Abstract
Objectives:
To document the prevalence and patient profiles of mental health concerns in patients with peripheral artery disease (PAD) seen in the vascular specialty setting.
Methods:
In a cohort of 1275 patients presenting to 16 specialty clinics with new or worsening claudication, symptoms of depression, anxiety, and stress were quantified in 957 patients. The Patient Health Questionnaire-8 (PHQ-8), Generalized Anxiety Disorder scale-2 (GAD-2), and Perceived Stress Scale-4 (PSS-4) were assessed for mental health concerns at the initial PAD work-up and repeated 12 months later. PHQ-8 ≥ 10, GAD-2 ≥ 3 and PSS-4 ≥ 6 were considered significant for depression, anxiety and stress respectively. Patient characteristics were compared in groups divided by presence of 0, 1, 2 or all 3 mental health concerns.
Results:
On the initial office visit, 336/957 (35%) of patients had high levels of at least one of the three mental health concerns. At both baseline and 12 months, high levels of perceived stress were most often reported (28.7% and 17.5% respectively), followed by symptoms of depression (14.1% and 8.9%) and then anxiety (8.3% and 5.7%). Patients with mental health concerns were more often female, younger, had more financial strain, less social support, and worse perceived health status.
Conclusions:
Mental health concerns, particularly stress, are highly prevalent in patients with PAD, especially upon first presenting with new or worsening symptoms. The role of stress and how it may impede successful PAD management and impact subsequent outcomes warrants further investigation.
Keywords: Anxiety, Depression, Perceived stress, Vascular disease
1. Introduction
Peripheral artery disease (PAD) is a highly prevalent condition affecting 8.5 million people in the United States alone [1]. PAD patients experience debilitating symptoms such as intermittent claudication and complications that can lead to undesirable outcomes, including amputation. The pain and complications severely affect patients' functioning and quality of life [2]. These patients tend to have additional co-morbid illnesses, such as hypertension and diabetes, and are at increased risk for myocardial infarction, stroke and death. Besides the high disease burden and physical limitations, patients may be at increased risk for mental distress [1,3-4].
The most commonly studied mental health burden in patients with PAD has been depression [1]. Studies documenting the depressive burden in PAD, however, differ greatly in their methodological approach and their estimates of depressive symptoms associated with PAD. Individuals in the general population who are of the age cohort typically affected by PAD have a depression prevalence of 5.4% [5]. The few studies documenting the prevalence of depression in PAD patients have reported a broad range (between 3 and 48%) which is much higher than in the general population [1]. In addition, the generalizability of the selected clinical populations and variability in the methods used to estimate the prevalence of depressive symptoms have further complicated estimates of the prevalence of this problem in the PAD population.
Moreover, the literature addressing other mental health concerns in this patient population is extremely limited. An isolated study suggests that the prevalence of anxiety is 29% [4], and exploratory studies have documented a potential association between stress and adverse health status in PAD [6]. Thus, despite preliminary evidence of a substantial mental health burden in patients with PAD, no systematic effort has been undertaken to document a broad range of mental health concerns among a cohort of patients seeking specialty vascular care when experiencing active symptoms of PAD. Similarly, there are no insights into the longitudinal nature of these symptoms among patients being actively treated for their PAD.
To address these gaps in knowledge, we used the Patient-centered Outcomes Related to Treatment practices in peripheral Arterial disease: Investigating Trajectories (PORTRAIT) Registry [7], to (1) document the prevalence of depression, anxiety, and perceived stress as well as the degree to which these concerns overlap in patients with PAD around the time of their diagnostic work-up, (2) examine changes in the prevalence of mental health concerns in the year following their diagnosis and treatment and (3) identify patient factors associated with experiencing one or more of these mental health concerns. Understanding the scope of these concerns is important to achieve successful chronic disease management that treats the total patient, as opposed to just their peripheral atherosclerotic disease.
2. Methods
2.1. Study population
PORTRAIT is a multicenter, international prospective registry that enrolled 1275 patients with new or worsening symptoms of PAD presenting to 16 PAD specialty clinics across the US, Netherlands and Australia from June 2011 to December 2015. Study details have been described elsewhere [7]. Briefly, consecutive patients age ≥ 18 presenting with new-onset or recent exacerbation of exertional leg symptoms and a resting ankle-brachial index (ABI) of ≤0.90 or a significant drop in post-exercise ankle pressure of ≥20 mmHg were included. Patients with non-compressible ankle-brachial indices (ABI ≥ 1.30), critical limb ischemia, revascularization of the ipsilateral leg with the symptoms in the 12 months prior to the visit, or inability to provide informed consent were excluded.
Information regarding patients' socioeconomic, psychosocial, and health status as well as symptoms and cardiovascular lifestyle factors were obtained by a standardized interview at the initial visit. Demographic information, medical history, co-morbidities, and PAD diagnostic information were abstracted from their medical records. Follow-up phone interviews gathered information about health and lifestyle status at 3, 6, and 12 months. All study participants provided informed consent; as per study protocol, informed consent could be obtained in writing or over the phone. For the patients included in this study, 65.7% (n = 629) were consented in writing and 34.3% (n = 328) over the phone. IRB approval was obtained from all participating centers.
2.2. Assessment of mental health concerns
Patients were considered to have high levels of depressive symptoms if they had a score of ≥10 on the Patient Health Questionnaire-8 (PHQ-8) [8-9]. This cutoff has both a sensitivity and specificity of 88% in detecting patients with major depressive disorder and has detected a similar prevalence of depression in the general population compared with the diagnostic algorithm in the Diagnostic and Statistical Manual of Mental Disorders IV [8,9]. The PHQ-8 is a modified version of the PHQ-9, which has previously been used successfully in PAD patients [10]. Additionally, prior studies in both the general population and in patients with coronary artery disease (CAD) have shown that these two tools have very comparable performance despite the elimination of item 9 inquiring about passive thoughts of death and active thoughts of self-harm to assess suicide risk [11,12]. The PHQ-8 consists of 8 items on a Likert scale addressing mood and psychomotor symptoms and asks patients to recall symptoms over the past two weeks. Scores range from 0 to 24 with higher scores indicative of more severe depressive symptoms.
Generalized anxiety was measured by the Generalized Anxiety Disorder scale-2 (GAD-2). Scoring ≥3 on the GAD-2 indicates high levels of anxiety symptoms with a sensitivity and specificity of 76% and 81%, respectively [13,14]. The screening tool consists of two items assessing symptoms of anxiety, including nervousness and worrying, on a three-point Likert scale. Patients recall symptoms over the past two weeks, and scores range from 0 to 6.
Perceived stress was measured by the Perceived Stress Scale-4 (PSS-4). The PSS-4 consists of four items scored on a 5-point Likert scale evaluating a patient's sense of control and confidence in handling stressful situations over the past month. The measure is reliable and valid in a variety of settings. Scores range from 0 to 16, but there is no established cut-off to screen for adverse levels of stress. Instead, patients' scores are compared to a normative value, and higher scores are associated with stress exceeding a patient's ability to cope. For example, Warttig, et al. found the normative score of an English population was six [15]. A score of ≥6 was also previously used to accurately depict post-myocardial infarction patients afflicted by moderate/high perceived stress and predicted worse patient outcomes [16]. Thus, in keeping with prior research, we used a score of ≥6 to describe patients with stress levels that were higher than the normative data.
