Abstract
Objective:
Despite overall improvements in the U.S. health care, older adults living in rural counties, such as Appalachian Virginia, continue to be underserved.
Method:
Multinomial regression models, including both individual and county data from 503 older adults aged 65+, were used to examine factors associated with informal and formal care use.
Results:
Older adults with stronger filial beliefs and less positive attitudes toward community services preferred informal help. If the county had more formal care services, however, older adults were more likely to use them, regardless of their filial beliefs. Disparities based on gender were observed, in that women who lived in counties with a higher percentage of older adults below the poverty line were more likely to receive no help than men.
Discussion:
Developing effective service promotion tactics, destigmatizing community services, and targeting services and support, especially to women, could decrease health disparities in rural Appalachia and similar geographic areas.
Keywords: care-mix, formal care, informal care, health disparities, rural
Embedded within rural America is a significant portion of the country’s elderly population, with more than one-quarter of all older adults living in rural and small-town areas (U.S. Census Bureau, 2015). Many rural elders are in worse health than their urban counterparts and face numerous care-related challenges including a dearth of available family caregivers, and less awareness of and access to formal long-term care services and supports (LTSS; McAuley, Spector, & Van Nostrand, 2009). Although individuals are situated within their broader social contexts, few investigators have considered the role of community-level or macro-level factors that create opportunities or challenges in accessing services and supports (Keating, 2008). Furthermore, traditional studies of state and regional differences (e.g., rural vs. urban) capture distal influences on the individual, but not the actual capacities of the communities in which older adults live. For example, older adults with mobility limitations may have fewer unmet needs if they live in a county with adequate transportation services than if they live in a county where such services are limited or nonexistent.
The present study is situated in the milieu of health disparities in rural Central Appalachian counties of Virginia. Compared with other parts of Appalachia, this mostly White, place-based population is known for its isolated communities distraught with concentrated areas of high poverty, unemployment, and economic distress (Deaton & Niman, 2012). The geographically isolated communities, characterized by rugged ridges surrounding remote valleys, sparse population, and inadequate transportation networks, create service access challenges for residents of the region (McGarvey, Leon-Verdin, Killos, Guterbock, & Cohn, 2011). As a case example of rural areas in the United States, these conditions are further compounded by barriers to health care and LTSS such as lower ratios of medical and para-medical professionals and home health workers, fragmented public transportation and/or very long distances to health services, inadequate knowledge of services offered; and inability to afford services (Hash, Jurkowski, & Krout, 2014). The geographic solitude of the region has also encouraged values of independence, individualism, skepticism for outsiders, and reliance on kinship networks (Halverson, Friedell, Cantrell, & Behringer, 2012; Wolff, Spillman, Freedman, & Kasper, 2016). At the same time, out-migration of younger adults has left a dearth of family care providers (Kratzer, 2015). Combined, these elements place older adults living in rural Appalachia in a triple jeopardy of being vulnerable people (i.e., older adults) in vulnerable places (i.e., under-serviced areas), with cultural views and beliefs that may negatively affect their use of formal care services. Thus, the purpose of this study was to examine the county-level contextual factors and individual-level personal characteristics of older adults, as well as the extent to which interactions among these contexts predict receipt of formal and informal care among older adults living in rural Appalachian counties.
Individual and Macro-Level Contextual Factors of Service Use
This study drew upon ecological and individual-based theories of service use to examine the various contextual factors associated with informal and formal care use in rural areas. According to Andersen’s behavioral model (Andersen & Newman, 1973), use of services is a function of an individual’s predisposing characteristics, enabling resources, and perceived or evaluated need for support. Previous research has consistently shown that personal characteristics such as older age and having more education predispose older adults to utilize formal services (Babitsch, Gohl, & von Lengerke, 2012). Also, significant gender disparities in the receipt of informal and formal help have been reported in the literature. Although it may seem that older women receive more formal services than older men (Gruneir, Forrester, Camacho, Gill, & Bronskill, 2013; Katz, Kabeto, & Langa, 2000), a few studies have shown that older women have to exhibit greater levels of disability before receiving formal help (Noel-Miller, 2010). This suggests that older women may have to rely heavily on their informal networks for support, or else experience daily life with unmet needs. Beliefs and values enable or discourage older adults’ willingness to seek formal services. For example, strong norms of filial obligation, distrust of outsiders, and availability of family support can increase resistance to the use of formal services (Coyne, Demian-Popescu, & Friend, 2006). This enduring view of rural residents can be problematic as it may drive policy initiatives that champion the values of self-reliance among residents, resulting in limited availability or withdrawal of services in these areas (Alston, 2007). The mixed findings in the literature suggest the need for further research on whether older residents in rural Appalachia would be willing to use services when available, despite their feelings of filial obligations and distrust of outsiders. Finally, need factors, which include an individual’s perceived or evaluated need for assistance, such as functional limitations and disability, also affect service utilization. The greater the impairment, the more likely elders are to use formal services (Penning, Cloutier, Nuernberger, MacDonald, & Taylor, 2016). Although Andersen and his colleagues revised the behavioral health model to include characteristics of the individuals’ environment (Andersen, 1995), researchers using this theoretical approach have mostly focused on individual-level characteristics, largely ignoring the environmental context when attempting to predict service use.
Ecological models, however, have illuminated the role of the environment or context in shaping individuals’ lives (e.g., Bronfenbrenner, 1979; Bubolz & Sontag, 1993). The main proposition of these models is that macrosystem social structures in which individuals are embedded (e.g., communities, society) interact with microsystems (e.g., family) and individual-level personal circumstances to shape lives. More recently, based on a meta-synthesis of the literature, researchers identified various characteristics of rural communities that provide a more nuanced conceptualization of the macrosystem in terms of its potential to influence outcomes for older adults (Winterton et al., 2016). According to these authors, macrosystem factors can be classified into socio-spatial and resource-based environments. The socio-spatial environment includes both socio-demographic characteristics, that is, factors that define the profile of community residents, for example, population size, area affluence, and rate of youth out-migration, and spatial characteristics that reflect the relative position of the community in relation to others, measured by indices such as the remoteness of communities and population density. The resource-based environment reflects the natural and built environments of communities as well as services and resources such as the presence of businesses and amenities, transportation infrastructure, and health and community services. Furthermore, these authors suggest that socio-spatial environment either can directly or through interactions with the resource environment, influence the types of resources and opportunities that are available for older adults in their environment.
