Abstract
OBJECTIVES:
While sarcopenia is prevalent after hip fracture in the acute postfracture period, little is known about the prevalence after discharge. This study assessed longitudinal trends in sarcopenia prevalence over 12 months after hip fracture using three different operational definitions.
DESIGN:
Prospective observational study.
SETTING:
Baltimore Hip Studies seventh cohort.
PARTICIPANTS:
A total of 82 men and 78 women, aged 65 years and older, with surgical repair of a nonpathological hip fracture.
MEASUREMENTS:
Baseline assessment included a dual-energy X-ray absorptiometry scan and interview. Follow-up assessments, which additionally included performance measures, occurred 2, 6, and 12 months after admission. Using these measures, three sarcopenia definitions were assessed over the year following hip fracture: European Working Group on Sarcopenia in Older Persons (EWGSOP), International Working Group on Sarcopenia (IWGS), and Foundation for the National Institutes of Health (FNIH).
RESULTS:
EWGSOP and IWGS provided the highest prevalence of sarcopenia (62%−69% in men, 42%−62% in women), while prevalence by FNIH was much lower for men (15%−19%) and women (5%−12%). For both men and women, the agreement between EWGSOP and IWGS definitions was excellent, and FNIH showed poor agreement with them, supported by various statistical measures across first-year follow-up. Prevalence was stable over time in men by all definitions, while the prevalence in women by FNIH was lowest at 2 months, significantly increased at 6 months (P = .03), and remained higher at 12 months. Whether sarcopenia prevalence differed significantly by sex varied by time point and definition; however, when different, men had a higher prevalence than women (P < .05). While some participants recovered from sarcopenia over time, some also became newly sarcopenic.
CONCLUSION:
The prevalence of sarcopenia after fracture differed greatly for EWGSOP and IWGS compared to FNIH. Overall, there appeared to be no reduction in sarcopenia over the year after hip fracture, regardless of definition. Future research should examine the relationship between sarcopenia prevalence and functional recovery.
Keywords: hip fracture, lower-extremity function, mobility disability, sarcopenia, sex differences
It is estimated more than 250,000 hospitalizations for hip fracture occur per year in the United States.1 Hip fractures result in increased risk of mortality and new disability.2,3 Osteoporosis, defined by low bone mineral density (BMD), is a known risk factor for hip fracture1; however, fracture risk and recovery are also related to sarcopenia.4 Sarcopenia, a geriatric syndrome of age-related loss of muscle and strength,5,6 is associated with disability and poor lower-extremity function in older adults.7 Studies have shown sarcopenia to be a risk factor for falls8 and fragility fractures (including hip fracture), independent of BMD.9,10 However, studies of sarcopenia after fracture have been limited to the acute postfracture period (typically a few days to within 1 month of fracture).11–19 Longitudinal changes in sarcopenia over a more extended postfracture period have not been examined.
The prevalence of sarcopenia in the acute period after fracture varies widely by study, ranging from 12%13 to 95%12 in men and from 18%13 to 68%15 in women. The heterogeneity in estimates is due, in part, to a lack of consensus on the definition of sarcopenia.20,21 There are several definitions of sarcopenia that incorporate different measurements for operationalization. The European Working Group on Sarcopenia in Older Persons (EWGSOP) definition6 and the International Working Group on Sarcopenia (IWGS)22 are two definitions that have cut points for lean mass and muscle function. Most recently, the Foundation of the National Institutes of Health (FNIH) sarcopenia project developed cut points to identify “clinically relevant weakness and low lean mass.”23 The criteria used to generate the cut points were predictive of increased mobility limitation.23 In the community-dwelling, older adult population, these three definitions do not have high agreement with each other.21
Despite the heterogeneity in estimates of sarcopenia after fracture, with one exception,13 studies find that men are more likely to be sarcopenic after fracture.12,14–16,19 Older men without fracture also have greater strength losses over time, compared to women.24 These findings suggest that longitudinal patterns of sarcopenia after fracture may differ by sex.
The aims of this study were to compare the prevalence of sarcopenia over the first year after hip fracture using three operational definitions, EWGSOP, IWGS, and FNIH, by (1) evaluating agreement and discrepancies across men and women, (2) determining whether there were longitudinal differences in sarcopenia prevalence within and between men and women, and (3) investigating the postfracture sarcopenia status transitions from month 2 to month 6, and from month 6 to month 12.
METHODS
Study Sample
Study subjects were from the seventh cohort of the Baltimore Hip Studies (BHS-7), a prospective observational study that frequency matched (1:1) men and women on calendar time of hip fracture and hospital. Participants received rehabilitation consistent with usual care, and no interventions were administered in this study. The sample comprised 339 hip fracture patients, aged 65 years and older, who were community dwelling with surgical repair of a nonpathological hip fracture at one of eight study hospitals in the Baltimore, MD, area. Participants were enrolled within 15 days after hospital admission. Patients who were not community dwelling, not English speaking, bed bound 6 months before fracture, weighed 300 pounds or more, lived 70 miles or more from the hospital of admission, did not have surgery, or had hardware in the non-fractured hip were excluded. At baseline and follow-up, patients underwent a dual-energy X-ray absorptiometry (DXA) scan and completed physical performance measures at 2, 6, and 12 months after admission. At all visits, participants completed an interview and had their grip strength assessed. The protocol was approved by the institutional review board (IRB) at the University of Maryland Baltimore, as well as by each study hospitalʼs IRB. Additional details of BHS-7 are described elsewhere.25 The analytic sample comprised 82 men and 78 women (N = 160) in BHS-7 who had DXA, grip strength, and physical performance measures available at 2 months after admission. Study participants who did not have the measures necessary for assessment of sarcopenia for all three definitions at 2 months after admission were excluded (N = 179). Participants who did not have an assessment of sarcopenia at 6 or 12 months after admission, or were lost to follow-up, were excluded from the analyses at those time points (excluded at 6 months: n = 19; excluded at 12 months: n = 35).