2.3. Other measures
The EQ5D is a standardized instrument for assessing generic health status and has been validated in a wide range of health conditions. It consists of a descriptive system and a Visual Analog Scale (VAS). The descriptive system addresses five domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Patients rank their state of health on a five-point Likert scale ranging from no problems to extreme problems in respect to each of the five domains. On the VAS, respondents grade their health status from 0 (worst possible health status) to 100 (best possible) [17].
The Peripheral Artery Questionnaire (PAQ) is a 20-item questionnaire developed as a disease-specific measure of health status in PAD [18]. The items address physical limitation, symptoms, social function, treatment satisfaction, and quality of life. Patients respond to each question based on how their symptoms of PAD have limited them over the past four weeks. Each question is answered on a Likert scale with lower scores indicating worse quality of life, physical functioning, and symptoms. Combining the scores for each domain can derive a summary score. The tool is valid, reliable, and responsive in patients with PAD [18].
The Enriched Social Support Index (ESSI) is a 7-item self-report tool used to assess social support, with higher scores indicating greater social support. It has previously been determined to be reliable and valid in patients with atherosclerotic disease [19].
2.4. Statistical analysis
We calculated the proportion of patients experiencing high levels of depressive symptoms, anxiety symptoms, and perceived stress at the time of their initial presentation for treatment of new-onset or a recent exacerbation of their PAD. Additionally, the proportion of mean scores for each screening test in patients experiencing two and three mental health concerns and mean scores for each screening test were determined. To understand the persistence of these symptoms, we also determined the proportion of patients with high levels of each mental health concern and with one, two, and three mental health concerns a year after their initial presentation. We examined changes in the prevalence of mental health concerns over this period using the Chi square test to determine statistical significance. We used the McNemar's test to evaluate change from baseline to 12 months in the proportion of patients who had mental health concerns.
Baseline patient and disease characteristics were compared among patients experiencing zero, one, two, or all three mental health concerns at their initial visit and at 12 month later using linear trend tests for continuous variables and Mantel-Haenszel trend tests for categorical variables. Patient and disease characteristics associated with higher scores on the PHQ-8, GAD-2, and PSS-4 were determined for both baseline and 12-month follow up using linear trend test for continuous variables and Mantel-Haenszel trend test for categorical variables.
Ordinal regression models were created for baseline and 12 months to determine the predictors of having zero, one, two or all three mental health concerns. Age, sex, race, education status, financial strain, ABI value, bilateral disease, baseline PAQ summary score, ESSI Social Support Score, and history of CAD, diabetes, stroke, heart failure, and sleep apnea were included in the models.
As part of patient profiling, we abstracted the proportion of patients on pharmacologic treatment for depression or anxiety at baseline and 12 months, and the proportion of patients newly referred to counselling following their baseline visit.
All statistical analyses were performed using SAS version 9.4 software (SAS Institute, Inc., Cary, NC). Two-sided p-values less than 0.05 were considered statistically significant.
2.5. Missing data
Only those patients that completed mental health screening both at baseline and 12 months follow-up were included in the analysis. An overview of excluded patients and the analytic cohort is presented in Fig. 1. Our cohort consisted of 957 (75%) of the 1275 enrolled patients. A total of 318 patients had either missing baseline or 12-month mental health screening and were excluded from the analysis: 60 were missing baseline screening and 258 completed the screening assessments for mental health concerns at baseline but not at 12 months. Overall, patients excluded from the analysis were more likely to be smokers and had lower scores on the PAQ compared with those who did; the patient populations were otherwise similar (see Supplemental Table 1). Among the patients who completed screening at baseline but not at 12 months, the percentage screening positive for each mental health concern at baseline was higher compared with those who completed 12-month screening (see Supplemental Table 2).
Fig. 1.
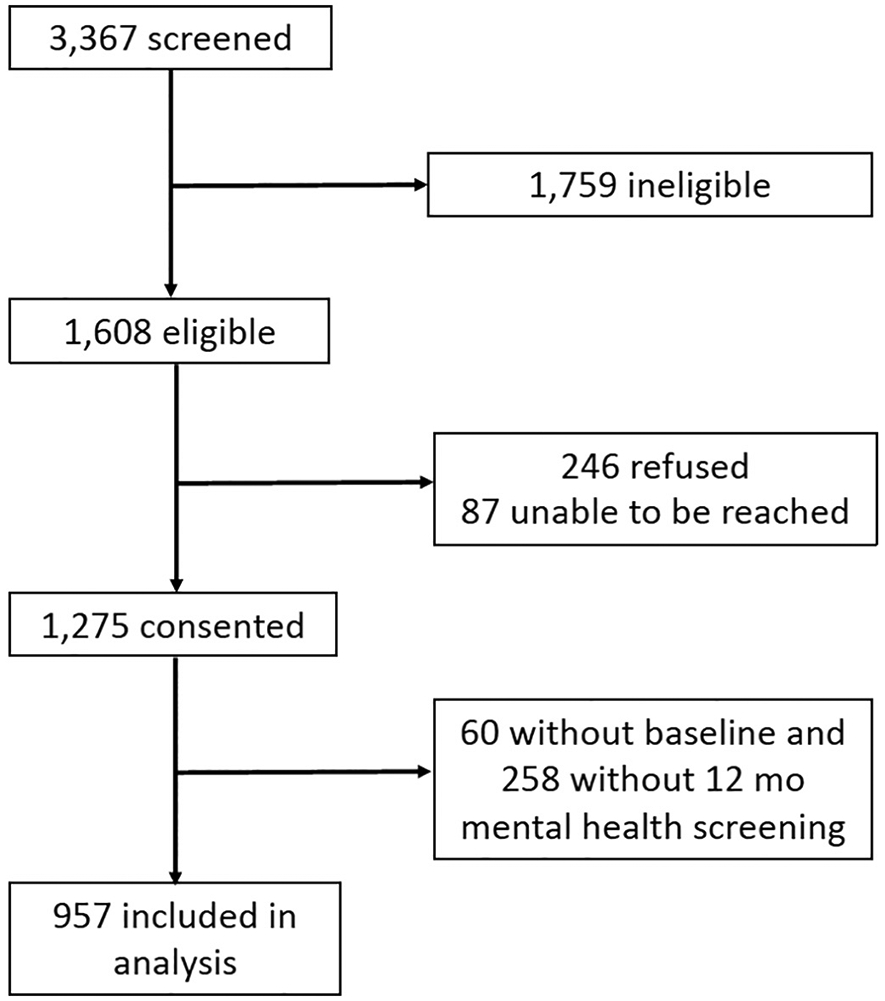
Consort diagram describing patients included in this study.
3. Results
Overall, 957 patients completed screening for mental health concerns at baseline and at 12 months. Mean age was 67.6 ± 9.2 years; 63.4% were male. Approximately half of the patients were presenting with new-onset PAD symptoms (53.3%) and half with an exacerbation of PAD symptoms (46.7%). Mean ABI was 0.7 ± 0.2 (Supplemental Table 1).
At baseline, symptoms of anxiety (8.3%) were the least prevalent mental health concern followed by depressive symptoms (14.1%); however, around one-third of patients (28.7%) had elevated perceived stress at presentation. Although the overall levels of mental health concerns decreased over the course of 12 months, 8.9%, 5.7%, and 17.5% still had high levels of depressive symptoms, anxiety, and perceived stress at 12 months (Table 1).
