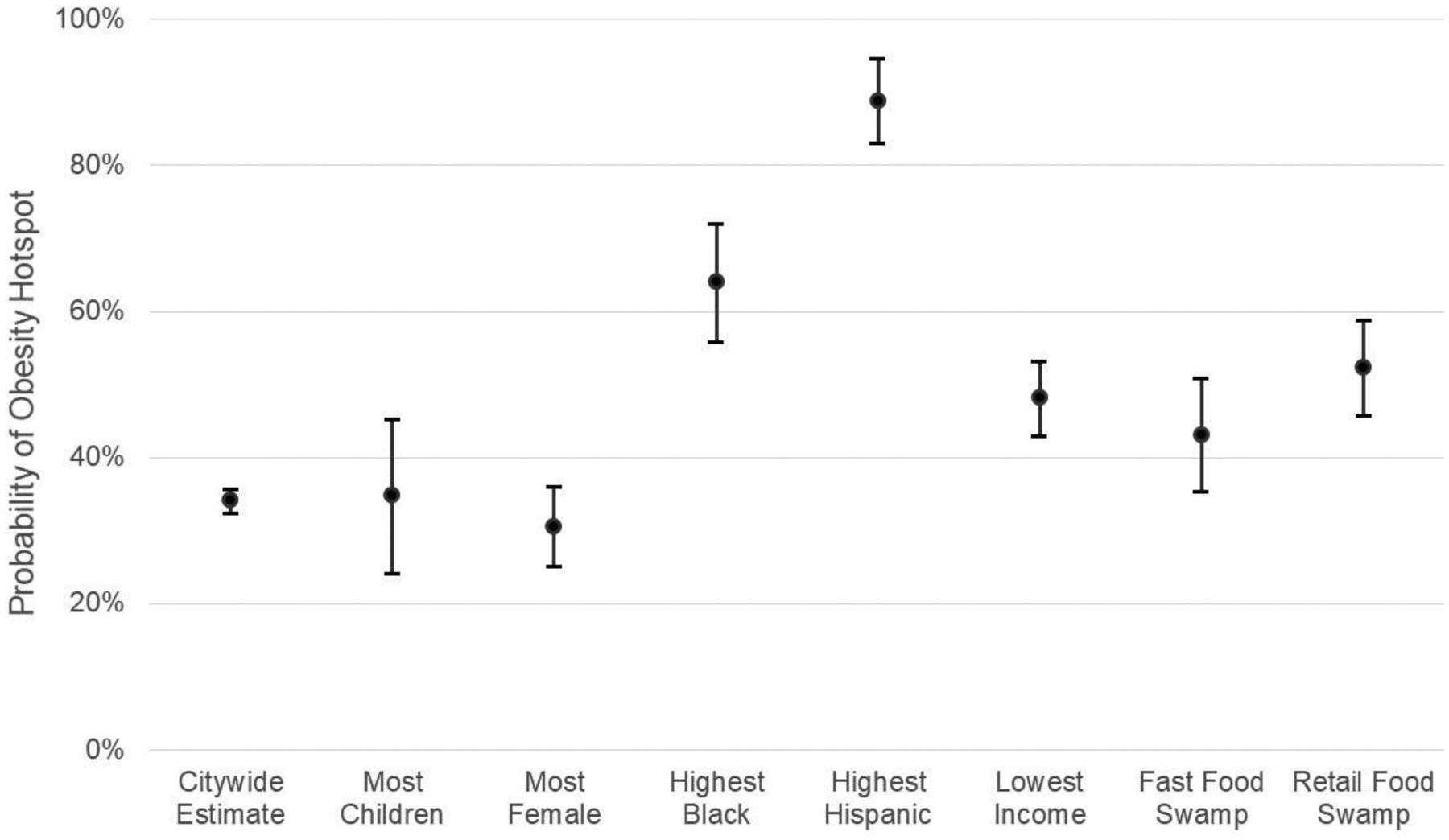
Neighborhood Characteristics Associated with Hotspots of Childhood Obesity
Factors Predicting the Location of Hotspots
In our multivariable logistic regression, we identified statistically significant factors associated with hotspots of childhood obesity and diabetes. Obesity hotspots were found in Census tracts with a higher proportion of residents who were Black or Hispanic, had low median household income, or located in a fast food or retail food swamp (Table 1). Comparing effect size through a margins analysis, we found Hispanic neighborhoods had the highest probability (88.9%) of being a hotspot of childhood obesity. This was followed by Black neighborhoods, retail food swamps, low income areas, and fast food swamps, which respectively had a 64.0%, 52.3%, 48.1%, and 43.1% probability of being a hotspot of childhood obesity (Figure 2a).
