Abstract
Background
Coronavirus disease-2019 (COVID-19) is a novel disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) that rapidly spread around the globe. The dramatic increase in the number of cases and deaths have placed tremendous strain on health care systems worldwide. As health care workers and society adjust to focus treatment and prevention of COVID-19, other facets of the health care enterprise are affected, particularly surgical volume and revenue. The purpose of this study was to describe the financial impact of COVID-19 on an academic neurosurgery department.
Methods
A retrospective review of weekly average daily work relative value units (wRVUs) were compared before and after COVID-19 in the fiscal year 2020. A comparative time period of the same months in the year prior was also included for review. We also review strategies for triaging neurosurgical disease as needing emergent, urgent, or routine operative treatment.
Results
Daily average wRVU after COVID-19 dropped significantly with losses in all weeks examined. Of the 7 weeks in the current post-COVID period, the weekly daily average wRVU was 173 (range, 128–363). The mean decline was 51.4% compared with the pre-COVID era. Both inpatient and outpatient revenue was affected.
Conclusions
COVID-19 had a profound detrimental effect on surgical productivity and revenue generation.
Key words: COVID-19, Health economics, Relative value unit
Abbreviations and Acronyms: AANS/CNS, American Association of Neurological Surgeons and Congress of Neurological Surgery; ACS, American College of Surgeons; CMS, Centers for Medicare and Medicaid Services; COVID-19, Coronavirus disease-2019; DRG, Diagnosis-related groups; RVU, Relative value unit; SARS-CoV-2, Severe acute respiratory syndrome coronavirus-2; UW, University of Washington; wRVU, Work relative value unit
Introduction
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is a novel coronavirus first detected in Wuhan, China in 2019. The World Health Organization declared a global pandemic in March 2020, and coronavirus disease-2019 (COVID-19) has resulted in over 5.5 million cases and approximately 350,000 deaths worldwide as of May 25, 2020.1 , 2 The first reported case in the United States occurred on January 19, 2020 in the state of Washington. Washington state has seen 21,349 cases and 1118 deaths as of April 29, 2020.3 Recently published data from Seattle health care systems estimate that half of those with COVID-19 admitted to an intensive care unit will die.4
Recent epidemics and pandemics, such as SARS, Swine Flu, and Ebola, have tested the capacity of health care systems worldwide.5 Historically, the largest of these pandemics, such as the bubonic plague, smallpox, and the Spanish Flu, took the lives of upward of 300 million people combined.5 In early 2020, the economic and financial impact of COVID-19 in the United States began to rapidly manifest itself as a complex phenomenon and encompassed every aspect of the American economy. In the health care industry, the virus induced a paradoxical increase in resource utilization, but decrease in productivity and revenue.6 , 7
The complete economic impact of COVID-19 on health care systems and the global economy will take time to fully evaluate. Early estimates from the Medical Group Management Association8 suggest that 97% of practices in their 724 practice survey experienced a negative financial impact either directly or indirectly associated with the virus. Practices also reported an average of 55% decrease in revenue and a 60% decrease in patient volume since the beginning of the COVID-19 crisis.8 To date, to our knowledge, there has been no published literature on the financial impact of the COVID-19 virus on surgical productivity and revenue. This report summarizes our experiences at the University of Washington (UW) Department of Neurological Surgery, in one of the first health care systems to directly confront this pandemic in the United States.
Methods
A retrospective review of our institutional case volume was conducted during the period of December 29, 2019 to May 1, 2020. The data included operative volume from the UW Medical Center and Harborview Medical Center, 2 of 4 entities comprising the UW Medicine hospital system (the others being Valley Medical Center and UW Northwest Hospital). Data were extracted from the billing records of our financial department. The total work relative value units (wRVUs) were measured, and wRVU variance was also calculated. The immediate pre-COVID comparative period was defined as January 1, 2020 through March 15, 2020. The post-COVID period in which stringent limits on elective cases were imposed began on March 16, 2020. A review of the total monthly relative value units (RVUs) for March, April, and May of 2019 were used for comparison. At our institution, COVID-19 operative restrictions involved limiting cases to the following: neurotrauma, acute stroke, subarachnoid hemorrhage, acutely worsening myelopathy, cauda equina, and neurooncology (Table 1 ). The breakdown between inpatient and outpatient services in terms of wRVUs was also examined.
