Abstract
We report 4 cases of post myocardial infarction complications due to the delay in presentation during COVID-19 era. We highlighted the need for auscultating the chest for early diagnosis. Through this case series, we urge to raise awareness among cardiac patients to access healthcare despite the fear of COVID-19.
Keywords: Ventricular septal rupture, Percutaneous repair, Acute coronary syndrome, COVID-19
1. Case #1
1.1. Medical history
A 68-year old female presented on 04/06/2020 with presyncope. A week ago, she developed right shoulder pain with radiation to her arm but did not seek medical attention due concerns for COVID-19 exposure. Initial vital signs on presentations were blood pressure of 143/38 mmHg, heart rate 82 bpm and saturating 95% on 4 L nasal canula.
1.2. Investigations
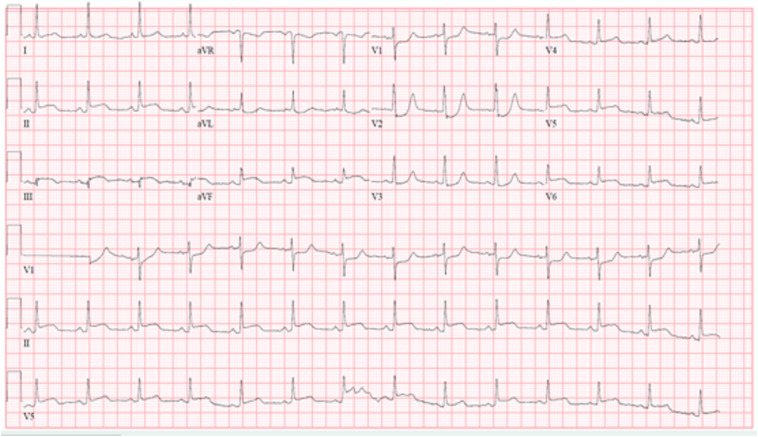
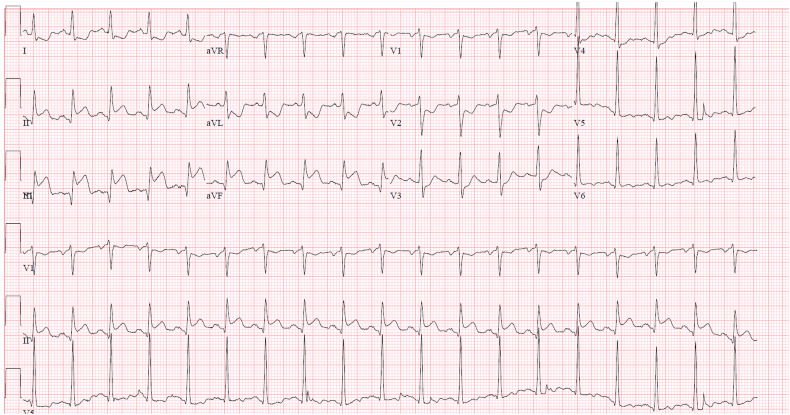
Electrocardiogram (EKG) was concerning for a posterior myocardial infarction (Fig. 1.1 ). Laboratory results showed troponin I of 4.42 ng/mL, serum lactic acid 8.4 mmol/L. COVID-19 PCR was negative. Bedside transthoracic echocardiogram showed a hyperdynamic left ventricle (LV), a large hemopericardium with signs of tamponade, and basal to mid posterior wall akinesis (Video 1).
Fig. 1.1.
Electrocardiogram (EKG) of Case #1 showing posterior myocardial infarction.