Traditionally, most studies on health disparities have examined broad macro-level contextual variables such as urban versus rural differences or differences among states. Research using state-level characteristics has found that density of the old adult population combined with poverty and disability rates predicted strain on the resource environment, such as funding for LTSS for elderly residents and that states under the highest strain ration their services (Davey, Takagi, Sundström, & Malmberg, 2013). Although these researchers reported large variability in resource allocations and services among states, the findings provide a false view of homogeneity of resources within states. In fact, studies have found large variations in available services across counties in the same state. For example, Krout (1991) examined Area Agencies on Aging (AAA), which serve as the focal point for many LTSS, and found that rural AAAs provided fewer services to larger geographic areas with smaller budgets than urban agencies did. Another survey of 1,430 local governments nationwide found that rural counties provided 56% of 43 potential LTSS whereas urban counties provided 75% of potential LTSS (Morken & Warner, 2012). Moreover, rural LTSS are more sparsely located, have fewer employees, and are more likely to use home aides than urban ones, which can affect the quantity and quality of services older residents receive (Barretto et al., 2014). Even when individuals with similar predisposing, enabling, and need factors had an equal likelihood of receiving formal care, those living in rural and remote areas received fewer days of LTSS than their urban counterparts (McAuley et al., 2009). Thus, although resource allocations are determined at the federal and state levels, county budgets, which depend heavily on real estate and personal property taxes, are more likely to influence allocation of local services (e.g., transportation, meal programs) and, therefore, have a more immediate and direct influence on sources of support available to older adults. These county-level differences reinforce the need to understand the systematic variations in the capacities of counties of the same state to provide for their elderly residents.
Winterton et al.’s (2016) framework considers the importance of macrosystem characteristics for older adults’ wellness; however, researchers rarely address the interactions between the environment and individuals’ circumstances that can potentially amplify constraints placed on them by the socio-spatial environment. A qualitative study involving in-depth interviews found that rural elders living in counties with fewer resource-based infrastructures (e.g., safe roads connected to grocery stores and health care centers) and services (e.g., home-delivered meal services) rely largely on family members to meet their needs (Scharf & Bartlam, 2008). Another study found that older adults wait-listed for home-delivered meals had poor self-reported health, were food insecure, and exhibited nutritional risks—all pointing to extensive unmet need even among those not categorized as “high need” for assistance (Lee, Sinnett, Bengle, Johnson, & Brown, 2011). We speculate that individual need factors such as functional limitations and access to informal care affect the utilization of LTSS; however, county-level factors including local supply and demand are responsible for the rationing of LTSS for those most in need, often ignoring a large population of capable individuals who are also vulnerable to health risks. These findings and the limited data available suggest the importance of situating individual-level circumstances in the context of the county’s supply and demands for LTSS to understand disparities in access to care.
Current Study
Although context is broadly known as the physical and social environment, in this study, we hypothesize that individuals are embedded in the microsystems of their family and the macrosystem of their county and the salience of these contexts may differ among older adults depending on their circumstances and personal dispositions. We combine ecological and individual-based theories of service use to examine contextual factors and individual circumstances associated with informal and formal care use in rural areas. The integrated heuristic model in Figure 1 illustrates how macrosystem characteristics may interact with the microsystem, or individual-level characteristics, to predict the utilization of both informal and formal sources of care (hereafter called care-mix). For the socio-spatial environment, we considered four county-level variables: the proportion of older adults in the county, proportion of community-living older adults with a disability, county affluence, and proportion of older adults at or below the poverty line. We used the counties’ tax rates and availability of LTSS to measure the counties’ resource-based environment. We included the availability of kin as a measure of the microsystem. Finally, at the individual level, we considered various predisposing, enabling, and need factors to understand their interaction with the geographic and social context variables as well as their association with informal and formal service use. Our research questions and hypotheses are as follows:
Figure 1.
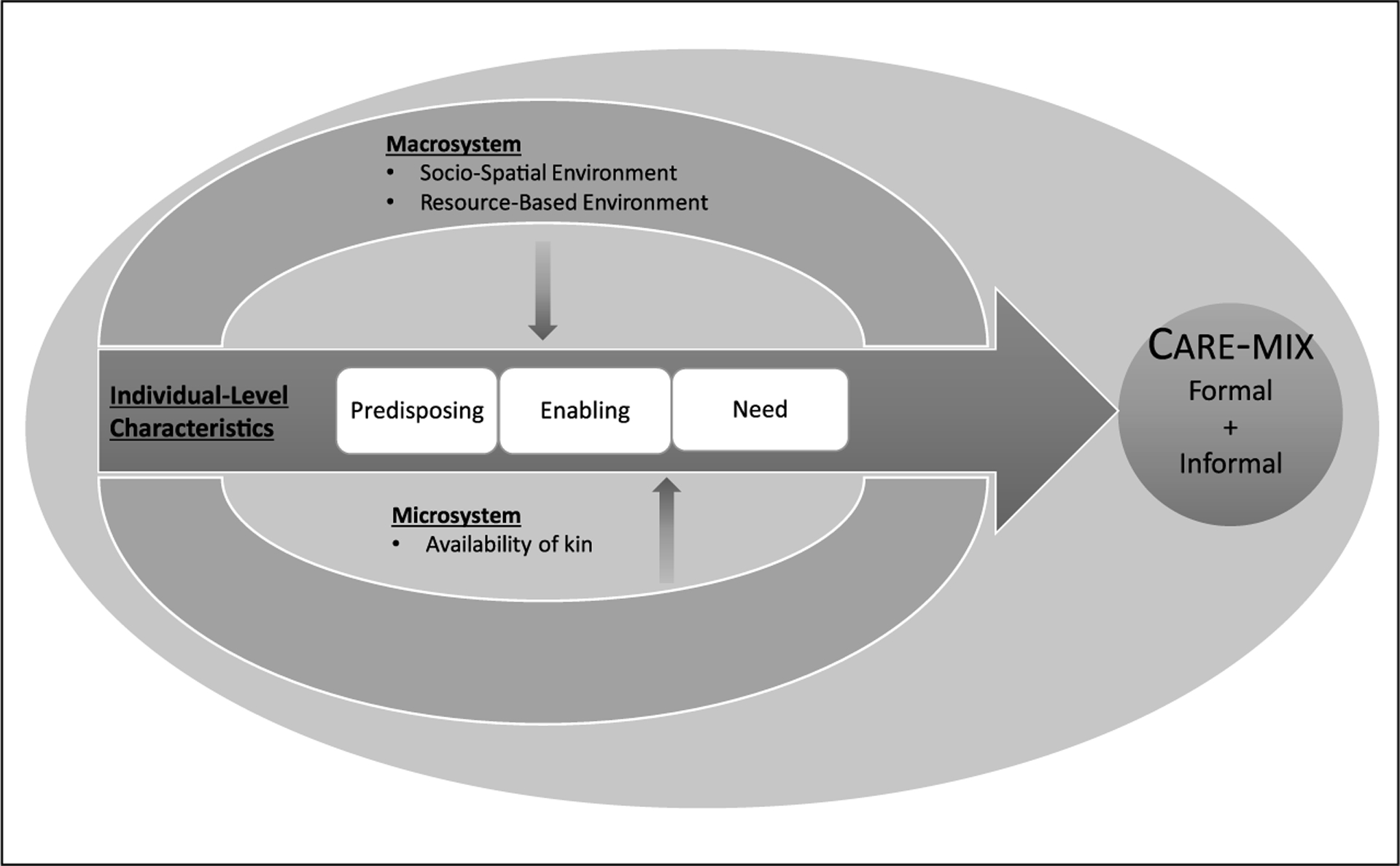
A heuristic model depicting interactions among contexts to predict care-mix.