Measures
A modified Charlson Comorbidity Index measured how many of the following comorbidities a participant had: myocardial infarction, congestive heart failure, peripheral vascular disease, dementia, chronic pulmonary disease, connective tissue disease, ulcers, diabetes, hemiplegia, moderate or severe renal disease, diabetes with end-organ damage, tumor, leukemia, lymphoma, moderate or severe liver disease, metastatic solid tumor, and AIDS.26 It was modified by excluding mild liver disease, which was not assessed in this study. Cognitive status was assessed for these analyses using the Modified Mini-Mental State Examination (3MS).27
The prevalence of sarcopenia at multiple time points was assessed using three different definitions: EWGSOP,6 IWGS,22 and FNIH.23 These three definitions were chosen because they are widely used and include an assessment of muscle mass as well as muscle strength and/or physical performance. A summary of these three definitions is shown in Table 1. Each definition included an assessment of muscle strength, appendicular lean mass, and physical performance, with the physical performance component in the EWGSOP and FNIH being optional. Due to the requirement of a physical performance measure, IWGS could not be assessed at baseline. As a result, sarcopenia was only captured with all three definitions at 2, 6, and 12 months after admission. There are both similarities and differences across these three operational definitions of sarcopenia. IWGS defines slowness as a usual gait speed less than1.0 m/s, while both the EWGSOP and FNIH definitions define slowness as usual gait speed less than 0.8 m/s. The FNIH definition has a lower, more stringent cut point for grip strength than EWGSOP and IWGS. While EWGSOP and IWGS assess lean mass relative to height squared (and use the same cut points for this measure), FNIH assesses lean mass relative to body mass index (BMI).
Table 1.
Summary of Sarcopenia Operational Definitions and Thresholds
| Definition | Criteria | Physical Performance Gait Speed (Slowness), m/s | Strength Grip Strength (Weakness), kg | Lean Mass | ||||
|---|---|---|---|---|---|---|---|---|
| ALMBMI (Low Lean Mass) | ALM/ht2 (Low Lean Mass), kg/m2 | |||||||
| EWGSOP | Slowness OR weakness AND low lean mass | <0.8a | Men, <30 | Women, <20 | Men, ≤7.23 | Women, ≤5.67 | ||
| FNIH | Weakness AND low lean mass | <0.8a | Men, <26 | Women, <16 | Men, <0.789 | Women, <0.512 | ||
| IWGS | Slowness AND low lean mass | <1.0 | Men, ≤7.23 | Women, ≤5.67 | ||||
Note: Grayed out cells indicate that there is no relevant measure threshold for that definition. Dual-energy X-ray absorptiometry (DXA) scans were conducted at seven facilities, and statistical analyses were adjusted for DXA scanner location and type.28
Abbreviations: ALM, appendicular lean mass; BMI, body mass index; EWGSOP, European Working Group on Sarcopenia in Older Persons; FNIH, Foundation for the National Institutes of Health; ht2, height squared; IWGS, International Working Group on Sarcopenia.
Physical performance component in the EWGSOP and FNIH is optional.
Statistical Analyses
Data were analyzed and compared across men and women in this study. When the baseline characteristics and sarcopenia prevalence were compared across men and women, P values were obtained by two-sample t-tests for continuous variables and Fisherʼs exact test and Pearson χ2 tests for categorical variables.
To assess the agreement among the three operational sarcopenia definitions in the absence of a gold standard criterion, we used three statistical measures: positive percentage agreement (PPA), negative percentage agreement (NPA), and Cohenʼs κ.21,29 The first two values measured the pairwise sensitivity and specificity of one definition vs the others. Dam et al defined the PPA as “the proportion of participants who were categorized as having the condition by both the FNIH criteria and a second set of criteria divided by the number of participants who were categorized as having the condition by the second set of criteria.”21 Similarly, they defined the NPA. Cohenʼs κ statistics were calculated for all pairwise comparisons of three sarcopenia definitions in men and women separately and their interpretations were: κ < 0.4 indicates poor agreement; κ = 0.4 to 0.75, fair to good agreement; and κ ≥ 0.75, excellent agreement.29,30
As an exploratory analysis of longitudinal trends, we plotted the prevalence of sarcopenia over time by sex using EWGSOP, IWGS, and FNIH definitions in several ways. First, we compared sarcopenia prevalence using three definitions in one longitudinal plot to visualize their agreement. Second, we compared longitudinal prevalence across men and women for each sarcopenia definition to show the sex-specific trends, then confirmed the comparison of prevalence across two adjacent visits using McNemarʼs tests. Third, we plotted a comparison of sarcopenia trajectory by sex. Last, we assessed sarcopenia transitions in the year after hip fracture for men and women by each operational definition.
