Abstract
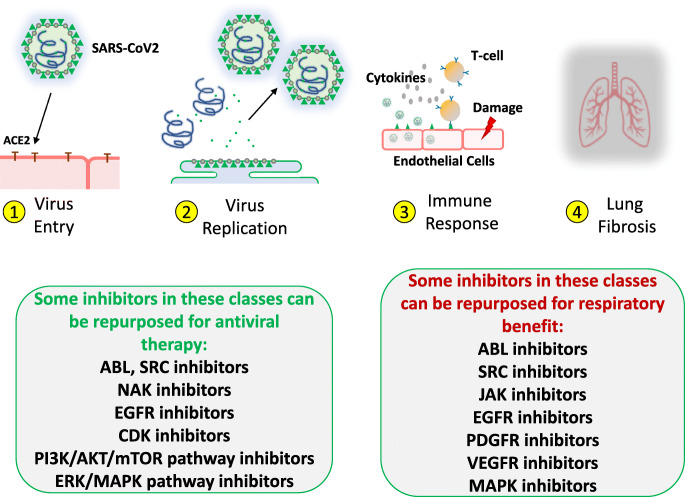
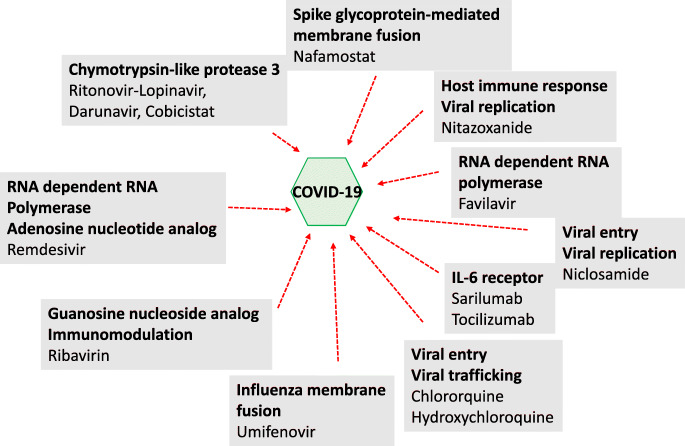
The outbreak of COVID-19, the pandemic disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has spurred an intense search for treatments by the scientific community. In the absence of a vaccine, the goal is to target the viral life cycle and alleviate the lung-damaging symptoms of infection, which can be life-threatening. There are numerous protein kinases associated with these processes that can be inhibited by FDA-approved drugs, the repurposing of which presents an alluring option as they have been thoroughly vetted for safety and are more readily available for treatment of patients and testing in clinical trials. Here, we characterize more than 30 approved kinase inhibitors in terms of their antiviral potential, due to their measured potency against key kinases required for viral entry, metabolism, or reproduction. We also highlight inhibitors with potential to reverse pulmonary insufficiency because of their anti-inflammatory activity, cytokine suppression, or antifibrotic activity. Certain agents are projected to be dual-purpose drugs in terms of antiviral activity and alleviation of disease symptoms, however drug combination is also an option for inhibitors with optimal pharmacokinetic properties that allow safe and efficacious co-administration with other drugs, such as antiviral agents, IL-6 blocking agents, or other kinase inhibitors.
Key words: Coronavirus, SARS-CoV-2, SARS-CoV, MERS-CoV, kinase inhibitors, pharmacokinetics, antiviral therapy, COVID-19
Clinical need for effective treatments for COVID-19
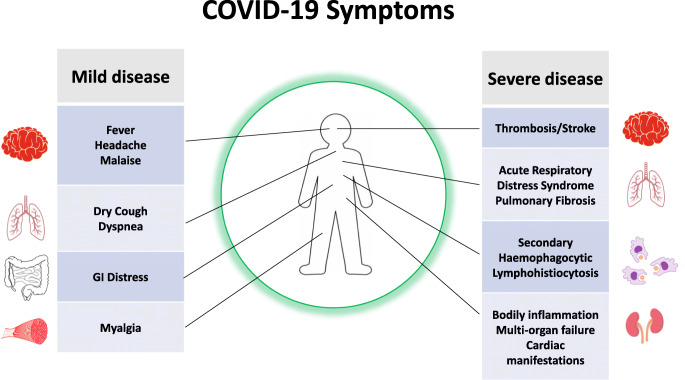
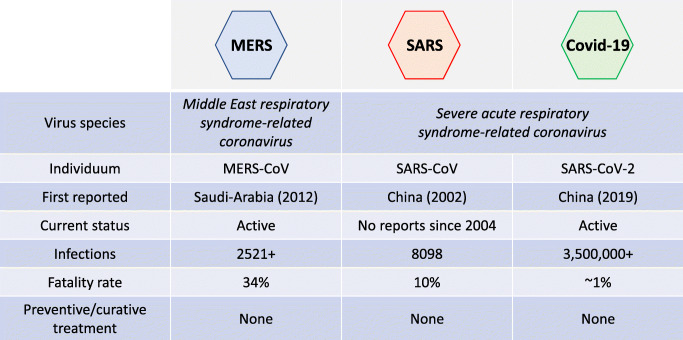
A novel human coronavirus, called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; formerly named 2019-nCoV), emerged in Wuhan, China. The outbreak in the previously unexposed human population was marked by high morbidity caused by SARS-CoV-2 as a result of the associated disease COVID-19 (Corona Virus Disease-2019). There is an urgent need for the development of therapies targeting both direct viral infection and the inflammatory immune response elicited by SARS-CoV-2. While many patients with documented SARS-CoV-2 infections have mild symptomatology, pathology can be severe in a subset of patients (Figure 1). Overall, COVID-19 has milder clinical manifestations and lower fatality than infections by the related viruses, SARS-CoV and MERS-CoV (Figures 1 and 2). However, COVID-19 infection can be fatal. Repurposing of drugs that have pre-existing FDA-approval as treatments for SARS-CoV-2 and related coronaviruses offers an attractive opportunity for the rapid deployment of effective therapeutics in the setting of the current pandemic outbreak, where treatment options are largely limited to supportive and symptomatic care.
Figure 1.
Covid-19 symptoms.
Figure 2.
Comparison of MERS-CoV, SARS-CoV, and SARS-CoV-2.
While symptoms associated with SARS-CoV-2 infection initiate with viral infection, the severe and sometimes fatal pathology seen with COVID-19 is primarily due to the onset of a virus-driven hyper-inflammatory response. For example, the first autopsy of a COVID-19 patient demonstrated the rapid progression of pneumonia and overactivation of T lymphocytes, which failed to establish an effective immune response and resulted in tissue injury, including lung damage and failure of other organs (1) (2). Consequently, while therapy-related suppression of viral infection and replication is a goal of current treatment approaches, it is posited that judicious suppression of the inflammatory response is also likely to benefit patients with severe COVID-19 disease. (3).
The most common presenting symptoms of SARS-CoV-2 are fever, dyspnea or dry cough, which are consistent with lower respiratory tract infection; other symptoms found to occur in less than 10% of COVID-19 patients analyzed include GI distress (diarrhea, vomiting), headache and weakness (4). Loss of smell and taste have also been reported in a sizable number of patients, including two-thirds of patients in Germany and 30% of patients in South Korea (5). A hallmark feature of COVID-19 infection is a distinct chest tomography pattern of bilateral peripheral ground-glass and consolidative pulmonary opacities (6). These findings can even be seen in patients with minimal symptoms. Potentially fatal sequelae of COVID-19 infection include respiratory failure in the form of acute respiratory distress syndrome (ARDS), which is typified by diffuse alveolar damage in early stages followed by fibroproliferation and fibrosis in prolonged cases. This leads to respiratory failure, requiring intubation and mechanical ventilation as a supportive therapy allowing time for viral clearance and lung healing. Also leading to complications and increased risk of death are pulmonary vascular endothelialitis, thrombosis and angiogenesis, symptoms of which distinguish lung pathobiology of COVID-19 patients from that of severe influenza infection (7).
Additionally, liver, heart and kidney failure, life-threatening coagulopathies, and cases of secondary haemophagocytic lymphohistiocytosis (sHLH) have been reported. Of note, sHLH is a syndrome characterized by systemic inflammation as demonstrated by markedly elevated levels of cytokines, including interleukin (IL)-2, IL-7, granulocyte-colony stimulating factor (GM-CSF), TNF-alpha, interferon-gamma inducible protein 10, macrophage inflammatory protein 1-alpha, and monocyte chemoattractant protein 1, resulting in elevated serum inflammatory markers such as ferritin, cytopenias, and multiorgan failure (8) (3) (9).
The point of entry for SARS-CoV-2, angiotensin-converting enzyme 2 (ACE2) is highly expressed in the heart and upregulated in the failing heart (10), and ACE2 receptor levels have been found to be significantly expressed in various organs in the body, such as the esophagus, kidney and bladder (11). These are potential target organs for SARS-CoV-2 and could explain the observed systemic inflammation beyond respiratory issues. In addition, there is evidence for the presence of ACE2 in brain tissue (12), which could explain some of the observed brain manifestations associated with COVID-19.
Long-term or permanent lung damage in the form of pulmonary fibrosis, an epidermal growth factor (EGFR)-mediated process, has been observed in survivors of SARS-CoV and MERS-CoV infections and occurs in up to 64% of patients with ARDS (13). In a study following a SARS-CoV outbreak, thin-section computed tomographic findings revealed fibrotic changes in 62 % of the patients observed (14).
Pre-existing co-morbidities that appear to worsen the course of SARS-CoV-2 disease include cancer, kidney disease, obesity, diabetes, hypertension, and cardiovascular disease (15). The elderly (>60 years of age) are generally the most vulnerable to the virus with significant increased mortality in patients over the age of 85, with precipitous onset of pneumonia and systemic inflammatory changes (15). Interestingly, unlike influenza, children, who account for 1-5% of COVID-19 cases, and those under the age of 30 are generally spared severe illness (16). The reason for this predilection for older adults is unclear, however may be related to dysregulated immune response in these individuals (17). Still, severe symptoms are observed in up to 6.7% of children, typically those with underlying health issues or who are under the age of 12 months (16).
As reviewed and proposed below, there are three major needs that have yet to be met for effective management of COVID19 disease: 1) anti-viral therapies that limit viral transmission, cell entry, and replication, 2) therapies that attenuate the non-productive immune response and thus decrease end-organ damage, and 3) therapies that have an anti-fibrotic effect in patients with ARDS and thus decrease long-term sequelae of disease.
Rationale for repurposing approved kinase inhibitors
SARS-CoV-2 belongs to the Baltimore Group IV classification of RNA viruses, which also includes hepatitits C virus (HCV), West Nile virus, dengue virus, and rhinoviruses, but it most closely resembles Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) and Middle East Respiratory Syndrome Coronavirus (MERS-CoV) (18) (Table 1). SARS-CoV-2, like SARS-CoV and MERS-CoV, is a member of the Betacoronavirus genus and shares 80% RNA sequence identity with SARS-CoV (19) (20), and 50% sequence identity with MERS-CoV (20) (Figure 2). While the rates of mortality and transmission differ between SARS-CoV, MERS-CoV, and SARS-CoV-2, there is substantial overlap in the pathogenesis, genetic makeup and clinical features of the diseases caused by these viruses (21). Numerous kinases have been suggested as being important mediators of various viral infections, in particular SARS-CoV and MERS-CoV, and these same proteins are predicted to be involved in mediating infection by SARS-CoV-2, as well.
Table 1.
Classification of viruses and the kinase inhibitors showing antiviral activity.
| Virus | Baltimore classification | Kinase inhibitors showing antiviral activity (potential kinase targets) |
|---|---|---|
| SARS-CoV-2 | Group IV, positive sense single-stranded RNA virus |
imatinib (unpublished; preprint: https://www.biorxiv.org/content/10.1101/2020.03.25.008482v2.full) abemaciclib, gilteritinib, osimertinib (unpublished; preprint: https://www.biorxiv.org/content/10.1101/2020.03.20.999730v3.full.pdf) |
| SARS-CoV | Group IV, positive sense single-stranded RNA virus |
imatinib, dasatinib, nilotinib (ABL2) |
| MERS-CoV | Group IV, positive sense single-stranded RNA virus |
imatinib, dasatinib (ABL2) (27) saracatinib (LYN, FYN) (33) sorafenib (RAF) (68) |
| Dengue | Group IV, positive sense single-stranded RNA virus |
dasatinib, saracatinib (SRC, FYN) (34) (35) (36) sunitinib, erlotinib (AAK1, GAK, AXL, KIT, RET) (46) |
| Hepatitis C | Group IV, positive sense single-stranded RNA virus | |
| West Nile | Group IV, positive sense single-stranded RNA virus | sunitinib, erlotinib (46) |
| Zika | Group IV, positive sense single-stranded RNA virus | sunitinib, erlotinib (46) |
| Ebola | Group V, negative sense single-stranded RNA virus | nilotinib (ABL1) (24) |
| Influenza A | Group V, negative sense single-stranded RNA virus | alvocidib (CDK9) |
| Human cytomegalovirus | Group 1, double-stranded DNA virus | gefitinib, erlotinib (EGFR) (59) (57) (56) |
| Vaccinia | Group 1, double-stranded DNA virus | imatinib (ABL) (25) |
| Herpes simplex type 1 | Group 1, double-stranded DNA virus | palbociclib (CDK6) (62) |
Protein kinases have become an exceptionally important group of drug targets, accounting for 20-30% of the drug discovery programs of major pharmaceutical companies and are thus an opportune target. Many kinase inhibitors that have pharmacologic effects that may be beneficial in ameliorating the severe and potentially life-threatening symptoms of COVID-19, such as anti-inflammatory activity, cytokine suppression, and antifibrotic activity, are already approved. Ideally, one kinase inhibitor with optimal pharmacokinetic properties could be repurposed as a dual function therapeutic that could reduce infection through direct viral targeting and could also provide clinical benefit by suppressing disease symptoms. Alternatively, kinase inhibitors could be tested in combination with antiviral agents or other targeted therapies that show promise in clinical trials for COVID-19 to achieve greater efficacy than any one agent alone.
Kinase inhibitors as potential antiviral therapeutics
The fact that treatments for respiratory viral infections like those caused by SARS-CoV, MERS-CoV, and SARS-CoV-2 are restricted to medications designed to treat only symptoms of pulmonary disease justifies the repurposing of drugs, preferably FDA-approved drugs already investigated in patients for tolerance and toxicity, with the dual ability to target the root causes of infection and to mitigate symptoms of respiratory distress caused by the infection. It would thus be beneficial to find and identify multi-targeted drugs in clinical use that encompass both properties. Such drugs would ideally also be able to potentiate the effectiveness of other more targeted antiviral agents or supportive therapies approved for severe or potentially fatal respiratory diseases.
A number of approved antiviral treatments are designed to inhibit enzymes such as polymerases or proteases through a “one drug, one bug” line of attack, which has been deemed inadequate due to the inefficiency of these treatments in working against multiple viruses, as well as failure to treat emerging new strains with accumulating mutations that are drug-resistant. The high cost and lengthy timeline for development of a novel agent are additional factors that dramatically limit the efficiency of this approach for covering a wide range of existing viruses as well as newly emerging ones or those that have developed resistance to current therapies. A different strategy involves targeting integral host cell proteins that are required by a broad spectrum of pathogens, including those that are emerging and novel and for which no effective treatment exists. An advantage of targeting host cellular proteins is that they do not undergo the same mutation rates that are seen for genomes of viruses.
There is a difference between developing drug therapies for a chronic virus, such as human immunodeficiency virus (HIV) or HCV, which the immune system cannot clear, versus developing drug therapies for acute viruses, such as influenza or SARS-CoV-2, which the immune system eventually does clear. For acute viruses, given the correlation of viral burden with disease severity, the goal may be to lower viral replication to prevent severe disease (flatten the curve of viral replication/burden). The potential drawback to direct-acting antiviral agents that do not have near sterilizing potency (or that cannot be used as a combination to suppress replication to near sterilizing levels), is that allowing the virus to replicate leads to resistance. Inhibiting a host target is unlikely ever to have the potency one can achieve with, as an example, an inhibitor of the viral RNA-dependent RNA polymerase (RdRp). However, host-targeted antiviral drugs exploit the dependence of the virus on specific host proteins and pathways during replication. Resistance may be less likely to develop against these agents because a single point mutation in the viral genome is unlikely to enable the virus to replicate independently of the targeted host factor. Another challenge in making antiviral agents against acute viral pathogens is that there is a narrow window in which the antiviral can have an effect (as an example influenza drugs). This raises the challenge of being able to diagnose and treat early in the disease course in order for the drug to provide clinical benefit.
Many FDA-approved, small molecule kinase inhibitors have multiple protein targets, including those identified in the host cell as being necessary or required for viral life cycle, replication, and infection of multiple virus types. This property could potentially be applied toward a more broad-spectrum antiviral therapy. The fact that approved therapies are well-characterized in terms of safety and pharmacokinetics and thus could be readily repurposed would reduce the cost and time involved for drug development and increase drug availability to patients.
ABL and SRC inhibitors
ABL kinase inhibitors have been demonstrated to inhibit replication of several unrelated viruses at different stages of their life cycle, including the coxsackie virus and dengue, Ebola, and vaccinia, in in vitro cell-based studies (Table 1) (22) (23) (24) (25) (26). For the coxsackie virus, ABL is activated following attachment of the virus to the glycosylphosphatidylinositol (GPI)-anchored protein decay-accelerating factor (DAF) on the apical cell surface; the ABL activation in turn triggers Rac-dependent actin reassembly that allows delivery of the virus to the tight junction (22). FYN kinase is also activated in response to viral attachment to DAF, and this leads to phosphorylation of the plasma membrane protein, caveolin, and viral transport into the cell through caveolin-containing vesicles (22). Activation of ABL by the coxsackie virus and the role ABL plays in viral infection are independent of SRC kinases (22), whereas in contrast ABL kinases partner with SRC family kinases to stimulate the actin-based movement of vaccinia virus (23). In the case of Ebola virus, regulation of viral replication by ABL1 was demonstrated by ABL1-specific siRNA inhibition of the release of virus-like particles in a cell culture co-transfection system; nilotinib also showed antiviral activity in this assay, at μM concentrations that were not cytotoxic (24). In vivo antiviral efficacy of imatinib was shown in a model of vaccinia virus; testing of imatinib in this model was based on the demonstrated involvement of ABL in release of cell-associated enveloped virions from the host cell (25). In this study, a dose of 200 mg/kg/day of imatinib was able to reduce the number of viral genome copies by around 4 logs (25). Lack of efficacy of dasatinib in the same model was attributed to immunotoxicity due to Src inhibition, however it is believed that dasatinib could still be a candidate coronavirus treatment with a dosing regimen that effectively blocks viral dissemination while exhibiting minimal Src-related immunotoxicity (27).
The ABL inhibitors, imatinib and dasatinib, were identified in a screen as inhibitors of both SARS-CoV and MERS-CoV replication, and nilotinib was identified as an inhibitor of only SARS-CoV, in vitro (27). Investigation of the mechanism for imatinib against SARS-CoV and MERS-CoV revealed inhibition of the early stages of the virus life cycle, and inhibition of viral replication through blocking the fusion of the coronavirus virion with the endosomal membrane (28) (29). Importantly, authors show that targeted knockdown of ABL2, however not ABL1, significantly inhibited SARS-CoV and MERS-CoV replication/entry in vitro (29). The relatively high, albeit minimally toxic, μM range concentrations of imatinib and dasatinib required to inhibit SARS-CoV and MERS-CoV in the aforementioned cell-based studies may be attributable to experimental factors such as drug resistance of the cell lines used as tools for propagating the viruses (27) (29), and thus in vivo testing would be needed to determine optimal dosing. It is worth noting that in many cell-based assays measuring drug effects on virus titer, the antiviral activity is cell-type dependent, and there is also variability depending on which virus strain is used. Recent, unpublished results, reported as a preprint, suggest that imatinib inhibits SARS-CoV-2 in vitro, among 17 other FDA-approved drugs with IC50 values similar to those observed for SARS-CoV and MERS-CoV; concentrations showing antiviral activity were not cytotoxic (BioRxiv, 2020, 10.1101/2020.03.25.008482)
As discussed above, infection by SARS-CoV is the result of several steps, including receptor binding, S glycoprotein conformational alterations, and proteolysis within endosomes that is mediated by capthepsin L (30). SARS-CoV infection has been shown to be blocked by targeted inhibitors of cathepsin L (30). On a related note, it has been shown that complete inhibition of viral entry and replication can result from treatment of cells with a cathepsin inhibitor as well as treatment with the serine protease inhibitor, camostat, which blocks activity of the type II transmembrane serine protease (TTSP) TMPRSS2, a surface-expressed serine protease that cleaves the coronavirus S protein and is involved in viral entry into a host cell (31). It has been proposed that imatinib may inhibit the function, localization or activity of TMPRSS2 (29). This suggests that this may be a promising drug:target match that could be further explored as a potential treatment for SARS-CoV-2 infection, since SARS-CoV-2 uses the SARS-CoV receptor ACE2 and the protease TMPRSS2 to enter host cells. In addition, ABL and ARG kinases have been found, in cancer cells, to promote secretion of the endosomal protease cathepsin L (30) (32). Thus, the testing of the ability of ABL inhibitors to inhibit cathepsin L in the context of viral infection may be warranted. It may generally be worthwhile to evaluate each of these targets with respect to what is known about SARS-CoV-2 infection and conduct further studies to elucidate potential therapeutic approaches involving ABL inhibition.