1.3. Management
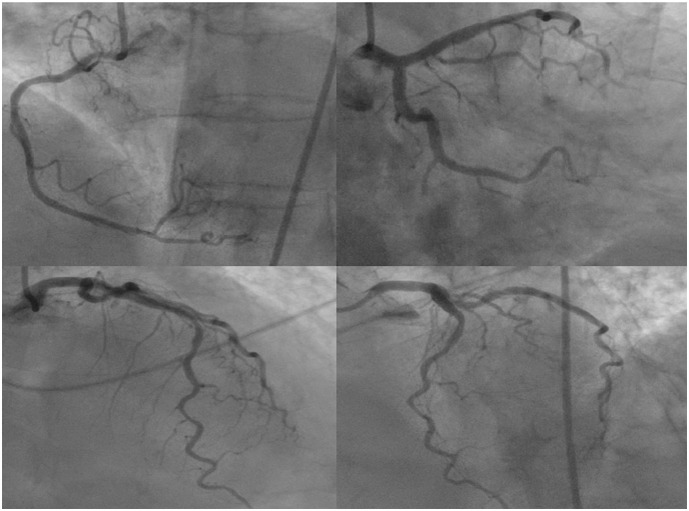
She subsequently became hypotensive and was started on norepinephrine drip after 2 L saline infusion. She was emergently taken to the cardiac catheterization laboratory where coronary angiography revealed a 100% occlusion of an inferior distal branch of a large second obtuse marginal (Fig. 1.2 ). Table 1 show the hemodynamics. An intra-aortic balloon pump (IABP) was placed. Due to concern for potential ventricular wall rupture secondary to late presenting posterior MI, patient was taken to the operative room emergently and underwent a subxiphoid pericardial window with evacuation of 700 mL of old clotted blood.
Fig. 1.2.
Angiogram of Case #1 showing occlusion of right posterolateral branch of right coronary artery.
Table 1.
Characteristics of case series patients.
| Case | Age (years) | Sex | Relevant comorbidities | Symptoms and signs | Hemodynamics | Length of hospitalization | Time from symptom onset to first medical contact | Final diagnosis |
|---|---|---|---|---|---|---|---|---|
| 1 | 68 | F | Hypertension Diabetes mellitus |
Lightheadedness Pre-syncope Shoulder pain |
LVEDP 20 mmHg RA 18 mmHg PA 32/19 (24) mmHg PCWP 18 mmHg Fick's CO/CI - 4.6 L/min/2.8 L/min/m2 |
10 days | 7 days | Ventricular free wall rupture |
| 2 | 72 | F | Hypertension Hyperlipidemia Chronic kidney disease Neurofibromatosis |
Shortness of breath Weakness Fall |
LVEDP 30 mmHg RA 14 mmHg PA 43/24 (31) mmHg PCWP 28 mmHg CO/CI 7.8 L/min/ 4.2 L/min/m2 Qp/Qs – 2.5 |
27 days | 4 days | Ventricular septal rupture |
| 3 | 53 | M | Hypertension Hyperlipidemia Obstructive sleep apnea |
Chest discomfort Shortness of breath Diaphoresis |
LVEDP 36 mmHg RA 10 mmHg PA 41/21 (32) mmHg PCWP 16 mmHg CO/ CI 2.4 L/min, 1.2 L/min/m2 Qp/Qs – 2.6 |
1 day | 5 days | Ventricular septal rupture |
| 4 | 72 | F | Hypertension | Shortness of breath | LVEDP 30 mmHg RA 10 mmHg PA 32/12 (19) mmHg PCWP 11 mmHg CO/CI 2.5 L/min, 1.3 L/min/m2 Qp/Qs: 2.8 |
14 days | 7 days | Ventricular septal rupture |
LVEDP – left ventricular end diastolic pressure. RA - right atrium. PA – pulmonary artery. CO – cardiac output. CI – cardiac index. Qp – pulmonary blood flow. Qs – systemic blood flow. Qp/Qs – shunt fraction. F – female. M – male.
1.4. Follow-up
Patient's hemodynamic status improved immediately. Norepinephrine and IABP were weaned off. Post- operative TTE showed LV ejection fraction (LVEF) of 35–40% with akinesis of the posterior wall. Pt was eventually discharged home on 04/14/2020.
2. Case #2
2.1. Medical history
A 72-year-old female presented on 04/15/2020 at a peripheral hospital with acute onset of weakness, shortness of breath followed by a mechanical fall. Prior to her presentation, patient reported four-day history of intermittent shortness of breath with exertion. Vital signs were stable except tachycardia. Physical exam was notable for a holosystolic murmur heard at the left lower sternal border and lungs were clear to auscultation.