Table 1.
Mental health concerns at baseline vs 12 months.
| Baseline | 12 Months | P value | |
|---|---|---|---|
| Individual mental health concerns | |||
| Depression | 135 (14.1%) | 85 (8.9%) | < 0.001 |
| Anxiety | 79 (8.3%) | 55 (5.7%) | 0.02 |
| Perceived stress | 275 (28.7%) | 167 (17.5%) | < 0.001 |
| By number of mental health concerns | |||
| One | 223 (23.3%) | 133 (13.9%) | |
| Two | 73 (7.6%) | 42 (4.4%) | |
| Three | 40 (4.2%) | 30 (3.1%) |
More than a third (n = 336, 35%) of patients presented to their initial visit with high levels of at least one of the mental health concerns; 7.6% (n = 73) had two concerns, and there were 4.2% (n = 40) with all three.
We highlight patient characteristics and co-morbidities that are clinically and statistically significant as well as consistent with the prior literature and a basis for possible future intervention. At baseline, patients with more mental health concerns were younger, female, non-Caucasian, and from the United States. These patients were more often presenting with an exacerbation of PAD symptoms and had more proximal distribution of their claudication pain. They had more financial strain, less social support (measured by the ESSI Social Support Score), worse quality of life (measured by the PAQ), and worse perceived health status (measured by the EQ5D). These patients were also more likely to suffer from co-morbid CAD, heart failure, and sleep apnea (Table 2). Baseline patient characteristics for each mental health concern are found in Supplementary Tables 3, 4, and 5.
Table 2.
Baseline characteristics of the study population according to number of mental health concerns at the initial visit.
| Number of mental health concerns at Baseline | P-Value | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||
| n = 621 | n = 223 | n = 73 | n = 40 | ||
| Demographics | |||||
| Age | 68.6 ± 9.1 | 67.3 ± 8.9 | 62.9 ± 8.9 | 61.7 ± 9.4 | < 0.001 |
| Male Gender | 414 (66.7%) | 135 (60.5%) | 43 (58.9%) | 15 (37.5%) | < 0.001 |
| Caucasian | 537 (86.5%) | 167 (74.9%) | 54 (74.0%) | 34 (85.0%) | 0.003 |
| Country | 0.003 | ||||
| (1) USA | 345 (55.6%) | 153 (68.6%) | 53 (72.6%) | 32 (80.0%) | |
| (2) Netherlands | 235 (37.8%) | 46 (20.6%) | 12 (16.4%) | 5 (12.5%) | |
| (3) Australia | 41 (6.6%) | 24 (10.8%) | 8 (11.0%) | 3 (7.5%) | |
| Smoke status | 0.16 | ||||
| (1) Never | 55 (8.9%) | 32 (14.3%) | 8 (11.0%) | 2 (5.0%) | |
| (2) Former | 352 (56.8%) | 115 (51.6%) | 29 (39.7%) | 20 (50.0%) | |
| (3) Current | 213 (34.4%) | 76 (34.1%) | 36 (49.3%) | 18 (45.0%) | |
| Insured | 618 (99.5%) | 223 (100%) | 71 (97.3%) | 39 (97.5%) | 0.046 |
| Work for pay | 58 (36.9%) | 21 (40.4%) | 11 (68.8%) | 3 (33.3%) | 0.18 |
| Finances at end of month | < 0.001 | ||||
| (1) Some money leftover | 384 (63.5%) | 102 (47.0%) | 23 (32.9%) | 11 (29.7%) | |
| (2) Just enough to make ends meet | 190 (31.4%) | 78 (35.9%) | 36 (51.4%) | 17 (45.9%) | |
| (3) Not enough to make ends meet | 31 (5.1%) | 37 (17.1%) | 11 (15.7%) | 9 (24.3%) | |
| PAD characteristics | |||||
| Complaint | 0.033 | ||||
| (1) New-onset | 360 (58.0%) | 88 (39.5%) | 40 (54.8%) | 22 (55.0%) | |
| (2) Exacerbation | 261 (42.0%) | 135 (60.5%) | 33 (45.2%) | 18 (45.0%) | |
| Duration of pain | 0.11 | ||||
| (1) < 1 Month | 16 (3.0%) | 4 (2.1%) | 0 (0.0%) | 1 (2.8%) | |
| (2) 1–6 Months | 169 (32.1%) | 53 (27.5%) | 16 (25.4%) | 7 (19.4%) | |
| (3) 7–12 Months | 87 (16.5%) | 28 (14.5%) | 17 (27.0%) | 11 (30.6%) | |
| (4) > 12 Months | 254 (48.3%) | 108 (56.0%) | 30 (47.6%) | 17 (47.2%) | |
| Symptomatic leg | 0.72 | ||||
| (1) Right leg | 151 (24.3%) | 59 (26.5%) | 17 (23.3%) | 12 (30.0%) | |
| (2) Left leg | 173 (27.9%) | 42 (18.8%) | 18 (24.7%) | 8 (20.0%) | |
| (3) Both legs | 297 (47.8%) | 122 (54.7%) | 38 (52.1%) | 20 (50.0%) | |
| Claudication | 618 (99.5%) | 223 (100.0%) | 73 (100.0%) | 39 (97.5%) | 0.55 |
| Location of highest claudication | 0.015 | ||||
| (1) Buttock | 99 (16.0%) | 40 (17.9%) | 13 (17.8%) | 11 (28.2%) | |
| (2) Hip | 61 (9.9%) | 13 (5.8%) | 8 (11.0%) | 5 (12.8%) | |
| (3) Thigh | 85 (13.8%) | 34 (15.2%) | 12 (16.4%) | 7 (17.9%) | |
| (4) Calf | 317 (51.3%) | 126 (56.5%) | 34 (46.6%) | 15 (38.5%) | |
| (5) Foot | 9 (1.5%) | 4 (1.8%) | 1 (1.4%) | 1 (2.6%) | |
| (6) Other | 47 (7.6%) | 6 (2.7%) | 5 (6.8%) | 0 (0.0%) | |
| Rutherford category | < 0.001 | ||||
| (1) Mild claudication | 157 (25.6%) | 43 (19.4%) | 16 (21.9%) | 3 (7.9%) | |
| (2) Moderate claudication | 313 (51.1%) | 103 (46.4%) | 30 (41.1%) | 21 (55.3%) | |
| (3) Severe claudication | 143 (23.3%) | 76 (34.2%) | 27 (37.0%) | 14 (36.8%) | |
| Lesion Site | 0.69 | ||||
| (1) Proximal | 176 (28.5%) | 57 (25.8%) | 20 (27.4%) | 11 (28.2%) | |