Several of the SRC family kinases have been implicated in replication of viruses, including those related to SARS-CoV-2, as well as unrelated viruses. The ABL/SRC inhibitor, saracatinib, has been shown to inhibit MERS-CoV at early stages of the viral life cycle, at μM range concentrations (33). In this study, siRNA knockdown of SRC family proteins, LYN and FYN, the latter implicated in coxsackievirus entry through epithelial tight junctions (22), led to significant reductions in MERS-CoV titer, suggesting these proteins may be important for MERS-CoV replication (33). Saracatinib was also shown to synergize with gemcitabine, which also exhibits anti-MERS-CoV activity (33). SRC has been shown, through siRNA knockdown, to be important for replication of dengue virus; dasatinib inhibited dengue infection by preventing infectious virus particle formation within the virus replication complex (34) (35). Saracatinib and dasatinib were shown to exhibit activity against dengue virus in vitro, with FYN implicated as a target for RNA replication (36). YES was demonstrated, through genetic knockdown, to reduce West Nile virus titers through effects on the viral replication cycle and to attenuate viral assembly and egress (37). Finally, siRNA library screenings focused on identifying host factors required for replication of HCV and dengue revealed c-terminal SRC kinase (Csk) as being important (38) (35).
NAK inhibitors
Important virus-associated protein targets include those associated with intracellular membrane trafficking, a cellular process vulnerable to “hijacking” by a broad range of unrelated viruses. Two host cell kinases that have been found to play an integral role in viral infection and life cycles are members of the numb-associated kinase (NAK) family: (1) AP2-associated protein kinase 1 (AAK1), which promotes endocytosis, and (2) cyclin G–associated kinase (GAK), which mediates endocytosis (39) (40). AAK1 and GAK are reported to be exploited by a variety of viruses, including HCV and dengue virus, which fall into the same Group IV Baltimore classification as SARS-CoV, MERS-CoV and SARS-CoV-2, and also the Ebola virus, which belongs to a different group (Table 1) (18) (41) (42) (43) (44) (45). The importance of AAK1 and GAK for HCV and dengue virus infection in vitro was shown via genetic (siRNA) silencing of AAK1 and GAK, which inhibited viral entry and infectious virus production (42) (46). Genetic (siRNA) silencing of AAK1 and GAK also decreased infection by Ebola virus (46).
Several kinase inhibitors have been proposed to exhibit antiviral activity based on their ability to potently target AAK1 and GAK. One drug, the FDA-approved janus kinase (JAK) inhibitor, baricitinib, was identified- in response to the SARS-CoV-2 outbreak- as a possible treatment for COVID-19 by investigators from BenevolentAl and Imperial College London (45). Baricitinib was proposed to potentially reduce infection, based on the drug’s ability to inhibit AAK1 and bind to GAK (45). It has been argued that the therapeutic dosing and low plasma protein binding of baricitinib, in contrast to the JAK kinase inhibitors, ruxolitinib and fedratinib, may make baricitinib more likely to inhibit AAK1 at therapeutically effective and tolerated doses and potentially reduce viral infectivity in patients than the other inhibitors (45) (47). AAK1 and GAK binding potency for these inhibitors is shown in Table 2.
Table 2.
FDA approved kinase inhibitors: Kinase targets and respiratory benefits
| Kinase Inhibitor (brand name) (indication; main therapeutic targets) |
Selected Kinase Target Affinity (antiviral and pulmonary benefit) KINOMEscan (kd<100 nM) |
Anti-inflammatory activity, cytokine suppression, antifibrotic activity |
|---|---|---|
|
Midostaurin (Rydapt) (acute myeloid leukemia, systemic mastocytosis; multi-targeted; FLT3-ITD, D816V-c-KIT) |
AAK1, JAK2, JAK3, Kd KIT (220nM), Kd RET (350nM) (48) |
Anti-inflammatory and cytokine suppression (107) |
|
Lestaurtinib (orphan drug status, acute myeloid leukemia; multi-targeted; FLT3, JAK2, TrkA, TrkB, TrkC) |
AAK1, AXL, FYN, GAK, JAK1, JAK2, JAK3, RET Kd KIT (150nM)* |
Anti-inflammatory and cytokine suppression (107) |
|
Gilteritinib (Xospata) (acute myeloid leukemia; FLT3-ITD; AXL) |
AXL IC50 (41 nM) (49)** |
|
|
Dasatinib (Sprycel) (chronic myeloid leukemia, Ph+acute lymphoblastic leukemia; multi-targeted; BCR-ABL, SRC) |
ABL1, ABL2, CSK, FYN, GAK, KIT, LYN, SRC, YES | Anti-inflammatory, cytokine suppression, antifibrotic (100) (99) (102) (103) (104) (101) |
|
Imatinib Mesylate (Gleevec (US)/Glivec (Europe/Australia) (chronic myeloid leukemia, Ph+acute lymphoblastic leukemia, gastrointestinal stromal tumor, chronic eosinophilic leukemia, hypereosinophilic syndrome, systemic mastocytosis; myelodysplastic syndrome; BCR-ABL, KIT, FIP1L1-PDGFRalpha) |
ABL1, ABL2, KIT | Anti-inflammatory, cytokine suppression/immunomodulatory, antifibrotic (91) (92) (90) (79) (94) (95) (96) (93) (77) |
|
Nilotinib (Tasigna) (chronic myeloid leukemia; BCR-ABL) |
ABL1, ABL2, KIT | Antifibrotic ((80) (81) (82) (83) (84) (85) (86) |
|
Ponatinib (Iclusig) (chronic myeloid leukemia, Ph+ acute lymphoblastic leukemia; BCR-ABL) |
ABL1, ABL2, KIT, RET, SRC | Cytokine suppression (78) |
|
Saracatinib (orphan drug status, idiopathic pulmonary fibrosis; ABL, SRC, LCK, FGR, BLK) |
ABL1 FYN, LYN, SRC, YES1 IC50 v-ABL (30 nM); IC50 FYN (10 nM); IC50 LYN (5 nM) (isolated protein kinase assay) (186)** |
Antifibrotic (100) (99) (105) |
|
Bosutinib (Bosulif) (chronic myeloid leukemia; ABL, SRC) |
ABL1, ABL2, AXL, CSK, EGFR, FYN, GAK, LYN, SRC, YES | Anti-inflammatory, cytokine suppression, and antifibrotic (104) (87) (88) |
|
Baricitinib (Olumiant) (rheumatoid arthritis; JAK1, JAK2) |
JAK1, JAK2, TYK2 Kd AAK1 (17 nM); Kd GAK (136 nM) (cell-free assay) (47)** |
Anti-inflammatory and cytokine suppression (106) (107) (108) |
|
Ruxolitinib (Jakafi) (myelofibrosis, polycythemia vera; JAK1, JAK2) |
GAK, JAK1, JAK2, JAK3, TYK2 Kd AAK1 (100 nM); Kd GAK (120 nM) (cell-free assay) (47)** |
Anti-inflammatory and cytokine suppression, antifibrotic (107) |
|
Fedratinib (Inrebic) (myelofibrosis; JAK2) |
AAK1, ABL1, FYN, GAK, JAK2, SRC Kd AAK1 32 nM; Kd GAK 1 nM (cell-free assay) (47)** |
Anti-inflammatory and cytokine suppression, (107) (115) |
|
Tofacitinib (XELJANZ XR) (ulcerative colitis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis; JAK1, JAK3) |
JAK1, JAK2, JAK3, TYK2 No AAK1 inhibitory activity (47) |
Anti-inflammatory and cytokine suppression (109) (110) (107) (111) |
|
Gefitinib (Iressa) (non-small cell lung cancer; EGFR) |
EGFR, GAK | Antifibrotic (119) (116) (178) (118) |
|
Afatinib (Gilotrif) (non-small cell lung cancer, advanced squamous cell carcinoma; Her2/EGFR) |
EGFR, GAK | Anti-inflammatory, antifibrotic (116) (178) (179) |
|
Lapatinib (Tykerb and Tyverb) (breast cancer; Erb1/Erb2, EGFR) |
EGFR | Antifibrotic (116) (178) |
|
Osimertinib (Tagrisso)’ (non-small cell lung cancer; EGFR) |
EGFR (60)** |
AZ5104, active metabolite of osimertinib, downregulates Th17-related cytokine production via inhibition of SRC-ERK-STAT3 (127) |
|
Erlotinib (Tarceva) (non-small cell lung cancer, pancreatic cancer; Erb1, EGFR) |
EGFR, GAK Kd ABL1 (310nM) (48) |
Antifibrotic (116) (178) |
|
Neratinib (Nerlynx) (breast cancer; Her2/EGFR) |
EGFR | |
|
Pazopanib (Votrient) (renal cell carcinoma, advanced soft tissue sarcoma; multi-targeted; c-KIT, FGFR, PDGFR, VEGFR) |
KIT |
Anti-inflammatory potential, antifibrotic (136) |
|
Sorafenib (Nexavar) (renal cell carcinoma, hepatocellular carcinoma, thyroid cancer; multi-targeted; PDGFR, VEGFR, RAF) |
KIT, RET | Antifibrotic (125) (126) (187) |
|
Sunitinib malate (Sutent) (renal cell carcinoma, gastrointestinal stromal tumor; multi-targeted; PDGFR, VEGFR) |
AAK1, AXL, GAK, JAK1, KIT, RET | Anti-inflammatory potential, cytokine suppression, antifibrotic (137) (135) (107) |
|
Axitinib (Inlyta) (renal cell carcinoma; c-KIT, PDGFR, VEGFR1, VEGFR2, VEGFR3) |
ABL1, ABL2, KIT | Anti-inflammatory and cytokine suppression (128) |
|
Vandetanib (Caprelsa) (medullary thyroid carcinoma; EGFR, RET, VEGFR) |
ABL2, EGFR, GAK, RET, SRC Kd ABL1 (270nM) (48) |
|
|
Regorafenib (Stivarga) (colorectal cancer, gastrointestinal stromal tumor, hepatocellular cancer; PDGFRβ, Raf-1, TIE2, VEGFR1/2/3) |
KIT, RET | |
|
Ibrutinib (Imbruvica) (mantel cell lymphoma, Waldenstrom macroglobulinemia, chronic lymphocytic leukemia, Small lymphocytic lymphoma, marginal zone lymphoma; BTK) |
EGFR, RET | Anti-inflammatory (132) (133) |
|
Palbociclib (Ibrance) (breast cancer; CDK4, CDK6) |
CDK6 | |
|
Abemaciclib (Verzenio and Verzenios) (breast cancer, CDK4,CDK6) |
CDK6 IC50 (10 nmol/L) CDK9 IC50 (57 nmol/L) (188)** |
Abemaciclib in combination with anastrozole led to increased cytokine signaling and immune activation (189) |
|
Alvocidib (orphan drug status, acute myeloid leukemia; CDK1, CDK2, CDK4, CDK9) |
CDK9 | Anti-inflammatory (134) |
|
Ceritinib (Zykadia) (non-small cell lung cancer; ALK, IGF1R, InsR, STK22D) |
||
|
Crizotinib (Xalkori) (non-small cell lung cancer; ALK/ROS1) |
ABL1, AXL | |
|
Masitinib (Masivet) (orphan drug status, potential amyotrophic lateral sclerosis drug; FAK, FGFR3, KIT, LCK, PDGFR) |
ABL1, KIT, LYN |
|
|
Nintedanib (Ofev and Vargatef) (idiopathic pulmonary fibrosis, non-small cell lung cancer; FGFR, PDGFR, VEGFR) |
AAK1, ABL1, AXL, JAK2, JAK3, KIT, RET, YES1 | Anti-inflammatory, cytokine suppression, antifibrotic (129) (130) (131) |
Left Column: Drug names and disease indication, and main therapeutic targets. Middle Column: Potency (based on KINOMEscan data) against key proteins associated with respiratory function and proteins involved in viral replication/life span/infection- believed to be necessary for a wide variety of viruses, including SARS-CoV and MERS-CoV and SARS-CoV-2. Right column: Anti-inflammatory activity, cytokine suppression, and antifibrotic activity of the kinase inhibitors.
*These values were derived from ChEMBL database: https://www.ebi.ac.uk/chembl/.
**These values were not derived from KINOMEscan; References are cited.
The multi-targeted kinase inhibitor sunitinib and the EGFR tyrosine kinase inhibitor erlotinib, which potently bind to AAK1 and GAK (dissociation constant [KD] of 11 and 3.1 nM, respectively) (48), were shown to block HCV assembly and inhibit HCV entry with overexpression of AAK1 or GAK effectively reversing their antiviral activity (41) (42). Sunitinib and erlotinib also exhibited broad spectrum activity against dengue, West Nile virus and Zika virus infection in vitro at μM concentrations that were nontoxic to cells (46). To confirm antiviral activity of sunitinib and erlotinib, levels of phospho-AP2, a substrate of AAK1 and GAK, were measured and were found to be reduced in a dose-dependent fashion (46). Genetic (siRNA) depletion of AXL, KIT, and RET, out of a total of 27 protein targets of sunitinib and erlotinib, were found to inhibit dengue infection in a cell-based assay (46). This suggests that these three proteins are potential host targets mediating antiviral effects of the two drugs. Synergy between sunitinib and erlotinib was observed in a murine model of dengue, with 30-60 mg/kg of the drugs administered (doses chosen were at or near the approved human dose) (46). Sunitinib showed some efficacy in this model as a single agent (46). The protective effects of the combination of sunitinib and erlotinib observed in this murine model suggest it is plausible to utilize tolerable drug dosages with the potential to inhibit viral replication (46). It has been suggested, however, that side effects associated with these agents at doses required to inhibit AAK1 may not be tolerated by patients infected with SARS-CoV-2 (45).
Gilteritinib is a potent inhibitor of AXL (49), which is one of the targets of sunitinib and erlotinib identified to be important for dengue infection (46). Gilteritinib was reported (unpublished results; preprint) to be one of 24 FDA-approved drugs to show in vitro activity against SARS-CoV-2 (0.1 μM<IC50<10 μM)) (BioRxiv. 10.1101/2020.03.20.999730) (Table 1). Gilteritinib has been approved for adult patients with mutant FLT3-positive refractory/relapsed AML (Table 2).
EGFR inhibitors
Epidermal growth factor receptor (EGFR) has been implicated in infection by a wide range of unrelated viruses (50), including the spread and motility of vaccinia virus (51) and the processes of endocytosis (for influenza A and HCV), and entry and/or post-entry events (for human cytomegalovirus (HCMV) and adeno-associated virus serotype A (AAV6) (Table 1) (52) (53) (54) (55) (56) (57). In fact, among the first studies to show that tyrosine kinase inhibitors can have significant antiviral activity was one identifying EGFR as a co-factor for entry of HCV into human host cells (56). EGFR is also used by different viruses, including many respiratory viruses, to evade the host immune response (58). Activity against HCMV and HCV in vitro and in vivo has been demonstrated by the EGFR-targeting inhibitors, gefitinib and erlotinib (59) (56) (57).
Osimertinib is a potent inhibitor of EGFR (60). Osimertinib was reported (unpublished results; preprint) to be one of 24 FDA-approved drugs to show in vitro activity against SARS-CoV-2 (0.1 μM<IC50<10 μM)) (BioRxiv. 10.1101/2020.03.20.999730) (Table 1). Osimertinib has been approved for non-small cell lung carcinoma (Table 2).
Cyclin-dependent kinase inhibitors
Cell cycle progression of host cells can be modulated by viruses through influences on host cell cyclin-dependent kinases (CDKs). As an example, CDK9 has been implicated in infection by herpes simplex virus type 1 (HSV-1) (Table 1) (61). Specifically, CDK9 was shown for HSV-1 to be involved in expression of genes controlled by the viral regulatory protein, ICP22, and through binding to ICP22 leads to phosphorylation of RNA polymerase II (61). Palbociclib, at least partly through inhibition of CDK6, inhibited HSV-1 replication in vitro (62), likely through blockade of cellular protein phosphorylation (62). CDK9-targeting alvocidib showed activity against influenza A (Table 1) (63). CDK9 has been found to mediate the activity of RdRp of the influenza virus; cells lacking CDK9 showed impairment of viral replication (64).
The CDK4/6 inhibitor, abemaciclib, was identified as one of 24 FDA-approved drugs to display in vitro activity against SARS-CoV-2 (0.1 μM<IC50<10 μM); these results are unpublished and are reported as a preprint (BioRxiv. 10.1101/2020.03.20.999730) (Table 1). Abemaciclib has been approved for advanced or metastatic breast cancer (Table 2).
PI3K/AKT/mTOR and ERK/MAPK inhibitors
Activation of the phosphatidylinositol 3’-kinase-Akt-mammalian target of rapamycin (PI3K/Akt/mTOR) pathway has been implicated in growth and replication of numerous viruses, including HCV, West Nile virus, and influenza A virus (65) (66) (67). Pathway overrepresentation analysis and functional network analysis employed to identify cell signaling changes occurring during MERS-CoV infection (68) revealed members of the PI3K/AKT/mTOR signaling pathway, including AKT, target of rapamycin (mTOR), RPS6KB1, PDPK1, PIK3R1, and PIK3R2, and members of the Ras/Raf/MEK/ERK signaling pathway signaling pathway, including MAP2K1, MAPK3 and MAPK14, to be upregulated (68). At a concentration of 10 μM, the mTOR inhibitor, rapamycin, caused significant (61%) inhibition of MERS-CoV infection (correlated with decreased viral titers) in MERS-CoV-infected cells (68). Treatment of cells prior to MERS-CoV infection with sorafenib, which targets RAF, strongly inhibited infection (93%) (68). The inhibitory activity was diminished when sorafenib was added post-infection, suggesting a possible role for RAF early in the viral life cycle. Genetic knockdown studies, focusing on mTOR and RAF and other signaling molecules shown to be overrepresented during MERS-CoV infection, are warranted to validate the role of these proteins in this process.
Activation of the MAPK/ERK1 pathway has been implicated in influenza A virus production and viral nuclear export of ribonucleoprotein complexes (69). The pathway has also been associated with Ebola virus entry coupled with cellular (glycoprotein-induced) damage and elevated cytokine production (70) (71).
Summary of kinase inhibitor activity against virus-associated proteins
Using KINOMEscan biochemical kinase profiling assay data from the Harvard Medical School Library of Integrated Network-based Cellular Signatures (LINCS) (72) and data derived from the ChEMBL database, we focused on the ability of a list of FDA-approved kinase inhibitors to target those proteins implicated in SARS-CoV, MERS-CoV and related virus infections, as well as several unrelated viral infections, including ABL proteins, AAK1, AXL, CDK6, CDK9, CSK, EGFR, FYN, GAK, KIT, LYN, RET, SRC, and YES (Table 2, Fig. 3).
Figure 3.
Repurposing of kinase inhibitors as antiviral therapies and for respiratory benefit.
Pharmacokinetics of kinase inhibitors
Kinase inhibitors are significantly metabolized by cytochrome P450 enzymes, and some are either inhibitors or substrates of drug transporters, including P-glycoprotein (P-gp; ABCB1) or Breast Cancer Resistance Protein (BCRP;ABCG2). The extent of plasma protein binding can also affect and in some cases lower drug potency, such as occurs with highly (>99.9% plasma protein bound) midostaurin (73) (74). These factors can lead to differences in the amount of circulating and cellular drug concentrations between patients, and thus the potential a drug has for tissue distribution/bioavailability may be helpful when considering repurposing a drug based on its anticipated targeted effects. Some drug characteristics are shown in Table 3 (75) (76).
Table 3.