Research Question 1:
How do individual-level factors and the availability of informal helpers (microsystem) affect the utilization of formal services and informal help by elders living in rural Appalachia?
Hypothesis 1 (H1): Being male, older, having more education and limited availability of informal helpers increases the odds of utilizing formal services.
Hypothesis 2 (H2): Having a positive attitude toward community services and a weaker belief in filial responsibility increases the odds of utilizing formal services.
Hypothesis 3 (H3): Older adults with more functional limitations will utilize both formal and informal care when they have more informal helpers, but will mobilize more formal services when they have fewer informal helpers.
Research Question 2:
How are socio-spatial and resource-based environment associated with individual-level influences on the use of informal help and formal services?
Hypothesis 4 (H4): County-level variables such as density of older adult population, percentage of older adults at or below the poverty level, percentage of older adults with a disability, county affluence as reflected in the tax rates, and number of LTSS catering to older adults are associated with older adults’ use of informal help and formal services.
Hypothesis 5 (H5)-Hypothesis 7 (H7): In counties that experience greater strain on resources (e.g., a higher percentage of residents aged 65+ at or below poverty level), older adults who have more functional limitations, are male, and are relatively older are more likely to use formal services, either alone or in combination with informal support.
Hypothesis 8 (H8): Older adults living in counties with more LTSS are more likely to use formal services, regardless of their beliefs about filial responsibility.
Design and Method
Dataset
Data for the current study come from the Older Families in Rural Communities: Personal and Social Influences on Service Use dataset compiled by the Virginia Tech Center for Survey Research. They were collected in 2000 through two telephone interviews with older adults and their informal helpers living in 17 rural counties in Central Appalachia Virginia. This article is based on the responses from the older adults only. Corresponding to the year of data collection, variables measuring geographic constructs in 17 counties were mined from the U.S. Census 2000 and Commonwealth of Virginia public documents.
Sample and Procedures
A targeted random sampling design was employed by the Virginia Tech Center for Survey Research to obtain a sample of 535 older adults (see Blieszner, Roberto & Singh, 2001). Eligibility requirements included living in the community, being 65 years of age or older, and having at least one functional limitation. Only households in 17 counties of southwest Virginia were included in the sampling frame. These counties were selected because they were located in rural Central Appalachia and were medically underserved (Health Resources and Services Administration Data Warehouse, n.d.).
Older adult households were targeted via age-specific telephone numbers and Federal Information Processing Standard codes provided by Survey Sampling Incorporated. From telephone numbers of 7,000 potential participants, 2,171 sample records were removed because the respondent reported there was no one in the household aged 65 or older. Another 779 records were removed because the telephone numbers were nonworking or nonresidential, or the respondent indicated a language or hearing problem that would make it difficult to complete the telephone interview. After the removal of these records, 2,034 individuals out of 4,050 (50.2%) participated in a 10-min telephone screening interview. Three-fourths of the respondents (n = 1,502; 74%) reported no limitations of daily activities for which they needed assistance and were, therefore, deemed ineligible for the study. The remaining 532 met all the inclusion criteria, yielding a representative sample of older adults residing in households in Southwest Virginia with a margin error of ±2.2% at the 95% level of confidence. Due to missing data on key predictors, the final analytic dataset consisted of 503 participants.
Study Measures
The telephone survey consisted of questions related to demographics, health, and physical functioning, informal and formal support, perceptions of community-based services, beliefs about filial responsibility, psychosocial functioning, and formal service use. The following measures were used:
Independent variables
Individual level
Predisposing factors.
Demographic characteristics included age, sex, and education. Age was dummy-coded 0 (65–79 years old) and 1 (80 or more years old). Sex was dummy-coded 0 (female) and 1 (male). Education was coded into four categories: 0 (postsecondary education: vocational school, community college, college/university, graduate/professional school), 1 (high school diploma/GED), 2 (some high school), or 3 (grade school completion or less).
Enabling factors.
Participants’ beliefs regarding filial responsibility were measured by two questions: “Parents are entitled to some return for the sacrifices they have made for their children” and “It is the responsibility of the adult children to take care of their parents when they become too old to care for themselves” rated on a 4-point Likert-type scale. Higher average scores indicated a stronger belief in filial responsibility (Cronbach’s α = .74). Participants’ attitudes about community services were measured by 16 items adapted from the Community Service Attitude Scale (Collins, Stommel, King, & Given, 1991). Example items were, “Community service providers do not provide good care,” and “I am fearful of having someone who works for community services to help me.” Participants rated these items on a 4-point rating scale with higher average scores indicating a positive attitude toward community services (Cronbach’s α = .75).
Need factor.
The degree of functional limitations was defined by two levels: difficulties with instrumental activities of daily living (IADL) only and difficulties with personal activities of daily living (PADL) regardless of IADL limitations. IADL questions addressed the participants’ need for assistance in six categories: cooking, driving, shopping, paying bills, performing minor household repairs, and cleaning house. PADL questions addressed assistance needed for walking, bathing/showering, dressing, eating, getting in and out of bed, getting in and out of chairs, toileting, personal grooming, and taking medications. Responses were collapsed to create a dummy-coded variable, with IADL difficulties coded as 0 and difficulties with PADLs regardless of difficulties with IADLs coded as 1.
Microsystem or social context.
Availability of informal help was determined from questions about living arrangements and availability of children. This variable was coded 0 (married and living with a spouse, with or without living children); 1 (currently not married, lives with someone); 2 (lives alone, has living children); and 3 (lives alone, has no living children).
Macrosystem.