RESULTS
Baseline sample descriptive characteristics were compared by sex (82 men and 78 women), and the results are shown in Table 2. The mean ages of men and women in the sample are similar, 81.0 years for men and 80.2 years for women. Both men and women were predominantly white (92% and 96%, respectively), had similar BMI, and had similar education, consistent with some college (13.7 and 13.3 years for men and women, respectively). Women had significantly fewer comorbidities (P < .01), higher prevalence of osteoporosis (P < .01), and marginally higher cognition, as measured by the 3MS, than men (P = .06).
Table 2.
Study Sample Characteristics Across Men and Women (N = 160)
| Characteristic | Men (n = 82) | Women (n = 78) | P Value |
|---|---|---|---|
| Age, y | 81.0 (7.5) | 80.2 (7.6) | .5 |
| Race, white, % | 91.5 | 96.2 | .19 |
| Education, y | 13.7 (3.6) | 13.3 (3.0) | .5 |
| BMI, kg/m2 | 25.4 (3.9) | 25.5 (6.0) | .92 |
| Charlson Comorbidity Index | 2.4 (1.8) | 1.5 (1.7) | .002 |
| Osteoporosis, % | 18.3 | 38.5 | .004 |
| 3MS score | 85.3 (14.9) | 89.3 (12.3) | .06 |
Note: Data are given as mean (SD), unless otherwise indicated. P values derived from two-sample t-tests, except for race, which was assessed via Fisherʼs exact test; and osteoporosis, which was assessed via the χ2 test.
Abbreviation: BMI, body mass index; 3MS, Modified Mini-Mental State Examination.
We examined the agreement among these three operational sarcopenia definitions at varying months. The agreement of sarcopenia prevalence across varying definitions was visualized in Figure 1. Figure 1A,B showed that EWGSOP and IWGS definitions had excellent agreement, with κ statistics ≥0.85 for all time points in both men and women, including 100% agreement at month 2 in men. Both PPAs and NPAs between the EWGSOP and IWGS were high, all greater than 97% PPAs across all time points with all greater than 81% NPAs. However, FNIH showed poor agreement with EWGSOP and IWGS across all months in both men and women, with κ statistics ranging in men from 0.09 to 0.12 for FNIH and EWGSOP and from 0.04 to 0.09 for FNIH and IWGS, and in women from 0.03 to 0.11 and 0.02 to 0.11 for FNIH and EWGSOP and FNIH and IWGS, respectively. The PPAs between the FNIH and other definitions were low, ranging from 0.17 to 0.24 in men and from 0.06 to 0.58 in women; however, the NPAs were high, with all greater than 0.87 in men and all greater than 0.92 in women. There were no significant differences in the agreement findings across men and women based on κ statistic values.
Figure 1.
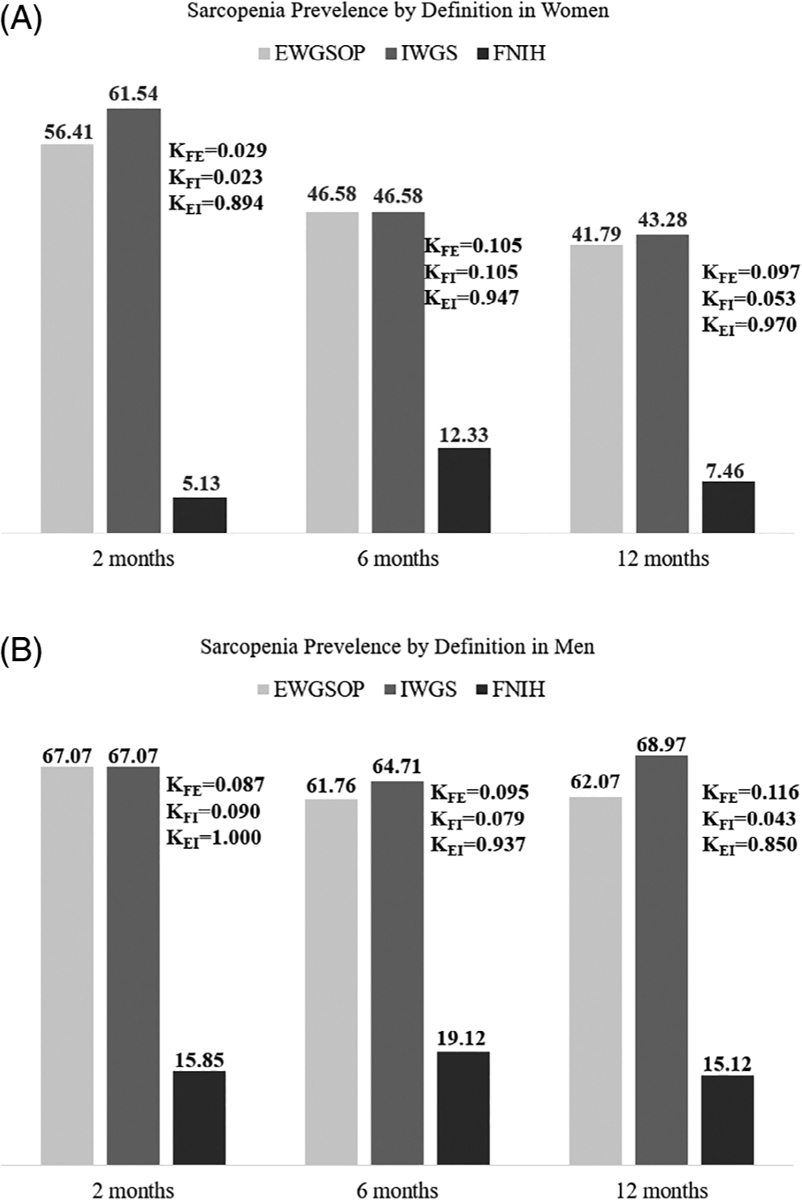
Sarcopenia prevalence and agreement by definition in men (A) and women (B). EWGSOP indicates European Working Group on Sarcopenia in Older Persons; FNIH, Foundations for National Institutes of Health; IWGS, International Working Group on Sarcopenia; κFE, κFI, κEI, Cohenʼs κ coefficients for the pairwise agreements with FNIH and EWGSOP pair, FNIH and IWGS pair, and EWGSOP and IWGS pair, respectively. Note. Study sample diminishes over time (6 months: n = 141; 12 months: n = 125).