Pharmacokinetics and reports of pulmonary toxicity for kinase inhibitors
| Kinase Inhibitor (brand name) (company) | Absorption/bioavailability/peak plasma levels/volume of distribution (adults) | Metabolism (adults) | Recommended daily dose (adults); serum protein matrix binding: human serum α-1 glycoprotein (AAG), human serum albumin (HSA) | Pulmonary Toxicity |
|---|---|---|---|---|
|
Midostaurin (Rydapt) (Novartis) |
Time to Tmax between 1-3 h post dose in fasted state; following 50 mg oral dose, mean Cmax (total circulating radioactivity, unchanged midostaurin, and metabolites CGP52421 and CGP62221)=2160 ng/mL, 1240 ng/mL, 328 ng/mL and 562 ng/mL, respectively; mean AUC (0-infinity) (total circulating radioactivity, unchanged midostaurin, and metabolites CGP52421 and CGP62221) =165 x 103 ng Eq*h/mL, 15.7 x 103 ng*h/mL, 146 x 103 ng*h/mL, and 27.1 x 103 ng*h/mL, respectively; high oral absorption rate following 50 mg dose (190); rat and dog: bioavailability low to moderate (9.3-48.5%); human oral bioavailability low to moderate (190); Vd =95.2L (parent drug and metabolites distributed in plasma) |
Metabolized by hepatic CYP3A4 (Yin et al.,2008); CYP3A4 inhibitors may increase exposure to midostaurin and active metabolites |
50 mg orally twice daily; >99.9% binding (AAG) |
One case reported of interstitial lung disease while on midostaurin therapy post allogeneic stem cell transplant (191); in phase III trial, 8% of midostaurin-treated patients had grade 3-5 pneumonitis or radiographic pulmonary opacities (192) |
|
Lestaurtinib (Cephalon) |
No information available | No information available |
80 mg orally twice daily; High protein binding (AAG) (193) |
|
|
Gilteritinib (Xospata) (Astellas Pharma) |
Cmax observed 2 h following oral administration; Cmax=374 ng/mL; AUC=6943 ng.L/mL; Vd=1092 L (central); Vd=1100 L (peripheral) |
Metabolized mainly by CYP3A4 |
120 mg orally once daily; 94% (HSA) |
Boxed warning: 3% of patients experienced differentiation syndrome, characterized by symptoms including dyspnea, pleural effusion, pulmonary edema; may be life-threatening or fatal if not treated; Occurred as early as 2 days and up to 75 days following treatment initiation (194) |
|
Dasatinib (Sprycel) (Bristol-Myers Squibb) |
Oral bioavailability ranged from 14% (mouse) to 34% (dog); incomplete bioavailability because of incomplete absorption and high first-pass metabolism; not due to Pgp (195); Vd= 2505 L |
Metabolized by CYP3A4; extensively metabolized with 29 metabolites resulting from oxidation; possible inhibitor of CYP3A4 and CYP2C8 |
140 mg orally once daily; 96% (AAG, HSA) |
Pleural effusions are more frequently observed in dasatinib-treated patients than imatinib-treated patients, with 10-35 % of dasatinib-treated patients developing pleural effusions (196); reversible pulmonary arterial hypertension has been observed in a small percentage of dasatinib-treated patients (197) |
|
Imatinib Mesylate (Gleevec (US)/Glivec (Europe/Australia) (Novartis) |
Well absorbed; absolute bioavailability=98%; maximum plasma levels within 2-4 h of dosing; Vd= 347 l (+/-62) (198) |
Metabolized mainly by hepatic CYP3A4 and to a lesser extent by CYP1A2, CYP2D6, CYP2C9, CYP2C19 |
400 mg orally daily (chronic myeloid leukemia (chronic phase); 600 mg orally daily (chronic myeloid leukemia (accelerated phase); 95% binding (AAG, HSA) |
Most pulmonary toxicities associated with imatinib are related to fluid retention, with peripheral and periorbital edema more common than pleural or pericardial effusions and pulmonary edema; acute pneumonia and subacute interstitial pneumonitis occur rarely (199) (200) (201) |
|
Nilotinib (Tasigna) (Novartis) |
Cmax 0.5-4 h; moderate bioavailability (17-44%); absolute oral bioavailability predicted to be low (< 25%) (202); Vd= 0.55 to 3.9 l/kg across several species (202); (transported by ABCB1 and ABCG2) (203) |
Metabolized mainly by CYP3A4 (203) |
400 mg orally twice daily (resistant or intolerant chronic myeloid leukemia (chronic and accelerated phases); 300 mg orally twice daily (newly diagnosed chronic myeloid leukemia (chronic phase)); 98% binding (AAG, HSA) |
Lung-related adverse effects are rare in comparison to imatinib and dasatinib; in one clinical trial, pleural effusion was observed in less than 1% of nilotinib-treated patients (204) (141); case report of acute respiratory failure from diffuse alveolar hemorrhage (205) |
|
Ponatinib (Iclusig) (Ariad) |
Absolute bioavailability unknown; peak concentrations within 6 h of dosing; following 45 mg dose: Cmax = 73 ng/mL; AUC = 1253 ng•hr/mL; Vd= 1223 L (oral administration, 45 mg ponatinib once daily for 28 days); (weak substrate for P-gp and ABCG2) |
Metabolized by CYP3A4 and to a lesser extent CYP2C8, CYP2D6, CYP3A5 involved in phase I metabolism in vitro; esterases and/or amidases |
Commence treatment at 45 mg once daily (chronic myeloid leukemia and Ph+ acute lymphoblastic leukemia) (due to severe vascular occlusive events at this dose lower doses are being explored); start at 30 mg once daily (patients taking strong CYP3A inhibitors; patients with hepatic impairment); >99 % binding |
Pulmonary arterial hypertension has been reported for ponatinib (206) |
|
Saracatinib (AstraZeneca) |
Linear pharmacokinetic properties with single dose range 50-175 mg/d; following dosing 50 mg/d, Cmax= 34 ng/mL, and AUC (0-24 h)= 399 ng*h/mL; slow elimination indicated that multiple administration may result in accumulation | Metabolized mainly by P4503A4 | Information not available | |
|
Bosutinib (Bosulif) (Pfiizer) |
Food increases exposure; following 15 daily doses of bosutinib 500 mg with food: Cmax = 200 ng/mL; AUC = 3650 ng∙h/mL; compared to initial administration, plasma drug exposure did not increase significantly; following 15 daily doses 400 mg once daily: AUC =2235 ng*h/mL; Tmax=4 h; Has acceptable exposure; Vd= 6080 ± 1230 L; (substrate of ABCB1) |
Metabolized mainly by CYP3A4, which can increase AUC and Cmax |
500 mg orally once daily (chronic myeloid leukmia (chronic and accelerated phases and blast crisis with resistance/intolerance to prior therapy)); 400 mg orally once daily (newly diagnosed chronic myeloid leukemia (chronic phase)); 94% binding to human plasma proteins in vitro; 96% bound to human plasma proteins in healthy subjects ex vivo |
Pleural effusion is the main lung toxicity associated with bosutinib; 8% of patients in one study developed pleural effusions (207) |
|
Baricitinib (Olumiant) (Eli Lilly) |
Rapid absorption; oral bioavailability=79 %; median time to peak plasma concentration (Tmax) 1h; food decreases exposure by up to 14 % and decreases peak plasma concentration (Cmax) by up to 18 % and Tmax by 0.5 h; Vd= 76 L (IV administration) |
Metabolized by CYP3A4; less than 10% of total dose prone to metabolism |
2 mg orally once daily; 50% binding |
Shown in clinical trials to cause a modest increase in upper respiratory tract infections (47) |
|
Ruxolitinib (Jakafi) (Incyte Corporation) |
Rapid absorption; not affected by food; Cmax, 15 mg, healthy subject = 649 nmol/L; Tmax 15 mg, healthy subject = 1.5 h; Vd= 76.6 L |
Metabolized by CYP3A4 |
Starting dose 5-20 mg orally twice daily (depending on platelet count, for myelofibrosis); 97% binding (HSA) |
Pleural effusion, pulmonary hypertension exacerbations, and acute respiratory distress are extremely rare (208); although rare, mild acute respiratory distress syndrome may occur secondary to ruxolitinib treatment (209) |
|
Fedratinib (Inrebic) (Celgene) |
Not affected by high fat breakfast; 400mg oral dose: Cmax= 1804ng/mL, AUC= 26,870 ng/*h/mL (210); rapidly absorbed, peak plasma concentration after 3 h after dosing; exposure increased in a greater than dose-proportional manner; Vd= 1770L |
Metabolized by CYP3A4, CYP2C19, flavin-containing monooxygenase 3; CYP3A4 inhibitor can increase exposure of tofacitinib in plasma |
400 mg orally once daily; reduced dose for patients taking strong CYP3A inhibitors or with severe renal impairment; > 92% binding |
|
|
Tofacitinib (XELJANZ XR) (Pfizer) |
AUC not affected by fatty meals, but reduction in Cmax by 32%; rapidly absorbed, plasma concentrations and total radioactivity peaking 1 h after oral dosing; after single oral dose (10 mg), Cmax=98.3 ng/mL, Tmax=0.5 h; AUC (0-infinity)=274 ng*h/mL; T1/2=2.49 hr; Absolute bioavailability=74% oral absorption; No accumulation effect; Vd= 87L (IV administration) |
Metabolized mainly by hepatic CYP3A4 and to a lesser extent by CYP2C19 |
5 mg orally twice daily; extended release 11 mg orally once daily; 40% binding (HSA) |
Increased risk of blood clots in the lungs and death when a 10 mg twice daily dose of tofacitinib was used in patients with rheumatoid arthritis. FDA has not approved this 10 mg twice daily dose for RA; this dose is only approved in the dosing regimen for patients with ulcerative colitis (163); pulmonary complications were only described in less than 1% of the patients participating in several clinical trials (211) (110) |
|
Gefitinib (Iressa) (AstraZeneca/Tiva) |
Bioavailability not affected by food; slowly absorbed following oral administration; mean bioavailability=60%. Peak plasma levels 3-7 h following dosing; Vd= 1400 L (IV administration) |
Metabolized mainly by hepatic CYP3A4 |
250 mg orally once daily; 90% binding (AAG, HSA) |
Associated with increased incidence of interstitial lung disease, which often acts as a precursor to pulmonary fibrosis; approximately 1 percent of patients treated with gefitinib develop pulmonary toxicity, within the first few months of treatment; gefitinib-related interstitial lung disease is generally uncommon (212) (213) (140) (214); shown to exacerbate bleomycin-induced pulmonary fibrosis in preclinical models (215) |
|
Afatinib (Gilotrif) (Boehringer Ingelheim) |
High fat meal decreases exposure by 50% (Cmax) and 39% (AUC (0 - infinity); following oral dosing, Tmax=2 to 5 h; Cmax and AUC (0-infinity) values increased slightly more than dose proportional in range 20 to 50 mg; geometric mean relative bioavailability of 20 mg tablets=92% compared to oral solution; Vd= 4500 L (suggests potentially high tissue distribution) (216); (P-gp substrate) (181) |
Enzyme-catalyzed metabolism plays insignificant role in vivo |
40 mg orally once daily; 30 mg orally once daily in patients with severe renal impairment; in vitro binding to human plasma proteins is around 95%; binds to proteins both non-covalently (traditional binding) and covalently |
In an NSCLC clinical trial, among 230 treated patients, there were 3 cases of potential interstitial lung disease (1 %); in another NSCLC clinical trial, of 242 treated patients, 1 developed grade 4 interstitial lung disease however recovered (217) (218) |
|
Lapatinib (Tykerb and Tyverb) (GlaxcoSmithKline) |
Incomplete/variable absorption after oral dosing; average absolute bioavailability 25% or less; consistent with low absorption/solubility, peak plasma concentrations do not occur until 4 h after dosing; following 25 mg oral dose, the median Tmax=3 h; geometric mean (95% CI) values; Cmax=349 ng/mL; AUC (0-infinity)=4410 ng*h/mL; half-life 14.8 h; absorption limited by first-pass metabolism by CYP3A4/5 and low solubility; transporters possibly involved, although lapatinib not a P-gp substrate (ABCB1) (219) |
Metabolized mainly by CYP3A4 and CYP3A5 and to a lesser extent by CYP2C19 and CYP2C8 |
1,250 mg orally once daily continuously in combination with capecitabine (for metastatic breast cancer); 1,500 mg orally once daily in combination with letrozole (for hormone receptor positive HER2 positive metastatic breast cancer); >99% binding (AAG, HSA) |
Unlike gefitinib and erlotinib, pulmonary toxicity due to lapatinib is very rare; only one case of interstitial pneumonitis has been reported for lapatinib (220) |
|
Osimertinib (Tagrisso) (AstraZeneca) |
Cmax=6 h (median time); Vd=986 L |
Metabolized mainly by CYP3A and metabolized to two pharmacologically active metabolites, AZ7550 and AZ5105 |
80 mg tablet orally once daily; 95% binding |
Interstitial lung disease associated with osimertinib; (221) the incidence of interstitial lung disease associated with osimertinib is unclear due to small sample sizes in published reports (222) |
|
Erlotinib (Tarceva) (Genentech, OSI Pharmaceuticals (US), Roche (elsewhere)) |
Bioavailability significantly enhanced by food to nearly 100%; 60% absorption following oral dosing; peak plasma levels 4 h after dosing; Vd= 232 L |
Metabolized mainly by hepatic CYP3A4 and to a lesser extent by CYP1A2 and extrahepatic isoform CYP1A1 |
150 mg (for non-small cell lung cancer); 100 mg (pancreatic cancer); 93% binding (AAG, HSA) |
Interstitial lung disease associated with erlotinib; approximately 1 percent of patients treated with erlotinib develop pulmonary toxicity, within the first few months of treatment (223) (140) |
|
Neratinib (Nerlynx) (Puma Biotechnology) |
High fat meal increases Cmax by 1.7-fold and increases total exposure by 2.2-fold; standard meal increases Cmax by 1.2-fold, increases total exposure by 1.1-fold; proton pump inhibitors decrease Cmax by 71% and decrease total exposure by 65%; neratinib/metabolites have a Tmax=2-8 h; Vd= 6433 L |
Metabolized mainly by CYP3A4 |
240 mg orally once daily; >99% binding (AAG, HSA) |
In a Phase III study, neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET), interstitial lung disease occurred in two patients in the neratinib group and one patient in the placebo group, pulmonary fibrosis in one and two patients, respectively, and pneumonitis in one patient in each group (224) |
|
Pazopanib (Votrient) (Novartis) |
Slow and incomplete absorption and bioavailability; over 50-2000 mg, absorption nonlinear (in cancer patients); substantial accumulation in patients receiving 800 mg once daily (22 days); bioavailability (cancer patient)=21% for oral tablet 800 mg; Cmax= 58.1 μg/mL; AUC= 1037 μg*h/mL; Vd= 11.1 L (IV administration 5 mg) |
Metabolized mainly by CYP3A4 and to a lesser extent by CYP1A2, CYP2C8 |
Not to exceed 800 mg; reduce to 200 mg daily in patients with moderate hepatic impairment; not recommended in patients with severe hepatic impairment; >99% binding |
Pneumothorax was reported in 3%-14% of pazopanib-treated patients in clinical trials (225) (226) |
|
Sorafenib (Nexavar) (Bayer and Onyx Pharmaceuticals) |
High fat meal decreases bioavailability by 29%; mean relative bioavailability=38-49% for tablet form; peak plasma levels achieved 3 h after dosing; Vd= 213 L (suggests potentially high tissue distribution despite a high level of plasma protein binding, likely due to high lipophilicity) (227) |
Metabolized mainly by hepatic CYP3A4; glucuronidation mediated by UGT1A9 |
400 mg (2x200 mg tablets) orally twice daily; 99.5% binding (AAG, HSA) |
There have been several reported cases of sorafenib-induced interstitial lung disease (203); pulmonary toxicity in association with sorafenib has been reported to be uncommon (228) |
|
Sunitinib malate (Sutent) (Pfizer) |
Bioavailability not affected by food; after oral dosing, Cmax observed 6-12 h (Tmax) Vd= 2230 L (substrate for ABCB1) (184) |
Metabolized mainly by CYP3A4 |
50 mg orally once daily (4 weeks on, 2 weeks off); 37.5 mg orally (continuous daily dosing); 95% binding for sunitinib, 90% binding for sunitinib’s primary metabolite (HSA) |
Dyspnea and cough have been reported in association with sunitinib treatment (229); there are no reports of sunitinib treatment-induced pneumonitis. |
|
Axitinib (Inlyta) (Pfizer) |
Following 5 mg dose, 2.5-4.1 h to reach Cmax; Cmax=32.2ng/ml, Tmax=3.2h, AUC (0-infinity)=160ng*h/ml, T1/2= 5.4 h; Vd=275L |
Metabolized mainly by CYP3A4 and CYP3A5 and to a lesser extent by CYP1A2, CYP2C19, UGT1A1 |
Starting dose 5 mg orally twice daily; >99% binding (moderate to AAG; preferential to HSA) |
The toxicity profile of axitinib in a Phase II clinical trial was consistent with the one reported with the VEGFR-TKI family with grade 3–4 adverse effects, including dyspnea (14.5%) as a respiratory symptom (230); in clinical trials, fatal pulmonary embolism was reported in 1/359 patients (<1%) receiving axitinib (Pfizer Labs Patient Information approved by FDA) |
|
Vandetanib (Caprelsa) (Sanofi Genzyme) |
Slow absorption; Cmax reached at median 6 h; Vd= 7450 L |
Metabolized by CYP3A4, flavin–containing monooxygenase enzymes FMO1 and FMO3 |
300 mg orally once daily; 90% binding (HSA) |
Interstitial lung disease and pneumonitis have been reported more often in patients receiving vandetanib as compared to those receiving placebo; fatal adverse reactions for patients receiving vandetanib (2%) were respiratory failure and arrest, aspiration pneumonia, cardiac failure with arrhythmia, and sepsis (231) |
|
Regorafenib (Stivarga) (Bayer) |
Cmax= 2.5 μg/mL; Tmax= 4 h; AUC= 70.4 μg*h/mL; mean relative bioavailability of tablets=69% to 83%; Vd= over 24 h dosing, enterohepatic circulation, multiple plasma concentration peaks; (inhibitor of P-gp) |
Metabolized by CYP3A4 and UGT1A9 (232) (metabolites substrates of Pgp) |
Starting dose 160 mg orally once daily for three weeks, followed by a one week treatment abstinence; 99.5% binding |
|
|
Ibrutinib (Imbruvica) (Pharmacyclics/Janssen) |
Rapid absorption following oral dosing; Cmax=35 ng/mL; Tmax=1-2 h; AUC= 953 mg*h/mL; Vd= 10,000 L |
Metabolized mainly by CYP3A5 and CYP3A4 and to a lesser extent by CYP2D6 (233) |
560 mg orally once daily (lymphoma); 420 mg orally once daily (chronic lymphocytic leukemia, non-Hodgkin’s lymphoma, Graft versus host disease); Irreversible protein binding=97.3% of administered dose (AAG, HSA) |
Shown to be an irreversible inhibitor of mutant EGFR in NSCLC (234), shown to exacerbate bleomycin-induced pulmonary fibrosis in preclinical models (235) |
|
Palbociclib (Ibrance) (Pfizer) |
Cmax 6-12 h following oral dosing; oral bioavailability =46%, steady-state reached after 8 days, median accumulation ratio of 2.4; Vd= 2583 L (suggests potentially high tissue distribution) (236) |
Metabolized mainly by CYP3A and the sulfotransferase 2A1 |
125 mg capsule orally once daily for 21 days followed by one week drug abstinence; binding to human plasma proteins accounts=85% of administered dose |
There is a small risk of potentially severe lung inflammation in palbociclib-treated patients. |
|
Abemaciclib (Verzenio and Verzenios) (Eli Lilly) |
Following oral dose 200 mg,Cmax=158 ng/mL (after 6 h); Tmax=4-6 h following oral dose 50-275 mg, but could range up to 24 h; Absolute bioavailability=45%; Vd=690.3L |
Metabolized by CYP3A4 |
200 mg tablet orally twice daily (as single agent); 95-98% (HAS, AAG) |
There is a small risk of potentially severe lung inflammation in abemaciclib-treated patients. |
|
Alvocidib (Tolero Pharmaceuticals) |
Dose (infusion dose plus loading dose), mg, 30+30, AUC (0-infinity) 14.5 uM*h/mL; Vz value = 367 L | No information available | >95% binding (HSA) | Alvocidib-related pro-inflammatory syndrome is associated with induction of IL-6 (237) |
|
Ceritinib (Zykadia) (Novartis) |
Cmax after approximately 4 to 6 h following oral dosin;g Vd= 4230 L (after 750 mg) |
Metabolized mainly by CYP3A |
450 mg orally once daily; 97% binding |
Pulmonary toxicity, such as interstitial lung disease, is a rare side effect associated with ALK inhibitors; most can be managed efficiently by lowering doses or interrupting treatment; in a clinical trial, pneumonitis was reported in 4% of ceritinib-treated patients (238) (239) (240) |
|
Crizotinib (Xalkori) (Pfizer) |
High-fat meal decreases Cmax and AUC; Cmax 4 to 6 h following oral dosing; M=Mean absolute bioavailability=43% after 250 mg oral dose; Vd= 1772 L (after IV administration 50 mg) (suggests potentially high tissue distribution) |
Metabolized by CYP3A4, CYP3A5 |
250 mg orally twice daily; 91% binding |
Pulmonary toxicity, such as interstitial lung disease, is a rare side effect associated with ALK inhibitors; most can be managed efficiently by lowering doses or interrupting treatment; crizotinib was responsible for adverse pulmonary interstitial lung disease and severe pneumonitis in a small percentage of patients (238) (239) (240); associated with ground-glass opacity predominant pattern interstitial lung disease (151) |
|
Masitinib (Masivet) (AB Science) |
Absorption: mean Tmax between 1.7 and 4.7 h; following oral administration of 8.4mg/kg (dog); good absorption/exposure with AUC (0-24 h)=4045 ng*h/mL | Phase I metabolic pathways: reduction, demethylation, hydroxylation, oxidative deamination, oxidation and N-oxide formation; phase II metabolic pathways: direct conjugation of masitinib, N-demethyl metabolites and oxidative metabolites with glucuronic acid | Information not available | |
|
Nintedanib (Ofev and Vargatef) (Boehringer Ingelheim) |
Fatty meal increased Cmax 15% and AUC by 20%; following oral dosing, Tmax after 2 hours in fasted patients, 4 hours in fed patients; absolute bioavailability is low (4.7%), likely due to P-gp transporters and significant first-pass metabolism (241); Vd= 1050 L (IV administration) (suggests potentially high tissue distribution) |
CYP3A4 plays a minor role, accounting for 5% metabolism; esterase cleavage accounts for 25% metabolism |
150 mg orally twice daily; 100 mg orally twice daily in patients with mild hepatic impairment; 97.8% binding (HSA) |
In placebo-controlled INPULSIS® trials, among adverse events leading to permanent treatment discontinuation was pneumonia (0.9%) (242) |
The majority of kinase inhibitors listed are recommended for repurposing for COVID-19 based on the volume of distribution (Vd), or the theoretical volume necessary to contain the amount of a dosed drug at the same concentration observed in plasma, the area under the curve (AUC), which defines the variation of a drug concentration in plasma as a function of time (AUC0-infinity describes total drug exposure across time), and maximum plasma levels (Cmax), or peak serum concentration achieved by a drug in an identified part of the body following administration of a drug dose. There are several drugs, however, which raise some concerns with respect to pharmacokinetic properties, with limitations that would need to be overcome in order to serve as appropriate therapeutics for SARS-CoV-2 infection. These drugs include nilotinib, ponatinib, saracatinib, tofacitinib, pazopanib, and axitinib (Table 3). For nilotinib, based on the dosage and bioavailability, the drug concentration is adequate, however the volume of distribution (0.55-3.9 L/kg) suggests that nilotinib is mainly distributed in the blood and poorly distributed in tissue. For ponatinib, the Cmax and Tmax of ponatinib were reported as 73 ng/mL and 6 hours, respectively, which suggests that drug absorption is slow and plasma drug concentrations are low. To increase exposure in the blood, ponatinib would need to be taken continuously for a number of days, and this would not be ideal for the rapid treatment necessary for a COVID-19 patient. For saracatinib, both the Cmax (34 ng/mL) and AUC (399 ng*h/mL) are low, which suggests that dosing continuously for a number of days could potentially increase the blood drug concentration, which is not desirable. For tofacitinib, an oral dose of 5 mg/kg, Cmax=34 ng/mL, AUC=144ng*h/mL and a half-life of 2.49h would require long-term dosing to achieve optimal drug concentrations and anti-inflammatory effects. Based on this timeline, this would not be ideal for the rapid treatment required for a patient with COVID-19. Pazopanib has been reported clinically to be associated with severe hepatotoxic deaths, and thus there may be potential safety issues for patients. The potential toxicity associated with pazopanib and the volume of distribution (only 11.1 liters) are issues that would need to be addressed for repurposing for COVID-19 treatment. For axitinib, the Tmax (3.2 hrs) and AUC0-infinity (160 mg*h/mL) values were very low, suggesting that multiple doses are necessary. Axitinib is prone to causing elevated blood pressure and arterial thromboembolism events, especially for elderly people, which for an older COVID-19 patient would mean a high risk of death. Lapatinib is more complicated and the following should be taken into consideration prior to using lapatinib as a therapy for COVID-19 patients: The bioavailability is not reported to be high and the recommended dose is considerably high, which are not ideal characteristics. However, the drug is likely to be safe at high doses, meaning that optimal blood concentrations can be reached, with a half-life of 14.8 hours.