Table 1.
University of Washington Medicine Guidelines for the Acuity and Management of Neurosurgical Disease
| Trauma | Vascular | Oncologic | Spine | Others | |
|---|---|---|---|---|---|
| Emergent (must be managed as soon as possible) | Traumatic brain injury with mass lesions (e.g., epidural/subdural hematoma), intraparenchymal hemorrhages, penetrating brain injuries, invasive ICP monitoring | Aneurysmal subarachnoid hemorrhages, ruptured arteriovenous malformations, acute ischemic strokes | Brain or spinal cord tumors causing acute neurologic decline (e.g., posterior fossa tumors, pituitary apoplexy) | Spine trauma causing neurologic deficit, spinal cord injury, unstable spine fractures | Acute hydrocephalus due to tumors, mass lesions, shunt malfunctions |
| Urgent (should be managed within 3 weeks) | Subacute-to-chronic subdural hematomas | Malformations causing neurologic symptoms (e.g., focal deficit, seizures, etc.) | Brain or spinal cord tumors causing progressive neurologic decline (e.g., malignant glioma, skull base tumors causing brainstem compression, sellar/suprasellar tumors causing visual decline) | Spine trauma without neurologic deficit, degenerative conditions causing significant pain, and/or progressive neurologic deficit, mechanical instability | Functional procedures with replacement of existing hardware at end-of-life |
| Routine (can be postponed indefinitely) | Cranioplasty | Unruptured aneurysms without high-risk features, unruptured arteriovenous malformations | Benign, slow-growing tumors without significant neurologic decline (e.g., vestibular schwannoma, meningiomas) | Degenerative conditions causing pain without neurologic deficit | Functional procedures requiring new hardware implantation (e.g., DBS, pumps) |
ICP, intracranial pressure; DBS, deep brain stimulation.
Results
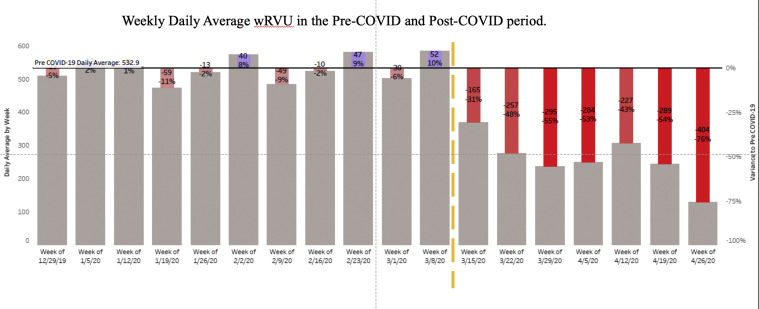
There was a total of 11 weeks in the pre-COVID period since the beginning of the 2020 fiscal year. The pre-COVID weekly daily average wRVU was 533.1, ranging from 474 to 582 (–11% to +10% variance). Of the 7 weeks in the current post-COVID period, the weekly daily average wRVU was 173, ranging from 363 to 128 (–31% to –76% variance) (Figure 1 ). The total number of wRVU performed in the month of March and April during COVID-19 was 12,540 and 7013, respectively. For comparison, wRVU data were queried for the months of March and April in the fiscal year 2019. The total wRVU for March and April 2019 was 11,587 and 11,880, respectively. This represents a 17% decline in total wRVU from the year prior during these 2 months.
Figure 1.
Daily average work relative value units (wRVUs) by week during the fiscal year 2020. The yellow dashed line indicates the start of COVID-19 surgical restrictions. The black solid line indicates the pre-COVID daily average wRVU of 532.9. Weekly average daily wRVUs are plotted as a variance of that average value.