2.2. Investigations
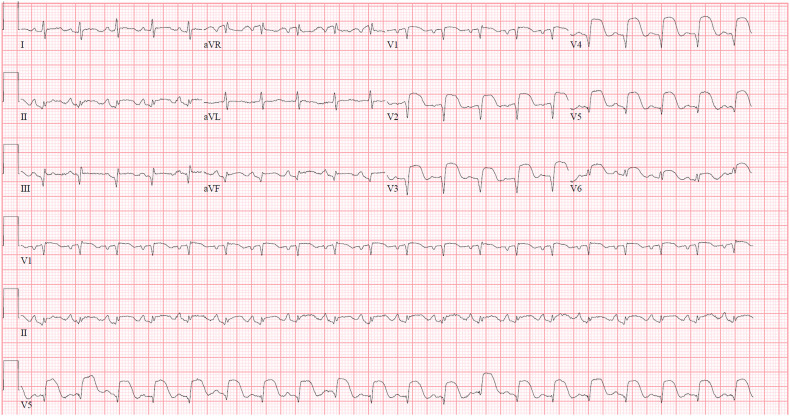
Initial EKG showed remote inferior infarct and anterolateral ST segment elevations (Fig. 2.1 ). Laboratory studies showed initial troponin I of 49.2 ng/mL, brain natriuretic peptide 2660 pg/mL, serum lactic acid of 7.3 mg/L, white blood count (WBC) 34,000/mL. COVID-19 PCR was negative.
Fig. 2.1.
Electrocardiogram (EKG) of Case #2 showing remote inferior infarct and acute anterolateral ST elevation infarction.
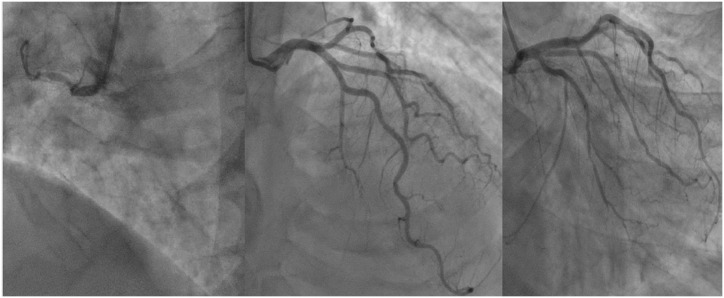
2.3. Management
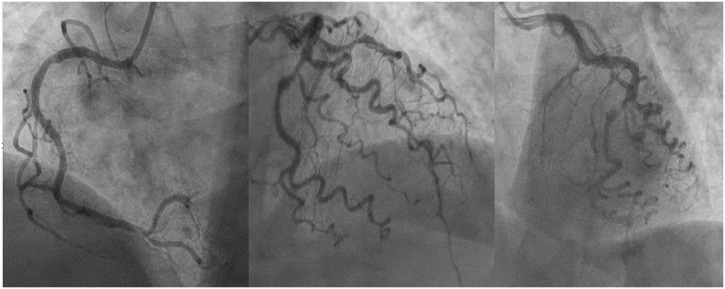
Patient was given aspirin, ticagrelor and heparin and was transferred to the tertiary care center cardiac catheterization laboratory emergently. Coronary angiography revealed serial 70% and 99% stenoses of the mid left anterior descending artery (LAD) (Fig. 2.2 ). Ventriculography showed LVEF 30% with antero-apical and apical akinesis and evidence of a distal ventricular septal rupture (VSD). Hemodynamics are shown in Table 1. An IABP was inserted for hemodynamic support and cardiac surgery were consulted for VSD repair. TTE obtain showed LVEF 45% with distal LAD territory hypokinesis to akinesis with a distal non-restrictive VSD with left to right shunting (Video 2). Patient underwent a VSD repair with a polytetrafluoroethylene (PTFE) over collage-impregnated Dacron Hemashield patch with intra-operative echocardiogram showing residual small restrictive VSD. Post operatively, patient developed worsening cardiogenic shock requiring vasopressor and inotropic support over a period of 2 weeks. Repeat TTE after 2 weeks showed persistent leak around the repair site.