| (2) Distal | 177 (28.6%) | 76 (34.4%) | 19 (26.0%) | 10 (25.6%) | |
| (3) Both | 265 (42.9%) | 88 (39.8%) | 34 (46.6%) | 18 (46.2%) | |
| ABI | 0.67 ± 0.18 | 0.64 ± 0.19 | 0.67 ± 0.20 | 0.73 ± 0.21 | 0.030 |
| Co-morbidities | |||||
| Hypertension | 485 (78.1%) | 194 (87.0%) | 63 (86.3%) | 30 (75.0%) | 0.12 |
| Dyslipidemia | 478 (77.0%) | 184 (82.5%) | 60 (82.2%) | 32 (80.0%) | 0.15 |
| Diabetes | 191 (30.8%) | 76 (34.1%) | 31 (42.5%) | 14 (35.0%) | 0.08 |
| TIA/CVA | 63 (10.1%) | 35 (15.7%) | 8 (11.0%) | 4 (10.0%) | 0.39 |
| CAD | 268 (43.2%) | 101 (45.3%) | 34 (46.6%) | 26 (65.0%) | 0.025 |
| Congestive heart failure | 51 (8.2%) | 25 (11.2%) | 10 (13.7%) | 6 (15.0%) | 0.030 |
| Chronic kidney disease | 62 (10.0%) | 25 (11.2%) | 8 (11.0%) | 6 (15.0%) | 0.34 |
| Chronic lung disease | 99 (15.9%) | 33 (14.8%) | 15 (20.5%) | 8 (20.0%) | 0.40 |
| Sleep apnea | 40 (6.4%) | 23 (10.3%) | 9 (12.3%) | 4 (10.0%) | 0.036 |
| Osteoarthritis (hip or knee) | 57 (9.2%) | 14 (6.3%) | 9 (12.3%) | 4 (10.0%) | 0.88 |
| Chronic back pain | 83 (13.4%) | 35 (15.7%) | 14 (19.2%) | 6 (15.0%) | 0.23 |
| History of depression | 19 (3.1%) | 9 (4.0%) | 5 (6.8%) | 1 (2.5%) | 0.32 |
| Health Status | |||||
| EQ5D: Score your health today (BL) | 70.6 ± 16.9 | 63.6 ± 18.6 | 50.8 ± 20.4 | 53.8 ± 22.1 | < 0.001 |
| EQ5D: Score your health today (12 M) | 74.7 ± 36.4 | 68.3 ± 19.4 | 57.8 ± 17.7 | 58.2 ± 19.9 | < 0.001 |
| ESSI Social Support Score (BL) | 23.1 ± 3.5 | 21.1 ± 5.0 | 19.9 ± 5.9 | 18.5 ± 6.9 | < 0.001 |
| PAQ: Quality of life (BL) | 58.3 ± 23.2 | 45.2 ± 26.2 | 28.4 ± 18.5 | 20.2 ± 16.7 | < 0.001 |
| PAQ: Quality of life (12 M) | 77.3 ± 24.6 | 66.9 ± 28.5 | 53.8 ± 31.0 | 50.2 ± 26.9 | < 0.001 |
| PAQ: Summary (BL) | 55.2 ± 19.3 | 46.2 ± 21.5 | 29.9 ± 18.9 | 23.9 ± 15.9 | < 0.001 |
| PAQ: Summary (12 M) | 75.1 ± 23.0 | 66.2 ± 26.4 | 53.3 ± 28.1 | 49.5 ± 25.9 | < 0.001 |
| PAQ: Physical limitation (BL) | 43.2 ± 26.3 | 34.9 ± 25.0 | 23.0 ± 24.5 | 22.3 ± 18.0 | < 0.001 |
| PAQ: Physical limitation (12 M) | 72.7 ± 29.0 | 64.9 ± 32.5 | 63.5 ± 32.5 | 44.8 ± 31.6 | < 0.001 |
| PAQ: Symptoms (BL) | 48.2 ± 21.2 | 42.8 ± 23.5 | 28.3 ± 21.6 | 25.6 ± 20.3 | < 0.001 |
| PAQ: Symptoms (12 M) | 66.9 ± 28.5 | 58.5 ± 29.9 | 44.2 ± 29.7 | 42.6 ± 29.2 | < 0.001 |
| PAQ: Social limitation (BL) | 70.7 ± 25.9 | 59.5 ± 30.7 | 38.8 ± 30.7 | 29.4 ± 23.9 | < 0.001 |
| PAQ: Social limitation (12 M) | 86.5 ± 21.7 | 80.1 ± 26.2 | 68.4 ± 30.5 | 65.2 ± 31.4 | < 0.001 |
ABI = ankle brachial index, TIA = transient ischemic attack, CVA = cerebral vascular accident, CAD = coronary artery disease, ESSI = Enriched Social Support Index, PAQ = Peripheral Artery Questionnaire, BL = baseline, 12 M = 12 months.
At 12 months follow-up, 21.4% of patients had at least one mental health concern; 4.4% had two concerns and 3.1% had all three (Fig. 2). Patients with more mental health concerns at 12 months were younger, non-Caucasian, smokers, had co-morbid CVA or TIA, diabetes, and CAD, and had a history of depression. They had bilateral disease, moderate claudication symptoms on the Rutherford scale, and had higher ABIs. These patients also had more financial strain, less social support, and worse quality of life and perceived health status (Table 3). Younger age, more financial strain, less social support, and poorer quality of life and perceived health status were associated with mental health concerns at both baseline and 12-month follow-up. For patient characteristics at 12 months associated with each individual mental health concern see Supplementary Tables 6, 7, and 8.
Table 3.
Characteristics of the study population according to number of mental health concerns at 12 months of follow up.
| Number of mental health concerns at 12 months | P-Value | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||
| n = 752 | n = 133 | n = 42 | n = 30 | ||
| Demographics | |||||
| Age | 68.2 ± 8.8 | 67.0 ± 10.3 | 63.9 ± 10.0 | 59.9 ± 8.0 | < 0.001 |
| Male Gender | 486 (64.6%) | 80 (60.2%) | 23 (54.8%) | 18 (60.0%) | 0.16 |
| Race: White/Caucasian | 639 (85.0%) | 103 (77.4%) | 30 (71.4%) | 20 (66.7%) | < 0.001 |
| Country | 0.50 | ||||
| (1) USA | 448 (59.6%) | 80 (60.2%) | 29 (69.0%) | 26 (86.7%) | |
| (2) Netherlands | 262 (34.8%) | 27 (20.3%) | 7 (16.7%) | 2 (6.7%) | |
| (3) Australia | 42 (5.6%) | 26 (19.5%) | 6 (14.3%) | 2 (6.7%) | |
| Smoke status | < 0.001 | ||||
| (1) Never | 79 (10.5%) | 14 (10.5%) | 3 (7.1%) | 1 (3.3%) | |
| (2) Former | 425 (56.6%) | 62 (46.6%) | 18 (42.9%) | 11 (36.7%) | |
| (3) Current | 247 (32.9%) | 57 (42.9%) | 21 (50.0%) | 18 (60.0%) | |
| Insured | 748 (99.5%) | 132 (99.2%) | 42 (100%) | 29 (96.7%) | 0.23 |
| Work for pay | 72 (38.1%) | 15 (48.4%) | 3 (33.3%) | 3 (60.0%) | 0.34 |