Kinase inhibitors as potential therapeutics for COVID-19 respiratory complications
Kinase inhibitors that have been approved for treatment of various malignancies have properties, such as anti-inflammatory and cytokine inhibitory activity, which may be able to reduce the likelihood of life-threatening conditions due to lung damage from respiratory virus infections. Numerous small molecule kinase inhibitors target proteins associated with severe respiratory distress, including cytokines (such as IL-6 and TNF-alpha) that contribute to cytokine release syndrome and sHLH, as well as proteins associated with inflammation and induction of pulmonary fibrosis (such as the pro-inflammatory cytokine TGF-beta).
ABL, PDGFR, and SRC inhibitors
Cytokine inhibition and anti-inflammatory and antifibrotic activity displayed by some inhibitors of Abelson murine leukemia viral oncogene homolog 1 or 2 (ABL1, ABL2), platelet-derived growth factor receptor, and SRC (proto-oncogene encoding a non-receptor tyrosine kinase, similar to the v-Src gene of the Rous sarcoma virus), could potentially provide benefit for SARS-CoV-, MERS-CoV-, or SARS-CoV-2-infected patients (77). For instance, the ABL inhibitor, ponatinib, exhibited cytokine storm suppression in a preclinical model of influenza (78). Imatinib inhibited TNF-alpha production in murine models of acute hepatitis and prevented TNF-alpha-dependent acute liver inflammation in these models (77), and attenuated signaling associated with rheumatoid arthritis, such as KIT-mediated signaling and TNF-alpha release by mast cells, macrophage FMS activation and production of cytokines (79). Nilotinib and bosutinib showed activity against pulmonary fibrosis and other models of fibrosis, through regulation of levels of pro-inflammatory cytokines such as IL-1 and IL-6 (80) (81) (82) (83) (84) (85) (86) (87) (88) (89).
Case study reports and small clinical trial data exist, generally in favor of the anti-inflammatory and antifibrotic effects of imatinib, although results have been variable. Two targets of imatinib are ABL, which is a key downstream mediator of profibrotic TGF-beta signaling, and PDGFR, also associated with fibrotic diseases (90). In chronic myeloid leukemia (CML) and gastrointestinal stromal tumor (GIST) patients, imatinib treatment improved rheumatoid arthritis symptoms, suggesting anti-inflammatory activity, and downregulated proinflammatory cytokines, IL-6 and IL-8 (91) (92) (93). Antifibrotic effects of imatinib were demonstrated in two patients with nephrogenic systemic fibrosis, with each patient showing progressive reduction of skin thickening and tethering following the start of imatinib treatment (94), and pulmonary fibrosis improved in a patient treated with imatinib for the 20 weeks the patient was on therapy (95). Antifibrotic activity of imatinib was also demonstrated in a patient with bleomycin interstitial pneumonitis, a condition sharing biochemical and histological features with idiopathic pulmonary fibrosis that is caused by the antibiotic chemotherapy agent bleomycin (96). However, imatinib was not observed to affect lung function or survival in idiopathic pulmonary fibrosis patients followed for 96 weeks in a randomized, placebo-controlled clinical trial (97), and limited success was observed for imatinib in a Hodgkin’s lymphoma patient with bleomycin interstitial pneumonitis due to adverse effects including thrombocytopenia with gastrointestinal bleeding (98).
SRC kinases are activated by profibrotic cytokines TGF-beta and PDGF (99), and SRC kinases are important for inflammatory responses (100). Dasatinib has been proposed as an agent for fibrotic diseases, based on its inhibition of TGFbeta-induced myofibroblast differentiation through SRC-mediated signaling in vitro (101). Dasatinib blocked production of pro-inflammatory cytokines in a model of autoimmune arthritis, including IL-1, TNF-alpha, and IL-6, and stimulated production of the anti-inflammatory cytokine IL-10 (102) (103), and caused macrophages to change to an anti-inflammatory phenotype marked by high IL-10 production and suppression of levels of pro-inflammatory cytokines (IL-6, TNF-alpha) (104). Preclinical studies with the SRC/ABL inhibitor, saracatinib, which has orphan drug status for idiopathic pulmonary fibrosis, showed that it decreases collagen deposition and fibroblast activity, which are characteristic of lung fibrosis (105). Specifically, saracatinib, in an in vitro lung fibroblast model, inhibited TGF-beta-induced SRC activation and consequently inhibited myofibroblast differentiation, supporting the notion that SRC promotes myofibroblast differentiation and lung fibroblast activation (105). Saracatinib also showed efficacy in a mouse model of bleomycin-induced lung fibrosis (105).
JAK inhibitors
Selective JAK inhibitors, such as baricitinib, through targeted inhibition of JAK1 and JAK2, inhibit production of cytokines, including IL-2, IL-6, GM-CSF, and IFN-gamma and exhibit significant anti-inflammatory effects in animal models (106) (107). Baricitinib, ruxolitinib, and tofacitinib are anti-inflammatory treatments for rheumatoid arthritis (108) (109) (110), with suppression of inflammatory cytokines associated with rheumatoid arthritis, including TNF-alpha, IL-6, IL-17, and IFN-gamma (111). Ruxolitinib has been observed to normalize the cytokine profile of myelofibrosis patients (112). Due to the JAK inhibitory activity of more multi-targeted agents such as midostaurin (Rydapt; Novaris), lestaurtinib (Cephalon), and sunitinib (Table 2, Fig. 3), each has anti-inflammatory potential as well as potential to combat cytokine release syndrome, which could benefit patients infected with respiratory viruses (107).
The peripheral blood of a patient with severe COVID-19 was shown to have a substantially high number of CCR6+ T helper 17 cells (TH17), a subset of pro-inflammatory T helper cells that produce IL-17 (1), and MERS-CoV and SARS-CoV patients also showed increased TH17 responses or IL-17-mediated signaling (113) (114). The TH17 type response is associated with the cytokine storm in SARS-CoV-2 infection that leads to pulmonary edema and lung damage. The JAK2 inhibitor, fedratinib, was observed to suppress production of TH17-related cytokines and is proposed to be potentially useful for patients with COVID-19 suffering from TH17-related cytokine storm (115).
EGFR inhibitors
Studies suggest that inhibiting EGFR signaling might prevent an excessive fibrotic response to SARS-CoV and other respiratory infections (like that characteristic of COVID-19). EGFR plays a role in interstitial lung disease, and interaction between EGF and TFG-beta signaling is believed to drive development of fibrosis (116) (117). The role of EGFR signaling in the development of lung fibrosis is complex, though, with data suggesting both profibrotic and antifibrotic roles for EGFR signaling, at least in part seeming to depend on the trigger for fibrosis (13). Gefitinib inhibited TGF-beta1 induction of fibrosis in vivo (118) and inhibited bleomycin-induced fibrosis in a mouse model (119), and erlotinib was reported to block fibrosis development in a variety of in vivo models (13).
TGF-beta induces the expression of EGFR ligands, which in turn activate EGFR. Of relevance, TGF-beta was one of several pro-inflammatory cytokines that were observed to be highly upregulated in SARS-CoV patients (120) (121) (122), and mouse models of SARS-CoV infection showed interferon, cytokine and lung-associated wound-healing and ARDS-related genes (123). These findings are consistent with TGF-beta being profibrotic, as has been demonstrated in animal models (124). The kinase inhibitor, sorafenib, attenuated bleomycin-induced pulmonary fibrosis in a preclinical model (125) and ameliorated fibrosis in liver fibrosis models through STAT3 inhibition and downregulation of TGF-beta- and PDGFRβ-mediated pathways of fibrogenesis (126).
The EGFR inhibitor, osimertinib, is metabolized and broken down into two pharmacologically active metabolites (AZ7550 and AZ5104), which circulate at around 10% of the concentration of the parent compound (Table 3). One metabolite, AZ5104, which is more potent than osimertinib, downregulates Th17-related cytokine production via inhibition of SRC-ERK-STAT3 (127) (Table 2).
Other kinase inhibitors
Among numerous other kinase inhibitors with demonstrated therapeutic potential are axitinib, which, through VEGFR-3 (vascular endothelial growth factor receptor-3) inhibition, improved lymphangiogenesis and oxygen saturation in preclinical model of aspiration pneumonia (128). Nintedanib is approved for idiopathic pulmonary fibrosis and displays anti-inflammatory activity through TNF-alpha and IL-6 inhibition (129) (130) (131). Ibrutinib exerted anti-inflammatory effects in a model of neuroinflammation-related disease (132) and mitigated acute lung inflammation in a model of pneumococcal pneumonia (133). Alvocidib also shows anti-inflammatory activity by blocking leukocyte-endothelial association by inhibiting CDK9 (134). Pazopanib exhibits antifibrotic activity through modulating inflammatory cytokines, and sunitinib inhibited bleomycin-induced pulmonary fibrosis in mice (135) (136). Sunitinib, believed to primarily work through PDGFR-mediated signaling, was also shown to suppress cytokine storm in a mouse model (137). Finally, sunitinib was shown to synergize with an anti-TNF antibody against lethal dengue infection (138).
Adverse pulmonary effects associated with kinase inhibitors
Pulmonary toxicity is reportedly a rare event with many targeted treatments. The incidence of lung toxicity with tyrosine kinase inhibitors is relatively low, although there is substantial variability in their occurrence with a reported range from 0.2-10.9% (139). However certain adverse side effects, such as pleural effusions associated with ABL inhibitors dasatinib or imatinib, interstitial lung disease associated with EGFR inhibitors erlotinib and gefitinib, or ALK inhibitors ceritinib or crizotinib, can occur but often reverse quickly with lowering the dose or terminating use (140). The timing of onset of toxicities following initial dosing needs to be considered for patients afflicted with cancer and other diseases, for whom therapy can be implemented for months, versus patients infected with a respiratory virus that require immediate treatment. Reported cases of adverse pulmonary effects for the listed kinase inhibitors are shown in Table 3.
Imatinib and dasatinib
Respiratory side effects of imatinib include pneumonia (1-10%). Generally, imatinib-induced pulmonary fibrosis and pneumonitis are very infrequently occurring (141) (142), and imatinib-induced pneumonitis develops in a median time of 49 days (143). In dasatinib-treated CML patients, pleural effusion and lung parenchyma changes (ground-glass or alveolar opacities and septal thickening) were described, however resolved after treatment was interrupted (144). The median time between dasatinib treatment initiation and respiratory symptoms was 229 days. In a case study of a dasatinib-treated Japanese patient, pneumonia developed two years after initiation of dasatinib therapy, and drug discontinuation along with corticosteroid therapy greatly improved symptoms (145).
Erlotinib and gefitinib
Pulmonary toxicities associated with erlotinib have been infrequently reported. Two cases were described that developed acute pneumonitis (chest tomography scan showed bilateral ground-glass infiltrates), 5-6 days following initiation of erlotinib treatment (146). Interstitial lung disease has been observed as a serious adverse side effect for gefitinib (147), with a 0.3% incidence in the U.S. and a 2% incidence in Japan. The median onset of gefitinib-induced interstitial pneumonia in the U.S. was 42 days, and in Japan was 24 days, with around one-third of all cases caused by gefitinib being fatal (148).
Ceritinib and crizotinib
Interstitial lung disease/pneumonitis resulting from ALK inhibitors is relatively rare (1.2-8% of patients) (149) (150) (151). In a case study of a Korean ALK-rearranged metastatic lung adenocarcinoma patient, ceritinib induced organizing pneumonia (152). Treatment was ceased and the patient was treated with antibiotics and recovered. In a study testing crizotinib in Japanese patients with ALK-positive non-small cell lung cancer, the incidence of interstitial lung disease was 5.77%, and interstitial lung disease developed within 4 weeks in 41.9% patients from the start of crizotinib treatment and within 8 weeks in 69.2% of patients (153). In a clinical study of 250 NSCLC patients treated with ALK inhibitors, including crizotinib or ceritinib, the median time from the start of treatment to the development of pneumonitis, which occurred in 11 of the patients, was 5 months (range 0.5-11 months) (154).
Risk of infection due to kinase inhibitor treatment
For ABL inhibitors, including imatinib, dasatinib, nilotinib, basutinib, and ponatinib, there is a modest increased risk of overall infection, with a risk of invasive fungal infection, tuberculosis, and cytomegalovirus (especially with dasatinib, particularly after hematopoietic stem cell transplantation), and a risk of hepatitis B virus reactivation (155). For the BTK/EGFR inhibitor, ibrutinib, there is a modest increased risk of overall infection, with a risk of pneumocystis jirovecil pneumonia, invasive fungal infection, and progressive multifocal leukoencephalopathy, and a risk of hepatitis B virus reactivation (155). For JAK inhibitors, including ruxolitinib, tofacitinib, baricitinib, there is a major increased risk of overall infection, with a risk of pneumocystis jirovecil pneumonia, herpes zoster, tuberculosis, cytomegalovirus, Epstein-Barr virus, and progressive multifocal leukoencephalopathy, as well as a risk of hepatitis B virus reactivation (155).
It should be noted that the overall risk of a COVID-19 patient being treated with JAK inhibitors and afflicted with tuberculosis as a side effect is likely exceptionally low, especially given that for a COVID-19 patient, treatments for many of the trials are carried out for a couple of weeks. The risk of developing serious infections, such as tuberculosis, is higher for patients that are on medication causing chronic immunosuppression, such as would be the case for a patient with a chronic illness like rheumatologic disorders, or patients with latent tuberculosis. However, with a short course of treatment in the case of a COVID-19 patient, it is unclear whether the period of immunosuppression would be long enough to result in a meaningful risk. In addition, latent tuberculosis can be tested for rather quickly (1-2 days) with a T-spot. TB test. This would normally be carried out for patients treated with JAK inhibitors, although there may be more of a delay than is ideal for patients with high risk COVID-19.
Clinical trials: single agent and combination therapy approaches
Based on a query of www.ClinicalTrials.gov, which lists numerous ongoing trials for COVID-19, a number of studies were found that include testing of kinase inhibitors listed in this article. There are currently several COVID-19 clinical studies investigating imatinib as a single agent (NCT04346147, NCT04357613, NCT04356495). COVID-19 trials are ongoing that investigate ruxolitinib as a single agent and in combination with the lipid-lowering medication, simvastatin (NCT04348071, NCT04355793, NCT04354714, NCT04362137, NCT04334044, NCT04366232, NCT04338958, NCT04331665, NCT04337359, NCT04361903, NCT04348695, NCT04359290). Although there is no strong clinical evidence to date that statins are beneficial for COVID-19 patients and the limited evidence is mixed (156) (157), statins are still under consideration due to possible generation of a greater potent adaptive immune response and a decreased mortality rate associated with patients with influenza, pneumonia, and MERS-CoV (158) (159) (160) (161). COVID-19 clinical studies are investigating baricitinib, both as a single agent and in combination with the antiviral drugs, lopinavir-ritonavir (NCT04340232, NCT04362943, NCT04346147, NCT04358614, NCT04320277, NCT04321993, NCT04345289, NCT04366206). Baricitinib does not interact with antiviral agents due to its prevalent renal elimination, and so it is proposed to suitable for combination therapy (162). There is one study investigating nintedanib, an FGFR (fibroblast growth factor receptor)/PDGFR/VEGFR inhibitor approved for idiopathic pulmonary fibrosis, as a single agent treatment for pulmonary fibrosis in patients with moderate to severe COVID-19 (NCT04338802).
A COVID-19 study is ongoing that investigates tofacitinib as a single agent at 10 mg twice a day for 14 days (NCT04332042). Of note, this dose of tofacitinib administration has been associated with an increased risk of thrombosis and death and the FDA has issued a boxed warning (163) (Table 3). In a clinical study investigating the predisposition of COVID-19 patients to venous and arterial thromboembolism, a 31% incidence of thrombotic complications, with pulmonary embolism being the most prevalent, was observed in intensive care unit SARS-CoV-2-infected patients (164). The blood clotting risk reported for tofacitinib pertains to patients receiving the drug chronically, and while the increased risk reported for tofacitinib at 10 mg twice daily for 14 days is not known, it is anticipated to be small. It is also general practice as a precaution to place hospital-admitted patients with COVID-19 on blood thinners as DVT/clot prophylaxis (most usually enoxaparin or heparin). This would likely make the risk of blood clots minimal (although not zero percent).
Though not included on www.ClinicalTrials.gov as a COVID-19 trial, results of a clinical trial with Waldenstrom’s macroglobulinemia patients suggest that ibrutinib might confer protection against lung damage in hypoxic COVID-19 patients, and it may possibly improve respiratory function (165). However, the study was small and involved 6 COVID-positive patients, 5 of whom received ibrutinib at 420 mg and presented with mild symptoms that did not require hospitalization. The 6th patient on a lower dose of ibrutinib had progressive dyspnea and hypoxia and was placed on treatments in addition to ibrutinib at the lower dose, including hydroxychloroquine, azithromycin and tocilizumab. Due to worsening hypoxia, the patient was eventually placed on the higher ibrutinib dose (420 mg) and this was followed by improvement of symptoms (165).
Kinase inhibitors with good safety profiles and desirable pharmacokinetics properties, including minimal association with drug transporters and CYP enzymes, warrant testing in combination with antiviral agents or other targeted agents, to more effectively decrease viral load and potentially more dramatically improve COVID-19 symptoms. There are currently numerous direct antiviral agents that are under consideration for COVID-19 (several prominent investigational drugs are shown in Fig. 4).