In addition to agreement, Figure 1 demonstrates differences in sarcopenia prevalence by definition in men and women. Under FNIH, women had a prevalence of sarcopenia at 2, 6, and 12 months of 5.1%, 12.3%, and 7.46%, respectively, while men had a prevalence of 15.9%, 19.1%, and 15.1%, respectively. These prevalences are also plotted in Figure 2A,B for men and women, respectively. Men had a relatively stable sarcopenia trajectory over time across the three definitions. Furthermore, McNemarʼs tests confirmed that there were no statistically significant sarcopenia prevalence changes in men across months 2 to 6 and months 6 to 12, with all P values >.05, across all three operational definitions. Figure 2B shows that the prevalence of sarcopenia in women per the EWGSOP and IWGS definitions trended downward, while the prevalence per the FNIH definition trended upward for the first 6 months after hip fracture. Sarcopenia prevalence increased in women from 2 to 6 months by the FNIH definition (McNemarʼs test P = .025). No other differences in sarcopenia prevalence were statistically significant in women.
Figure 2.
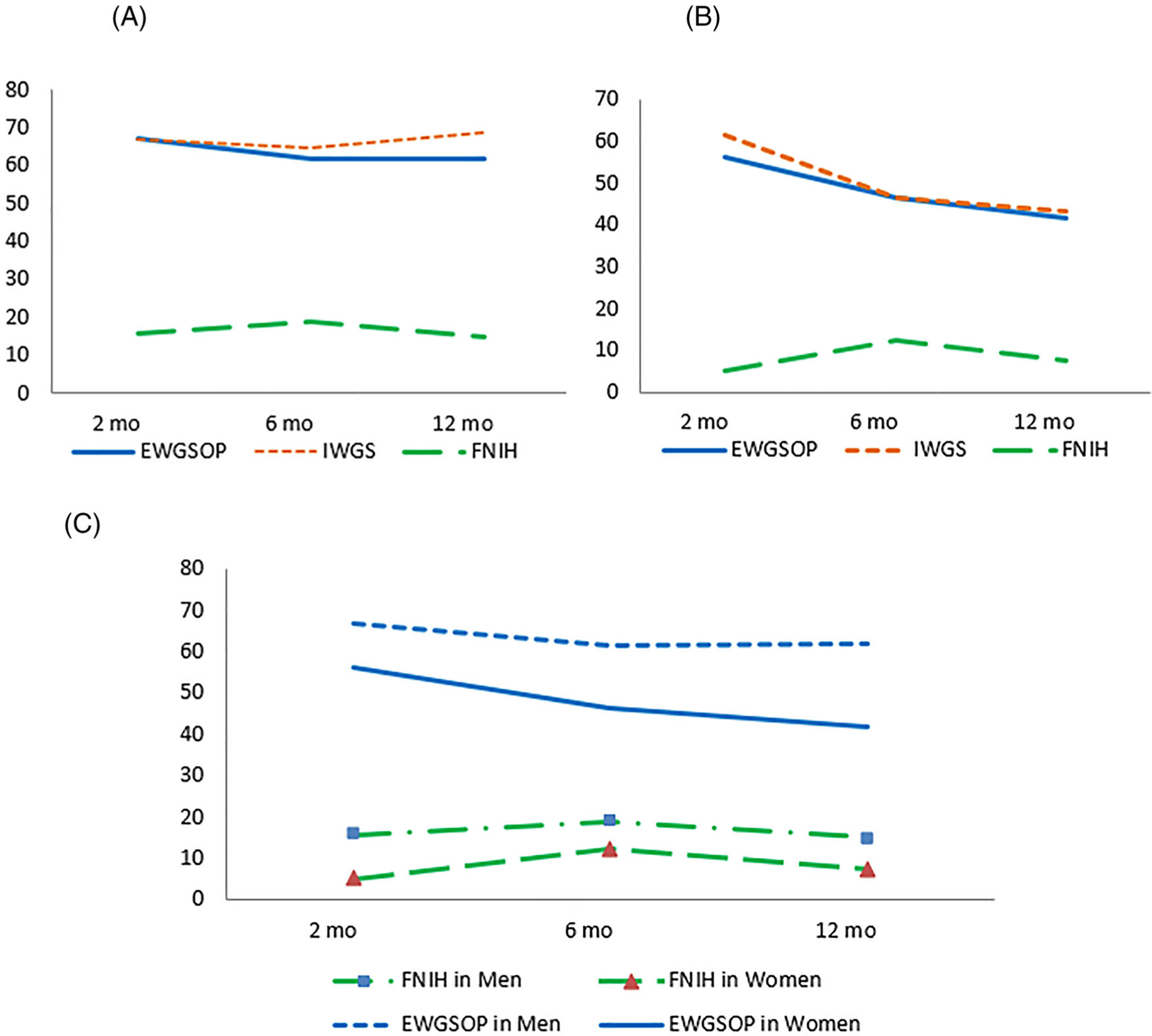
Longitudinal plots of sarcopenia prevalence by sex using European Working Group on Sarcopenia in Older Persons (EWGSOP), International Working Group on Sarcopenia (IWGS), and Foundations for National Institutes of Health (FNIH) definitions in the first year after hip fracture. A, Sarcopenia prevalence using three definitions in men. B, Sarcopenia prevalence using three definitions in women. C, Sarcopenia prevalence across men and women using EWGSOP and FNIH definitions. Note. Significant increase by the FNIH definition from month 2 to 6 (P = .03). Also, study sample diminishes over time (6 months: n = 141; 12 months: n = 125).