| Finances at end of month | < 0.001 | ||||
| (1) Some money leftover | 441 (60.4%) | 60 (46.9%) | 13 (31.7%) | 6 (20.0%) | |
| (2) Just enough to make ends meet | 236 (32.3%) | 51 (39.8%) | 22 (53.7%) | 12 (40.0%) | |
| (3) Not enough to make ends meet | 53 (7.3%) | 17 (13.3%) | 6 (14.6%) | 12 (40.0%) | |
| PAD Characteristics | |||||
| Complaint | 0.74 | ||||
| (1) New-onset | 404 (53.7%) | 68 (51.1%) | 22 (52.4%) | 16 (53.3%) | |
| (2) Exacerbation | 348 (46.3%) | 65 (48.9%) | 20 (47.6%) | 14 (46.7%) | |
| Duration of pain | 0.51 | ||||
| (1) < 1 Month | 19 (3.0%) | 1 (0.9%) | 0 (0.0%) | 1 (3.7%) | |
| (2) 1–6 Months | 192 (30.0%) | 37 (32.2%) | 9 (24.3%) | 7 (25.9%) | |
| (3) 7–12 Months | 110 (17.2%) | 18 (15.7%) | 10 (27.0%) | 5 (18.5%) | |
| (4) > 12 Months | 318 (49.8%) | 59 (51.3%) | 18 (48.6%) | 14 (51.9%) | |
| Symptomatic leg | 0.05 | ||||
| (1) Right leg | 193 (25.7%) | 33 (24.8%) | 5 (11.9%) | 8 (26.7%) | |
| (2) Left leg | 196 (26.1%) | 30 (22.6%) | 13 (31.0%) | 2 (6.7%) | |
| (3) Both legs | 363 (48.3%) | 70 (52.6%) | 24 (57.1%) | 20 (66.7%) | |
| Claudication | 748 (99.5%) | 133 (100.0%) | 42 (100.0%) | 30 (100.0%) | 0.36 |
| Location of highest claudication | 0.11 | ||||
| (1) Buttock | 124 (16.6%) | 20 (15.0%) | 13 (31.0%) | 6 (20.0%) | |
| (2) Hip | 71 (9.5%) | 15 (11.3%) | 1 (2.4%) | 0 (0.0%) | |
| (3) Thigh | 99 (13.2%) | 28 (21.1%) | 7 (16.7%) | 4 (13.3%) | |
| (4) Calf | 391 (52.3%) | 62 (46.6%) | 19 (45.2%) | 20 (66.7%) | |
| (5) Foot | 10 (1.3%) | 3 (2.3%) | 2 (4.8%) | 0 (0.0%) | |
| (6) Other | 53 (7.1%) | 5 (3.8%) | 0 (0.0%) | 0 (0.0%) | |
| Rutherford category | 0.039 | ||||
| (1) Mild claudication | 181 (24.4%) | 27 (20.3%) | 6 (14.3%) | 5 (16.7%) | |
| (2) Moderate claudication | 365 (49.3%) | 66 (49.6%) | 20 (47.6%) | 16 (53.3%) | |
| (3) Severe claudication | 195 (26.3%) | 40 (30.1%) | 16 (38.1%) | 9 (30.0%) | |
| Lesion Site | 0.67 | ||||
| (1) Proximal | 210 (28.1%) | 37 (28.0%) | 14 (33.3%) | 3 (10.0%) | |
| (2) Distal | 215 (28.8%) | 41 (31.1%) | 14 (33.3%) | 12 (40.0%) | |
| (3) Both | 322 (43.1%) | 54 (40.9%) | 14 (33.3%) | 15 (50.0%) | |
| ABI | 0.67 ± 0.19 | 0.64 ± 0.20 | 0.67 ± 0.18 | 0.73 ± 0.17 | 0.07 |
| Co-morbidities | |||||
| Hypertension | 603 (80.2%) | 110 (82.7%) | 34 (81.0%) | 25 (83.3%) | 0.53 |
| Dyslipidemia | 589 (78.3%) | 103 (77.4%) | 36 (85.7%) | 26 (86.7%) | 0.21 |
| Diabetes | 236 (31.4%) | 46 (34.6%) | 18 (42.9%) | 12 (40.0%) | 0.08 |
| TIA/CVA | 74 (9.8%) | 24 (18.0%) | 8 (19.0%) | 4 (13.3%) | 0.015 |
| History of CAD | 327 (43.5%) | 59 (44.4%) | 26 (61.9%) | 17 (56.7%) | 0.024 |
| Congestive heart failure | 66 (8.8%) | 18 (13.5%) | 7 (16.7%) | 1 (3.3%) | 0.39 |
| Chronic kidney disease | 75 (10.0%) | 18 (13.5%) | 6 (14.3%) | 2 (6.7%) | 0.59 |
| Chronic lung disease | 117 (15.6%) | 23 (17.3%) | 5 (11.9%) | 10 (33.3%) | 0.10 |
| Sleep apnea | 56 (7.4%) | 12 (9.0%) | 5 (11.9%) | 3 (10.0%) | 0.26 |
| Osteoarthritis (hip or knee) | 63 (8.4%) | 15 (11.3%) | 5 (11.9%) | 1 (3.3%) | 0.86 |
| Chronic back pain | 105 (14.0%) | 21 (15.8%) | 9 (21.4%) | 3 (10.0%) | 0.63 |
| History of depression | 22 (2.9%) | 7 (5.3%) | 3 (7.1%) | 2 (6.7%) | 0.044 |
| Health status | |||||
| EQ5D: Score your health today (BL) | 68.2 ± 18.4 | 65.2 ± 18.7 | 58.1 ± 15.2 | 48.8 ± 22.5 | < 0.001 |
| EQ5D: Score your health today (12 M) | 73.2 ± 16.4 | 68.5 ± 74.0 | 55.3 ± 18.7 | 53.5 ± 18.2 | < 0.001 |
| ESSI Social Support Score (BL) | 22.7 ± 3.9 | 21.0 ± 5.2 | 18.4 ± 6.8 | 19.2 ± 6.2 | < 0.001 |
| PAQ: Quality of life (BL) | 55.2 ± 24.5 | 42.5 ± 25.0 | 28.8 ± 24.0 | 25.8 ± 24.1 | < 0.001 |
| PAQ: Quality of life (12 M) | 77.5 ± 23.8 | 58.4 ± 28.9 | 41.8 ± 28.8 | 34.5 ± 28.1 | < 0.001 |
| PAQ: Summary (BL) | 53.3 ± 20.5 | 41.5 ± 21.2 | 30.3 ± 18.8 | 28.8 ± 18.8 | < 0.001 |
| PAQ: Summary (12 M) | 75.3 ± 22.3 | 58.9 ± 26.4 | 42.3 ± 25.7 | 33.3 ± 25.7 | < 0.001 |
| PAQ: Physical limitation (BL) | 42.3 ± 26.6 | 29.9 ± 22.9 | 21.7 ± 20.1 | 19.0 ± 17.0 | < 0.001 |
| PAQ: Physical limitation (12 M) | 74.0 ± 27.9 | 56.1 ± 33.3 | 39.8 ± 31.9 | 34.7 ± 33.1 | < 0.001 |
| PAQ: Symptoms (BL) | 46.8 ± 21.7 | 39.6 ± 24.3 | 28.9 ± 20.2 | 29.1 ± 24.7 | < 0.001 |
| PAQ: Symptoms (12 M) | 66.4 ± 28.5 | 52.6 ± 30.4 | 38.0 ± 25.7 | 31.2 ± 26.6 | < 0.001 |
| PAQ: Social limitation (BL) | 68.4 ± 28.1 | 52.5 ± 29.3 | 40.2 ± 29.7 | 37.5 ± 27.3 | < 0.001 |
| PAQ: Social limitation (12 M) | 87.6 ± 20.1 | 73.0 ± 27.3 | 55.1 ± 32.5 | 40.2 ± 28.8 | < 0.001 |
ABI = ankle brachial index, TIA = transient ischemic attack, CVA = cerebral vascular accident, CAD = coronary artery disease, ESSI = Enriched Social Support Index, PAQ = Peripheral Artery Questionnaire, BL = baseline, 12 M = 12 months.