Figure 4.
Drug therapies under investigation for COVID-19.
Although imatinib is, at the time of the writing of this article, under investigation in COVID-19 patients as a single agent, it may effectively combine with certain antiviral agents and this might be an approach worth considering for COVID-19 trials. For instance, ribavirin has demonstrated synergy in vitro with imatinib against leukemia growth (166). Despite proposed lack of efficacy of ribavirin as a single agent against SARS-CoV-2 (167), it is possible that it could synergize with imatinib against SARS-CoV-2 if the drugs are able to be administered at doses that are effective but safe.
The drug-drug interactions between imatinib and a wide variety of antiviral and other agents have been thoroughly assessed. Imatinib displays variable drug-drug interactions and so its potential for effective combination needs to be taken on a case by case basis. For instance, protease inhibitors ritonavir-lopinavir and darunavir increase imatinib exposure, and saquinavir and indinavir decrease imatinib exposure (168). Contrarily, there is no interaction between imatinib and the antiviral/nucleoside analogs acyclovir and valaciclovir, although its intracellular exposure is reduced by ganciclovir and valganciclovir (168). The antimalarial drug, chloroquine, decreases imatinib intracellular exposure (168).
The FDA-approved tapeworm medication, niclosamide, reported as having antiviral activity against SARS-CoV and MERS-CoV is presently under investigation as a SARS-CoV-2 agent (169). Niclosamide has been reported (unpublished results; preprint) to be one of 24 FDA-approved drugs to show in vitro activity against SARS-CoV-2, with an IC50 of 0.28 μM (https://www.biorxiv.org/content/10.1101/2020.03.20.999730v3.full.pdf). The inhibitory activity of niclosamide against SKP2, which diminishes MERS-CoV replication and augments autophagy (170), is proposed to be the potential mechanism through which niclosamide acts against SARS-CoV-2. Niclosamide was demonstrated to synergize in preclinical studies with imatinib and other kinase inhibitors against different malignancies. For instance, synergy between niclosamide and imatinib, as well as niclosamide and dasatinib or ponatinib, against CML cells was demonstrated (171). Niclosamide was also found to potentiate the effects of erlotinib against head and neck cancer cells through STAT3 inhibition (172), with erlotinib against human colon cancer lines (173), and with sorafenib against human renal cell cancer cells (174).
EGFR-targeting kinase inhibitors are characterized by extensive tissue distribution, moderate to high plasma protein binding, and a relatively high volume of distribution (>1700 L) (175). Although not currently under investigation for COVID-19 as of this writing, the non-small cell lung cancer drug and EGFR inhibitor, afatinib, has been shown to be able to be safely administered with various antiviral agents in clinical studies (176) (177). In a phase I study in human papillomavirus (HPV)-associated head and neck squamous cell carcinoma, afatinib, with demonstrated anti-inflammatory and antifibrotic activity (116) (178) (179), was tested in combination with ribavirin and standard chemotherapy (176). Afatinib was used because of its targeting of ErbB proteins associated with HPV infection, and ribavirin was chosen due to its targeting of oncogenic eIF4E (180) (176). In this study, there were no dose-limiting toxicities, supporting the safe, clinical use of ribavirin with a kinase inhibitor having key virus-associated protein targets and those with respiratory benefit. Another clinical study showed low potential for interaction between afatinib, a P-gp pump transporter substrate, and the protease inhibitor, ritonavir, a potent inhibitor of P-gp (181) (177). This was partially attributed to the fact that afatinib is not a modulator of substrate of cytochrome P450 enzymes. It is possible that the combination of afatinib and antiviral agents, such as ribavirin or ritonavir, which show little activity on their own against COVID-19, may be synergistic in the context of the disease. Alternatively afatinib could potentially be combined with remdesivir, more recently shown to reduce the length of hospital stay for COVID-19 patients and thus exhibiting a degree of activity against SARS-CoV-2 in patients. Or perhaps afatinib could be investigated as a treatment for COVID-19 in combination with several antiviral drugs as part of a cocktail.
Afatinib has also been tested in combination with nintedanib in a Phase I dose-escalation study in patients with advanced solid tumors (182). It was determined that afatinib at 10 mg/day combined with nintedanib at 200 mg twice a day had a manageable safety profile, however the doses were subtherapeutic. The antifibrotic and anti-inflammatory potential of afatinib and nintedanib, coupled with key virus-associated protein targets for each (Table 2, Fig. 3), warrant investigation of this drug combination for treatment of COVID-19.
Ritonavir is a strong inhibitor of CYP3A4 and it also inhibits ABCB1, and the multi-targeted inhibitor sunitinib is metabolized by CYP3A4 and is a substrate for ABCB1 (183) (184). Consequently, this combination has the potential for reduced efficacy and/or increased toxicity. Sunitinib was investigated in HIV-positive cancer patients treated with ritonavir, and due to toxicities was recommended to be dosed at 37.5mg/day on a 4 week on/2 week off schedule in these patients (185). These results suggest that drug-drug interactions between sunitinib and ritonavir require dosing modifications for sunitinib. Should sunitinib, with key virus-associated targets and anti-inflammatory, cytokine-suppressive and antifibrotic potential, be considered for co-administration with a protease inhibitor like ritonavir for COVID-19, this established dosing regimen would need to be considered to control toxicity.
Table 4 shows the chemical structures and molecular weights of a panel of the most promising kinase inhibitors in terms of their pharmacokinetics, potential antiviral targets and anti-inflammatory, cytokine suppressive, or antifibrotic activity. Also included in Table 4 are those kinase inhibitors with potential to effectively synergize with other agents, including antiviral drugs.
Table 4.
Chemical structures of kinase inhibitor candidates for COVID-19 treatment. Chemical structures and molecular weights were obtained on chemspider.com
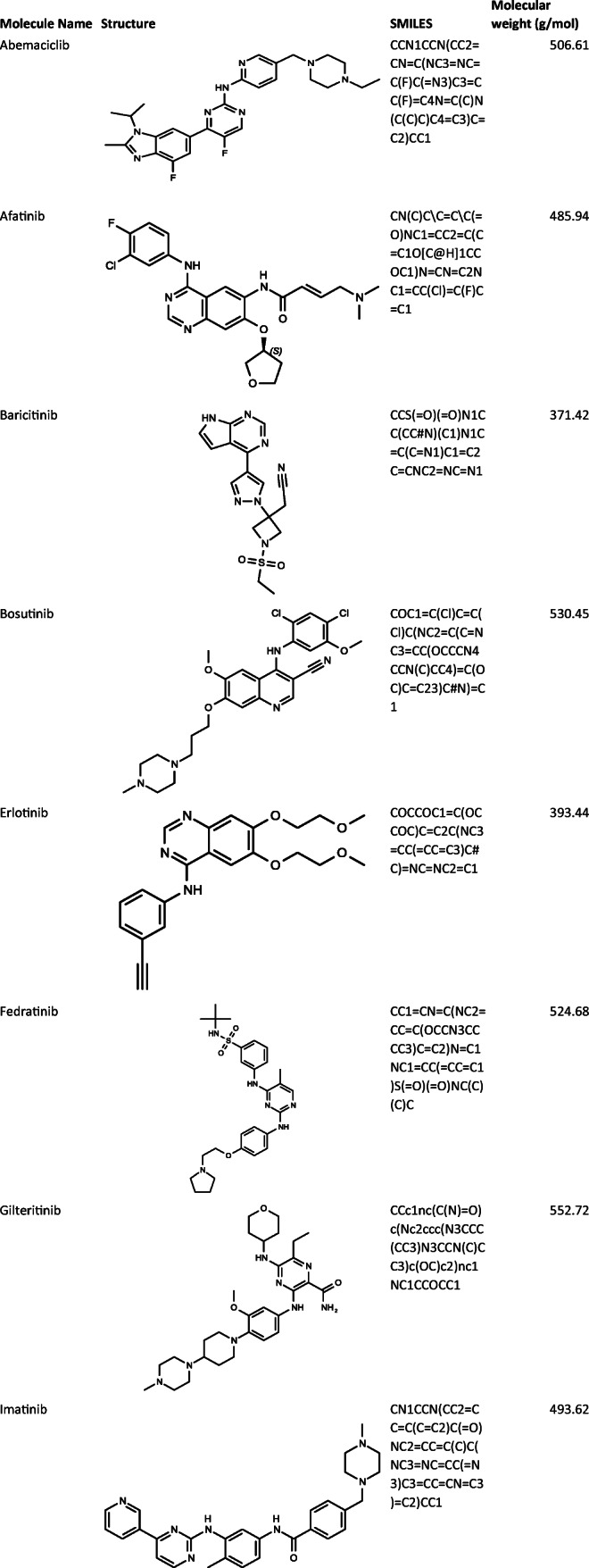
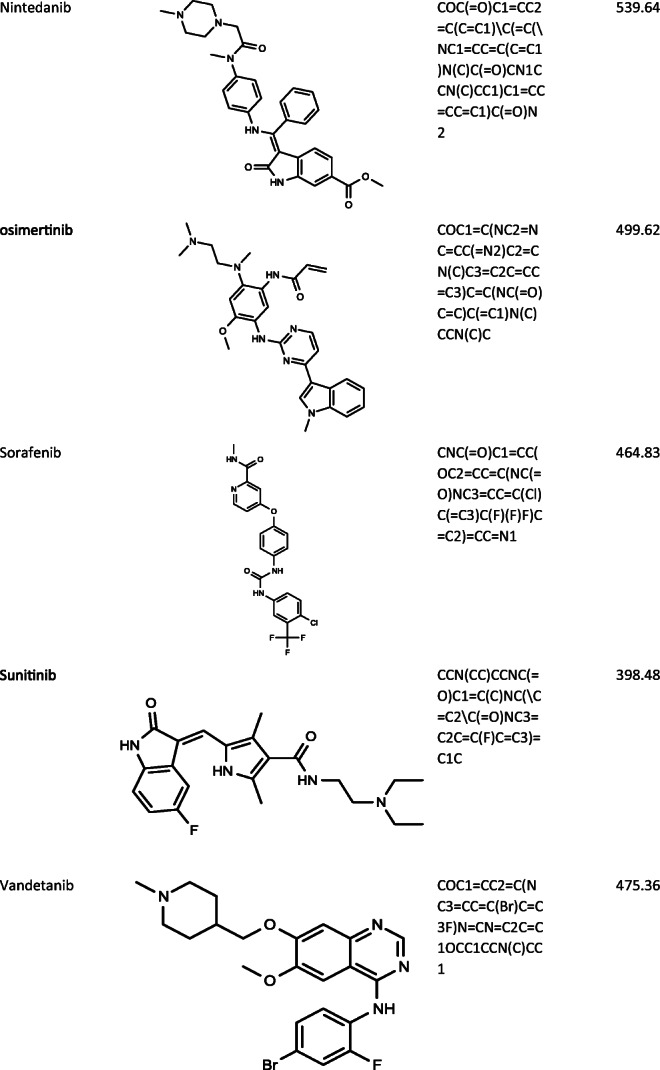
Conclusion
There are many factors to consider when repurposing approved drugs for a new indication, and identification of key protein targets that are potently inhibited offers an attractive option for a new therapeutic application. The urgency of need and constraints of time, however, which come with developing effective therapeutic approaches during a pandemic crisis can make it challenging to conduct well-controlled studies with data that definitively attribute efficacy to a drug. Numerous agents, which show promise based on preclinical studies and anecdotal data, are presently under clinical investigation as single agents or in combination with other therapies. Several kinase inhibitors are under clinical investigation for COVID-19 that target key virus-associated proteins as well as proteins that play a role in development of symptoms associated with COVID-19, including pneumonia, fibrosis and inflammation. For optimal drug repurposing, the pharmacokinetics of agents need to be taken into consideration. For instance, drugs that require long-term dosing to achieve optimal drug concentrations and anti-inflammatory effects, may not easily treat the symptoms of COVID-19 due to the immediacy of treatment requirement for afflicted patients. Similarly, adverse effects associated with some kinase inhibitors also need to be considered and may present a challenge for treatment of some COVID-19 patients. However, short-term dosing may minimize these risks.
Roads less traveled might also be considered over time as an alternative to the current therapies being tested in COVID-19 clinical trials, such as the combination of IL-6 blocking agents (tocilizumab sarilumab) or antiviral therapies (ribavirin, ritonavir-lopinavir, remdesivir, niclosamide), with kinase inhibitors (imatinib, osimertinib, gilteritinib, abemaciclib, afatinib, sunitinib, sorafenib, erlotinib), or the direct combination of kinase inhibitors with each other that target relevant virus-associated proteins and proteins associated with pulmonary health (sunitinib and erlotinib, or afatinib and nintedanib). As historically drug combinations and cocktails have offered substantial clinical benefit in the context of other life-threatening diseases, such as AIDS caused by HIV, there is reason to believe the same approach with drugs shown to safely combine and that have provided some benefit on their own, warrants testing in the context of the current SARS-CoV-2 pandemic.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cao YC, Deng QX, Dai SX. Remdesivir for severe acute respiratory syndrome coronavirus 2 causing COVID-19: An evaluation of the evidence. Travel Med Infect Dis. 2020;101647. [DOI] [PMC free article] [PubMed]
- 3.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gautier JF, Ravussin Y. A new symptom of COVID-19: loss of taste and smell. Obesity (Silver Spring) 2020;28(5):848. doi: 10.1002/oby.22809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al.. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020:200463. [DOI] [PMC free article] [PubMed]
- 7.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al.. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in covid-19. N Engl J Med 2020. [DOI] [PMC free article] [PubMed]
- 8.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seguin A, Galicier L, Boutboul D, Lemiale V, Azoulay E. Pulmonary Involvement in Patients With Hemophagocytic Lymphohistiocytosis. Chest. 2016;149(5):1294–1301. doi: 10.1016/j.chest.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Goulter AB, Goddard MJ, Allen JC, Clark KL. ACE2 gene expression is up-regulated in the human failing heart. BMC Med. 2004;2:19. doi: 10.1186/1741-7015-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med 2020. [DOI] [PMC free article] [PubMed]
- 12.Xia H, Lazartigues E. Angiotensin-converting enzyme 2 in the brain: properties and future directions. J Neurochem. 2008;107(6):1482–1494. doi: 10.1111/j.1471-4159.2008.05723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Venkataraman T, Coleman CM, Frieman MB. Overactive epidermal growth factor receptor signaling leads to increased fibrosis after severe acute respiratory syndrome coronavirus infection. J Virol. 2017;91(12). [DOI] [PMC free article] [PubMed]
- 14.Antonio GE, Wong KT, Hui DS, Wu A, Lee N, Yuen EH, et al. Thin-section CT in patients with severe acute respiratory syndrome following hospital discharge: preliminary experience. Radiology. 2003;228(3):810–815. doi: 10.1148/radiol.2283030726. [DOI] [PubMed] [Google Scholar]
- 15.Borges do Nascimento IJ, Cacic N, Abdulazeem HM, von Groote TC, Jayarajah U, Weerasekara I, et al. Novel coronavirus infection (covid-19) in humans: a scoping review and meta-analysis. J Clin Med. 2020;9(4). [DOI] [PMC free article] [PubMed]
- 16.Tezer H, Bedir DT. Novel coronavirus disease (COVID-19) in children. Turk J Med Sci. 2020;50(SI-1):592–603. doi: 10.3906/sag-2004-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alpert A, Pickman Y, Leipold M, Rosenberg-Hasson Y, Ji X, Gaujoux R, et al. A clinically meaningful metric of immune age derived from high-dimensional longitudinal monitoring. Nat Med. 2019;25(3):487–495. doi: 10.1038/s41591-019-0381-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baltimore D. Expression of animal virus genomes. Bacteriol Rev. 1971;35(3):235–241. doi: 10.1128/br.35.3.235-241.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morse JS, Lalonde T, Xu S, Liu WR. Learning from the Past: Possible Urgent Prevention and Treatment Options for Severe Acute Respiratory Infections Caused by 2019-nCoV. Chembiochem. 2020;21(5):730–738. doi: 10.1002/cbic.202000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katsiki N, Banach M, Mikhailidis DP. Lipid-lowering therapy and renin-angiotensin-aldosterone system inhibitors in the era of the COVID-19 pandemic. Arch Med Sci. 2020;16(3):485–489. doi: 10.5114/aoms.2020.94503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coyne CB, Bergelson JM. Virus-induced Abl and Fyn kinase signals permit coxsackievirus entry through epithelial tight junctions. Cell. 2006;124(1):119–131. doi: 10.1016/j.cell.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 23.Newsome TP, Weisswange I, Frischknecht F, Way M. Abl collaborates with Src family kinases to stimulate actin-based motility of vaccinia virus. Cell Microbiol. 2006;8(2):233–241. doi: 10.1111/j.1462-5822.2005.00613.x. [DOI] [PubMed] [Google Scholar]
- 24.Garcia M, Cooper A, Shi W, Bornmann W, Carrion R, Kalman D, et al. Productive replication of Ebola virus is regulated by the c-Abl1 tyrosine kinase. Sci Transl Med. 2012;4(123):123ra24. doi: 10.1126/scitranslmed.3003500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reeves PM, Smith SK, Olson VA, Thorne SH, Bornmann W, Damon IK, et al. Variola and monkeypox viruses utilize conserved mechanisms of virion motility and release that depend on abl and SRC family tyrosine kinases. J Virol. 2011;85(1):21–31. doi: 10.1128/JVI.01814-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clark MJ, Miduturu C, Schmidt AG, Zhu X, Pitts JD, Wang J, et al. GNF-2 Inhibits Dengue Virus by Targeting Abl Kinases and the Viral E Protein. Cell Chem Biol. 2016;23(4):443–452. doi: 10.1016/j.chembiol.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dyall J, Coleman CM, Hart BJ, Venkataraman T, Holbrook MR, Kindrachuk J, et al. Repurposing of clinically developed drugs for treatment of Middle East respiratory syndrome coronavirus infection. Antimicrob Agents Chemother. 2014;58(8):4885–4893. doi: 10.1128/AAC.03036-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sisk JM, Frieman MB, Machamer CE. Coronavirus S protein-induced fusion is blocked prior to hemifusion by Abl kinase inhibitors. J Gen Virol. 2018;99(5):619–630. doi: 10.1099/jgv.0.001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coleman CM, Sisk JM, Mingo RM, Nelson EA, White JM, Frieman MB. Abelson Kinase Inhibitors Are Potent Inhibitors of Severe Acute Respiratory Syndrome Coronavirus and Middle East Respiratory Syndrome Coronavirus Fusion. J Virol. 2016;90(19):8924–8933. doi: 10.1128/JVI.01429-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simmons G, Gosalia DN, Rennekamp AJ, Reeves JD, Diamond SL, Bates P. Inhibitors of cathepsin L prevent severe acute respiratory syndrome coronavirus entry. Proc Natl Acad Sci U S A. 2005;102(33):11876–11881. doi: 10.1073/pnas.0505577102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shirato K, Kawase M, Matsuyama S. Middle East respiratory syndrome coronavirus infection mediated by the transmembrane serine protease TMPRSS2. J Virol. 2013;87(23):12552–12561. doi: 10.1128/JVI.01890-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tripathi R, Fiore LS, Richards DL, Yang Y, Liu J, Wang C, et al. Abl and Arg mediate cysteine cathepsin secretion to facilitate melanoma invasion and metastasis. Sci Signal. 2018;11(518). [DOI] [PMC free article] [PubMed]
- 33.Shin JS, Jung E, Kim M, Baric RS, Go YY. Saracatinib inhibits middle east respiratory syndrome-coronavirus replication In vitro. Viruses. 2018;10(6). [DOI] [PMC free article] [PubMed]
- 34.Chu JJ, Yang PL. c-Src protein kinase inhibitors block assembly and maturation of dengue virus. Proc Natl Acad Sci U S A. 2007;104(9):3520–3525. doi: 10.1073/pnas.0611681104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kumar R, Agrawal T, Khan NA, Nakayama Y, Medigeshi GR. Identification and characterization of the role of c-terminal Src kinase in dengue virus replication. Sci Rep. 2016;6:30490. doi: 10.1038/srep30490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Wispelaere M, LaCroix AJ, Yang PL. The small molecules AZD0530 and dasatinib inhibit dengue virus RNA replication via Fyn kinase. J Virol. 2013;87(13):7367–7381. doi: 10.1128/JVI.00632-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hirsch AJ, Medigeshi GR, Meyers HL, DeFilippis V, Fruh K, Briese T, et al. The Src family kinase c-Yes is required for maturation of West Nile virus particles. J Virol. 2005;79(18):11943–11951. doi: 10.1128/JVI.79.18.11943-11951.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Supekova L, Supek F, Lee J, Chen S, Gray N, Pezacki JP, et al. Identification of human kinases involved in hepatitis C virus replication by small interference RNA library screening. J Biol Chem. 2008;283(1):29–36. doi: 10.1074/jbc.M703988200. [DOI] [PubMed] [Google Scholar]
- 39.Conner SD, Schmid SL. Identification of an adaptor-associated kinase, AAK1, as a regulator of clathrin-mediated endocytosis. J Cell Biol. 2002;156(5):921–929. doi: 10.1083/jcb.200108123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee DW, Zhao X, Zhang F, Eisenberg E, Greene LE. Depletion of GAK/auxilin 2 inhibits receptor-mediated endocytosis and recruitment of both clathrin and clathrin adaptors. J Cell Sci. 2005;118(Pt 18):4311–4321. doi: 10.1242/jcs.02548. [DOI] [PubMed] [Google Scholar]