Sarcopenia prevalence over time was compared in men and women using both EWGSOP and FNIH definitions (Figure 2C). Since EWGSOP and IWGS have excellent agreement and similar prevalence, IWGS prevalence was not plotted in Figure 2C. Furthermore, χ2 tests were used to quantitatively compare sex differences in sarcopenia prevalence over time using the three operational definitions. Both exploratory and confirmatory analysis found that, compared to women, men had a significantly higher prevalence of sarcopenia at 2 months by FNIH (P = .03), at 6 months by IWGS (P = .03), and at 12 months by EWGSOP and IWGS (P = .02 and P < .01, respectively).
How participantsʼ sarcopenia status transitioned over time by the varying definitions is shown in Figure 3. Among men with sarcopenia data at adjacent time points, there were some changes in sarcopenia status (Figure 3A). Using the FNIH definition, changes in sarcopenic status were seen in 18% of men (9/51; 6 newly sarcopenic, 3 recovered sarcopenic) between 2 and 6 months, but only 13% of men (6/45; 4 newly sarcopenic, 2 recovered sarcopenic) between 6 and 12 months. For the IWGS definition, the values for men were 18% (9/51; 5 newly sarcopenic, 4 recovered sarcopenic) between 2 and 6 months and 7% (3/43; 2 newly sarcopenic, 1 recovered sarcopenic) between 6 and 12 months; for the EWGSOP definition, the values for men were 20% (11/53; 5 newly sarcopenic, 6 recovered sarcopenic) between 2 and 6 months and 11% (5/46; 3 newly sarcopenic, 2 recovered sarcopenic) between 6 and 12 months.
Figure 3.
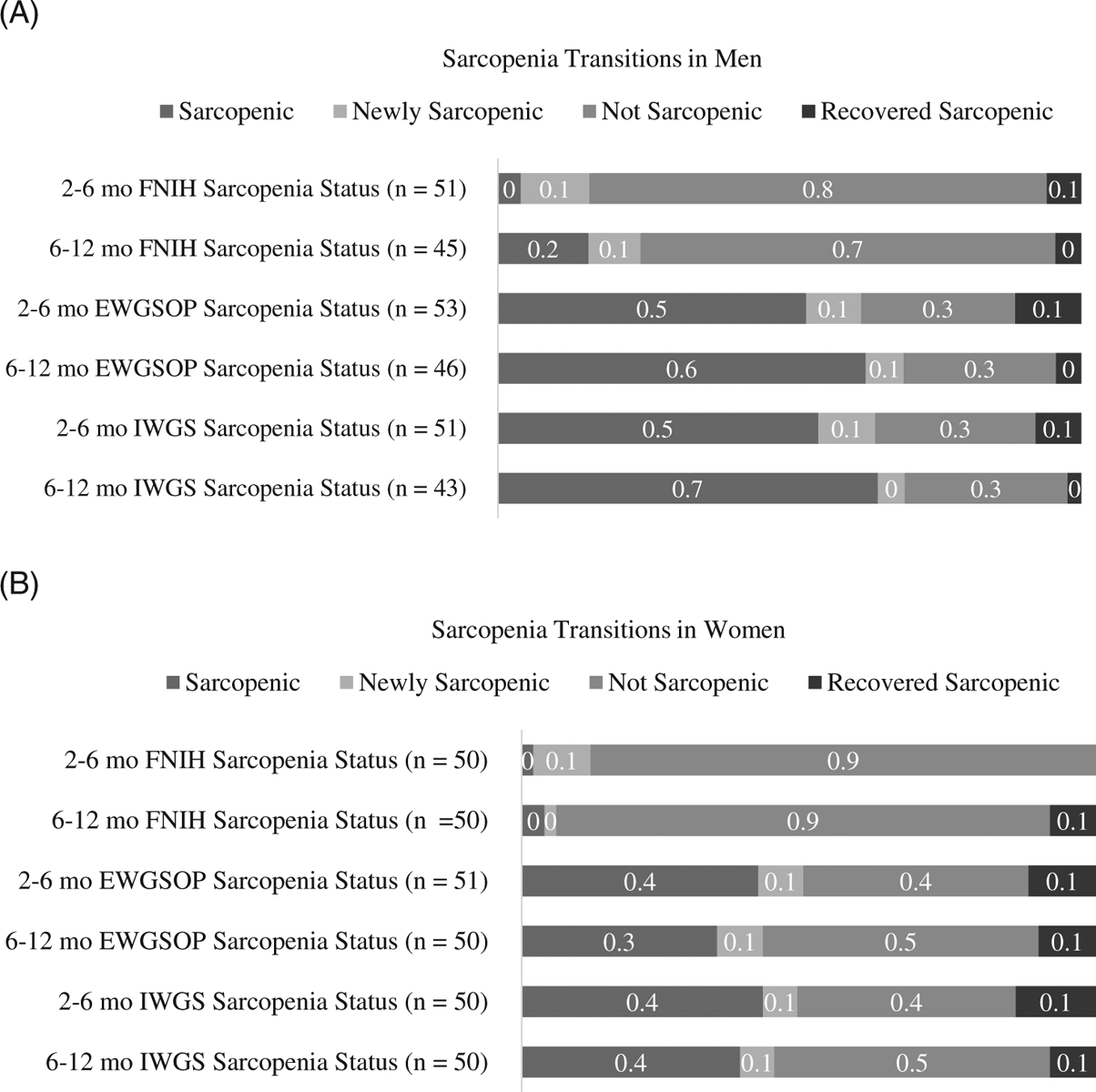
Sarcopenia transitions within the first year after hip fracture by definition. A, Men. B, Women. EWGSOP indicates European Working Group on Sarcopenia in Older Persons; FNIH, Foundations for National Institutes of Health; IWGS, International Working Group on Sarcopenia.