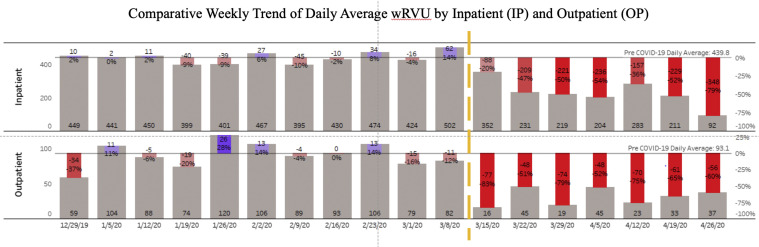
Data were further analyzed by separating inpatient and outpatient weekly daily average wRVU (Figure 2 ). The inpatient pre-COVID daily average was 439.8, ranging from 395–449 (–10% to +14% variance). The post-COVID inpatient daily average was 227, ranging from 92–283 (–79% to –36% variance). The outpatient daily average wRVU was 93.1 in the pre-COVID time, ranging from 59 (–37% variance) to 120 (+30% variance). The post-COVID outpatient daily average wRVU ranged from 16 to 45 (–83% to –52% variance) with a mean of 23.3.
Figure 2.
Weekly daily average work relative value units (wRVUs) are plotted by week. The yellow dashed line indicates the start of the COVID-19 surgical restrictions. Inpatient and outpatient data are separated. Gray solid line indicates pre-COVID daily average of 439.8 for inpatient and 93.1 for outpatient. Weekly average daily wRVUs are plotted as a variance of that average value.
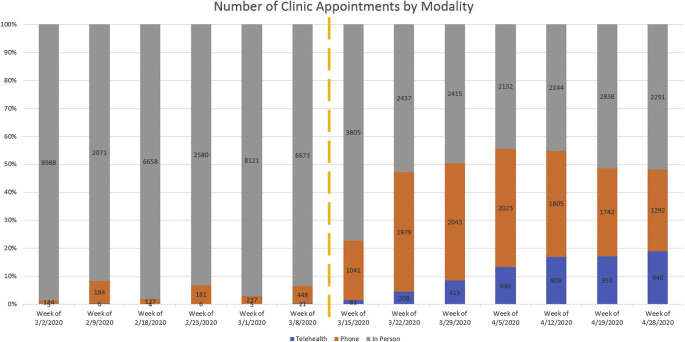
Outpatient visit data were examined for utilization of services (Figure 3 ). At UW, outpatient services were rendered as either in-person clinical visits, telehealth visits via teleconference, or telephone visits. Before COVID-19 the overwhelming majority of clinic appointments occurred in person ranging from 6673 (93%) to 8988 (99%) per week. Telephone visits represented no more than 6% of all visits, and likewise telehealth represented no more than 2% of all visits in the pre-COVID period. In the post-COVID period, there was a significant decline in the number of in-person clinic visits and a transition to increased utilization of telehealth. In-person visits ranged from 2132 (44%) to 3805 (77%) per week. Telephone and telehealth visits, however, ranged from 81 (2%) and 1041 (25%) to 953 (17%) and 2025 (42%) per week, respectively.
Figure 3.
Total number of clinic appointments are plotted by week. Gray represents in-person visits, orange represents telephone visits, and blue represents telehealth (teleconference) visits. The yellow dashed line indicates the start of the COVID-19 surgical restrictions.
Discussion
Economists and public health personnel have produced models for studying economic impact of pandemics.9 , 10 Rapid changes in the delivery and costs of health care, public policy changes, and societal behavioral changes during a pandemic make modeling challenging.