Based on the ordinal regression models, younger patients, patients presenting with an exacerbation of PAD symptoms, and those with worse disease-specific health status, less social support, and more financial strain had an increased odds of having more mental health concerns at baseline. Similar results were found at 12-months except that the initial presenting complaint (new onset PAD vs exacerbation) was no longer significant (Supplemental Tables 9 and 10).
Although the overall proportion of patients with each mental health concern decreased, a large proportion of patients with mental health concerns at 12 months were screening positive for the first time: 42.3% for depression (36/85), 67.3% for anxiety (37/55), and 46.7% for perceived stress (78/167; Supplemental Tables 11, 12, and 13).
Prior to the baseline visit, of the patients with at least one mental health concern, only 18.1% were on an antidepressant including a selective serotonin reuptake inhibitor or a selective norepinephrine reuptake inhibitor and 5.4% were on an anxiolytic including a benzodiazepine or non-benzodiazepine anxiolytic such as buspirone or hydroxyzine (Supplemental Table 14). Following a visit in which they screened positive for at least one mental health concern, there was little if any change in the proportion of patients on these medications (18.6% for antidepressants and 4.9% for anxiolytics). Details on the specific classes of medications used are found in Supplemental Table 15. Additionally, referral to counselling after the baseline visit was low: 8.9% (n = 12) of patients with depressive symptoms, 8.9% (n = 7) of patients with anxiety, and 7.6% (n = 21) of patients with high stress.
4. Discussion
While there is certainly a need to aggressively treat the atherosclerotic process among patients with new-onset or recent exacerbations of their PAD, it is also important to recognize that these patients may be suffering from significant mental health concerns associated with the chronic debilitating nature of the disease. In this prospective, multi-center, international cohort study, we found that a third of patients presenting with new or worsening symptoms of PAD also had significant mental health concerns at the time of their baseline presentation. While the majority of these patients were struggling with perceived stress, the rates of depressive symptoms were higher in our patient population than in the general population and similar to those reported in patients with coronary artery disease [1,5]. Additionally, the observed prevalence of anxiety symptoms in our patient population was at the higher end of the reported prevalence rates for the general population [20]. Although the burden of mental health concerns decreased at 12 months, there were still a significant number of patients burdened by mental health concerns, including around half of patients with new mental health concerns at this time.
To our knowledge, this is the first report that has documented the prevalence of increased stress levels in this patient population, and only the second reporting the prevalence of anxiety. In contrast, the prevalence of depression in PAD patients is more commonly reported but varies greatly (3–48%) [1]. The wide range of documented prevalence likely has to do with the variability in tools used to measure depression as well as the subset of patients with PAD studied. Other studies have limited generalizability due to the patient populations selected—single centers, patients with self-reported history of PAD, or patients with a history of CAD or type 2 diabetes or elderly patients. Our prevalence for depressive symptoms is derived from a multicenter, international registry of PAD patients regardless of age or co-morbidities which represents a larger subset of the PAD population.
Our findings extend prior literature in important ways. First, we found that these mental health concerns have a dynamic course with around half of patients screening positive for a new mental health concern at 12 months. Therefore, in addition to screening at baseline, providers need to have continued appreciation of these issues and screen for them on a routine basis as lack of mental health symptoms at baseline does not mean the patient is not at risk of developing a mental health concern subsequently. This is particularly important in patients who have a history of depression as they were more likely to develop mental health concerns at follow up. Additionally, many patients had resolution of their mental health concerns; whether this coincides with their clinical course of PAD and treatment of their PAD is an area of future study. Secondly, despite having a positive screen for a mental health concern, relatively low rates of referral for counselling were noted. Further, there were low rates of prescription for pharmacologic therapy for patients with a positive screen. These findings are consistent with prior findings of low recognition and treatment of mental health concerns in cardiovascular disease and suggests that further action is required.
The high prevalence of perceived stress in patients with PAD is important to acknowledge as smoking cessation, lifestyle changes, and medication adherence are important for treatment of PAD but are difficult to achieve in patients struggling with high levels of stress [21-24]. In a study of 7066 healthy Danish people, those with high stress levels were less likely to quit smoking and more likely to become physically inactive [24]. Additionally, those with high stress were less likely to be financially secure at the end of the month, which may interfere with their ability to pay for treatments and medications not covered by insurance. Our study also underscores that even without a formal diagnosis of a mental health disorder, patients with PAD seem to experience high stress levels that may impact their disease management.
While there has not been any literature documenting the prevalence of perceived stress in a patient population with PAD, prior research has shown that chronic stress contributes to development and progression of cardiovascular disease and cardiovascular death [25-27]. Additionally, post-myocardial infarction patients with moderate-high perceived stress (PSS-4 ≥ 6) had worse health status at one year and higher 2-year mortality [16]. These studies, in addition to our findings, underscore the importance of documenting the high prevalence of perceived stress in the PAD population.
In addition to the high prevalence of stress, both the prevalence of depression and generalized anxiety in this patient population were higher as compared with those without PAD [5,20]. Studies investigating outcomes in PAD patients with co-morbid depression revealed worse functional status, increased risk of revascularization failure, and increased mortality compared to PAD patients without depression [28-33]. The literature on the prevalence and outcomes of PAD patients with co-morbid anxiety is lacking; however, co-morbid anxiety in patients' post-myocardial infarction has been associated with worse quality of life [34-35].
Patients most vulnerable to be dealing with these mental health concerns were younger, female, under more financial strain and were less likely to have social support. Similar associations have been documented in both PAD populations with depression as well as in populations with CAD with depression and with higher levels of perceived stress [1,16,36]. Additionally, at initial presentation, patients with an exacerbation of PAD symptoms had higher odds of having a co-morbid mental health concern, while at the 12-month follow up, those with a history of depression were more likely to have mental health concerns. This suggests to providers who could benefit most from screening for these mental health concerns.
The significant burden of mental health concerns in the PAD population suggests an area for improvement in caring for these patients. Several small studies have already investigated such interventions. Two studies have shown that interventions, a 12-week rehabilitation program and a cognitive-behavioral self-help program, improved mental health concerns in PAD patients [37,38]. Although these studies showed improvement in mental health concerns, they were not designed to demonstrate whether this in turn resulted in improving the outcomes of the patients with these co-morbid conditions. In contrast, a study from Sweden which specifically aimed at mechanisms to ameliorate stress in women with CAD, patients in the treatment group had reduced mortality compared to patients who received usual care [39].