Sarcopenia status transitions for women are shown in Figure 3B. The following transitions were noted for FNIH: 10% changed (5/50; 6 newly sarcopenic, 0 recovered sarcopenic) between 2 and 6 months and 10% changed (5/50; 1 newly sarcopenic, 4 recovered sarcopenic) between 6 and 12 months. For IWGS, the corresponding values were 20% (10/50; 3 newly sarcopenic, 7 recovered sarcopenic) and 14% (7/50; 3 newly sarcopenic, 4 recovered sarcopenic) for 2 and 6 months and 6 and 12 months, respectively; for EWGSOP, the values were 20% (10/51; 4 newly sarcopenic, 6 recovered sarcopenic) and 18% (9/50; 4 newly sarcopenic, 5 recovered sarcopenic) for 2 and 6 months and 6 and 12 months, respectively.
DISCUSSION
We sought to examine the prevalence of sarcopenia in the year after hip fracture overall and by sex across three definitions, and whether sarcopenia prevalence changed over the year after hip fracture. Our findings suggest that the prevalence of sarcopenia among hip fracture patients differs by definition and persists over time in men. Where sex differences in sarcopenia exist, sarcopenia prevalence is higher in men than women. Recovery from sarcopenia in the year after hip fracture was low in both men and women.
The prevalence of sarcopenia for the EWGSOP and IWGS definitions, depending on time point, was 61% to 69% in men and 41% to 62% in women. For the FNIH definition, the prevalence was substantially lower, 15% to 20% in men and 5% to 13% in women. A systematic literature review by Cruz-Jentoft et al found that the prevalence of sarcopenia among community-dwelling older adults is between 1% and 29%.31 These estimates were obtained using the EWGSOP definition of sarcopenia. A pooled study by Dam et al found the prevalence of sarcopenia to be 5.3% (EWGSOP), 5.1% (IWGS), and 1.3% (FNIH) for men; among women, the prevalence was 13.3% (EWGSOP), 11.8% (IWGS), and 2.3% (FNIH).21 In comparison, our study found that the prevalence of sarcopenia is substantially higher among hip fracture patients.
Studies have reported a lower prevalence of sarcopenia by the FNIH definition compared to EWGSOP and IWGS in the general population, consistent with that observed in our hip fracture sample. The higher prevalence when using the EWGSOP or IWGS definition may be driven by slowness (gait speed <0.8 m/s or <1.0 m/s, respectively), which is not included in the FNIH definition of sarcopenia. In our hip fracture sample, over 90% of individuals met the EWGSOP or IWGS threshold for slowness. The FNIH definition uses more strict thresholds for weakness than EWGSOP; thus, fewer participants were identified as weak by the FNIH definition, despite this population recently experiencing a hip fracture. Additionally, a smaller proportion in our sample met the FNIH threshold for low lean mass (49% and 26% in men and women, respectively, for FNIH at 2 months vs 67% and 72% in men and women, respectively, for EWGSOP and IWGS at 2 months). While the FNIH definition was created to identify clinically meaningful weakness and low lean mass, it did not identify weakness and low lean mass in this population whom you would expect to be experiencing weakness and low lean mass after hip fracture. Different criteria may be necessary to identify older adults at greatest risk of disability after an acute event, such as a hip fracture, as opposed to the typical definitions of sarcopenia that were designed to identify those at greatest risk of functional decline in a general population of older persons.
Despite differing criteria, the EWGSOP and IWGS definitions had excellent agreement in our sample. EWGSOP and IWGS agreement with FNIH was poor. Dam et al found that among male older adults, FNIH has poor agreement with the IWGS (κ = 0.14) and fair to good agreement with EWGSOP (κ = 0.53).21 Among women, the agreement between FNIH and both IWGS (κ = 0.12) and EWGSOP (κ = 0.14) was poor21; however, agreement was better among men. We found no sex differences in agreement. We also observed weaker agreement between FNIH and both IWGS and EWGSOP, despite the higher prevalence of sarcopenia observed compared to the community-dwelling older adult population. Future studies will need to determine which definition is the most valid in a hip fracture population. Specifically, studies will need to examine the association between various measures of sarcopenia and outcomes of recovery.