- 41.Neveu G, Barouch-Bentov R, Ziv-Av A, Gerber D, Jacob Y, Einav S. Identification and targeting of an interaction between a tyrosine motif within hepatitis C virus core protein and AP2M1 essential for viral assembly. PLoS Pathog. 2012;8(8):e1002845. doi: 10.1371/journal.ppat.1002845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Neveu G, Ziv-Av A, Barouch-Bentov R, Berkerman E, Mulholland J, Einav S. AP-2-associated protein kinase 1 and cyclin G-associated kinase regulate hepatitis C virus entry and are potential drug targets. J Virol. 2015;89(8):4387–4404. doi: 10.1128/JVI.02705-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zheng H, Yin C, Hoang T, He RL, Yang J, Yau SS. Ebolavirus classification based on natural vectors. DNA Cell Biol. 2015;34(6):418–428. doi: 10.1089/dna.2014.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pu SY, Xiao F, Schor S, Bekerman E, Zanini F, Barouch-Bentov R, et al. Feasibility and biological rationale of repurposing sunitinib and erlotinib for dengue treatment. Antivir Res. 2018;155:67–75. doi: 10.1016/j.antiviral.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Richardson P, Griffin I, Tucker C, Smith D, Oechsle O, Phelan A, et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395(10223):e30–ee1. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bekerman E, Neveu G, Shulla A, Brannan J, Pu SY, Wang S, et al. Anticancer kinase inhibitors impair intracellular viral trafficking and exert broad-spectrum antiviral effects. J Clin Invest. 2017;127(4):1338–1352. doi: 10.1172/JCI89857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stebbing J, Phelan A, Griffin I, Tucker C, Oechsle O, Smith D, et al. COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect Dis. 2020;20(4):400–402. doi: 10.1016/S1473-3099(20)30132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karaman MW, Herrgard S, Treiber DK, Gallant P, Atteridge CE, Campbell BT, et al. A quantitative analysis of kinase inhibitor selectivity. Nat Biotechnol. 2008;26(1):127–132. doi: 10.1038/nbt1358. [DOI] [PubMed] [Google Scholar]
- 49.Lee LY, Hernandez D, Rajkhowa T, Smith SC, Raman JR, Nguyen B, et al. Preclinical studies of gilteritinib, a next-generation FLT3 inhibitor. Blood. 2017;129(2):257–260. doi: 10.1182/blood-2016-10-745133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zheng K, Kitazato K, Wang Y. Viruses exploit the function of epidermal growth factor receptor. Rev Med Virol. 2014;24(4):274–286. doi: 10.1002/rmv.1796. [DOI] [PubMed] [Google Scholar]
- 51.Beerli C, Yakimovich A, Kilcher S, Reynoso GV, Flaschner G, Muller DJ, et al. Vaccinia virus hijacks EGFR signalling to enhance virus spread through rapid and directed infected cell motility. Nat Microbiol. 2019;4(2):216–225. doi: 10.1038/s41564-018-0288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang X, Huong SM, Chiu ML, Raab-Traub N, Huang ES. Epidermal growth factor receptor is a cellular receptor for human cytomegalovirus. Nature. 2003;424(6947):456–461. doi: 10.1038/nature01818. [DOI] [PubMed] [Google Scholar]
- 53.Wang X, Huang DY, Huong SM, Huang ES. Integrin alphavbeta3 is a coreceptor for human cytomegalovirus. Nat Med. 2005;11(5):515–521. doi: 10.1038/nm1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weller ML, Amornphimoltham P, Schmidt M, Wilson PA, Gutkind JS, Chiorini JA. Epidermal growth factor receptor is a co-receptor for adeno-associated virus serotype 6. Nat Med. 2010;16(6):662–664. doi: 10.1038/nm.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Eierhoff T, Hrincius ER, Rescher U, Ludwig S, Ehrhardt C. The epidermal growth factor receptor (EGFR) promotes uptake of influenza A viruses (IAV) into host cells. PLoS Pathog. 2010;6(9):e1001099. doi: 10.1371/journal.ppat.1001099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lupberger J, Zeisel MB, Xiao F, Thumann C, Fofana I, Zona L, et al. EGFR and EphA2 are host factors for hepatitis C virus entry and possible targets for antiviral therapy. Nat Med. 2011;17(5):589–595. doi: 10.1038/nm.2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Diao J, Pantua H, Ngu H, Komuves L, Diehl L, Schaefer G, et al. Hepatitis C virus induces epidermal growth factor receptor activation via CD81 binding for viral internalization and entry. J Virol. 2012;86(20):10935–10949. doi: 10.1128/JVI.00750-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ueki IF, Min-Oo G, Kalinowski A, Ballon-Landa E, Lanier LL, Nadel JA, et al. Respiratory virus-induced EGFR activation suppresses IRF1-dependent interferon lambda and antiviral defense in airway epithelium. J Exp Med. 2013;210(10):1929–1936. doi: 10.1084/jem.20121401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schleiss M, Eickhoff J, Auerochs S, Leis M, Abele S, Rechter S, et al. Protein kinase inhibitors of the quinazoline class exert anti-cytomegaloviral activity in vitro and in vivo. Antivir Res. 2008;79(1):49–61. doi: 10.1016/j.antiviral.2008.01.154. [DOI] [PubMed] [Google Scholar]
- 60.Cross DA, Ashton SE, Ghiorghiu S, Eberlein C, Nebhan CA, Spitzler PJ, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4(9):1046–1061. doi: 10.1158/2159-8290.CD-14-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Durand LO, Roizman B. Role of cdk9 in the optimization of expression of the genes regulated by ICP22 of herpes simplex virus 1. J Virol. 2008;82(21):10591–10599. doi: 10.1128/JVI.01242-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Badia R, Angulo G, Riveira-Munoz E, Pujantell M, Puig T, Ramirez C, et al. Inhibition of herpes simplex virus type 1 by the CDK6 inhibitor PD-0332991 (palbociclib) through the control of SAMHD1. J Antimicrob Chemother. 2016;71(2):387–394. doi: 10.1093/jac/dkv363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Perwitasari O, Yan X, O'Donnell J, Johnson S, Tripp RA. Repurposing Kinase Inhibitors as Antiviral Agents to Control Influenza A Virus Replication. Assay Drug Dev Technol. 2015;13(10):638–649. doi: 10.1089/adt.2015.0003.drrr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang J, Li G, Ye X. Cyclin T1/CDK9 interacts with influenza A virus polymerase and facilitates its association with cellular RNA polymerase II. J Virol. 2010;84(24):12619–12627. doi: 10.1128/JVI.01696-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mannova P, Beretta L. Activation of the N-Ras-PI3K-Akt-mTOR pathway by hepatitis C virus: control of cell survival and viral replication. J Virol. 2005;79(14):8742–8749. doi: 10.1128/JVI.79.14.8742-8749.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shives KD, Beatman EL, Chamanian M, O'Brien C, Hobson-Peters J, Beckham JD. West nile virus-induced activation of mammalian target of rapamycin complex 1 supports viral growth and viral protein expression. J Virol. 2014;88(16):9458–9471. doi: 10.1128/JVI.01323-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hale BG, Jackson D, Chen YH, Lamb RA, Randall RE. Influenza A virus NS1 protein binds p85beta and activates phosphatidylinositol-3-kinase signaling. Proc Natl Acad Sci U S A. 2006;103(38):14194–14199. doi: 10.1073/pnas.0606109103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kindrachuk J, Ork B, Hart BJ, Mazur S, Holbrook MR, Frieman MB, et al. Antiviral potential of ERK/MAPK and PI3K/AKT/mTOR signaling modulation for Middle East respiratory syndrome coronavirus infection as identified by temporal kinome analysis. Antimicrob Agents Chemother. 2015;59(2):1088–1099. doi: 10.1128/AAC.03659-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pleschka S, Wolff T, Ehrhardt C, Hobom G, Planz O, Rapp UR, et al. Influenza virus propagation is impaired by inhibition of the Raf/MEK/ERK signalling cascade. Nat Cell Biol. 2001;3(3):301–305. doi: 10.1038/35060098. [DOI] [PubMed] [Google Scholar]
- 70.Zampieri CA, Fortin JF, Nolan GP, Nabel GJ. The ERK mitogen-activated protein kinase pathway contributes to Ebola virus glycoprotein-induced cytotoxicity. J Virol. 2007;81(3):1230–1240. doi: 10.1128/JVI.01586-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Johnson JC, Martinez O, Honko AN, Hensley LE, Olinger GG, Basler CF. Pyridinyl imidazole inhibitors of p38 MAP kinase impair viral entry and reduce cytokine induction by Zaire ebolavirus in human dendritic cells. Antivir Res. 2014;107:102–109. doi: 10.1016/j.antiviral.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rouillard AD, Gundersen GW, Fernandez NF, Wang Z, Monteiro CD, McDermott MG, et al.. The harmonizome: a collection of processed datasets gathered to serve and mine knowledge about genes and proteins. database (Oxford). 2016;2016. [DOI] [PMC free article] [PubMed]
- 73.Kremer JM, Wilting J, Janssen LH. Drug binding to human alpha-1-acid glycoprotein in health and disease. Pharmacol Rev. 1988;40(1):1–47. [PubMed] [Google Scholar]
- 74.Gescher A. Analogs of staurosporine: potential anticancer drugs? Gen Pharmacol. 1998;31(5):721–728. doi: 10.1016/S0306-3623(98)00069-X. [DOI] [PubMed] [Google Scholar]
- 75.Wishart DS, Knox C, Guo AC, Shrivastava S, Hassanali M, Stothard P, et al. DrugBank: a comprehensive resource for in silico drug discovery and exploration. Nucleic Acids Res. 2006;34(Database issue):D668–D672. doi: 10.1093/nar/gkj067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zsila F, Fitos I, Bencze G, Keri G, Orfi L. Determination of human serum alpha1-acid glycoprotein and albumin binding of various marketed and preclinical kinase inhibitors. Curr Med Chem. 2009;16(16):1964–1977. doi: 10.2174/092986709788682191. [DOI] [PubMed] [Google Scholar]
- 77.Wolf D, Tilg H, Rumpold H, Gastl G, Wolf AM. The kinase inhibitor imatinib--an immunosuppressive drug? Curr Cancer Drug Targets. 2007;7(3):251–258. doi: 10.2174/156800907780618293. [DOI] [PubMed] [Google Scholar]
- 78.Chen S, Liu G, Chen J, Hu A, Zhang L, Sun W, et al. Ponatinib Protects Mice From Lethal Influenza Infection by Suppressing Cytokine Storm. Front Immunol. 2019;10:1393. doi: 10.3389/fimmu.2019.01393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Paniagua RT, Sharpe O, Ho PP, Chan SM, Chang A, Higgins JP, et al. Selective tyrosine kinase inhibition by imatinib mesylate for the treatment of autoimmune arthritis. J Clin Invest. 2006;116(10):2633–2642. doi: 10.1172/JCI28546.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rhee CK, Lee SH, Yoon HK, Kim SC, Lee SY, Kwon SS, et al. Effect of nilotinib on bleomycin-induced acute lung injury and pulmonary fibrosis in mice. Respiration. 2011;82(3):273–287. doi: 10.1159/000327719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu Y, Wang Z, Kwong SQ, Lui ELH, Friedman SL, Li FR, et al. Inhibition of PDGF, TGF-beta, and Abl signaling and reduction of liver fibrosis by the small molecule Bcr-Abl tyrosine kinase antagonist Nilotinib. J Hepatol. 2011;55(3):612–625. doi: 10.1016/j.jhep.2010.11.035. [DOI] [PubMed] [Google Scholar]
- 82.Shiha G, Nabil A, Lotfy A, Soliman R, Hassan AA, Ali IS, et al. Antifibrotic Effect of Combination of Nilotinib and Stem Cell-Conditioned Media on CCl4-Induced Liver Fibrosis. Stem Cells Int. 2020;2020:6574010. doi: 10.1155/2020/6574010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lemos DR, Babaeijandaghi F, Low M, Chang CK, Lee ST, Fiore D, et al. Nilotinib reduces muscle fibrosis in chronic muscle injury by promoting TNF-mediated apoptosis of fibro/adipogenic progenitors. Nat Med. 2015;21(7):786–794. doi: 10.1038/nm.3869. [DOI] [PubMed] [Google Scholar]
- 84.Khanjarsim V, Karimi J, Khodadadi I, Mohammadalipour A, Goodarzi MT, Solgi G, et al. Ameliorative Effects of Nilotinib on CCl4 Induced Liver Fibrosis Via Attenuation of RAGE/HMGB1 Gene Expression and Oxidative Stress in Rat. Chonnam Med J. 2017;53(2):118–126. doi: 10.4068/cmj.2017.53.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mohammadalipour A, Hashemnia M, Goudarzi F, Ravan AP. Increasing the effectiveness of tyrosine kinase inhibitor (TKI) in combination with a statin in reducing liver fibrosis. Clin Exp Pharmacol Physiol. 2019;46(12):1183–1193. doi: 10.1111/1440-1681.13157. [DOI] [PubMed] [Google Scholar]
- 86.Karimi J, Mohammadalipour A, Sheikh N, Khodadadi I, Hashemnia M, Goudarzi F, et al. Protective effects of combined Losartan and Nilotinib on carbon tetrachloride (CCl4)-induced liver fibrosis in rats. Drug Chem Toxicol. 2018:1–11. [DOI] [PubMed]
- 87.Piera-Velazquez S, Jimenez SA. Simultaneous inhibition of c-Abl and Src kinases abrogates the exaggerated expression of profibrotic genes in cultured systemic sclerosis dermal fibroblasts. Clin Exp Rheumatol. 2018;36 Suppl 113(4):36-44. [PubMed]
- 88.Wermuth PJ, Jimenez SA. Abrogation of transforming growth factor-beta-induced tissue fibrosis in TBRIcaCol1a2Cre transgenic mice by the second generation tyrosine kinase inhibitor SKI-606 (Bosutinib) PLoS One. 2018;13(5):e0196559. doi: 10.1371/journal.pone.0196559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Marinelli Busilacchi E, Costantini A, Mancini G, Tossetta G, Olivieri J, Poloni A, et al. Nilotinib treatment of patients affected by chronic graft-versus-host disease reduces collagen production and skin fibrosis by downmodulating the tgf-beta and p-smad pathway. Biol Blood Marrow Transplant. 2020. [DOI] [PubMed]
- 90.Daniels CE, Wilkes MC, Edens M, Kottom TJ, Murphy SJ, Limper AH, et al. Imatinib mesylate inhibits the profibrogenic activity of TGF-beta and prevents bleomycin-mediated lung fibrosis. J Clin Invest. 2004;114(9):1308–1316. doi: 10.1172/JCI200419603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Miyachi K, Ihara A, Hankins RW, Murai R, Maehiro S, Miyashita H. Efficacy of imatinib mesylate (STI571) treatment for a patient with rheumatoid arthritis developing chronic myelogenous leukemia. Clin Rheumatol. 2003;22(4-5):329–332. doi: 10.1007/s10067-003-0716-3. [DOI] [PubMed] [Google Scholar]
- 92.Eklund KK, Joensuu H. Treatment of rheumatoid arthritis with imatinib mesylate: clinical improvement in three refractory cases. Ann Med. 2003;35(5):362–367. doi: 10.1080/07853890310001339. [DOI] [PubMed] [Google Scholar]
- 93.Ciarcia R, Vitiello MT, Galdiero M, Pacilio C, Iovane V, d'Angelo D, et al. Imatinib treatment inhibit IL-6, IL-8, NF-KB and AP-1 production and modulate intracellular calcium in CML patients. J Cell Physiol. 2012;227(6):2798–2803. doi: 10.1002/jcp.23029. [DOI] [PubMed] [Google Scholar]
- 94.Kay J, High WA. Imatinib mesylate treatment of nephrogenic systemic fibrosis. Arthritis Rheum. 2008;58(8):2543–2548. doi: 10.1002/art.23696. [DOI] [PubMed] [Google Scholar]
- 95.Distler JH, Manger B, Spriewald BM, Schett G, Distler O. Treatment of pulmonary fibrosis for twenty weeks with imatinib mesylate in a patient with mixed connective tissue disease. Arthritis Rheum. 2008;58(8):2538–2542. doi: 10.1002/art.23694. [DOI] [PubMed] [Google Scholar]
- 96.Carnevale-Schianca F, Gallo S, Rota-Scalabrini D, Sangiolo D, Fizzotti M, Caravelli D, et al. Complete resolution of life-threatening bleomycin-induced pneumonitis after treatment with imatinib mesylate in a patient with Hodgkin's lymphoma: hope for severe chemotherapy-induced toxicity? J Clin Oncol. 2011;29(24):e691–e693. doi: 10.1200/JCO.2011.35.6733. [DOI] [PubMed] [Google Scholar]
- 97.Daniels CE, Lasky JA, Limper AH, Mieras K, Gabor E, Schroeder DR, et al. Imatinib treatment for idiopathic pulmonary fibrosis: Randomized placebo-controlled trial results. Am J Respir Crit Care Med. 2010;181(6):604–610. doi: 10.1164/rccm.200906-0964OC. [DOI] [PubMed] [Google Scholar]
- 98.Banakh I, Lam A, Tiruvoipati R, Carney I, Botha J. Imatinib for bleomycin induced pulmonary toxicity: a case report and evidence-base review. Clin Case Rep. 2016;4(5):486–490. doi: 10.1002/ccr3.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Skhirtladze C, Distler O, Dees C, Akhmetshina A, Busch N, Venalis P, et al. Src kinases in systemic sclerosis: central roles in fibroblast activation and in skin fibrosis. Arthritis Rheum. 2008;58(5):1475–1484. doi: 10.1002/art.23436. [DOI] [PubMed] [Google Scholar]
- 100.Okutani D, Lodyga M, Han B, Liu M. Src protein tyrosine kinase family and acute inflammatory responses. Am J Phys Lung Cell Mol Phys. 2006;291(2):L129–L141. doi: 10.1152/ajplung.00261.2005. [DOI] [PubMed] [Google Scholar]
- 101.Abdalla M, Thompson L, Gurley E, Burke S, Ujjin J, Newsome R, et al. Dasatinib inhibits TGFbeta-induced myofibroblast differentiation through Src-SRF Pathway. Eur J Pharmacol. 2015;769:134–142. doi: 10.1016/j.ejphar.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fraser CK, Lousberg EL, Kumar R, Hughes TP, Diener KR, Hayball JD. Dasatinib inhibits the secretion of TNF-alpha following TLR stimulation in vitro and in vivo. Exp Hematol. 2009;37(12):1435–1444. doi: 10.1016/j.exphem.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 103.Guo K, Bu X, Yang C, Cao X, Bian H, Zhu Q, et al. Treatment Effects of the Second-Generation Tyrosine Kinase Inhibitor Dasatinib on Autoimmune Arthritis. Front Immunol. 2018;9:3133. doi: 10.3389/fimmu.2018.03133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ozanne J, Prescott AR, Clark K. The clinically approved drugs dasatinib and bosutinib induce anti-inflammatory macrophages by inhibiting the salt-inducible kinases. Biochem J. 2015;465(2):271–279. doi: 10.1042/BJ20141165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hu M, Che P, Han X, Cai GQ, Liu G, Antony V, et al. Therapeutic targeting of SRC kinase in myofibroblast differentiation and pulmonary fibrosis. J Pharmacol Exp Ther. 2014;351(1):87–95. doi: 10.1124/jpet.114.216044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fridman JS, Scherle PA, Collins R, Burn TC, Li Y, Li J, et al. Selective inhibition of JAK1 and JAK2 is efficacious in rodent models of arthritis: preclinical characterization of INCB028050. J Immunol. 2010;184(9):5298–5307. doi: 10.4049/jimmunol.0902819. [DOI] [PubMed] [Google Scholar]
- 107.Roskoski R., Jr Janus kinase (JAK) inhibitors in the treatment of inflammatory and neoplastic diseases. Pharmacol Res. 2016;111:784–803. doi: 10.1016/j.phrs.2016.07.038. [DOI] [PubMed] [Google Scholar]
- 108.Kuriya B, Cohen MD, Keystone E. Baricitinib in rheumatoid arthritis: evidence-to-date and clinical potential. Ther Adv Musculoskelet Dis. 2017;9(2):37–44. doi: 10.1177/1759720X16687481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yazici Y, Regens AL. Promising new treatments for rheumatoid arthritis - the kinase inhibitors. Bull NYU Hosp Jt Dis. 2011;69(3):233–237. [PubMed] [Google Scholar]
- 110.Fleischmann R, Kremer J, Cush J, Schulze-Koops H, Connell CA, Bradley JD, et al. Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med. 2012;367(6):495–507. doi: 10.1056/NEJMoa1109071. [DOI] [PubMed] [Google Scholar]