The financing of health care in the United States includes private health insurance and public funding through Medicare/Medicaid. In this system, a so-called “cost-shift hydraulic” exists in which one payor group (usually private health insurers) pay substantially higher prices to offset lower prices paid by another payor group (usually the government or out-of-pocket payers). During a large-scale pandemic in which there is a drop in the gross domestic product and increased unemployment, there is a shift from employment-based private financing to public health care and/or being uninsured.11
In addition to the macroeconomics of public health, an understanding of the microeconomics of physician reimbursement and hospital finance is required.12 , 13 Physician reimbursement can be separated into 3 parts: coding for procedures, coding for diagnoses, and Centers for Medicare and Medicaid Services (CMS) determination of reimbursement. Procedural coding is accomplished by the Current Procedural Terminology,14 which is a proprietary uniform coding system developed by the American Medical Association. RVUs are the primary driver for physician reimbursement. The RVU consists of several subcomponents, including a wRVU (estimating physician work), practice expense RVU, and a malpractice expense RVU. These component RVUs are multiplied by the geographic practice cost index, which is intended to be an adjustment for geographic differences in cost of care.
Hospitals are reimbursed for inpatient care based on diagnosis-related groups (DRG).15 Every inpatient admission is classified into a DRG that is based on diagnosis, complications, and comorbidities associated with each patient. This is different from ICD coding in that a patient can have multiple ICD codes (e.g., diagnoses) but can only have 1 DRG (e.g., reason for admission). The compensation that CMS provides hospitals is based on this calculated DRG multiplied by the federal operating rate and a geographic adjustment factor, as well as a series of modifiers. Uncomplicated cases, with fewer services utilized, are more lucrative than complex cases that utilize more resources. Similarly, DRGs for many elective surgeries result in net profits for the hospitals. In the case of a pandemic in which there is high resource utilization with complex care and concomitant sharp decrease in elective and otherwise uncomplicated medical care, the mathematics are not favorable.
Surgical practices nationally and internationally were significantly affected by this pandemic. Perhaps the greatest impact was in the postponement of elective surgeries. Different national entities have published guidelines on elective case scheduling during a pandemic, including the American College of Surgeons (ACS)16 and the CMS.17 The ACS guidelines were broad, stating that all elective surgeries and elective inpatient diagnostic procedures should be postponed. In addition, they recommended limiting visitors to known COVID-19-positive patients and surge planning with reorganization of hospital resources. The CMS proposed a 3-tiered algorithm in which low-acuity services were postponed or accomplished via telehealth, intermediate-acuity services (wherein not providing the service has the potential for increasing morbidity or mortality) were triaged, and high-acuity services (lack of in-person treatment or service would result in patient harm) would proceed as normal.
The joint American Association of Neurological Surgeons and Congress of Neurological Surgery (AANS/CNS)18 Tumor Section published their own guidelines owing to the unique nature of neurooncologic disease. They advocated for urgent surgical intervention for all newly diagnosed high-grade gliomas and cranial or spinal metastatic disease. They were proponents of close observation of low-grade gliomas and benign asymptomatic lesions. Tumors that caused hydrocephalus or visual loss were generally considered urgent but they suggested a case-by-case evaluation. Several institutions and multiinstitutional cohorts published their guidelines as well. The University of California San Francisco group published their algorithm,19 which considered the disease burden with surge level. In their model, with increased surge level there was a progressive decrease in elective cases and transfers. They also published a standardized protocol for authorizing elective surgery during the outbreak.
A multiinstitutional group also published guidelines on the urgency of specific procedures related to spine pathologies.20 Risk of permanent and/or potentially reversible serious neurologic dysfunction, new and progressive foot drop or hand weakness, acute cauda equina, progressive myelopathy, and a very select group of patients in severe pain met the requirement for expedited treatment. A recent international review of the effect of COVID-19 on neurosurgery has been published.21 In their survey of 147 respondents from 96 countries the authors found that 57.5% of respondents in private practice and 51.9% of respondents in governmental practice experienced cancellation of all elective procedures. A total of 27.9% of private and 31.8% of governmental respondents experienced reduction of 50%–99% of all elective surgical volume. Likewise, outpatient clinic appointments were cancelled without rescheduling in 47.6% of respondents. Interestingly, only 29.9% of respondents endorsed using some form of telemedicine. Although their article did not specify numeric losses, they did say that 62.5% of respondents experienced significant financial burden.