Sarcopenia has been found to be more prevalent in women in the general, older adult population.21 However, in this study, prevalence was higher in men. This finding is consistent with several other studies in the literature.12,14–16,19 This sex difference is likely because men who fracture are typically sicker than women who fracture.12 In our sample, the number of comorbidities at baseline was significantly higher in male hip fracture patients.
Sarcopenia, regardless of definition used, persists over time among men, but small changes were seen among women. For EWGSOP and IWGS, sarcopenia peaked at 2 months after admission in women, while it peaked at 6 months for the FNIH definition. The FNIH definition was the only definition that showed an increase in sarcopenia over time (among women from 2 to 6 months). The lack of recovery in sarcopenia status over time may be because standard rehabilitation in the year after fracture has little impact on sarcopenia, or it may indicate that standard rehabilitation after fracture does not overcome aging-related losses of muscle and strength as the focus is more on eliminating disability in activities of daily living (ADLs) and instrumental ADLs than in increasing muscle mass and strength. Preliminary studies suggest that exercise may have beneficial effects on sarcopenia.32 However, it is difficult to make these conclusions without examining sarcopenia levels prefracture and/or immediately after fracture and in response to specific interventions designed to increase muscle mass and strength.
Another difficulty arises when considering the transitions in and out of sarcopenia that we observed over time. Although pairwise data were not available for the entire analytic sample, at adjacent time points between 7% and 20% of men and 10% and 20% of women had a change in sarcopenia status, inclusive of 0% to 10% of men and women becoming newly sarcopenic. Further study is needed to determine if changes in sarcopenia, either developing or resolving, impact clinical outcomes.33 Also, analyzing the characteristics of sarcopenic recoverers may provide insight on how to intervene and reverse sarcopenia after an acute event.
This study may be limited by its small sample size, and findings may not generalize to patients seen outside of metropolitan areas in Baltimore or elsewhere in the United States, where case mix and care practices are similar to those in the Baltimore region. The study population also is predominately white, with an average education consistent with some college education. Additionally, missing data prevented us from examining trends in sarcopenia outcomes for all subjects. Selection bias, including attrition bias, may be present if those who had sufficient data available to assess sarcopenia were healthier than those who did not. Additionally, in a population recovering from hip fracture, specific fracture-related issues may interfere with mobility and this can cause slow gait speed not related to sarcopenia. This challenge suggests that it may be more appropriate to use a sarcopenia definition that does not require gait speed to assess sarcopenia in a patient population prone to mobility issues. Despite some limitations, this study is the first to assess prevalence of sarcopenia longitudinally over the year after hip fracture in both men and women.
In conclusion, the prevalence of sarcopenia after fracture is higher than that of the general older adult population and shows little improvement over time, differs by sex, and is lowest by the FNIH definition. Future studies are needed to determine which definition of sarcopenia is most appropriate in a hip fracture population, as sarcopenia prevalence estimates were drastically different when comparing EWGSOP or IWGS estimates to FNIH estimates, and the EWGSOP recently updated their definition (EWGSOP2).34 Future research should also assess what role sarcopenia plays in recovery trajectories and how addressing deficits that define sarcopenia affect clinically relevant outcomes.
ACKNOWLEDGMENTS
Financial Disclosure: This work was supported by grants from the National Institute on Aging at the National Institutes of Health (grants: R37 AG09901 MERIT Award, R01 AG029315, T32 AG00262, and P30 AG028747).
Footnotes
Conflicts of Interest: Dr Hochberg has no conflicts of interest related to this article. During the past year, Dr Magaziner consulted or served on advisory boards for American Orthopedic Association, Novartis, UCB, and Pluristem. None of these entities provided funding for the current project.
Portions of the article were presented at the International Conference on Frailty and Sarcopenia Research in 2015 and Gerontological Society of America Annual Meeting in 2015.
Sponsorʼs Role: The sponsors had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript or in the review or approval of the manuscript.