Macrosystem independent variables were attained for each participant’s county. Socio-spatial variables included the percentage of the county’s population aged 65+ years, percentage of the county’s population aged 65+ years who were at or below the poverty level, and percentage of the county’s population aged 65+ years, community-dwelling, with a disability. The affluence of counties was determined through county data on real estate and tangible personal property taxes, obtained from state documents (www.tax.virginia.gov). Tax rates (per US$100 assessed value) were transformed using a logarithm function to normalize the distribution.
The number of LTSS businesses catering to older adults was used to index the resource-based environment. The number of LTSS businesses (i.e., count of each business location or branch) catering to older adults per county was determined by cross-referencing North American Industry Classification System (NAICS) codes in the 2000 U.S. Census. NAICS codes directly related to the care of older adults in community settings were utilized (i.e., NAICS 621610 and 62412, Home Health Care Services and Services for the Elderly and Persons with Disabilities, respectively). The first code includes LTSS primarily engaged in providing skilled nursing services in the home such as personal care services, physical therapy, medical social services, medications, medical equipment and supplies, counseling, 24-hr home care, occupational and vocational therapy, nutritional services, speech therapy, and high-tech care such as intravenous therapy. The second NAICS code includes social assistance services to improve the quality of life of elders and persons with disabilities and mental retardation such as day care centers, nonmedical home care, social activities, group support, and companionship.
Dependent variable
Care-mix.
For each activity of daily living (PADLs and IADLs) with which participants reported needing help, they were asked if they received help from anyone. If the participant said yes, they were asked to identify the source of help by responding to the following question: “Did you get help from … a family member, a friend/neighbor, or from someone with a community service/government agency/a paid individual for…?” We coded help from a family member or friend/neighbor as informal help, and help from community service/agency/paid individual as formal help. Using this coding, we collapsed the type of care across all PADLs and IADLs into the following four categories: 0 (needs help, but received neither formal nor informal help), 1 (received informal help only), 2 (received formal help only), and 3 (received both formal and informal help).
Analytic Plan
Descriptive statistics for all variables and correlations were examined for spurious relationships among variables. Older adults in the four care-mix categories were compared using ANOVA and chi-square tests. Due to the nested nature of the data (503 participants from 17 counties), we used multinomial logistic regression (MNR) models with robust standard errors corrected for county-level clustering of data. The main effects model included the individual- and macro-level county predictors to test H1, H2, and H4. Separate interaction effects were tested as follows:
H3: Functional Limitations × Availability of Informal Helpers
H5: Sex × Percentage of County’s Residents Age 65+ at or Below the Poverty Level
H6: Age Group × Percentage of County’s Residents Age 65+ at or Below the Poverty Level
H7: Functional Limitations × Percentage of County’s Residents Age 65+ at or Below the Poverty Level
H8: Number of LTSS in County × Belief in Filial Responsibility
The dependent variable category “Help From Informal Caregivers Only” was the reference group for all MNR analyses (see Supplementary Table for reference category “Formal Help Only”). To aid the interpretation of the findings, relative-risk ratios (RRs) are presented. Only interactions that were significantly associated with care-mix are discussed.
Results
Comparing characteristics of older adults from the four care-mix groups revealed important between-group differences (see Table 1). A higher percentage of women than men received no help (87.9%) or received informal help only (84.4%). Significant differences in education level showed that a higher percentage of older adults who had a postsecondary education (50.0%) received formal help only. The formal help only group also included a slightly higher percentage of older adults who lived alone (11.7%). Finally, the group that received both formal and informal care had a higher percentage of older adults who needed help with PADLs (44.2%) compared with the other three groups. A trend occurred for group differences in beliefs in filial responsibility (p = .058). Post hoc comparisons revealed that the group receiving formal services only had weaker beliefs in filial obligation (p < .05) than the group receiving both formal and informal services.
Table 1.
Descriptive Statistics: Individual Variables.
| Care-mix group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total sample (n = 503) | No help (n = 58) | Informal help only (n = 308) | Formal help only (n = 60) | Informal and formal help (n = 77) | |||||||
| n | % | n | % | n | % | n | % | n | % | χ2 | |
| Sex | 8.01* | ||||||||||
| Male | 90 | 17.9 | 7 | 12.1 | 48 | 15.6 | 16 | 26.7 | 19 | 24.7 | |
| Female | 413 | 82.1 | 51 | 87.9 | 260 | 84.4 | 44 | 73.3 | 58 | 75.3 | |
| Age category | 4.89 | ||||||||||
| 65–79 | 335 | 66.6 | 45 | 77.6 | 206 | 66.9 | 37 | 61.7 | 47 | 61.0 | |
| 80 and older | 168 | 33.4 | 13 | 22.4 | 102 | 33.1 | 23 | 38.3 | 30 | 39.0 | |
| Education | 28.28** | ||||||||||
| Postsecondary education | 134 | 26.6 | 16 | 27.6 | 61 | 19.8 | 30 | 50.0 | 27 | 35.1 | |
| High school diploma/General Educational Developmental Test (GED) diploma | 105 | 20.9 | 12 | 20.7 | 73 | 23.7 | 8 | 13.3 | 12 | 15.6 | |
| Some high school | 136 | 27.0 | 14 | 24.1 | 92 | 29.9 | 12 | 20.0 | 18 | 23.4 | |
| Grade school completion or less | 128 | 25.5 | 16 | 27.6 | 82 | 26.6 | 10 | 16.7 | 20 | 26.0 | |
| Functional limitations | 16.90** | ||||||||||
| Only instrumental limitations | 372 | 74.0 | 45 | 77.6 | 234 | 76.0 | 50 | 83.3 | 43 | 55.8 | |
| Physical limitations regardless of instrumental limitations | 131 | 26.0 | 13 | 22.4 | 74 | 24.0 | 10 | 16.7 | 34 | 44.2 | |
| Availability of informal help | 18.35* | ||||||||||
| Married, with or without living children | 158 | 31.4 | 19 | 32.8 | 108 | 35.1 | 17 | 28.3 | 14 | 18.2 | |
| Not currently married, living with someone | 84 | 16.7 | 7 | 12.1 | 58 | 18.8 | 5 | 8.3 | 14 | 18.2 | |
| Lives alone, has living children | 227 | 45.1 | 30 | 51.7 | 124 | 40.3 | 31 | 51.7 | 42 | 54.6 | |
| Lives alone, no living children | 34 | 6.8 | 2 | 3.5 | 18 | 5.8 | 7 | 11.7 | 7 | 9.1 | |
| M | SD | M | SD | M | SD | M | SD | M | SD | F | |
| Belief in filial responsibility | 2.59 | 0.60 | 2.61 | 0.61 | 2.60 | 0.61 | 2.41 | 0.65 | 2.68 | 0.49 | 2.51† |
| Community service attitude | 2.67 | 0.25 | 2.68 | 0.28 | 2.65 | 0.24 | 2.74 | 0.25 | 2.71 | 0.27 | 2.49† |
p < .10.
p < .05.
p < .01.