Fig. 2.2.
Angiogram of Case #2 showing serial 70% and 99% stenoses of the mid left anterior descending artery.
2.4. Follow-up
Given worsening hemodynamics, patient underwent a percutaneous closure of VSD using a 16 mm Amplatzer® post infarct VSD occluder after sizing it. Follow up TTE showed persistent left to right shunt suggestive of VSD despite it appearing relatively smaller than before. Patient's clinical status continued to deteriorate with increasing need for hemodynamic support and evidence of multiorgan failure over the course of next week. Care was withdrawn by the family after another week of supportive management and patient expired on 05/12/2020.
3. Case #3
3.1. Medical history
A 53-year-old male presented on 05/30/2020 with 5-day history of progressively worsening chest pain, shortness of breath and diaphoresis. Vital signs were stable. Physical examination was notable for a holosystolic murmur with radiation to the apex.
3.2. Investigations
EKG showed sinus tachycardia, with ST segment elevations in the inferior leads and reciprocal depressions in the lateral leads (Fig. 3.1 ). Laboratory studies were significant for troponin I of 6.56 ng/mL and negative COVID-19 PCR.
Fig. 3.1.
Electrocardiogram (EKG) of Case #3 showing acute inferior ST elevation infarction.
3.3. Management
Patient was given aspirin, ticagrelor and heparin and transferred emergently to the tertiary care center cardiac catheterization laboratory. Coronary angiography revealed a 100% proximal RCA occlusion with left to right collaterals (Fig. 3.2 ). Ventriculogram showed an LVEF of 35% and distal ventricular septal rupture. Table 1 shows hemodynamics. TTE showed EF of 65–70% with large apical muscular ventricular septal defect with left to right shunting (Video 3). Patient was taken emergently for surgical repair of VSD with 2 Dacron patches. While taking the patient off cardiac bypass, patient developed significant bleeding from tears in the inferior wall of left ventricle.
Fig. 3.2.
Angiogram of Case #3 showing proximal RCA occlusion with left to right collaterals.