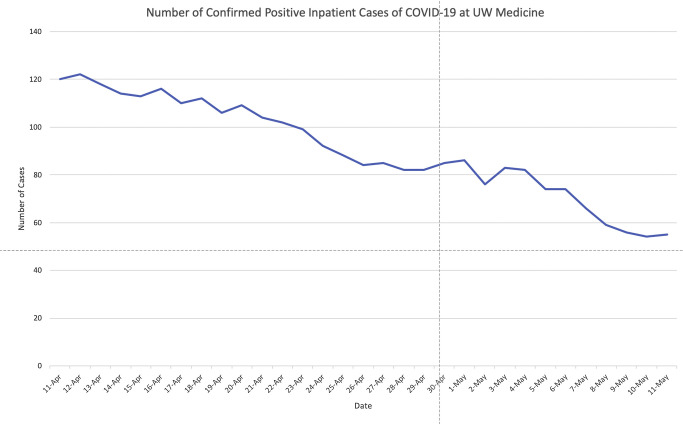
In our review, COVID-19 had a significant impact on our department’s surgical productivity with total wRVU production decreased as much as 75%. The effect was immediate with the initial week after COVID-19 restrictions seeing reduction in both inpatient (29%) and outpatient (85%) wRVUs. The inpatient decline is, as predicted, linear as increasing restriction on elective surgical volume caused increasingly lower wRVUs. This also corresponded to a decrease in hospital occupancy from 98%–68% within the first few weeks of the pandemic. The outpatient wRVU decline was seen in the months leading up to the operating room freeze, however, there was an increase in the second week. We believe the initial prelude to the sharper decline to be because of the effect of public fear in response to the local outbreak of the virus,22 with a subsequent increase in wRVU in the following week. On March 23, 2020, Washington state faced the institution of a statewide stay-at-home mandate,23 which again significantly decreased our outpatient productivity. This corresponded to the peak of inpatient COVID cases (Figure 3). In response to this mandate, telemedicine was instituted. Our hospital system embraced the use of telehealth (both video and telephone call), which likely mitigated outpatient losses (Figure 4 ).
Figure 4.
Total number of positive inpatient cases of COVID-19 across all University of Washington Medicine hospitals are plotted by date.
This study is limited in that is represents an incomplete assessment of the total financial impact of COVID-19, which will likely not be completely appreciable until many months after normal operations has resumed. Additionally, although they are familiar and easy to understand, wRVUs represent just a component of the true costs and revenue in a health care system.
Conclusions
In this preliminary analysis, COVID-19 had a significant detrimental impact on surgical volume and revenue generation with up to 76% loss of wRVU with a mean weekly wRVU loss of 51%. This effect was seen in both inpatient and outpatient care, with up to 79% loss of inpatient wRVU and up to 83% loss of outpatient wRVU. These data, however, are not complete as follow-up studies in time are needed to fully elucidate the full financial effect of the virus.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.IMHE COVID-19 projections. https://covid19.healthdata.org/united-states-of-america Available at: Accessed January 7, 2020.
- 2.Johns Hopkins Coronavirus Resource Center COVID-19 United Staes cases by county. https://coronavirus.jhu.edu/us-map Available at: Accessed January 7, 2020.
- 3.Washington State Department of Health 2019 Novel coronavirus outbreak (COVID-19) https://www.doh.wa.gov/Emergencies/Coronavirus Available at: Accessed January 7, 2020.
- 4.Bhatraju P.K., Ghassemieh B.J., Nichols M., et al. Covid-19 in critically ill patients in the Seattle region—case series. N Engl J Med. 2020;382:2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LePan N. Visualizing the history of pandemics. https://www.visualcapitalist.com/history-of-pandemics-deadliest/ Available at:
- 6.Bebinger M. COVID-19 hits some health care workers with pay cuts and layoffs. https://www.npr.org/sections/health-shots/2020/04/02/826232423/covid-19-hits-some-health-care-workers-with-pay-cuts-and-layoffs Available at: Accessed January 7, 2020.