As shown in Table 2, approximately 15% of the population in the 17 counties was 65 years of age and older. Furthermore, 18% of the elderly population was at or below the poverty level, and 50% reported a disability. The average number of LTSS in these counties was 4.2.
Table 2.
Descriptive Statistics: County Predictors.
| M | SD | Range | |
|---|---|---|---|
| Total population age 65+ (%) | 15.08 | 2.27 | 8.62–17.98 |
| Total 65+ population who are at or below poverty level (%) | 18.02 | 3.95 | 10.50–26.60 |
| Total 65+ population who are community dwelling with a disability (%) | 50.22 | 7.20 | 39.94–63.31 |
| Personal property and real estate tax rate (per US$ 100 assessed value) | 2.01 | 1.31 | 1.15–7.00 |
| Total LTSS businesses catering to older adults | 4.22 | 3.10 | 1.00–12.00 |
Note. LTSS = long-term care services and supports.
Results for the multinomial regression are shown in Table 3. Compared with men, women were less likely to receive both formal and informal care and more likely to receive informal care only (RR = 0.43, p < .01). Women were also more likely to receive no care than formal care only (RR = 3.36, p < .01; supplementary table). More education was associated with increased odds of formal care utilization (RR = 3.28, p < .01) and combined informal and formal care utilization (RR = 2.38, p < .05), as compared with informal help only. Participants who had a more positive outlook toward community services utilization were more likely to receive a formal informal care-mix, whereas those with less positive view were more likely to receive informal care only (RR = 3.27, p < .05). Likewise, older adults who held stronger beliefs regarding filial responsibility were less likely to use formal care only and more likely to receive both formal and informal care (RR = 2.23, p < .05). Limitations in PADLs compared with limitations in IADLs increased the older adults’ odds of receiving both formal and informal care compared with formal care only (RR = 3.75, p < .01; supplementary table) or informal care only (RR = 3.01, p < .01). Greater availability of informal help greatly increased the odds of an individual receiving no care or informal care only. On the contrary, compared with participants who were married, those who lived alone with (RR = 2.83, p < .05) or without living children (RR = 3.55, p < .05) were more likely to receive both formal and informal care and were more likely to utilize formal care only when they lived alone and had no living children (RR = 4.54, p < .05).
Table 3.
Individual and County Predictors Associated With Informal and Formal Care in Rural Appalachian Counties of Virginia.
| No care vs. informal care only | Formal care vs. informal care only | Formal and informal care vs. informal care only | |
|---|---|---|---|
| RR (Robust SE) | RR (Robust SE) | RR (Robust SE) | |
| Individual-level predictors | |||
| Predisposing | |||
| Age category | |||
| 65–79 (Ref.) | |||
| 80 and older | 0.52 (0.24) | 1.17 (0.53) | 1.03 (0.25) |
| Sex | |||
| Male (Ref.) | |||
| Female | 1.51 (0.45) | 0.45 (0.21)† | 0.43 (0.15)** |
| Education | |||
| Grade school completion or less (Ref.) | |||
| Postsecondary education | 1.42 (0.65) | 3.28 (1.57)** | 2.38 (0.96)* |
| High school diploma/GED | 0.87 (0.37) | 0.85 (0.43) | 0.92 (0.48) |
| Some high school | 0.82 (0.28) | 1.00 (0.42) | 0.82 (0.43) |
| Enabling | |||
| Belief in filial responsibility | 1.17 (0.15) | 0.63 (0.20) | 1.41 (0.33) |
| Attitude toward community services | 1.29 (1.05) | 2.27 (1.30) | 3.27 (1.82)* |
| Need | |||
| Functional limitations | |||
| Only instrumental limitations (Ref.) | |||
| Physical limitations regardless of instrumental limitations | 1.01 (0.44) | 0.80 (0.34) | 3.01 (1.05)** |
| Microsystem: Social context | |||
| Availability of kin | |||
| Married, with or without living children (Ref.) | |||
| Not currently married, living with someone | 0.70 (0.40) | 0.73 (0.52) | 1.94 (0.98) |
| Lives alone, has living children | 1.57 (0.62) | 1.87 (1.23) | 2.83 (1.38)* |
| Lives alone, no living children | 0.60 (0.52) | 4.54 (3.42)* | 3.55 (2.11)* |
| Macrosystem: County-level predictors | |||
| 65+ population who are community dwelling with a disability (%) | 0.97 (0.01)** | 0.98 (0.03) | 1.00 (0.01) |
| Total population age 65+ (%) | 1.03 (0.04) | 0.94 (0.06) | 0.98 (0.02) |
| 65+ population who are at or below poverty level (%) | 1.00 (0.04) | 1.00 (0.09) | 1.02 (0.04) |
| Personal property and real estate tax rate (per US$ 100 assessed value)a | 0.73 (0.22) | 0.70 (0.25) | 1.09 (0.13) |
| Total LTSS catering to older adults | 0.94 (0.05) | 0.94 (0.06) | 0.97 (0.02) |
| Constant | 0.34 (1.06) | 0.64 (2.83) | 0.02 (0.00)** |
| Interaction effects | |||
| Functional Limitations x Percentage of 65+ at or Below Poverty | |||
| Only instrumental limitations (Ref.) | |||
| Physical limitations regardless of instrumental limitations | 0.87 (0.10) | 1.08 (0.10) | 1.11 (0.10) |
| Sex x Percentage of 65+ at or Below Poverty | |||
| Male (Ref.) | |||
| Female | 1.26 (0.09)** | 0.98 (0.06) | 0.99 (0.09) |
| Age Categories x Percentage of 65+ at or Below Poverty | |||
| 65–79 (Ref.) | |||
| 80 and older | 0.96 (0.07) | 1.12 (0.06)* | 1.04 (0.04) |
| Belief in Filial Responsibility x Total LTSS in County | 0.92 (0.04)† | 1.19 (0.08)* | 1.02 (0.04) |
Note. RR = relative-risk ratio; Robust SE = robust standard error; Ref. = Reference group; LTSS = long-term care services and supports.
Log transformed.
p < .10.
p < .05.
p < .01.