Table 1:
Logistic Regression of Factors Predicting Hotspots of Childhood Obesity and Pediatric Diabetes
| Predictor Factors | Coefficient | Confidence Interval | P-Value |
|---|---|---|---|
| Hotspots of Childhood Obesity | |||
| % Children | +0.76 | −3.30, +4.83 | 0.653 |
| % Female | −2.92 | −7.32, +1.47 | 0.112 |
| % Non-Hispanic Black | +4.37 | +3.37, +5.36 | < 0.001 |
| % Hispanic | +7.94 | +6.73, +9.16 | < 0.001 |
| Median Household Income | −3.03 | −4.14, −1.92 | < 0.001 |
| % Fast Food Restaurants | +3.05 | +0.14, +5.97 | 0.012 |
| % Convenience Stores | +10.80 | +7.62, +13.98 | < 0.001 |
| Hotspots of Pediatric Type 2 Diabetes | |||
| % Children | +0.00 | −2.47, +2.46 | 0.999 |
| % Female | −0.21 | −4.01, +3.58 | 0.892 |
| % Non-Hispanic Black | +3.35 | +2.52, +4.17 | < 0.001 |
| % Hispanic | −1.07 | −1.88, −0.26 | 0.002 |
| Median Household Income | −0.10 | −0.82, +0.62 | 0.736 |
| % Fast Food Restaurants | −0.37 | −2.44, +1.69 | 0.666 |
| % Convenience Stores | −1.38 | −3.37, +0.62 | 0.099 |
For pediatric T2D, hotspots were predicted to be in Census tracts with a higher proportion of Black residents and a lower proportion of Hispanic residents (Table 1). Comparing effect size through a margins analysis, we found that Black neighborhoods had the highest probability at 70.3% of being in a hotspot of type 2 diabetes. Hispanic neighborhoods had the lowest probability at 11.8% of being in a hotspot of type 2 diabetes (Figure 2b).
Figure 2b:
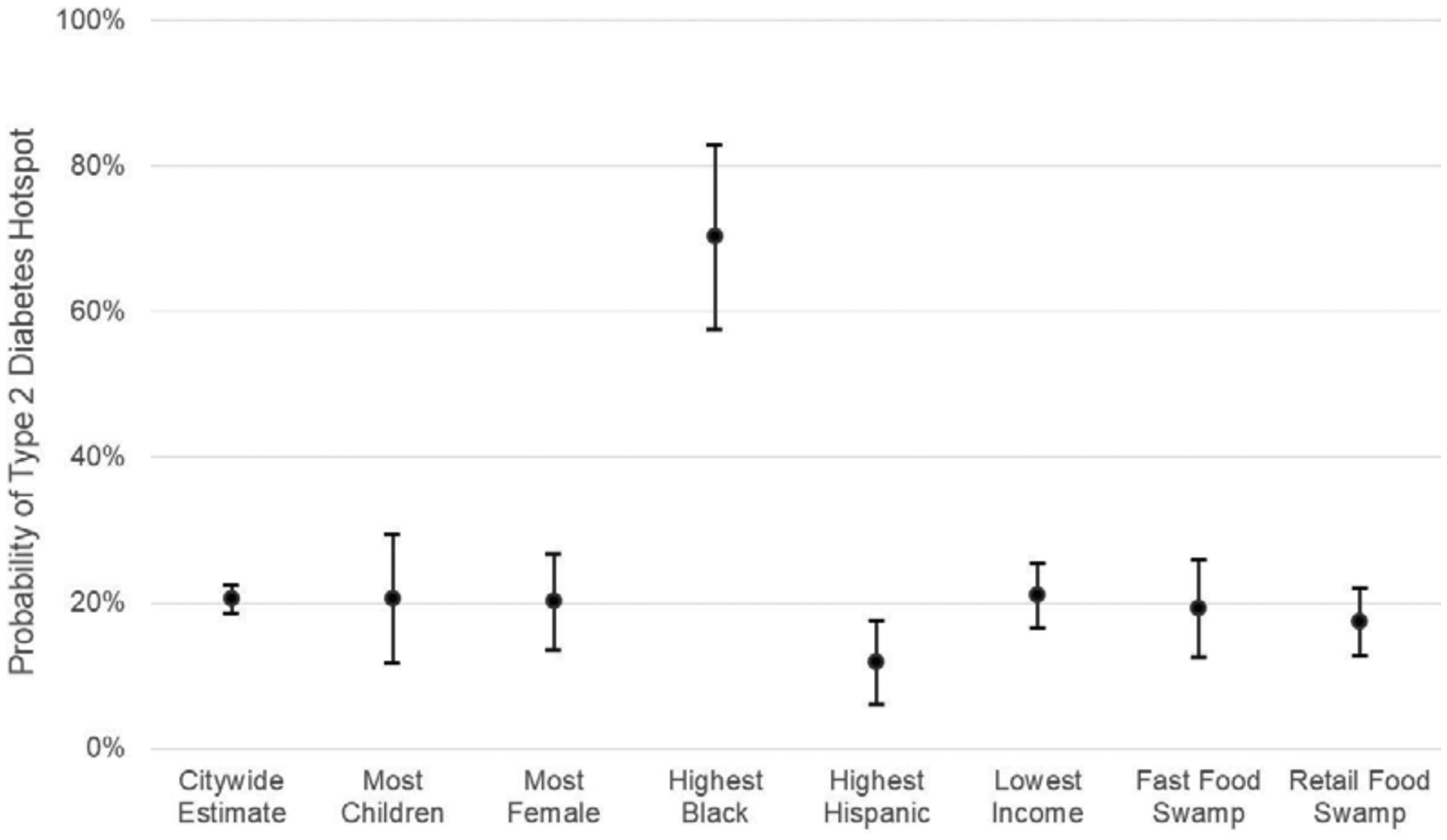
Neighborhood Characteristics Associated with Hotspots of Pediatrics Type 2 Diabetes
DISCUSSION
This study compared NYC hotspots of childhood obesity and pediatric type 2 diabetes in order to better understand which subgroups of children are more likely to develop type 2 diabetes with and without concurrent obesity. Our data showed that predominantly Black neighborhoods in NYC had a greater than 60% probability of being a pediatric obesity hotspot and an approximately 50% probability of being a hotspot for pediatric T2D, suggesting that Black children in NYC are at higher risk for both conditions. Although this is consistent with current literature on the subject, it is surprising that the factor most associated with pediatric T2D prevalence was the proportion of Black residents, and not household income or food environment.24