3.4. Follow-up
Due to persistent bleeding, patient expired while in the operation room.
4. Case #4
4.1. Medical history
A 72-year-old female presented to a peripheral hospital with 2 days of shortness of breath. Patient reported symptoms of chest pain 1 week prior to arrival. Her initial vitals were unstable. She was transferred to tertiary care center for further care.
4.2. Investigations
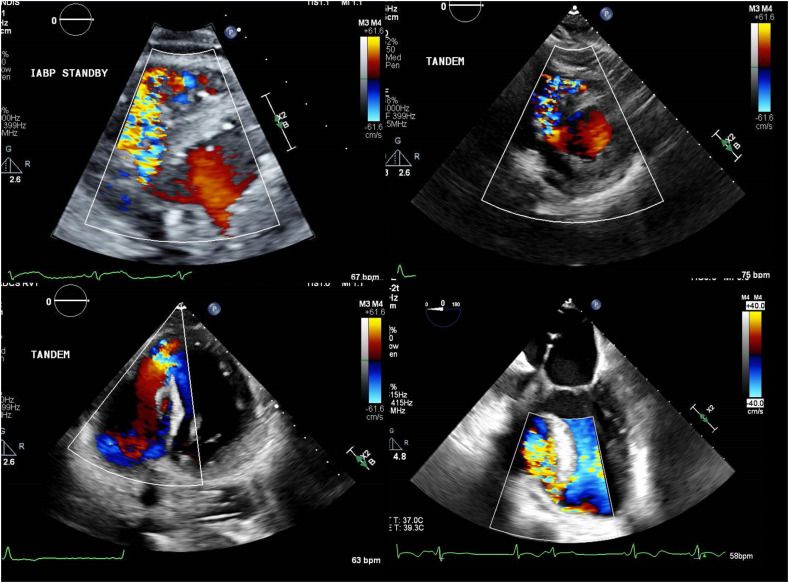
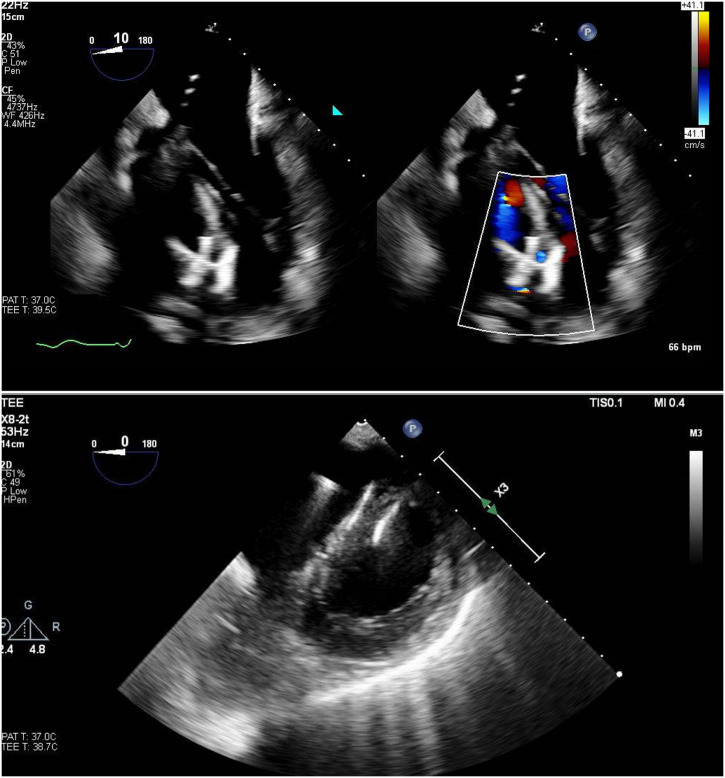
COVID PCR was negative. Upon arrival, the patient had severe lactic acidosis (ABG = pH 7.05 mmHg, pO2 134 mmHg, pCO2 18, bicarbonate 5 meq/L, lactic acid >12 mg/dL), was on BiPAP but was still following commands. Shortly after arrival, an IABP was placed at bedside and she was emergently intubated in lieu of poor oxygenation. During this process, the patient had a pulseless electrical activity arrest requiring several rounds of cardiopulmonary resuscitation before achieving return of spontaneous circulation. TTE (Fig. 4.1 ) showed a serpiginous mid-apical infero-septal VSD; LVEF 40–45% with regional wall motion abnormalities consistent with recent anterior MI.
Fig. 4.1.
Transthoracic echocardiogram of Case #4 showing serpiginous mid-apical infero-septal ventricular septal rupture.
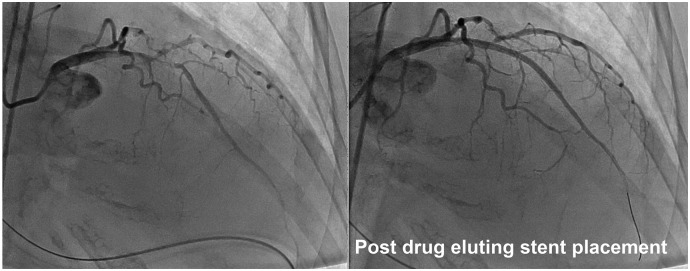
4.3. Management
The patient was brought to the catheterization lab urgently and was found to have a severely stenotic LAD artery with evidence of thrombus. The patient underwent successful stenting of the LAD artery with two drug eluting stents aided by aspiration thrombectomy (Fig. 4.2 ). This improved the flow from TIMI 0 to TIMI 2. At this stage, due to severe cardiogenic shock, the patient was supported with TandemHeart® percutaneous left ventricular assist device. Table 1 shows hemodynamics. After a week of care, patient underwent percutaneous closure of the VSD with 25 mm Amplatzer® Cribriform device. Transesophageal echocardiography showed no significant shunting thereafter (Fig. 4.3 ).