At the county level, older adults who lived in counties with a higher prevalence of disability were more likely to receive informal care only (RR = 0.81, p < .01). Although none of the other county-level predictors were directly associated with care-mix, we found some cross-level interactions. Participants who had greater functional limitations (i.e., PADL limitations) and resided in counties with a higher percentage of older adults who were at or below the poverty level were more likely to receive formal care (RR = 0.81, p < .01; supplementary table) than no care. Conversely, older adults with fewer functional limitations residing in these counties were more likely to receive no care. Another interaction effect depicting gender disparity was that women living in counties with higher poverty among the residents were more likely to receive no care than to receive informal care only (RR = 1.26, p < .01) or formal care only (RR = 1.29, p < .01; supplementary table). Compared with the older group (aged 80+), those in the younger group (aged 65–79) were less likely to receive formal care (RR = 1.12, p < .05) if they lived in counties with a higher percentage of older adults at or below the poverty level. Finally, despite their beliefs about filial obligation, older adults who lived in counties with more LTSS available were more likely to utilize formal care than use informal care only (RR = 1.19, p < .05).
Discussion
Health disparities are often driven by the social context in which individuals live, learn, work, and play (U.S. Department of Health and Human Services, 2010). Yet, previous investigations have ignored county-level contextual variables that affect resource allocations and the experiences of aging in rural areas. This study begins to fill the gap in the literature by integrating ecological and individual-based theories of service use to examine differences in care-mix patterns based on the differential effects of county-level resources and their interactions with older adults’ personal circumstances and family contexts. Overall, our findings reveal that where one ages matters. Consistent with previous studies, we found that individual-level factors such as functional limitations and limited access to informal care necessitate the use of LTSS. Extending the previous literature, the current study demonstrates intersecting influences of county-level factors, including local supply and demand, that are the basis for rationing LTSS to those most in need, thereby ignoring a large population of individuals with unmet needs and increased susceptibility to health risks.
Social context provides a significant safety net for older adults living in rural areas. We found a belief among elders in rural Appalachia that families should take care of their own, as well as reluctance to accept help from formal organizations. Elders who needed help with PADLs, or who lacked a spouse or a child in a position to provide informal support, however, received formal care services alone or in combination with informal help, supporting the complementarity theory of care-mix (Cantor, 1991; Denton, 1997). Conversely, older adults with low care needs (i.e., IADLs needs) typically received help from informal caregivers only. The lack of community services such as transportation and meal delivery programs in their counties may intensify the need for these older adults to rely on their informal support network (Thomas, Smego, Akobundu, & Dosa, 2017). Combined, our results provide new evidence that underscores the importance of social context for understanding rural elders’ reliance on others both to provide direct care and to navigate the formal care system (Scharf & Bartlam, 2008).
Our findings also show that macrosystem variables amplified the effect of individual-level characteristics that contribute to disparities in care. Older women who lived in counties with higher poverty levels were more likely to receive no care. However, men in the same counties were more likely to receive care from both informal and formal sources. We speculate that men receive priority in the distribution of scarce resources because they are presumed to be less capable of caring for themselves than women are. In addition, many older women may not have sufficient financial savings or resources to pay out-of-pocket for formal services (Katz et al., 2000). Furthermore, many older women in our study cared for themselves or relied on only one source of support, drawing attention to the social isolation that older women may experience in rural communities. Combined, these results support the prediction that women have to exhibit a greater level of disability before help is provided to them (Noel-Miller, 2010). These findings also reflect a dire need for more support structures for older women, especially in rural Appalachian communities where they head a disproportionate number of single-person households (Haaga, 2004; Rural Health Reform Policy Research Center, 2015).
Health care services have long been inadequate in rural areas such as Appalachia. Controlling for all other factors, we found that having more LTSS available increased the likelihood that residents utilized formal care, either alone or in conjunction with informal care, despite the cultural notion that Appalachian older adults are not willing to accept help from outsiders or hold strong beliefs about filial obligation. It may be that rural elders are stoic when their needs are minimal; however, when their needs increase, they may be willing to receive care from outsiders (Eales, Keefe, & Keating, 2008).
Disparities in health and differential use of health-related services continue to be problematic in many U.S. regions; Central Appalachia is only one example (McGarvey et al., 2011). The social and geographic context highlighted in this research sheds new light on older people’s sense of place and how where they live influences the care they receive. Although the culture of communities may compensate for health disparities experienced by older adults—by caring for their own—culture may also conceal unmet need among older residents in general, and specifically among older women. Ensuring the availability of a continuum of preventive and supportive services and encouraging their use can help assuage some of the vulnerability and risk associated with growing old in rural areas.
Limitations
Although our study contributes new insights on the relationships among individual- and county-level predictors of service use in rural Appalachia, it has some limitations. First, the data were collected in 2000. Since this time, there have been numerous additions to the delivery systems for LTSS, including Medicaid-funded Alzheimer’s Assisted Living Waiver (AAL; effective date 2006), Elderly or Disabled With Consumer Direction Waiver (EDCD; effective date 2005), and Program for All Inclusive Care for the Elderly (PACE; effective date 2007), that are available to some, but not all, elderly residents of Central Appalachia. Nevertheless, many challenges of service access and delivery remain within Appalachia as income, poverty rates, unemployment rates, and education levels still lag behind performance at the national level (Appalachian Regional Commission, 2017). The second limitation was our reliance on secondary data, which restricted the selection of study variables. Specifically, we used the availability of a spouse and adult children as an indication of one’s potential informal care network. Although previous studies have shown that not all relatives live in the vicinity or are willing to provide care (Davis & Bartlett, 2008), we argue that availability of family members can predict one’s likelihood to receive care or seek formal services (Larsson & Silverstein, 2004). We used the occurrence of PADLs and IADLs as the measure of impairment; measures of their severity were not available. Although the Department for Aging and Rehabilitative Services has offered consumer-directed home care services through the Personal Assistance Services Program (PAS) since 1990, how the use of such services was coded in NAICS 2000 was unclear. Third, while equal numbers of older men and women were included in the sampling plan, men comprised only 17% of the study sample, which prohibited a deeper analysis of gender differences on care-mix. Older men in our sample, however, had similar characteristics and care-mix ratios as those in a nationally representative study using Medicare Current Beneficiary Survey (Shea et al., 2003), which provides support for our findings. Fourth, securing access to LTSS data in this region is complicated, and our use of free-access data merely scratched the surface. We were also not able to capture alternate sources of formal support such as not-for-profit organizations, community clubs, faith-based organizations, private workers, or those hired through a referral agency (for other potential NAICS codes, see Newquist, DeLiema, & Wilber, 2015). Furthermore, it will be beneficial for future studies to use other geographically and culturally sensitive variables to understand disparities in Appalachia and other underserved areas. For example, the mountainous terrain in the Central Appalachian region makes access to LTSS not only challenging but also time-consuming. Using geographical-information systems to analyze spatial data could improve understanding of the challenges of health care delivery and access in rural and remote counties of Appalachia. Finally, while we situated our study within the larger U.S. rural context, the findings may not generalize to all rural areas because of varied racial, cultural, and economic settings. Nonetheless, this study highlights the importance of considering county-level contextual factors that may influence the service delivery and use.