5. Limitations
Our findings should be interpreted in the context of several potential limitations. The PHQ-8, GAD-2, and PSS-4 are screening tests and are not designed to establish a clinical diagnosis. Additionally, these screening tests rely on self-reported measures and patient recall of symptoms over the past two weeks or month; however, our results are consistent with other studies that used patient-reported measures and primary care physician diagnosis to determine prevalence [1]. The PHQ was also recommended by the AHA as one of the screening tests to be used to identify an increased risk of depression in patients with CAD [40]. The PSS-4 does not have an established cutoff; the developers of the tool recommend using a cutoff based on the study population. We used a score of ≥6 as this has been utilized in patients with non-PAD atherosclerotic disease when describing patients with moderate-high stress. While the PORTRAIT registry includes a broad distribution of outpatient practices in the U.S., the Netherlands, and Australia, it may not be generalizable to all practice settings and only includes patients that signed informed consent and exhibited the ability to complete multiple surveys over time. Additionally, the registry enrolled patients presenting with new or worsening symptoms, and therefore, our results are not generalizable to those with a stable disease state. Additionally, while information on baseline medications was collected in the registry, we are unable to say the reason the medication was prescribed, which is important to note as antidepressants and anxiolytics can be prescribed for reasons other than depression and anxiety, respectively. Lastly, while we were able to describe patient characteristics and co-morbidities associated with the presence of mental health concerns, we were unable to describe characteristics that differentiated patients with 0, 1, 2, or 3 mental health concerns because the sample sizes for four groups vary and as the comparator groups (number of comorbid conditions) represent a scale variable, not nominal, the unavoidable interpretation of such analyses would be a “tipping point” inference. As such we did not feel that comparing patients by 0 vs 1, 1 vs 2, etc. mental health concerns would provide further valuable information than did the test of trends in Tables 2 and 3.
6. Conclusion
Mental health concerns, in particular perceived stress, are highly prevalent in patients with PAD, especially upon first presenting with new or worsening symptoms. Given prior work done in cardiac populations, we know that heightened levels of stress may complicate successful disease management and may predispose patients to adverse cardiovascular outcomes. Whether these associations extend to the PAD population warrants further investigation. Regardless, greater awareness of the significant mental health burdens experienced by this at-risk population is needed to successfully provide holistic management.
Supplementary Material
Acknowledgments
Disclosures
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: research reported in this manuscript was partially funded through a Patient-Centered Outcomes Research Institute (PCORI) award (IP2PI000753-01; CE-1304-6677); The Netherlands Organization for Scientific Research (VENI grant no. 916.11.179); and an unrestricted grant from WL Gore & Associates, Inc. (Flagstaff, AZ, USA).
The statements in this manuscript are solely the responsibility of the authors and do not necessarily represent the views of the PCORI, its Board of Governors or Methodology Committee.
All manuscripts for the PORTRAIT study are prepared by independent authors who are not governed by the funding sponsors and are reviewed by an academic publications committee before submission.
The funding organizations and sponsors of the study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Merrill Thomas and Krishna K. Patel are supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number T32HL110837. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Dr. Mena-Hurtado serves as a consultant for Abbott, Boston Scientific, Cardinal Health, COOK, Medtronic, and Bard.
Dr. Smolderen is supported by unrestricted research grants provided by Terumo Corporation, Abbott Vascular, and Boston Scientific.
Dr. Spertus has received grant support from Bayer and serves as a consultant to AstraZeneca, Bayer, Novartis and United Healthcare. He is on the board of directors of Blue Cross Blue Shield of Kansas City and owns the copyright to the PAQ.
Abbreviations:
- PAD
Peripheral Arterial Disease
- CAD
Coronary Artery Disease
- PHQ-8
Patient Health Questionnaire-8
- GAD-2
Generalized Anxiety Disorder scale-2
- PSS-4
Perceived Stress Scale-4
- ABI
Ankle Brachial Index
Footnotes
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychores.2020.109963.
References
- [1].Brostow D, Petrik M, Starosta A, Waldo S, Depression in patients with peripheral arterial disease: a systematic review, Eur. J. Cardiovasc. Nurs. 16 (2017) 181–193, 10.1177/1474515116687222. [DOI] [PubMed] [Google Scholar]
- [2].Regensteiner J, Hiatt W, Coll J, Criqui M, Treat-Jacobson D, McDermott M, et al. , The impact of peripheral arterial disease on health-related quality of life in the peripheral arterial disease awareness, risk, and treatment: new resources for survival (PARTNERS) program, Vasc. Med 13 (2008) 15–24, 10.1177/1358863X07084911. [DOI] [PubMed] [Google Scholar]
- [3].Smolderen K, Aquarius A, De Vries J, Smith O, Hamming J, Denollet J, Depressive symptoms in peripheral arterial disease: a follow-up study on prevalence, stability, and risk factors, J. Affect. Disord 110 (2008) 27–35, 10.1016/j.jad.2007.12.238. [DOI] [PubMed] [Google Scholar]
- [4].Smolderen K, Hoeks S, Pedersen S, Van Domburg R, De Liefde I, Poldermans D, Lower-leg symptoms in peripheral arterial disease are associated with anxiety, depression, and anhedonia, Vasc. Med. 14 (2009) 297–304, 10.1177/1358863X09104658. [DOI] [PubMed] [Google Scholar]
- [5].Pratt LA, Brody DJ. Depression in the U.S. Household Population, 2009–2012 NCHS Data Brief, no 172, CDC/NCHS, National Health and Nutrition Examination Survey, 2009–2012. Hyattsville, MD: National Center for Health Statistics; 2014. https://www.cdc.gov/nchs/data/databriefs/db172.htm [Google Scholar]
- [6].Aquarius AE, De Vries J, Henegouwen DP, Hamming JF, Clinical indicators and psychosocial aspects in peripheral arterial disease, Arch. Surg 141 (2006) 161–166. [DOI] [PubMed] [Google Scholar]
- [7].Smolderen KG, Jones S, Hirsch AT, Beltrame J, Filtridge R, Shishehbor M, et al. , Patient-centered outcomes related to treatment practices in peripheral arterial disease: investigating trajectories (PORTRAIT): overview of design and rationale of an international prospective peripheral arterial disease study, Circ. Cardiovasc. Qual. Outcome 11 (2018), 10.1161/CIRCOUTCOMES.117.003860. [DOI] [PubMed] [Google Scholar]
- [8].Kroenke K, Spitzer RL, Williams JB, The PHQ-9, J. Gen. Intern. Med 16 (2001) 606–613, 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH, The PHQ-8 as a measure of current depression in the general population, J. Affect. Disord. 114 (2009) 163–173, 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- [10].Smolderen KG, Safley DM, House JA, Spertus JA, Marso SP, Percutaneous transluminal angioplasty: association between depressive symptoms and diminished health status benefits, Vasc. Med 16 (2011) 260–266, 10.1177/1358863X11415568. [DOI] [PubMed] [Google Scholar]
- [11].Corson K, Gerrity SM, Dobscha SK, Screening for depression and suicidality in a VA primary care setting: 2 items are better than 1 item, Am. J. Manag. Care (2004) 839–845 11pt2. [PubMed] [Google Scholar]