Fig. 4.2.
Coronary angiogram of Case #4 showing pre and post stenting of left anterior descending artery stenosis.
Fig. 4.3.
Transesophageal echocardiography of Case #4 showed no significant shunting after ventricular septal rupture repair.
4.4. Follow-up
Unfortunately, the hospital course was complicated by sepsis and multi-system organ failure, the patient expired approximately 2 weeks after VSD closure device implantation.
5. Discussion
The novel coronavirus 2 (SARS-CoV2), is a viral disease that leads to severe respiratory syndrome termed coronavirus disease 2019 (COVID-19) that has affected more than 10 million people and has killed more than half a million worldwide [1]. Several measures including social distancing and #stayhome campaigns are being run. However, due to COVID-19, nearly half of the public (48%) has delayed their health care as found by Kaiser Family Foundation poll [2]. In the pre percutaneous coronary intervention era, the incidence of free wall rupture was 6%, papillary muscle rupture was 2% and ventricular septal defect was 2% [3]. The incidences of all these complications decreased to 0.2% in the post PCI era and is rarely witnessed in areas where PCI is readily available [4,5].
An important aspect of this case series was that there was already a suspicion of VSD in two of these cases because of the physical examination finding of murmur prior to arrival to the cardiac catheterization lab. It is important to auscultate these patients prior to bringing to the catheterization laboratory as it may impact the follow up management. Though a small case series, this rapid increase in post MI complications cases in less 2 months at these institutions highlights the “unmeasured” toll and impact of COVID-19 on patients during this pandemic. This further highlights the crucial role that cardiologists could play in educating patients to recognize and seek medical help for their cardiovascular symptoms.
6. Conclusion
Post MI complications have high morbidity and mortality. Early identification may impact the outcomes and patients should be encouraged to seek health care for their cardiovascular symptoms during COVID pandemic.
The following are the supplementary data related to this article.
Transthoracic echocardiogram of Case #1 showing pericardial clot.
Transthoracic echocardiogram of Case #2 showing ventricular septal rupture.
Transthoracic echocardiogram of Case #3 showing ventricular septal rupture.
Declaration of competing interest
The authors have nothing to disclose. This manuscript is an original effort that has not been submitted or is under consideration for publication elsewhere. All co-authors have contributed substantially to the manuscript preparation and are wholly responsible for the manuscript content without any associated conflicts of interest or financial incentives.
References
- 1.Johns Hopkins Coronavirus Resource Center . 2020. Covid-19 dashboard by the center for systems science and engineering (csse) at johns hopkins university. [Google Scholar]
- 2.Kaiser Family Foundation Impact of coronavirus on personal health,economic and food security, and medicaid. 2020. https://www.kff.org/report-section/kff-health-tracking-poll-may-2020-health-and-economic-impacts/
- 3.Bajaj A., Sethi A., Rathor P., Suppogu N. Acute complications of myocardial infarction in the current era: diagnosis and management. J Inves Med. 2015;63:844–855. doi: 10.1097/JIM.0000000000000232. [DOI] [PubMed] [Google Scholar]
- 4.Figueras J., Alcalde O., Barrabes J.A., Serra V., Alguersuari J., Cortadellas J., et al. Changes in hospital mortality rates in 425 patients with acute st-elevation myocardial infarction and cardiac rupture over a 30-year period. Circulation. 2008;118:2783–2789. doi: 10.1161/CIRCULATIONAHA.108.776690. [DOI] [PubMed] [Google Scholar]
- 5.Elbadawi A., Elgendy I.Y., Mahmoud K., Barakat A.F., Mentias A., Mohamed A.H., et al. Temporal trends and outcomes of mechanical complications in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2019;12:1825–1836. doi: 10.1016/j.jcin.2019.04.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiogram of Case #1 showing pericardial clot.
Transthoracic echocardiogram of Case #2 showing ventricular septal rupture.
Transthoracic echocardiogram of Case #3 showing ventricular septal rupture.