Implications
Analysis of service utilization rarely considers regional influences on personal values and beliefs and on community attributes. Yet, this information is vital for program planners and policymakers to support and build upon the unique strengths and needs of their specific localities. Researchers must continue to extend the focus beyond individuals and pay greater attention to the influence of community-level variables on service utilization. Having demonstrated the importance of county-level variables, despite the use of secondary data, suggests that research designs intentionally incorporating these features will better reflect the lived experiences of older residents and their families.
Community-based LTSS, especially services that allow individuals to age in place, are of critical importance to older adults and communities at-large. As service providers and policy analysts consider how best to meet the needs of their aging population in an efficient, caring, and economical fashion, evidence-based research is needed to guide their decisions. Although the emphasis is often placed on developing service delivery models that can be duplicated, such programs may need to be tailored to the distinctive features of rural communities and geography (Krout, 2015). Our findings show that even in a defined geographic region such as Central Appalachia, within-county variations contributed to differential service utilization. Thus, collaborations between researchers and service providers are vital to promoting sharing of local information and ideologies to inform the systematic examination of older adults’ needs, the contexts affecting their lives, and the implementation and evaluation of services.
Understanding key explanatory variables of service use will allow providers to disentangle the complex relationships among individual and geographic contexts and in turn, better align outreach and service delivery in rural areas based on these characteristics. Thus, integrating micro- and macro-level data will contribute depth and breadth of information about care-mix patterns and needs so service providers and policymakers can address the cultural, economic, and geographic variability within the resource constraints of the regions they serve. Understanding the needs of their constituents makes it possible to identify if and how a community-based strategy can help address and overcome particular barriers to care. Community partnerships and collaborative strategies, such as mobilizing advocacy efforts for legislative change; developing volunteer programs, including community exchange programs; integrating services sectors; and providing workforce training and career advancement opportunities, can provide the building blocks. Systemic changes in financing and public policy to meet the care needs of older adults in Appalachia and other underserved rural communities rely on these measures.
The balance of funding for formal services has shifted and likely will continue to shift among federal, state, and local jurisdictions (Thomas & Applebaum, 2015). As our findings suggest, limited economic resources may prohibit adequate funding for local service systems, disadvantaging vulnerable people living in vulnerable places. Thus, policymakers should promote greater resource and economic development in rural areas to generate revenues that support and sustain public and private services for older adults. Facilitating partnerships with business leaders, consumers, health and service providers, academic institutions, financial institutions, and technology experts spanning multiple rural communities also may be a viable approach to expanding or securing access to needed elder care options.
Supplementary Material
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors gratefully acknowledge support from the National Research Initiative Competitive Grants Program, USDA (Project 99-35401-7769); the Cooperative State Research, Education, and Extension Service, USDA, under Project VA-135528 of the Virginia Agricultural Experiment Station, and the NIH (R21 AG054682).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplementary material for this article is available online.
References
- Alston M (2007). Globalisation, rural restructuring and health service delivery in Australia: policy failure and the role of social work? Health & Social Care in the Community, 15, 195–202. doi: 10.1111/j.1365-2524.2007.00696.x [DOI] [PubMed] [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36, 1–10. doi: 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- Andersen R, & Newman JF (1973). Societal and Individual Determinants of Medical Care Utilization in the United States. The Milbank Memorial Fund Quarterly. Health and Society, 51, 95–124. doi: 10.2307/3349613 [DOI] [PubMed] [Google Scholar]
- Appalachian Regional Commission (2017, August). Health disparities in Appalachia. Retrieved from https://www.arc.gov/research/ResearchReports.asp?F_YEAR=2017
- Babitsch B, Gohl D, & von Lengerke T (2012). Re-revisiting Andersen’s behavioral model of health services use: A systematic review of studies from 1998–2011. GMS Psycho-Social Medicine, 9: Doc 11 doi: 10.3205/psm000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barretto T, Varghese R, Pedersen S, Clark-Shirley L, Shetty S, Roy M, … Buatti L (2014). National Study of Aging and Disability Resource Centers process and outcome study report. Retrieved from http://www.aoa.acl.gov/Program_Results/docs/ADRCs-final-study-report.pdf
- Blieszner R, Roberto KA, & Singh K (2001). The helping networks of rural elders: Demographic and social psychological influences on service use. Ageing International, 27, 89–119. doi: 10.1007/s12126-001-1017-2 [DOI] [Google Scholar]
- Bronfenbrenner U (1979). The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press. [Google Scholar]
- Bubolz MM, & Sontag MS (1993). Human ecology theory In Boss PG, Doherty WJ, LaRossa R, Schumm WR, & Steinmetz SK (Eds.), Sourcebook of family theories and methods (pp. 419–450). New York, NY: Springer. [Google Scholar]
- Cantor MH (1991). Family and community: Changing roles in an aging society. The Gerontologist, 31, 337–346. doi: 10.1093/geront/31.3.337 [DOI] [PubMed] [Google Scholar]
- Collins CE, Stommel M, King S, & Given CW (1991). Assessment of the attitudes of caregivers toward community services. The Gerontologist, 31, 756–761. doi: 10.1093/geront/31.6.756 [DOI] [PubMed] [Google Scholar]
- Coyne CA, Demian-Popescu C, & Friend D (2006). Social and cultural factors influencing health in southern West Virginia: A qualitative study. Preventing Chronic Disease, 3(4), 1–8. Retrieved from www.cdc.gov/pcd/issues/2006/oct/06_0030.htm [PMC free article] [PubMed] [Google Scholar]
- Davey A, Takagi E, Sundström G, & Malmberg B (2013). (In)formal support and unmet needs in The National Long-Term Care Survey. Journal of Comparative Family Studies, 44, 437–453. [Google Scholar]