- [12].Razykov I, Ziegelstein RC, Whooley MA, Thombs BD, The PHQ-9 versus the PHQ-8—is item 9 useful for assessing suicide risk in coronary artery disease patients? Data from the heart and soul study, J. Psychosom. Res 73 (2012) 163–168, 10.1016/j.jpsychores.2012.06.001. [DOI] [PubMed] [Google Scholar]
- [13].Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B, Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection, Ann. Intern. Med 146 (2007) 317–325. [DOI] [PubMed] [Google Scholar]
- [14].Plummer F, Manea L, Trepel D, McMillan D, Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis, Gen. Hosp. Psychiatry 39 (2016) 24–31, 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- [15].Warttig SL, Forshaw MJ, South J, White AK, New, Normative English-Sample Data for the Short-Form Perceived Stress Scale (PSS-4), Journal of Health Psychology 18 (2013) 1617–1628, 10.1177/1359105313508346. [DOI] [PubMed] [Google Scholar]
- [16].Arnold SV, Smolderen KG, Buchanan DM Li Y, Spertus JA, Perceived Stress in Myocardial Infarction: Long-Term Mortality and Health Status Outcomes, J Am Coll Cardiol 60 (2012) 1756–1763, 10.1016/j.jacc.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Balestroni G, Bertolotti G, EuroQol-5D (EQ-5D): an Instrument for Measuring Quality of Life, Monaldi Arch. Chest Dis. 78 (2012) 155–159, 10.4081/monaldi.2012.121. [DOI] [PubMed] [Google Scholar]
- [18].Spertus J, Jones P, Poler S, Rocha-Singh K, The Peripheral Artery Questionnaire: a New Disease-Specific Health Status Measure for Patients with Peripheral Arterial Disease, Am Heart J 147 (2004) 301–308, 10.1016/j.ahj.2003.08.001. [DOI] [PubMed] [Google Scholar]
- [19].Vaglio J Jr, Conrad M, Poston WS, O’Keefe J, Haddock CK, House J, et al. , Testing the Performance of the ENRICHED Social Support Instrument in Cardiac Patients, Health Qual Life Outcomes 2 (2004) 24, 10.1186/1477-7525-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Facts & Statistics, Anxiety and Depression Association of America, ADAA, 2020, adaa.org/about-adaa/press-room/facts-statistics. [Google Scholar]
- [21].Nohlert E, Ohrvik J, Helgason AR, Self-perceived ability to cope with stress and depressive mood without smoking predicts successful smoking cessation 12 months later in a quitline setting: a secondary analysis of a randomized trial, BMC Public Health 18 (2018) 1066, 10.1186/s12889-018-5973-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Chlebowy DO, Batscha C, Kubiak N, Crawford T , Relationships of Depression, Anxiety, and Stress with Adherence to Self-Management Behaviors and Diabetes Measures in African American Adults with Type 2 Diabetes, J Racial Ethn Health Disparities 6 (2018) 71–76, 10.1007/s40615-018-0500-3. [DOI] [PubMed] [Google Scholar]
- [23].Chandler JL, Sox LR, Gunsolley JR, Treiber FA, McGillicuddy JW, Associations Between Medication Nonadherence and Perceived Stress Among Kidney Transplant Recipients, Prog Transplant 27 (2017) 396–397, 10.1177/1526924817732023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rod NH, Gronbaek M, Schnohr P, Prescott E, Kristensen TS, Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study, J Intern Med 266 (2009) 467–475, 10.1111/j.1365-2796.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- [25].Iso H, Date C, Yamamoto A, Toyoshima H, Tanabe N, Kikuchi S, et al. , Perceived Mental Stress and Mortality from Cardiovascular Disease Among Japanese Men and Women: The Japan Collaborative Cohort Study for Evaluation of Cancer Risk Sponsored by Monbusho (JACC Study), Circulation 106 (2002) 1229–1236, 10.1161/01.cir.0000028145.58654.41. [DOI] [PubMed] [Google Scholar]
- [26].KA Matthews BB Gump, Chronic Work Stress and Marital Dissolution Increase Risk of Posttrial Mortality in Men from the Multiple Risk Factor Intervention Trial, Archives of Internal Medicine 162 (2002) 309–315, 10.1001/archinte.162.3.309. [DOI] [PubMed] [Google Scholar]
- [27].Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. , Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study, Lancet 364 (2004) 953–962. [DOI] [PubMed] [Google Scholar]
- [28].Smolderen K, Aquarius A, DeVries J, Smith O, Hamming J, Denollet J, Depressive symptoms in peripheral arterial disease: A follow-up study on prevalence, stability, and risk factors, J Affect Disord 110 (1-2) (2008) 27–35, 10.1016/j.jad.2007.12.238. [DOI] [PubMed] [Google Scholar]
- [29].McDermott MM, Greenland P, Guralnik J, Liu K, Criqui M, Pearce W, et al. , Depressive symptoms and lower extremity functioning in men and women with peripheral arterial disease, J. Gen. Intern. Med. 18 (6) (2003) 461–467, 10.1046/j.1525-1497.2003.20527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].McDermott M, Guralnik J, Tian L, Kibbe M, Ferrucci L, Zhao L, et al. , Incidence and Prognostic Significance of Depressive Symptoms in Peripheral Artery Disease, J Am Heart Assoc 5 (3) (2016) e002959, , 10.1161/JAHA.115.002959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Ruo B, Liu K, Tian L, Tan J, Ferrucci L, Guralnik J, et al. , Persistent Depressive Symptoms and Functional Decline Among Patients With Peripheral Arterial Disease, Psychosom Med 69 (5) (2007) 415–424, 10.1097/PSY.0b013e318063ef5c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Cherr G, Wang J, Zimmerman P, Dosluoglu H, Depression is associated with worse patency and recurrent leg symptoms after lower extremity revascularization, J. Vasc. Surg. 45 (4) (2007) 744–750, 10.1016/j.jvs.2006.11.057. [DOI] [PubMed] [Google Scholar]
- [33].Cherr G, Zimmerman P, Wang J, Dosluoglu H, Patients with Depression are at Increased Risk for Secondary Cardiovascular Events after Lower Extremity Revascularization, J Gen Intern Med 23 (5) (2008) 629–634, 10.1007/s11606-008-0560-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Lane D, Carroll D, Ring C, Beevers DG, Lip GY, Mortality and quality of life 12 months after myocardial infarction: effects of depression and anxiety, Psychosom Med 63 (2001) 221–230. [DOI] [PubMed] [Google Scholar]
- [35].Mayou RA, Gill D, Thompson DR, Day A, Hicks N, Volmink J, et al. , Depression and anxiety as predictors of outcome after myocardial infarction, Psychosom Med 62 (2) (2000) 212–219, 10.1097/00006842-200003000-00011. [DOI] [PubMed] [Google Scholar]
- [36].Huffman JC, Celano CM, Beach SR, Motiwala SR, Januzzi JL, Depression and cardiac disease: epidemiology, mechanisms, and diagnosis, Cardiovasc Psychiatry Neurol 2013 (2013) 1–14, 10.1155/2013/695925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Stauber S, Guera V, Barth J, Schmid JP, Saner H, Znoj H, et al. , Psychosocial Outcome in Cardiovascular Rehabilitation of Peripheral Artery Disease and Coronary Artery Disease Patients, Vasc Med 18 (2013) 257–262, 10.1177/1358863X13505861. [DOI] [PubMed] [Google Scholar]
- [38].Garnefskiz N, Kraaij V, Wijers E, Hamming J, Effects of a Cognitive-Behavioral Self-Help Program on Depressed Mood for People with Peripheral Arterial Disease, J Clin Psychol Med Settings 20 (2012) 186–191, 10.1007/s10880-012-9336-x. [DOI] [PubMed] [Google Scholar]
- [39].Orth-Gomer K, Schneiderman N, Wang HX, Walldin C, Blom M, Jernberg T, Stress reduction prolongs life in women with coronary disease: the Stockholm Women’s Intervention Trial for Coronary Heart Disease (SWITCHD), Circ. Cardiovasc. Qual. Outcome. 2 (2009) 25–32, 10.1161/CIRCOUTCOMES.108.812859. [DOI] [PubMed] [Google Scholar]
- [40].Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, et al. , AHA science advisory depression and coronary heart disease, Circulation 118 (2008) 1768–1775, 10.1161/CIRCULATIONAHA.108.190.76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