REFERENCES
- 1.Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49(8):1458–1460. [DOI] [PubMed] [Google Scholar]
- 2.Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ III. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50(10):1644–1650. [DOI] [PubMed] [Google Scholar]
- 3.Bianchi L, Ferrucci L, Cherubini A, et al. The predictive value of the EWGSOP definition of sarcopenia: results from the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2016;71(2):259–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tarantino U, Baldi J, Scimeca M, et al. The role of sarcopenia with and without fracture. Injury. 2016;47:S3–S10. [DOI] [PubMed] [Google Scholar]
- 5.Morley JE, Baumgartner RN, Roubenoff R, Mayer J, Nair KS. Sarcopenia. J Lab Clin Med. 2001;137(4):231–243. [DOI] [PubMed] [Google Scholar]
- 6.Cruz-Jentoft A, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing. 2010;39(4):412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hairi NN, Cumming RG, Naganathan V, et al. Loss of muscle strength, mass (sarcopenia), and quality (specific force) and its relationship with functional limitation and physical disability: the Concord Health and Ageing in Men Project. J Am Geriatr Soc. 2010;58(11):2055–2062. [DOI] [PubMed] [Google Scholar]
- 8.Landi F, Liperoti R, Russo A, et al. Original article: sarcopenia as a risk factor for falls in elderly individuals: results from the ilSIRENTE study. Clin Nutr. 2012;31:652–658. [DOI] [PubMed] [Google Scholar]
- 9.Yu R, Leung J, Woo J. Incremental predictive value of sarcopenia for incident fracture in an elderly Chinese cohort: results from the Osteoporotic Fractures in Men (MrOs) Study. J Am Med Dir Assoc. 2014;15(8):551–558. [DOI] [PubMed] [Google Scholar]
- 10.Hong W, Cheng Q, Zhu X, et al. Prevalence of sarcopenia and its relationship with sites of fragility fractures in elderly Chinese men and women. PLoS One. 2015;10(9):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Monaco M, Castiglioni C, De Toma E, et al. Presarcopenia and sarcopenia in hip-fracture women: prevalence and association with ability to function in activities of daily living. Aging Clin Exp Res. 2015;27(4):465–472. [DOI] [PubMed] [Google Scholar]
- 12.Di Monaco M, Castiglioni C, Vallero F, Di Monaco R, Tappero R. Sarcopenia is more prevalent in men than in women after hip fracture: a cross-sectional study of 591 inpatients. Arch Gerontol Geriatr. 2012;55(2):e48–e52. [DOI] [PubMed] [Google Scholar]
- 13.González-Montalvo JI, Alarcón T, Gotor P, et al. Prevalence of sarcopenia in acute hip fracture patients and its influence on short-term clinical outcome. Geriatr Gerontol Int. 2016;16(9):1021–1027. [DOI] [PubMed] [Google Scholar]
- 14.Hida T, Ishiguro N, Shimokata H, et al. High prevalence of sarcopenia and reduced leg muscle mass in Japanese patients immediately after a hip fracture. Geriatr Gerontol Int. 2013;13(2):413–420. [DOI] [PubMed] [Google Scholar]
- 15.Ho AW, Lee MM, Chan EW, et al. Prevalence of pre-sarcopenia and sarcopenia in Hong Kong Chinese geriatric patients with hip fracture and its correlation with different factors. Hong Kong Med J. 2016;22(1):23–29. [DOI] [PubMed] [Google Scholar]
- 16.Landi F, Calvani R, Ortolani E, et al. The association between sarcopenia and functional outcomes among older patients with hip fracture undergoing in-hospital rehabilitation. Osteoporos Int. 2017;28(5):1569–1576. [DOI] [PubMed] [Google Scholar]
- 17.Ole MS, Clara GG, Bogen B, Målfrid HK, Lien G, Anette HR. Sarcopenia in patients with hip fracture: a multicenter cross-sectional study. PLoS One. 2017;12(9):e0184780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MAF S, Singh NA, Hansen RD, et al. Methodology and baseline characteristics for the sarcopenia and hip fracture study: a 5-year prospective study. J Gerontol A Biol Sci Med Sci. 2009;64A(5):568–574. [DOI] [PubMed] [Google Scholar]
- 19.Yoo JI, Ha YC, Kwon HB, Lee YK, Koo KH, Yoo MJ. High prevalence of sarcopenia in Korean patients after hip fracture: a case-control study. J Korean Med Sci. 2016;31(9):1479–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bijlsma A, Meskers C, Ling C, et al. Defining sarcopenia: the impact of different diagnostic criteria on the prevalence of sarcopenia in a large middle aged cohort. Age (Dordr). 2013;35(3):871–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dam T, Peters KW, Fragala M, et al. An evidence-based comparison of operational criteria for the presence of sarcopenia. J Gerontol A Biol Sci Med Sci. 2014;69(5):584–590. 10.1093/gerona/glu013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fielding RA, Vellas B, Evans WJ, et al. Special article: sarcopenia: an undiagnosed condition in older adults: current consensus definition: prevalence, etiology, and consequences. International Working Group on Sarcopenia. J Am Med Dir Assoc. 2011;12:249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69(5):547–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–1064. [DOI] [PubMed] [Google Scholar]
- 25.Orwig D, Hochberg MC, Gruber-Baldini A, et al. Examining differences in recovery outcomes between male and female hip fracture patients: design and baseline results of a prospective cohort study from the Baltimore hip studies. J Frailty Aging. 2018;7(3):162–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 27.Teng EL, Chui HC. The modified mini-mental state (3MS) examination. J Clin Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- 28.Rathbun AM, Shardell M, Orwig D, Hebel JR, Hicks GE, Beck T., … Magaziner J. Differences in the trajectory of bone mineral density change measured at the total hip and femoral neck between men and women following hip fracture. Archives of Osteoporosis, 2016;11(1). 10.1007/s11657-016-0263-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Armitage P, Colton T. Encyclopedia of Biostatistics. Vol 6 Hoboken, NJ: John Wiley & Sons; 1998. [Google Scholar]
- 30.Fleiss JL. Statistical Methods for Rates and Proportions. 2nd ed. New York, NY: Wiley; 1981. [Google Scholar]
- 31.Cruz-Jentoft A, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review: report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. 2014;43(6):748–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lozano-Montoya I, Correa-Pérez A, Abraha I, et al. Nonpharmacological interventions to treat physical frailty and sarcopenia in older patients: a systematic overview – the SENATOR Project ONTOP Series. Clin Interv Aging. 2017;12:721–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cawthon PM, Blackwell TL, Cauley J, et al. Evaluation of the usefulness of consensus definitions of sarcopenia in older men: results from the observational osteoporotic fractures in men cohort study. J Am Geriatr Soc. 2015;63(11):2247–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48(1):16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