- Davis S, & Bartlett H (2008). Review Article: Healthy ageing in rural Australia: Issues and challenges. Australasian Journal on Ageing, 27, 56–60. doi: 10.1111/j.1741-6612.2008.00296.x [DOI] [PubMed] [Google Scholar]
- Denton M (1997). The linkages between informal and formal care of the elderly. Canadian Journal on Aging, 16, 30–50. doi: 10.1017/s0714980800014148 [DOI] [Google Scholar]
- Deaton BJ, & Niman E (2012). An empirical examination of the relationship between mining employment and poverty in the Appalachian region. Applied Economics, 44, 303–312. doi: 10.1080/00036846.2010.505558 [DOI] [Google Scholar]
- Eales J, Keefe J, & Keating J (2008). Age-friendly rural communities In Keating N (Ed.), Rural aging: A good place to grow old? (pp. 109–120). Bristol, UK: Policy Press. [Google Scholar]
- Gruneir A, Forrester J, Camacho Z, Gill SS, & Bronskill SE (2013). Gender differences in home care clients and admission to long-term care in Ontario, Canada: A population-based retrospective cohort study. BMC Geriatrics, 13, Article 48. doi: 10.1186/1471-2318-13-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haaga J (2004). The aging of Appalachia. Washington, DC: Appalachian Regional Commission. [Google Scholar]
- Halverson JA, Friedell GH, Cantrell ES, & Behringer BA (2012). Health care systems In Ludke RL & Obermiller PJ (Eds.), Appalachian health and well-being (pp. 89–108). Lexington: University Press of Kentucky. [Google Scholar]
- Hash KM, Jurkowski ET, & Krout J (2014). Aging in rural places: Programs, policies, and professional practice. New York, NY: Springer Publishing Company. [Google Scholar]
- Health Resources and Service Administration Data Warehouse. (n.d.). Retrieved from https://datawarehouse.hrsa.gov/Tools/Analyzers/MuaSearchResults.aspx
- Katz SJ, Kabeto M, & Langa KM (2000). Gender disparities in the receipt of home care for elderly people with disability in the United States. Journal of the American Medical Association, 284, 3022–3027. doi: 10.1001/jama.284.23.3022 [DOI] [PubMed] [Google Scholar]
- Keating NC (2008). Rural ageing: A good place to grow old? Bristol: Policy Press at the University of Bristol. [Google Scholar]
- Kratzer NW (2015). Coal Mining and Population Loss in Appalachia. Journal of Appalachian Studies, 21, 173–188. doi: 10.5406/jappastud.21.2.0173 [DOI] [Google Scholar]
- Krout JA (1991). Rural area agencies on aging: An overview of activities and policy issues. Journal of Aging Studies, 5, 409–424. doi: 10.1016/0890-4065(91)90019-o [DOI] [Google Scholar]
- Krout JA (2015). Providing services to rural older adults In Harsh KM, Jurkowski ET, & Krout JA (Eds.), Aging in rural places: Programs, policies, and professional practice (pp. 119–134). New York, NY: Springer. [Google Scholar]
- Larsson K, & Silverstein M (2004). The effects of marital and parental status on informal support and service utilization: A study of older Swedes living alone. Journal of Aging Studies, 18, 231–244. doi: 10.1016/j.jaging.2004.01.001 [DOI] [Google Scholar]
- Lee JS, Sinnett S, Bengle R, Johnson MA, & Brown A (2011). Unmet needs for the Older Americans Act Nutrition Program. Journal of Applied Gerontology, 30, 587–606. doi: 10.1177/0733464810376512 [DOI] [Google Scholar]
- McAuley WJ, Spector W, & Van Nostrand J (2009). Formal home care utilization patterns by rural–urban community residence. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 64, 258–268. doi: 10.1093/geronb/gbn003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarvey EL, Leon-Verdin M, Killos LF, Guterbock T, & Cohn WF (2011). Health disparities between Appalachian and non-Appalachian counties in Virginia USA. Journal of Community Health, 36, 348–356. doi: 10.1007/s10900-010-9315-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morken L, & Warner M (2012). Planning for the aging population: Rural responses to the challenge [Issue brief]. Ithaca, NY: Cornell University; Retrieved from http://cms.mildredwarner.org/p/146 [Google Scholar]
- Newquist DD, DeLiema M, & Wilber KH (2015). Beware of data gaps in home care research: The streetlight effect and its implications for policy making on long-term services and support. Medical Care Research and Review, 72, 622–640. doi: 10.1177/1077558715588437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noel-Miller C (2010). Longitudinal changes in disabled husbands’ and wives’ receipt of care. The Gerontologist, 50, 681–693. doi: 10.1093/geront/gnq028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penning MJ, Cloutier DS, Nuernberger K, MacDonald SW, & Taylor D (2016). Long-term care trajectories in Canadian context: Patterns and predictors of publicly funded care. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences. Advance online publication. doi: 10.1093/geronb/gbw104 [DOI] [PubMed] [Google Scholar]
- Rural Health Reform Policy Research Center. (2015). Exploring rural and urban mortality differences in the Appalachian region. Retrieved from https://rural-health.und.edu/projects/health-reform-policy-research-center/pdf/exploring-rural-urban-mortality-differences-appalachian-region.pdf
- Scharf T, & Bartlam B (2008). Ageing and social exclusion in rural communities In Keating N (Ed.), Rural ageing (pp. 97–108). Chicago, IL: Policy Press. [Google Scholar]
- Shea D, Davey A, Femia EE, Zarit SH, Sundström G, Berg S, & Smyer MA (2003). Exploring assistance in Sweden and the United States. The Gerontologist, 43, 712–721. doi: 10.1093/geront/43.5.712 [DOI] [PubMed] [Google Scholar]
- Thomas KS, & Applebaum R (2015). Long-term services and supports (LTSS): A growing challenge for an aging America. Public Policy & Aging Report, 25, 56–62. doi: 10.1093/ppar/prv003 [DOI] [Google Scholar]
- Thomas KS, Smego R, Akobundu U, & Dosa D (2017). Characteristics of older adults on waiting lists for meals on wheels: Identifying areas for intervention. Journal of Applied Gerontology, 36, 1228–1242. doi: 10.1177/0733464815614918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. (2015). Geographic comparison tables 0103 and 0104, 2011–2015. American Community Survey 5-Year Estimates. Retrieved from http://factfinder.census.gov/bkmk/table/1.0/en/ACS/15_5YR/GCT0103.US26 [Google Scholar]
- U.S. Department of Health and Human Services (2010, October 26). Healthy People 2020: An Opportunity to Address Societal Determinants of Health in the United States. Retrieved from https://www.healthypeople.gov/2010/hp2020/advisory/SocietalDeterminantsHealth.htm
- Winterton R, Warburton J, Keating N, Petersen M, Berg T, & Wilson J (2016). Understanding the influence of community characteristics on wellness for rural older adults: A meta-synthesis. Journal of Rural Studies, 45, 320–327. doi: 10.1016/j.jrurstud.2015.12.010 [DOI] [Google Scholar]
- Wolff JL, Spillman BC, Freedman VA, & Kasper JD (2016). A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Internal Medicine, 176, 372–379. doi: 10.1001/jamainternmed.2015.7664 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