These results suggest that although physical food environment plays a role in the development of T2D, roles of other factors such as genetics, health behaviors, environmental exposures, and family influences must also be strongly considered.5 As expected, obesity hotspots were strongly associated with the food environment with most obesity hotspots being located in food swamps.20 In addition, more than half of pediatric T2D hotspots overlapped with obesity hotspots. These overlapping hotspots were primarily found in Brooklyn neighborhoods with predominantly Black residents. In a prior study, Brooklyn was found to have three of the seven largest food swamps in NYC, and East Harlem had the second largest food swamp.25 Both locations demonstrated overlapping hotspots of pediatric obesity and T2D.5, 20 It should be noted that several areas in northern Staten Island, northeast Queens and parts of Manhattan were hotspots of pediatric T2D but not hotspots of childhood obesity. These neighborhoods warrant further investigation as they may be areas where children are developing type 2 diabetes without concurrent obesity; identifying ecologic variables contributing to this disparity may be of public health relevance.
A substantial discordance between rates of obesity and diabetes was observed among Hispanic neighborhoods. Predominantly Hispanic neighborhoods in NYC had nearly a 90% probability of being a hotspot of obesity, yet simultaneously had the lowest probability at 12% of being a hotspot of T2D. Diabetes prevalence among Hispanics can differ by race, country of origin, and the number of years spent living in the United States.26 In NYC, Mexicans, Puerto Ricans, and Dominicans have the highest prevalence of diabetes within the Hispanic community, and a large percentage of these populations live in the areas we identified as hotspots of obesity.27 Thus, the discordance between pediatric obesity and T2D was unexpected, especially given that both Black and Hispanic adults have a higher risk of developing diabetes with both groups demonstrating an increasing incidence of diabetes.28, 29 This finding may be a significant limitation of our approach of identifying cases of diabetes using emergency claims data. It might also suggest that there is significant under-detection or under-diagnosis of diabetes among Hispanic children, which means more effort needs to be directed towards identifying these cases.