- 111.Li Y, Yuan L, Yang J, Lei Y, Zhang H, Xia L, et al. Changes in Serum Cytokines May Predict Therapeutic Efficacy of Tofacitinib in Rheumatoid Arthritis. Mediat Inflamm. 2019;2019:5617431. doi: 10.1155/2019/5617431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Mesa RA, Gotlib J, Gupta V, Catalano JV, Deininger MW, Shields AL, et al. Effect of ruxolitinib therapy on myelofibrosis-related symptoms and other patient-reported outcomes in COMFORT-I: a randomized, double-blind, placebo-controlled trial. J Clin Oncol. 2013;31(10):1285–1292. doi: 10.1200/JCO.2012.44.4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Faure E, Poissy J, Goffard A, Fournier C, Kipnis E, Titecat M, et al. Distinct immune response in two MERS-CoV-infected patients: can we go from bench to bedside? PLoS One. 2014;9(2):e88716. doi: 10.1371/journal.pone.0088716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Josset L, Menachery VD, Gralinski LE, Agnihothram S, Sova P, Carter VS, et al. Cell host response to infection with novel human coronavirus EMC predicts potential antivirals and important differences with SARS coronavirus. mBio. 2013;4(3):e00165–e00113. doi: 10.1128/mBio.00165-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wu D, Yang XO. TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib. J Microbiol Immunol Infect 2020. [DOI] [PMC free article] [PubMed]
- 116.Hardie WD, Davidson C, Ikegami M, Leikauf GD, Le Cras TD, Prestridge A, et al. EGF receptor tyrosine kinase inhibitors diminish transforming growth factor-alpha-induced pulmonary fibrosis. Am J Phys Lung Cell Mol Phys. 2008;294(6):L1217–L1225. doi: 10.1152/ajplung.00020.2008. [DOI] [PubMed] [Google Scholar]
- 117.Cho HJ, Kang JH, Kim T, Park KK, Kim CH, Lee IS, et al. Suppression of PAI-1 expression through inhibition of the EGFR-mediated signaling cascade in rat kidney fibroblast by ascofuranone. J Cell Biochem. 2009;107(2):335–344. doi: 10.1002/jcb.22130. [DOI] [PubMed] [Google Scholar]
- 118.Zhou Y, Lee JY, Lee CM, Cho WK, Kang MJ, Koff JL, et al. Amphiregulin, an epidermal growth factor receptor ligand, plays an essential role in the pathogenesis of transforming growth factor-beta-induced pulmonary fibrosis. J Biol Chem. 2012;287(50):41991–42000. doi: 10.1074/jbc.M112.356824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ishii Y, Fujimoto S, Fukuda T. Gefitinib prevents bleomycin-induced lung fibrosis in mice. Am J Respir Crit Care Med. 2006;174(5):550–556. doi: 10.1164/rccm.200509-1534OC. [DOI] [PubMed] [Google Scholar]
- 120.Wong CK, Lam CW, Wu AK, Ip WK, Lee NL, Chan IH, et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136(1):95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Huang KJ, Su IJ, Theron M, Wu YC, Lai SK, Liu CC, et al. An interferon-gamma-related cytokine storm in SARS patients. J Med Virol. 2005;75(2):185–194. doi: 10.1002/jmv.20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Baas T, Taubenberger JK, Chong PY, Chui P, Katze MG. SARS-CoV virus-host interactions and comparative etiologies of acute respiratory distress syndrome as determined by transcriptional and cytokine profiling of formalin-fixed paraffin-embedded tissues. J Interf Cytokine Res. 2006;26(5):309–317. doi: 10.1089/jir.2006.26.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rockx B, Baas T, Zornetzer GA, Haagmans B, Sheahan T, Frieman M, et al. Early upregulation of acute respiratory distress syndrome-associated cytokines promotes lethal disease in an aged-mouse model of severe acute respiratory syndrome coronavirus infection. J Virol. 2009;83(14):7062–7074. doi: 10.1128/JVI.00127-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sime PJ, Xing Z, Graham FL, Csaky KG, Gauldie J. Adenovector-mediated gene transfer of active transforming growth factor-beta1 induces prolonged severe fibrosis in rat lung. J Clin Invest. 1997;100(4):768–776. doi: 10.1172/JCI119590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chen YL, Zhang X, Bai J, Gai L, Ye XL, Zhang L, et al. Sorafenib ameliorates bleomycin-induced pulmonary fibrosis: potential roles in the inhibition of epithelial-mesenchymal transition and fibroblast activation. Cell Death Dis. 2013;4:e665. doi: 10.1038/cddis.2013.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Su TH, Shiau CW, Jao P, Liu CH, Liu CJ, Tai WT, et al. Sorafenib and its derivative SC-1 exhibit antifibrotic effects through signal transducer and activator of transcription 3 inhibition. Proc Natl Acad Sci U S A. 2015;112(23):7243–7248. doi: 10.1073/pnas.1507499112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Karas K, Salkowska A, Karwaciak I, Walczak-Drzewiecka A, Dastych J, Bachorz RA, et al. The dichotomous nature of az5104 (an egfr inhibitor) towards RORgamma and RORgammaT. Int J Mol Sci. 2019;20(22). [DOI] [PMC free article] [PubMed]
- 128.Nihei M, Okazaki T, Ebihara S, Kobayashi M, Niu K, Gui P, et al. Chronic inflammation, lymphangiogenesis, and effect of an anti-VEGFR therapy in a mouse model and in human patients with aspiration pneumonia. J Pathol. 2015;235(4):632–645. doi: 10.1002/path.4473. [DOI] [PubMed] [Google Scholar]
- 129.Varone F, Sgalla G, Iovene B, Bruni T, Richeldi L. Nintedanib for the treatment of idiopathic pulmonary fibrosis. Expert Opin Pharmacother. 2018;19(2):167–175. doi: 10.1080/14656566.2018.1425681. [DOI] [PubMed] [Google Scholar]
- 130.Liu F, Bayliss G, Zhuang S. Application of nintedanib and other potential anti-fibrotic agents in fibrotic diseases. Clin Sci (Lond) 2019;133(12):1309–1320. doi: 10.1042/CS20190249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gad ES, Salama AAA, El-Shafie MF, Arafa HMM, Abdelsalam RM, Khattab M. The Anti-fibrotic and Anti-inflammatory Potential of Bone Marrow-Derived Mesenchymal Stem Cells and Nintedanib in Bleomycin-Induced Lung Fibrosis in Rats. Inflammation. 2020;43(1):123–134. doi: 10.1007/s10753-019-01101-2. [DOI] [PubMed] [Google Scholar]
- 132.Nam HY, Nam JH, Yoon G, Lee JY, Nam Y, Kang HJ, et al. Ibrutinib suppresses LPS-induced neuroinflammatory responses in BV2 microglial cells and wild-type mice. J Neuroinflammation. 2018;15(1):271. doi: 10.1186/s12974-018-1308-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.de Porto AP, Liu Z, de Beer R, Florquin S, de Boer OJ, Hendriks RW, et al. Btk inhibitor ibrutinib reduces inflammatory myeloid cell responses in the lung during murine pneumococcal pneumonia. Mol Med. 2019;25(1):3. doi: 10.1186/s10020-018-0069-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Schmerwitz UK, Sass G, Khandoga AG, Joore J, Mayer BA, Berberich N, et al. Flavopiridol protects against inflammation by attenuating leukocyte-endothelial interaction via inhibition of cyclin-dependent kinase 9. Arterioscler Thromb Vasc Biol. 2011;31(2):280–288. doi: 10.1161/ATVBAHA.110.213934. [DOI] [PubMed] [Google Scholar]
- 135.Huang X, Wang W, Yuan H, Sun J, Li L, Wu X, et al. Sunitinib, a Small-Molecule Kinase Inhibitor, Attenuates Bleomycin-Induced Pulmonary Fibrosis in Mice. Tohoku J Exp Med. 2016;239(4):251–261. doi: 10.1620/tjem.239.251. [DOI] [PubMed] [Google Scholar]
- 136.Elshal M, Abu-Elsaad N, El-Karef A, Ibrahim TM. The multi-kinase inhibitor pazopanib targets hepatic stellate cell activation and apoptosis alleviating progression of liver fibrosis. Naunyn Schmiedeberg's Arch Pharmacol. 2015;388(12):1293–1304. doi: 10.1007/s00210-015-1157-7. [DOI] [PubMed] [Google Scholar]
- 137.Zhao S, Gao N, Qi H, Chi H, Liu B, He B, et al. Suppressive effects of sunitinib on a TLR activation-induced cytokine storm. Eur J Pharmacol. 2019;854:347–353. doi: 10.1016/j.ejphar.2019.04.045. [DOI] [PubMed] [Google Scholar]
- 138.Branche E, Tang WW, Viramontes KM, Young MP, Sheets N, Joo Y, et al. Synergism between the tyrosine kinase inhibitor sunitinib and Anti-TNF antibody protects against lethal dengue infection. Antivir Res. 2018;158:1–7. doi: 10.1016/j.antiviral.2018.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Peerzada MM, Spiro TP, Daw HA. Pulmonary toxicities of tyrosine kinase inhibitors. Clin Adv Hematol Oncol. 2011;9(11):824–836. [PubMed] [Google Scholar]
- 140.Barber NA, Ganti AK. Pulmonary toxicities from targeted therapies: a review. Target Oncol. 2011;6(4):235–243. doi: 10.1007/s11523-011-0199-0. [DOI] [PubMed] [Google Scholar]
- 141.Kantarjian HM, Hochhaus A, Saglio G, De Souza C, Flinn IW, Stenke L, et al. Nilotinib versus imatinib for the treatment of patients with newly diagnosed chronic phase, Philadelphia chromosome-positive, chronic myeloid leukaemia: 24-month minimum follow-up of the phase 3 randomised ENESTnd trial. Lancet Oncol. 2011;12(9):841–851. doi: 10.1016/S1470-2045(11)70201-7. [DOI] [PubMed] [Google Scholar]
- 142.Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM, et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med. 2001;344(14):1031–1037. doi: 10.1056/NEJM200104053441401. [DOI] [PubMed] [Google Scholar]
- 143.Stakhina OV, Turkina AG, Kostina IE, Kochkareva IB. A rare complication of imatinib mesylate therapy: drug-induced pneumonitis. Ter Arkh. 2010;82(2):59–61. [PubMed] [Google Scholar]
- 144.Bergeron A, Rea D, Levy V, Picard C, Meignin V, Tamburini J, et al. Lung abnormalities after dasatinib treatment for chronic myeloid leukemia: a case series. Am J Respir Crit Care Med. 2007;176(8):814–818. doi: 10.1164/rccm.200705-715CR. [DOI] [PubMed] [Google Scholar]
- 145.Sato M, Watanabe S, Aoki N, Asakawa K, Moriyama H, Oshima Y, et al. A Case of Drug-Induced Organizing Pneumonia Caused by Dasatinib. Gan To Kagaku Ryoho. 2018;45(5):851–854. [PubMed] [Google Scholar]
- 146.Vahid B, Esmaili A. Erlotinib-associated acute pneumonitis: report of two cases. Can Respir J. 2007;14(3):167–170. doi: 10.1155/2007/832605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Cersosimo RJ. Gefitinib: an adverse effects profile. Expert Opin Drug Saf. 2006;5(3):469–479. doi: 10.1517/14740338.5.3.469. [DOI] [PubMed] [Google Scholar]
- 148.Luo C, Lv M, Li Y, Liu P, Yang J. Gefitinib-induced interstitial pneumonia: A case report and review of the literature. Exp Ther Med. 2014;7(4):855–859. doi: 10.3892/etm.2014.1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Hida T, Nokihara H, Kondo M, Kim YH, Azuma K, Seto T, et al. Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): an open-label, randomised phase 3 trial. Lancet. 2017;390(10089):29–39. doi: 10.1016/S0140-6736(17)30565-2. [DOI] [PubMed] [Google Scholar]
- 150.Kazandjian D, Blumenthal GM, Chen HY, He K, Patel M, Justice R, et al. FDA approval summary: crizotinib for the treatment of metastatic non-small cell lung cancer with anaplastic lymphoma kinase rearrangements. Oncologist. 2014;19(10):e5–11. doi: 10.1634/theoncologist.2014-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Yoneda KY, Scranton JR, Cadogan MA, Tassell V, Nadanaciva S, Wilner KD, et al. Interstitial Lung Disease Associated With Crizotinib in Patients With Advanced Non-Small Cell Lung Cancer: Independent Review of Four PROFILE Trials. Clin Lung Cancer. 2017;18(5):472–479. doi: 10.1016/j.cllc.2017.03.004. [DOI] [PubMed] [Google Scholar]
- 152.Lim SM, An HJ, Park HS, Kwon HJ, YK E, Hur J, et al. Organizing pneumonia resembling disease progression in a non-small-cell lung cancer patient receiving ceritinib: a case report. Medicine (Baltimore) 2018;97(31):e11646. doi: 10.1097/MD.0000000000011646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Gemma A, Kusumoto M, Kurihara Y, Masuda N, Banno S, Endo Y, et al. Interstitial Lung Disease Onset and Its Risk Factors in Japanese Patients With ALK-Positive NSCLC After Treatment With Crizotinib. J Thorac Oncol. 2019;14(4):672–682. doi: 10.1016/j.jtho.2018.11.022. [DOI] [PubMed] [Google Scholar]
- 154.Hwang HJ, Kim MY, Choi CM, Lee JC. Anaplastic lymphoma kinase inhibitor related pneumonitis in patients with non-small cell lung cancer: Clinical and radiologic characteristics and risk factors. Medicine (Baltimore) 2019;98(48):e18131. doi: 10.1097/MD.0000000000018131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Reinwald M, Silva JT, Mueller NJ, Fortun J, Garzoni C, de Fijter JW, et al. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: an infectious diseases perspective (Intracellular signaling pathways: tyrosine kinase and mTOR inhibitors) Clin Microbiol Infect. 2018;24(Suppl 2):S53–S70. doi: 10.1016/j.cmi.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 156.Makris D, Manoulakas E, Komnos A, Papakrivou E, Tzovaras N, Hovas A, et al. Effect of pravastatin on the frequency of ventilator-associated pneumonia and on intensive care unit mortality: open-label, randomized study. Crit Care Med. 2011;39(11):2440–2446. doi: 10.1097/CCM.0b013e318225742c. [DOI] [PubMed] [Google Scholar]
- 157.Papazian L, Roch A, Charles PE, Penot-Ragon C, Perrin G, Roulier P, et al. Effect of statin therapy on mortality in patients with ventilator-associated pneumonia: a randomized clinical trial. JAMA. 2013;310(16):1692–1700. doi: 10.1001/jama.2013.280031. [DOI] [PubMed] [Google Scholar]
- 158.Frost FJ, Petersen H, Tollestrup K, Skipper B. Influenza and COPD mortality protection as pleiotropic, dose-dependent effects of statins. Chest. 2007;131(4):1006–1012. doi: 10.1378/chest.06-1997. [DOI] [PubMed] [Google Scholar]
- 159.Douglas I, Evans S, Smeeth L. Effect of statin treatment on short term mortality after pneumonia episode: cohort study. BMJ. 2011;342:d1642. doi: 10.1136/bmj.d1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Vandermeer ML, Thomas AR, Kamimoto L, Reingold A, Gershman K, Meek J, et al. Association between use of statins and mortality among patients hospitalized with laboratory-confirmed influenza virus infections: a multistate study. J Infect Dis. 2012;205(1):13–19. doi: 10.1093/infdis/jir695. [DOI] [PubMed] [Google Scholar]
- 161.Yuan S. Statins may decrease the fatality rate of middle east respiratory syndrome infection. mBio. 2015;6(4):e01120. doi: 10.1128/mBio.01120-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Schwartz DM, Kanno Y, Villarino A, Ward M, Gadina M, O'Shea JJ. JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat Rev Drug Discov. 2017;16(12):843–862. doi: 10.1038/nrd.2017.201. [DOI] [PubMed] [Google Scholar]
- 163.Aschenbrenner DS. Tofacitinib Receives New Boxed Safety Warning. Am J Nurs. 2019;119(11):20. doi: 10.1097/01.NAJ.0000605328.68897.ed. [DOI] [PubMed] [Google Scholar]
- 164.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020. [DOI] [PMC free article] [PubMed]
- 165.Treon SP, Castillo J, Skarbnik AP, Soumerai JD, Ghobrial IM, Guerrera ML, et al. The BTK-inhibitor ibrutinib may protect against pulmonary injury in COVID-19 infected patients. Blood. 2020. [DOI] [PMC free article] [PubMed]
- 166.Shi F, Len Y, Gong Y, Shi R, Yang X, Naren D, et al. Ribavirin Inhibits the Activity of mTOR/eIF4E, ERK/Mnk1/eIF4E Signaling Pathway and Synergizes with Tyrosine Kinase Inhibitor Imatinib to Impair Bcr-Abl Mediated Proliferation and Apoptosis in Ph+ Leukemia. PLoS One. 2015;10(8):e0136746. doi: 10.1371/journal.pone.0136746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Yan Y, Shin WI, Pang YX, Meng Y, Lai J, You C, et al. The first 75 days of novel coronavirus (SARS-CoV-2) outbreak: recent advances, prevention, and treatment. Int J Environ Res Public Health. 2020;17(7). [DOI] [PMC free article] [PubMed]
- 168.Haouala A, Widmer N, Duchosal MA, Montemurro M, Buclin T, Decosterd LA. Drug interactions with the tyrosine kinase inhibitors imatinib, dasatinib, and nilotinib. Blood. 2011;117(8):e75–e87. doi: 10.1182/blood-2010-07-294330. [DOI] [PubMed] [Google Scholar]
- 169.Xu J, Shi PY, Li H, Zhou J. Broad spectrum antiviral agent niclosamide and its therapeutic potential. ACS Infect Dis. 2020. [DOI] [PMC free article] [PubMed]
- 170.Gassen NC, Niemeyer D, Muth D, Corman VM, Martinelli S, Gassen A, et al. SKP2 attenuates autophagy through Beclin1-ubiquitination and its inhibition reduces MERS-Coronavirus infection. Nat Commun. 2019;10(1):5770. doi: 10.1038/s41467-019-13659-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Jin B, Wang C, Shen Y, Pan J. Anthelmintic niclosamide suppresses transcription of BCR-ABL fusion oncogene via disabling Sp1 and induces apoptosis in imatinib-resistant CML cells harboring T315I mutant. Cell Death Dis. 2018;9(2):68. doi: 10.1038/s41419-017-0075-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Li R, You S, Hu Z, Chen ZG, Sica GL, Khuri FR, et al. Inhibition of STAT3 by niclosamide synergizes with erlotinib against head and neck cancer. PLoS One. 2013;8(9):e74670. doi: 10.1371/journal.pone.0074670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Shi L, Zheng H, Hu W, Zhou B, Dai X, Zhang Y, et al. Niclosamide inhibition of STAT3 synergizes with erlotinib in human colon cancer. Onco Targets Ther. 2017;10:1767–1776. doi: 10.2147/OTT.S129449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yu X, Liu F, Zeng L, He F, Zhang R, Yan S, et al. Niclosamide Exhibits Potent Anticancer Activity and Synergizes with Sorafenib in Human Renal Cell Cancer Cells. Cell Physiol Biochem. 2018;47(3):957–971. doi: 10.1159/000490140. [DOI] [PubMed] [Google Scholar]
- 175.Peters S, Zimmermann S, Adjei AA. Oral epidermal growth factor receptor tyrosine kinase inhibitors for the treatment of non-small cell lung cancer: comparative pharmacokinetics and drug-drug interactions. Cancer Treat Rev. 2014;40(8):917–926. doi: 10.1016/j.ctrv.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 176.Dunn LA, Fury MG, Sherman EJ, Ho AA, Katabi N, Haque SS, et al. Phase I study of induction chemotherapy with afatinib, ribavirin, and weekly carboplatin and paclitaxel for stage IVA/IVB human papillomavirus-associated oropharyngeal squamous cell cancer. Head Neck. 2018;40(2):233–241. doi: 10.1002/hed.24938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wind S, Giessmann T, Jungnik A, Brand T, Marzin K, Bertulis J, et al. Pharmacokinetic drug interactions of afatinib with rifampicin and ritonavir. Clin Drug Investig. 2014;34(3):173–182. doi: 10.1007/s40261-013-0161-2. [DOI] [PubMed] [Google Scholar]