- 7.Eldred S.M. Firings, furlloughs and pay cuts in advance of COVID-19 surge. https://www.medscape.com/viewarticle/927897 Available at: Accessed January 7, 2020.
- 8.Medical Group Management Association COVID-19 financial impact on medical practices. https://www.mgma.com/getattachment/9b8be0c2-0744-41bf-864f-04007d6adbd2/2004-G09621D-COVID-Financial-Impact-One-Pager-8-5x11-MW-2.pdf.aspx?lang=en-US&ext=.pdf Available at: Accessed January 7, 2020.
- 9.Meltzer M.I., Cox N.J., Fukuda K. The economic impact of pandemic influenza in the United States: priorities for intervention. Emerg Infect Dis. 1999;5:659–671. doi: 10.3201/eid0505.990507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murray C.J. Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. https://doi.org/10.1101/2020.03.27.20043752 [e-pub ahead of print]. medRxiv. accessed January 7, 2020.
- 11.Matheny J., Toner E., Waldhorn R. Financial effects of an influenza pandemic on US hospitals. J Health Care Finance. 2007;34:58–63. [PubMed] [Google Scholar]
- 12.Economic and social impact of epidemic and pandemic influenza. Vaccine. 2006;24:6776–6778. doi: 10.1016/j.vaccine.2006.06.072. [DOI] [PubMed] [Google Scholar]
- 13.Beck D.E., Margolin D.A. Physician coding and reimbursement. Ochsner J. 2007;7:8–15. [PMC free article] [PubMed] [Google Scholar]
- 14.American Medcial Association CPT (Current Procedural Terminology) https://www.ama-assn.org/amaone/cpt-current-procedural-terminology Available at: Accessed January 7, 2020.
- 15.Rimler S.B., Gale B.D., Reede D.L. Diagnosis-related groups and hospital inpatient federal reimbursement. Radiographics. 2015;35:1825–1834. doi: 10.1148/rg.2015150043. [DOI] [PubMed] [Google Scholar]
- 16.American College of Surgeons COVID-19: recommendations for management of elective surgical procedures. https://www.facs.org/covid-19/clinical-guidance/elective-surgery Available at: Accessed January 7, 2020.
- 17.Centers for Medicare and Medicaid Services Non-emergent, elective medical services, and treatment recommendations. https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf Available at:
- 18.Ramakrishna R., Zadeh G., Sheehan J.P., Aghi M.K. Inpatient and outpatient case prioritization for patients with neuro-oncologic disease amid the COVID-19 pandemic: general guidance for neuro-oncology practitioners from the AANS/CNS Tumor Section and Society for Neuro-Oncology. J Neurooncol. 2020;147:525–529. doi: 10.1007/s11060-020-03488-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burke J.F., Chan A.K., Mummaneni V., et al. Letter: The coronavirus disease 2019 global pandemic: a neurosurgical treatment algorithm. Neurosurgery. 2020;87:E50–E56. doi: 10.1093/neuros/nyaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghogawala Z., Kurpad S., Falavigna A., et al. Editorial. COVID-19 and spinal surgery. J Neurosurg Spine. 2020;33:1–3. doi: 10.3171/2020.4.SPINE20468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El-Ghandour N.M.F., Elsebaie E.H., Salem A.A., et al. Letter: The impact of the coronavirus (COVID-19) pandemic on neurosurgeons worldwide. Neurosurgery. 2020;87:E250–E257. doi: 10.1093/neuros/nyaa212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNerthney C. Coronavirus in Washington state: a timeline of the outbreak through March 2020. https://www.kiro7.com/news/local/coronavirus-washington-state-timeline-outbreak/IM65JK66N5BYTIAPZ3FUZSKMUE/ Available at: Accessed January 7, 2020.
- 23.Inslee J. Proclamation by the Governor Amending Proclamation 20-05. https://www.governor.wa.gov/sites/default/files/proclamations/20-25%20Coronovirus%20Stay%20Safe-Stay%20Healthy%20%28tmp%29%20%28002%29.pdf Available at: Accessed January 7, 2020.