In our study, both Black and Hispanic children in NYC largely live in hotspots of obesity, yet may have substantial differences in their risk of type 2 diabetes. These differences may be due to family influences, environmental exposures, health behaviors, and genetic differences between the two minority subgroups. Some studies have shown differences in dietary composition between Black and Hispanic children, which may account for some of the differences in diabetes risk.30, 31 Data from the SEARCH studies have found that Black and Hispanic children generally showed similar exercise time and television consumption, but differ in other demographic characteristics.32, 33 While there is a large body of literature examining health outcomes and risk factors among minorities as compared to their White counterparts, more studies are needed to analyze the differences and similarities among minority subgroups and differences between specific geographic areas.
Limitations
This study has certain limitations. First, BMI measurements are calculated only among public school children. There may be a small bias due to exclusion of school aged children who attend private or home schooling. Second, emergency department utilization is higher among certain populations, especially those who are publicly insured, impoverished, and in minority groups.34, 35 Thus, our estimates of diabetes prevalence may be influenced by these biases. However, the impact is minimized by the use of small geographic units as patients are assigned to the exact geographic location where they live. Attribution is at the Census tract level, which are much more demographically homogenous than larger geographic units. Finally, our multivariable analysis may not have included all salient variables and other factors may better explain the lack of overlap between hotspots of childhood obesity and diabetes.
Conclusions
The strongest predictor of hotspots of pediatric obesity in NYC was a higher proportion of Hispanic residents. Whereas, the strongest predictor of hotspots of pediatric T2D in NYC was a higher proportion of Black residents. Though we found that children living in predominately Black neighborhoods had a higher risk of living in a hotspot of both childhood obesity and pediatric T2D, we identified a discordance between hotspots of childhood obesity and pediatric diabetes among Hispanic neighborhoods. Our results may suggest significant under-detection or under-diagnosis of diabetes among Hispanic children, or could also suggest that obesity may affect these two populations differently and also influence diabetes risk differently. These findings warrant further investigation of the relationship between childhood obesity and pediatric diabetes, especially among different racial and ethnic groups.
WHAT’S NEW.
Our study analyzed childhood obesity and diabetes in New York City. The factor most associated with diabetes or obesity, respectively, was the proportion of Black residents or Hispanic residents. These findings can help direct public health interventions to specific neighborhoods.
Acknowledgements:
This study was funded by grant K23DK110316 from the National Institute of Diabetes and Digestive and Kidney Disease and grant 1-INO-2017-449-A-N from the Juvenile Diabetes Research Foundation. The funding sources had no involvement in the study design, collection, analysis, interpretation of the data, writing of the report, nor the decision to submit the article for publication. There are no potential conflicts of interest to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Liu LL, Lawrence JM, Davis C, et al. Prevalence of overweight and obesity in youth with diabetes in USA: the SEARCH for Diabetes in Youth study. Pediatr Diabetes. 2010;11:4–11. [DOI] [PubMed] [Google Scholar]
- 2.Minges KE, Whittemore R, Weinzimer SA, Irwin ML, Redeker NS, Grey M. Correlates of overweight and obesity in 5529 adolescents with type 1 diabetes: The T1D Exchange Clinic Registry. Diabetes Res Clin Pract. 2017;126:68–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Libman IM, Pietropaolo M, Arslanian SA, LaPorte RE, Becker DJ. Changing prevalence of overweight children and adolescents at onset of insulin-treated diabetes. Diabetes Care. 2003;26:2871–2875. [DOI] [PubMed] [Google Scholar]
- 4.Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311:1778–1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee DC, Gallagher MP, Gopalan A, et al. Identifying Geographic Disparities in Diabetes Prevalence Among Adults and Children Using Emergency Claims Data. J Endocr Soc. 2018;2:460–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NYC Health. Pediatric Obesity Action Kit. https://www1.nyc.gov/site/doh/providers/resources/public-health-action-kits-pediatric-obesity.page. [Google Scholar]
- 7.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics. 2018;141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schroeder K, Jia H, Wang YC, Smaldone A. Implementation of a School Nurse-led Intervention for Children With Severe Obesity in New York City Schools. J Pediatr Nurs. 2017;35:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014;370:403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elbel B, Corcoran SP, Schwartz AE. Neighborhoods, Schools and Obesity: The Potential for Place-Based Approaches to Reduce Childhood Obesity. PLoS One. 2016;11:e0157479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.New York City Department of Health and Mental Hygiene. Epiquery: Child Community Health Survey. https://a816-healthpsi.nyc.gov/epiquery/Child/CCHSIndex.html2009. [Google Scholar]