- 178.Beyer C, Distler JH, Distler O. Are tyrosine kinase inhibitors promising for the treatment of systemic sclerosis and other fibrotic diseases? Swiss Med Wkly. 2010;140:w13050. doi: 10.4414/smw.2010.13050. [DOI] [PubMed] [Google Scholar]
- 179.Chen YJ, Hsu CC, Shiao YJ, Wang HT, Lo YL, Lin AMY. Anti-inflammatory effect of afatinib (an EGFR-TKI) on OGD-induced neuroinflammation. Sci Rep. 2019;9(1):2516. doi: 10.1038/s41598-019-38676-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Casaos J, Gorelick NL, Huq S, Choi J, Xia Y, Serra R, et al. The Use of Ribavirin as an Anticancer Therapeutic: Will It Go Viral? Mol Cancer Ther. 2019;18(7):1185–1194. doi: 10.1158/1535-7163.MCT-18-0666. [DOI] [PubMed] [Google Scholar]
- 181.van Hoppe S, Sparidans RW, Wagenaar E, Beijnen JH, Schinkel AH. Breast cancer resistance protein (BCRP/ABCG2) and P-glycoprotein (P-gp/ABCB1) transport afatinib and restrict its oral availability and brain accumulation. Pharmacol Res. 2017;120:43–50. doi: 10.1016/j.phrs.2017.01.035. [DOI] [PubMed] [Google Scholar]
- 182.Gordon MS, Springett GM, Su YB, Ould-Kaci M, Wind S, Zhao Y, et al. A Phase I dose-escalation study of afatinib combined with nintedanib in patients with advanced solid tumors. Future Oncol. 2015;11(10):1479–1491. doi: 10.2217/fon.15.50. [DOI] [PubMed] [Google Scholar]
- 183.Lee CG, Gottesman MM, Cardarelli CO, Ramachandra M, Jeang KT, Ambudkar SV, et al. HIV-1 protease inhibitors are substrates for the MDR1 multidrug transporter. Biochemistry. 1998;37(11):3594–3601. doi: 10.1021/bi972709x. [DOI] [PubMed] [Google Scholar]
- 184.Tang SC, Lagas JS, Lankheet NA, Poller B, Hillebrand MJ, Rosing H, et al. Brain accumulation of sunitinib is restricted by P-glycoprotein (ABCB1) and breast cancer resistance protein (ABCG2) and can be enhanced by oral elacridar and sunitinib coadministration. Int J Cancer. 2012;130(1):223–233. doi: 10.1002/ijc.26000. [DOI] [PubMed] [Google Scholar]
- 185.Rudek MA, Moore PC, Mitsuyasu RT, Dezube BJ, Aboulafia D, Gerecitano J, et al. A phase 1/pharmacokinetic study of sunitinib in combination with highly active antiretroviral therapy in human immunodeficiency virus-positive patients with cancer: AIDS Malignancy Consortium trial AMC 061. Cancer. 2014;120(8):1194–1202. doi: 10.1002/cncr.28554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Green TP, Fennell M, Whittaker R, Curwen J, Jacobs V, Allen J, et al. Preclinical anticancer activity of the potent, oral Src inhibitor AZD0530. Mol Oncol. 2009;3(3):248–261. doi: 10.1016/j.molonc.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ma R, Chen J, Liang Y, Lin S, Zhu L, Liang X, et al. Sorafenib: A potential therapeutic drug for hepatic fibrosis and its outcomes. Biomed Pharmacother. 2017;88:459–468. doi: 10.1016/j.biopha.2017.01.107. [DOI] [PubMed] [Google Scholar]
- 188.Corona SP, Generali D. Abemaciclib: a CDK4/6 inhibitor for the treatment of HR+/HER2- advanced breast cancer. Drug Des Devel Ther. 2018;12:321–330. doi: 10.2147/DDDT.S137783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Hurvitz SA, Martin M, Press MF, Chan D, Fernandez-Abad M, Petru E, et al. Potent Cell-Cycle Inhibition and Upregulation of Immune Response with Abemaciclib and Anastrozole in neoMONARCH, Phase II Neoadjuvant Study in HR(+)/HER2(-) Breast Cancer. Clin Cancer Res. 2020;26(3):566–580. doi: 10.1158/1078-0432.CCR-19-1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.He H, Tran P, Gu H, Tedesco V, Zhang J, Lin W, et al. Midostaurin, a Novel Protein Kinase Inhibitor for the Treatment of Acute Myelogenous Leukemia: Insights from Human Absorption, Metabolism, and Excretion Studies of a BDDCS II Drug. Drug Metab Dispos. 2017;45(5):540–555. doi: 10.1124/dmd.116.072744. [DOI] [PubMed] [Google Scholar]
- 191.Vaidya P, Khedro T, Yaghmour B, Yaghmour G. Midostaurin-Related Interstitial Lung Injury in FLT3(+) Acute Myeloid Leukemia Post-Allogeneic Transplant. World J Oncol. 2019;10(6):237–239. doi: 10.14740/wjon1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, et al. Midostaurin plus Chemotherapy for Acute Myeloid Leukemia with a FLT3 Mutation. N Engl J Med. 2017;377(5):454–464. doi: 10.1056/NEJMoa1614359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Hexner EO, Mascarenhas J, Prchal J, Roboz GJ, Baer MR, Ritchie EK, et al. Phase I dose escalation study of lestaurtinib in patients with myelofibrosis. Leuk Lymphoma. 2015;56(9):2543–2551. doi: 10.3109/10428194.2014.1001986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Levis M, Perl AE. Gilteritinib: potent targeting of FLT3 mutations in AML. Blood Adv. 2020;4(6):1178–1191. doi: 10.1182/bloodadvances.2019000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kamath AV, Wang J, Lee FY, Marathe PH. Preclinical pharmacokinetics and in vitro metabolism of dasatinib (BMS-354825): a potent oral multi-targeted kinase inhibitor against SRC and BCR-ABL. Cancer Chemother Pharmacol. 2008;61(3):365–376. doi: 10.1007/s00280-007-0478-8. [DOI] [PubMed] [Google Scholar]
- 196.Brixey AG, Light RW. Pleural effusions due to dasatinib. Curr Opin Pulm Med. 2010;16(4):351–356. doi: 10.1097/MCP.0b013e328338c486. [DOI] [PubMed] [Google Scholar]
- 197.Montani D, Bergot E, Gunther S, Savale L, Bergeron A, Bourdin A, et al. Pulmonary arterial hypertension in patients treated by dasatinib. Circulation. 2012;125(17):2128–2137. doi: 10.1161/CIRCULATIONAHA.111.079921. [DOI] [PubMed] [Google Scholar]
- 198.Widmer N, Decosterd LA, Csajka C, Leyvraz S, Duchosal MA, Rosselet A, et al. Population pharmacokinetics of imatinib and the role of alpha-acid glycoprotein. Br J Clin Pharmacol. 2006;62(1):97–112. doi: 10.1111/j.1365-2125.2006.02719.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Rosado MF, Donna E, Ahn YS. Challenging problems in advanced malignancy: Case 3. Imatinib mesylate-induced interstitial pneumonitis. J Clin Oncol. 2003;21(16):3171–3173. doi: 10.1200/JCO.2003.03.037. [DOI] [PubMed] [Google Scholar]
- 200.Yokoyama T, Miyazawa K, Kurakawa E, Nagate A, Shimamoto T, Iwaya K, et al. Interstitial pneumonia induced by imatinib mesylate: pathologic study demonstrates alveolar destruction and fibrosis with eosinophilic infiltration. Leukemia. 2004;18(3):645–646. doi: 10.1038/sj.leu.2403251. [DOI] [PubMed] [Google Scholar]
- 201.Breccia M, D'Elia GM, D'Andrea M, Latagliata R, Alimena G. Pleural-pericardic effusion as uncommon complication in CML patients treated with Imatinib. Eur J Haematol. 2005;74(1):89–90. doi: 10.1111/j.1600-0609.2004.00347.x. [DOI] [PubMed] [Google Scholar]
- 202.Xia B, Heimbach T, He H, Lin TH. Nilotinib preclinical pharmacokinetics and practical application toward clinical projections of oral absorption and systemic availability. Biopharm Drug Dispos. 2012;33(9):536–549. doi: 10.1002/bdd.1821. [DOI] [PubMed] [Google Scholar]
- 203.Tanaka C, Yin OQ, Smith T, Sethuraman V, Grouss K, Galitz L, et al. Effects of rifampin and ketoconazole on the pharmacokinetics of nilotinib in healthy participants. J Clin Pharmacol. 2011;51(1):75–83. doi: 10.1177/0091270010367428. [DOI] [PubMed] [Google Scholar]
- 204.Saglio G, Kim DW, Issaragrisil S, le Coutre P, Etienne G, Lobo C, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362(24):2251–2259. doi: 10.1056/NEJMoa0912614. [DOI] [PubMed] [Google Scholar]
- 205.Donatelli C, Chongnarungsin D, Ashton R. Acute respiratory failure from nilotinib-associated diffuse alveolar hemorrhage. Leuk Lymphoma. 2014;55(10):2408–2409. doi: 10.3109/10428194.2014.887714. [DOI] [PubMed] [Google Scholar]
- 206.Quilot FM, Georges M, Favrolt N, Beltramo G, Foignot C, Grandvuillemin A, et al. Pulmonary hypertension associated with ponatinib therapy. Eur Respir J. 2016;47(2):676–679. doi: 10.1183/13993003.01110-2015. [DOI] [PubMed] [Google Scholar]
- 207.Khoury HJ, Cortes JE, Kantarjian HM, Gambacorti-Passerini C, Baccarani M, Kim DW, et al. Bosutinib is active in chronic phase chronic myeloid leukemia after imatinib and dasatinib and/or nilotinib therapy failure. Blood. 2012;119(15):3403–3412. doi: 10.1182/blood-2011-11-390120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ayli M, Ozcan M, Cengiz SG. Ruxolitinib Treatment in a Patient with Primary Myelofibrosis Resistant to Conventional Therapies and Splenectomy: A Case Report. Turk J Haematol. 2015;32(2):180–183. doi: 10.4274/tjh.2013.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Kerget B, Araz O, Ucar EY, Akgun M, Saglam L. Acute respiratory distress syndrome; A rare complication caused by usage of ruxolitinib. Respir Med Case Rep. 2017;22:243–245. doi: 10.1016/j.rmcr.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zhang M, Xu C, Ma L, Shamiyeh E, Yin J, von Moltke LL, et al. Effect of food on the bioavailability and tolerability of the JAK2-selective inhibitor fedratinib (SAR302503): Results from two phase I studies in healthy volunteers. Clin Pharmacol Drug Dev. 2015;4(4):315–321. doi: 10.1002/cpdd.161. [DOI] [PubMed] [Google Scholar]
- 211.van Vollenhoven RF, Fleischmann R, Cohen S, Lee EB, Garcia Meijide JA, Wagner S, et al. Tofacitinib or adalimumab versus placebo in rheumatoid arthritis. N Engl J Med. 2012;367(6):508–519. doi: 10.1056/NEJMoa1112072. [DOI] [PubMed] [Google Scholar]
- 212.Ando M, Okamoto I, Yamamoto N, Takeda K, Tamura K, Seto T, et al. Predictive factors for interstitial lung disease, antitumor response, and survival in non-small-cell lung cancer patients treated with gefitinib. J Clin Oncol. 2006;24(16):2549–2556. doi: 10.1200/JCO.2005.04.9866. [DOI] [PubMed] [Google Scholar]
- 213.Kato T, Nishio K. Clinical aspects of epidermal growth factor receptor inhibitors: benefit and risk. Respirology. 2006;11(6):693–698. doi: 10.1111/j.1440-1843.2006.00940.x. [DOI] [PubMed] [Google Scholar]
- 214.Shi L, Tang J, Tong L, Liu Z. Risk of interstitial lung disease with gefitinib and erlotinib in advanced non-small cell lung cancer: a systematic review and meta-analysis of clinical trials. Lung Cancer. 2014;83(2):231–239. doi: 10.1016/j.lungcan.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 215.Suzuki H, Aoshiba K, Yokohori N, Nagai A. Epidermal growth factor receptor tyrosine kinase inhibition augments a murine model of pulmonary fibrosis. Cancer Res. 2003;63(16):5054–5059. [PubMed] [Google Scholar]
- 216.Stopfer P, Marzin K, Narjes H, Gansser D, Shahidi M, Uttereuther-Fischer M, et al. Afatinib pharmacokinetics and metabolism after oral administration to healthy male volunteers. Cancer Chemother Pharmacol. 2012;69(4):1051–1061. doi: 10.1007/s00280-011-1803-9. [DOI] [PubMed] [Google Scholar]
- 217.Sequist LV, Yang JC, Yamamoto N, O’Byrne K, Hirsh V, Mok T, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol. 2013;31(27):3327–3334. doi: 10.1200/JCO.2012.44.2806. [DOI] [PubMed] [Google Scholar]
- 218.Wu YL, Zhou C, Hu CP, Feng J, Lu S, Huang Y, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(2):213–222. doi: 10.1016/S1470-2045(13)70604-1. [DOI] [PubMed] [Google Scholar]
- 219.Burris HA, 3rd, Hurwitz HI, Dees EC, Dowlati A, Blackwell KL, O'Neil B, et al. Phase I safety, pharmacokinetics, and clinical activity study of lapatinib (GW572016), a reversible dual inhibitor of epidermal growth factor receptor tyrosine kinases, in heavily pretreated patients with metastatic carcinomas. J Clin Oncol. 2005;23(23):5305–5313. doi: 10.1200/JCO.2005.16.584. [DOI] [PubMed] [Google Scholar]
- 220.Capri G, Chang J, Chen SC, Conte P, Cwiertka K, Jerusalem G, et al. An open-label expanded access study of lapatinib and capecitabine in patients with HER2-overexpressing locally advanced or metastatic breast cancer. Ann Oncol. 2010;21(3):474–480. doi: 10.1093/annonc/mdp373. [DOI] [PubMed] [Google Scholar]
- 221.Kiriu T, Tamura D, Tachihara M, Sekiya R, Hazama D, Katsurada M, et al. Successful Osimertinib Rechallenge with Steroid Therapy after Osimertinib-induced Interstitial Lung Disease. Intern Med. 2018;57(1):91–95. doi: 10.2169/internalmedicine.8947-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Fan M, Mo T, Shen L, Yang L. Osimertinib-induced severe interstitial lung disease: A case report. Thorac Cancer. 2019;10(7):1657–1660. doi: 10.1111/1759-7714.13127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Yoneda KY, Shelton DK, Beckett LA, Gandara DR. Independent review of interstitial lung disease associated with death in TRIBUTE (paclitaxel and carboplatin with or without concurrent erlotinib) in advanced non-small cell lung cancer. J Thorac Oncol. 2007;2(6):537–543. doi: 10.1097/JTO.0b013e318060d329. [DOI] [PubMed] [Google Scholar]
- 224.Chan A, Delaloge S, Holmes FA, Moy B, Iwata H, Harvey VJ, et al. Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2016;17(3):367–377. doi: 10.1016/S1470-2045(15)00551-3. [DOI] [PubMed] [Google Scholar]
- 225.van der Graaf WT, Blay JY, Chawla SP, Kim DW, Bui-Nguyen B, Casali PG, et al. Pazopanib for metastatic soft-tissue sarcoma (PALETTE): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2012;379(9829):1879–1886. doi: 10.1016/S0140-6736(12)60651-5. [DOI] [PubMed] [Google Scholar]
- 226.Verschoor AJ, Gelderblom H. Pneumothorax as adverse event in patients with lung metastases of soft tissue sarcoma treated with pazopanib: a single reference centre case series. Clin Sarcoma Res. 2014;4:14. doi: 10.1186/2045-3329-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Jain L, Woo S, Gardner ER, Dahut WL, Kohn EC, Kummar S, et al. Population pharmacokinetic analysis of sorafenib in patients with solid tumours. Br J Clin Pharmacol. 2011;72(2):294–305. doi: 10.1111/j.1365-2125.2011.03963.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Horiuchi-Yamamoto Y, Gemma A, Taniguchi H, Inoue Y, Sakai F, Johkoh T, et al. Drug-induced lung injury associated with sorafenib: analysis of all-patient post-marketing surveillance in Japan. Int J Clin Oncol. 2013;18(4):743–749. doi: 10.1007/s10147-012-0438-0. [DOI] [PubMed] [Google Scholar]
- 229.Goodman VL, Rock EP, Dagher R, Ramchandani RP, Abraham S, Gobburu JV, et al. Approval summary: sunitinib for the treatment of imatinib refractory or intolerant gastrointestinal stromal tumors and advanced renal cell carcinoma. Clin Cancer Res. 2007;13(5):1367–1373. doi: 10.1158/1078-0432.CCR-06-2328. [DOI] [PubMed] [Google Scholar]
- 230.Rixe O, Bukowski RM, Michaelson MD, Wilding G, Hudes GR, Bolte O, et al. Axitinib treatment in patients with cytokine-refractory metastatic renal-cell cancer: a phase II study. Lancet Oncol. 2007;8(11):975–984. doi: 10.1016/S1470-2045(07)70285-1. [DOI] [PubMed] [Google Scholar]
- 231.Thornton K, Kim G, Maher VE, Chattopadhyay S, Tang S, Moon YJ, et al. Vandetanib for the treatment of symptomatic or progressive medullary thyroid cancer in patients with unresectable locally advanced or metastatic disease: U.S. Food and Drug Administration drug approval summary. Clin Cancer Res. 2012;18(14):3722–3730. doi: 10.1158/1078-0432.CCR-12-0411. [DOI] [PubMed] [Google Scholar]
- 232.Hotta K, Ueyama J, Tatsumi Y, Tsukiyama I, Sugiura Y, Saito H, et al. Lack of Contribution of Multidrug Resistance-associated Protein and Organic Anion-transporting Polypeptide to Pharmacokinetics of Regorafenib, a Novel Multi-Kinase Inhibitor, in Rats. Anticancer Res. 2015;35(9):4681–4689. [PubMed] [Google Scholar]
- 233.Scheers E, Leclercq L, de Jong J, Bode N, Bockx M, Laenen A, et al. Absorption, metabolism, and excretion of oral (1)(4)C radiolabeled ibrutinib: an open-label, phase I, single-dose study in healthy men. Drug Metab Dispos. 2015;43(2):289–297. doi: 10.1124/dmd.114.060061. [DOI] [PubMed] [Google Scholar]
- 234.Wu H, Wang A, Zhang W, Wang B, Chen C, Wang W, et al. Ibrutinib selectively and irreversibly targets EGFR (L858R, Del19) mutant but is moderately resistant to EGFR (T790M) mutant NSCLC Cells. Oncotarget. 2015;6(31):31313–31322. doi: 10.18632/oncotarget.5182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Gu Y, Huang B, Yang Y, Qi M, Lu G, Xia D, et al. Ibrutinib Exacerbates Bleomycin-Induced Pulmonary Fibrosis via Promoting Inflammation. Inflammation. 2018;41(3):904–913. doi: 10.1007/s10753-018-0745-3. [DOI] [PubMed] [Google Scholar]
- 236.Beaver JA, Amiri-Kordestani L, Charlab R, Chen W, Palmby T, Tilley A, et al. FDA Approval: Palbociclib for the Treatment of Postmenopausal Patients with Estrogen Receptor-Positive, HER2-Negative Metastatic Breast Cancer. Clin Cancer Res. 2015;21(21):4760–4766. doi: 10.1158/1078-0432.CCR-15-1185. [DOI] [PubMed] [Google Scholar]
- 237.Messmann RA, Ullmann CD, Lahusen T, Kalehua A, Wasfy J, Melillo G, et al. Flavopiridol-related proinflammatory syndrome is associated with induction of interleukin-6. Clin Cancer Res. 2003;9(2):562–570. [PubMed] [Google Scholar]
- 238.Pellegrino B, Facchinetti F, Bordi P, Silva M, Gnetti L, Tiseo M. Lung Toxicity in Non-Small-Cell Lung Cancer Patients Exposed to ALK Inhibitors: Report of a Peculiar Case and Systematic Review of the Literature. Clin Lung Cancer. 2018;19(2):e151–ee61. doi: 10.1016/j.cllc.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 239.Kassem L, Shohdy KS, Lasheen S, Abdel-Rahman O, Ali A, Abdel-Malek RR. Safety issues with the ALK inhibitors in the treatment of NSCLC: A systematic review. Crit Rev Oncol Hematol. 2019;134:56–64. doi: 10.1016/j.critrevonc.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 240.Bender L, Meyer G, Quoix E, Mennecier B. Ceritinib-related interstitial lung disease improving after treatment cessation without recurrence under either crizotinib or brigatinib: a case report. Ann Transl Med. 2019;7(5):106. doi: 10.21037/atm.2019.01.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Wind S, Schmid U, Freiwald M, Marzin K, Lotz R, Ebner T, et al. Clinical Pharmacokinetics and Pharmacodynamics of Nintedanib. Clin Pharmacokinet. 2019;58(9):1131–1147. doi: 10.1007/s40262-019-00766-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Corte T, Bonella F, Crestani B, Demedts MG, Richeldi L, Coeck C, et al. Safety, tolerability and appropriate use of nintedanib in idiopathic pulmonary fibrosis. Respir Res. 2015;16:116. doi: 10.1186/s12931-015-0276-5. [DOI] [PMC free article] [PubMed] [Google Scholar]