- 12.Lee DC, Yi SS, Fong HF, et al. Identifying Local Hot Spots of Pediatric Chronic Diseases Using Emergency Department Surveillance. Acad Pediatr. 2017;17:267–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rundle A, Richards C, Bader MD, et al. Individual-and school-level sociodemographic predictors of obesity among New York City public school children. 2012;176:986–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quan JM. SPARCS: the New York State health care data system. J Clin Comput. 1980;8:255–263. [PubMed] [Google Scholar]
- 15.U.S. Census Bureau. 2009–2013 American Community Survey 5-Year Estimates. https://www.census.gov/programs-surveys/acs/data/summary-file.2013.html. [Google Scholar]
- 16.New York State Department of Agriculture and Markets Bureau of Community Environmental Health and Food Protection. Food Service Establishment: Last Inspection. https://data.ny.gov/Economic-Development/Retail-Food-Stores/9a8c-vfzj. [Google Scholar]
- 17.Centers for Disease Control and Prevention. BMI for Children and Teens. https://www.cdc.gov/obesity/childhood/defining.html. [Google Scholar]
- 18.Zhong VW, Pfaff ER, Beavers DP, et al. Use of administrative and electronic health record data for development of automated algorithms for childhood diabetes case ascertainment and type classification: the SEARCH for Diabetes in Youth Study. Pediatr Diabetes. 2014;15:573–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lawrence JM, Black MH, Zhang JL, et al. Validation of pediatric diabetes case identification approaches for diagnosed cases by using information in the electronic health records of a large integrated managed health care organization. Am J Epidemiol. 2014;179:27–38. [DOI] [PubMed] [Google Scholar]
- 20.Cooksey-Stowers K, Schwartz MB, Brownell KD. Food Swamps Predict Obesity Rates Better Than Food Deserts in the United States. Int J Environ Res Public Health. 2017;14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hirsch JA, Hillier A. Exploring the role of the food environment on food shopping patterns in Philadelphia, PA, USA: a semiquantitative comparison of two matched neighborhood groups. Int J Environ Res Public Health. 2013;10:295–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee DC, Jiang Q, Tabaei BP, et al. Using Indirect Measures to Identify Geographic Hot Spots of Poor Glycemic Control: Cross-sectional Comparisons With an A1C Registry. Diabetes Care. 2018;41:1438–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonferroni CE. Teoria statistica delle classi e calcolo delle probabilità: Libreria internazionale Seeber; 1936. [Google Scholar]
- 24.Bancks MP, Kershaw K, Carson AP, Gordon-Larsen P, Schreiner PJ, Carnethon MR. Association of Modifiable Risk Factors in Young Adulthood With Racial Disparity in Incident Type 2 Diabetes During Middle Adulthood. JAMA. 2017;318:2457–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.González-Rivera C State of the Chains, 2017 In: Dvorkin E, ed: Center for an Urban Future; 2017. [Google Scholar]
- 26.Schneiderman N, Llabre M, Cowie CC, et al. Prevalence of diabetes among Hispanics/Latinos from diverse backgrounds: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Diabetes Care. 2014;37:2233–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greer S, Naidoo M, Hinterland K, et al. Health of Latinos in NYC. 1–32. [Google Scholar]
- 28.Mayer-Davis EJ, Dabelea D, Lawrence JM. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002–2012. N Engl J Med. 2017;377:301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gregg EW, Zhuo X, Cheng YJ, Albright AL, Narayan KM, Thompson TJ. Trends in lifetime risk and years of life lost due to diabetes in the USA, 1985–2011: a modelling study. Lancet Diabetes Endocrinol. 2014;2:867–874. [DOI] [PubMed] [Google Scholar]
- 30.Vikraman S, Fryar CD, Ogden CL. Caloric Intake From Fast Food Among Children and Adolescents in the United States, 2011–2012 NCHS data brief, no213. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 31.Skala K, Chuang RJ, Evans A, Hedberg AM, Dave J, Sharma S. Ethnic differences in the home food environment and parental food practices among families of low-income Hispanic and African-American preschoolers. J Immigr Minor Health. 2012;14:1014–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lawrence JM, Mayer-Davis EJ, Reynolds K, et al. Diabetes in Hispanic American youth: prevalence, incidence, demographics, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32 Suppl 2:S123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mayer-Davis EJ, Beyer J, Bell RA, et al. Diabetes in African American youth: prevalence, incidence, and clinical characteristics: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2009;32 Suppl 2:S112–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004;42:176–182. [DOI] [PubMed] [Google Scholar]
- 35.Luo X, Liu G, Frush K, Hey LA. Children’s health insurance status and emergency department utilization in the United States. Pediatrics. 2003;112:314–319. [DOI] [PubMed] [Google Scholar]


